Abstract
Introduction:
The National Comprehensive Cancer Network (NCCN) Best Practices Committee created an Advanced Practice Provider (APP) Workgroup to develop recommendations to support APP roles at NCCN Member Institutions.
Methods:
The Workgroup conducted three surveys to understand APP program structure, staffing models, and professional development opportunities at NCCN Member Institutions.
Results:
The total number of new and follow-up visits a 1.0 APP full-time equivalent conducts per week in shared and independent visits ranged from 11 to 97, with an average of 40 visits per week (n = 39). The type of visits APPs conduct include follow-up shared (47.2%), follow-up independent (46%), new shared (6.5%), and new independent visits (0.5%). Seventy-two percent of respondents utilize a mixed model visit type, with 15% utilizing only independent visits and 13% utilizing only shared visits (n = 39). Of the 95% of centers with APP leads, 100% indicated that leads carry administrative and clinical responsibilities (n = 20); however, results varied with respect to how this time is allocated. Professional development opportunities offered included posters, papers, and presentations (84%), leadership development (57%), research opportunities (52%), writing book chapters (19%), and other professional development activities (12%; n = 422). Twenty percent of APPs indicated that protected time to engage in development opportunities should be offered.
Conclusion:
As evidenced by the variability of the survey results, the field would benefit from developing standards for APPs. There is a lack of information regarding leadership structures to help support APPs, and additional research is needed. Additionally, centers should continuously assess the career-long opportunities needed to maximize the value of oncology APPs.
There is growing concern that oncologists will soon be in short supply in the US, creating a significant problem for cancer centers across the nation. A 2014 study predicts a shortage of 2,258 medical oncologists and radiation oncologists by 2025. Demand is expected to increase by 40% while clinical capacity by these physicians is expected to only increase by 25% (Yang et al., 2014). According to census bureau projections, the number of Americans ages 65 and older is anticipated to double between 2000 and 2030 and likely result in an increase in age-related cancer rates as well as a rise in the number of cancer survivors who will require ongoing monitoring. Further, younger physicians entering the workforce are more likely to cite the need for work-life balance, resulting in less visit capacity (Erikson et al., 2007).
The impending shortage of physicians has prompted increased use of specialized oncology nurse practitioners (NPs) and physician assistants (PAs), collectively referred to as advanced practice providers (APPs; Levy et al., 2013). Both NPs and PAs are capable of enhancing the care of oncology patients and often work together on collaborative teams and practices. Previous studies have found that APPs increase capacity by seeing their own patients, increasing physician productivity, and improving practice flexibility (Hinkel et al., 2010). Moreover, APPs are identified as a way to help ensure coordinated and comprehensive patient care as recommended by the Institute of Medicine (IOM) for improving quality of care (Bruinooge et al., 2018).
As the number of APPs in oncology increases, various leadership structures to help support APPs are also emerging. However, there is no standardization or identified best practices regarding APP leadership structure, staffing, or type of visits (shared vs. independent; Bruinooge et al., 2018; Hinkel et al., 2010; McCorkle et al., 2015; Towle et al., 2011). Additionally, a recent study of burnout and career satisfaction among PAs in oncology indicated that spending less time in direct patient care and more time in administrative activities, a lack of acknowledgement of contributions to patient care and the oncology practice, and deficiencies in teamwork and organizational leadership have led to burnout among PAs (Bruinooge et al., 2018). Having a generalizable, evidence-based framework for APP staffing and leadership structure could help decrease the incidence of dissatisfaction and burnout leading to attrition of experienced oncology APPs.
In order to address these concerns, the National Comprehensive Cancer Network (NCCN) Best Practices Committee created an APP Workgroup to develop recommendations and best practices to support the roles of APPs at NCCN Member Institutions. The group comprises 14 APP leaders from NCCN Member Institutions. As part of the work effort, the group conducted surveys to better understand the current state of APP program structure, staffing models, and productivity measures. The focus of this article is to highlight the current state of APP leadership and staffing structures at NCCN Member Institutions. Additionally, the article will review the professional development opportunities available to APPs in order for them to perform at the top of their license. Finally, this article will identify recommendations for standardizing APP leadership and staffing structures and improving APP professional development opportunities nationwide.
SURVEY METHODS
The Best Practices Committee conducted its first APP survey in 2017, before the inception of the APP Workgroup. Members were interested in learning more about the structure of centers' APP programs and questions focused on the number of independent vs. shared APP visits, number of half-day clinics, relative value unit (RVU) targets, clinical support provided to APPs, time spent credentialing APPs, and APP training. The survey was drafted by members of the Best Practices Committee and was distributed to two cancer centers to pilot for content accuracy. Following the pilot, the survey was distributed via a web-based survey tool (SurveyMonkey) to the entire Committee (27 Member Institutions in 2017) for completion. Survey responses were categorized by specialty, which included medical oncology, surgical oncology, radiation oncology, and stem cell/bone marrow transplant. The data were analyzed using descriptive statistics in Microsoft Excel and the results were sent to the Committee for review.
Following the initial APP survey, the APP Workgroup was developed to further assess the 2017 survey results, collect additional information, and make recommendations for optimizing the role of APPs in oncology. The APP Workgroup designed two additional surveys, the APP Structure and Productivity survey and the APP Productivity and Professional Development survey. Both surveys were piloted by two cancer centers to ensure content accuracy. After the surveys were piloted, they were administered through SurveyMonkey and the data were analyzed.
The APP Structure and Productivity survey was conducted in March 2019 and distributed to each center's APP Lead or Director of APPs for completion. The survey requested data related to the structure of inpatient and outpatient APP programs, professional development opportunities offered to APPs, and metrics utilized to measure APP productivity.
The APP Productivity and Professional Development survey was also conducted in March 2019. This survey was anonymous, included more subjective questions, and was sent to NCCN Best Practices Committee members with the request to distribute the survey to multiple APPs throughout NCCN's Member Institutions. The survey requested APPs' thoughts related to productivity metrics and professional development opportunities. Survey results were maintained and analyzed in a deidentified database to ensure participant confidentiality. Preliminary results for both APP Workgroup surveys were presented to Workgroup members during monthly calls and sent to the Best Practices Committee for reference.
SURVEY RESULTS
Survey 1: 2017 Best Practices APP Survey
Seventy-one APPs from 20 NCCN Member Institutions responded to Survey 1. Fifteen institutions had multiple APPs submit responses, representing differing specialties. Specialties included medical oncology (27%), hematology (17%), surgical oncology (14%), bone marrow transplant (14%), radiation oncology (6%), pediatric oncology (4%), neuro-oncology (4%), and other (14%).
The total number of new and follow-up visits a 1.0 APP full-time equivalent (FTE) conducts per week in shared and independent visits ranged from 11 to 97, with an average of 40 visits per week (n = 39). Four institutions reported that APPs can see new patients as an independent visit, with those being in the surgical oncology and medical oncology specialties. The majority of the visits reported were in follow-up shared visits (47.2%), followed closely by follow-up independent visits (46%), then new shared visits (6.5%), and lastly new independent visits (0.5%). Seventy-two percent of respondents surveyed utilize a mixed model of visit type (both independent and shared visits), with 15% utilizing only independent visits and 13% utilizing only shared visits (n = 39).
Twenty-one percent of centers have some type of formal APP oncology training program in place for medical oncology (n = 19). The sources of continuing education that centers support for APPs in medical oncology included internal general education available to all providers (e.g., grand rounds; 94%), American Society of Clinical Oncology (ASCO) programs (78%), internal curriculum specifically for APPs (67%), NCCN programs (61%), Oncology Nursing Society (ONS) programs (56%), Advanced Practitioner Society for Hematology and Oncology (APSHO) programs (50%), American Society of Hematology (ASH) programs (39%), other national conferences (39%), and other continuing education (33%; n = 18). Fifteen Member Institutions reported the amount of funding provided to an APP for continuing education annually, and responses ranged from $500 to $2,500 for APPs in medical oncology. Sixteen institutions reported professional development opportunities for APPs, in which centers provided resources for posters, papers and presentations at conferences (88%), leadership development activities (69%), writing book chapters (63%), and conducting research (44%; n = 16).
Survey 2: APP Productivity and Professional Development
A total of 492 APPs from 23 NCCN Member Institutions submitted responses to Survey 2. In 2018, APPs reported that professional development opportunities offered included posters, papers, and presentations at conferences (84%), leadership development activities (57%), research opportunities (52%), writing book chapters (19%), and other professional development activities (12%; n = 422). Twenty percent of APPs indicated in an open-ended question that protected time to engage in professional development opportunities should be offered but is currently not provided, as well as leadership development opportunities (19%), research opportunities (14%), communication skills development (11%), and other professional development activities (11%; n = 196). Other activities that APPs believed should be included in professional development opportunities were writing development, paid certifications, mentorship programs, fellowship and residency opportunities, quality improvement projects, networking with external APPs, and journal clubs.
Survey 3: APP Structure and Productivity
Of the 28 NCCN Member Institutions, 23 responded to Survey 3. This survey further evaluated the responsibilities of APPs in leadership roles among NCCN institutions. The survey found that 95% of NCCN institutions have APP leads for the centers' inpatient and outpatient APP programs (n = 23), with 85% utilizing both PA and NP leads in the inpatient setting (n = 20), and 90% utilizing both PA and NP leads in the outpatient setting (n = 20). The number of APP lead FTEs in the inpatient and outpatient programs ranged from 1 to 20 and 1 to 40, respectively (n = 18, n = 17). Of the 95% of centers that have APP leads, 100% of them indicated that APP leads carry administrative and clinical responsibilities (n = 20); however, results varied with respect to how APP leads' time is allocated for these responsibilities. Fifty percent of APP leads allocate 80% of their time to clinical responsibilities and 20% for administrative duties, 36% allocate time in a 50/50 split between clinical and administrative responsibilities, followed by 7% of APPs who allocate 60% of their time to clinical responsibilities and 40% for administrative, and 7% who allocate the majority of time (90%) to clinical activities and 10% to administrative duties (n = 14).
Forty-two percent of centers have APP leads oversee more than 15 APP FTEs in the inpatient setting and 37% of centers have APP leads oversee more than 15 APP FTEs in the outpatient setting (n = 19). Only two centers have APP leads oversee 4 to 6 APPs in the inpatient, and one center has APP leads manage 4 to 6 APPs in the outpatient setting. The remaining centers had a mix of APPs overseeing anywhere from 7 to 9 APPs to 13 to 15 APPs in the inpatient and outpatient units (Figure 1).
Figure 1.
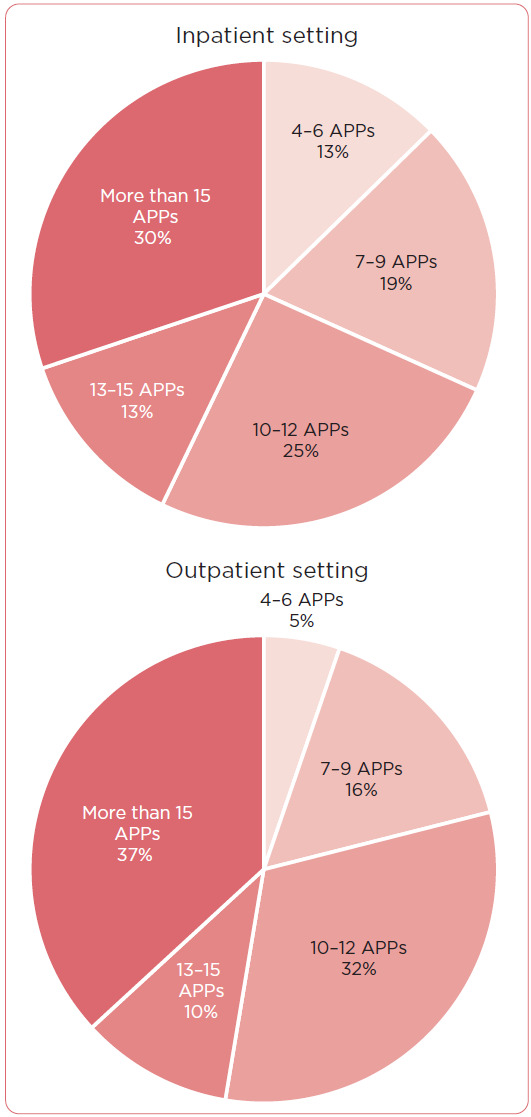
Number of APP full-time equivalents that APP leads are responsible for in inpatient and outpatient settings (N = 19).
DISCUSSION
APPs from NCCN Member Institutions are practicing in a number of different roles and specialties with varying expectations in regards to the number and type of visits per week, practice setting, and leadership structure. It is well documented that the addition of APPs to oncology practices has the potential to not only address the growing demand for an increased supply of oncology services, but also improve practice quality and efficiency, enhance patient care, and increase APP satisfaction. A number of studies have examined the roles and responsibilities, staffing patterns, and productivity of APPs in oncology in efforts to illustrate how APPs are well positioned to fill the widening oncology service gap (Bruinooge et al., 2018; Hinkel et al., 2010; McCorkle et al., 2015; Reynolds & McCoy, 2016).
Takeaway 1: Independent vs. Shared APP Visits
The survey results demonstrate considerable differences among NCCN Member Institutions regarding both the expected number and type of visits a 1.0 APP FTE conducts per week. The majority of institutions reported that they use a mixed model of visit type with both shared (patient visits with the presence of a physician) and independent visits (patient visits without the presence of a physician). Collaborative practice models where APPs are engaging in both shared and independent visits appears to be optimal across NCCN Member Institutions. This model allows APPs to not only work autonomously but also be able to work alongside a physician to determine the best course of treatment for complex patients, furthering their expertise and knowledge.
Takeaway 2: APP Leads
Beyond general oncology APP characteristics, the survey results indicate that the use of APP leads in oncology has become ubiquitous across NCCN institutions in both the inpatient and outpatient settings. There exists much diversity in the number of APP lead FTEs per institution, the type of APP lead (NP vs. PA), and the number of APPs they are responsible for managing. The role of the APP lead is complex, demanding both patient-focused clinical leadership and organizational responsibilities. To date, there does not exist a formal definition of an APP lead and the responsibilities this role requires. APP lead job descriptions that do exist are institution specific and developed by individual departments. This lack of knowledge about APP leadership is problematic because it has the potential to hinder APP scope of practice utility, thus limiting the potential impact of APPs on patient care and health-care operations. As the demand for oncology APPs continues to grow, there will be a subsequent need for APP leadership to effectively advance the profession and develop efficient models for APP staffing and productivity.
From Survey 3, it was apparent that many centers structured APP lead time by allocating a split of 80% clinical time and 20% administrative time. This split could serve as a baseline minimum when centers are defining the time APP leads should spend on specific clinical and administrative tasks. Centers could adjust the time that APPs spend on clinical and administrative duties according to factors such as the number of APPs they manage and the staff support they have available to assist with these duties. Centers must ensure that APP leads have ample time to complete administrative tasks but must also allow them to dedicate a sufficient amount of time to patient care.
Takeaway 3: Professional Development Opportunities
Leadership must also ensure that professional development opportunities are available to APPs in order for APPs to perform at the top of their license, retain talented APPs, and allow APPs to advance in their career. It is important to note that there is variance in background experience upon entry to practice, in training programs, and ongoing developmental needs that are not always generalizable. Early career needs include access to safe, quality onboarding, residencies, fellowships, mentoring, and constructive evaluation and feedback. As APPs advance in their careers, there are areas of opportunity to participate in leading in their field as well as offering contributions in the interdisciplinary academic setting.
When those APPs surveyed were asked to reflect on which professional development opportunities were available over the past year, a majority of APPs indicated that there were opportunities to produce or be included in posters, papers, and presentations at conferences (Survey 2, Figure 2). APPs reported that there were fewer opportunities to participate in initiatives such as leadership development research, writing book chapters, and other professional development activities. Many APPs are offered these opportunities, but do not have time to engage in these activities throughout their workday.
Figure 2.
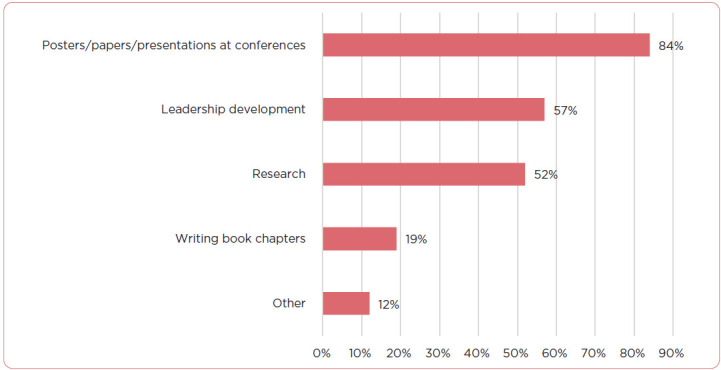
Professional development opportunities for APPs at institutions in 2020 (N = 422).
Respondents were asked to reflect (in an open-ended question) on what opportunities should be offered to APPs at NCCN Member Institutions. 20% indicated that protected time to engage in professional development opportunities should be offered but is currently not provided (n = 196; Figure 3). If APPs are interested in participating in professional development opportunities, oftentimes they must dedicate time outside of work to gain additional skills and qualifications.
Figure 3.
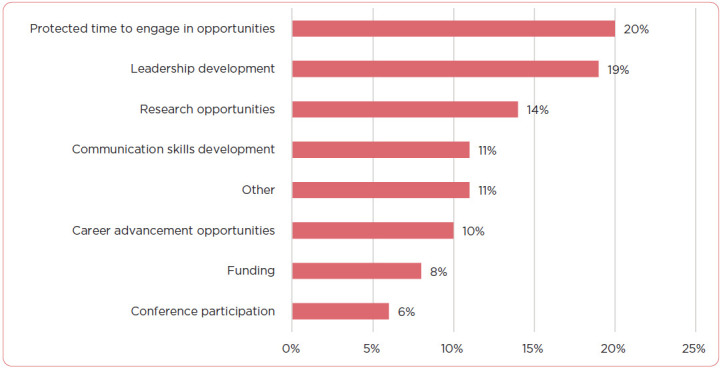
Professional development opportunities survey respondents believe should be offered (N = 196).
In order to retain APPs and promote career advancement internally, leadership must vocalize these opportunities, as it was apparent from the survey results that some respondents were unaware of professional development opportunities available to them. During the APP onboarding process, APP leads should discuss the professional development opportunities that are available for APPs to utilize. Additionally, from Survey 2, APPs believed that more leadership development opportunities should be offered especially with the rise in the number of APP lead roles throughout cancer centers. Creating leadership development opportunities for NPs and PAs would help with APP retention and employee satisfaction.
Takeaway 4: Continuing Education
Many APPs responded that fellowship and mentorship programs would help enhance their knowledge and education related to the field. From Survey 1, it was clear that only a small percentage of centers offer some type of formal oncology training program for APPs (Figure 4).
Figure 4.
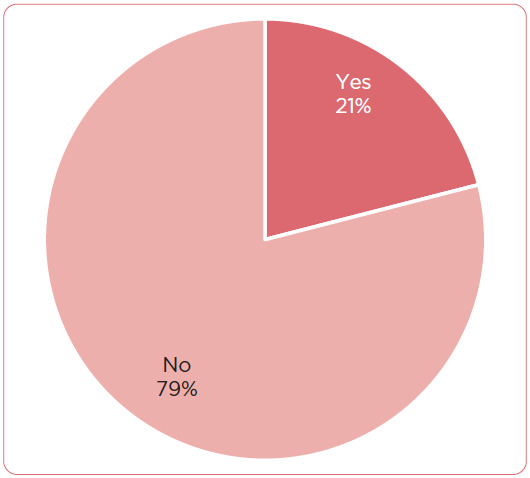
Percentage of survey respondents who have a formal APP oncology training program (N = 19).
As noted by Cairo and colleagues (2017), the focus of APP education and training is on health promotion, disease prevention, and primary care medical management, but most post-graduate APPs have limited exposure to the management of cancer patients. Some centers are choosing to respond to these needs by connecting their experts with novices and developing their own internal APP residency and fellowship opportunities, mentorship programs, as well as internal leadership development tracks. In the academic space, the postmaster's education and terminal degree options are not uniform and include tracks into clinical, administrative, and academic leadership.
APP fellowships have been most prevalent in areas such as primary care, emergency medicine, critical care, and palliative care. With the increase in APPs throughout oncology, centers should assess the benefits of the APP fellowship and training programs in those departments to see if it would be valuable to create a formal oncology program for practicing APPs. Creating APP oncology fellowship programs would ensure that APPs are receiving the proper, specialized training and education to be successful at their roles. Centers could also work together to develop standardized training programs that could benefit APPs across the country. The establishment of formal programs would enhance the quality and safety of care across the institution. These programs would also give APPs additional continuing education opportunities and in turn, lead to improved job satisfaction.
CONCLUSION
Throughout the literature, full professional integration, including high-level use of APPs, opportunities for professional growth, and a supportive educational environment are major components of retention. Several studies have demonstrated that when APPs practice to the full extent of their scope, visit capacity increases and APP satisfaction improves. With the tremendous growth oncology care is currently experiencing, APPs in cancer today are uniquely positioned to help shape the APP role within cancer.
As evidenced by the variability of the survey results, the field would benefit from developing core responsibilities and standards for APPs in oncology and its subspecialties (hematology, radiation, stem cell transplant, surgery, etc.) in order to create useful staffing structures and productivity benchmarks. More research is needed to determine the number of APPs practicing within oncology and determine how they are practicing throughout the country at both NCCN and non-NCCN institutions to help develop such core competencies. The lack of a national repository of APPs working in oncology will hinder additional research. Advanced oncology certification is currently only available to nurse practitioners; however, having a streamlined certification available to all APPs may help to create a database of APPs practicing in oncology. To further optimize the use of the APP lead role, additional research is needed on the responsibilities of the APP lead role and its intended impact on job satisfaction and health-care delivery.
Various studies, including Survey 3 in this article, indicate that there is a remarkable lack of information regarding leadership structures in place to help support APPs within oncology. Centers should continue to assess the multilevel and career-long opportunities needed to maximize the value this group can offer to patients within the oncology community.
Limitations
Limitations to the study include use of a convenience sample of APPs from NCCN Member Institutions, which may limit the generalizability of observed results. Only certain questions from the survey delineated between NPs and PAs; thus, the authors are unable to make broad associations regarding differences between NPs and PAs in oncology practice. As NPs and PAs continue to collaborate under the umbrella term of “APPs,” future studies should evaluate how PAs and NPs differ in relation to both patient and physician satisfaction, productivity, and quality of care in order to identify areas for improvement. A further limitation of these studies is the lack of a clear definition of independent and shared visits given the middle ground of collaborative visits (APPs engaging in both shared and independent visits) was not captured.
Acknowledgment
The authors would like to acknowledge the NCCN Advanced Practice Provider Workgroup, comprising nurse practitioner and physician assistant leaders who manage APPs, as well as perform daily clinical operations at their respective NCCN Member Institutions.
Footnotes
The authors have no conflicts of interest to disclose.
References
- Bruinooge, S. S., Pickard, T. A., Vogel, W., Hanley, A., Schenkel, C., Garrett-Mayer, E., Williams, S. F. (2018). Understanding the Role of Advanced Practice Providers in Oncology in the United States. Journal of Oncology Practice, 14(9), 518–532. doi: 10.1200/JOP.18.00181 [DOI] [PubMed] [Google Scholar]
- Cairo, J., Muzi Mary Ann, Ficke, D., Ford-Pierce, S., Goetzke, K., Stumvoll, D.,…Sanchez, F. A. (2017). Practice model for advanced practice providers in oncology. American Society of Clinical Oncology Educational Book, 37(October 29, 2018), 40–43. 10.14694/EDBK_175577 [DOI] [PubMed] [Google Scholar]
- Erikson, C., Salsberg, E., Forte, G., Bruinooge, S., & Goldstein, M. (2007). Future Supply and Demand for Oncologists: Challenges to Assuring Access to Oncology Services. Journal of Oncology Practices, 3(2), 79–86. doi: 10.1200/JOP.0723601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinkel, J. M., Vandergrift, J. L., Perkel, S. J., Waldinger, M. B., Levy, W., & Stewart, F. M. (2010). Practice and Productivity of Physician Assistants and Nurse Practitioners in Outpatient Oncology Clinics at National Comprehensive Cancer Network Institutions. Journal of Oncology Practice, 6(4), 182–187. doi: 10.1200/JOP.777001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy, W., Gagnet, S., & Stewart, F. M. (2013). Appreciating the role of advanced practice providers in oncology. Journal National Comprehensive Cancer Network, 11(5), 508–11. DOI: 10.6004/jnccn.2013.0067 [DOI] [PubMed] [Google Scholar]
- McCorkle, R., Jeon, S., Ercolano, E., Lazenby, M., Reid, A., Davies, M., Gettinger, S. (2015). An Advanced Practice Nurse Coordinated Multidisciplinary Intervention for Patients with Late-Stage Cancer: A Cluster Randomized Trial. Journal of Palliative Medicine, 18(11), 962–969. doi: 10.1089/jpm.2015.0113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Towle, E. L., Barr, T. R., Hanley, A., Kosty, M., Williams, S., & Goldstein, M. A. (2011). Results of the ASCO Study of Collaborative Practice Arrangements. Journal of Oncology Practice, 7(5), 278–282. DOI: 10.1200/JOP.2011.000385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds, R. B., & McCoy, K. (2016). The role of Advanced Practice Providers in interdisciplinary oncology care in the United States. Chinese clinical oncology, 5(3), 44. 10.21037/cco.2016.05.01 [DOI] [PubMed] [Google Scholar]
- Yang, W., Williams, J. H., Hogan, P. F., Bruinooge, S. S., Rodriguez, G. I., Kosty, M. P., Goldstein, M. (2014). Projected supply of and demand for oncologists and radiation oncologists through 2025: an aging, better-Insured population will result in shortage. Journal of Oncology Practice, 10(1), 39–45. DOI: 10.1200/JOP.2013.001319 [DOI] [PubMed] [Google Scholar]


