Abstract
Objective
To analyze the medication rules of traditional Chinese medicine (TCM) preventive oral prescriptions for COVID-19.
Methods
The preventive oral prescriptions for COVID-19 published by national and provincial health and wellness committees, administrations of TCM, medical institutions at all levels, medical masters and Chinese medicine experts were collected to establish a database, manual screening was carried out according to the inclusion and exclusion criteria, and frequency statistics, association rule analysis. The mutual information method, entropy hierarchical clustering and other methods were improved through Excel and the TCM inheritance auxiliary platform V2.5 to mine the rules and characteristics of medication.
Results
The selected 157 prescriptions contained a total of 130 TCMs. The top five TCMs with the highest use frequency were Glycyrrhizae Radix et Rhizoma (86), Astragali Radix (80), Lonicerea Japonicae Flos (70), Atractylodis Macrocephalae Rhizoma (62), Saposhnikoviae Radix (60). In accordance with TCM efficacy classification, most of them were medicines for qi-tonifying (279), followed by medicines for clearing heat and drying dampness (163), dispelling pathogenic wind-cold (126), resolving dampness (111), as well as dispelling pathogenic wind-heat (99). The characteristics of four-natures of the selected medicines are as follows: most of them were cold (59), followed by warm (38) and mild (21). In terms of five-taste, most of them were sweet (26) and acrid-and-bitter (24), followed by sweet-and-bitter (20), bitter (20) and acrid (15). For the meridian attribution, the five-zang organs and six-fu organs were all involved, most of them attributed to lung meridian (80), followed by stomach meridian (57) and spleen meridian (40). Based on association rule analysis, 12 commonly used medicine combinations with two or three TCMs were found. The commonly used medicinal pairs included Astragali Radix and Saposhnikoviae Radix (51), Astragali Radix and Atractylodis Macrocephalae Rhizoma (46), Atractylodis Macrocephalae Rhizoma and Saposhnikoviae Radix (43), Astragali Radix and Atractylodis Macrocephalae Rhizoma and Saposhnikoviae Radix (38), Forsythiae Fructus and Astragali Radix (37), and so on. In addition, 14 core combinations of medicines were obtained by complex system entropy cluster analysis, on this basis, six new prescriptions were screened out based on unsupervised entropy hierarchical clustering analysis. According to The Catalogue of Edible Traditional Chinese Medicinal Materials, Traditional Chinese Medicinal Materials for Health Food, and New Resources of Food published by National Health Commission of the People’s Republic of China, there are 35 species belonging to the group of edible traditional Chinese medicinal materials, 20 species belonging to the group of new resources of food, 31 species belonging to the group of traditional Chinese medicinal materials for health food, 19.11% of the preventive oral prescriptions for COVID-19 were composed of the medicines belonging to the above three groups. Besides, there are 11 toxic species, and 24.84% of the preventive oral prescriptions for COVID-19 contained toxic TCMs.
Conclusion
We found that invigorating qi and resolving dampness were the main treatment used to prevent for COVID-19, combined with the methods for strengthening vital energy and eliminating pathogenic factors. Most of the preventive oral prescriptions for COVID-19 were treated in lung, spleen and stomach meridians. In the process of selecting prescriptions and using TCMs to prevent for COVID-19, the safety of preventive medicines was also emphasized. And the theory of “Preventive Treatment of Disease” was embodied in these preventive oral prescriptions for COVID-19. For the prescriptions containing toxic TCMs, special attention should be paid to their safety in clinical application.
Keywords: COVID-19, medication rule, oral, preventive prescriptions
1. Introduction
Novel coronavirus pneumonia (NCP) is an acute respiratory infectious disease caused by a beta family New Coronavirus (COVID-19), whose clinical manifestation characterized by dry cough, fever and fatigue. It can spread by contact, droplet and fecal-oral route (Zhu et al., 2020). It’s considered that the pathogenesis of epidemic disease is that the lung meridian being invaded by the epidemic pathogenic factor from outside while the vital qi being deficient, which related to the pathological properties of dampness, heat, toxin, deficiency and stasis. For thousands of years, TCM has played an important role in the prevention and treatment of epidemic diseases. The Huangdi's Classic on Medicine of Western Han Dynasty put forward that “Five-pestilences are easy to be contagious, and their symptoms are similar regardless of their severity.” In the Plague Diseases of Ming Dynasty, it is pointed out that “the plague victims get ill because of that infected by epidemic pathogenic factor…When the epidemic pathogenic factor comes, the people are infected with it no matter how strong or weak”. “ All pathogenic factors invading the human body should be expelled as soon as possible.” “The disease will not be cured until the evil qi is eliminated.” In the Differentiation of Epidemic Febrile Diseases of Qing Dynasty, it is said that “Pestilence is characterized by the epidemic of pathogenic qi, and most of them are accompanied by filth.”
In the process of the prevention and control of COVID-19, TCM was involved in it in the early stage, the TCM treatments have been written into the national and local diagnosis and treatment protocols for COVID, and have achieved good results in clinical treatment. Clinical application has proved that the treatments of TCM can effectively relieve the symptoms of COVID-19, keep down the development of mild and common types to serious types, improve the cure rate and reduce the death rate, and promote the rehabilitation of the convalescent crowd (Gao et al., 2020, Wang et al., 2020, You et al., 2020).
As of September 2021, although COVID-19 has been well controlled in China, only few provinces have occasionally imported cases and asymptomatic infections. However, the epidemic situation in the United States, India, Japan, Iran and other countries is still not optimistic. At present, due to the absence of specific medicines for the treatment of COVID-19, the combination of TCM and Western medicine is mainly used for symptomatic treatment, and TCM is mainly used for prevention in clinic.
We collected preventive oral prescriptions for COVID-19 which are recorded in related literatures and protocols, and built a database to analyze oral medication rules of TCM prescriptions for preventing COVID-19, to provide basis for better use of TCM to prevent and treat COVID-19 effectively in clinical practice.
2. Materials and methods
2.1. Data sources
The preventive oral prescriptions for COVID-19 were collected from national and provincial health committees of the people’s republic of China, administrations of TCM, medical institutions, national TCM masters and TCM experts to establish a database and conduct manual screening according to the inclusion and exclusion criteria, so as to analyze these prescriptions.
2.2. Inclusion criteria
The inclusion criteria is that the prescriptions were for prevention, mainly were Chinese herbal compounds with clear provenance, composition and dosage.
2.3. Exclusion criteria
The prescriptions with a single medicine, the prescriptions with imperfect composition and dosage, the same prescriptions used for the same syndrome type according to the thoughts of syndrome differentiation and treatment, the prescriptions of recommended Chinese patent medicines, the prescriptions of non-oral dosage forms of medicines, the prescriptions with unclear source, were not counted in.
2.4. Data screening
According to the above inclusion and exclusion criteria, a total of 157 preventive oral prescriptions for COVID-19 were selected.
2.5. Prescriptions input and medicine name specification
Taking the Pharmacopoeia of the people's Republic of China (National Pharmacopoeia Committee, 2015), Chinese Materia Medica (Editorial Committee of Chinese Materia Medica of the State Administration of Traditional Chinese Medicine, 1999) and Chinese Pharmacy (Gao, 2002) as the standards, the names of TCMs used in 157 selected prescriptions were standardized. The names of ethnic medicines and the idiomatic names of commonly known medicines were entered in the standard names into The Auxiliary Platform of Traditional Chinese Medicine Inheritance software, for example, “Yinhua”, “Erhua” and “Shuanghua” were unified as “Lonicerea Japonicae Flos”. Processed medicines and raw medicines were entered with the same standard name, for example, “Raw Astragali Radix ”, “Fried Astragali Radix” and “ Astragali Radix ” were unified as “ Astragali Radix ”; “ Atractylodis Macrocephalae Rhizoma ” and “Fried Atractylodis Macrocephalae Rhizoma ” were input as “ Atractylodis Macrocephalae Rhizoma”. All genuine medicinal materials were entered with their original medicine names without the abbreviation of genuine medicinal materials producing regions in front of their name. For example, “Lu Codonopsis Radix” and “ Codonopsis Radix” were input as “ Codonopsis Radix ”.
As “nine out of ten prescriptions have Glycyrrhizae Radix et Rhizoma ”, Glycyrrhizae Radix et Rhizoma mostly plays a role in coordinating the medicine actions of a prescription, but no other functions. It is not meaningful to analyze its drug pairs and formulations. Therefore, the prescriptions selected were entered into the auxiliary platform of traditional Chinese medicine inheritance for the analysis of association rules and new prescriptions after Glycyrrhizae Radix et Rhizoma having been removed.
2.6. Data analysis
Both excel software and the Auxiliary Platform of Traditional Chinese Medicine Inheritance were used for data management and mining. And statistics and analysis were made on the frequency, dosage, four-nature, five-taste and meridian attribution of TCMs, the classification of TCM efficacy, the prescription-formulating principles based on association rules, the core combinations based on complex system entropy clustering and the new prescriptions based on unsupervised entropy hierarchical clustering.
For dose statistics of the selected prescriptions, the calculation of dose statistics of TCMs is as follows: 1) The average dose is the “arithmetic mean” in Statistics (“n” is the total frequency); 2) The most commonly used dose: that is, the dose value with the highest frequency of a certain TCM, which reflects that the dose distribution of a certain TCM is the most intensive at this dose value point, and it together with the average dose affects the dose distribution of a certain TCM; 3) Dose distribution interval: refers to the range between the minimum dose and the maximum dose of a certain TCM, which can reflect the flexibility of the clinical dosage of a certain TCM; 4) Common dose range: the concept of statistical percentile was led to calculate the commonly used dose range. The formula is (in the formula, “L” represents the lower limit of PX group, “i” represents the group distance, represents the frequency of group, “n” represents the total frequency, represents the cumulative frequency less than “L”, and the difference between “P10” and “P90” represents the common dose range).
3. Results
3.1. Analysis of medication frequency
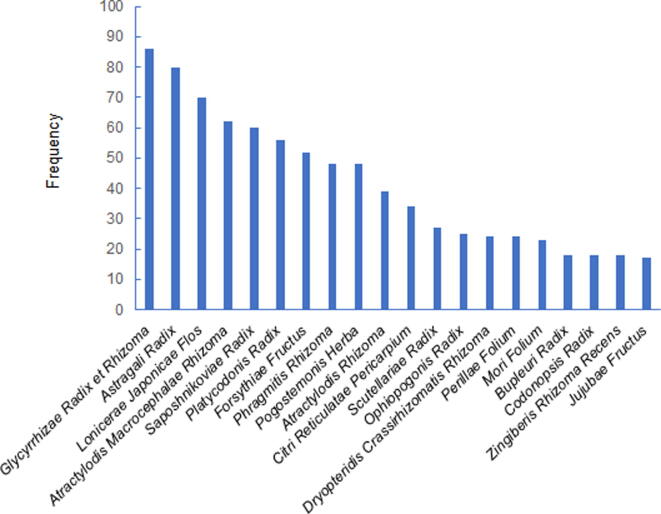
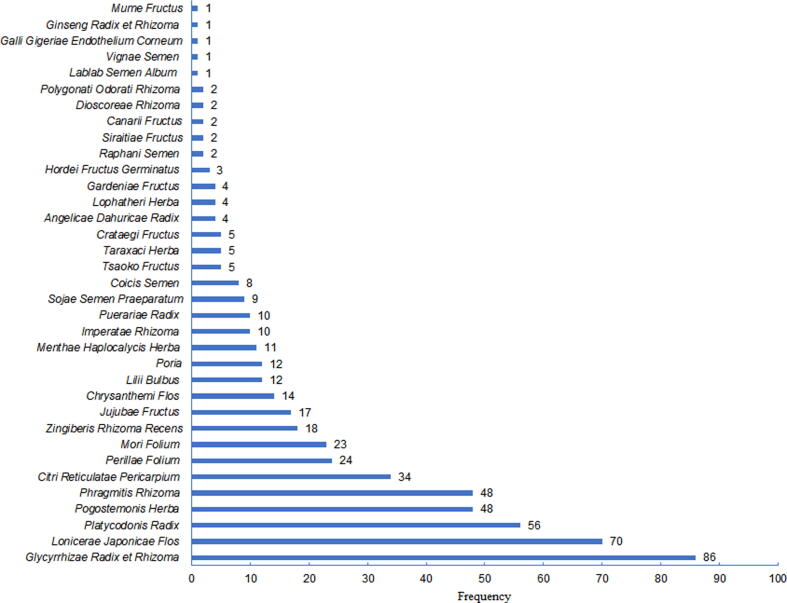
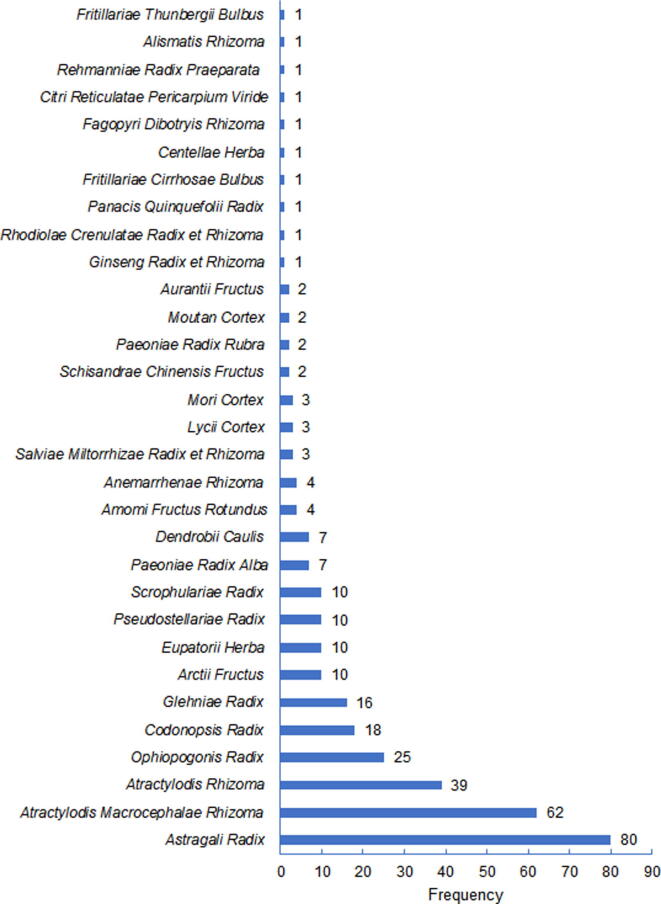
A total of 157 preventive oral prescriptions for COVID-19 were selected, in which 130 species of TCMs were used. The top 10 medicines in order of frequency (Fig. 1) were Glycyrrhizae Radix et Rhizoma (86), Astragali Radix (80), Lonicerae Japonicae Flos (70), Atractylodis Macrocephalae Rhizoma (62), Saposhnikoviae Radix (60), Platycodonis Radix (56), Forsythiae Fructus (52), Phragmitis Rhizoma (48), Pogostemonis Herba (48), Atractylodis Rhizoma (39).
Fig. 1.
Frequency of usage of single TCM used in preventive oral prescriptions for COVID-19.
3.2. Efficacy statistical analysis
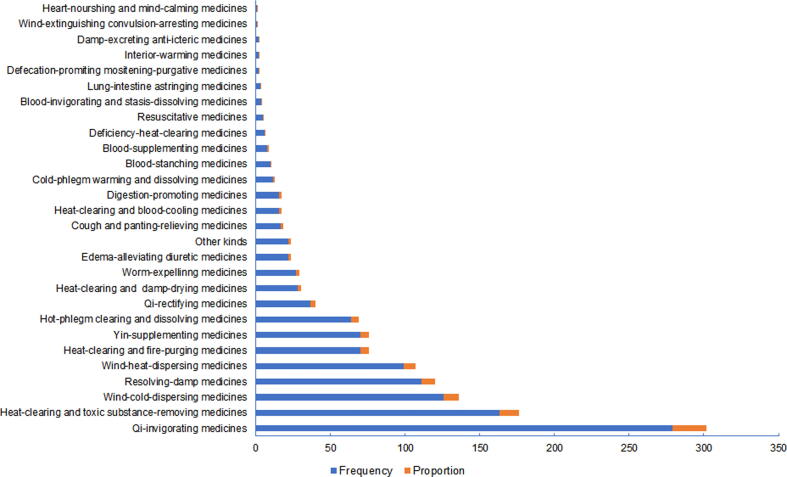
The TCMs involved can be classified into 28 categories according to their efficacy in the 157 preventive oral prescriptions for COVID-19. The top five efficacy categories of TCMs in order of frequency of usage (Fig. 2) were herbal medicines for invigorating qi (2 7 9), clearing heat and removing toxic substance (1 6 3), dispelling pathogenic wind-cold (1 2 6), resolving dampness (1 1 1), dispelling pathogenic wind-heat (99).
Fig. 2.
Frequency and proportion of efficacy categories of TCMs used in preventive oral prescriptions for COVID-19.
3.3. Analysis on four-nature, five-taste and meridian attribution of TCMs used in 157 prescriptions
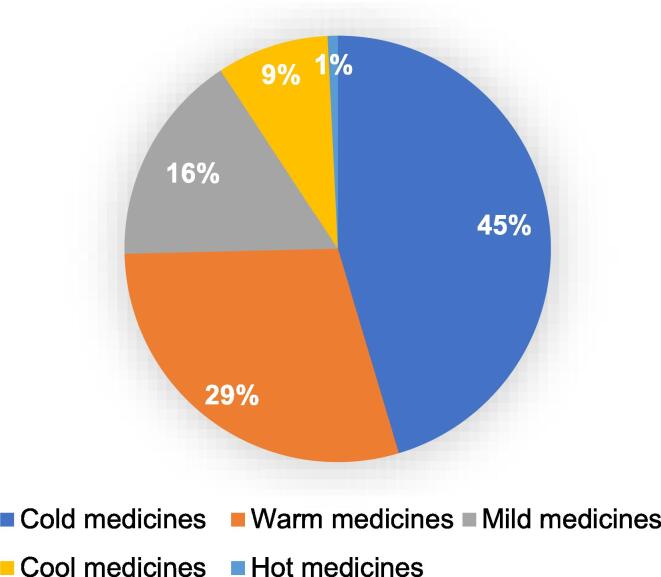
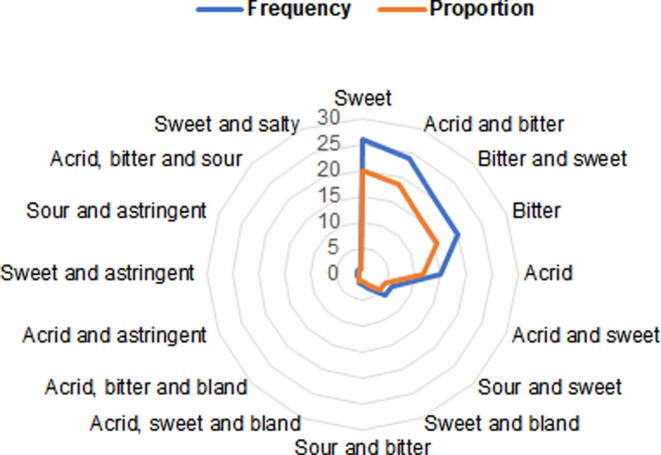
The TCMs contained in the 157 prescriptions were 59 cold medicines, 38 warm medicines, 21 mild medicines, 11 cool medicines, and one hot medicine; The tastes of these medicines involve seven tastes: sour, bitter, sweet, acrid, salty, astringent and bland. In terms of five-taste, most of them were sweet (26) and acrid-and-bitter (24), followed by sweet-and-bitter (20), bitter (20) and acrid (15). The tastes of 67 medicines contain bitterness, 65 medicines contain sweet, 50 medicines contain acrid. The analysis of the meridian attribution of all medicines showed that the meridian attribution of the 130 medicines included all the five zang and six fu organs. The top five types of meridians to which the medicines attribute were lung-stomach meridians (12), spleen-stomach-lung meridians (9), lung meridians (9), spleen-stomach meridians (7), spleen-lung meridians (6). The main meridians to which these medicines attribute were the three meridians of lung, spleen and stomach. The meridians in attribution of 67 medicines contain lung meridian, 65 medicines attribute to stomach, 50 medicines attribute to spleen. The specific usages were shown in Fig. 3, Fig. 4 and Table 1.
Fig. 3.
Proportion of four-nature of single TCM used in preventive oral prescriptions for COVID-19.
Fig. 4.
Frequency and proportion of five-taste of single TCM used in preventive oral prescriptions for COVID-19.
Table 1.
Analysis on meridian attribution of TCMs used in 157 preventive oral prescriptions for COVID-19.
| Ranking | Meridian tropism | Frequency | Proportion/% | Ranking | Meridian tropism | Frequency | Proportion/% |
|---|---|---|---|---|---|---|---|
| 1 | Lung and stomach meridians | 12 | 9.23 | 32 | Heart, lung, liver and kidney meridians | 1 | 0.77 |
| 2 | Spleen, stomach and lung meridians | 9 | 6.92 | 33 | Heart meridian | 1 | 0.77 |
| 3 | Lung meridian | 9 | 6.92 | 34 | Stomach and kidney meridians | 1 | 0.77 |
| 4 | Spleen and stomach meridians | 7 | 5.38 | 35 | Spleen, stomach and heart meridians | 1 | 0.77 |
| 5 | Spleen and lung meridians | 6 | 4.62 | 36 | Spleen, stomach, small intestine and urinary bladder meridians | 1 | 0.77 |
| 6 | Other meridians | 5 | 3.85 | 37 | Spleen, stomach, kidney, heart and lung meridians | 1 | 0.77 |
| 7 | Lung and liver meridians | 5 | 3.85 | 38 | Spleen, stomach, lung and large intestine meridians | 1 | 0.77 |
| 8 | Heart and stomach meridians | 4 | 3.08 | 39 | Spleen, stomach, large intestine, pericardium and liver meridians | 1 | 0.77 |
| 9 | Heart and lung meridians | 4 | 3.08 | 40 | Spleen, kidney, heart and lung meridians | 1 | 0.77 |
| 10 | Heart and liver meridians | 3 | 2.31 | 41 | Spleen, lung and heart meridians | 1 | 0.77 |
| 11 | Liver and kidney meridians | 3 | 2.31 | 42 | Spleen, lung, kidney and urinary bladder meridians | 1 | 0.77 |
| 12 | Hear, stomach and small intestine meridians | 2 | 1.54 | 43 | Spleen, lung and kidney meridians | 1 | 0.77 |
| 13 | Heart, lung and kidney meridians | 2 | 1.54 | 44 | Urinary bladder and spleen meridians | 1 | 0.77 |
| 14 | Lung, stomach and kidney meridians | 2 | 1.54 | 45 | Urinary bladder, liver and spleen meridians | 1 | 0.77 |
| 15 | Kidney and urinary bladder meridians | 2 | 1.54 | 46 | Urinary bladder meridian | 1 | 0.77 |
| 16 | Spleen, stomach and liver meridians | 2 | 1.54 | 47 | Liver and pericardium meridians | 1 | 0.77 |
| 17 | Liver and stomach meridians | 2 | 1.54 | 48 | Liver, spleen, lung and large intestine meridians | 1 | 0.77 |
| 18 | Liver and spleen meridians | 2 | 1.54 | 49 | Liver, lung and stomach meridians | 1 | 0.77 |
| 19 | Liver, gallbladder and lung meridians | 2 | 1.54 | 50 | Liver, gallbladder and stomach meridians | 1 | 0.77 |
| 20 | Liver meridian | 2 | 1.54 | 51 | Liver and gallbladder meridians | 1 | 0.77 |
| 21 | Lung, stomach and large intestine meridians | 2 | 1.54 | 52 | Lung and small intestine meridians | 1 | 0.77 |
| 22 | Lung and urinary bladder meridians | 2 | 1.54 | 53 | Lung, stomach and heart meridians | 1 | 0.77 |
| 23 | Lung, liver and kidney meridians | 2 | 1.54 | 54 | Lung, stomach and urinary bladder meridians | 1 | 0.77 |
| 24 | Lung and large intestine meridians | 2 | 1.54 | 55 | Lung, kidney and urinary bladder meridians | 1 | 0.77 |
| 25 | Heart and small intestine meridians | 1 | 0.77 | 56 | Lung and kidney meridians | 1 | 0.77 |
| 26 | Heart, stomach and lung meridians | 1 | 0.77 | 57 | Lung, urinary bladder and heart meridians | 1 | 0.77 |
| 27 | Heart, spleen, stomach, gallbladder, large intestine and liver meridians | 1 | 0.77 | 58 | Lung, liver and heart meridians | 1 | 0.77 |
| 28 | Heart, liver and kidney meridians | 1 | 0.77 | 59 | Lung, gallbladder, large intestine and small intestine meridians | 1 | 0.77 |
| 29 | Heart, lung and small intestine meridians | 1 | 0.77 | 60 | Large intestine, small intestine and stomach meridians | 1 | 0.77 |
| 30 | Heart, lung and sanjiao meridians | 1 | 0.77 | 61 | Large intestine and stomach meridians | 1 | 0.77 |
| 31 | Heart, lung, spleen and stomach meridians | 1 | 0.77 | Total | 130 | 100 |
3.4. Analysis on prescription-formulating principles based on association rules
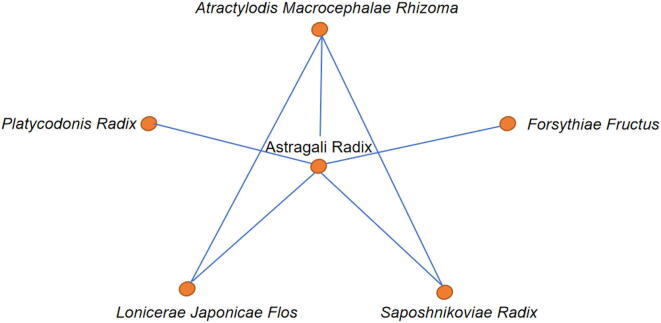
The 157 prescriptions were analyzed by using the “the prescription-formulating principles” in the Auxiliary Platform of Traditional Chinese Medicine Inheritance software. And when the support was set to 31 while the confidence was set to 0.6, we obtained eight commonly used medicine combinations in preventive oral prescriptions for COVID-19. The top five commonly used medicine combinations in order of frequency (Table 2) were Astragali Radix and Saposhnikoviae Radix (51), Astragali Radix and Atractylodis Macrocephalae Rhizoma (46), Atractylodis Macrocephalae Rhizoma and Saposhnikoviae Radix (43), Astragali Radix and Atractylodis Macrocephalae Rhizoma and Saposhnikoviae Radix (38), Forsythiae Fructus and Astragali Radix (37). By using the “rule analysis” module in the software, 12 medication rules of common medicine pairs were obtained that is when the medicines on the left side of “->” appeared, the probability of medicines on the right side appeared, and the network diagram was derived. According to the confidence level, the top five medicine combinations were Atractylodis Macrocephalae Rhizoma and Saposhnikoviae Radix -> Astragali Radix, Saposhnikoviae Radix -> Astragali Radix, Astragali Radix and Atractylodis Macrocephalae Rhizoma -> Saposhnikoviae Radix, Astragali Radix and Saposhnikoviae Radix -> Atractylodis Macrocephalae Rhizoma, Atractylodis Macrocephalae Rhizoma -> Astragali Radix, as shown in Table 3, Fig. 5.
Table 2.
Commonly used medicine combinations of TCM preventive oral prescriptions for COVID-19.
| No. | Medicine combinations | Frequency of occurrence | Efficacy categories |
|---|---|---|---|
| 1 | Astragali Radix, Saposhnikoviae Radix | 51 | Invigorating qi and relieving exterior syndrome |
| 2 | Astragali Radix, Atractylodis Macrocephalae Rhizoma | 46 | Invigorating qi |
| 3 | Atractylodis Macrocephalae Rhizoma, Saposhnikoviae Radix | 43 | Invigorating qi and relieving exterior syndrome |
| 4 | Astragali Radix, Atractylodis Macrocephalae Rhizoma, Saposhnikoviae Radix | 38 | Invigorating qi and relieving exterior syndrome |
| 5 | Forsythiae Fructus, Astragali Radix | 37 | Clearing heat and invigorating qi |
| 6 | Lonicerae Japonicae Flos, Astragali Radix | 35 | Clearing heat and invigorating qi |
| 7 | Astragali Radix, Platycodonis Radix | 33 | Invigorating qi and dissolving phlegm |
| 8 | Lonicerae Japonicae Flos, Atractylodis Macrocephalae Rhizoma | 31 | Clearing heat and invigorating qi |
Table 3.
Commonly used medicine combinations of TCM preventive oral prescriptions for COVID-19 based on correlation analysis.
| No. | Rules | Confidence |
|---|---|---|
| 1 | Forsythiae Fructus -> Astragali Radix | 0.711538462 |
| 2 | Platycodonis Radix -> Astragali Radix | 0.611111111 |
| 3 | Atractylodis Macrocephalae Rhizoma -> Astragali Radix | 0.741935484 |
| 4 | Saposhnikoviae Radix -> Astragali Radix | 0.86440678 |
| 5 | Astragali Radix -> Saposhnikoviae Radix | 0.62962963 |
| 6 | Saposhnikoviae Radix -> Atractylodis Macrocephalae Rhizoma | 0.728813559 |
| 7 | Atractylodis Macrocephalae Rhizoma -> Saposhnikoviae Radix | 0.693548387 |
| 8 | Atractylodis Macrocephalae Rhizoma, Saposhnikoviae Radix -> Astragali Radix | 0.88372093 |
| 9 | Astragali Radix, Saposhnikoviae Radix -> Atractylodis Macrocephalae Rhizoma | 0.745098039 |
| 10 | Astragali Radix, Atractylodis Macrocephalae Rhizoma -> Saposhnikoviae Radix | 0.826086957 |
| 11 | Saposhnikoviae Radix -> Astragali Radix, Atractylodis Macrocephalae Rhizoma | 0.644067797 |
| 12 | Atractylodis Macrocephalae Rhizoma -> Astragali Radix, Saposhnikoviae Radix | 0.612903226 |
Fig. 5.
Network chart of commonly used medicine combinations in TCM preventive oral prescriptions for COVID-19.
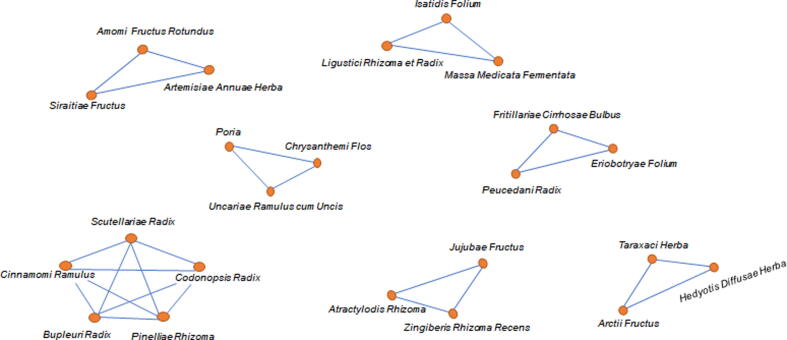
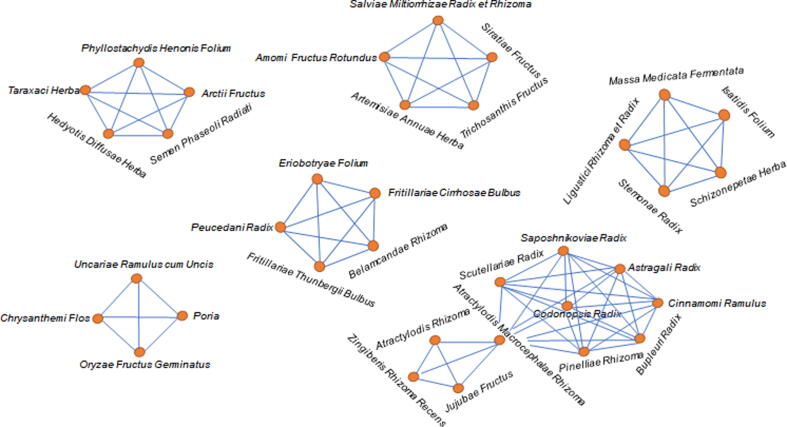
3.5. New prescription analysis based on core combination of entropy clustering of complex systems and unsupervised entropy hierarchy clustering
In the “Analysis of new prescriptions” module of Auxiliary Platform of Traditional Chinese Medicine Inheritance, when the correlation coefficient was set as 8 while the penalty coefficient was set as 2, we got 14 core combinations including 3–5 TCMs by the complex system entropy cluster analysis, such as Saposhnikoviae Radix and Astragali Radix and Atractylodis Macrocephalae Rhizoma, Pinelliae Rhizoma and Cinnamomi Ramulus and Codonopsis Radix and Scutellariae Radix and Bupleuri Radix, Eriobotryae Folium and Peucedani Radix and Fritillariae Cirrhosae Bulbus, etc, as shown in Table 4. Then their network diagrams were generated as shown in Fig. 6. On this basis, we extracted medicine-related combinations to furtherly cluster to obtain six new prescriptions by the unsupervised entropy hierarchical clustering algorithm, and generate their network diagrams, such as Phyllostachydis Henonis Folium and Taraxaci Herba and Semen Phaseoli Radiati and Arctii Fructus and Hedyotis Diffusae Herba, Dendrobii Caulis and Acori Tatarinowii Rhizoma and Polygonati Odorati Rhizoma and Angelicae Dahuricae Radix and Crataegi Fructus, Saposhnikoviae Radix and Astragali Radix and Atractylodis Macrocephalae Rhizoma and Pinelliae Rhizoma and Codonopsis Radix and Scutellariae Radix and Bupleuri Radix, etc, as shown in Table 5 and Fig. 7 for details.
Table 4.
Core combinations of TCM preventive oral prescriptions for COVID-19 based on complex system entropy cluster.
| No. | Core combinations |
|---|---|
| 1 | Amomi Fructus Rotundus_Salviae Miltorrhizae Radix et Rhizoma_Trichosanthis Fructus |
| 2 | Belamcandae Rhizoma_Eriobotryae Folium_Fritillariae Thunbergii Bulbus |
| 3 | Phyllostachydis Henonis Folium_Taraxaci Herba_Semen Phaseoli Radiati |
| 4 | Schizonepetae Herba_Massa Medicata Fermentata_Stemonae Radix |
| 5 | Poria_Chrysanthemi Flos_Oryzae Germinatus Fructus |
| 6 | Atractylodis Rhizoma_Jujubae Fructus_Atractylodis Macrocephalae Rhizoma |
| 7 | Saposhnikoviae Radix_Astragali Radix_Atractylodis Macrocephalae Rhizoma |
| 8 | Amomi Fructus Rotundus_Artemisiae Annuae Herba_Siraitiae Fructus |
| 9 | Eriobotryae Folium_ Peucedani Radix_Fritillariae Cirrhosae Bulbus |
| 10 | Taraxaci Herba_Arctii Fructus_Hedyotis Diffusae Herba |
| 11 | Massa Medicata Fermentata_Isatidis Folium_Ligustici Rhizoma et Radix |
| 12 | Poria_Chrysanthemi Flos_Uncariae Ramulus cum Uncis |
| 13 | Atractylodis Rhizoma_Jujubae Fructus_Zingiberis Rhizoma Recens |
| 14 | Pinelliae Rhizoma_Cinnamomi Ramulus_Codonopsis Radix_Scutellariae Radix_Bupleuri Radix |
Fig. 6.
Network diagrams of Core combinations of preventive oral prescriptions for COVID-19 based on complex system entropy cluster.
Table 5.
New prescriptions for prevention of COVID-19 based on entropy hierarchical clustering.
| No. | New prescriptions |
|---|---|
| 1 | Amomi Fructus Rotundus_Salviae Miltorrhizae Radix et Rhizoma_ Trichosanthis Fructus_Artemisiae Annuae Herba_Siraitiae Fructus |
| 2 | Belamcandae Rhizoma_Eriobotryae Folium_Fritillariae Thunbergii Bulbus_Peucedani Radix_Fritillariae Cirrhosae Bulbus |
| 3 | Phyllostachydis Henonis Folium_Taraxaci Herba_Semen Phaseoli Radiati_Arctii Fructus_Hedyotis Diffusae Herba |
| 4 | Schizonepetae Herba_Massa Medicata Fermentata_Stemonae Radix_Isatidis Folium_Ligustici Rhizoma et Radix |
| 5 | Poria_Chrysanthemi Flos_Oryzae Fructus Germinatus_Uncariae Ramulus cum Uncis |
| 6 | Atractylodis Rhizoma_ Jujubae Fructus_Atractylodis Macrocephalae Rhizoma_Zingiberis Rhizoma Recens |
| 7 | Saposhnikoviae Radix_Astragali Radix_Atractylodis Macrocephalae Rhizoma_Pinelliae Rhizoma_Cinnamomi Ramulus_Codonopsis Radix_Scutellariae Radix_Bupleuri Radix |
Fig. 7.
Network diagrams of new prescriptions for prevention of COVID-19 based on entropy hierarchical clustering.
3.6. Analysis on usage of edible traditional Chinese medicinal materials, traditional Chinese medicinal materials for health food, new resources of food
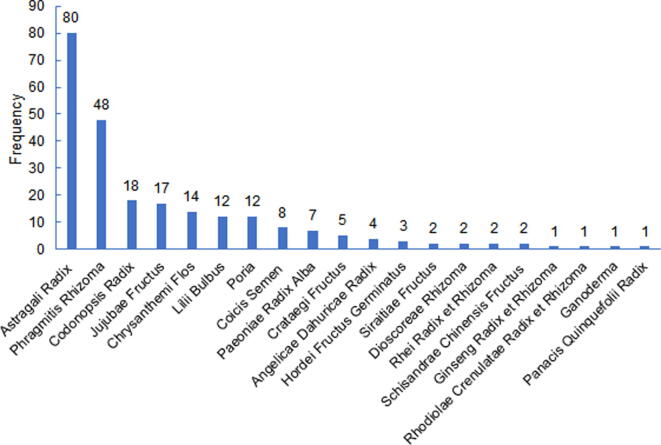
That a large of edible traditional Chinese medicinal materials, traditional Chinese medicinal materials for health food, new resources of food were widely used was a major characteristic of preventive oral prescriptions for COVID-19. According to statistics, a total of 35 species of edible traditional Chinese medicinal materials were used in preventive oral prescriptions for COVID-19. The top five edible traditional Chinese medicinal materials were Glycyrrhizae Radix et Rhizoma (86), Lonicerae Japonicae Flos (70), Platycodonis Radix (56), Pogostemonis Herba (48) and Phragmitis Rhizoma (48) in order of frequency of usage as shown in Fig. 8. A total of 31 traditional Chinese medicinal materials for health food were used in preventive oral prescriptions for COVID-19. The top five traditional Chinese medicinal materials for health food were Astragali Radix (80), Atractylodis Macrocephalae Rhizonma (62), Atractylodis Rhizoma (39), Ophiopogonis Radix (25) and Codonopsis Radix (18) in terms of frequency of usage as shown in Fig. 9. There were a total of 20 new resources of food being used in preventive oral prescriptions for COVID-19. The top five new resources of food in order of frequency of usage (Fig. 10) were Astragali Radix (80), Phragmitis Rhizoma (48), Codonopsis Radix (18), Jujubae Fructus (17) and Chrysanthemi Flos (14).
Fig. 8.
Usage of edible traditional Chinese medicinal materials in preventive oral prescriptions for COVID-19.
Fig. 9.
Usage of traditional Chinese medicinal materials for health food in preventive oral prescriptions for COVID-19.
Fig. 10.
Frequency of usage of new resources of food in preventive oral prescriptions for COVID-19.
3.7. Comparative statistical analysis on edible traditional Chinese medicinal materials and non-edible traditional Chinese medicinal materials in preventive oral prescriptions for COVID-19
Edible traditional Chinese medicinal materials and non-edible traditional Chinese medicinal materials were separated in preventive oral prescriptions for COVID-19. And the frequency, efficacy classification and dosage of these two classes of medicines were respectively compared and analyzed. The results showed that the frequency of usage of edible traditional Chinese medicinal materials was obviously more than that of non-edible traditional Chinese medicinal materials. In terms of efficacy classification, they all involve medicines with high frequency of usage, such as herbal medicines for invigorating qi, herbal medicines for clearing heat and removing toxic substance, herbal medicines for dispelling pathogenic wind-heat, aromatic herbal medicines for resolving damp, herbal medicines for invigorating yin and herbal medicines for dispelling pathogenic wind-cold. In terms of dose, the average dose, the most common dose and the common dose range of the high-frequency edible traditional Chinese medicinal materials and non-edible traditional Chinese medicinal materials were basically within the prescribed range of pharmacopoeia, which met the requirements of safe medicine use. The specific usages were shown Table 6, Table 7, Table 8.
Table 6.
Comparison on frequency of top 10 single edible traditional Chinese medicinal materials and non-edible traditional Chinese medicinal materials.
| Ranking | Edible traditional Chinese medicinal materials | Frequency | Proportion of medicine use frequency of edible traditional Chinese medicinal materials | Proportion of medicine use frequency of all medicines | Ranking | Non-edible traditional Chinese medicinal materials | Frequency | Proportion of medicine use frequency of non-edible traditional Chinese medicinal materials | Proportion of medicine use frequency of all medicines |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Glycyrrhizae Radix et Rhizoma | 86 | 15.50 | 7.03 | 1 | Astragali Radix | 80 | 11.98 | 6.54 |
| 2 | Lonicerae Japonicae Flos | 70 | 12.61 | 5.72 | 2 | Atractylodis Macrocephalae Rhizoma | 62 | 9.28 | 5.07 |
| 3 | Platycodonis Radix | 56 | 10.09 | 4.58 | 3 | Saposhnikoviae Radix | 60 | 8.98 | 4.91 |
| 4 | Pogostemonis Herba | 48 | 8.65 | 3.92 | 4 | Forsythiae Fructus | 52 | 7.78 | 4.25 |
| 5 | Phragmitis Rhizoma | 48 | 8.65 | 3.92 | 5 | Atractylodis Rhizoma | 39 | 5.84 | 3.19 |
| 6 | Citri Reticulatae Pericarpium | 34 | 6.13 | 2.78 | 6 | Scutellariae Radix | 27 | 4.04 | 2.21 |
| 7 | Perillae Folium | 24 | 4.32 | 1.96 | 7 | Ophiopogonis Radix | 25 | 3.74 | 2.04 |
| 8 | Mori Folium | 23 | 4.14 | 1.88 | 8 | Dryopteridis Crassirhizomatis Rhizoma | 24 | 3.59 | 1.96 |
| 9 | Zingiberis Rhizoma Recens | 18 | 3.24 | 1.47 | 9 | Bupleuri Radix | 18 | 2.69 | 1.47 |
| 10 | Jujubae Fructus | 17 | 3.06 | 1.39 | 10 | Codonopsis Radix | 18 | 2.69 | 1.47 |
Table 7.
Comparison on frequency and proportion of efficacy categories of top 10 edible traditional Chinese medicinal materials and non-edible traditional Chinese medicinal materials.
| Ranking | Efficacy categories of edible traditional Chinese medicinal materials | Frequency | Proportion of medicine use frequency of edible traditional Chinese medicinal materials (%) | Proportion of medicine use frequency of all medicines (%) | Ranking | Efficacy categories of non-edible traditional Chinese medicinal materials | Frequency | Proportion of medicine use frequency of non-edible traditional Chinese medicinal materials (%) | Proportion of medicine use frequency of all medicines (%) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Qi-invigorating medicines | 107 | 19.28 | 1.58 | 1 | Qi-invigorating medicines | 172 | 25.75 | 2.11 |
| 2 | Heat-clearing and toxic substance-removing medicines | 77 | 13.87 | 1.13 | 2 | Heat-clearing and toxic substance-removing medicines | 86 | 12.87 | 1.05 |
| 3 | Wind-heat-dispersing medicines | 67 | 12.07 | 0.99 | 3 | Wind-cold-dispersing medicines | 80 | 11.98 | 0.98 |
| 4 | Hot-phlegm clearing and dissolving medicines | 56 | 10.09 | 0.83 | 4 | Yin-supplementing medicines | 56 | 8.38 | 0.69 |
| 5 | Heat-clearing and fire-purging medicines | 56 | 10.09 | 0.83 | 5 | Resolving-damp medicines | 54 | 8.08 | 0.66 |
| 6 | Resolving-dampness medicines | 53 | 9.55 | 0.78 | 6 | Wind-heat-dispersing medicines | 32 | 4.79 | 0.39 |
| 7 | Wind-cold-dispersing medicines | 46 | 8.29 | 0.68 | 7 | Heat-clearing and dampness-drying medicines | 28 | 4.19 | 0.34 |
| 8 | Qi-regulating medicines | 34 | 6.13 | 0.50 | 8 | Worm-expelling medicines | 27 | 4.04 | 0.33 |
| 9 | Edema-alleviating diuretic medicines | 21 | 3.78 | 0.31 | 9 | Other categories | 27 | 4.04 | 0.33 |
| 10 | Yin-supplementing medicines | 14 | 2.52 | 0.21 | 10 | Heat-clearing and blood-cooling medicines | 16 | 2.40 | 0.20 |
Table 8.
Comparison on dosage of top 10 single edible traditional Chinese medicinal materials and non-edible traditional Chinese medicinal materials.
| Ranking | Edible traditional Chinese medicinal materials | Frequency | Average dose (g) | Most commonly used dose (g) | Dose distribution interval (g) | Common dose range (g) | Pharmacopoeia dose (g) | Ranking | Non-edible traditional Chinese medicinal materials | Frequency | Average dose (g) | Most commonly used dose (g) | Dose distribution interval (g) | Common dose range (g) | Pharmacopoeia dose (g) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Glycyrrhizae Radix et Rhizoma | 86 | 5.48 | 6 | 1.5–30 | 3–6 | 2–10 | 1 | Astragali Radix | 80 | 14.11 | 15 | 3–30 | 9–20 | 9–30 |
| 2 | Lonicerae Japonicae Flos | 70 | 9.31 | 10 | 6–15 | 3–15 | 6–15 | 2 | Atractylodis Macrocephalae Rhizoma | 62 | 10.10 | 10 | 3–22.5 | 6–15 | 6–12 |
| 3 | Platycodonis Radix | 56 | 8.21 | 10 | 2–12 | 4.4–30 | 3–10 | 3 | Saposhnikoviae Radix | 60 | 8.06 | 10 | 3–15 | 3–10 | 5–10 |
| 5 | Pogostemonis Herba | 48 | 8.50 | 10 | 3–15 | 6–10 | 3–10 | 4 | Forsythiae Fructus | 52 | 10.71 | 10 | 5–30 | 9–15 | 6–15 |
| 4 | Phragmitis Rhizoma | 48 | 14.74 | 15 | 2–30 | 4.8–10 | 15–30 | 5 | Atractylodis Rhizoma | 39 | 8.36 | 10 | 3–12 | 4.6–12 | 3–9 |
| 6 | Citri Pericarpium Reticulatae | 34 | 6.94 | 10 | 2–15 | 2–10 | 5–10 | 6 | Scutellariae Radix | 27 | 8.93 | 6 | 3–15 | 5–15 | 3–10 |
| 7 | Perillae Folium | 24 | 7.69 | 6 | 2–15 | 3.6–10 | 5–10 | 7 | Ophiopogonis Radix | 25 | 8.28 | 6 | 3–15 | 3.8–15 | 6–12 |
| 8 | Mori Folium | 23 | 6.17 | 3 | 3–15 | 2.2–10 | 5–10 | 8 | Dryopteridis Crassirhizomatis Rhizoma | 24 | 9.21 | 10 | 2–20 | 5–15 | 4.5–9 |
| 9 | ZingiberisRhizoma Recens | 18 | 6.61 | 2 | 2–30 | 2–12.3 | 3–10 | 9 | Bupleuri Radix | 18 | 10.78 | 10 | 6–18 | 6–15 | 3–10 |
| 10 | Jujubae Fructus | 17 | 6.71 | 6 | 1–10 | 4–10 | 6–15 | 10 | Codonopsis Radix | 18 | 10.61 | 12 | 5–30 | 5–12.9 | 9–30 |
3.8. Statistics on toxic or contraindicated TCMs used in preventive oral prescriptions for COVID-19
Through statistical analysis on the TCMs used in preventive oral prescriptions for COVID-19 by consulting Chinese Pharmacopoeia and Chinese Materia Media, it was found that four medicines were clearly considered as toxic, another five were contraindicated medicines, and two were the medicines that cannot be used for the patients with special constitutions, as shown in Table 9.
Table 9.
Statistics on toxic or contraindicated TCMs used in preventive oral prescriptions for COVID-19.
| No. | TCM names | Toxicity/Contraindication |
|---|---|---|
| 1 | Dryopteridis Crassirhizomatis Rhizoma | Slight toxic |
| 2 | Pinelliae Rhizoma | Toxic |
| 3 | Armeniacae Semen Amarum | Slight toxic |
| 4 | Rhei Radix et Rhizoma | Cautiously used during women in pregnancy, menstrual period and lactation period |
| 5 | Moutan Cortex | Cautiously used during women in pregnancy |
| 6 | Polygoni Cuspidati Rhizoma et Radix | Cautiously used during women in pregnancy |
| 7 | Curcumae Rhizoma | Forbidden during women pregnancy |
| 8 | Pyrrosiae Folium | Forbidden during patients with yin deficiency and no damp heat |
| 9 | Trichosanthis Radix | Cautiously used during women in pregnancy |
| 10 | Paridis Rhizoma | Slight toxic, and forbidden during patients with sores and ulcers of yin Syndrome |
| 11 | Violae Herba | Forbidden for patients with the constitutions of deficient-cold |
3.9. Statistics on TCM preventive oral prescriptions for COVID-19 containing edible traditional Chinese medicinal materials, traditional Chinese medicinal materials for health food, new sources of food and toxic TCMs
In the 157 preventive oral prescriptions for COVID-19, there were 88 prescriptions composed of edible traditional Chinese medicinal materials, traditional Chinese medicinal materials for health food, new sources of food or other medicines, accounting for 56.05%. And there were 39 prescriptions containing toxic medicines accounting for 24.84%. There were 30 prescriptions composed only of edible traditional Chinese medicinal materials, traditional Chinese medicinal materials for health food, new sources of food, accounting for 19.11%. In these 157 prescriptions, there were 56 prescriptions composed of edible traditional Chinese medicinal materials, traditional Chinese medicinal materials for health food, new sources of food and other medicines, accounting for 35.67%; 27 prescriptions composed of edible traditional Chinese medicinal materials, traditional Chinese medicinal materials for health food and other medicines, accounting for 17.19%; 10 prescriptions that only consist of edible traditional Chinese medicinal materials, traditional Chinese medicinal materials for health food and new sources of food, accounting for 6.37%, and 10 prescriptions that are only consist of edible traditional Chinese medicinal materials and traditional Chinese medicinal materials for health food, accounting for 6.37%; 11 prescriptions composed of edible traditional Chinese medicinal materials, traditional Chinese medicinal materials for health food, toxic medicines and other medicines, accounting for 7.01%. The above five types of prescriptions accounted for the majority, and the others are shown for details in Table 10.
Table 10.
Frequency and proportion of TCM preventive oral prescriptions for COVID-19 containing medicinal and edible medicines, medicines for health food, medicines as new food resources and toxic TCMs.
| No. | Prescription Categories | Category of prescription medicines | Frequency | Total Frequency | Proportion |
|---|---|---|---|---|---|
| 1 | Prescriptions composed only of edible traditional Chinese medicinal materials, traditional Chinese medicinal materials for health food and new resources of food | Edible traditional Chinese medicinal materials, traditional Chinese medicinal materials for health food, new resources of food | 10 | 30 | 19.11% |
| 2 | Edible traditional Chinese medicinal materials, new resources of food | 3 | |||
| 3 | Edible traditional Chinese medicinal materials | 7 | |||
| 4 | Edible traditional Chinese medicinal materials, traditional Chinese medicinal materials for health food | 10 | |||
| 5 | Prescriptions composed of edible traditional Chinese medicinal materials, traditional Chinese medicinal materials for health food, new resources of food or other medicines | Edible traditional Chinese medicinal materials, new resources of food and other medicines | 2 | 88 | 56.05% |
| 6 | Edible traditional Chinese medicinal materials, new resources of food, traditional Chinese medicinal materials for health food and other medicines | 56 | |||
| 7 | Edible traditional Chinese medicinal materials and other medicines | 1 | |||
| 8 | Edible traditional Chinese medicinal materials, traditional Chinese medicinal materials for health food and other medicines | 27 | |||
| 9 | Traditional Chinese medicinal materials for health food, new resources of food and other medicines | 1 | |||
| 10 | Traditional Chinese medicinal materials for health food and other medicines | 1 | |||
| 11 | Prescriptions containing toxic medicines | Edible traditional Chinese medicinal materials, new resources of food, toxic medicines and other medicines | 2 | 39 | 24.84% |
| 12 | Edible traditional Chinese medicinal materials, traditional Chinese medicinal materials for health food, new resources of food, toxic and other medicines | 26 | |||
| 13 | Edible traditional Chinese medicinal materials, traditional Chinese medicinal materials for health food, toxic medicines and other medicines | 11 |
Note: Other medicines refer to non-edible traditional Chinese medicinal materials, non-traditional Chinese medicinal materials for health food, non-new resources of food and non-toxic medicines.
4. Discussion
4.1. Understanding of oral administration of taking TCMs to prevent epidemic disease
COVID-19 belongs to the category of “epidemic of dampness toxin”, whose pathological core is to feel the pathogenic factor of dampness-toxin. The disease location of COVID-19 lies in the lungs, and the basic pathogenesis is characterized by “dampness, toxin, stagnate and closure”(Wang et al, 2020). Pestilential pathogens are kind of exogenous pathogens with strong infectivity. They are also called pestilential qi, toxic qi, poisonous qi, epidemic qi and special pathogens. The disease syndromes of pestilential qi vary with different pestilential pathogens, which include many contagious in modern medicine such as smallpox, cholera, plague, SARS, dengue fever, erysipelas of the face, mumps, bacillary dysentery and so on. The causes for the occurrence and epidemic of pestilential pathogens includes abnormal climates, environmental and food pollution, lack of strict preventive measures, social factors, etc. Pestilential qi has the characteristics of strong infectivity, easy epidemic, sudden onset, critical illness, one qi and one disease. And the diseases caused by pestilential qi have similar symptoms (Zheng, 2016). The Yellow Emperor's Classic of Internal Medicine records that “Keep healthy, do not be evil.” Therefore, in the aspect of the prevention of pestilential qi, it’s the key to improve the body's own immunity. Prevention plays an important role in the change of the epidemic situation, which is even more important than “treatment”(Ding, Wang, & Lin, 2020). The theory and practice of TCM to prevent epidemic diseases is unique in the world medical system.“ Avoid the pathogenic qi” and “Keep healthy qi inside” are the core for TCM to prevent epidemic diseases. The principle of prevention for epidemic diseases can be summarized as prevention before disease, prevention of change after disease and prevention of relapse after disease (Zhong and Yang, 2011, Chen, 2011). In the process of epidemic prevention, TCM intervention should be carried out at the same time of using conventional prevention methods to avoid the invasion and transformation of pestilential qi. In addition, it is the key link to prevent for epidemic disease by TCM oral administration. General Treatise on Causes and Manifestations of All Diseases emphasizes that epidemics can be prevented before they occur, and “pretake medicine and prevent it”. Several preventive prescriptions of epidemics are listed in Handbook of Prescriptions for Emergencies· Several Prescriptions for Treating Epidemic Disease of Dampness Toxin. “if there are epidemics in the world, they should be prevented by something produced in nature.” was put forward by Si-miao Sun. Tian-shi Ye believes that “before suffering from the disease, people usually have misgivings, and it is essential to take the aromatic herbal medicines for resolving damp and herbal medicines for invigorating immediately” and so on (Wang, 2011). Oral administration has the advantages of safety, convenience and patient compliance, which is the most common route of administration in daily life. For the above reasons, oral TCMs has played an important role in the prevention of COVID-19.
4.2. Medication rules and characteristics of TCM preventive oral prescriptions for COVID-19
4.2.1. Efficacy classification of TCMs used in TCM preventive oral prescriptions for COVID-19
TCM holds that “where evil comes together, the vital qi will be deficient”. To prevent COVID-19, there were a large number of herbal medicines for invigorating qi used in TCM preventive oral prescriptions for COVID-19 to invigorate qi and strengthen the spleen, enhance the body's healthy qi and resolve damp, including Glycyrrhizae Radix et Rhizoma, Astragali Radix and Atractylodis Macrocephalae Rhizoma. Modern studies have shown that Glycyrrhizae Radix et Rhizoma, Astragali Radix and Atractylodis Macrocephalae Rhizoma all have the pharmacological effects of enhancing and regulating human immunity (Li et al., 2019, Hu and Zhang, 2019, Zhang and Zuo, 2018). The extensive application of herbal medicines for dispelling pathogenic wind-cold in these prescriptions was intended to relieve exterior syndromes such as fever, headache and aversion to cold. Saposhnikoviae Radix, “general medicine for dispelling pathogenic wind”, was most widely used in these prescriptions. Modern studies have confirmed that it has antipyretic and analgesic effects (Liu et al., 2017). Dampness is the most fundamental pathological factor of COVID-19. The purpose of using a lot of aromatic herbal medicines for resolving damp such as Pogostemonis Herba and Atractylodis Rhizoma is to focus on eliminating damp in the body and outside. The reason why Lonicerae Japonicae Flos, Forsythiae Fructus and other heat clearing and detoxification medicines were used together with aromatic herbal medicines for resolving dampness was that it has heat clearing effect on the one hand, and it has obvious antiviral effect on the other hand. Since the pathogenesis of COVID-19 lies in “damp, heat, toxicity and stagnation”, prevention of COVID-19 should adopt the treatments of nourishing yin, moistening the lung, promoting the production of fluid, moistening dryness, and releasing the stagnated lung-qi. Therefore, Platycodonis Radix was used to release the stagnated lung-qi, expel phlegm, relieve sore-throat and promote pus discharge; Phragmitis Rhizoma was used to clear heat, product fluid, arrest vomiting in attribution.
4.2.2. Characteristics of four-nature and five-taste of TCMs used in preventive oral prescriptions for COVID-19
The properties of Chinese herbal medicine refer to the characters and feature of the effect of Chinese herbal medicine. The theory of the properties, the core of fundamental theory of Chinese herbal medicine, includes five aspects: four natures, five tastes, attributive meridians, properties of ascending and descending, floating and sinking as well as the toxicity. Four natures refer to four properties of herbal medicine, namely, cold, hot, warm and cool. It is one of the most important concepts concerning the character of effect. The property of TCMs is closely related to the therapeutic methods and principles. Shennong's classic of Herbology says: “cold and cool medicines are used to treat yang-heat syndrome, while hot and warm medicines are used to treat yin-cold syndrome.” It can be seen from the analysis of the four-nature and five-taste of TCMs used in preventive oral prescriptions for COVID-19 that they were mostly cold (59), warm (38), and mild (21) in nature. For the pathogenesis of COVID-19, there are two judgments which are cold-dampness obstructing lung and heat-dampness accumulating lung. So in the prevention, it should be treated according to the syndrome differentiation of cold-dampness and heat-dampness constitutions. Some herbal medicines that have mild effects without predominant cold or hot nature are considered as mild medicine. From the perspective of the synergies of TCMs, when a mild medicine is used with cold medicines, the mild medicine will have the same properties as a cold medicine; when it is used with warm medicines, the mild medicine will have the same properties as a warm medicine (Deng, 2007). After taking mild medicines, according to the different pathological conditions of the body, mild medicines can reconcile and balance the qi and blood in zang-fu organs, stimulate the body's own ability to reestablish yin and yang equilibrium, and promote the movement of yin and yang to restore the state of relative equilibrium of yin and yang. Mild medicines can play a therapeutic role in the treatment of diseases without damaging the body's vital qi, and are widely used in the prevention of epidemic disease. Five tastes originally refer to the actual tastes of herbs and foods. The tastes of herbal medicines are determined by their actual tastes as well as the effects of herbs. Therefore, five-taste reflects the effective ranges of herbal medicines. Sweet taste can tonify, regulate middle-jiao, relieve spasm as well as moderate medicinal properties. Sweet medicine can provide raw materials that are lacking in the recovery and treatment of various types of deficiency syndromes, provide energy for life activities and the body to repair lesions, and stimulate and improve the body's physiological functions (Hong & Cheng, 2003). Herbal medicines for invigorating are the most frequently used medicines in the TCM oral prescriptions for the prevention of COVID-19. Most of them have sweet taste, can improve immune function, and promote and regulate humoral immunity and cellular immunity (Zhu & Lou, 2011). Sweet medicines also have the effects of slowing down the acting speed and prolong the acting time of the main medicines in prescriptions. Bitter taste can dry, and dry means drying dampness and it is used for damp-syndrome. Bitter taste can be divided into bitter warm and bitter cold. Bitter warm herbal medicines are used for cold-damp syndrome, such as Atractylodis Rhizoma, Magnoliae Officinalis Cortex, etc, whereas bitter cold ones are used for dampness-heat syndrome, such as Coptidis Rhizoma, Phellodendri Chinensis Cortex, etc. Acrid taste has the effects of dispersing, promoting qi and blood circulation. Generally, herbal medicines for relieving exterior syndromes, herbal medicines for treating qi and blood stagnated syndromes and aromatic herbal medicines for resolving damp are acrid. Since COVID-19 belongs to the category of “dampness toxin epidemic”, a large number of bitter and acrid medicines were used in preventive oral prescriptions for COVID-19 in order to remove damp and relieve exterior syndromes.
4.2.3. Characteristics of meridian attribution of TCMs used in preventive oral prescriptions for COVID-19
Attribution refers to the domains of medicinal action whereas meridian refers to the outline of zang-fu organs and collaterals. Meridian attribution explains the location where herbal medicines act. Meridian attribution reflects the curative effects of herbal medicines on some special disorders of zang-fu organs and meridians. Grasping the medicinal meridian attribution will improve the correctness of medicinal application. The TCMs used in the TCM oral prescriptions for the prevention of COVID-19 mostly attribute to the lung (80), stomach (57), and spleen (40) meridians. The medicines attributing to the three meridians can promote the metaplasia of vital qi and the metabolism of damp in the body. Therefore, taking these medicines can fundamentally strengthen the body and eliminate the pathogenic factors to prevent COVID-19. Pathogenesis refers to the course of the onset of a disease. In Chinese medicine, the occurrence of disease involves two aspects: vital qi and pathogenic factors. The invasion of the pathogenic factors is an important factor causing disease while the deficiency of vital qi is the intrinsic factor. When the pathogenic factors defeat the vital qi, disease occurs. Under certain circumstances, pathogenic qi can play a leading role in disease onset, and “avoiding poisonous factors” is important in health maintenance to prevent the occurrence of disease. Vital qi has the functions of preventing the invasion of exogenous pathogenic factors from entering the body, resisting pathogenic factors to drive it out during the disease occurrence, restoring of health after disease occurring or from weakness, maintaining the normal structure and function of viscera and meridians. Therefore, it is an important content of preventive treatment of disease in TCM to invigorate vital qi. The generation and distribution of qi in human body are closely related to the physiological functions of spleen, stomach and lung. The spleen and stomach from an exterior-interior relation through their meridian’s connection and affiliation. The spleen governs transportation and transformation while the stomach control reception and digestion. They both cooperate each other in digestion and absorption of food, and in the transformation of essence of water and grain. And the main physiological functions of the lung are to dominate qi, control respiration, smooth water passage, and assemble vessels. The lung dominating qi and controlling respiration is shown in two ways: taking charge of the qi in respiration and operating the qi of the whole body. Lung qi can enter the respiratory tract to make the human body breathe normally, flows into vessels to make the qi and blood run smoothly, accumulate in Dantian to promote the generation of primordial qi. The secondary pathogenesis of COVID-19 is that yin-fire gathered in the lung, while the root pathogenesis is the weakness of the spleen and stomach (Ling et al., 2020). The pathological core of COVID-19 is “dampness toxin”. The relationships between lung and spleen are mainly reflected on the coordination between the generation of qi and water metabolism. As for the fluid metabolism, the lung regulates the water passage and belongs to the upper source of water, while the spleen transforms and transports water to guarantee generation and distribution of water. The lung distributes water to all parts of the body and the spleen absorbs and transports water as well as permeates water upwards to lung. The lung and spleen need to cooperate harmoniously in order to participate the fluid metabolism smoothly.
4.2.4. Analysis of association rules and new prescription of TCM preventive oral prescriptions for COVID-19
The synergy of herbal medicines means to match and combine more than two herbal medicines according to the requirement of treatment and the medicinal property. It is conducive to apply herbal medicines correctly, fully realize their therapeutic effects, and ensure their safety. By the analysis of the prescription-formulating principles based on association rules, eight commonly used medicine combinations in preventive oral prescriptions for COVID-19 were obtained, involving six medicines such as Astragali Radix, Saposhnikoviae Radix, Atractylodis Macrocephalae Rhizoma, Forsythiae Fructus, Lonicerae Japonicae Flos and Platycodonis Radix. They are mainly the medicine combinations in Yupingfeng San. These medicine combinations were arranged in order of frequency from highest to lowest: Astragali Radix and Saposhnikoviae Radix (51), Astragali Radix and Atractylodis Macrocephalae Rhizoma (46), Atractylodis Macrocephalae Rhizoma and Saposhnikoviae Radix (43), Astragali Radix and Atractylodis Macrocephalae Rhizoma and Saposhnikoviae Radix (38), Forsythiae Fructus and Astragali Radix (37), Lonicerae Japonicae Flos and Astragali Radix (35), Astragali Radix and Platycodonis Radix (33), Lonicerae Japonicae Flos and Saposhnikoviae Radix (31). In Yupingfeng San, Astragali Radix is sweet in taste and warm in nature, which can tonify the spleen and lung internally, consolidate superficial resistance to arrest sweating, and used as monarch medicine; Atractylodis Macrocephalae Rhizoma has the actions of invigorating qi, strengthening the lung by the way of reinforcing the spleen, acting as minister medicine to improve the effect of Astragalis Radix on tonifying qi and strengthening exterior. The synergy of the two medicines can make qi plentiful to safeguard the body surface as well as tighten the skin and striae enough to keep sweat from escaping and resist the invasion of pathogens. Saposhnikoviae Radix can dispel wind, and when in compatibility with the rest two, build up body resistance and eliminate pathogenic factors as adjuvant medicine. The synergy of the three medicines has the characteristic of reinforcing the superficies while eliminating pathogenic factors without impairing the body resistance. Therefore, it is good for the patients with spontaneous perspiration because it replenishes qi, strengthens superficial resistance and arrests perspiration. As for those with general debility and apt to be attacked by wind, it can reinforce the body resistance to wind (Jia, 2016). Modern research has found that Yupingfeng San has some pharmacological activities such as immune regulation, anti-inflammatory, anti-cancer and regulation of the micro-ecological environment of the body (Wang et al., 2020). Forsythiae Fructus and Astragali Radix both have good effect in treating sores and ulcers. Forsythiae Fructus is a kind of heat-clearing and toxic substance-removing medicines, which has the functions of clearing heat, removing toxin substance, relieving abscess and promoting diuresis. It is acrid in taste and cold in nature, and attributes to the lung meridian, so it has the action of floating to disperse wind-heat. Astragali Radix is good at strengthening and consolidating body resistance, tonifying qi of spleen and lung. In addition, it has the actions of consolidating superficial resistance to arrest sweating, promoting diuresis, relieving edema, producing fluid, slaking thirst, dispersing stagnation, promoting tissue regeneration and wound healing. The synergy of Forsythiae Fructus and Astragali Radix has the action of promoting diuresis, clearing heat, removing toxic substance, strengthen the middle-jiao, removing the stagnation, which is exactly suitable for treating COVID-19 with the pathogenesis of “damp, heat, toxicity and stasis”.
Lonicerae Japonicae Flos is sweet in taste, cold in nature, which is good at clearing heart and stomach heat to eliminate carbuncle. It can disperse wind-heat to be used in affection of exogenous wind-heat and the initial stage of febrile disease. In addition, it has the actions of cooling the blood and ease the throat to treat the disease of the sore throat caused by upward attack of wind-heat. Lonicerae Japonicae Flos is used with Astragali Radix for skin infection, carbuncle. The two medicines used together have the dual effects of tonifying qi and clearing heat, which cannot produce heat while invigorating qi, and can clear away heat without damaging the vital qi of the human body, and make the action of promoting tissue regeneration and wound healing more effective. In addition, the synergy of them can invigorate qi, nourish yin, promote to expel internal toxin and pus, break blood-stasis and restore menstruation (Ding, 2001). Platycodonis Radix has the action of releasing the stagnated lung-qi, expelling phlegm, relieve sore-throat, promoting pus discharge. In clinical practice, it is used for cough due to wind-cold manifested as thin phlegm and stuffy nose, aversion to cold and headache, for pulmonary abscess manifested as pain in the chest, fever, hemoptysis, yellow phlegm with fishy smell. Truth-seeking Herbal Foundation calls it “boat medicine” because it can render other medicines to act on the upper-jiao. When Platycodonis Radix and Astragali Radix are used together, they cannot only remove the phlegm and pathogenic qi of the lung, but also replenish the deficiency of the lung to invigorate qi and strengthen exterior to reduce sweat. The synergy of the two medicines has the characteristics of the integration of dispersing the pathogenic factors on the upper and expelling the pathogenic damp on the lower, dispersing the pathogenic factors in the outer and tonifying the vital qi in the inner, strengthening the vital and dispelling the pathogen, releasing the stagnated lung-qi and invigorating the lung-qi. Lonicerae Japonicae Flos is good at clearing the pathogenic heat and toxin of lung, heat and stomach with sweet in taste and cold in nature, in addition, it has the actions of clearing away heat and tonifying. Atractylodis Macrocephalae Rhizoma can strengthen the spleen and stomach, dry dampness and promote diuresis to reduce edema and resolve phlegm. When used together, the two medicines can not only clear the pathogenic heat of the middle- and upper-jiao, but also invigorate the qi of the middle-jiao to dispel water and reduce edema, which can strengthen the vital and dispel the pathogen, and treat the branch and the root of disease simultaneously.
A prescription is composed of selected medicines and suitable doses based on syndrome differentiation for etiology and the composition of therapies in accordance with the principle of formulating a prescription. It serves as a chief means of treating diseases clinically. Based on entropy hierarchical cluster analysis, six new prescriptions were obtained, which were not only the prescriptions for relieving exterior syndrome and expelling pathogenic factors, but also the prescriptions for strengthening the body resistance to consolidate the constitution, as well as the prescriptions for expelling pathogenic factors and strengthening the body simultaneously to treat both principal and secondary aspect of disease. The prescription composed of Phyllostachydis Henonis Folium, Taraxaci Herba, Semen Phaseoli Radiati, Arctii Fructus and Hedyotis Diffusae Herba is a prescription for relieving exterior syndrome and expelling pathogenic factors. In the prescription, Phyllostachydis Henonis Folium can clear heat, produce fluid and promote diuresis; Taraxaci Herba has the actions of clearing heat, removing toxic substance, promoting diuresis and relieving stranguria; Hedyotis Diffusae Herba has the actions of clearing heat and relieving carbuncle, and expelling and relieving stranguria; Semen Phaseoli Radiati is used to clear heat, remove toxic substance, and eliminate summer-heat and promote diuresis. These four medicines are all herbal medicines for clearing heat, and all have the actions of clearing heat and removing toxic substance, and are beneficial to promote diuresis. And when used together, they can eliminate the pathogen factors of dampness, heat, toxins and blood stasis. Arctii Fructus is a herbal medicine for dispelling pathogenic wind-heat, which is used for the exterior syndrome of the affection of exogenous wind-heat with sore throat, cough, difficult expectoration. The synergy of all these medicines has the effect of relieving exterior syndrome and expelling the pathogenic factors.
The prescription composed of Atractylodis Rhizoma, Jujubae Fructus, Atractylodis Macrocephalae Rhizoma and Zingiberis Rhizoma Recens is used for strengthening the body resistance to consolidate the constitution. In this prescription, the three medicines of Atractylodis Rhizoma, Jujubae Fructus and Atractylodis Macrocephalae Rhizoma all have the effect of strengthening the spleen; Atractylodis Rhizoma and Atractylodis Macrocephalae Rhizoma also have the action of removing dampness; Zingiberis Rhizoma Recens has the actions of relieving exterior syndrome, warming middle-jiao to arrest vomiting. The main effect of this prescription is to strengthen the spleen to expel dampness. Ingredient-added Yupingfeng San is made by adding four TCMs, Codonopsis Radix, Bupleuri Radix, Scutellariae Radix, Pinelliae Rhizoma, on the basis of Yupingfeng San. And Yupingfeng San is composed of Astragali Radix, Atractylodis Macrocephalae Rhizoma, Saposhnikoviae Radix, which is used to expel pathogenic factors and strengthen the body simultaneously to treat both principal and secondary aspect of disease. This prescription is mainly composed of the medicines which are sweet in taste and warm in nature to invigorate qi and strengthen spleen, and secondly composed of the medicines which are acrid to disperse the pathogenic factors. The actions of strengthening the body resistance and dispersing pathogenic factors are both opposite and complementary to each other in Yupingfeng San. Codonopsis Radix added to this prescription enhance the Invigorating qi effect of Astragali Radix, and Bupleuri Radix was added to this prescription to enhance the relieving exterior syndrome effect of Saposhnikoviae Radix. And Scutellariae Radix and Pinelliae Rhizoma can be used together to dry dampness, clearing heat to treat the cases with damp-phlegm blocking the lung and accompanied with heat-syndrome which manifested as thick and yellow phlegm.
4.3. Universality and safety of TCM preventive oral prescriptions for COVID-19 epidemic disease
4.3.1. Application of TCMs with toxicity and contraindications
Toxicity refers to the harmful effects produced by herbal medicines on human body. Toxic herbal medicines refer to those that can easily induce toxic reaction and damage the function of human body and some tissues and organs. It is very important to recognize their toxicity to guide reasonable clinical application and ensure the safe use of herbal medicines. Through statistical analysis of the TCMs used in the preventive oral prescriptions for COVID-19, it was found that four medicines were clearly considered as toxic, another five were contraindicated medicines, and two were the medicines that cannot be used for the patients with special constitutions. Dryopteridis Crassirhizomatis Rhizoma is bitter in taste and cold in nature, has the actions of clearing heat, removing toxic substance, relieving bleeding and killing intestinal parasites. Modern research has found that the two species of medicinal Dryopteridis Crassirhizomatis Rhizoma have no obvious toxic effects within the range of medicinal use. And the phloroglucinol compounds such as foliaceae acid AB contained in Dryopteridis Crassirhizomatis Rhizoma have anti-viral and anti-tumor effects (Zhao et al., 2019); Pinelliae Rhizoma is good at drying the spleen to dissolve turbid dampness, warming the lung to dissolve cold-phlegm, warming the viscera and reducing cold and phlegm, descending gastric qi to relieve vomiting. It is considered to be an essential medicine for dissolving cold and wet phlegm, and relieving vomiting. The main toxic components of Pinelliae Rhizoma are needle-like calcium oxalate crystal and lectin protein (Wang & Liang, 2019). The amygdalin in Armeniacae Semen Amarum is a kind of cyanogenic glycoside. Under the action of emulsin, it can produce excessive hydrocyanic acid and cause poisoning (Fu & Ye, 2015). Paridis Rhizoma has the actions of clearing liver-fire, reducing swelling and relieving convulsion. However, Paris Polyphylla saponin has certain hepatotoxicity and hemolytic activity (Xiao, Yang & Li, 2019) and reproductive system toxicity, while paridin, paristyhnin and alkaloids can cause poisoning by excessive application, which is manifested as digestive system, nervous system and cardiac toxicity (Chen & Yan, 2012).
In addition, “arsenic has therapeutic effects, Glycyrrhizae Radix et Rhizoma also has toxic reactions”, although some TCMs have not been recorded in various literature as having toxic and side effects, adverse reactions have been reported from time to time in recent years. It has been reported that Glycyrrhizae Radix et Rhizoma also leads to several adverse reactions such as allergic reaction, glucocorticoid-like effect, injury of liver and kidney system (Wu & Chen, 2007). In terms of TCM, Uncariae Ramulus cum Uncis has obvious effects on calming wind, relieving convulsion and clearing the liver-heat to calm the liver. Clinical studies have found that it has a significant effect on lowering blood pressure to treat hypertension. However, modern pharmacological studies believe that Tianma Gouteng Yin is toxic. And under the effective dose of antihypertensive, rhynchophylla total alkaloids are hepatotoxic, and long-term use may cause death (Liu et al., 2014, Zhang et al., 2015). Pogostemonis Herba is considered to be an essential medicine for expelling pathogenic dampness. Its main components are patchouli oil, patchoulicalcohol and patchoulenone, which are teratogenic and cardiotoxic to the development of zebrafish embryo (Yang et al., 2015), and patchouli oil has certain ciliotoxicity. Long-term oral administration of Gardeniae Fructus can cause liver and kidney toxicity in rats (Wang, Zhou, Zhang, & Deng, 2017), and its main toxic component is geniposide (Yang et al., 2006). The androsin extracted from Belamcandae Rhizoma is toxic (Liu, Wu, Zhang, & Tian, 2011). Alisol C, 16,23-epoxy alisol B and alisol O in Alismatis Rhizoma may cause nephrotoxicity (Zhao, Lu, Zhang, & Zhang, 2011), long-term high dose oral administration of water extract of Alismatis Rhizoma can lead to chronic nephrotoxicity (Le et al., 2012). TCM preventive oral prescriptions for COVID-19 are mainly aimed at prevention, strengthening the body's vital qi and removing pathogenic qi from the body outside. Moreover, they should be taken for a long time and targeted at a wide range of people, so more attention should be paid to the rational application of medicines. Toxic TCMs should be used with caution or avoided, and non-toxic TCM with similar properties should be used instead of them. For potentially toxic medicines, such as Uncariae Ramulus cum Uncis and Gardeniae Fructus with liver and kidney toxicity, attention should also be paid to the safe range of medicine use, and the dosage should not be too much, or their processed products should be selected appropriately according to needs. In the process of medication, we should grasp the relationship between efficacy and safety. At the same time, it is particularly important to control the dose of TCMs, because the medicine toxicity is closely related to the dose, and some effective components of TCMs are also toxic components. Therefore, the dosage of each TCM used in preventive oral prescriptions for COVID-19 should be in line with the safe medicine use range of Chinese Pharmacopoeia, so as to ensure certain safety and play the role of disease prevention but non-toxicity. Some medicines in preventive oral prescriptions for COVID-19 are also cautiously used for pregnant women. Most of them have the effects of promoting blood circulation and removing blood-stasis, for example, Polygoni Cuspidati Rhizoma et Radix, Curcumae Rhizoma, Moutan Cortex; and some of them are herbal medicines for purgation such as Rhei Radix et Rhizoma. There are also a few medicines that cannot be used in preventive oral prescriptions for COVID-19 for the patients with special constitutions. For example, Pyrrosia Folium cannot be applied to patients with deficiency of yin and no damp-heat; and Violae Herba cannot be used in patients with deficiency-cold constitution. The formulation of preventive oral prescriptions for COVID-19 should vary from person to person, and we should formulate different prescriptions for different groups of people. Therefore, the preventive oral prescriptions for COVID-19 in various regions are different for adults, children and pregnant women, and the medicines and their dosages used are also different. The application of toxic and contraindicated medicines is also based on this. There are also some self-designed prescriptions that do not have specific applicable populations. If they are used improperly, there may be some potential safety hazards.
4.3.2. Application of edible traditional Chinese medicinal materials, traditional Chinese medicinal materials for health food, new resources of food
“Homology of medicine and food” means that some medicines have the dual attributes of food and medicine, which can be used as food and medicine, and have therapeutic effects on some diseases. National Health Commission of the People's Repulic of China has published a list of the raw materials of edible traditional Chinese medicinal materials in 2017, including 101 kinds of edible traditional Chinese medicinal materials, and another 113 kinds of traditional Chinese medicinal materials for health food (Yu, 2017). And new resources of food refer to newly developed, newly discovered, newly introduced materials that do not meet people's eating habits or only eaten in individual areas and meet the basic requirements of food (Wang, Gao, & Yang, 2006). There were 35 kinds of edible traditional Chinese medicinal materials used in preventive oral prescriptions for COVID-19, most of which were mostly acrid and sweet in taste and tend to nourish the body. Their tastes are easy to be accepted by patients. And they have the effects of anti-tumor and enhancing immunity, which are conducive to long-term use of disease prevention. High safety is the primary feature of edible traditional Chinese medicinal materials. They do not contain toxic ingredients and will not cause toxic and side effects to the body even if taken for a long time at conventional doses (Xing, Cheng, & Shen, 2018). In addition, there were 31 kinds of traditional Chinese medicinal materials for health food and 20 kinds of new resources of food in preventive oral prescriptions for COVID-19. As new resources of food, TCMs should also be safe. They do not contain toxic and harmful substances or unsafe factors that may damage or threaten human health. They cannot lead to acute and chronic poisoning or infectious diseases of consumers, and cannot produce hidden dangers that endanger the health of consumers and their offspring (Yang & Yu, 2008). Therefore, the similarities between edible traditional Chinese medicinal materials, traditional Chinese medicinal materials for health food and new resources of food are their significant safety, mild nature and suitable for long-term use, thus also suitable for oral medication for prevention of COVID-19. In the preventive oral prescriptions for COVID-19, these three types of medicines were used significantly more frequently than other medicines. In terms of dose, the average dose, the most common dose and the common dose range of the high-frequency edible traditional Chinese medicinal materials and non-edible traditional Chinese medicinal materials were basically within the prescribed range of pharmacopoeia, which met the requirements of safe medicine use. In effect, they are almost the same as other medicines, and play an important role in invigorating qi, expelling pathogenic dampness and relieving exterior syndrome. According to statistics, there were 157 preventive oral prescriptions for COVID-19, in which were composed of edible traditional Chinese medicinal materials, traditional Chinese medicinal materials for health food, new resources of food and other medicines, accounting for 56.05%, the largest proportion; 24.84% of 157 oral preventive oral prescriptions for COVID-19 contain toxic TCMs. We should pay attention to the dosage of the medicines used in these prescriptions, and should not take them for a long time; 19.11% of the 157 preventive oral prescriptions for COVID-19 were composed only of the edible traditional Chinese medicinal materials, traditional Chinese medicinal materials for health food, new resources of food. These prescriptions reflect the safety of medicine use for preventing COVID-19, and should be advocated in clinical practice.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
Authors thank for the support of the science foundation projects: a. Sino-Singapore Cooperation for Evaluating the Effectiveness and Application of Guangxi Zhuang/Yao Medicines against COVID-19 (No. GUIKE AB20036001); b. Anti-COVID-19 Drug Study Based on Chinese and Thai Medicinal Materials (No. GUIKE AB20036002); c. Guangxi Science and Technology Plan Project (No. GUIKE AA19254033, No. GUIKE AD19110155).
Contributor Information
Zheng-cai Du, Email: duzhengcai8@163.com.
Jia-gang Deng, Email: dengjg53@126.com.
References
- Chen M.F. Nanjing University of Traditional Chinese Medicine; Nanjing: 2011. Studies on the prevention of pestilential diseases of Chinese medicine. [Google Scholar]
- Chen Q., Yan S. Research progress on pharmacological effects and toxic reactions of Paris polyphylla. Herald of Medicine. 2012;31(07):886–888. [Google Scholar]
- Deng J.G. On the drug properties of “body and flat use bias” of ordinary drugs. World Chinese Medicine. 2007;2(5):302–303. [Google Scholar]
- Ding Y.Q. Compatibility and application of Radix Astragali and Flos Lonicerae Japonica. Guangming Journal of Chinese Medicine. 2001;16(93):6–7. [Google Scholar]
- Ding S.Y., Wang Q.G., Lin M.X. The enlightenment of the ancient and modern times traditional Chinese medicine literature on the prevention and treatment of coronavirus disease 2019 (COVID-19) Journal of Traditional Chinese Medicine. 2020;61(16):1397–1400. [Google Scholar]
- Fu M.D., Ye J. Analysis on toxicity of Armeniacae Amarum. Liaoning Journal of Traditional Chinese Medicine. 2015;42(2):382–384. [Google Scholar]
- Gao S.M., Ma Y., Yang F.W., Zhang J.H., Yu C.Q. Zhang Boli: Chinese medicine plays a role in the whole process of preventing and treating New Coronavirus pneumonia. Tianjin Chinese Medicine. 2020;37(2):121–124. [Google Scholar]
- Gao X.M. China Traditional Chinese Medicine Press; Beijing: 2002. Traditional chinese medicine. [Google Scholar]
- Hong Z.G., Cheng W.Y. Efficacy and chemical basis of sweet medicine. Chinese Archives of Traditional Chinese Medicine. 2003;21(9):1594–1595. [Google Scholar]
- Hu G.X., Zhang H.F. Analysis of pharmacology and clinical application value of Astragalus. Electronic Journal of Clinical Medical Literature. 2019;6(93):166–169. [Google Scholar]
- Jia B. China Press of Traditional Chinese Medicine; Beijing: 2016. Pharmacology of traditional chinese medical formulae. [Google Scholar]
- Li J., Li X., Cao M.M., Dong W.R., Jiang J.Q. Research progress in pharmacological actions of liquorice and proportion of couplet medicines in combination. Shanghai Journal of Traditional Chinese Medicine. 2019;53(7):83–87. [Google Scholar]
- Ling J.H., Xie S., Shen D.Z., Cong J., Gu Z.J., Li L., Cai G. Discussion on TCM prevention and treatment of COVID-19 based on Treatise on Spleen and Stomach. Shanghai Journal of Traditional Chinese Medicine. 2020;54(6):6–8. [Google Scholar]
- Liu S.L., Jiang C.X., Zhao Y., Xu Y.H., Wang Z., Zhang L.X. Advance in study on chemical constituents of Saposhnikovia divaricate and their pharmacological effects. Chinese Traditional and Herbal Drugs. 2017;48(10):2146–2152. [Google Scholar]
- Liu W., Wang Z.S., Zhang H., Zhang X., Jiang X.L., Gao Y.S. Hepatotoxicity of oral rhynchophylline total alkalodis in hypertensive rats. Chinese Pharmacological Bulletin. 2014;30(6):883–884. [Google Scholar]
- Liu Y.J., Wu B., Zhang Y., Tian X.Y. Toxicity componential analysis of Belamcanda chinensis (L.) DC. Journal of Shenyang Agricultural University. 2011;42(4):491–493. [Google Scholar]
- Le Z.Y., Song C.W., Jiang L.J., Qin X.L., Lu K.G., Fang N.B., Yu S.G. Study on chronic toxicity of aqueous extract of Alisma orientalis on kidney of mice of different sexes. Hubei Journal of Traditional Chinese Medicine. 2012;34(7):22–23. [Google Scholar]
- Wang L., Gao X.Q., Yang Y.X. The current situation and discussion on the novel food management in China. Chinese Journal of Health Inspection. 2006;13(04):263–265. [Google Scholar]
- Wang Q.R., Zhou B., Zhang Z.A., Deng Z.P. Time-and dose-effect of Gardenia jasminoides extract on hepatoxicity in rats. Chinese Traditional Patent Medicine. 2017;39(4):689–694. [Google Scholar]
- Wang W.Y. Nanjing University of Traditional Chinese Medicine; Nanjing: 2011. Concept and methods of epidemic prevention in ancient China and their modern applications research. [Google Scholar]
- Wang H.J., Liang J. Study on toxic components and processing detoxification mechanism of Pinellia ternata. Technology and Economic Guide. 2019;27(31):108–109. [Google Scholar]
- Wang Q.N., Lv W.L., Li J.M., Ni Y., Hu L.Z., Zhang R.X. Advances in experimental study and application of Yupingfeng Powder. Chinese Archives of Traditional Chinese Medicine. 2020;38(09):165–168. [Google Scholar]
- Wang Y.G., Qi W.S., Ma J.J., Ruan L.G., Lu Y.R., Li X.C., Liu Q.Q. Clinical features and syndrome differentiation of Novel Coronavirus Pneumonia in traditional Chinese medicine. Journal of Traditional Chinese Medicine. 2020;61(04):281–285. [Google Scholar]
- Wu Bo, Chen Yu-huang. Adverse reactions of glycyrrhizin. Lishizhen Medicine and Materia Medica Research. 2007;18(8):2042–2043. [Google Scholar]
- Xiao W.H., Yang Z.W., Li Y. Analysis of the cytotoxicity of polyphyllin I on human erythrocytes in vitro based on three-dimensional morphology of single cell. Chinese Journal of Blood Transfusion. 2019;32(4):334–338. [Google Scholar]
- Xing B.B., Cheng H.B., Shen W.X. Application discussion of edible source of Chinese materia medica used in malignant tumor prevention. Journal of Sichuan of Traditional Chinese Medicine. 2018;36(2):46–48. [Google Scholar]
- Yang Y.T., He Y.L., Zhang X., Lu J.Y., Li Y.Z., He B.X.…Cao Z.X. Safety evaluation of oil of Pogostemon cablin its main monomer in development of zebrafish embryos. Chinese Journal of Ethnomedicine and Ethnopharmacy. 2015;24(21):14–16. [Google Scholar]
- Yang H.J., Fu M.H., Wu Z.L., Liang R.X., Huang L.Q., Fang J.…Cao Y. Experimental studies on hepatotoxicity of rats induced by Fructus Gardeniae. Chinese Journal of traditional Chinese Medicine. 2006;31(13):1091–1093. [PubMed] [Google Scholar]
- Yang X., Yu L. Utilization status and development value of new food resources. Agricultural Technology Service. 2008;25(7):120–121. [Google Scholar]
- You Y.N., Yan H., Wang S.C., Luo X.H., Zhao X. Therapeutic strategy of traditional Chinese medicine for COVID-19. Drug Evaluation Research. 2020;43(04):613–619. [Google Scholar]
- Yu J. (2017). Catalogue of homologous raw materials for medicine and food (2017 Edition). Oral Care Industry, 27(6), 24–28.
- Zhang R.M., Zhang X., Guo W., Gao W.X., Liu W. Inhibition of Gardenia jasminoides and Scutellaria baicalensis on hepatotoxicity of rhynchophylline total alkaloids: Experimental study. Practical Journal of Medicine & Pharmacy. 2015;32(5):449–450. [Google Scholar]
- Zhang X.J., Zuo D.D. New research progress on chemical constituents and pharmacological effects of Atractylodes macrocephala. Information on Traditional Chinese Medicine. 2018;35(6):101–106. [Google Scholar]
- Zheng H.X. 10th ed. China Press of Traditional Chinese Medicine; Beijing: 2016. Basic theory of traditional chinese medicine. [Google Scholar]
- Zhao X.P., Lu L., Zhang Y.F., Zhang B.L. Study on discriminating nexphrotoxic components in zexie. China Journal of Chinese Materia Medica. 2011;36(06):758–761. [PubMed] [Google Scholar]
- Zhao X.Y., Liang Y., Kong D.W., Zhang L., Du G.H. The historical cognition and evaluation of Cyrtomium fortunei. Pharmacology and Clinics of Chinese Materia Medica. 2019;35(2):156–159. [Google Scholar]
- Zhong Y.C., Yang J. Studies on the prevention of pestilential diseases of Chinese medic. Journal of Nanjing University of Traditional Chinese Medicine. 2011;27(3):209–212. [Google Scholar]
- Zhu Y.F., Lou Y. Analysis of action features of sweet-taste herbs. Shanghai Journal of Traditional Chinese Medicine. 2011;45(4):18–19. [Google Scholar]
- Zhu N.a., Zhang D., Wang W., Li X., Yang B., Song J.…Tan W. A novel coronavirus from patients with pneumonia in China, (2019) New England Journal of Medicine. 2020;382(8):727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]