Abstract
Purpose
Human alveolar echinococcosis (AE) is a potentially lethal zoonosis caused by the cestode Echinococcus multilocularis. The aim of this systematic review is to establish a comprehensive global AE literature overview taking into account the epidemiologically relevant AE research of the twenty-first century.
Methods
We systematically searched the global literature published from 2001 through 2018 via MEDLINE, EMBASE, the Russian databases eLIBRARY.RU, CyberLeninka, the Chinese databases CNKI, VIP, Journals.research.ac.ir (Farsi language-based), Jordan E-Library (Arab language-based) and supplementary Google Scholar, in accordance with the PRISMA guidelines. QGIS software was used for the mapping of the affected countries.
Results
We have listed 154 relevant publications in the final literature synopsis in consideration of our quality assessment. Including non-autochthonous cases, human AE was reported in 36 countries within the northern hemisphere from 2001 to 2018. The first publication of AE in Tajikistan, Pakistan, South Korea, Belgium, the Netherlands, Slovakia, Hungary, Lithuania, Latvia, Slovenia and Morocco occurred in this century; further first cases in Taiwan, Thailand, and Denmark were considered to be non-autochthonous by the authors. The highest total case numbers (n ≥ 100 in a single article) were reported in France, Germany, Switzerland, Poland, and Lithuania, including China and Kyrgyzstan with by far the highest prevalence figures.
Conclusions
Our paper emphasises the increasing spread of reported cases and the rise in its numbers in the literature of the twenty-first century, especially in western, northern and eastern Europe, as well as in central Asia. Epidemiological studies on human infections are lacking in many parts of the world.
Keywords: Alveolar echinococcosis, Echinococcus multilocularis, Worldwide epidemiology, Geographical distribution, Prevalence, Maps
Introduction
Human alveolar echinococcosis (AE) is a rare, life-threatening zoonosis caused by the larvae of Echinococcus multilocularis (E. multilocularis), a helminth of the Cestoda class. Transmission is through ingestion of parasite eggs, which are excreted in the faeces of the definitive host. The life cycle of E. multilocularis takes place between canids as the definitive hosts and their prey, small mammals such as rodents, which act as intermediate hosts [1]. Besides the original cycles in wild animals [red foxes (Vulpes vulpes) and voles being the most important in Europe], cycles also seem to have become established in domestic dogs (Canis lupus familiaris) [2]. In the Chinese province of Ningxia, for example, wild canids are virtually non-existent and dogs are the most significant transmitters of AE [2]. Humans are accidental intermediate hosts. In 98% of cases, infection manifests primarily in the liver, showing a tumour-like malignant growth which, left untreated, leads to death in 90% of cases within 10–15 years of diagnosis [3, 4]. Annually there are estimated more than 18,000 new cases worldwide of AE, with 91% of those occurring in China [5].
Corresponding to the hazardous nature of the disease, WHO has designated AE as 1 of the 20 neglected tropical diseases and E. multilocularis as the food-borne parasite with the third largest global impact of 24 ranked parasites [6, 7].
Echinococcus multilocularis is found throughout the animal world in moderate to cold climate zones in the northern hemisphere. It extends from western, northern and eastern Europe and Russia into Asia, from eastern Turkey across central Asia into western and northern China, and is endemic on the northern Japanese island of Hokkaido. In North America, the helminth is endemic to the northwest coastal areas of Alaska, the western Canadian Arctic, southern Canada, and the neighbouring central northern states of the USA [8]. Cases of human disease do not necessarily occur in all endemic areas. The different rates of parasitic infection observed in the wildlife compared with the spread of human AE rest on various factors, such as host-dependant transmission patterns, landscape characteristics such as grass lands, local socioeconomic conditions including awareness of the disease within the public health system and general population [9–11]. A further deciding factor is thought to be the considerable variation in the intraspecific human pathogenicity of the parasite and the human host susceptibility [2]. Analyses of the genetic diversity of E. multilocularis have already demonstrated variants of the so-called Asian, European, North American, and Mongolian strains [12–14].
This review article is intended to provide the basis for a literature synopsis on the prevalence of AE worldwide. This should help to depict the spread of the disease across the globe, demonstrate current trends, and reveal gaps in our epidemiological knowledge. Furthermore, a global map focussing only on human cases should give an overview in which countries AE has been described in the current literature.
Methods
Search strategy and selection criteria
We performed a systematic literature search for worldwide relevant publications in the bibliographical databases MEDLINE (via the PubMed metasearch engine), EMBASE (via the OVID metasearch engine), the Chinese databases CNKI, VIP, and the Russian Scientific Electronic Library (via eLIBRARY.RU). These searches were supplemented with the Russian open access repository CyberLeninka, the Farsi language-based database Journals.research.ac.ir, the Arab language-based database of the University of Jordan E-Library and the web search engine Google Scholar.
The countries for our area-specific search strategy were selected after an initial screening of general reviews on E. multilocularis distribution, and its neighbouring nations. All the internationally relevant keywords for the disease were linked with the Boolean operator “OR”. The search key was designed to be as narrow as possible to ensure goal-oriented results but at the same time broad enough to capture all the relevant world literature. Search key optimisation was carried out by analysing the search details of each search term and subsequent pilot testing. The width of the search came primarily through automatic term mapping, the automatic generation of a more detailed search string, which also covered Medical Subject Headings (MeSH) terms (e.g. the MeSH term “Echinococcus multilocularis”). MeSH is the controlled vocabulary thesaurus generated in MEDLINE. A similar procedure was carried out with EMBASE (Emtree). The Boolean operator “AND” was used to add the country to be screened and the corresponding adjective, as well as any possible ethnonym, superordinate region (e.g. “Slavic” or “Baltic”) or subordinate region (e.g. “Alaska”, “Tibet”) to the end of the general search string. This resulted in PubMed search keys such as the one for France: Echinococcus multilocularis OR echinococcus alveolaris OR alveolar hydatid disease OR alveolar hydatid cyst OR alveolar hydatidosis OR alveococcosis AND (France OR French). Truncation, double quotes, and also the search term “alveolar echinococcosis” did not lead to a higher number of search results. Alongside the terms in Latin letters, synonyms in Chinese, Cyrillic and Arabic script were also searched through the suitable data bases.
The search was restricted to articles that were published from 2001 to 2018. There were neither restrictions in terms of language, place of publication, nor the time of the initial AE diagnosis; therefore, it can be dated before 2001. Overall case numbers included non-autochthonous cases, which were given in parenthesis in the final synopsis (e.g. a total of 65 cases, two of which were considered non-autochthonous, was given as “65 (2) cases”). With respect to the assumed infection locality, we used the information given by the authors. The searches were carried out between 01 June 2017 and 15 October 2017, February 2018, and between 14 January and 15 March 2019.
In order to be included in the final literature list, we established a quality assessment following previously defined including and excluding criteria for the collected data.
Inclusion criteria:
The article concerned epidemiological data on human AE (case numbers, prevalence, incidence) including transparent units (e.g. the incidence given as the number of cases per 100,000 inhabitants per year).
The data arose from clearly documented diagnostic criteria [serology, ultrasound (US), computed tomography (CT), magnetic resonance imaging (MRI), histopathology, nucleic acid-based testing] or from an official registry.
Exclusion criteria:
Articles in governmental publications for public health monitoring, or data that came from another study, reports of non-governmental organisations, congress contributions, or opinions of expert committees.
Data that were based on serological investigations without additional imaging.
No distinction was made between AE and cystic echinococcosis (CE).
Data that were interpolated or estimated.
Data that did not represent the basic population of AE cases, meaning certain preselected groups with no relation to a larger population size, or that came from a case report (with the exception of articles reporting cases in countries where no studies from 2001 to 2018 could be found with case numbers of n ≥ 10).
Qualification for the final literature list was carried out in two steps. First, we inspected all the articles found in the search results and applied the defined criteria. Then, we looked closely at all references that appeared relevant in each article. All the literature then discovered was inspected in the same way. We repeated the procedure until no more relevant information was generated (snowball method). The data obtained were stored in an Excel table (Microsoft Office 2017, version 15.30) and divided into the following categories: country, subordinate region (administrative unit), paper (ID, lead author, year of publication, title, journal, volume, pages), period of data collection, epidemiological data (case numbers, prevalence, incidence), case definition (serology, US, CT, MRI, histopathology, nucleic acid-based testing), and non-autochthonous cases.
A multilinguistic team of researchers screened the articles. Two researchers (SB, physician; JS, epidemiologist) independently inspected the literature according to the inclusion and exclusion criteria. In general, the full article was screened, unless the abstract was not clearly leading to an exclusion (e.g. the article was only about CE cases). All non-English articles were analysed in cooperation with native speakers. Literature in the Chinese language was independently screened by WXL, physician and RS, physician. Any uncertainties about the inclusion of an article were discussed, and if a consensus was not met, WK, physician, and HB, physician, were consulted to obtain it. An attempt was made to contact the corresponding author whenever there were any unresolved questions regarding the period of data collection or the case definition.
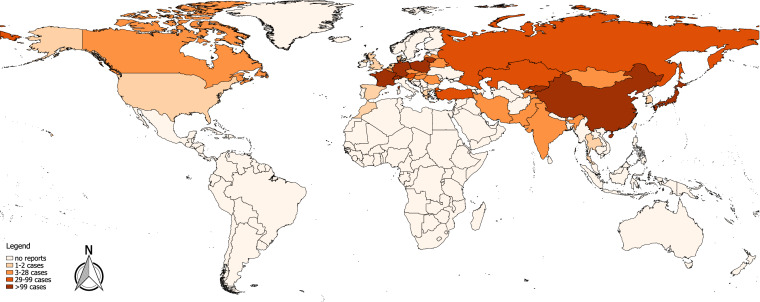
We used QGIS software (version 2.18.21) to generate the world map. Each country in which cases of AE had been reported in the literature between 2001 and 2018 was mapped. For the topographical colour shading of a country, the highest total number of cases in one reference within this period was the deciding factor.
This systematic overview follows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines to ensure a transparent study [15]. The corresponding checklist is attached as supporting information. The search protocol was entered into the International Prospective Register of Systematic Reviews (PROSPERO) under Registration number CRD42017079097.
Results
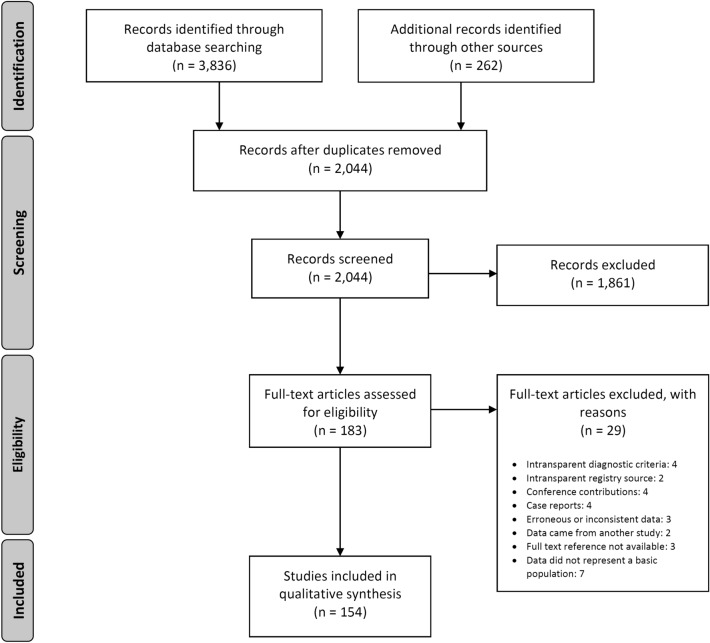
The numerical results of our search for the worldwide literature on AE through MEDLINE, EMBASE, the Chinese databases CNKI, VIP, Russian Scientific Electronic Library, CyberLeninka, Journals.research.ac.ir, Jordan E-Library and Google Scholar are presented as a flowchart in Fig. 1. Overall, we screened 99 countries or national territories independently, for potentially relevant publications. Relevant sources were found in 75 countries (n = 3836). A further 262 articles were detected in the course of our research, as relevant citations in the literature originally inspected (snowball method), giving a total of 4098 identified articles. We eliminated any duplicates in the various databases found with the country-specific key. Of the 2044 publications now under consideration, 1861 were excluded on inspection, as they obviously did not meet our requirements. The 183 remaining articles were then examined in detail with respect to the inclusion and exclusion criteria, where 29 further publications were excluded. Therefore, the final number of references was 154 (Tables 1, 2, 3). Figure 2 portrays the world map of all the affected countries and Fig. 3 depicts all the involved Chinese provinces.
Fig. 1.
Following the PRISMA guidelines, the flowchart represents the algorithm for article selection
Table 1.
Asia
| Country | Region | Total case number (n) | Prevalence (n/105) | Incidence (n/105/year) | Period covered by data | Particulars of the population | S | I | US | CT | MRI | HP | DNA | References |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| China | Gansu (Zhang and Min Counties) | 84 | 3400 | 1994–1997 | Han Chinese population | (+) | + | + | n/a | n/a | n/a | n/a | Bartholomot [126], Shi [127] | |
| Gansu | 119b | 3390 | 1996–1997, 2003 | (+) | (+) | (+) | n/a | n/a | n/a | n/a | Shi [36] | |||
| Gansu (Gannan Tibetan Autonomous Prefecture) | 3 | 1 | 2007–2013 | (+) | + | + | n/a | n/a | n/a | n/a | Ma [128], Wang [129] | |||
| Gansu (Minle County) | 9b | n/a | Han Chinese population | (+) | (+) | (+) | (+) | n/a | (+) | (+) | Han [130] | |||
| Gansu | 1 | 450 | Sep 2011–Jun 2012, 2017 | Tibetan rural population | + | + | + | n/a | n/a | n/a | n/a | Wang [131] | ||
| Ningxia | 263 | 1985–2001 | (+) | + | + | (+) | n/a | (+) | n/a | Li [132] | ||||
| Ningxia | 11 | 1730 | 2002 | + | + | + | n/a | n/a | n/a | n/a | Li [133] | |||
| Ningxia (Xiji, Guayan, Haiyuan Counties) | 82 | 3700 | 1985–2001 | n/a | (+) | (+) | (+) | n/a | (+) | n/a | Yang [35] | |||
| Ningxia (Xiji County) | 9 g | 2001–2002 | Hui rural population (113 inhabitants of Nanwan village)g | (+) | + | + | n/a | n/a | n/a | n/a | Yang [134] | |||
| Ningxia | 96 | 2000 | 2002–2003 | (+) | + | + | n/a | n/a | n/a | n/a | Yang [135] | |||
| Ningxia | 79 | 2200 | 2002 | Schoolchildren, 7–18 years | (+) | + | + | n/a | n/a | n/a | n/a | Yang [87], Yang [135] | ||
| Ningxia | 96 | 3000 | 2002–2003 | Non-student subset of data of [135] | (+) | + | + | n/a | n/a | n/a | n/a | Pleydell [136], Yang [135] | ||
| Ningxia (Xiji County) | 15 | 2006–2007 | Children/Adolescents, 6–20 years | (+) | + | + | n/a | n/a | n/a | n/a | Fang [137] | |||
| Qinghai (Xinghai County) | 1 | 160 | Jun–Jul 1999 | + | + | + | n/a | n/a | n/a | n/a | Wu [138] | |||
| Qinghai and Sichuan | 108 | 1400 | Jun 1997–Aug 1998 | + | + | + | n/a | n/a | n/a | n/a | Qiu [139] | |||
| Qinghai (Chindu, Zeko, Gade Counties) | 31 | 800 | 1997–1998 | + | + | + | n/a | n/a | n/a | n/a | Schantz [140] | |||
| Qinghai (Yushu County) | 4 | 500 | 2001 | + | + | + | n/a | n/a | n/a | n/a | He [141] | |||
| Qinghai | 125 | 1910 | 1995–2005 | + | + | + | n/a | n/a | n/a | n/a | Wang [142] | |||
| Qinghai (Jiuzhi County) | 39 | 2250 | Sep–Oct 2005 | + | + | + | n/a | n/a | n/a | n/a | Wu [143] | |||
| Qinghai (Zhiduo County) | 200 | 2006 | (+) | + | + | n/a | n/a | n/a | n/a | Wu [144] | ||||
| Qinghai (Jiuzhi County) | 39 | 2500 | 2005 | Tibetan population | (+) | + | + | n/a | n/a | n/a | n/a | Yu [145] | ||
| Qinghai | 141 | 8200 | Aug–Sep 2007 | + | + | + | n/a | n/a | n/a | n/a | Han [146] | |||
| Qinghai | 114 | 1000 | 1990–2010 | Children, 6–15 years/Tibetan rural population | + | + | + | n/a | n/a | n/a | n/a | Cai [147] | ||
| Qinghai | 114 | 600 | 2000–2010 | Children, 6–15 years | (+) | + | + | n/a | n/a | n/a | n/a | Cai [148] | ||
| Qinghai and Sichuan | 577 | 3700 | 2002–2008 | (+) | + | + | n/a | n/a | n/a | n/a | Giraudoux [149] | |||
| Qinghai | 17 | 2006–2014a | n/a | n/a | n/a | n/a | n/a | n/a | + | Ma [150] | ||||
| Qinghai (Maqên County) | 34 | 2200 | n/a | (+) | + | + | n/a | n/a | n/a | n/a | Ma [151] | |||
| Qinghai (Banma County) | 170 | 9430 | Jul–Aug 2014 | + | + | + | n/a | n/a | n/a | n/a | Ren [17] | |||
| Qinghai (Banma and Dari Counties) | 16 | 1670 | 2015 | R; Children, 3–17 years | + | + | + | n/a | n/a | n/a | n/a | Hou [152] | ||
| Qinghai (Hainan Tibetan Autonomous Prefecture) | 1 | 2780 | 2016 | Tibetan rural population | + | + | + | n/a | n/a | n/a | n/a | Cai [153] | ||
| Quinghai (Maqin, Gander, Dari, Jiuzhi, Banma Counties) | 146 | 1300 | 2011 | Schoolchildren, 6–16 years | + | + | + | n/a | n/a | n/a | n/a | Cai [86] | ||
| Qinghai (Yushu and Guoluo Prefectures) | 221 | 1130 | 2012–2014 | Children, 6–12 years/Tibetan rural population | + | + | + | n/a | n/a | n/a | n/a | Han [154] | ||
| Qinghai (Huangnan Prefecture) | 29 | 1150 | 2012–2014, 2017 | Tibetan rural population | + | + | + | n/a | n/a | n/a | n/a | Niang [155] | ||
| Qinghai | 222 | 1100 | 2010–2011 | Schoolchildren, 6–18 years | (+) | + | + | n/a | n/a | n/a | n/a | Han [156] | ||
| Sichuan (Shiqu County) | 60 | 8500 | 2001–2002 | Village-based study population | n/a | + | + | n/a | n/a | n/a | n/a | Wang [31] | ||
| Sichuan (Shiqu County) | 180 | 5740 | 2001–2003 | n/a | + | + | n/a | n/a | n/a | n/a | Budke [157] | |||
| Sichuan (Shiqu County) | 198 | 6200 | 2000–2002 | Village-based study population | (+) | + | + | n/a | n/a | n/a | n/a | Li [158] | ||
| Sichuan (Baiyü, Seda, Batang, Litang Counties) | 37 | 1230 | 2002–2003 | (+) | + | + | n/a | n/a | n/a | n/a | Yu [159] | |||
| Sichuan | 85 | 2540 | 2004–2005 | n/a | + | + | n/a | n/a | n/a | n/a | Renqingpengcuo [160] | |||
| Sichuan (Ganzi and Shiqu Counties) | 223 | 3100 | 1997, 2001, 2002, 2003 | + | + | + | n/a | n/a | n/a | n/a | Wang [161] | |||
| Sichuan | 311 | 3050 | 2001–2008 | (+) | + | + | n/a | n/a | n/a | n/a | Li [162] | |||
| Sichuan (Aba Prefecture) | 19 | 40 | Apr–Dec 2008 | + | + | + | n/a | n/a | n/a | n/a | Li [163] | |||
| Sichuan (Shiqu County) | 3028 | 3570 | Nov 2015–May 2017 | n/a | + | + | n/a | n/a | n/a | n/a | Yu [18] | |||
| Sichuan | 165 | May–Oct 2016 | (+) | + | + | n/a | n/a | n/a | n/a | Gao [164] | ||||
| TAR (Changdu Prefecture) | 4 | 2001–2005 | n/a | + | n/a | + | n/a | n/a | n/a | Feng [34] | ||||
| TAR (Dingqing County) | 12 | 5200 | 2007 | (+) | + | + | n/a | n/a | n/a | n/a | Feng [34] | |||
| TAR (Nyingchi City) | 5 | 990 | Aug–Oct 2016 | Tibetan rural population | + | + | + | n/a | n/a | n/a | n/a | Wang [165] | ||
| Xinjiang | 84 | 4000 | 1993–2003 | + | + | + | + | + | (+) | n/a | Gao [166] | |||
| Xinjiang (Nileke County) | 13 | 6360 | 2004 | + | + | + | n/a | n/a | n/a | n/a | Dingmu [32], Meng [33] | |||
| Xinjiang (Hoboksar Mongol Autonomous County) | 2 | 300 | 2007 | (+) | + | + | n/a | n/a | + | n/a | Wang [167] | |||
| Xinjiang (Hoboksar Mongol Autonomous County) | 4 | 800 | Apr–May 2013 | n/a | + | + | n/a | n/a | + | n/a | Li 168] | |||
| India | Chandigarhe | 1 | n/a | C | + | + | + | n/a | n/a | + | n/a | Nagesh [23] | ||
| 1 | n/a | C | + | + | + | + | n/a | + | n/a | Shaw [24] | ||||
| Maharashtra | 1 | n/a | C | – | +f | – | +f | +f | + | n/a | Tyagi [25] | |||
| Maharashtra | 1 | n/a | C | + | + | n/a | + | + | + | n/a | Bhatia [26] | |||
| 1 | n/a | C | n/a | + | + | + | n/a | + | n/a | Prabhakar [27] | ||||
| 4 (4) | Mar 2010–May 2016 | + | + | + | + | (+) | n/a | n/a | Goja [28] | |||||
| 3 | n/a | C | (+) | + | (+) | (+) | n/a | + | n/a | Bansal [29] | ||||
| Iran | Razavi Khorasan Province | 18 (1) | 1997–2012 | n/a | + | + | + | + | + | n/a | Maddah [20] | |||
| Japan | Hokkaido | 373 (14) | 1937–1997 | R | (+) | (+) | n/a | n/a | n/a | (+) | n/a | Ito [169] | ||
| Hokkaido | 424 | 1937–2003 | R | n/a | n/a | n/a | n/a | n/a | n/a | n/a | Oku [170] | |||
| 50b (1) | 1999–2002 | R | (+) | (+) | (+) | (+) | n/a | (+) | n/a | Arai [171], Arai [172] | ||||
| Hokkaido | 500 | 1937–2005 | R | n/a | n/a | n/a | n/a | n/a | n/a | n/a | Inoue [173] | |||
| 109 | Apr 1999–2005 | R | n/a | n/a | n/a | n/a | n/a | n/a | n/a | Taniguchi [39] | ||||
| 0.013 | 2000–2005 | R | n/a | n/a | n/a | n/a | n/a | n/a | n/a | Taniguchi [39] | ||||
| 154 (1) | Apr 1999–Mar 2008 | R | n/a | n/a | n/a | n/a | n/a | n/a | n/a | Taniguchi [174] | ||||
| 0.013 | 1999–2008 | R | n/a | n/a | n/a | n/a | n/a | n/a | n/a | Taniguchi [174] | ||||
| Hokkaido | 715 | 1937a–2016 | R | n/a | n/a | n/a | n/a | n/a | n/a | n/a | Ito [38] | |||
| Kazakhstan | Almaty Oblastc | 46 | 2006–2014 | n/a | + | n/a | n/a | n/a | + | n/a | Abdybekova [82] | |||
| Aqmola and Almaty Oblasts | 4 | 2007–2013 | R | n/a | n/a | n/a | n/a | n/a | n/a | n/a | Abdybekova [82] | |||
| Almaty Oblast | 6 | 2012–2015 | n/a | + | + | + | + | n/a | n/a | Baimakhanov [175] | ||||
| Kyrgyzstan | Naryn Oblast (Kochkor District) | 92 | 1970 | 2000–2007 | n/a | n/a | n/a | n/a | n/a | n/a | n/a | Bodoshova [176] | ||
| 186 | 1996–2007 | R | n/a | n/a | n/a | n/a | n/a | n/a | n/a | Bodoshova [78] | ||||
| Naryn Oblast | 7.1 | 2010–2011 | R | n/a | n/a | n/a | n/a | n/a | + | n/a | Usubalieva [16] | |||
| Osh Oblast | 122 | 2000–2013 | R | n/a | n/a | n/a | n/a | n/a | + | n/a | Raimkylov [79] | |||
| Osh Oblast | 60 | 6.0 | 2013 | n/a | n/a | n/a | n/a | n/a | + | n/a | ||||
| 26 | 2007 | R | n/a | n/a | n/a | n/a | n/a | + | n/a | |||||
| 148 | 2.6 | 2013 | n/a | n/a | n/a | n/a | n/a | + | n/a | |||||
| 581 | 1996–Mar 2016 | n/a | + | + | n/a | + | n/a | n/a | Omorov [80] | |||||
| Osh Oblast (Alay District) | 104d | 6400d | 2012 | (+) | + | + | n/a | n/a | (+) | (+) | Bebezov [21] | |||
| Mongolia | 4 | 2002, 2006, 2007, 2009 | (+) | n/a | n/a | n/a | n/a | + | + | Ito [37] | ||||
| Pakistan | Khyber Pakhtunkhwa | 3 | 2012–2014a | n/a | n/a | n/a | n/a | n/a | n/a | + | Ali [30] | |||
| South Korea | Gyeongsangnam-do | 1 | 2001 | C | + | + | n/a | + | n/a | + | + | Kim [40], Jeong [177] | ||
| Taiwan | 1 (1) | n/a | C | n/a | + | n/a | + | + | + | n/a | Huang [41] | |||
| Tajikistan | Dushanbee | 22 | 2010–2013 | n/a | + | + | + | + | n/a | n/a | Ahmedov [83] | |||
| Thailand | 1 (1) | n/a | C | n/a | + | + | + | n/a | + | n/a | Warnnissorn [42], Limawongpranee [43] | |||
| Turkey | Erzurum Provincee | 40 | Feb 1987–Dec 2000 | (+) | + | + | (+) | (+) | (+) | n/a | Polat [178] | |||
| Southeastern Anatolia | 47 | 1980–2000 | (+) | (+) | n/a | n/a | n/a | (+) | n/a | Uzunlar [19] | ||||
| Southeastern Anatolia | 18 | 0.49 | 1980–1990 | |||||||||||
| Southeastern Anatolia | 29 | 0.63 | 1991–2000 | |||||||||||
| Southeastern Anatolia | 19 | 0.4 | 2000 | |||||||||||
| Izmir, Afyonkarahisar, Kütahya, Muş, Erzurum Provinces | 8 | 1980–2001 | n/a | n/a | n/a | n/a | n/a | + | n/a | Canda [179] | ||||
| Diyarbakır Provincee | 47 | 1980–2002 | n/a | n/a | n/a | n/a | n/a | + | n/a | Kılınç [180] | ||||
| Erzurum, Ağrı, Kars, Iğdır, Erzincan, Ardahan, Bayburt, Muş Provinces | 22 | 1999–Jul 2004 | n/a | n/a | n/a | n/a | n/a | + | n/a | Gündoğdu [181] |
S serology, I diagnostic imaging (includes US, CT, MRI), US ultrasonography, CT computed tomography, MRI magnetic resonance imaging, HP histopathology, DNA DNA testing/genotyping, + positive diagnostic test using the particular method, − negative diagnostic test using the particular method, n/a no information on diagnostic investigation using the particular method; (+) diagnostic test using the particular method possibly positive in some of the cases, aAdditional information obtained by personal communication with the corresponding author of the publication, bcase number includes cases allowing a serological diagnosis without additional findings on imaging, c“a number of cases were referred from other regions”, including 8 cases from eastern Kazakhstan, dcumulative prevalence of 4.2% (n = 68) [US + , S(+), HP(+), DNA(+)] and 2.2% (n = 36) (US + “and no follow-up”), elocation of the institution where all patients have been diagnosed for AE, fimaging of the brain, gtotal case number (20 cases/221 villagers/1950s–2001s) based on additional questionnaires; C: case report; R: data from an official registry
Table 2.
Europe
| Country | Region | Total case number (n) | Prevalence (n/105) | Incidence (n/105/year) | Period covered by data | Particulars of the population | S | I | US | CT | MRI | HP | DNA | References |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Austria | 54 (1) | 1982–2000 | R | (+) | (+) | (+) | (+) | (+) | (+) | n/a | Kern [68] | |||
| 65 (2) | 1968–2005 | + | + | n/a | n/a | n/a | (+) | n/a | Auer [183] | |||||
| 65 | 1991–2011 | + | + | n/a | n/a | n/a | (+) | (+) | Schneider [44] | |||||
| 24 | 0.029 | 1991–2000 | + | + | n/a | n/a | n/a | (+) | (+) | |||||
| 28 | 0.034 | 2001–2010 | + | + | n/a | n/a | n/a | (+) | (+) | |||||
| 13 | 0.158 | 2011 | + | + | n/a | n/a | n/a | (+) | (+) | |||||
| Vorarlberg | 22 | 1991–2011 | + | + | n/a | n/a | n/a | (+) | (+) | Schneider [44] | ||||
| Vorarlberg | 3 | 0.08 | 1991–2000 | + | + | n/a | n/a | n/a | (+) | (+) | ||||
| Vorarlberg | 12 | 0.32 | 2001–2010 | + | + | n/a | n/a | n/a | (+) | (+) | ||||
| Vorarlberg | 7 | 1.9 | 2011 | + | + | n/a | n/a | n/a | (+) | (+) | ||||
| Tyrol | 21 | 1991–2011 | + | + | n/a | n/a | n/a | (+) | (+) | Schneider [44] | ||||
| Tyrol | 12 | 0.17 | 1991–2000 | + | + | n/a | n/a | n/a | (+) | (+) | ||||
| Tyrol | 5 | 0.07 | 2001–2010 | + | + | n/a | n/a | n/a | (+) | (+) | ||||
| Tyrol | 4 | 0.56 | 2011 | + | + | n/a | n/a | n/a | (+) | (+) | ||||
| Belarus | Gomel Oblast | 1 | 2008 | n/a | n/a | n/a | n/a | n/a | + | n/a | Krasavtsev [65] | |||
| Grodno | 5 | 2008–2017 | n/a | + | + | (+) | (+) | + | n/a | Prokopchik [64] | ||||
| Belgium | 3 | 1982–2000 | R | (+) | (+) | (+) | (+) | (+) | (+) | n/a | Kern [68] | |||
| 13 | 1999a–2003, 2006, 2007, 2010, 2011 | R | n/a | n/a | n/a | n/a | n/a | n/a | n/a | Landen [55] | ||||
| Liège, Luxembourg, Namur Provinces | 22 | 1999–Feb 2018 | + | + | n/a | n/a | n/a | + | (+) | Cambier [184] | ||||
| Czechia | 20 (2) | 1998–2014 | (+) | + | (+) | (+) | (+) | (+) | (+) | Kolářová [62] | ||||
| Denmark | 1 (1) | n/a | + | + | n/a | + | n/a | n/a | n/a | Laursen [90] | ||||
| France | 260 | 1982–2000 | R | n/a | n/a | n/a | n/a | n/a | n/a | n/a | Bresson-Hadni [185] | |||
| 235 | 1982–2000 | R | (+) | (+) | (+) | (+) | (+) | (+) | n/a | Kern [68] | ||||
| 417 | 0.026 | 1982–2009 | R | n/a | n/a | n/a | n/a | n/a | n/a | n/a | Grenouillet [46] | |||
| 258 | 0.023 | 1982–2000 | R | (+) | + | (+) | (+) | (+) | (+) | (+) | Piarroux [186] | |||
| 66 | 0.025 | Jan 2001–Jun 2005 | R | (+) | + | (+) | (+) | (+) | (+) | (+) | Piarroux [186] | |||
| 387b | 1982–2007 | R | (+) | (+) | (+) | (+) | (+) | (+) | (+) | Piarroux [187] | ||||
| 407b | 1982–2007 | R | (+) | (+) | (+) | (+) | (+) | (+) | (+) | Piarroux [188] | ||||
| Doubs department | 0.7619 | 1982–2009 | R | n/a | n/a | n/a | n/a | n/a | n/a | n/a | Comte [45], Grenouillet [46] | |||
| Haute-Savoie department | 0.2329 | 1982–2009 | R | n/a | n/a | n/a | n/a | n/a | n/a | n/a | Comte [45], Grenouillet [46] | |||
| 509b | 0.027 | 1982–2011 | R | (+) | (+) | (+) | (+) | (+) | (+) | (+) | Said-Ali [125] | |||
| 575 | 1982–2013 | R | n/a | n/a | n/a | n/a | n/a | n/a | n/a | Charbonnier [52] | ||||
| 509 | Jul 1982–Jun 2012 | R | n/a | n/a | n/a | n/a | n/a | n/a | n/a | Chauchet [93] | ||||
| Germany | 132 (6) | 1982–2000 | R | (+) | (+) | (+) | (+) | (+) | (+) | n/a | Kern [68] | |||
| 136 (6) | 1994–2004 | R | n/a | n/a | n/a | n/a | n/a | n/a | n/a | Kern [189] | ||||
| 114 | 2003–2005 | R | n/a | (+) | n/a | n/a | n/a | (+) | n/a | Jorgensen [190] | ||||
| 312 | 1992–2011 | + | + | (+) | (+) | (+) | + | n/a | Grüner [191] | |||||
| 523b | 0.64 | 1992–2016 | R | n/a | n/a | n/a | n/a | n/a | n/a | n/a | Schmidberger [51] | |||
| Baden-Württemberg | 237b | 2.18 | 1992–2016 | R | n/a | n/a | n/a | n/a | n/a | n/a | n/a | Schmidberger [51] | ||
| Bavaria | 190b | 1.48 | 1992–2016 | R | n/a | n/a | n/a | n/a | n/a | n/a | n/a | Schmidberger [51] | ||
| Greece | 1 | 1982–2000 | R | (+) | (+) | (+) | (+) | (+) | (+) | n/a | Kern [68] | |||
| Hungary | 1 | 2004 | C | + | + | + | + | + | + | n/a | Horváth [192] | |||
| 3b | 2004–2010a | R | + | n/a | n/a | n/a | n/a | n/a | n/a | Dezsényi [57] | ||||
| 1 | 2012 | C | + | + | + | + | + | + | n/a | Dezsényi [57] | ||||
| Latvia | 14 | 1999–2010 | R | (+) | + | + | n/a | n/a | n/a | n/a | Marcinkutė [47] | |||
| Lithuania | 47 | 1998–2005 | R | (+) | + | (+) | (+) | n/a | n/a | n/a | Marcinkutė [61] | |||
| 80 | 1997–Jul 2006 | (+) | (+) | (+) | (+) | n/a | + | n/a | Bružinskaitė [193] | |||||
| 58 | Jun 2003–2007 | R | (+) | (+) | (+) | (+) | (+) | (+) | n/a | Strupas [194] | ||||
| 179 | 1997–2013 | R | n/a | n/a | n/a | n/a | n/a | n/a | n/a | Marcinkutė [47] | ||||
| 0.54 | 2013 | R | n/a | n/a | n/a | n/a | n/a | n/a | n/a | Marcinkutė [47] | ||||
| Netherlands | 1 (1) | 1982–2000 | R | (+) | (+) | (+) | (+) | (+) | (+) | n/a | Kern [68] | |||
| Limburg Province | 1 | 2008 | C | +c | + | n/a | + | + | + | + | van Dommelen [54] | |||
| Poland | Warmia-Masuria, Pomerania, Lubusz Provinces | 20 | Sep 1992–May 2002 | R | n/a | (+) | (+) | n/a | n/a | (+) | n/a | Stefaniak [195] | ||
| 14 | 1982–2000 | R | (+) | (+) | (+) | (+) | (+) | (+) | n/a | Kern [68] | ||||
| 6 | n/a | (+) | n/a | n/a | n/a | n/a | + | (+) | Myjak [58] | |||||
| Warmia-Masuria, Pomerania, Lubusz and Podkarpackie Provinces | 45 | 1992–2006 | R | (+) | (+) | (+) | (+) | n/a | (+) | n/a | Stefaniak [196], Stefaniak [197] | |||
| 4b | 2011 | R | (+) | (+) | n/a | n/a | n/a | (+) | (+) | Czarkowski [199] | ||||
| 7b | 2012 | R | (+) | (+) | n/a | n/a | n/a | (+) | (+) | Gołąb [200] | ||||
| 121b | 0.014 | 1990–2011 | (+) | (+) | (+) | n/a | n/a | (+) | (+) | Nahorski [49] | ||||
| Warmia-Masuria Province | 65b | 0.20 | 1990–2011 | (+) | (+) | (+) | n/a | n/a | (+) | (+) | Nahorski [49] | |||
| Romania | Iași, Botoșani, Vaslui Counties | 5 | Feb 2007–Jun 2007a | n/a | n/a | n/a | n/a | n/a | n/a | + | Šnábel [59] | |||
| Russia | Kamchatka Kraid | 9 | n/a–2008 | n/a | + | + | n/a | n/a | n/a | n/a | Kharchenko [100] | |||
| Sakha Republicd | 2 | 2006–2011 | n/a | + | + | n/a | + | + | n/a | Sleptsov [99] | ||||
| 41 | 2008 | R | n/a | n/a | n/a | n/a | n/a | n/a | n/a | Konyaev [98] | ||||
| Altai Kraid | 8 | 2008 | R | n/a | n/a | n/a | n/a | n/a | n/a | n/a | Konyaev [98] | |||
| Tomsk Oblastd | 42 | n/a–2012 | n/a | + | + | + | + | n/a | n/a | Kuracheva [66] | ||||
| 30 | 2001 | R | n/a | n/a | n/a | n/a | n/a | n/a | n/a | Konyaev [13] | ||||
| Moscow | 1 | May 2008–Jun 2014 | n/a | + | + | + | n/a | n/a | n/a | Gautier [94] | ||||
| Republic of Bashkortostan | 1 | 2014 | n/a | n/a | n/a | n/a | n/a | + | n/a | Nartaylakov [96] | ||||
| Moscow | 5 | n/a–2015 | n/a | + | n/a | + | + | n/a | n/a | Kotlayrov [95] | ||||
| Chelyabinsk Oblaste | 1 | 2017 | n/a | + | n/a | + | + | n/a | n/a | Zotova [97] | ||||
| Slovakia | Žilina, Prešov, Košice, Trenčín and Banská Bystrica Regions | 10 | 2000–2007 | + | + | + | + | n/a | + | (+) | Kinčeková [201] | |||
| Prešov, Žilina, Košice, Trenčín Regions | 16 | 2000–2010 | R | n/a | n/a | n/a | n/a | n/a | n/a | n/a | Miterpáková [60] | |||
| Žilina, Prešov, Košice, Trenčín Regions | 26 | 2000–2013 | (+) | (+) | (+) | (+) | (+) | (+) | (+) | Antolová [63] | ||||
| 37 | 2000–2014 | (+) | (+) | (+) | (+) | (+) | (+) | (+) | Antolová [202] | |||||
| Slovenia | 9b | 0.45b | 0.09b | 2001–2005 | + | (+) | (+) | (+) | n/a | n/a | n/a | Logar [50] | ||
| Spain | Navarre | 1 | n/a | C | n/a | + | n/a | + | n/a | + | n/a | Arrechea Irigoyen [67] | ||
| Switzerland | Canton of Fribourg | 1 | 1993–1998 | + | + | + | + | n/a | n/a | n/a | Gottstein [203] | |||
| 118 (6) | 1982–2000 | R | (+) | (+) | (+) | (+) | (+) | (+) | n/a | Kern [68] | ||||
| 113 | 1976–May 2003 | n/a | + | n/a | + | n/a | n/a | n/a | Kadry [204] | |||||
| 60 | 0.10 | 1993–2000 | + | + | n/a | n/a | n/a | (+) | (+) | Schweiger [48] | ||||
| 96 | 0.26 | 2001–2005 | + | + | n/a | n/a | n/a | (+) | (+) | Schweiger [48] | ||||
| United Kingdom | 1 (1) | n/a | C, Rg | + | + | + | + | + | + | n/a | Graham [22], Kern [68]g | |||
| 1 (1) | n/a | C | + | + | n/a | + | +f | + | n/a | Svrckova [91] |
S serology, I diagnostic imaging (includes US, CT, MRI), US ultrasonography, CT computed tomography, MRI magnetic resonance imaging, HP histopathology, DNA DNA testing/genotyping, + positive diagnostic test using the particular method, − negative diagnostic test using the particular method, n/a no information on diagnostic investigation using the particular method; (+) diagnostic test using the particular method possibly positive in some of the cases, aAdditional information obtained by personal communication with the corresponding author of the publication, bcase number includes cases allowing a serological diagnosis without additional findings on imaging, cEchinococcus spp. IgG weakly positive; Echinococcus multilocularis-specific ELISA negative, dAsian part of Russia, eborder region of European and Asian part of Russia, fMRI of the brain; gsame case (Petra Kern, personal communication) has also been registered as only case from UK in European Echinococcosis Registry (1982–2000) [70]; C: case report; R: data from an official registry
Table 3.
Rest of the world
| Country | Region | Total case number (n) | Prevalence (n/105) | Incidence (n/105/year) | Period covered by data | Particulars of the population | S | I | US | CT | MRI | HP | DNA | Reference |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Canada | Alberta, Ontario, British Columbia, Saskatchewan | 12b | 2001–2014 | R | n/a | n/a | n/a | n/a | n/a | n/a | n/a | Massolo [69] | ||
| Alberta, Ontario, British Columbia, Saskatchewan and the Territoriesa | 16b | 2002–2011 | R | n/a | n/a | n/a | n/a | n/a | n/a | n/a | Schurer [70] | |||
| Morocco | 1 | n/a | C | + | + | + | + | n/a | + | n/a | Maliki [72] | |||
| USA | Minnesota | 1 | 1977 | C | + | n/a | n/a | n/a | n/a | + | + | Yamasaki [71] | ||
| City of Chicago | 2 | 2003–2013 | (+) | (+) | n/a | (+) | n/a | + | (+) | Taxy [198] |
S serology, I diagnostic imaging (includes US, CT, MRI), US ultrasonography, CT computed tomography, MRI magnetic resonance imaging, HP histopathology, DNA DNA testing/genotyping, + positive diagnostic test using the particular method, (+) diagnostic test using the particular method possibly positive in some of the cases, n/a no information on diagnostic investigation using the particular method; aAdditional information obtained by personal communication with the corresponding author of the publication/Territories (Northwest Territories, Nunavut, Yukon) are coded the same in the registry; bauthors assume high probability of non-autochthonous infection; C: case report; R: data from an official registry
Fig. 2.
Worldwide distribution of alveolar echinococcosis in humans according to the published literature 2001–2018. Each country in which cases of AE had been reported in the literature between 2001 and 2018 was mapped. For the topographical colour shading of a country, the highest total number of cases in one reference within this period was the deciding factor
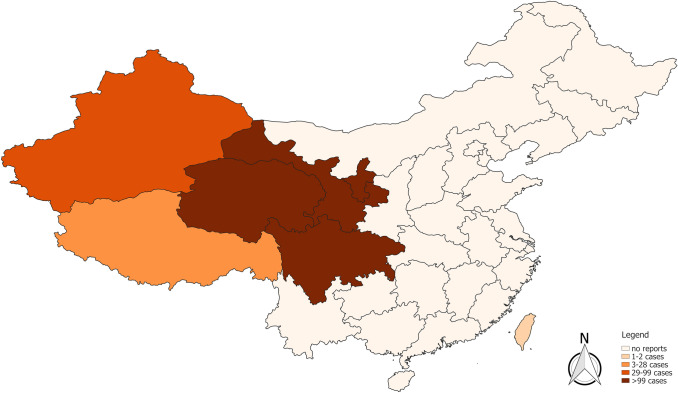
Fig. 3.
Current distribution of alveolar echinococcosis in humans according to the published literature 2001–2018 in China. Each province in which cases of AE had been reported in the literature between 2001 and 2018 was mapped. For the topographical colour shading of a province, the highest total number of cases in one reference within this period was the deciding factor
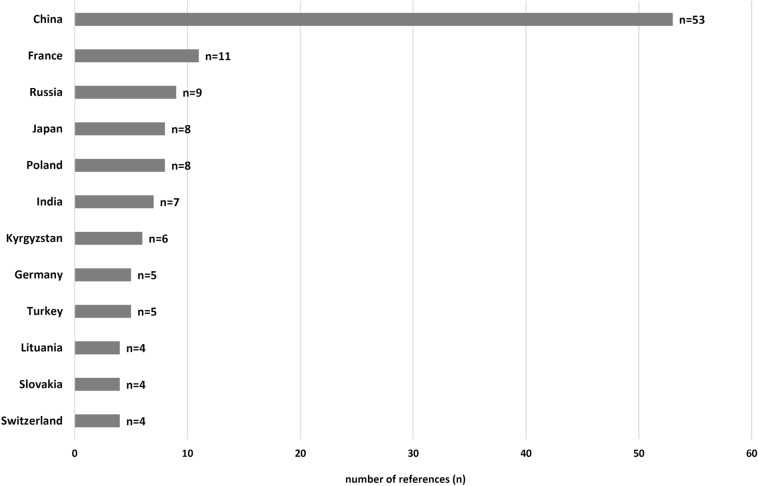
The data obtained from the literature published between 2001 and 2018 showed the presence of human AE in 36 countries within the northern hemisphere. Excluding those countries with a single case report of apparently non-autochthonous origin (United Kingdom, Denmark, Taiwan, and Thailand) leaving a total of 32 countries. In no other country, more epidemiological data were generated than China, with 53 publications, followed by France (n = 11), Russia (n = 9), Poland (n = 8) and Japan (n = 8), see also Fig. 4. Apart from two references out of Kyrgyzstan, one from Germany, Slovenia and Turkey, prevalence figures were given only in China (n = 47). The incidence was calculated in 14 articles, particularly in France (n = 4). Human AE was reported for the first time in this century in Tajikistan, Pakistan, South Korea, Belgium, the Netherlands, Slovakia, Hungary, Lithuania, Latvia, Slovenia, and Morocco, as well as in three countries where the authors considered the cases to be non-autochthonous (Denmark, Taiwan and Thailand).
Fig. 4.
The twelve most frequently listed countries on which epidemiologically relevant papers on AE were published, according to the inclusion and exclusion criteria (data of publication 2001–2018). Redundancy possible
Asia
Based on reports from 13 Asiatic countries published since 2001, the epidemiological AE zone stretches across the north of the continent from Turkey to Japan, but with considerable gaps. The highest mean incidence of 7.1/105/year was calculated in Oblast Nary, Kyrgyzstan (2010–2011) [16]. The highest prevalence of 9.43% was found in Banma County in the province of Qinghai, China, in 2014 [17]. The highest absolute number of cases, 3028 patients, came from an US screening in Shiqu County, Sichuan Province (2015–2017) in China [18].
From Turkey, there were five publications with data prior to 2005; in Southeastern Anatolia, the prevalence was calculated to be 0.4/105 in the year 2000 [19]. In central Asia, we found literature from Kazakhstan, Kyrgyzstan and Tajikistan, however no original papers concerning Turkmenistan or Uzbekistan. Reporting the non-autochthonous case from Iran, Maddah and co-authors described the patient as being of Turkmen origin [20]. In the Kyrgyz Alay district, a study has been demonstrated a prevalence of 6.4% in 2012 [21]. From the west of Iran, we found a publication describing 18 cases. There was no literature describing possible Iraqi patients. Noticeably, a paper from the UK showed an Afghan patient who migrated from Pakistan; the authors discuss the infection originating in Afghanistan [22]. There was evidence of isolated cases in India and, as far as we know, the first case was reported in Pakistan [23–30].
Apart from Kyrgyzstan, by far the highest prevalences of human AE were reported in China. Reports have been related exclusively to Western China, namely to the provinces of Qinghai, Gansu, Sichuan and the autonomous regions Xinjiang, Tibet and Ningxia. The highest prevalences were reported from counties of the eastern Tibetan Plateau, ranking up to 9.43% in Banma County (Qinghai, July–August 2014) [17] and 8.5% in Shiqu County (Sichuan, 2001–2002) including a prevalence of 15% in one of the 11 villages being studied [31]. In further administrative divisions of China, the highest prevalences were 6.36% in Xinjiang (2004) [32, 33], 5.2% in Tibet Autonomous Region (TAR) (2007) [34], 3.7% in Ningxia (1985–2001) [35] and 3.39% in Gansu (1996–1997, 2003) [36]. Up north in neighbouring Mongolia, four cases in the west of the country were confirmed by histopathology and molecular genetic testing; the rare Mongolian haplotype was identified in two of these cases [37]. In Japan, it is assumed that nearly all human infections occurred on the northern island of Hokkaido [38]; one paper calculated the mean incidence for the whole of the country to be 0.013/105/year in the period from 2000 to 2005 [39]. The first case from South Korea was reported in a woman who had apparently never left the country [40]. The first AE reports in Taiwan and Thailand were considered to be non-autochthonous by the authors [41–43].
Europe
In the twenty-first century, AE has been reported in 20 European countries, although the cases in the United Kingdom and Denmark were considered to be non-autochthonous by the authors. A (mean) incidence was calculated in six countries, the highest being in the Austrian Federal State of Vorarlberg in 2011 at 1.9/105/year [44]. The incidence was up to 0.76/105/year in France (in Doubs 1982–2009), up to 0.54/105/year in Lithuania (2013), up to 0.26/105/year in Switzerland (2001–2005), up to 0.20/105/year in Poland (in Warmia-Masuria Province, 1990–2011) and 0.09/105/year in Slovenia (2001–2005) [45–50]. The prevalence was calculated only in a German and a Slovenian study, with the highest German figure of 2.18/105 in the Federal State of Baden-Württemberg (1992–2016) and 0.45/105 for whole Slovenia in the period from 2001 to 2005 [50, 51]. Highest case numbers were registered in the national databases in France (575 from 1982 to 2013) and Germany (523 in 1992–2016) [51, 52]. The first case thought to be autochthonously acquired in the Netherlands was reported in the province of Limburg [53, 54]. The first reported cases from neighbouring Belgium appeared nearly exclusively in Wallonia [55, 56]. Also for the first time in Hungary, a case of AE was thought to be autochthonous in the south-west of the country [57]. Evidence of the disease was found for the first time in Poland and in five patients in north-eastern Romania by molecular genetic testing [58, 59]. To the best of our knowledge, the first reported cases of human AE also originated in Slovakia, Lithuania, Latvia, and Slovenia [47, 50, 60, 61]. Since 2007, 20 cases were registered by the Czech National Reference Laboratory for Tissue Helminthoses [62]. Of the 26 confirmed AE cases in Slovakia between 2000 and 2013, Antolová et al. found that 23 of them occurred in the north-west of the country, in the Žilina and Prešov regions [63]. In Belarus, there were five case reports described in Grodno, a city in the border area to Poland and Lithuania [64], and one post-mortem diagnosis out of Gomel Oblast [65]. From Russia, the highest figure of 42 AE cases was reported in Tomsk Oblast until 2012 [66]. Literature focussing on human AE cases in Ukraine could not be found. In Southern Europe, single cases were documented in the north Spanish province of Navarre and in Greece [67, 68].
North America
Figures from the Canadian Institute for Health Statistics were published in two articles from Canada, including a total of 12 cases in the southern states of British Columbia, Alberta, Saskatchewan, and Ontario for the period 2001–2014 [69, 70]. In the USA, molecular genetic analysis of the sample from a case reported in Minnesota in 1977 gave a 99.9% agreement in sequence homology with an E. multilocularis isolate of a fox in South Dakota and 99.4% agreement with a human sample from Japan [71].
Africa
In the literature from 2001 to 2018, we found only a single case report of a 54-year-old Moroccan man. This was the first reported case of AE in Morocco [72].
Discussion
Compared with review articles from around the turn of the millennium [73–77], our work confirms the increasing number of reported cases of human infection in western, northern and eastern Europe, as well as in central Asia. In addition, we found regions in which AE had not been documented before 2001. Even so, there are still fundamental gaps in our knowledge of the distribution of AE.
Asia
A huge increase in case numbers was seen in central Asia, especially in Kyrgyzstan, the only region in the world where prevalence dimensions were published which otherwise only could be found in China [21, 78]. While only 0–3 cases per annum were recorded in the period 1996–2003, numbers rose continuously from 2004 onwards, reaching 61 cases in 2011 [16]. And more than twice that number of patients was recorded in 2013 (148 cases) [79]. Omorov and Co-Workers collected 1179 AE cases (1996–2015) from nine different Kyrgyz institutions, though diagnostic criteria have been shown for 581 patients [80]. Possible reasons for the upsurge were the improved medical care and diagnostic investigation after the difficult economic period following the dissolution of the Soviet Union and the increasing spread of E. multilocularis-infected stray dogs [16, 81]. In Kazakhstan, one hospital in Almaty found that the recorded cases of AE more than doubled from 15 cases in 2004–2011 to 32 cases in 2012–2014 [82]. For the first time, AE cases were published from Tajikistan, where 22 patients were diagnosed from 2010 through 2013 [83]. Only a congress contribution, referring to 83 surgical AE patients missing diagnostic criteria, has been suggested the presence of the disease in Uzbekistan [84].
There is a distinct lack of studies from western Asia, with only estimates of a few AE cases per year existing for Armenia, Georgia and Azerbaijan [5]. Current epidemiological studies out of Turkey are missing. One publication reported 202 AE patients (1980–1998) for the whole country; no diagnostic criteria were given [182]. There are merely sporadic data or none at all from the countries that stretch across central Asia towards China (Iraq, Iran, Afghanistan, Pakistan, and India), so that we have to assume an under-representation [20, 30]. One case report from Iraq suggesting E. multilocularis as the causative agent has obviously not been presenting an AE patient [85], as the published CT figure showed the morphologic criteria of a CE lesion (WHO-type 3b) [Tilmann Graeter, personal communication].
By far the highest prevalences, apart from the discussed Kyrgyz numbers, are still to be found in China. Overall, the figures are unchanged and no recent spread, increase, or decrease of case numbers has been described by authors publishing Chinese data. The high prevalence in schoolchildren is particularly remarkable, as paediatric cases of disease are absolute rarities in other parts of the world [86–88].
Europe
In recent years, there has been both a spread of AE reports across Europe and an increase in case numbers. Until the end of the 1980s, the disease was considered endemic only in the ‘historical’ AE area of western Europe (France, Germany, Switzerland, and Austria) [89], but human infection has already been reported in 20 European countries since 2001. Only the cases in Denmark and the United Kingdom were considered to be non-autochthonous in the respective publications [68, 90, 91]. Figures for all the affected western European countries have shown an increase. In France, according to the FrancEchino Register, the number of new cases per year in the period 2003–2012 (239 cases) almost doubled in comparison with the previous 10 years (122 cases); in particular, there was a significant increase in the incidence of AE in immunosuppressed patients [92, 93]. The mean incidence in Switzerland rose from 0.1/105/year (1993–2000) to 0.26/105/year (2001–2005) [48]. Austria had an average of 2.4 cases in 1991–2000, 2.8 in 2001–2010, and a sudden unexpected rise to 13 cases in 2011 alone [44]. Germany showed a progressive increase in the figures over five-year periods, with 97 cases (2002–2006), 107 cases (2007–2011), and 165 cases (2012–2016) [51]. In addition, AE seems to have spread to previously non-endemic areas such as Belgium and the Netherlands [54–56].
Increasing figures were reported in the literature for all affected eastern European countries. In the five-year periods of the 1990s, the highest number of AE cases detected in Poland was 10, rising to more than 20 cases in 2000–2004, and then over 55 cases in 2005–2009, with a cluster in the north-east of the country bordering Lithuania [49]. Interestingly, five Belarusian case reports were described in a hospital, close to the border area of Poland and Lithuania [64]. In the region of Brest, there are partially unpublished data regarding eight registered AE patients since 1995 (Alla Korzan, personal communication). In Slovakia, there were 11 confirmed cases from 2000 to 2009, but already 15 cases in 2010–2013 [63]. No Czech cases were registered between 1998 and 2006, however 20 cases in the period of 2007–2014 [62]. We can assume the further spread of the disease from the first molecular genetic evidence for the existence of human AE in Romania, as well as the first autochthonous case from south-western Hungary [57, 59]. Despite some high estimated figures of more than 1000 new cases annually [5], there is a distinct lack of data from Russia. Besides numerous single-centre studies with preselected study groups undergoing surgery, epidemiological data could only be found from Moscow [94, 95], the south of the Volga and Ural Federal Districts (neighbouring Republic of Bashkortostan and Chelyabinsk Oblast) [96, 97], the southwest of Siberia Federal District (Tomsk Oblast, Altai Krai) [66, 98] and the Far East Sakha Republic and the peninsula of Kamchatka [99, 100]. Nevertheless, the official registry of the Russian federal agency Rospotrebnadzor reported higher figures in 2008 (41 cases) than in 2001 (30 cases) [13, 98].
Knapp and co-workers studied the genetics of the observed spread to eastern Europe. They used the EmsB microsatellite marker to analyse the genetic diversity of E. multilocularis in various European endemic areas. They found the lowest diversity in Slovakia and Poland and the highest in Switzerland and the Swabian Jura, arguing for the two latter regions being the oldest endemic areas in Europe in evolutionary terms and for a ‘mainland-island’ system governing pathogen transmission [101]. In northern Europe, the number of cases in Lithuania rose: the incidence increased from 0.03/105/year in 2004 to 0.57/105/year in 2009 and 0.74/105/year in 2012, exceeding all the overall national incidences in Europe published since 2001 [47]. Six Swedish AE patients with assumed infection abroad were officially reported in the Public Health Agency in 2014 and 2017, with the first two diagnoses in 2012 [102, 103]. The European Food Safety Authority registered three cases in Estonia in 2013 (no information about site of infection or diagnostic criteria) [104]. In Finland, there are unpublished data about a native patient with PCR-confirmed AE and a travel history to endemic destinations in Europe (Antti Lavikainen, personal communication) [105].
In Southern Europe, Slovenian AE cases have been published for the first time. Although there have already been cases of the disease reported in Spain, E. multilocularis has never been demonstrated in the wildlife to date, so there is not sufficient evidence for the endemicity of the parasite [67, 106]. In Greece, a patient of Macedonian origin living in Thessaloniki was registered via the European Echinococcosis Registry (Petra Kern, personal communication) [68]. Since its reporting in the late 1990s, no new cases were documented out of this area. In summary, we can say that without exception, we found an increase in reported case numbers in all significant endemic European countries (i.e. countries from which there are at least 20 reported cases of AE). There are three relevant hypotheses to explain this rise in Europe.
First of all, there is an increase in the red fox population in Europe, which is also related to the elimination of rabies, together with higher infection rates with E. multilocularis [63, 106, 107]. One Swiss study showed a direct correlation between the growing fox population and the increase in human echinococcosis [43]. The observed increasing urbanisation of the fox habitat is also noteworthy [108–110]. Secondly, improved awareness of AE in the general population and healthcare workers may also have contributed to more cases being diagnosed or fewer incorrect diagnoses being made [111]. Thirdly, the possibilities for diagnostic investigation have improved considerably in the last 20 years, particularly with respect to imaging and molecular genetics [8, 63].
If we compare our findings with the current literature on the distribution of E. multilocularis in European red foxes, there are several countries in which the parasite has been detected in red foxes in this century but not in humans (Serbia, Croatia, Italy, Luxembourg, and Ukraine) [106, 112]. Human cases in these countries probably have to be reckoned with in the future.
North America
AE is extremely rare in North America, even though the infection rates recorded in animals are relatively high, e.g. 44.6% of foxes in northeast Nebraska and 35.3% of coyotes in Illinois [113, 114]. Despite these high figures, only two new cases have reliably been diagnosed in humans in the USA since more than four decades [198]. However, the literature was supplemented by two native individuals from the states of Alaska and Washington who were registered as deaths to AE on a death certificate in the National Center for Health Statistics (NCHS) and, therefore, convincing evidence is still lacking [115, Ben Bristow, personal communication]. From Alaska, where 54 human infections have been reported from 1947 to 1986 [reviewed by 116], no confirmed subsequent cases were found. In Canada, AE cases are thought to be (predominantly) non-autochthonous [69, 70]. Interestingly, a public health report of the government of the province of Alberta suggests some diagnosed autochthonous cases since 2013 [117]. Furthermore, the Canadian Institute for Health Information has documented at least three human infections in Ontario between 2014 and May 2018 [118] and a recent review of Wen and co-workers has mentioned unpublished case reports in Quebec and Manitoba [119]. Besides the possibility of misdiagnosis, one hypothesis to explain the discrepancy between the high infection rates in the wildlife and the extreme rarity of autochthonous cases in North America is the genetic expression of E. multilocularis in these areas combined with a human population of correspondingly low susceptibility. To the best of our knowledge, in fact, there has been only one proven case of human infection with the North American haplotype so far, detected in a DNA-based analysis of a sample of a patient diagnosed in Minnesota in 1977 [12, 120]. Remarkably, since 2009, multiple cases of animals infected with the European-type strain have been documented in Canada, including dogs infected as intermediate hosts. Unlike the North American strain, this strain is typically associated with human disease. We can, therefore, speculate that the European strain could have become established in the region and any human cases in Canada in the future may indeed be autochthonous in nature [121, 122, Janna Schurer, personal communication].
Africa
As with the case in Spain, despite the transparency of the diagnostic investigations in the case report from Morocco, E. multilocularis has not been confirmed in North African wildlife and there is not yet any concrete evidence of its presence [5, 8].
Limitations
On the basis of the available literature, it is currently not possible to obtain a valid list of the worldwide prevalence of human AE without many gaps, as both the quantity and quality of the published data are insufficient for the purpose. The reasons for this are manifold. AE is a notifiable disease only in some places, e.g. in most European countries but, on the North American continent, only in the Northwest Territories and Ontario in Canada [105, 111, 118]. AE is frequently not distinguished from CE, even though the latter is a distinct disease entity with different transmission profiles, risk factors, and clinical manifestations, requiring quite different control and surveillance measures and treatment [1, 123]. Out of the echinococcosis cases officially notified to the European Union in 2013, 31.7% (253 cases) did not differentiate between AE and CE [124]. Furthermore, due to the initial asymptomatic period of 5–15 years, it is usually not possible to pinpoint the precise location where the parasite was ingested [75]. In addition, most entries in the registries do not have a case definition, i.e. are not based on firm diagnostic criteria, which makes it more difficult to compare the recorded data. If there was a case definition given by the authors, we could not verify its quality by reviewing the defining imaging data or other diagnostic criteria.
Because of the long incubation period, we have to suspect the existence of a large proportion of asymptomatic individuals, who have also not been recorded. There are probably also considerable numbers of symptomatic patients living in poor economic and/or remote areas who remain undiagnosed and are therefore not included in epidemiological registries or corresponding studies [8, 75].
One limitation of this article is the lack of comparability of the units in the data. The prevalence or incidence is only rarely calculated in the scientific papers, which makes the interpretation of case numbers more challenging.
Another limitation can be found in the fact that, although the literature was published in 2001–2018, the time frame of the diagnosed cases ranged from 1937 up to 2017, giving the data a temporal inhomogeneity. Even though an increase of reported cases as well as a spread in several mentioned areas has been confirmed by this work, a significant bias cannot be excluded; a statistical analysis did not seem reasonable due to the inhomogeneity of the collected data. Due to recent improvement of diagnostics, as discussed above, an increase in data quantity can be assumed [8, 63].
Following our inclusion and exclusion criteria, it can be supposed that grey literature of interest is missing in our synopsis. We discussed some of these sources above; adding those cases from Uzbekistan, Sweden, Finland and Estonia, AE could be assumed to have been reported in overall 40 countries in the twenty-first century. However, only in 36 of those nations, publications which meet some basic quality criteria were existent.
With respect to the mapping, the main limitation is the worldwide lack of valid data, insufficient even for topographical interpolation estimating the borders of endemic disease areas and the corresponding prevalences.
From the epidemiological point of view, a national obligation to report AE as a notifiable disease, including its differentiation from CE, would be desirable in endemic countries. The data should be entered into national AE registries, which should be standardised and coordinated on an international level to generate comparable datasets and ultimately ensure high validity [125]. In addition, every effort should be made to achieve a precisely defined uniform terminology relating to echinococcosis and its pathogenic agents.
Conclusions
This systematic review provides an overview of the epidemiologically relevant literature on AE in the twenty-first century and underlines trends in the distribution of human AE. Our paper demonstrates an increasing number of reported cases in western, northern and eastern Europe, as well as in central Asia. In addition, we have established areas in which AE was not reported prior to 2001. The study shows that there are still fundamental gaps in our knowledge on the endemicity of the disease, as well as its prevalence and incidence. Original studies on the prevalence and incidence of AE are lacking from many parts of the world and further research on the subject is required.
Acknowledgements
Members of the Echinococcosis Working Group Ulm: Thomas FE Barth, Sven Baumann, Johannes Bloehdorn, Iris Fischer, Tilmann Graeter, Natalja Graf, Beate Gruener, Doris Henne-Bruns, Andreas Hillenbrand, Tanja Kaltenbach, Peter Kern, Petra Kern, Katharina Klein, Wolfgang Kratzer, Niloofar Ehteshami, Patrycja Schlingeloff, Julian Schmidberger, Rong Shi, Yael Staehelin, Frauke Theis, Daniil Verbitskiy, Ghaith Zarour.
Abbreviation
- SB
Sven Baumann
- RS
Rong Shi
- WL
Wenya Liu
- HB
Haihua Bao
- JS
Julian Schmidberger
- WK
Wolfgang Kratzer
- WXL
Weixia Li
Funding
The results included data and results from a German Research Foundation (DFG) funded project called “Establishment of a national database for alveolar echinococcosis” (Ref. no. KA 4356/3-1 and Ref. no. KR 5204/1-2), Natural Science Foundation of China (NSFC, 81260232) “Multiple imaging study of the Hepatic Alveolar Echinococcosis after albendazole treatment”, the Qinghai Science & Technology Department (Ref. no. 2017-SF-158), Science and Technology Major Project of Qinghai Province (Ref. no. 2016-SF-A5), and Müller Holding Ltd. & Co. KG Ulm.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no competing interests.
Footnotes
Members of “The interdisciplinary Echinococcosis Working Group Ulm” are listed in acknowledgement section.
Fig. 3 in the original version of this article has been replaced. The corrected Fig. 3 is given below.
Change history
10/11/2021
A Correction to this paper has been published: 10.1007/s15010-021-01695-6
Contributor Information
Wolfgang Kratzer, Email: wolfgang.kratzer@uniklinik-ulm.de.
the interdisciplinary Echinococcosis Working Group Ulm:
Thomas F. E. Barth, Sven Baumann, Johannes Bloehdorn, Iris Fischer, Tilmann Graeter, Natalja Graf, Beate Gruener, Doris Henne-Bruns, Andreas Hillenbrand, Tanja Kaltenbach, Peter Kern, Petra Kern, Katharina Klein, Wolfgang Kratzer, Niloofar Ehteshami, Patrycja Schlingeloff, Julian Schmidberger, Rong Shi, Yael Staehelin, Frauke Theis, Daniil Verbitskiy, and Ghaith Zarour
References
- 1.Eckert J, Deplazes P. Biological, epidemiological, and clinical aspects of echinococcosis, a zoonosis of increasing concern. Clin Microbiol Rev. 2004;17:107–135. doi: 10.1128/CMR.17.1.107-135.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Romig T, Deplazes P, Jenkins D, Giraudoux P, Massolo A, Craig PS, et al. Ecology and life cycle patterns of echinococcus species. Adv Parasitol. 2017;95:213–314. doi: 10.1016/bs.apar.2016.11.002. [DOI] [PubMed] [Google Scholar]
- 3.Eckert J. Guidelines for treatment of cystic and alveolar echinococcosis in humans. WHO Informal Working Group on Echinococcosis. Bull World Health Organ. 1996;74:231–242. [PMC free article] [PubMed] [Google Scholar]
- 4.Torgerson PR, Schweiger A, Deplazes P, Pohar M, Reichen J, Ammann RW, et al. Alveolar echinococcosis: from a deadly disease to a well-controlled infection. Relative survival and economic analysis in Switzerland over the last 35 years. J Hepatol. 2008;49:72–77. doi: 10.1016/j.jhep.2008.03.023. [DOI] [PubMed] [Google Scholar]
- 5.Torgerson PR, Keller K, Magnotta M, Ragland N. The global burden of alveolar echinococcosis. PLoS Negl Trop Dis. 2010;4:e722. doi: 10.1371/journal.pntd.0000722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization (WHO) World health statistics: monitoring health for the SDGs, sustainable development goals. Geneva: WHO; 2018. p. 2018. [Google Scholar]
- 7.Food and Agriculture Organization of the United Nations (FAO)/World Health Organization (WHO) Multicriteria-based ranking for risk management of food-borne parasites. Microbiological risk assessment series no 23. Rome: FAO/WHO; 2014. [Google Scholar]
- 8.Deplazes P, Rinaldi L, Alvarez Rojas CA, Torgerson PR, Harandi MF, Romig T, et al. Global distribution of alveolar and cystic echinococcosis. Adv Parasitol. 2017;95:315–493. doi: 10.1016/bs.apar.2016.11.001. [DOI] [PubMed] [Google Scholar]
- 9.Craig PS. An epidemiological and ecological study of human alveolar echinococcosis transmission in south Gansu, China. Acta Trop. 2000;77:167–177. doi: 10.1016/s0001-706x(00)00134-0. [DOI] [PubMed] [Google Scholar]
- 10.McManus DP, Li Z, Yang S, Gray DJ, Yang YR. Case studies emphasising the difficulties in the diagnosis and management of alveolar echinococcosis in rural China. Parasit Vectors. 2011;4:196. doi: 10.1186/1756-3305-4-196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Otero-Abad B, Torgerson PR. A systematic review of the epidemiology of echinococcosis in domestic and wild animals. PLoS Negl Trop Dis. 2013;7:e2249. doi: 10.1371/journal.pntd.0002249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nakao M, Xiao N, Okamoto M, Yanagida T, Sako Y, Ito A. Geographic pattern of genetic variation in the fox tapeworm Echinococcus multilocularis. Parasitol Int. 2009;58:384–389. doi: 10.1016/j.parint.2009.07.010. [DOI] [PubMed] [Google Scholar]
- 13.Konyaev SV, Yanagida T, Nakao M, Ingovatova GM, Shoykhet YN, Bondarev AY, et al. Genetic diversity of Echinococcus spp. in Russia. Parasitology. 2013;140:1637–1647. doi: 10.1017/S0031182013001340. [DOI] [PubMed] [Google Scholar]
- 14.Knapp J, Gottstein B, Saarma U, Millon L. Taxonomy, phylogeny and molecular epidemiology of Echinococcus multilocularis: from fundamental knowledge to health ecology. Vet Parasitol. 2015;213:85–91. doi: 10.1016/j.vetpar.2015.07.030. [DOI] [PubMed] [Google Scholar]
- 15.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Usubalieva J, Minbaeva G, Ziadinov I, Deplazes P, Torgerson PR. Human alveolar echinococcosis in Kyrgyzstan. Emerg Infect Dis. 2013;19:1095–1097. doi: 10.3201/eid1907.121405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ren L, Zhang L, Zhou F, Fan H, Deng Y, Wang H, et al. Epidemiological investigation on hepatic hydatid disease in Banma County. Chin J Dis Control Prev. 2016;20:1032–1035. [Google Scholar]
- 18.Yu W, Wang Q, Liao S, Zhong B, Liu L, Huang Y, et al. Echinococcosis prevalence in humans in Shiqu County of Sichuan in 2017. Prev Med Inf. 2018;34:545–549. [Google Scholar]
- 19.Uzunlar AK, Yilmaz F, Bitiren M. Echinococcosis multilocularis in south-eastern Anatolia, Turkey. East Afr Med J. 2003;80:395–397. [PubMed] [Google Scholar]
- 20.Maddah G, Abdollahi A, Sharifi-Nooghabi R, Tavassoli A, Rajabi-Mashadi MT, Jabbari-Nooghabi A, et al. Difficulties in the diagnosis and management of alveolar hydatid disease: a case series. Caspian J Intern Med. 2016;7:52–56. [PMC free article] [PubMed] [Google Scholar]
- 21.Bebezov B, Mamashev N, Umetaliev T, Ziadinov I, Craig PS, Joekel DE, et al. Intense focus of alveolar echinococcosis, South Kyrgyzstan. Emerg Infect Dis. 2018;24:1119–1122. doi: 10.3201/eid2406.161641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Graham JC, Gunn M, Hudson M, Orr KE, Craig PS. A mass in the liver. J Infect. 2002;45:121–122. doi: 10.1053/jinf.2002.0997. [DOI] [PubMed] [Google Scholar]
- 23.Nagesh BS, Kakkar N, Katariya RN, Vasishta RK. Recurrent alveolar hydatid disease of liver. Indian J Gastroenterol. 2002;21:235–236. [PubMed] [Google Scholar]
- 24.Shaw AK, Gambhir RPS, Chaudhry R, Jaiswal SS. Ecchinococcus multilocularis causing alveolar hydatid disease liver: a rare occurrence in Indian subcontinent. Trop Gastroenterol. 2010;31:119–120. [PubMed] [Google Scholar]
- 25.Tyagi DK, Balasubramaniam S, Sawant HV. Primary calcified hydatid cyst of the brain. J Neurosci Rural Pract. 2010;1:115–117. doi: 10.4103/0976-3147.71729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bhatia JK, Ravikumar R, Naidu CS, Sethumadhavan T. Alveolar hydatid disease of the liver: a rare entity in India. Med J Armed Forces India. 2016;72:S126–S129. doi: 10.1016/j.mjafi.2015.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Prabhakar N, Kalra N, Behera A, Das A, Lal A, Dhiman RK, et al. Large heterogeneous calcified masses in liver: a diagnostic dilemma. J Clin Exp Hepatol. 2017;7:385–386. doi: 10.1016/j.jceh.2017.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Goja S, Saha SK, Yadav SK, Tiwari A, Soin AS. Surgical approaches to hepatic hydatidosis ranging from partial cystectomy to liver transplantation. Ann Hepatobiliary Pancreat Surg. 2018;22:208. doi: 10.14701/ahbps.2018.22.3.208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bansal N, Vij V, Rastogi M, Wadhawan M, Kumar A. A report on three patients with Echinococcus multilocularis: lessons learned. Indian J Gastroenterol. 2018;37:353–358. doi: 10.1007/s12664-018-0860-y. [DOI] [PubMed] [Google Scholar]
- 30.Ali I, Khan Panni M, Iqbal A, Iqbal M, Ahmad A, Ali A. Molecular characterization of echinococcus species in Khyber pakhtunkhwa, pakistan. Acta Sci Vet. 2015;43:1277. [Google Scholar]
- 31.Wang Q, Vuitton DA, Qiu J, Giraudoux P, Xiao Y, Schantz PM, et al. Fenced pasture: a possible risk factor for human alveolar echinococcosis in Tibetan pastoralist communities of Sichuan, China. Acta Trop. 2004;90:285–293. doi: 10.1016/j.actatropica.2004.02.004. [DOI] [PubMed] [Google Scholar]
- 32.Dingmu L, Guo Y, Gao Y, Chu Y, Zhu M, Xu S, et al. 丁木拉提,郭永 忠,高永盛,初伊明,朱马拜,许舒波,温浩.新疆自治区尼勒克县乌拉斯台乡包虫 病流行病学调查[J].中华流行病学杂. Chin J Epidemiol. 2005;26:131. [Google Scholar]
- 33.Meng K, Yin Y, Yan X. 新疆尼勒克县乌拉斯台乡包虫病流行情况调查分析. Xinjiang Medicine. 2005;35:182–183. [Google Scholar]
- 34.Feng X, Qi X, Yang L, Duan X, Fang B, Gongsang Q, et al. Human cystic and alveolar echinococcosis in the Tibet Autonomous Region (TAR), China. J Helminthol. 2015;89:671–679. doi: 10.1017/S0022149X15000656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yang YR, Cheng L, Yang SK, et al. A hospital-based retrospective survey of human cystic and alveolar echinococcosis in Ningxia Hui Autonomous Region, PR China. Acta Trop. 2006;97:284–291. doi: 10.1016/j.actatropica.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 36.Shi D, Zhao Y, Guo Z, Bao G, Li F, Chen G, et al. Prevalence and risk factor analysis of alveolar echinococcosis in Dingxi Prefecture of Gansu province. Chin J Zoonoses. 2004;20:815–818. [Google Scholar]
- 37.Ito A, Agvaandaram G, Bat-Ochir OE, Chuluunbaatar B, Gonchigsenghe N, Yanagida T, et al. Histopathological, serological, and molecular confirmation of indigenous alveolar echinococcosis cases in Mongolia. Am J Trop Med Hyg. 2010;82:266–269. doi: 10.4269/ajtmh.2010.09-0520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ito A, Budke CM. The echinococcoses in Asia: the present situation. Acta Trop. 2017;176:11–21. doi: 10.1016/j.actatropica.2017.07.013. [DOI] [PubMed] [Google Scholar]
- 39.Taniguchi K, Hashimoto S, Kawado M, Murakami Y, Izumida M, Otha A, et al. Overview of infectious disease surveillance system in Japan, 1999-2005. J Epidemiol. 2007;17(Suppl):S3–S13. doi: 10.2188/jea.17.S3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kim SJ, Kim JH, Han SY, Kim YH, Cho JH, Chai JY, et al. Recurrent hepatic alveolar echinococcosis: report of the first case in Korea with unproven infection route. Korean J Parasitol. 2011;49:413–418. doi: 10.3347/kjp.2011.49.4.413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Huang J, Wu YM, Liang PC, Lee PH. Alveolar hydatid disease causing total occlusion of the inferior vena cava. J Formos Med Assoc. 2004;103:633–636. [PubMed] [Google Scholar]
- 42.Warnnissorn N, Uiprasertkul M, Atisook K, Sirivatanauksorn Y, Limawongpranee S. Alveolar echinococcosis in a Thai patient after migration to an endemic area in Central Europe. Travel Med Infect Dis. 2006;4:34–37. doi: 10.1016/j.tmaid.2004.07.010. [DOI] [PubMed] [Google Scholar]
- 43.Limawongpranee S, Uiprasertkul M, Sirivatanauksorn Y, Keerasuntonpong A. Alveolar echinococcosis: An unusual liver mass in a Thai Patient. Siriraj Hosp Gaz. 2004;56:308–314. [Google Scholar]
- 44.Schneider R, Aspöck H, Auer H. Unexpected increase of alveolar echincoccosis, Austria, 2011. Emerg Infect Dis. 2013;19:475–477. doi: 10.3201/eid1903.120595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Comte S, Raton V, Raoul F, Hegglin D, Giraudoux P, Deplazes P, et al. Fox baiting against Echinococcus multilocularis: contrasted achievements among two medium size cities. Prev Vet Med. 2013;111:147–155. doi: 10.1016/j.prevetmed.2013.03.016. [DOI] [PubMed] [Google Scholar]
- 46.Grenouillet F, Knapp J, Millon L, Raton V, Richou C, Piarroux M, et al. Encadré–L’échinococcose alvéolaire humaine en France en 2010/Box–Human alveolar echinococcosis in France, update 2010. BEH Hors-sér. 2010;24.
- 47.Marcinkutė A, Šarkūnas M, Moks E, Saarma U, Jokelainen P, Bagrade G, et al. Echinococcus infections in the Baltic region. Vet Parasitol. 2015;213:121–131. doi: 10.1016/j.vetpar.2015.07.032. [DOI] [PubMed] [Google Scholar]
- 48.Schweiger A, Ammann RW, Candinas D, Clavien PA, Eckert J, Gottstein B, et al. Human alveolar echinococcosis after fox population increase, Switzerland. Emerg Infect Dis. 2007;13:878–882. doi: 10.3201/eid1306.061074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nahorski WL, Knap JP, Pawłowski ZS, Krawczyk M, Polanski J, Stefaniak J, et al. Human alveolar echinococcosis in Poland: 1990–2011. PLoS Negl Trop Dis. 2013;7:e1986. doi: 10.1371/journal.pntd.0001986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Logar J, Soba B, Lejko-Zupanc T, Kotar T. Human alveolar echinococcosis in Slovenia. Clin Microbiol Infect. 2007;13:544–546. doi: 10.1111/j.1469-0691.2007.01701.x. [DOI] [PubMed] [Google Scholar]
- 51.Schmidberger J, Kratzer W, Stark K, Grüner B, Echinococcosis Working Group Alveolar echinococcosis in Germany, 1992–2016. An update based on the newly established national AE database. Infection. 2018;46:197–206. doi: 10.1007/s15010-017-1094-0. [DOI] [PubMed] [Google Scholar]
- 52.Charbonnier A, Knapp J, Demonmerot F, Bresson-Hadni S, Raoul F, Grenouillet F, et al. A new data management system for the French National Registry of human alveolar echinococcosis cases. Parasite. 2014;21:69. doi: 10.1051/parasite/2014075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.van Dommelen L, Stelma FF, Cappendijk VC, Abdul Hamid MA, Kortbeek LM, von Meyenfeldt MF, et al. First case of Echinococcus multilocularis acquired in the Netherlands. Antonie Van Leeuwenhoek. 2009;95:17–133. [Google Scholar]
- 54.van Dommelen L, Stoot JH, Cappendijk VC, Abdul Hamid MA, Stelma FF, Kortbeek LM, et al. The first locally acquired human infection of Echinococcus multilocularis in the Netherlands. J Clin Microbiol. 2012;50:1818–1820. doi: 10.1128/JCM.06355-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Landen S, Van de Sande J, Berger P, Ursaru D, Baert J, Delugeau V. Alveolar echinococcosis in a Belgian urban dweller. Acta Gastroenterol Belg. 2013;76:317–321. [PubMed] [Google Scholar]
- 56.Cambier A, Leonard P, Losson B, Giot J-B, Bletard N, Meunier P, et al. Alveolar echinococcosis in southern Belgium: retrospective experience of a tertiary center. Eur J Clin Microbiol Infect Dis. 2018;37:1195–1196. doi: 10.1007/s10096-018-3233-7. [DOI] [PubMed] [Google Scholar]
- 57.Dezsényi B, Strausz T, Makrai Z, Csomor J, Danka J, Kern P, et al. Autochthonous human alveolar echinococcosis in a Hungarian patient. Infection. 2017;45:107–110. doi: 10.1007/s15010-016-0918-7. [DOI] [PubMed] [Google Scholar]
- 58.Myjak P, Nahorski W, Pietkiewicz H, von Nickisch-Rosenegk M, Stolarczyk J, Kacprzak E, et al. Molecular confirmation of human alveolar echinococcosis in Poland. Clin Infect Dis. 2003;37:e121–e125. doi: 10.1086/378296. [DOI] [PubMed] [Google Scholar]
- 59.Šnábel V, Calma C, Georgescu SO, Cavallero S, D’Amelio S, Vasilkova Z, et al. Genetic survey of alveolar and cystic echinococcoses in Romania: first molecular evidence of Echinococcus multilocularis in humans in the country. Helminthologia. 2017;54:189–198. [Google Scholar]
- 60.Miterpakova M, Dubinsky P. Fox tapeworm (Echinococcus multiloculoaris) in Slovakia—summarizing the long-term monitoring. Helminthologia. 2011;48:155. [Google Scholar]
- 61.Marcinkute A, Virbaliene R, Ziliukiene J, Barakauskiene A, Valantinas J, Strupas K, et al. Some aspects of Echinococcus multilocularis infection in humans in Lithuania. Bull Scand Baltic Soc Parasitol. 2005;14:102. [Google Scholar]
- 62.Kolářová L, Matějŭ J, Hrdỳ J, Kolarova H, Hozakova L, Zampachova V, et al. Human alveolar echinococcosis, Czech Republic, 2007–2014. Emerg Infect Dis. 2015;21:2263–2265. doi: 10.3201/eid2112.150743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Antolová D, Miterpakova M, Radoňak J, Hudackova D, Szilagyiova M, Zacek M. Alveolar echinococcosis in a highly endemic area of Northern Slovakia between 2000 and 2013. Euro Surveill. 2014;19:20882. [PubMed] [Google Scholar]
- 64.Prokopchik N, Grivachevsky A, Butolina K, Gavrilik A. Characteristics of alveococcosis of liver and other organs. Hepatology and Gastroenterology (Grodno). 2017;2:175–182. [Google Scholar]
- 65.Krasavtsev E, Nadyrov E, Zinovkin D, Loginov R, Doroshenko R, Tischenko V. Analysis of autopsies of the HIV-infected died in Gomel region in the period of 2006–2008. Пpoблeмы здopoвья и экoлoгии. 2009;2:111–113. [Google Scholar]
- 66.Kuracheva NA, Yaroshkina TN, Tolkayeva MV, Merzlikin NV, Brazhnikova NA, Tskhai VF, et al. Differential mechanical jaundices in ultrasonic diagnosis of parasitic liver problems. Бюллeтeнь cибиpcкoй мeдицины. 2012;11:135–145. [Google Scholar]
- 67.Arrechea Irigoyen MA, Córdoba Iturriagagoitia A, Tuñón Álvarez MT, Gómez Dorronsoro ML, Martínez-Peñuela Virseda JM. Equinococosis alveolar humana. Presentación de un caso. Rev Esp Patol. 2008;41:203–206. [Google Scholar]
- 68.Kern P, Bardonnet K, Renner E, Auer H, Pawlowski Z, Ammann RW, et al. European echinococcosis registry: human alveolar echinococcosis, Europe, 1982–2000. Emerg Infect Dis. 2003;9:343–349. doi: 10.3201/eid0903.020341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Massolo A, Liccioli S, Budke C, Klein C. Echinococcus multilocularis in North America: the great unknown. Parasite. 2014;21:73. doi: 10.1051/parasite/2014069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Schurer JM, Rafferty E, Farag M, Zeng W, Jenkins EJ. Echinococcosis: an economic evaluation of a veterinary public health intervention in rural Canada. PLoS Negl Trop Dis. 2015;9:e0003883. doi: 10.1371/journal.pntd.0003883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Yamasaki H, Nakao M, Nakaya K, Schantz PM, Ito A. Genetic analysis of Echinococcus multilocularis originating from a patient with alveolar echinococcosis occurring in Minnesota in 1977. Am J Trop Med Hyg. 2008;79:245–247. [PubMed] [Google Scholar]
- 72.Maliki M, Mansouri F, Bouhamidi B, Nabih N, Bernoussi Z, Mahassini N, et al. Hepatic alveolar hydatidosis in Morocco. Med Trop (Mars). 2004;64:379–380. [PubMed] [Google Scholar]
- 73.Eckert J, Deplazes P. Alveolar echinococcosis in humans: the current situation in Central Europe and the need for countermeasures. Parasitol Today. 1999;15:315–319. doi: 10.1016/s0169-4758(99)01476-3. [DOI] [PubMed] [Google Scholar]
- 74.Eckert J, Conraths FJ, Tackmann K. Echinococcosis: an emerging or re-emerging zoonosis? Int J Parasitol. 2000;30:1283–1294. doi: 10.1016/s0020-7519(00)00130-2. [DOI] [PubMed] [Google Scholar]
- 75.Eckert J, Gemmell MA, Meslin FX, Pawlowski ZS. WHO-OIE manual on echinococcosis in humans and animals: a public health problem of global concern. World Organisation for Animal Health Paris, 2001.
- 76.Craig P. Echinococcus multilocularis. Curr Opin Infect Dis. 2003;16:437–444. doi: 10.1097/00001432-200310000-00010. [DOI] [PubMed] [Google Scholar]
- 77.Vuitton DA, Zhou H, Bresson-Hadni S, Wang Q, Piarroux M, Raoul F, et al. Epidemiology of alveolar echinococcosis with particular reference to China and Europe. Parasitology. 2003;127:S87–S107. [PubMed] [Google Scholar]
- 78.Bodoshova A. Modern situation of patients with alveolar echinococcosis from hospital dates of Kyrgyz Republic. ЗДPABOOXPAHEHИE КЫPГЫЗCTAHA. 2011;2:93–97. [Google Scholar]
- 79.Raimkylov KM, Kuttubaev OT, Toigombaeva VS. Epidemiological analysis of the distribution of cystic and alveolar echinococcosis in Osh Oblast in the Kyrgyz Republic, 2000–2013. J Helminthol. 2015;89:651–654. doi: 10.1017/S0022149X15000565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Omorov RA, Aitbaev SA, Kanietov AK, Abdiev AA. Dynamics of patients admissions with liver alveolar echinococcosis in Kyrgyz Republic. ИЗBECTИЯ BУЗOB КЫPГЫЗCTAHA. 2017;6:41–42. [Google Scholar]
- 81.Torgerson PR. The emergence of echinococcosis in central Asia. Parasitology. 2013;140:1667–1673. doi: 10.1017/S0031182013000516. [DOI] [PubMed] [Google Scholar]
- 82.Abdybekova A, Sultanov A, Karatayev B, Zhumabayeva A, Shapiyeva Z, Yeshmuratov T, et al. Epidemiology of echinococcosis in Kazakhstan: an update. J Helminthol. 2015;89:647–650. doi: 10.1017/S0022149X15000425. [DOI] [PubMed] [Google Scholar]
- 83.Ahmedov SM, Safarov BD, Tabarov ZV, Radzhabov AM. Diagnostic and surgical treatment of alveococcosis of liver. ЗДPABOOXPAHEHИE TAДЖИКИCTAHA. 2014;1:60–65. [Google Scholar]
- 84.Madatov KA, Allazarov UA, Lukmonov SN. Stress ulcers as complications after liver resection and their prevention. In: Liver Cancer the 9th Asia-Pacific primary liver cancer expert meeting, APPLE 2018 South Korea [Internet]. Seoul: Karger AG Basel; 2018. S. 136. https://www.karger.com/Article/FullText/490877. Accessed 20 Mar 2019.
- 85.Benyan AK, Mahdi NK, Abdul-Amir F, Ubaid O. Second reported case of multilocular hydatid disease in Iraq. Qatar Med J. 2013;2013:28–29. doi: 10.5339/qmj.2013.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Cai H, Guan Y, Ma X, Wang L, Wang H, Su G, et al. Epidemiology of echinococcosis among schoolchildren in Golog Tibetan Autonomous Prefecture, Qinghai, China. Am J Trop Med Hyg. 2017;96:674–679. doi: 10.4269/ajtmh.16-0479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Yang YR, Craig PS, Vuitton DA, Williams GM, Sun T, Liu TX, et al. Serological prevalence of echinococcosis and risk factors for infection among children in rural communities of southern Ningxia, China. Trop Med Int Health. 2008;13:1086–1094. doi: 10.1111/j.1365-3156.2008.02101.x. [DOI] [PubMed] [Google Scholar]
- 88.Oral A, Ozturk G, Aydinli B, Kantarci M, Salman AB. An unusual presentation of alveolar echinococcosis in a 12-yr-old immunocompetent child. Pediatr Transplant. 2012;16:E375–E378. doi: 10.1111/j.1399-3046.2012.01735.x. [DOI] [PubMed] [Google Scholar]
- 89.Vuitton DA, Wang Q, Zhou HX, Raoul F, Knapp J, Bresson-Hadni S, et al. A historical view of alveolar echinococcosis, 160 years after the discovery of the first case in humans: part 1. What have we learnt on the distribution of the disease and on its parasitic agent? Chin Med J. 2011;124:2943–2953. [PubMed] [Google Scholar]
- 90.Laursen AL, David KP. A Danish case of Echinococcus multiocularis. Ugeskr Laeger. 2004;166:911–912. [PubMed] [Google Scholar]
- 91.Svrckova P, Nabarro L, Chiodini PL, Jäger HR. Disseminated cerebral hydatid disease (multiple intracranial echinococcosis) Pract Neurol. 2019;19:156–163. doi: 10.1136/practneurol-2018-001954. [DOI] [PubMed] [Google Scholar]
- 92.Bresson-Hadni S, Grenouillet F, Chauchet A, Richou C, Knapp J, Delabrousse E, et al. Diagnostic de l’échinococcose alvéolaire. Rev Francoph Lab. 2014;2014:77–87. [Google Scholar]
- 93.Chauchet A, Grenouillet F, Knapp J, Richou C, Delabrousse E, Dentan C, et al. Increased incidence and characteristics of alveolar echinococcosis in patients with immunosuppression-associated conditions. Clin Infect Dis. 2014;59:1095–1104. doi: 10.1093/cid/ciu520. [DOI] [PubMed] [Google Scholar]
- 94.Gautier SV, Tsiroulnikova OM, Moysyuk YG, Akhaladze DG, Tsiroulnikova IE, Silina OV, et al. Liver transplantation in children: six-year experience analysis. Russ J Transplantol Artif Organs. 2014;16:54. [Google Scholar]
- 95.Kotlayrov PM. Beam methods of research in diagnostics of parasitic damages of lungs. ВЕСТНИК РОССИЙСКОГО НАУЧНОГО ЦЕНТРА РЕНТГЕНОРАДИОЛОГИИ МИНЗДРАВА РОССИИ. 2015;14:51–63.
- 96.Nartaylakov MARR, Abdeev R, Kurbangulov I, Gritsaenko A, Zagitov A, Mukhamedjanov G. Difficulties in the development of liver transplantation. Becтник Кaзaxcкoгo Haциoнaльнoгo мeдицинcкoгo yнивepcитeтa. 2015;1:223–232. [Google Scholar]
- 97.Zotova A, Afanasyieva N, Vazhenina D. Combined positron emission and computed tomography (PET-CT): potential of the method in differential diagnosis of hepatic masses, and also in detection of the primary sites at suspicion of metastatic malignancies in the liver. Human Sport Med. 2017;17:32–42. [Google Scholar]
- 98.Konyaev SV, Yanagida T, Ingovatova GM, Shoikhet YN, Nakao M, Sako Y, et al. Molecular identification of human echinococcosis in the Altai region of Russia. Parasitol Int. 2012;61:711–714. doi: 10.1016/j.parint.2012.05.009. [DOI] [PubMed] [Google Scholar]
- 99.Sleptsov K, Baranova T. Immediate results of minimally invasive treatment of liver abscesses. Ближaйшиe peзyльтaты мaлoинвaзивнoгo лeчeния aбcцeccoв пeчeни. Acta Biomed Sci. 2012;4:92–94. [Google Scholar]
- 100.Kharchenko V, Kotlyarov P, Karpenko V. Intervention under the ultrasonic control in liver focal disease treatment. Дaльнeвocтoчный мeдицинcкий жypнaл. 2007;2:46–49. [Google Scholar]
- 101.Knapp J, Bart JM, Giraudoux P, Glowatzki ML, Breyer I, Raoul F, et al. Genetic diversity of the cestode Echinococcus multilocularis in red foxes at a continental scale in Europe. PLoS Negl Trop Dis. 2009;3:e452. doi: 10.1371/journal.pntd.0000452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Echinokockinfektion under 2014. https://www.folkhalsomyndigheten.se/folkhalsorapportering-statistik/statistikdatabaser-och-visualisering/sjukdomsstatistik/echinokockinfektion/kommentarer-och-specialstatistik/2014/. Accessed 20 Mar 2019.
- 103.Echinokockinfektion under 2017. https://www.folkhalsomyndigheten.se/folkhalsorapportering-statistik/statistikdatabaser-och-visualisering/sjukdomsstatistik/echinokockinfektion/kommentarer-och-specialstatistik/2017/. Accessed 20 Mar 2019.
- 104.EFSA/ECDC (European Food Safety Authority/European Centre for Disease Prevention and Control): The European Union summary report on trends and sources of zoonoses, zoonotic agents and food-borne outbreaks in 2013. EFSA J. 2015;13:3991.
- 105.Davidson RK, Lavikainen A, Konyaev S, Schurer J, Miller AL, Oksanen A, et al. Echinococcus across the north: current knowledge, future challenges. Food Waterborne Parasitol. 2016;4:39–53. [Google Scholar]
- 106.Oksanen A, Siles-Lucas M, Karamon J, Possenti A, Conraths FJ, Romig T, et al. The geographical distribution and prevalence of Echinococcus multilocularis in animals in the European Union and adjacent countries: a systematic review and meta-analysis. Parasit Vectors. 2016;9:519. doi: 10.1186/s13071-016-1746-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Combes B, Comte S, Raton V, Raoul F, Boué F, Umhang G, et al. Westward spread of Echinococcus multilocularis in foxes, France, 2005–2010. Emerg Infect Dis. 2012;18:2059–2062. doi: 10.3201/eid1812.120219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Gloor S, Bontadina F, Hegglin D, Deplazes P, Breitenmoser U. The rise of urban fox populations in Switzerland. Mamm Biol. 2001;66:155–164. [Google Scholar]
- 109.Deplazes P, Hegglin D, Gloor S, Romig T. Wilderness in the city: the urbanization of Echinococcus multilocularis. Trends Parasitol. 2004;20:77–84. doi: 10.1016/j.pt.2003.11.011. [DOI] [PubMed] [Google Scholar]
- 110.Liccioli S, Giraudoux P, Deplazes P, Massolo A. Wilderness in the ‘city’ revisited: different urbes shape transmission of Echinococcus multilocularis by altering predator and prey communities. Trends Parasitol. 2015;31:297–305. doi: 10.1016/j.pt.2015.04.007. [DOI] [PubMed] [Google Scholar]
- 111.Vuitton DA, Demonmerot F, Knapp J, Richou C, Grenouillet F, Chauchet A, et al. Clinical epidemiology of human AE in Europe. Vet Parasitol. 2015;213:110–120. doi: 10.1016/j.vetpar.2015.07.036. [DOI] [PubMed] [Google Scholar]
- 112.Lalosevic D, Lalosevic V, Simin V, Miljevic M, Cabrilo B, Cabrilo OB. Spreading of multilocular echinococcosis in southern Europe: the first record in foxes and jackals in Serbia, Vojvodina Province. Eur J Wildl Res. 2016;62:793–796. [Google Scholar]
- 113.Storandt ST, Kazacos KR. Echinococcus multilocularis identified in Indiana, Ohio, and east-central Illinois. J Parasitol. 1993;79:301–305. [PubMed] [Google Scholar]
- 114.Storandt ST, Virchow DR, Dryden MW, Hygnstrom SE, Kazacos KR. Distribution and prevalence of Echinococcus multilocularis in Wild Predators in Nebraska, Kansas, and Wyoming. J Parasitol. 2002;88:420–422. doi: 10.1645/0022-3395(2002)088[0420:DAPOEM]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 115.Bristow BN, Lee S, Shafir S, Sorvillo F. Human echinococcosis mortality in the United States, 1990–2007. PLoS Negl Trop Dis. 2012;6:e1524. doi: 10.1371/journal.pntd.0001524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Jenkins EJ, Castrodale LJ, de Rosemond SJC, Dixon BR, Elmore SA, Gesy KM, et al. Chapter two—tradition and transition: parasitic zoonoses of people and animals in Alaska, Northern Canada, and Greenland. Adv Parasitol. 2013;82:33–204. doi: 10.1016/B978-0-12-407706-5.00002-2. [DOI] [PubMed] [Google Scholar]
- 117.Government of Alberta: Public health notifiable disease management guidelines: echinococcosis (alveolar) – Epidemiology (January 2018). https://open.alberta.ca/dataset/140a7c4a-d7bd-4909-b02f-24c7b35afc63/resource/16526c63-fffb-4330-9df2-51c16578c7cf/download/guidelines-echinococcus-2018-04.pdf. Accessed 20 Mar 2019.
- 118.Kotwa JD, Isaksson M, Jardine CM, Campbell GD, Berke O, Pearl DL, et al. Echinococcus multilocularis infection, Southern Ontario, Canada. Emerg Infect Dis. 2019;25:265–272. doi: 10.3201/eid2502.180299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Wen H, Vuitton L, Tuxun T, Li J, Vuitton DA, Zhang W, et al. Echinococcosis: advances in the 21st century. Clin Microbiol Rev. 2019;32:e00075–e00118. doi: 10.1128/CMR.00075-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Klein C, Massolo A. Demonstration that a case of human alveolar echinococcosis in Minnesota in 1977 was caused by the N2 strain. Am J Trop Med Hyg. 2015;92:477–478. doi: 10.4269/ajtmh.14-0484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Jenkins EJ, Peregrine AS, Hill JE, Somers C, Gesy K, Barnes B, et al. Detection of European strain of Echinococcus multilocularis in North America. Emerg Infect Dis. 2012;18:1010–1012. doi: 10.3201/eid1806.111420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Trotz-Williams LA, Mercer NJ, Walters JM, Wallace D, Gottstein B, Osterman-Lind E, et al. Public health follow-up of suspected exposure to Echinococcus multilocularis in Southwestern Ontario. Zoonoses Public Health. 2017;64:460–467. doi: 10.1111/zph.12326. [DOI] [PubMed] [Google Scholar]
- 123.Brunetti E, Kern P, Vuitton DA, Writing Panel for the WHO-IWGE Writing panel for the WHO-IWGE expert consensus for the diagnosis and treatment of cystic and alveolar echinococcosis in humans. Acta Trop. 2010;114:1–16. doi: 10.1016/j.actatropica.2009.11.001. [DOI] [PubMed] [Google Scholar]
- 124.EFSA and ECDC (European Food Safety Authority, European Centre for Disease Prevention and Control) The European Union summary report on trends and sources of zoonoses, zoonotic agents and food-borne outbreaks in 2016. EFSA J. 2017;15:5077. doi: 10.2903/j.efsa.2017.5077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Said-Ali Z, Grenouillet F, Knapp J, Bresson-Hadni S, Vuitton DA, Raoul F, et al. Detecting nested clusters of human alveolar echinococcosis. Parasitology. 2013;140:1693–1700. doi: 10.1017/S0031182013001352. [DOI] [PubMed] [Google Scholar]
- 126.Bartholomot B, Vuitton DA, Harraga S, Shi DZ, Giraudoux P, Barnish G, et al. Combined ultrasound and serologic screening for hepatic alveolar echinococcosis in central China. Am J Trop Med Hyg. 2002;66:23–29. doi: 10.4269/ajtmh.2002.66.23. [DOI] [PubMed] [Google Scholar]
- 127.Shi D, Li W, Bao G. Approach to risk factor of human behavior on epidemic of alveolar echinococcosis. Chin J Public Health. 2003;19:973–974. [Google Scholar]
- 128.Ma Y, Shang W. Endemic situation of echinococcosis in Gannan Tibetan Autonomous Prefecture. Chin J Parasitol Parasit Dis. 2015;33:352–356. [PubMed] [Google Scholar]
- 129.Wang QH, Shang WJ, Zhao CT, Zhang SW, Lu SL, Liu XD. Epidemic status of echinococcosis in Gannan Tibetan Autonomous prefecture of Gansu Province during 2007–2011. Chin J Parasitol Parasit Dis. 2015;33:45–48. [PubMed] [Google Scholar]
- 130.Han J, Bao G, Zhang D, Gao P, Wu T, Craig P, et al. A newly discovered epidemic area of Echinococcus multilocularis in West Gansu Province in China. PLoS One. 2015;10:e0132731. doi: 10.1371/journal.pone.0132731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Wang D, Feng Y, Li F, Ge P, Zhang T, Hu W, et al. An epidemiological survey on hydatid disease in Tibetan autonomous areas of Gansu Province. Chin J Parasitol Parasit Dis. 2017;35:140–144. [Google Scholar]
- 132.Li M, Li J, Liu X. A retrospect on the diagnosis and treatment of 263 cases of hepatic alveolar echinococcosis in 17 years. Chin J Parasitol Parasit Dis. 2003;21:192. [PubMed] [Google Scholar]
- 133.Li L, Xia Q, Fu D. Epidemiological survey of echinococcosis in rural population of Ningxia Hui Autonomous Region. Chin J Zoonoses. 2005;21:359–360. [Google Scholar]
- 134.Yang YR, Ellis M, Sun T, Li Z, Liu X, Vuitton DA, et al. Unique family clustering of human echinococcosis cases in a chinese community. Am J Tropical Med Hyg. 2006;74:487–494. [PubMed] [Google Scholar]
- 135.Yang YR, Sun T, Li Z, Zhang J, Teng J, Liu X, et al. Community surveys and risk factor analysis of human alveolar and cystic echinococcosis in Ningxia Hui Autonomous Region, China. Bull World Health Organ. 2006;84:714–721. doi: 10.2471/blt.05.025718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Pleydell DR, Yang YR, Danson FM, Raoul F, Craig PS, McManus DP, et al. Landscape composition and spatial prediction of alveolar echinococcosis in southern Ningxia, China. PLoS Negl Trop Dis. 2008;2:e287. doi: 10.1371/journal.pntd.0000287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Fang L, Huang L, Li Y, Yuan F, Li H, Yang Y. Analysis of echinococcosis infection among teenagers in Xiji County. J Ningxia Med Univ. 2012;8:798–801. [Google Scholar]
- 138.Wu XH, Ma X, Ning G, He DL, Mao JS, Wen X. 青海省兴海县包虫病流行 病学调查报告. Endem. Dis. Bull. 2001;16:98. [Google Scholar]
- 139.Qiu J, Li D, Wang H, Ito A, Liu F, Schantz P. Comparison of image techniques with serological tests for diagnosing echinococcosis. Am J Trop Med Hyg. 2003;1:97–100. [Google Scholar]
- 140.Schantz PM, Wang H, Qiu J, Liu FJ, Saito E, Emshoff A, et al. Echinococcosis on the Tibetan Plateau: prevalence and risk factors for cystic and alveolar echinococcosis in Tibetan populations in Qinghai Province, China. Parasitology. 2003;127(Suppl):S109–S120. [PubMed] [Google Scholar]
- 141.He D, Wu X, Liu B. An epidemiological survey on hydatid disease in Yushu connty, Qinghai Province. J Trop Dis Parasitol. 2003;1(24–25):44. [Google Scholar]
- 142.Wang H, Zhang J, Schantz P, Ito A, Craig P, Wu X, et al. Epidemiologic survey and analysis on echinococcosis in humans and animals from 1995 to 2005 in Qinghai province. Chin J Zoonoses. 2006;22:1129–1134. [Google Scholar]
- 143.Wu XH, Wang H, Kawanaka M, Morishima Y, Ma X, Liu P, et al. Epidemiologic survey and studies on echinococcosis in humans in Jiuzhi county of Qinghai province. Chin J Zoonoses. 2007;23:813–815. [Google Scholar]
- 144.Wu X, Wang H, Zhang J, Ma X, Liu Y, Han X, et al. An epidemiological survey on echinococcosis in Zhiduo County of Qinghai Province. Zhongguo Ji Sheng Chong Xue Yu Ji Sheng Chong Bing Za Zhi. 2007;25:229–231. [PubMed] [Google Scholar]
- 145.Yu SH, Wang H, Wu XH, Ma X, Liu PY, Liu YF, et al. Cystic and alveolar echinococcosis: an epidemiological survey in a Tibetan population in southeast Qinghai, China. Jpn J Infect Dis. 2008;61:242–246. [PubMed] [Google Scholar]
- 146.Han X, Wang H, Cai H, Ma X, Liu Y, Wei B, et al. Epidemiological survey on echinococcosis in Darlag County of Qinghai Province. Chin J Parasitol Parasit Dis. 2009;27:22–26. [PubMed] [Google Scholar]
- 147.Cai H, Guan Y, Wang H, Wu W, Han X, Ma X, et al. Geographical distribution of echinococcosis among children in Qinghai Province. Chin J Parasitol Parasit Dis. 2012;30:127–130. [PubMed] [Google Scholar]
- 148.Cai H, Wang H, Han X, Ma X. Correlation between definitive hosts of Echinococcus and echinococcosis in children in Qinghai plateau, China, 1990-2010. Chin J Zoonoses. 2012;28:500–502. [Google Scholar]
- 149.Giraudoux P, Raoul F, Pleydell D, Li T, Han X, Qiu J, et al. Drivers of Echinococcus multilocularis transmission in China: small mammal diversity, landscape or climate? PLoS Negl Trop Dis. 2013;7:e2045. doi: 10.1371/journal.pntd.0002045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Ma J, Wang H, Lin G, Zhao F, Li C, Zhang T, et al. Surveillance of Echinococcus isolates from Qinghai, China. Vet Parasitol. 2015;207:44–48. doi: 10.1016/j.vetpar.2014.11.012. [DOI] [PubMed] [Google Scholar]
- 151.Ma X, Wang H, Han X, Zhang J, Liu Y, Zhao Y, et al. Survey on Echinococcosis in Maqing County of Qinhai Province. Chin J Parasitol Parasit Dis. 2015;33:269–272. [PubMed] [Google Scholar]
- 152.Hou YH, Ma SM, Fan HN, Ren L. The prevalence of liver echinococcosis of pupils in Banma Dari. Qinghai. Mod. Prev. Med. 2016;43:2363–2365. [Google Scholar]
- 153.Cai H, Wang H, Han X, Ma X, Zhang J, Liu X, et al. A survey on echinococcosis in Hainan Tibetan Autonomous Prefecture of Qinghai Province. J Pathog Biol. 2016;11:1022–1025. [Google Scholar]
- 154.Han X, Zhang X, Cai Q, Zhang J, Wang Y, Zhang Q. Epidemic status of alveolar echinococcosis in Tibetan children in south Qinghai Province. Chin J Schisto Control. 2017;29:53–58. doi: 10.16250/j.32.1374.2016235. [DOI] [PubMed] [Google Scholar]
- 155.Niang GCR. 黄南州包虫病流行病学调查报告分析. World Latest Med. Inf. 2017;17:210. [Google Scholar]
- 156.Han XM, Cai QG, Wang W, Wang H, Zhang Q, Wang YS. Childhood suffering: hyper endemic echinococcosis in Qinghai-Tibetan primary school students, China. Infect Dis Poverty. 2018;7:71. doi: 10.1186/s40249-018-0455-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Budke CM, Jiamin Q, Zinsstag J, Qian Q, Torgerson PR. Use of disability adjusted life years in the estimation of the disease burden of echinococcosis for a high endemic region of the Tibetan plateau. Am J Trop Med Hyg. 2004;71:56–64. [PubMed] [Google Scholar]
- 158.Li TY, Qiu JM, Yang W, Craig PS, Chen XW, Xiao N, Ito A, Giraudoux P, Mamuti W, Yu W, Schantz PM. Echinococcosis in Tibetan populations, western Sichuan Province, China. Emerg Infect Dis. 2005;11:1866–1873. doi: 10.3201/eid1112.050079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Yu W, Li D, Chen X, Yang W, Qiu J. Epidemiological survey on human echinococcosis in four counties of Gaizi Tibetan Autonomous Prefecture, Sichuan. Parasit Infect Dis. 2005;3:170–172. [Google Scholar]
- 160.Pengcuo R, Li G, Zong K, Mao Y, Wenxiu S. Human echinococcosis survey using ultrasound B in Shiqu county, Sichuan province. Parasit Infect Dis. 2005;3:92. [Google Scholar]
- 161.Wang Q, Qiu J, Yang W, Schantz PM, Raoul F, Craig PS, et al. Socioeconomic and behavior risk factors of human alveolar echinococcosis in Tibetan communities in Sichuan, People’s Republic of China. Am J Trop Med Hyg. 2006;74:856–862. [PubMed] [Google Scholar]
- 162.Li T, Chen X, Zhen R, Qiu J, Qiu D, Xiao N, Ito A, Wang H, Giraudoux P, Sako Y, Nakao M, Craig PS. Widespread co-endemicity of humancystic and alveolar echinococcosis on the eastern Tibetan Plateau, northwestSichuan/southeast Qinghai, China. Acta Trop. 2010;113:248–256. doi: 10.1016/j.actatropica.2009.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Li NJ, Zhang X, Qiu H. Epidemic Survey echinococcosis for human and livestock in Aba Prefecture of Sichuan Province of year 2008. Chin J Evid-based Med. 2010;10:26–29. [Google Scholar]
- 164.Gao C, Wang J, Shi F, Steverding D, Wang X, Yang Y, et al. Field evaluation of an immunochromatographic test for diagnosis of cystic and alveolar echinococcosis. Parasit Vectors. 2018;11:311. doi: 10.1186/s13071-018-2896-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Wang D, He R, Gongsang Q, Xiao D, Suolang W, Xue L, et al. Prevalence of echinococcosis in Nyingchi City. Chin J Parasitol Parasit Dis. 2018;36:75–79. [Google Scholar]
- 166.Gao Y, Zhu M, Guo Y, Dil M, Wang Y, et al. Clinical analysis on hepatic hydatid disease in Yili River Valley. Chin J Parasitol Parasit Dis. 2005;23:10–13. [PubMed] [Google Scholar]
- 167.Wang GZ, Feng XH, Chu XD, Erxiding A, Zhou JX, et al. Epidemiology study on human echinococcosis in Hobukesar Mongolian Autonomous County of Xinjiang. Chin J Endemiol. 2009;28:214–217. [Google Scholar]
- 168.Li H, Song T, Duan X, Qi X, Feng X, Wang Y, et al. Prevalence of human and ovine hepatic hydatid disease diagnosed by ultrasound in Hobukesar Mongolian Autonomous County of Xinjiang. Chin J Epidemiol. 2013;34:1176–1178. [PubMed] [Google Scholar]
- 169.Ito A, Romig T, Takahashi K. Perspective on control options for Echinococcus multilocularis with particular reference to Japan. Parasitology. 2003;127(Suppl):S159–S172. [PubMed] [Google Scholar]
- 170.Oku Y. Biology of echinococcus. Prog Med Parasitol Jpn. 2003;8:293–318. [Google Scholar]
- 171.Arai S, Suzuki S, Tanaka-Taya K, Ohyama T, Osaka K, Taniguchi K, et al. Evaluation of national surveillance for echinococcosis in Japan, 1999 to 2002. Kansenshogaku Zasshi. 2003;77:957–964. doi: 10.11150/kansenshogakuzasshi1970.77.957. [DOI] [PubMed] [Google Scholar]
- 172.Arai S, Suzuki S, Tanaka-Taya K, Ohyama T, Osaka K, Taniguchi K, et al. Compile and evaluation of national surveillance on human echinococcosis in Japan, 1999 to 2002. Kansenshogaku Zasshi. 2005;79:181–190. doi: 10.11150/kansenshogakuzasshi1970.79.181. [DOI] [PubMed] [Google Scholar]
- 173.Inoue T, Nonaka N, Kanai Y, Iwaki T, Kamiya M, Oku Y. The use of tetracycline in anthelmintic baits to assess baiting rate and drug efficacy against Echinococcus multilocularis in foxes. Vet Parasitol. 2007;150:88–96. doi: 10.1016/j.vetpar.2007.08.027. [DOI] [PubMed] [Google Scholar]
- 174.Taniguchi K, Yoshida M, Sunagawa T, Tada Y, Okabe N. Imported infectious diseases and surveillance in Japan. Travel Med Infect Dis. 2008;6:349–354. doi: 10.1016/j.tmaid.2008.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Baimakhanov BB, Kyzhyrov ZN, Sahipov MM, Bozshagulov TT, Mauleno NB, Birzhanbekov NN, et al. Diagnosis and surgical treatment of focal liver disease. Medicine (Almaty). 2015;8:18–21. [Google Scholar]
- 176.Bodoshova A. Problem of alveococcosus in Kyrgyz Republic. BECTHИК КГMA ИM ИК AXУHБAEBA. 2009;1:145–147. [Google Scholar]
- 177.Jeong JS, Han SY, Kim YH, Sako Y, Yanagida T, Ito A, et al. Serological and molecular characteristics of the first Korean case of Echinococcus multilocularis. Korean J Parasitol. 2013;51:595–597. doi: 10.3347/kjp.2013.51.5.595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Polat KY, Balik AA, Celebi F. Hepatic alveolar echinococcosis: clinical report from an endemic region. Can J Surg. 2002;45:415–419. [PMC free article] [PubMed] [Google Scholar]
- 179.Canda MS, Güray M, Canda T, Astarcioglu H. The pathology of echinococcosis and the current echinococcosis problem in western Turkey (A Report of Pathologic Features in 80 Cases) Turk J Med Sci. 2003;33:369–374. [Google Scholar]
- 180.Kılınç N, Uzunlar A, Özaydın M. Uncommonly localized cases of Echinococcosis (Report of 45 cases) Türkiye Ekopatoloji Dergisi. 2003;9:25–30. [Google Scholar]
- 181.Gündoğdu C, Arslan R, Arslan MO, Gicik Y. Evaluation of cystic and alveolar echinococcosis cases in people in Erzurum and surrounding cities. Turkiye Parazitol Derg. 2005;29:163–166. [PubMed] [Google Scholar]
- 182.Altintas N. Parasitic zoonotic diseases in Turkey. Vet Ital. 2008;44:633–646. [PubMed] [Google Scholar]
- 183.Auer H. Die Bedeutung laboratoriumsdiagnostischer Untersuchungen für die Klinik, die Epidemiologie und Prävention der alveolären Echinokokkose—Erfahrungen zweier Jahrzehnte in Österreich. Wien Klin Wochenschr. 2006;118:18–26. doi: 10.1007/s00508-006-0673-3. [DOI] [PubMed] [Google Scholar]
- 184.Cambier A, Giot JB, Leonard P, Bletard N, Meunier P, Hustinx R, et al. Multidisciplinary management of alveolar echinococcosis : Echino-Liege Working Group. Rev Med Liege. 2018;73:135–142. [PubMed] [Google Scholar]
- 185.Bresson-Hadni S, Vuitton DA. Echinococcosis. Rev Prat. 2001;51:2091–2098. [PubMed] [Google Scholar]
- 186.Piarroux M, Bresson-Hadni S, Capek I, Knapp J, Watelet J, Dumortier J, et al. Surveillance de l’échinococcose alvéolaire en France: bilan de cinq années d’enregistrement, 2001–2005. Numéro thématique. Les zoonoses en France. Bull Epidemiol Hebd. 2006;2728:206–208. [Google Scholar]
- 187.Piarroux M, Piarroux R, Giorgi R, Knapp J, Bardonnet K, Sudre B, et al. Clinical features and evolution of alveolar echinococcosis in France from 1982 to 2007: results of a survey in 387 patients. J Hepatol. 2011;55:1025–1033. doi: 10.1016/j.jhep.2011.02.018. [DOI] [PubMed] [Google Scholar]
- 188.Piarroux M, Piarroux R, Knapp J, Bardonnet K, Dumortier J, Watelet J, et al. Populations at risk for alveolar echinococcosis, France. Emerg Infect Dis. 2013;19:721–728. doi: 10.3201/eid1905.120867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Kern P. Epidemiologie der Fuchsbandwurmerkrankungen in Deutschland—Daten des Echinokokkose Registers. Epidemiol Bull. 2006;2006:115–120. [Google Scholar]
- 190.Jorgensen P, van der Heiden M, Kern P, Schöneberg I, Krause G, Alpers K. Underreporting of human alveolar echinococcosis. Germany. Emerg Infect Dis. 2008;14:935–937. doi: 10.3201/eid1406.071173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Grüner B, Kern P, Mayer B, Gräter T, Hillenbrand A, Barth TEF, et al. Comprehensive diagnosis and treatment of alveolar echinococcosis: a single-center, long-term observational study of patients in Germany. GMS Infect Dis. 2017;5:1–12. doi: 10.3205/id000027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Horváth A, Patonay A, Bánhegyi D, Szlávik J, Balázs G, Görög D, et al. The first case of human alveolar echinococcosis in Hungary. Orv Hetil. 2008;149:795–799. doi: 10.1556/OH.2008.28281. [DOI] [PubMed] [Google Scholar]
- 193.Bruzinskaite R, Marcinkute A, Strupas K, Sokolovas V, Deplazes P, Mathis A, et al. Alveolar echinococcosis, Lithuania. Emerg Infect Dis. 2007;13:1618–1619. doi: 10.3201/eid1310.061161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Strupas K, Sokolovas V, Brimas G, Paškonis M, Jurgaitis J, Valantinas J, et al. Echinokokozė. Lietuvos echinokokozės registro pirmieji duomenys. Lietuvos chirurgija. 2007;5:119–129. [Google Scholar]
- 195.Stefaniak J. Alveococcosis of the Liver. Med po Dypl. 2002;11:236–243. [Google Scholar]
- 196.Stefaniak J. Alveolar echinococcosis due to Echinococcus multilocularis as a common cause of diagnostic mistakes in differential diagnosis of the liver cancer. Pol Arch Med Wewn. 2006;116:896–902. [PubMed] [Google Scholar]
- 197.Stefaniak J. Guidelines for diagnosis and treatment of liver alveococcosis caused by Echinococcus multilocularis. Wiad Parazytol. 2007;53:189–194. [PubMed] [Google Scholar]
- 198.Taxy JB, Gibson WE, Kaufman MW. Echinococcosis: unexpected occurrence and the diagnostic contribution of routine histopathology. Am J Surg Pathol. 2017;41:94–100. doi: 10.1097/PAS.0000000000000742. [DOI] [PubMed] [Google Scholar]
- 199.Czarkowski MP, Gołąb E. Invasive tapeworm infections in Poland in 2011. Przegl Epidemiol. 2013;67(263–6):365–367. [PubMed] [Google Scholar]
- 200.Gołąb E, Czarkowski MP. Echinococcosis and cysticercosis in Poland in 2012. Przegl Epidemiol. 2014;68(279–82):379–381. [PubMed] [Google Scholar]
- 201.Kinčeková J, Pavlínová J, Dubinský P, Bober J, Vrzgula A, Zachar M. Occurrence of echinococcosis and its clinical symptoms in humans—current status in Slovakia. Slovenský Veterinársky Časopis. 2008;33:170–172. [Google Scholar]
- 202.Antolová D, Miterpáková M, Škútová M, Szilágyiová M, Hudáčková D. Echinococcus multilocularis na Slovensku—aktuálna situácia. Infovet. 2014;21:245–249. [Google Scholar]
- 203.Gottstein B, Saucy F, Deplazes P, Reichen J, Demierre G, Busato A, et al. Is high prevalence of Echinococcus multilocularis in wild and domestic animals associated with disease incidence in humans? Emerg Infect Dis. 2001;7:408–412. doi: 10.3201/eid0703.010307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Kadry Z, Renner EC, Bachmann LM, Attigah N, Renner EL, Ammann RW, et al. Evaluation of treatment and long-term follow-up in patients with hepatic alveolar echinococcosis. Br J Surg. 2005;92:1110–1116. doi: 10.1002/bjs.4998. [DOI] [PubMed] [Google Scholar]