Abstract
Objective:
The massive increase in COVID-19 cases led to the implementation of nationwide lockdown in Turkey. While enforced lockdown is an effective strategy to abate the transmission of the virus, it causes significant lifestyle changes in every part of the community. This study aims to assess the changes in eating habits, sleeping behaviour and physical activity status of final-year medical students (interns) whose education was suspended during the pandemic.
Design:
In this cross-sectional epidemiological study, an online questionnaire was created. Interns were asked questions regarding socio-demographic status, eating habits, sleeping behaviour and physical activity status before and during COVID-19 pandemic. Changes in dietary habits and sleep quality were evaluated under the guidance of Turkey Dietary Guidelines, Determination of Nutritional Status Report, Turkey National Nutrition and Health Survey and Pittsburgh Sleep Quality Index.
Setting:
Hacettepe University Faculty of Medicine – Ankara, Turkey.
Participants:
Among 536 students, a total of 340 students (63·4 %) answered the questionnaire.
Results:
After the beginning of lockdown, an increase in BMI was observed in both female (P = 0·002) and male students (P = 0·013). Students having healthy dietary habits increased by 18·8 % and unhealthy dietary habits decreased by 3·2 % during lockdown (P < 0·001). Overall, 63·2 % of students reported a decrease in physical activity, and 33·6 % reported a reduction in sleep quality, whereas 38·6 % reported an improvement in sleep quality. There was no significant difference in sleep quality between genders (P = 0·075).
Conclusions:
This study indicated that medical school suspension and enforced lockdown led to significant changes in interns’ eating behaviour, physical activity and sleeping habits.
Keywords: COVID-19, Eating behaviour, Medical students, SARS-CoV-2, Sleeping habits
COVID-19 is a multi-systemic disease caused by a novel type of coronavirus (SARS-CoV-2) which first emerged in December 2019 in Wuhan, China. The disease has become a significant public health problem after the virus’s rapid spread to other continents and WHO declared this infection as a pandemic(1). Until now, about 3 000 000 people have died from disease and it led to a massive global impact on every aspect of daily life(2).
Countries have implemented different strategies according to the decisions of their scientific committees in order to slow down the transmission of the virus. The nationwide lockdown was thought to be one of the most effective strategies against the spread of the virus and it was implemented by most of the countries having a large population(3,4), one of which was Turkey. Although this approach appeared to be successful in reducing the spread of the virus, it has caused significant changes in daily habits and behaviour patterns. The majority of the society who had to spend the pandemic in home isolation changed their eating behaviours and consumed unhealthy food products(5). Besides, the physical activity levels of most of the population considerably reduced after the implementation of lockdown strategies(6). It is predicted that changes in the diet, especially with physical inactivity, may cause important public health problems in the long term(7). The sleeping habit was also severely affected during the period of isolation and people who were experiencing known consequences of lockdown like anxiety and depression suffered more from stress-related sleep disturbances(8,9). Additionally, the massive changes in our daily routines were also associated with alterations of circadian rhythm which reduced sleep quality(10). It is known that sleep pattern is a critical determinant of eating behaviour in humans. Numerous studies indicated that reduced sleep quality adversely affects both physiological and psychological health by causing poor eating habits(11,12).
Healthcare providers are frontline defence against COVID-19, and they are at increased risk of becoming infected compared with the general population due to close contact with COVID-19 positive patients(13). In Turkey, final-year medical students (also called ‘interns’) are seen as an indispensable part of the healthcare system and participate in the execution of daily work routines in hospitals, although they are legally accepted as undergraduate students. After the emergence of the first COVID-19 case in Turkey, the Turkish Ministry of Health and the Turkish Council of Higher Education decided to suspend internship training and switch to online education on 16 March 2020 (14). Although the impact of the pandemic on education and medical proficiency of interns was investigated in detail(15,16), to our knowledge, no studies have been evaluated whether interns experienced any change in their lifestyle during the lockdown.
The present study aimed to investigate the changes in eating habits, sleeping behaviour and physical activity status of interns who continued their medical education under lockdown. For this purpose, a web-based survey was shared with the interns of Hacettepe University and conducted between 8 June 8 and 16 June 2020. This study will provide valuable information about lifestyle modifications of interns during pandemic and contribute to the current literature on COVID-19.
Methods
Study design and selection of target population
This cross-sectional epidemiological study aimed to assess the effects of COVID-19 pandemic on the eating, sleeping behaviour and physical activity level of interns who have continued their online medical education under lockdown. In order to reach all interns during the lockdown, it was decided to create a web-based survey. The survey was conducted between 8 June 2020 and 16 June 2020 on the internet. The main eligibility criterion for participation was that participants should not be graduated from medical school and continued their medical education at the above-mentioned time period. A web-based questionnaire was created by using Google Forms. Google Forms is a free and web-based software for creating surveys and questionnaires which can be easily accessed with all electronic devices having an internet connection. The questionnaire was shared with the target population (n 536) with the help of different social media (Facebook groups) and communication platforms (WhatsApp groups). Via these platforms, the participation in the study was requested and reminded each day during the data collection period. During the sampling process, it was attempted to reach every student in the target population to avoid the selection bias. Consequently, the response rate of the study was calculated as 63·4 % (n 340). When the socio-demographic characteristics of the target population were compared with our sample, it was similar in terms of age and gender.
This study was conducted in the last month of the final year of education of Hacettepe University Faculty of Medicine interns and therefore, the students who participated in this research are now actively fighting against the COVID-19 pandemic as medical doctors in the field.
Methodology of the survey
The ‘pre-COVID-19 period’ was defined as the time period before the suspension of the medical education (16 March 2020) and the time period after this date was accepted as the ‘COVID-19 period’. The questionnaire consisted of three main parts: socio-demographic features and health status, eating habits, and sleep quality.
In the first part of the questionnaire, gender (male/female/others); age ((2020 – the year of birth)); height (in centimetres); weight (pre-COVID-19 and COVID-19 period – in kilograms); marital status; living place (pre-COVID-19 and COVID-19 period); physical activity: physical activity level of the students during the last 3 months and its change during the pandemic based on the statements of the students (the physical activity status was questioned secondarily, the change in the pandemic period and the current average physical activity duration were asked pragmatically, and the findings were evaluated considering the Turkey Physical Activity Guideline)(17); health status according to statements of the students (extremely unhealthy to extremely healthy); body perception (underweight to obese); dietary habits according to statements of the students before and during the pandemic (extremely unhealthy to extremely healthy) were used as variables.
In the second part of the questionnaire, the eating habits of the students were evaluated. The questions about nutrition used in the questionnaire were created by considering the aims of the research, the literature and the recommendations in the Turkey Dietary Guidelines. Classifications in National Nutrition and Health Surveys were used. To evaluate the food frequency and eating habits of interns in pre-COVID-19 and COVID-19 periods, individuals were evaluated according to the recommendations of the Turkey Dietary Guidelines which defined the daily consumption of different food groups and balanced meal routines required for a healthy diet(18). We requested the participants to evaluate their health status based on their eating habits according to above-mentioned guidelines and thus we conducted a self-assessment strategy. Those who consume food in concordance with the recommendations chose the healthy diet option in the questionnaire, and those who did not chose the unhealthy diet option. Based on these guidelines, we also questioned the food frequency, daily meal routines of the participants, and the frequency of eating and food ordering from outside.
The food frequency was assessed considering the Turkey National Nutrition and Health Survey-2019 (TNHS-2019)(19) which is prepared with the recommendations of WHO and European Food Safety Authority to ensure the unity in method can be constituted and comparisons can be made(20–23), and food frequency was assessed considering the Determination of Nutritional Status Report which is an official publication of the Turkish Ministry of Health(24).
To assess the sleep quality in the third part of the questionnaire, The Pittsburgh Sleep Quality Index (PSQI) was used, which was defined by Buyyse et al. (25) in 1988 and shown to provide information about sleep quality and type and severity of sleep disorder in the last 1 month. The index consists of a total of twenty-four questions, nineteen questions are answered by the person him/herself, while five questions are filled by the bed mate of the person. In this study, questions answered by the person him/herself were taken into consideration. However, the questions answered by his/her bed mate were not evaluated, since these answers do not affect the final PSQI score. With nineteen questions answered by the person, seven components such as subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction are evaluated. The total PSQI score is determined by the sum of the scores of the seven components. The score of each component ranges from 0 to 3. The total PSQI score varies between 0 and 21. The sleep quality of those with a total score of 5 or less is considered to be ‘good’ and total score more than 5 is accepted to be ‘poor’. To avoid memory-related bias, interns’ sleep behaviour was assessed only for the COVID-19 period with PSQI, not for the pre-COVID-19 period. However, it was also asked the participants whether their sleep quality improved or reduced during COVID-19 pandemic. Thus, we could obtain information about their sleep quality according to their personal statements. The PSQI was previously adapted to Turkish and its clinical validity and reliability was evaluated on Turkish patients suffering from sleep disturbances(26). Therefore, the Turkish version of the PSQI was used to assess the sleep quality of interns in this study.
Statistical analysis
Descriptive analyses were presented as percentage and frequency tables for categorical variables and as mean-standard deviation or median-minimum/maximum values for numerical variables. Normal distribution of variables was analysed with visual (histograms, probability graphs) and analytical methods (variation coefficient, Kolmogorov–Smirnov, skewness–kurtosis). McNemar test was performed to evaluate the changes in living place, daily meal routines, frequency of eating out and food order from outside between the ‘pre-COVID-19 period’ and the ‘COVID-19 period’. BMI met the parametric test assumptions and difference of means between the ‘pre-COVID-19 period’ and the ‘COVID-19 period’ was compared with paired t test. The effect of gender on PSQI score was analysed with chi-square test. Mann–Whitney U test was used to compare medians among independent parameters with non-normal distribution. The cut-off value for statistical significance was accepted as α: 0·05. Statistical analyses were performed by using the SPSS software version 23. All statistical analyses were performed at least two times by two different authors with the same software, and the same results were obtained after each analysis. Hacettepe University provides free rights of use of SPSS software for its students and faculty members.
Results
Socio-demographic characteristics and anthropometrics measurements of interns
A total of 340 interns accounting for 63·4 % of the target population completed the online questionnaire. Almost 60 % of the participants were composed of females and the mean age was 24·89 (Table 1). In the pre-COVID-19 period, 37 % of the interns were living with their families, whereas more than a twofold increase was observed, and the frequency reached up to 82·6 % during the COVID-19 period (P < 0·001). Body weight and BMI values were compared between the pre-COVID-19 and COVID-19 period and it was found that the mean body weight increased 0·7 (P < 0·001) and the mean BMI increased 0·2 (P < 0·001) compared to the pre-COVID-19 period. When the effect of gender on the mean BMI was examined, 0·2 increase was shown in both males (P = 0·013) and females (P = 0·002). Change in the number of interns categorised in different BMI groups were also evaluated. 0·3 % and 2·4 % decrease in underweight and normal weight group was seen, respectively. In contrast, the frequency of both pre-obese and obese individuals increased 1·5 %, and 1·1 %, respectively, during the COVID-19 period (Table 2).
Table 1.
Socio-demographic characteristics of interns (Ankara, 2020)
| n 340 | Number of interns (n) | Percentage (%) |
|---|---|---|
| Gender | ||
| Female | 203 | 59·7 |
| Male | 131 | 38·5 |
| Other | 6 | 1·8 |
| Age groups | ||
| ≤ 23 | 6 | 1·8 |
| 24 | 163 | 47·9 |
| ≥ 25 | 171 | 50·3 |
| Age (years) | ||
| Mean | 24·89 | |
| sd | 1·975 | |
| Marital status | ||
| Single | 334 | 98·2 |
| Married | 6 | 1·8 |
Table 2.
Living place, body weight and BMI values of interns before and during the COVID-19 (Ankara, 2020)
| n 340 | Pre-COVID-19 | COVID-19 | t | P | ||
|---|---|---|---|---|---|---|
| Living place | n | % | n | % | ||
| Living with family | 126 | 37·1 | 281 | 82·6 | <0·001* | |
| Living without family | 214 | 62·9 | 59 | 17·4 | ||
| Living with home mate(s) | 80 | 23·5 | 18 | 5·3 | ||
| Living in dormitory | 80 | 23·5 | 3 | 0·9 | ||
| Living alone | 48 | 14·1 | 30 | 8·8 | ||
| Other | 6 | 1·8 | 8 | 2·4 | ||
| BMI categories | ||||||
| Underweight (<18·50) | 18 | 5·3 | 17 | 5·0 | ||
| Normal (18·50–24·99) | 245 | 72·1 | 237 | 69·7 | ||
| Pre-obesity (25·00–29·99) | 69 | 20·3 | 74 | 21·8 | ||
| Obesity (≥ 30·00) | 8 | 2·4 | 12 | 3·5 | ||
| Body weight (kg) | ||||||
| Mean | 66·8 | 67·5 | 3·932 | <0·001† | ||
| sd | 14·1 | 14·3 | ||||
| BMI female (n 203) | ||||||
| Mean | 21·6 | 21·8 | 3·173 | 0·002† | ||
| sd | 2·4 | 2·6 | ||||
| BMI male (n 131) | ||||||
| Mean | 24·7 | 24·9 | 2·518 | 0·013† | ||
| sd | 3·5 | 3·5 | ||||
| BMI | ||||||
| Mean | 22·8 | 23·0 | 3·993 | <0·001† | ||
| sd | 3·2 | 3·3 | ||||
McNemar test.
Paired sample t test.
Evaluation of eating habits and physical activity of interns during pandemic
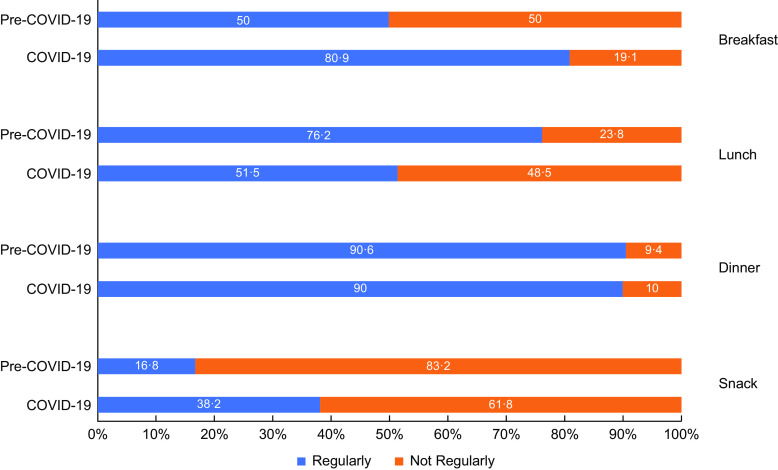
To assess the impact of lockdown on eating habits, interns were first questioned how they described their eating behaviour in the pre-COVID-19 and COVID-19 period. Although only 30 % of interns described their dietary habits as healthy in the pre-COVID-19 period, a significant improvement was seen in COVID-19 period, and this ratio reached 48·8 % (P < 0·001). The food frequency during the pre-COVID-19 and COVID-19 periods was also evaluated (online Supplementary Fig. 1). We observed a considerable change in the food frequency of milk products, eggs, fresh vegetables and fresh fruits during the COVID-19 period. As an essential component of a healthy diet, we examined whether interns had a breakfast, lunch, dinner or snack every day in pre-COVID-19 and COVID-19 period. Although only 50 % of participants reported that they had their breakfast regularly, an increase of more than 30 % was observed in the frequency of interns having breakfast during the COVID-19 period (P < 0·001). Same analyses were also applied to lunch and, an almost 25 % reduction was seen in the frequency of interns having lunch during the COVID-19 period (P < 0·001). In contrast to breakfast and lunch, no significant difference was detected in the number of participants having dinner regularly before and during the COVID-19 period (P = 0·860). Lastly, the snack food consumption frequency of interns was assessed and the frequency of those who eat snacks regularly was 16·8 % in the pre-COVID-19 period, whereas during the COVID-19 period this ratio increased up to 38·2 % (P < 0·001) (Fig. 1).
Fig. 1.
Daily meal routines of interns before and during COVID-19 (Ankara, 2020)
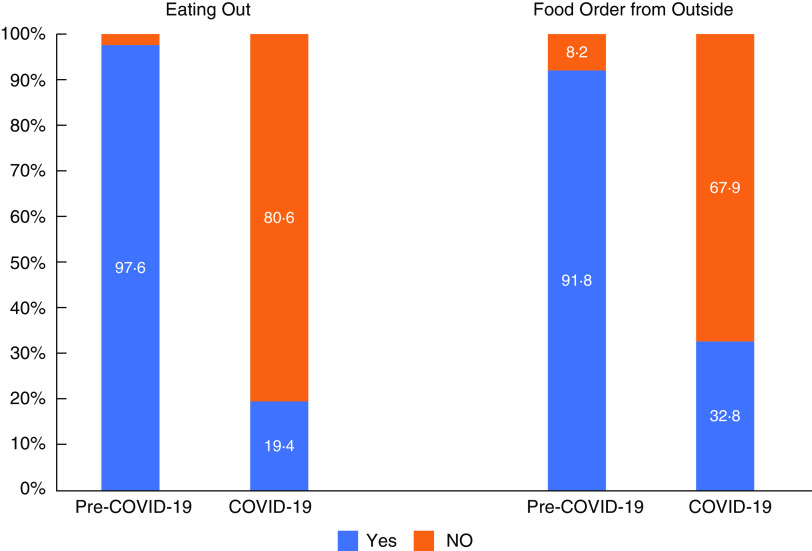
Interns’ interest in eating outside and food order from outside was also evaluated. It was first asked whether they were going out for a meal before and during the COVID-19 period and a reduction from 97·6 % to 19·4 % was observed in the frequency of eating outside (P < 0·001). Similarly, a change in the frequency of food order from outside during COVID-19 period was also assessed and almost 60 % decrease was observed compared to the pre-COVID-19 period (P < 0·001) (Fig. 2).
Fig. 2.
Frequency of eating out and ordering food from the outside before and during COVID-19 (Ankara, 2020)
In addition to alterations in eating habits, notable changes occurred in the period spent for physical activity. 63·2 % of interns stated that their physical activity reduced during COVID-19 period and only 15 % could spend more time to physical activity compared to their previous daily routine. Similar differences were observed in both genders.
Evaluation of sleeping quality of interns during pandemic
Based on the personal statements of the interns, the change in sleep quality during the COVID-19 compared to the pre-COVID-19 period was assessed and it was found that only 27·8 % of the interns observed no change in sleep quality. However, 38·6 % of the interns experienced an improvement and 33·6 % had a reduction in sleep quality. Then, the sleep quality of interns was evaluated with PSQI and 53·4 % of the students were found to have poor sleep quality during the COVID-19 period. The effect of gender on sleep quality was also evaluated and even though female students had a predilection towards poor sleep quality, there was no significant difference between genders (P = 0·075) (Table 3).
Table 3.
Sleep quality of interns according to PSQI score by gender during COVID-19 (Ankara, 2020)
| Female | Male | ||||
|---|---|---|---|---|---|
| Min-max | Median | Min-max | Median | P * | |
| PSQI score (total) | 2–16 | 6 | 0–13 | 5 | 0·065 |
| Comp 1. Sleep quality | 0–3 | 1 | 0–3 | 1 | 0·539 |
| Comp 2. Sleep latency | 0–3 | 1 | 0–3 | 1 | 0·298 |
| Comp 3. Sleep duration | 0–2 | 0 | 0–2 | 0 | 0·106 |
| Comp 4. Habitual sleep efficiency | 0–3 | 0 | 0–3 | 0 | 0·569 |
| Comp 5. Sleep disturbances | 0–3 | 1 | 0–2 | 1 | 0·013 |
| Comp 6. Sleeping medication | 0–3 | 0 | 0–3 | 0 | 0·531 |
| Comp 7. Daytime dysfunction | 0–3 | 2 | 0–3 | 1 | 0·001 |
| Frequency (%) | n | Frequency (%) | n | P † | |
| Good sleep quality (PSQI Score ≤ 5) | 42·6 | 84 | 52·8 | 67 | 0·075 |
| Poor sleep quality (PSQI Score > 5) | 57·4 | 113 | 47·2 | 60 | |
| Total | 100·0 | 197 | 100·0 | 127 | |
Mann–Whitney U test.
Chi-square test. Chi-score: 3·176.
‡PSQI scores of twelve students cannot be calculated due to given misinformation.
Discussion
This cross-sectional study aimed to investigate interns’ lifestyle changes during the medical school suspension due to COVID-19 pandemic. It was first examined whether there was a significant change in weight and BMI of students. In previous studies examining the eating behaviour of population during quarantine, it was commonly observed that people tended to increase their energy intake and gain weight during this period(27). We made almost the same observation and found that both genders gained weight and their mean BMI increased. We found that weight gain and BMI difference between the pre-COVID-19 and COVID-19 period was small in both genders, although it reached statistical significance. It is known that young adults experience high rates of weight gain and this increase is found to be associated with myriad of diseases notably CVD(28,29). Therefore, even small increase in weight and BMI may have serious impact on the health of those in this age group. Despite weight gain, interns surprisingly described their eating habits during lockdown as healthier than the pre-COVID-19 period. The main reason for this finding is that most of the students were living in dormitories or shared flats away from their parents before pandemic and thus tended to consume ready-made products with low nutritional value. As we observed in this study, more than 80 % of the students went back to their hometown due to suspension of internship training, and thus they were able to consume home-made food regularly. The increase in body weight of interns despite healthier food consumption can be explained by the fact that interns educated in Turkey actively participate in various medical procedures during their final year and in contrast to many other countries they also work night shifts which makes internship physically more exhausting. Therefore, reduction in physical activity may lead to weight gain due to loss of daily work routine. As expected, it was found that physical activity level of more than 60 % of students reduced after lockdown.
The notable change in work routine of interns may also affect their daily meal routine. Since they began working early in the morning, almost half of the students did not prefer having breakfast. However, it was shown that after closure of the medical school, most of the students have had their breakfast regularly but preferred skipping lunch instead. As seen similarly in the rest of the population, the habit of eating out and ordering food from outside also decreased significantly due to the nationwide lockdown and fear of becoming infected(30).
Sleep deprivation and reduction in sleep quality are commonly seen during stressful conditions, as was observed during COVID-19 pandemic(31). In this study, however, only one-third of interns experienced sleep deprivation, whereas most of the students felt no change or improvement in sleep quality. Altena et al. (32) proposed that home confinement might result in both positive and negative sleep-related consequences which supports our results. The absence of night shifts and stressful daily work might enable interns to create a better sleeping schedule for their sleep–wake cycle. In addition, after the suspension of practical training and rapid transition to online education, interns were able to find more time to prepare for their final-year exam (Medical Specialty Exam of Turkey) which ameliorates sleep quality due to a substantial reduction in the anxiety of getting low test scores in the exam. In previous studies, female gender was found to be associated with stress, anxiety and poor sleep quality(33,34). Although female students were tended to have poorer sleep quality during lockdown, no significant difference was observed between genders.
Limitation and strength
There are some limitations in our study. At the beginning of the study, target population was determined as the final-year medical students of Hacettepe University, and all inferences about lifestyle modifications were made from this population. However, almost 10 000 medical students graduate from medical schools every year in Turkey and therefore our sample can only represent the interns of Hacettepe University Faculty of Medicine. After the emergence of COVID-19 pandemic, a synchronised online education programme was developed to ensure that all interns could attend their trainings online. For this reason, the online survey was chosen as the data collection method in order to reach the majority of the target population; however, the validity and reliability of interns’ responses to the survey might limit making accurate inferences from the results. To assess the sleep quality of the students, the Turkish version of PSQI was used which had been previously shown to be clinically valid and reliable(26). To assess the food frequency of the students, a FFQ was created. Within this study, the validity of this questionnaire compared with dietary records or recalls has not been examined. However, this questionnaire has already been used and supported by various national nutrition surveys and reports like TNHS-2019(19) and Determination of Nutritional Status Report(24). The strength of the study is that this work was carried out when the interns continued their final-year medical education online and before their return of practical training in the hospital.
Conclusions
Interns are an important part of the healthcare system in Turkey. Since they are undergraduate students, their education was suspended after the emergence of COVID-19 pandemic and their practice-based trainings in hospitals were seriously disrupted. In this study, it was found that not only education but also their eating habits, physical activity level and sleeping behaviour changed significantly during pandemic. These changes showed slight differences compared to general population as it was observed that most of the students started to eat healthier and a significant part of the students noticed an improvement in sleep quality. To our knowledge, this is the first study investigating the lifestyle changes of interns during the COVID-19 pandemic and further studies will help us better understand the effects of the pandemic on the daily habits of interns.
Acknowledgements
Acknowledgements: None. Financial support: None. Conflict of interest: There are no conflicts of interest. Authorship: T. A. B. B. was involved in the study’s design, collected the data, carried out statistical analysis, interpreted the results and critically reviewed the study. A. K., E. S., G. G. and H. B. T. were involved in the study’s design, collected the data and drafted the manuscript. E. Ö. was involved in the study’s design, collected the data, carried out statistical analysis, interpreted the results and critically reviewed the study. S. U. was involved in the study’s design, collected the data and critically reviewed the study. All authors read and approved the final version of this manuscript. This study was not submitted or published elsewhere. Ethics of human subject participation: This study was conducted according to the guidelines laid down in the Declaration of Helsinki. All procedures involving research study participants were approved by the Deanery of Hacettepe University Faculty of Medicine (2020/737) and executed according to the ethical regulations of Hacettepe University. Written informed consent was obtained from all subjects/patients.
Supplementary material
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/S1368980021003906.
click here to view supplementary material
References
- 1. World Health Organization (2020) WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19. Geneva: WHO. [Google Scholar]
- 2. World Health Organization (2020) WHO Coronavirus Disease (COVID-19) Dashboard. Geneva: WHO.
- 3. Lau H, Khosrawipour V, Kocbach P et al. (2020) The positive impact of lockdown in Wuhan on containing the COVID-19 outbreak in China. J Travel Med 27, taaa037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Pachetti M, Marini B, Giudici F et al. (2020) Impact of lockdown on Covid-19 case fatality rate and viral mutations spread in 7 countries in Europe and North America. J Transl Med 18, 338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ammar A, Brach M, Trabelsi K et al. (2020) Effects of COVID-19 home confinement on eating behaviour and physical activity: results of the ECLB-COVID19 International Online Survey. Nutrients 12, 1583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Polero P, Rebollo-Seco C, Adsuar JC et al. (2020) Physical activity recommendations during COVID-19: narrative review. Int J Environ Res Public Health 18, 65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Butler MJ & Barrientos RM (2020) The impact of nutrition on COVID-19 susceptibility and long-term consequences. Brain Behav Immun 87, 53–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Stanton R, To QG, Khalesi S et al. (2020) Depression, anxiety and stress during COVID-19: associations with changes in physical activity, sleep, tobacco and alcohol use in Australian adults. Int J Environ Res Public Health 17, 4065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Cellini N, Canale N, Mioni G et al. (2020) Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J Sleep Res 29, e13074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Morin CM, Carrier J, Bastien C et al. (2020) Sleep and circadian rhythm in response to the COVID-19 pandemic. Can J Public Health 111, 654–657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Shoff S, Nuss E, Horacek T et al. (2009) Sleep quality is associated with eating behavior in 18–24 year old college students. J Nutr Educ Behav 41, S8–S9. [Google Scholar]
- 12. Chaput J-P (2014) Sleep patterns, diet quality and energy balance. Physiol Behav 134, 86–91 [DOI] [PubMed] [Google Scholar]
- 13. Nguyen LH, Drew DA, Graham MS et al. (2020) Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet Public Health 5, e475–e483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. The Council of Higher Education (2020) Coronavirus (COVID-19) Information Note: 1. https://covid19.yok.gov.tr/Documents/alinan-kararlar/02-coronavirus-bilgilendirme-notu-1.pdf (accessed September 2020).
- 15. Choi B, Jegatheeswaran L, Minocha A et al. (2020) The impact of the COVID-19 pandemic on final year medical students in the United Kingdom: a national survey. BMC Med Educ 20, 206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Çalışkan F, Mıdık Ö, Baykan Z et al. (2020) The knowledge level and perceptions toward COVID-19 among Turkish final year medical students. Postgrad Med 132, 764–772. [DOI] [PubMed] [Google Scholar]
- 17. Turkish Ministry of Health (2019) Turkey Physical Activity Guideline. 940. https://hsgm.saglik.gov.tr/depo/birimler/saglikli-beslenme-hareketli-hayat-db/Fiziksel_Aktivite_Rehberi/Turkiye_Fiziksel_Aktivite_Rehberi.pdf (accessed September 2020).
- 18. Turkish Ministry of Health (2016) Turkey Dietary Guidelines. 1046. https://dosyasb.saglik.gov.tr/Eklenti/10922,17ocaktuberingilizcepdf.pdf?0 (accessed September 2020). [Google Scholar]
- 19. Turkish Ministry of Health (2019) Turkey National Nutrition and Health Survey 2019. 1132. https://hsgm.saglik.gov.tr/depo/birimler/saglikli-beslenme-hareketli-hayat-db/Yayinlar/kitaplar/TBSA_RAPOR_KITAP_20.08.pdf (accessed July 2020). [Google Scholar]
- 20. European Food Safety Authority (2009) General principles for the collection of national food consumption data in the view of a pan-European dietary survey. EFSA J 7, 1435. [Google Scholar]
- 21. European Food Safety Authority (2011) Use of the EFSA comprehensive European food consumption database in exposure assessment. EFSA J 9, 2097. [Google Scholar]
- 22. European Food Safety Authority (2014) Guidance on the EU Menu methodology. EFSA J 12, 3944. [Google Scholar]
- 23. World Health Organization (2014) Noncommunicable Diseases Country Profiles. https://www.euro.who.int/en/health-topics/noncommunicable-diseases/ncd-background-information/noncommunicable-diseases-country-profiles-2014 (accessed July 2021).
- 24. Pekcan G (2008) Determination of Nutritional Status. Ministry of Health Turkey 726. https://sbu.saglik.gov.tr/Ekutuphane/kitaplar/A%2014.pdf (accessed May 2021).
- 25. Buysse DJ, Reynolds CF, Monk TH et al. (1989) The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatr Res 28, 193–213. [DOI] [PubMed] [Google Scholar]
- 26. Ağargün MY, Kara H & Anlar Ö (1996) The validity and reliability of the Pittsburgh sleep quality index. Turk J Psychiatr 7, 107–115. [Google Scholar]
- 27. Zachary Z, Brianna F, Brianna L et al. (2020) Self-quarantine and weight gain related risk factors during the COVID-19 pandemic. Obes Res Clin Pract 14, 210–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Truesdale KP, Stevens J, Lewis CE et al. (2006) Changes in risk factors for CVD by baseline weight status in young adults who maintain or gain weight over 15 years: the CARDIA study. Int J Obes 30, 1397–1407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Wing RR, Tate D, Espeland M et al. (2013) Weight gain prevention in young adults: design of the study of novel approaches to weight gain prevention (SNAP) randomized controlled trial. BMC Public Health 13, 300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Deloitte (2020) State of the Consumer Tracker. https://www2.deloitte.com/global/en/insights/industry/retail-distribution/consumer-behavior-trends-state-of-the-consumer-tracker.html# (accessed September 2020).
- 31. Gupta R, Grover S, Basu A et al. (2020) Changes in sleep pattern and sleep quality during COVID-19 lockdown. Indian J Psychiatr 62, 370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Altena E, Baglioni C, Espie CA et al. (2020) Dealing with sleep problems during home confinement due to the COVID-19 outbreak: practical recommendations from a task force of the European CBT-I Academy. J Sleep Res 29, e13052. [DOI] [PubMed] [Google Scholar]
- 33. Mazza C, Ricci E, Biondi S et al. (2020) A nationwide survey of psychological distress among Italian people during the COVID-19 Pandemic: immediate psychological responses and associated factors. Int J Environ Res Public Health 17, 3165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Jahrami H, BaHammam AS & AlGahtani H et al. (2020) The examination of sleep quality for frontline healthcare workers during the outbreak of COVID-19. Sleep Breath 25, 503–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/S1368980021003906.
click here to view supplementary material