Abstract
Objectives
To explore if consumer interest in digital health products (DHPs), changed following the COVID-19 pandemic and the lockdown measures that ensued.
Design
Retrospective time-series analysis of web-based internet searches for DHPs in the UK, split over two periods, pre-COVID-19 lockdown (January 2019–23 March 2020) and post-COVID-19 lockdown (24 March 2020–31 December 2020).
Setting
The UK.
Participants
Members of the UK general population using health-app libraries provided by the Organisation for the Review of Care and Health Applications.
Primary and secondary outcome measures
The primary outcome was volume of searches for DHPs. Secondary outcomes considered search volumes for 25 different therapeutic areas. Outcomes were assessed for significance using a two-stage Poisson test.
Results
There were 126 640 searches for DHPs over the study period. Searches for DHPs increased by 343% from 2446 per month prior to COVID-19 lockdown measures being introduced to 8996 per month in the period following the first COVID-19 lockdown in the UK. In total, 23/25 (92%) of condition areas experienced a significant increase in searches for DHPs, with the greatest increases occurring in the first 2 months following lockdown. Musculoskeletal conditions (2,036%), allergy (1,253%) and healthy living DHPs (1,051%) experienced the greatest increases in searches compared with pre-lockdown. Increased search volumes for DHPs were sustained in the 9 months following the introduction of lockdown measures, with 21/25 (84%) of condition areas experiencing monthly search volumes at least 50% greater than pre-lockdown levels.
Conclusions
The COVID-19 pandemic has profoundly disrupted the routine delivery of healthcare, making face-to-face interaction difficult, and contributing to unmet clinical needs. This study has demonstrated significant increases in internet searches for DHPs by members of the UK population since COVID-19, signifying an increased interest in this potential therapeutic medium. Future research should clarify whether this increased interest has resulted in increased acceptance and utilisation of these technologies also.
Keywords: COVID-19, telemedicine, primary care
Strengths and limitations of this study.
This study is a first of its kind in using real-world internet search data for digital health products (DHPs), providing novel insights into consumer interest in this novel therapeutic medium.
Segmentation of data into 25 different condition areas has enabled exploration of the interest in digital health (at the condition level) in previously unexplored ways.
The collection of data from members of the UK general public, in significant numbers, allows generalisation beyond this study, suggesting that DHPs may be a valuable tool in the event of further COVID-19 lockdown measures.
A limitation of the study is that searches for DHPs do not always result in downloads and subsequent usage, limiting interpretation in terms of what we believe the observed increase in internet searches for DHPs means in terms of improvements in tangible health outcomes.
Introduction
The traditional model of healthcare delivery is based on providing medical services through systems of hospitals, primary care facilities and outpatient clinics.1 However, the COVID-19 pandemic has profoundly disrupted the routine delivery of physical healthcare, resulting in the widespread deferral of elective, preventive and outpatient appointments by health authorities.2–4 Estimates suggest that as many as 40% of appointments have been cancelled or postponed by patients, as part of efforts to avoid public spaces as much as possible.5 In the USA, ambulatory care visits fell by 60% in the early phase of the pandemic,6 while in the UK alone, an estimated 1.5 million elective admissions and 2.6 million outpatient attendances were forgone as a result of COVID-19.7 While the details of the longer-term impact of this significant change in access to services are unclear, short-term cracks are beginning to emerge. Reduced access to services,8 restrictions on social contact and concerns regarding future employment insecurity have contributed to a significant increase in mental-health sequelae.9 Additionally, we are yet to observe the full impact that disruptions to cancer services may have. Cancer Research UK estimated that 2400 fewer people started treatment for lung cancer in April–December 2020, compared with the same time in 2019.10 Similarly, an estimated 344, 1563 and 342 avoidable deaths are expected to occur in the UK as a result of breast cancer, colorectal cancer and oesophageal cancer, respectively, with an estimated 63 229 years of life lost as a result.11
Given the increasing barriers to both accessing and using a variety of face-to-face health services, the potential for digital health to address at least some of the mounting unmet clinical needs has gained traction during the pandemic. Digital health products (DHPs) have been available for many years now, slowly increasing in popularity across a wide range of health-related applications in almost all sectors of healthcare.12 National bodies, including the National Institute for Health and Care Excellence (NICE), are now providing recommendations and guidelines on both the utilisation and evaluation of DHPs.13 14 These technologies, which are widely accessible and fundamentally flexible, continue to provide an additional means to achieve a continuity of care among those with unmet medical needs.15 With many clinicians now realising the full potential of these digital tools, and becoming more accepting of DHPs as a potential therapeutic option during the COVID-19 pandemic, including not just notifiable medical devices, but also simpler diet and fitness applications, it is uncertain how consumer attitudes, interest and demand for DHPs have changed during this period. Using data from the world’s largest digital health evaluation formulary, provided by the Organisation for the Review of Care and Health Applications (ORCHA),16 with over 10 000 DHPs reviewed to date, the aim of this study is to determine how internet searches for DHPs for various health conditions has changed since COVID-19 lockdown measures were introduced in March 2020 and throughout the pandemic. Furthermore, this study will also explore whether changes in search volumes for DHPs differed by therapeutic area.
Materials and methods
The methodology for this study is a retrospective time-series analysis of real-world internet searches for DHPs within ORCHA’s digital health library, split over two time periods, before and after the initiation of COVID-19 lockdown procedures in the UK, which commenced on 23 March 2020. For the purpose of this analysis, DHPs were defined as health apps, including all health apps with the potential to improve health outcomes, not limited to medical devices, but also including diet and fitness health apps. Our aim was to determine if searches for DHPs changed following the first phase of lockdown, and throughout the pandemic. Additionally, the study aims to explore whether changes in search volumes for DHPs differed by therapeutic area.
ORCHA are the world’s largest independent reviewer of DHPs, providing a repository of DHPs, evaluated using a ~350 point objective ‘yes’ or ‘no’ scale. These questions take into account a variety of factors, including user experience and usability, clinical assurance and evidence of effectiveness, clinical safety, and data privacy.16 To date more than 10 000 DHPs have been reviewed and included on ORCHA’s ‘app-finder’ website. During the period of analysis, ORCHA health-app libraries were procured by councils, NHS trusts, clinical commissioning groups and integrated care systems in approximately 70% of NHS regions, providing the ORCHA health-app library free to use, to healthcare providers and members of the public alike. Additionally, during this time period, anyone in the UK could access the ORCHA health-app library free of charge by simply typing ORCHA into their chosen search engine. For the purpose of this study, user’s digital health search term data, used across all ORCHA digital health libraries from 1 January 2019 to 31 December 2020, were collected using Google Analytics. We removed 2486 searches which were exclusively alphanumeric, clear typos, or which consisted of just two letters or less. Following this process, there were 126 640 web searches for DHPs within the study period, equal to approximately 5276 searches per month. From this group of 126 640 searches, we identified every unique search term, determining the frequency of use for each over the study period. In order to explore the different types of DHPs searched for, search terms were subsequently attributed to one of 25 condition areas. These condition areas were identified following multidisciplinary input from three healthcare professionals (a midwife, a pharmacy specialist lead and an ophthalmologist) and a health economist, with the aim of covering a broad representation of functions and conditions throughout the human body. An iterative process was used where each contributor added to (or recommended removing conditions) from the contribution of the last. Once all contributors had the opportunity to recommend therapeutic areas for inclusion, a final discussion between all four contributors took place, at which point the condition areas were finalised. We developed an expansive list of search terms attributable to each of the 25 condition areas, using both MESH headings and condition-specific terms (such as insulin in the case of diabetes, or inhalers for asthma) following methodological guidance for the purpose of literature reviewing. Each of the four contributors then provided independent iterative curation of the search terms, creating a quality control chain. In the event that search terms were missed, they were added and synonyms provided. The search strings used to tag and classify the unique search terms into each of the 25 condition areas are provided in online supplemental file 1.
bmjopen-2021-053891supp001.pdf (1.6MB, pdf)
Remaining terms which had not been initially attributed to one of the 25 condition areas were then attributed using an iterative two-phase tagging approach. First, we used data from the digital health libraries to identify the names of DHPs associated with each of the 25 condition areas. We used a list of the names of the most commonly searched DHPs for each condition, which were then also added to the relevant search strings. This was supplemented by asking a team of several digital health assessors to provide the names of any DHPs they could recall for each of the 25 condition areas. While most DHPs tended to include the name of the condition within the name of the DHP, and, therefore, would have been automatically attributed to a condition, this method was particularly useful for DHPs with names that did not obviously link to a condition area, such as Wysa in the case of mental health, or Xploro for oncology. Following this process, search terms which had not already been attributed to a condition area (untagged) were ordered from the most to least searched (frequency of searches) and reviewed by two independent researchers. Researchers manually descended the list of terms, and in the event, terms were related to one of the 25 condition areas; they were added to the pre-existing search strings. Due to the gamma distribution of search term frequency (non-negative with a significant positive skew), reviewers stopped classifying search terms for any term with less than 10 searches over the 2-year period of investigation. This figure was the cut-off for classification as it was at this point that clear typos and alphanumeric searches which could not clearly be linked to either condition areas with any certainty were most common.
Statistical analysis
Given the differential time periods for data collection and analysis (~15 months before lockdown measures were introduced in the UK on 23 March 2020, and ~9 months after), search frequencies were standardised by determining the mean number of searches per calendar month. The overall change in search frequency (and for DHPs associated with each of the 25 condition areas), between the two time periods under consideration, was determined by comparing the mean frequency of searches (per month) before and after 23 March 2020 (COVID-19 lockdown). A two-sample Poisson test was used to identify if any changes in the volume of web searches for DHPs, both overall, and by condition area, were statistically significant at the conventional 95% level. Data cleaning was performed using Microsoft Office Excel 2013 (Microsoft, Redmond, Washington, DC, USA), with all statistical analyses conducted using Stata V.14.
Patient and public involvement
For this retrospective study of real-world DHP search patterns, formal patient and public involvement was not sought.
Results
Searches for DHPs
In the period prior to COVID-lockdown measures being introduced (1 January 2019–23 March 2020), 36 685 searches for DHPs were undertaken using ORCHA digital health libraries, equivalent to 2446 per month. As detailed in table 1, DHPs dedicated to mental health, diabetes and healthy living were the most frequently searched for during this period. In the period following the introduction of lockdown measures (24 March 2020 onwards), a total of 89 955 searches for DHPs took place, equivalent to 8996 per month, a 343.4% increase on the previous period (p<0.0001).
Table 1.
Comparison of search frequency pre-COVID-19 and post-Covid-19 lockdown measures, by condition area
| Category | Searches per month pre-lockdown* (mean) | Searches per month post-lockdown† (mean) | Increase (%) | Significance‡ |
| COVID | 4 | 197 | 4622.4 | p<0.01 |
| Musculoskeletal and physiotherapy | 34 | 683 | 2035.5 | p<0.01 |
| Allergy | 4 | 45 | 1253.1 | p<0.01 |
| Fitness, diet and weight loss | 320 | 1663 | 1050.8 | p<0.01 |
| Gastroenterology | 12 | 92 | 767.6 | p<0.01 |
| Ears and hearing | 22 | 152 | 700.0 | p<0.01 |
| Kidney | 4 | 27 | 632.3 | p<0.01 |
| Children’s health | 34 | 211 | 613.6 | p<0.01 |
| Neurological and neurodevelopmental | 119 | 698 | 588.3 | p<0.01 |
| Cancer | 22 | 131 | 581.1 | p<0.01 |
| Women’s health | 27 | 158 | 576.5 | p<0.01 |
| Respiratory | 78 | 398 | 510.4 | p<0.01 |
| Men’s health | 4 | 18 | 487.9 | p<0.01 |
| Heart | 31 | 131 | 422.9 | p<0.01 |
| Dental | 3 | 13 | 399.3 | p<0.01 |
| Pain and chronic fatigue | 49 | 191 | 389.6 | p<0.01 |
| Nose and throat | 1 | 5 | 363.6 | p<0.01 |
| Mental health | 723 | 2536 | 350.7 | p<0.01 |
| Pregnancy | 48 | 161 | 338.2 | p<0.01 |
| Eyes and vision | 11 | 29 | 255.8 | p<0.01 |
| Diabetes | 244 | 589 | 241.8 | p<0.01 |
| Addiction | 136 | 274 | 201.4 | p<0.01 |
| Sleep | 259 | 474 | 183.0 | p<0.01 |
| Guidance and info | 21 | 16 | 74.3 | p=0.64 |
| Carer | 45 | 28 | 63.2 | p=0.14 |
| Combined | 2256 | 8920 | 395 | N/A |
*Starts from January 2019 to 23 March 2020 (~15 months).
†Starts from 24 March 2020 to the end of December 2020 (~9 months).
‡Significance determined using two-staged Poisson test.
Searches for DHPs by condition area
There was substantial variation in changes in DHP search frequency by condition area (pre-COVID-19 vs post COVID-19 lockdown), as demonstrated in table 1. COVID-19, musculoskeletal (MSK) and physiotherapy, allergy and fitness/diet and weight loss DHPs experienced ~4,622%, ~2,036%, ~1,253% and ~1,051% increases in monthly searches for DHPs following COVID-19 lockdown measures, the largest increases observed. Every condition area, other than carer support and guidance/info, experienced a statistically significant increase in searches for DHPs in the period following COVID-19 lockdown measures.
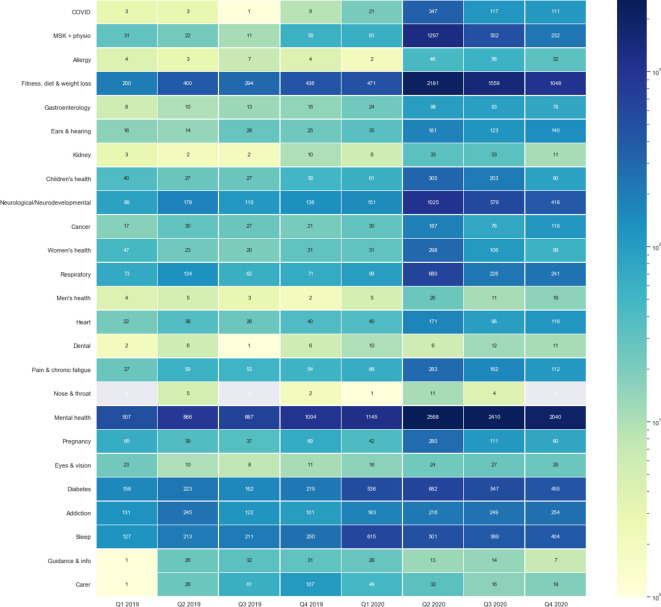
Searches for DHPs by condition area, over time
While the increased frequency of searches for DHPs occurred immediately following the introduction of lockdown proceedings, as demonstrated within figure 1, the interest in DHPs in different condition areas was sustained over the 9-month period following COVID-19 lockdown measures. In total, 23/25 (92%) of the condition areas analysed experienced monthly search volumes at least 25% greater than pre-lockdown levels, 21/25 (84%) had monthly search volumes at least 50% greater than pre-lockdown levels and 14/25 (56%) experienced search volumes more than 100% greater than pre-lockdown levels.
Figure 1.
How interest in digital health changed throughout the COVID-19 pandemic?
Discussion
Principal findings
The study provides a first-of-its-kind exploration of the impact of COVID-19, and the ensuing difficulties in accessing face-to-face care, on consumer interest for DHPs under real-world conditions. Using 2 years of retrospective data (January 2019–December 2020) from the world’s largest formulary of DHPs, available to healthcare providers and members of the public in the UK, we observed a significant increase in searches for DHPs. Searches for DHPs increased by 343% from an average 2446 per month prior to COVID-19 lockdown measures being introduced to an average 8996 per month in the 9-month period following the first COVID-19 lockdown. Despite observing a statistically significant increase in searches for DHPs for all but two of the 25 condition areas listed, increases in searches varied substantially by condition area, with MSK and physiotherapy (2,036%), allergy (1,253%) and fitness, diet and weight loss (1,051%) DHPs experiencing the greatest increases in searches. While searches for DHPs should not be considered a perfect proxy for DHP acceptance, downloads and usage, the data presented here suggest that openness to considering DHPs, and at least researching these tools for the purpose of independent condition and health management, increased following COVID-19 lockdowns.
The strengths of this analysis include the fact that the dataset used includes over 125 000 searches for DHPs by members of the public from the UK, over a 2-year period. As such, when increases in searches for DHPs were observed post-COVID-19 lockdown, the likelihood of this being down to random chance is minimised through the extensive periods of analysis and the high frequency of search data, both pre-lockdown and post-lockdown, under consideration. Additionally, segmentation of search data into different condition areas allowed exploration of internet search volumes for digital health technologies in previously unexplored ways. There are, however, several limitations of this analysis, which must also be considered when interpreting the findings. First, this analysis focused exclusively on searches for DHPs. While this in itself is not a limitation, and was the subject of the research question, searches do not always result in downloads and subsequent usage, nor do they signify acceptance of such technologies, or a changing of beliefs towards digital health Therefore, while we can say with relative certainty that interest in DHPs as proxied by internet search volumes, and consideration of their potential usage as therapeutic options increased as a result of COVID-19 lockdown measures, we cannot definitively confirm whether this increased interest generated tangible improvements in health as a result. Second, while every attempt was made to ensure that the conditions under consideration were varied and representative, using an iterative process of healthcare provider and researcher review, it is possible and also likely that both important and prevalent conditions may not have been addressed by the analysis. This may affect the findings by underestimating (if web searches for the DHPs increased significantly) or overestimating (if web searches hardly changed) the impact that COVID-19 had on web searches for DHPs. Similarly, although the process used to identify terms to classify DHPs was thorough and multidisciplinary, it is possible that DHPs could have been misclassified or missed altogether. While it is unlikely that key terms were omitted, such as diabetes, cancer, mental health or smoking, it is possible that less obvious names of DHPs were missed, where the name of the DHP has no obvious medical link to the condition under consideration. This may have led to an underestimation of searches for condition-specific DHPs in the periods both pre-COVID-19 and post-COVID-19 lockdown. Finally, as ORCHA libraries are not the only place on the internet to search for health apps, we, therefore, cannot be sure that the findings observed here would be reflected in the wider population, nor can we be certain that the increased interest in searching for DHPs. Additionally, based on the existing study structure, there is no guarantee that the findings observed here will continue to be observed once the COVID-19 pandemic has concluded, something which future research will need to address.
Interpretation in light of other evidence
We found that searches for DHPs increased by 343%, a statistically significant increase from 2446 per month prior to COVID-19 lockdown measures to 8996 per month in the 9 months following the first COVID-19 lockdown. Although this rise may plausibly be attributed to a shift in treatment seeking behaviour for those experiencing denied or delayed access to routine face-to-face appointments with healthcare professionals,17–19 there could be alternative justifications for this observed increase in searches for DHPs. These include, but are not limited to, the widespread increase in acceptance of DHPs over time,20–22 and promotion of this relatively new therapeutic medium by health authorities. Previous studies, including two conducted by the authors of this study,23 24 have shown that recommendations from health authorities to use DHPs, including the NHS and NICE, can significantly enhance acceptance and utilisation. Recently, the UK has experienced a substantial increase in regulative clarity, and with this, recommendations considering potential uses of digital health have increased significantly; these include the recent release of the NHSX digital technology assessment criteria,25 and revisions to NICE evidence standards framework.14 As such, at least some of the increases seen here may have been attributable to latent shifts in attitudes towards digital health, although accelerating them as a result of COVID-19.
Another key finding of this study concerned the impact that lockdown measures may have had, and across different condition areas, as the pandemic progressed. Initially, in the UK, leisure facilities, organised sports and the requirement to stay home, where possible, with the exception of one period of exercise a day, led to individuals going out and taking part in physical activity, whether direct, including organised sports, or indirect, including walking to work, far less than previous. This indirectly may have made physical exercise more ‘attractive’ as an activity, as one of the only permissible reasons to leave home once a day. Therefore, it is to be expected that the need for fitness DHPs increased, as observed within this study. In the first 3 months following the first period of lockdown, internet searches for fitness-related DHPs increased by 2000%. As the pandemic progressed, and people either worked from home more or were furloughed, which for many was a significant adjustment, the UK also observed a significant surge in alcohol consumption,4 with a corresponding increase in internet searches for DHPs centred around addiction, as observed in this study.
What does this mean for clinical practice?
While it is unlikely that a face-to-face health service will ever be completely replaced by a virtual experience of any kind, there are clear signs that the healthcare system as we know it is on the verge of change. As evidenced by the findings of this study, it is clear that people are increasingly willing to consider digital health when contemplating seeking treatment for a variety of health conditions. DHPs offer the ability to gather more accurate timely information for healthcare appointments, allow advice to be reinforced and provide new convenient ways to connect with healthcare advice or professionals. Given the potential for a third wave of COVID-19 restrictions in light of new variants, and increased transmissibility, it is, therefore, critical that consumers are directed to safe, trusted and evidence-based solutions, if the demand for such technologies should arise. This is critical such that any benefits which may be realised either in the absence of, or in addition to face-to-face services, are not overshadowed or negated by the potential dangers of using potentially unsafe and unproven technologies. A large part of this process is informing, and enabling healthcare professionals to also recognise this opportunity, to become more actively involved in the provision of high-quality, trusted and safe DHPs for a variety of conditions. This is not limited solely to high functioning medical devices, but also to DHPs with the aim of improving lifestyle decisions and promoting healthy living, with interest in DHPs from both ends of the spectrum increasingly significantly, as observed in this analysis.
Future research
Future research, which empirically explores attitudes towards digital health and the barriers and facilitators to use among members of the public, is likely to be of a significant value for the NHS in realising its long-term goals. This study has provided a basis for a hypothesis that the interest in digital health increased immediately following the introduction of COVID-19 restrictions. These restrictions undoubtedly impacted access to incumbent services and, therefore, the argument may be made that DHPs were sought as an interim or ‘placeholder’ measure in order to fulfil unmet clinical needs. While this is a plausible hypothesis, it does require confirming, while the future role of DHPs beyond the pandemic, as things slowly begin to normalise, also requires exploration. Attention should be paid to the specifics of DHPs and how willingness to use such technologies differs by functionality. It is plausible that members of the public were happy to use DHPs, which had limited functionality in the absence of being able to visit a qualified healthcare professional, but would have concerns about using DHPs classed as medical devices. This ‘classification’ of DHPs, and the different ‘types’ of DHP consumers are willing to use, is a largely unexplored area of research. Unfortunately, this could not be discerned in this analysis and should be addressed, in addition to the other points raised above, before we can determine whether the observed increase in searches for DHPs was a one-time occurrence, or indeed, the start of a new era of digital medicine.
Conclusion
The COVID-19 pandemic has profoundly disrupted the routine delivery of healthcare, contributing to unmet clinical needs and significant increases in related sequelae. Digital health has been posed as one solution to address unmet needs resulting from COVID-19.
This study, which explored real-world interest in DHPs over a 2-year period, has demonstrated significant increases in internet searches for DHPs by members of the UK population since COVID-19, signifying an increased interest in this potential therapeutic medium. Searches for DHPs increased by 343%, with technologies dedicated to mental health and fitness among those experiencing the greatest increases. Future research should clarify whether this increased interest has also resulted in increased acceptance and utilisation of these technologies also.
Supplementary Material
Footnotes
Correction notice: This article has been corrected since it first published. Commas have been swapped with decimal in numerical values.
Contributors: SL, TA and LA-P devised the study. RD led the data collection. LL and CC provided curation of the data. RD, SL and SS planned and conducted the statistical analysis. SL, SS, RD, LL and CC drafted the manuscript. All authors read and approved the final manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
We used the ethical approval decision tool provided by the University of Manchester and following discussion among the scientific steering committee for the study, ethical approval was not sought. The reason being that the study falls under market research using secondary data, which was completely anonymous data, with no confidential, personal or sensitive information and, therefore, no possible risk of disclosures. Additionally, we received explicit consent from the data controller to access and utilise the data, with all users of the Organisation for the Review of Care and Health Applications health-app library also consenting to the use of this data for the purpose of research, as detailed in the privacy policy provided to users.
References
- 1.Senbekov M, Saliev T, Bukeyeva Z, et al. The recent progress and applications of digital technologies in healthcare: a review. Int J Telemed Appl 2020;2020:8830200. 10.1155/2020/8830200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schmid-Küpke NK, Matysiak-Klose D, Siedler A, et al. Cancelled routine vaccination appointments due to COVID-19 pandemic in Germany. Vaccine X 2021;8:100094. 10.1016/j.jvacx.2021.100094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Spalletta G, Porcari DE, Banaj N, et al. Effects of COVID-19 infection control measures on appointment Cancelation in an Italian outpatient memory clinic. Front Psychiatry 2020;11:599844. 10.3389/fpsyt.2020.599844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mansfield KE, Mathur R, Tazare J, et al. Indirect acute effects of the COVID-19 pandemic on physical and mental health in the UK: a population-based study. Lancet Digit Health 2021;3:e217–30. 10.1016/S2589-7500(21)00017-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shayganfard M, Mahdavi F, Haghighi M, et al. Health anxiety predicts postponing or Cancelling routine medical health care appointments among women in perinatal stage during the Covid-19 Lockdown. Int J Environ Res Public Health 2020;17. 10.3390/ijerph17218272. [Epub ahead of print: 09 11 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mehrotra A, Chernew M, Linetsky D, et al. The impact of the COVID-19 pandemic on outpatient care: visits return to Prepandemic levels, but not for all providers and patients. The commonwealth fund 2020. [Google Scholar]
- 7.The British Medical Association . The hidden impact of COVID-19 on patient care in the NHS in England, 2020. Available: https://www.bma.org.uk/media/2841/the-hidden-impact-of-covid_web-pdf.pdf
- 8.The Lancet Infectious Diseases. The intersection of COVID-19 and mental health. Lancet Infect Dis 2020;20:1217. 10.1016/S1473-3099(20)30797-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Holmes EA, O'Connor RC, Perry VH, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry 2020;7:547–60. 10.1016/S2215-0366(20)30168-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cancer Research UK . Lung cancer risks becoming ‘forgotten disease’ of the coronavirus pandemic, 2020. Available: https://www.cancerresearchuk.org/about-us/cancer-news/news-report/2020-09-17-lung-cancer-risks-becoming-forgotten-disease-of-the-coronavirus-pandemic
- 11.Maringe C, Spicer J, Morris M, et al. The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population-based, modelling study. Lancet Oncol 2020;21:1023–34. 10.1016/S1470-2045(20)30388-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gordon WJ, Landman A, Zhang H, et al. Beyond validation: getting health apps into clinical practice. NPJ Digit Med 2020;3:14. 10.1038/s41746-019-0212-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.The National Institute for Health and Care Excellence (NICE) . Evidence standards framework for digital health products. Available: https://www.nice.org.uk/about/what-we-do/our-programmes/evidence-standards-framework-for-digital-health-technologies
- 14.The National Institute for Health and Care Excellence (NICE) . NG183. behaviour change: digital and mobile health interventions, 2020. Available: https://www.nice.org.uk/guidance/ng183/documents/draft-guideline
- 15.Banskota S, Healy M, Goldberg EM. 15 smartphone Apps for older adults to use while in isolation during the COVID-19 pandemic. West J Emerg Med 2020;21:514–25. 10.5811/westjem.2020.4.47372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.ORCHA. Available: www.orchahealth.com
- 17.Iyengar K, Upadhyaya GK, Vaishya R, et al. COVID-19 and applications of smartphone technology in the current pandemic. Diabetes Metab Syndr 2020;14:733–7. 10.1016/j.dsx.2020.05.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vidal-Alaball J, Acosta-Roja R, Pastor Hernández N, et al. Telemedicine in the face of the COVID-19 pandemic. Aten Primaria 2020;52:418–22. 10.1016/j.aprim.2020.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Monaghesh E, Hajizadeh A. The role of telehealth during COVID-19 outbreak: a systematic review based on current evidence. BMC Public Health 2020;20:1193. 10.1186/s12889-020-09301-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Simpson AJ, Honkoop PJ, Kennington E, et al. Perspectives of patients and healthcare professionals on mHealth for asthma self-management. Eur Respir J 2017;49. 10.1183/13993003.01966-2016. [Epub ahead of print: 01 05 2017]. [DOI] [PubMed] [Google Scholar]
- 21.Kong T, Scott MM, Li Y, et al. Physician attitudes towards-and adoption of-mobile health. Digit Health 2020;6:205520762090718. 10.1177/2055207620907187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rowland SP, Fitzgerald JE, Holme T, et al. What is the clinical value of mHealth for patients? NPJ Digit Med 2020;3:4. 10.1038/s41746-019-0206-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Leigh S, Ashall-Payne L, Andrews T. Barriers and facilitators to the adoption of mobile health among health care professionals from the United Kingdom: discrete choice experiment. JMIR Mhealth Uhealth 2020;8:e17704. 10.2196/17704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Leigh S, Ashall-Payne L. The role of health-care providers in mHealth adoption. Lancet Digit Health 2019;1:e58–9. 10.1016/S2589-7500(19)30025-1 [DOI] [PubMed] [Google Scholar]
- 25.NHSX . Digital technology assessment criteria (DTAC). Available: https://www.nhsx.nhs.uk/key-tools-and-info/digital-technology-assessment-criteria-dtac/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-053891supp001.pdf (1.6MB, pdf)
Data Availability Statement
Data are available upon reasonable request.