Abstract
There has been some concern expressed by UK regulator, the Professional Standards Authority regarding the risks arising from Independent sonographer practices. The Professional Standards Authority presented evidence demonstrating that there are instances of harm occurring because of errors made by non-radiologists performing musculoskeletal ultrasound (MSKUS), particularly MSKUS-guided interventions. This document summarises British Society of Skeletal Radiologists position for Musculoskeletal use of ultrasound in UK, representing the agreed consensus of experts from the British Society of Skeletal Radiologists Ultrasound committee. The purpose of this position statement is to review the current practices affecting the delivery of MSKUS. Recommendations are given for education and training, audit and clinical governance, reporting, and medicolegal issues.
Introduction
The purpose of this position statement is to review the current practices affecting the delivery of musculoskeletal ultrasound (MSKUS) in the UK and recommend improvements in training, retention and development of medical personnel involved in the delivery MSKUS services. The role of the practitioner performing ultrasound is highly skilled and requires individuals to exercise a significant degree of autonomy.1 Currently, MSKUS training for Clinical Radiologists, and Sports and Exercise Physicians is delivered as an apprenticeship with theoretical and practical components, setting targets to achieve within an agreed standardised curriculum issued by the Royal College of Radiologists. Training is typically delivered by an experienced consultant radiologist in addition to other practitioners where available.2–6 For non-radiologists, there are other several non-standardised routes for training and education particularly for training sonographers7; where this is delivered as a postgraduate Diploma or Certificate in Medical Ultrasound by Universities accredited by the Consortium for the Accreditation of Sonography Education (CASE).1
There are some concerns regarding the risks arising from Independent sonographer practices, particularly MSKUS-guided interventions, as well as complex MSKUS diagnostic imaging and reporting. Such concerns are linked to training, skills set as well as the setting where non-radiologists are working in, and the vulnerability associated with treating the patient groups that are referred for diagnosis and management.1
In a report to Health Education England (HEE), the Professional Standards Authority presented evidence demonstrating that there are instances of harm occurring because of errors made by non-radiologists performing MSKUS (particularly sonographers) and that the consequences of this can be severe.1 Harms range from psychological distress caused to patients who have received incorrect information or diagnoses, through to serious physical harm.1
BSSR key principles for MSKUS practice
In order to objectively assess the expected standards of MSKUS performed by radiologists, the BSSR collated the key principles for MSKUS practice delivered by radiologists formally in the UK.
Robust RCR-led national curriculum and standardised training, leading to formal certification: a certificate of completion of training (CCT); issued jointly by the RCR and GMC.
Recommendations and means of maintaining and updating skill sets required as a minimum to practice MSKUS independently in the UK. This is overseen by the GMC, which issues the license to practice initially followed by annual appraisals and revalidation every 5 years.
Scanning is provided in an appropriate environment, utilising dedicated scanners and transducers specific to the region imaged.7
Biopsies and interventions are only offered in an appropriate environment following the completion of specific supervised training. Outcomes of procedures are correlated with histological and clinical outcomes (including PROMs: patient reported outcome measures), infection rates, adverse effects and evidence of completion of a modified WHO-check list.
A report will be issued by the scanning practitioner to include the indications, describe the pathology and conclude with a clear, concise diagnosis. The report should address the clinical indications for the study, in addition to management plan recommendations when required. Reports should conform to the appropriate national standards set by the RCR and GMC, and/or adjust international reporting standards to local UK needs and guidelines.
Reports are alerted to the referring teams if there are any urgent findings in line with NHS referral pathways. This alert system should be adhered to strictly, both in NHS and private settings, to include the date, time of the alert, clear documentation and confirmation of receipt from the referring medical personnel.
Familiarity of requirements for further imaging to evaluate the findings need to be robust. Further imaging with other modalities should take place in a timely fashion
Production and storage of adequate representative imaging of each study, accurately and adequately labelled, and issued with a satisfactory report to describe the findings, include a diagnosis in the conclusion with any further recommendations, if necessary.
Professional indemnity: All MSKUS practitioners are required to have formal professional indemnity arrangements as a condition of their statutory registration. Indemnity is agreed and standardised, issued by medical protection groups and NHS trusts.
Access to a unified system for patients to report complaints against professional practices that led to harm. Any complaints, serious incidents or side-effects are documented and eligible for full disclosure and annual review.
Access to effective clinical governance which takes into consideration clinical outcomes to assess the level of harm and make efforts to prevent it, as well as provide a supportive environment for learning, reflection and professional development.
Auditing of ultrasound practice and report quality: Framework for regular MSKUS auditing of practice by colleagues blinded to the reporting radiologist to ensure independent and impartial assessment of the quality of the studies. Attendance of at least four audits/discrepancy meetings a year.1,4
Regulation of practitioners performing MSKUS to incorporate the responsibility for maintaining up-to-date knowledge and skills, engage in MDMs as peer review, supportive environment to enable learning from discrepancies and association to a regulating body to prevent incompetent practitioners from causing further harm.
Standards of equipment: Annual QA reports for all ultrasound machines should be sought and made available for inspection. QA reports to be issued by trained physicists who work in non-ionising radiation safety and affiliated to a recognised institution (ideally a Member of the Institute of Physics and Engineering in Medicine). Regular maintenance contracts to be agreed and made available and maintain standards of machines.8
Access to other imaging modalities already performed with ability to interpretation of these imaging or access to a second opinion for complex cases to provide patients with a safe and relevant report and avoid diagnostic delays.9
Radiologists performing MSKUS are bound by GMC good medical practice, including Continuous professional development.1–3 Consent should be obtained and adhere to re-procedural and post-procedural care principles.1
For CCG and other commissioning bodies, full access to qualifications, appraisal and indemnity documents to enable informed decision-making and ensure standards of service are maintained upon commissioning.
Evidence of current UK practice
National Survey
The BSSR recently conducted a national survey consisting of a questionnaire distributed amongst trainees and newly qualified MSK consultants. The aim was to gauge their views on training opportunities in MSK radiology, including MSKUS. All 19 regions and training schemes were represented.
Training in diagnostic MSKUS was delivered in 88% of schemes, with 71% of schemes providing dedicated interventional MSKUS training.
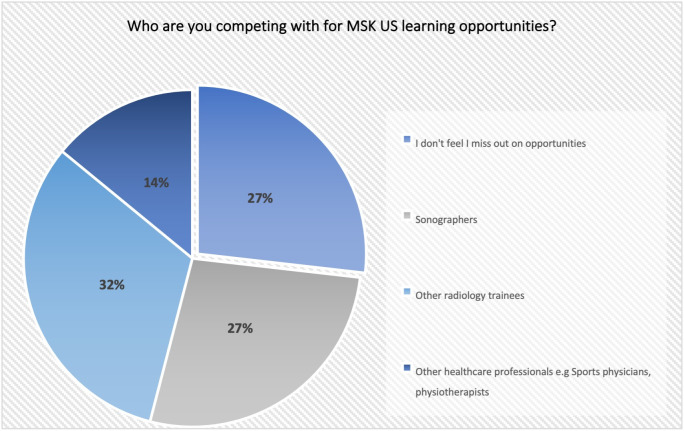
61% of respondents felt that they sometimes missed out on MSK ultrasound training opportunities due to competition from other trainees or other health-care professionals, or by sonographers or from other health-care professionals as core/higher subspecialty trainees (Figure 1).
Figure 1.
Pie chart illustrating detailed responses on the question regarding competition for core training MSK ultrasound learning opportunities. MSK, musculoskeletal
Regarding interdisciplinary training, 20% of respondents reported sonographers and 1.7% reported other health-care professionals playing a secondary role in their daily MSKUS training, whilst 40% of those qualified to train others (Post-CCT and newly qualified consultants) were expected to provide training to sonographers and other healthcare professionals.
The national survey highlighted various factors contributing to high-quality training. and emphasised the BSSR’s concerns with standards of practice by non-radiologists undertaking MSKUS examinations:
Summary of BSSR concerns
Training is not standardised across practitioners. Apart from the FSEM ultrasound curriculum5 – which is approved by the BSSR – there are no national curricula even where PG certificates are issued.
The familiarity of requirements for further imaging to evaluate the findings may not be robust. Further imaging with other modalities may not take place in a timely fashion with possible delays in diagnosis and management.
Formal alert pathways are not consistently followed.1
Non-radiologist MSKUS practitioners performing ultrasound imaging tend to integrate the ultrasound findings in their clinical letters rather than to issue independent reports for ultrasound akin to those issued by radiologists. Images are not stored, and PACs storage is not standard practice for all disciplines.
Images and reports may not be stored in a format available to other clinical teams in the future, for review or comparison, e.g. ultrasound performed in the clinic by a rheumatologist demonstrating a tendon tear may not be available to an orthopaedic surgeon in a year.
Sonography is not recognised as a registered profession by the Health and Care Professions Council.1 Currently, registration is voluntary, and there is no guarantee that the sonography profession will achieve statutory regulation1,10
No obligation for annual MSKUS appraisal and full disclosure of complications by non-doctors.
Regular auditing of practice and report quality is not performed.
Indemnity boundaries and cover are not agreed.
Sonographers performing MSKUS are not bound by GMC good medical practice.
Concerns for self-referrals and lack of peer review.11
Concerns regarding the impact on MSK subspecialty training for Clinical Radiology registrars and young Consultants.
Potential issues Identified
Availability of MSKUS training lists
The ability to attend MSK ultrasound lists regularly with an appropriate trainer (usually an MSK consultant radiologist) is crucial for subspecialty training in MSK. Depending on the hospital setting (e.g. DGH vs teaching hospital), the number of MSK consultants and their working patterns, these ultrasound lists can be a scarce resource. There is, therefore, the definite potential for non-radiologists’ attendance at these lists to compromise the training of radiology subspecialty trainees (senior registrars and fellows). The actual impact this has had has not been studied systematically but seems to vary depending on the region.
Training burden on MSK radiology subspecialty trainees
Particularly in larger hospitals, it is our anecdotal experience that MSK radiology subspecialty trainees who have gained some competence in MSK ultrasound will often “run” the list of a consultant colleague who is nominally attached to it – that is, they will perform the list under indirect supervision. Non-radiologists who are attempting to learn MSKUS may wish to attend these lists. In this case, the training burden could be transferred onto the MSK subspecialty trainee, which may be inappropriate for their career stage and adversely affect their learning.
Responsibility for "checking" MSKUS examinations
There is the sense of an increasing burden of responsibility placed onto radiologists having to check (most of the time static images) MSKUS scans performed by non-radiologists and having their names placed onto the final reports by someone who has been deemed 'competent' to be performing the examination. Where this is somewhat accepted practice for general ultrasound examinations, for more specialised MSK imaging, this seems more of a hazard. This burden is generally felt more by MSK consultants but could also affect senior MSK subspecialty trainees.
General departmental workload
There is concern that with the growing number of specialised ultrasound examinations performed by non-medical practitioners that the quality of diagnostic reports and answering clinical questions in certain instances may be less than adequate. This can result in patients being recalled for repeat examinations or further radiological studies that may not necessarily have been indicated. These issues are amplified when requests are accepted from non-specialist clinicians. While not a training issue per se, increasing departmental workload has the potential to impact training by reducing the amount of time consultants have to allocate to their trainees.
Patient safety, clinical Governance, quality assurance, quality improvement & audit
There are concerns regarding engagement with patient safety and quality assurance processes which are integrated into routine practices of radiologists undertaking ultrasound.
Ultrasound services delivered by FSEM doctors, rheumatologists and orthopaedic surgeons are incorporated into their outcome assessments, peer review, multidisciplinary meetings and revalidation processes. This is not the case for non-doctors who deliver MSKUS services in the NHS as well as in the independent sector.
A Quality assurance programme4 should be defined in a written policy with regular Audit of all policies and procedures. Radiographers/technologists and medical physics staff must be fully involved in this process with appropriate analysis and monitoring of the data obtained
Recommendations for action
MSKUS delivered by radiologists
Should adhere to the BSSR key principles.
Maintain up to date knowledge of RCR, BSSR and NICE guidelines.
Including MSKUS early on in radiology training, to engage and attract high calibre trainees, incentivising them to pursue a career in MSK as a radiology subspecialty.
Develop leadership competencies that enable MSKUS radiologists to create and manage safe patient pathways across complex scenarios (e.g. COVID-19 guidelines).12,13
MSKUS delivered by non-radiologists
Adhere to the BSSR key principles or establish their own within similar frameworks, jointly approved by the RCR.
Developing services and workforce.
There should be equal access to specialist MSKUS services for all UK citizens.
Multidisciplinary working models should be adapted where possible, to utilise skill mix and local expertise whilst ensuring a standardised and highly maintained level of services to all attending patients.3,7,8
Improving registration: MSKUS national register for all procedures, both diagnostic and/or therapeutic. To record all clinical incident data, complications and who performs the studies to be used for appraisal and revalidation.
Provide evidence of good medical practices, including PROMs, clinical outcomes and impact on patient’s presenting symptoms.
Provide evidence for value-based health-care provision, e.g. one-stop-shop, improved outcomes and patient pathways.
Indemnity should be agreed and standardised to all MSKUS providers taking into consideration the level of complexity and knowledge required to deliver services, with track records of each speciality. This should be eligible for annual review and full disclosure of any complaints, serious incidents or side-effects are documented as part of appraisal.
Training and education of MSKUS healthcare providers:
MSKUS education should be clearly defined in the curricula of all healthcare professionals expected to deliver MSKUS services, to encompass the level of background clinical knowledge required.
Clear educational strategies derived to plan both strategy of delivery of this knowledge, methods of evaluating the acquired knowledge as well as resources required for these educational programmes.
MSKUS education is iterative: Basic concepts are introduced in undergraduate training and knowledge and skills are developed through postgraduate training, reinforced by hands-on experience and CPD.
More in-depth learning is needed, both clinical skills and theoretical, relevant to the services delivered. A good example is the training offered to OBGYN and sonographers for obstetric and gynaecological US training in the UK7.
Accreditation
Working closely with regulating bodies and Royal Colleges to standardise the requirement for accreditation.8–11,14
Conclusion
The MSKUS profession has developed significantly over recent years. Many of the duties now undertaken by non-radiologists are tasks that were previously performed by Radiologists. However, the quality of the service that is provided for patients remains paramount. Standardised training, practices and competencies are required to deliver a high-quality MSK ultrasound service.7
Footnotes
Funding: This article presents independent research funded/supported by the National Institute for Health Research (NIHR) Leeds Biomedical Research Centre (BRC).
BSSR Council: BSSR council members who reviewed and approved this document: Dr Philip Robinson (President)Dr Robert Campbell (Vice president)Dr Radhesh Lalam (Secretary)Dr Winston Rennie (Treasurer)Dr Andrew Carne (Executive Officer)Dr Daniel Fascia (Executive Officer)Dr Ramy Mansour (Executive Officer)Dr Emma Rowbotham (Executive Officer)Dr Danoob Dalili (Associate Representative)
Contributor Information
Danoob Dalili, Email: ddalili@gmail.com.
Andrew Carne, Email: andrew.carne@nhs.net.
James MacKay, Email: W.Mackay@uea.ac.uk.
Philip O'Connor, Email: philip.oconnor@nhs.net.
David Silver, Email: davidsilver@nhs.net.
Philip Robinson, Email: philip.robinson10@nhs.net.
Ramy Mansour, Email: ramy.mansour@ouh.nhs.uk.
REFERENCES
- 1.Health Education England HEE. Right-touch assurance for sonographers based on risk of harm arising from practice: report to Health Education England. Professional Standards Authority for Health and Social Care. 2019. Available from: https://www.professionalstandards.org.uk/docs/default-source/publications/policy-advice/right-touch-assurance-for-sonographers-a-report-for-hee.pdf?sfvrsn=9cfd7420_13.
- 2.The Royal College of Radiologists. Focused ultrasound training standards Board of the Faculty of Clinical Radiology. 2012. Available from: https://www.rcr.ac.uk/system/files/publication/field_publication_files/BFCR(12)18_focused_training.pdf.
- 3.Spencer P, Thomson N, Cozens N. Standards for the provision of ultrasound service. The Royal College of Radiologists. 2014. Available from: https://www.rcr.ac.uk/publication/standards-provision-ultrasound-service.
- 4.RCR .Ultrasound training recommendations for medical and surgical specialties. Third edition. London: RCR; 2017. https://www.rcr.ac.uk/publication/ultrasound-training-recommendations-medical-and-surgical-specialties-third-edition. [Google Scholar]
- 5.Training I. FSEM UK MSK Guidelines These Guidelines have been produced in conjunction with The British Society of Skeletal Radiologists (BSSR). May 2019 FSEM UK MSK Guidelines © FSEM UK 2019. 2019. Available from: https://www.fsem.ac.uk/wp-content/uploads/2019/08/FSEM-UK-MSK-US-Guidelines-May-2019.pdf.
- 6.Professions C. Sonographer independent prescribing BMUS position statement... Available from: https://www.bmus.org/policies-statements-guidelines/position-statements/BMUS Position Statement – December 2017
- 7.Clevert DA, Nyhsen C, Ricci P, .European Society of Radiology (ESR) . Position statement and best practice recommendations on the imaging use of ultrasound from the European Society of radiology ultrasound Subcommittee. Insights Imaging 2020; 11: 115. doi: 10.1186/s13244-020-00919-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Team NI NHS improvement: Safe, sustainable and productive staffing for maternity services. 2018. Available from: https://improvement.nhs.uk/documents/1354/Safe_Staffing_Maternity_Appendices_proofed.pdf.
- 9.Provision N, Training I, Accreditation IP. Delivering Cardiovascular Magnetic Resonance In the UK. BSCMR / BSCI guidelines 1. Introduction : CMR in the UK. Including results for delivering Cardiovascular Magnetic Resonance In the UK. BSCMR / BSCI guidelines 1. Introduction : CMR in the UK%0ASearch only for elivering Cardiovascular Magnetic Resonance In the UK. BSCMR / BSCI guidelines 1. Introduction : CM; 2012. [Google Scholar]
- 10.Health Education England HEE. Sonography workforce development briefing note. 2018. Available from: https://healtheducationengland.sharepoint.com/Comms/Digital/Shared Documents/Forms/AllItems.aspx?id=%2FComms%2FDigital%2FShared Documents%2Fhee.nhs.uk documents%2FWebsite files%2FSonography%2FPosition Statement v5.0_FINAL.pdf&parent=.
- 11.Lenthall R, McConachie N, White P, Clifton A, Rowland-Hill C, .UK Neurointerventional Group and British Society of Neuroradiologists . BSNR training guidance for mechanical thrombectomy. Clin Radiol 2017; 72: 175.e11–175.e18. doi: 10.1016/j.crad.2016.11.007 [DOI] [PubMed] [Google Scholar]
- 12.Sharpe RE, Nazarian LN, Parker L, Rao VM, Levin DC. Dramatically increased musculoskeletal ultrasound utilization from 2000 to 2009, especially by podiatrists in private offices. J Am Coll Radiol 2012; 9: 141–6. doi: 10.1016/j.jacr.2011.09.008 [DOI] [PubMed] [Google Scholar]
- 13.Fascia D, Dalili D, Rennie W, Rowbotham E, Carne A, Robinson P. The safety of corticosteroid injections during the COVID-19 pandemic. 2020. recommendations of the British Society of skeletal radiologists. BSSR. [Google Scholar]
- 14.Jenssen C, Gilja O, Serra A, Piscaglia F, Dietrich C, Rudd L, et al. European Federation of societies for ultrasound in medicine and biology (EFSUMB) policy document development strategy – clinical practice guidelines, position statements and technological reviews. Ultrasound Int Open 2019; 5: E2–10. doi: 10.1055/a-0770-3965 [DOI] [PMC free article] [PubMed] [Google Scholar]