1. Main body
Since the early part of December 2019, the entire world is witnessing the challenges of the pandemic of COVID-19 with the Wuhan city, Hubei Province of China being the epicenter of the novel pandemic. By January 2020, India reported the first case of COVID-19 in Kerala through a 20-year-old female returnee from the city of the epicenter. Later in June 2021, the state of Kerala faced the re-emergence of Zika virus outbreak with 65 confirmed cases amid the strict vigilance of COVID-19 protocols (Zika Virus). To continue with the series on September 1, 2021, a 12-year-old boy with fever visited Kerala’s Kozhikode hospital and was confirmed to be a case of Nipah virus (NiV) encephalitis on September 5, 2021 (12-year-old boy dies of Nipah virus in Kerala’s Kozhikode) and succumbed to the illness. Thereby emphasizing the prediction of Priya Joi, published in Gavi (The Vaccine Alliance) entitled “The next pandemic: Nipah virus?” (The next pandemic).
Since the first identification of NiV in Malaysia way back in 1999, till date, more than 260 people have lost their lives worldwide. At the juncture when the state is already struggling with the pandemic of COVID-19 and the outbreak of Zika, the surfacing of Nipah cases would burden the health care system and the resources. Interesting to note that the Kozhikode district of Kerala had already faced the first outbreak of Nipah in May 2018 claiming 17/18 lives (Arunkumar et al., 2018). It was the immediate outbreak response and implementation of effective control measures that helped to cordon the deadliest outbreak within the shortest span and geographical limits. The incidences of two Nipah outbreaks within a defined geographical location would certainly point towards over-incubation of the virus within the reservoir hosts over three calendar years. It would be worth understanding the epidemiologic dynamics of the NiV, its reservoir hosts, the natural habitat, the flora and fauna supporting the reservoir, and the virus inside. However, the work done by Yadav et al., (Yadav et al., 2018) indicated the role of Frugivorous bats (Pteropus medius) be a possible reservoir of infection during the 2018 outbreak of Kozhikode with 13/52 (25%) bats being positive for the Nipah viral RNA. The Siliguri outbreak of Nipah encephalitis was a devastating experience first of its kind in India claiming 45/66 lives (68.1%) in 2001 (Chadha et al., 2006). Also in 2019, a single case of Nipah infection was identified in Ernakulum district of Kerala (Sudeep et al., 2019).
2. Why a major concern
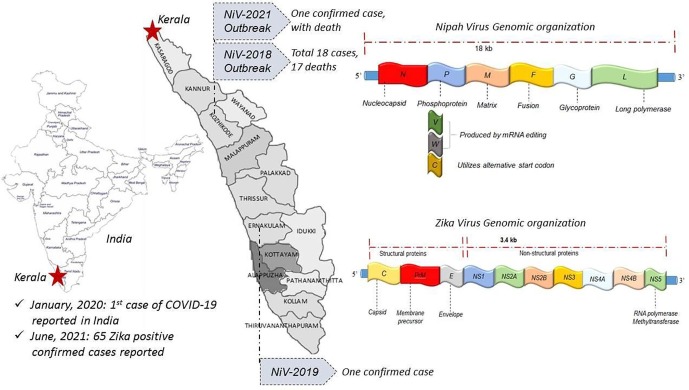
Nipah virus belongs to the group of Biosafety Level-4 pathogen associated with high case fatality rate (40–75%) (Singh et al., 2019), whereas the ongoing pandemic of COVID-19 has 1–2% mortality. NiV is a single-stranded, negative-sense RNA virus of 18.2 kb genome encoded by three non-structural and six structural proteins i.e. nucleo-, phosphor-, matrix-, fusion-, glycol-, and RNA polymerase proteins (Wang et al., 2001) Fig. 1 . Being an emerging zoonotic virus, it gets transmitted from animals to humans. Among humans, the virus spreads through body fluids, respiratory droplets, blood, and urine. Fruit bat (Pteropus medius) is the reservoir host and can spread the infection to pigs and sheep as the first infection was identified in the Nipah village of Malaysia in a pig farm (Chua, 2012).
Fig. 1.
Representative map of Kerala (India) showing Nipah outbreak sites and genomic organization of Nipah virus and Zika virus.
It is responsible for encephalitis and myocarditis involving the brain and heart respectively. Sometimes patients may experience drowsiness and mental confusion, progressing to coma. Residual neurological complications have been encountered in some of the survivors.
3. Containment of 2021 Nipah and lesson learned from previous outbreaks
The experience from the previous Nipah outbreak of 2018 and the current COVID-19 pandemic has taught good lessons towards control measures which have become a boon towards controlling the emergence of the single case of Nipah in 2021. The use of established protocols, contact tracing, restriction in population movement within the infected area, isolation of close contacts, and high-risk exposures effectively possibly have restricted the spread of infection to health care workers and close contacts. The establishment of control rooms, diagnostic and counseling centers further helps towards its control.
In the absence of a specific vaccine, symptomatic treatment is the only option. Recent studies have shown that the HeV-sG vaccine against Hendra virus could protect the African green monkeys against the lethal NiV disease seven days post-immunization (Geisbert et al., 2021). However, preliminary trials by Oxford University and the National Institute of Health (NIH) with Nipah virus glycoprotein infused ChadOx1NiV vaccine vector provide close to complete protective immunity in African green monkeys (Covishield-like vaccine reports success in monkey trials against Nipah virus). This study could be instrumental in the development of a rapid vaccine, as has been observed with the SARS-CoV-2 vaccine developed in the shortest possible time with authorization under emergency use.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
None. The views expressed are personal and not necessarily the views of the author-affiliated institute.
References
- Zika Virus: Zika Virus Latest News, Zika Virus Updates | The Economic Times [Internet]. [cited 2021 Sep 8]. Available from: https://economictimes.indiatimes.com/news/zika-virus.
- 12-year-old boy dies of Nipah virus in Kerala’s Kozhikode - India News [Internet]. [cited 2021 Sep 8]. Available from: https://www.indiatoday.in/india/story/boy-dies-nipah-virus-kerala-kozhikode-1849329-2021-09-05.
- The next pandemic: Nipah virus? | Gavi, the Vaccine Alliance [Internet]. [cited 2021 Sep 8]. Available from: https://www.gavi.org/vaccineswork/next-pandemic/nipah-virus.
- Arunkumar, G., Chandni, R., Mourya, D.T., Singh, S.K., Sadanandan, R., Sudan, P., et al. Outbreak Investigation of Nipah Virus Disease in Kerala, India, 2018. J Infect Dis [Internet]. 2019 May 24 [cited 2021 Sep 8];219(12):1867–78. Available from: https://academic.oup.com/jid/article/219/12/1867/5144922. [DOI] [PubMed]
- Yadav, P.D., Shete, A.M., Kumar, G.A., Sarkale, P., Sahay, R.R., Radhakrishnan, C., et al. Nipah Virus Sequences from Humans and Bats during Nipah Outbreak, Kerala, India, 2018 - Volume 25, Number 5—May 2019 - Emerging Infectious Diseases journal - CDC. Emerg Infect Dis [Internet]. 2019 May 1 [cited 2021 Sep 16];25(5):1003–6. Available from: https://wwwnc.cdc.gov/eid/article/25/5/18-1076_article. [DOI] [PMC free article] [PubMed]
- Chadha M.S., Comer J.A., Lowe L., Rota P.A., Rollin P.E., Bellini W.J., et al. Nipah virus-associated encephalitis outbreak, Siliguri. India. Emerg Infect Dis. 2006;12(2):235–240. doi: 10.3201/eid1202.051247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sudeep, A.B., Yadav, P.D, Gokhale, M.D, Balasubramanian, R., Gupta, N., Shete, A., et al. Detection of Nipah virus in Pteropus medius in 2019 outbreak from Ernakulam district, Kerala, India. BMC Infect Dis 2021 211 [Internet]. 2021 Feb 9 [cited 2021 Sep 16];21(1):1–Available from: https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-021-05865-7. [DOI] [PMC free article] [PubMed]
- Singh R.K., Dhama K., Chakraborty S., Tiwari R., Natesan S., Khandia R., et al. Nipah virus: epidemiology, pathology, immunobiology and advances in diagnosis, vaccine designing and control strategies – a comprehensive review. Vet Q [Internet]. 2019 doi: 10.1080/01652176.2019.1580827. Jan 1 [cited 2021 Sep 8];39(1):26. Available from: /pmc/articles/PMC6830995/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- L. Wang, B.H. Harcourt, M. Yu, A. Tamin, P.A. Rota, W.J. Bellini, B.T. Eaton. Molecular biology of Hendra and Nipah viruses. Microbes Infect [Internet]. 2001 [cited 2021 Sep 14];3(4):279–87. Available from: https://pubmed.ncbi.nlm.nih.gov/11334745/. [DOI] [PubMed]
- K.B. Chua. Introduction: Nipah virus--discovery and origin. Curr Top Microbiol Immunol [Internet]. 2012 [cited 2021 Sep 15];359:1–9. Available from: https://pubmed.ncbi.nlm.nih.gov/22782307/. [DOI] [PubMed]
- Geisbert, T.W., Bobb, K., Borisevich, V., Geisbert, J.B., Agans, K.N., Cross, R.W., et al. A single dose investigational subunit vaccine for human use against Nipah virus and Hendra virus. npj Vaccines 2021 61 [Internet]. 2021 Feb 8 [cited 2021 Sep 8];6(1):1–12. Available from: https://www.nature.com/articles/s41541-021-00284-w. [DOI] [PMC free article] [PubMed]
- Covishield-like vaccine reports success in monkey trials against Nipah virus - The Hindu [Internet]. [cited 2021 Sep 8]. Available from: https://www.thehindu.com/sci-tech/health/covishield-like-vaccine-reports-success-in-monkey-trials-against-nipah/article36322790.ece.