Abstract
Background
Acupuncture treatment of chronic insomnia (CI) was effective. Anxiety and depression symptoms of the CI patients were improved to varying degrees after acupuncture treatment. Corticosterone (CORT) and 5-hydroxytryptamine (5-HT) are involved in the occurrence and development of comorbidity of insomnia, anxiety, and depression. Whether acupuncture can treat insomnia and accompany anxiety and depression symptoms by regulating CORT and 5-HT is still unclear.
Methods
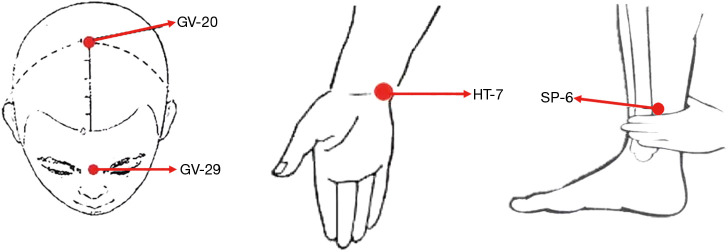
This was a randomized, single-blind (participant), parallel, placebo-controlled trial. Sixty CI patients were randomly divided into acupuncture and sham acupuncture groups, with 30 patients in each group. In the acupuncture group, acupuncture was applied at Baihui (GV20), Yintang (GV29), Shenmen (HT7, bilateral), and Sanyinjiao (SP6, bilateral), while in the sham acupuncture group, superficial needles were used on non-disorder-related acupoints. Both groups were treated 3 times a week (once every other day) for 4 weeks and at the 3-month follow-up. The patients were assessed using the Pittsburgh Sleep Quality Index (PQSI), Hamilton Anxiety Rating Scale (HAMA), and Hamilton Depression Rating Scale (HAMD). The serum concentrations of CORT and 5-HT were also measured before and after treatment.
Results
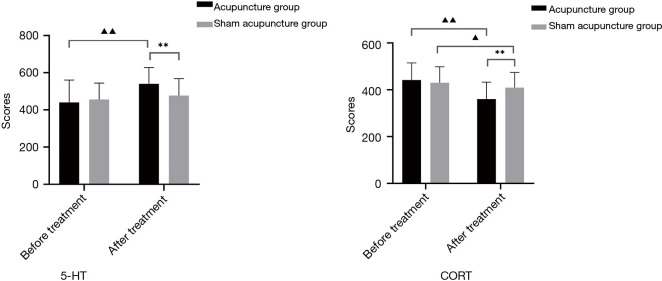
After treatment, the decrease in serum CORT and the increase in serum 5-HT were significantly greater in the acupuncture group than in the sham acupuncture group. At follow-up, the PSQI, HAMA, and HAMD scores in the acupuncture group were significantly lower than those in the sham acupuncture group.
Conclusions
Elevated serum CORT and decreased serum 5-HT levels may be associated with mood regulation disorders in CI patients. Acupuncture can significantly improve the sleep quality, efficiency, and latency of CI patients, and it can alleviate anxiety and depression in such patients. Compared with the sham acupuncture group, the acupuncture group showed a stable long-term efficacy.
Trial Registration
Chinese Clinical Trials Register ChiCTR1800020298.
Keywords: Chronic insomnia (CI), acupuncture, anxiety, depression
Introduction
With the escalating pace of modern society, the mounting pressures of work-life, and inadequate lifestyle practices, the global incidence of CI is increasing, with approximately 10–20% of people worldwide suffering from insomnia (1). Clinically, CI is often accompanied by anxiety and depression symptoms to different degrees. Epidemiological investigation shows that about more than 70% of CI patients with depressive symptoms (2), about 20–30% of CI patients are accompanied by anxiety symptoms (3). Foreign studies have shown that the incidence of comorbid anxiety and depression in CI patients is 18.0 times than that in healthy individuals, while the incidences of anxiety alone and depression alone are 8.8 and 8.4 times than those in healthy individuals, respectively (4). Insomnia is an important risk factor leading to anxiety and depression (5,6), which aggravates the insomnia symptoms of patients. The symptoms of insomnia and anxiety/depression are closely related and can promote and affect each other (7-9). They can seriously affect patients’ prognoses and quality of life (10) and even increase the risk of suicide (11). Therefore, the study of CI cannot be limited to night sleep, and attention should also be paid to anxiety and depression in CI patients.
Acupuncture is an important part of Chinese medicine, and rich experience has been accumulated in its use as a treatment for CI. A large number of studies have shown that acupuncture is safe and effective in the treatment of insomnia, with good long-term efficacy and high patient compliance. It has been widely used in clinical practice (12,13). However, most studies only focus on the clinical efficacy of acupuncture in the treatment of insomnia, and rarely discuss its mechanism. Numerous studies have found that acupuncture can significantly improve sleep and alleviate anxiety and depression symptoms (14). In recent years, the hypothalamic-pituitary-adrenal (HPA) axis, as the central link between CI and pathogenesis of anxiety and depression, has become a research hotspot in the field of sleep medicine. The levels of 5-HT, CORT, and other stress hormones are involved in the occurrence and development of insomnia and comorbidity of anxiety and depression (15). Studies have reported that the serum CORT levels of CI patients with depression are significantly higher than those in healthy individuals, while the levels of 5-HT are significantly lower (16). CORT is an independent risk factor for the occurrence of moderate and severe depression in CI patients. At the same time, 5-HT is a protective factor, which suggests that the clinical detection of 5-HT and CORT levels has important guiding significance for the severity evaluation of CI patients with anxiety and depression (17).
In this study, we aim to explore the therapeutic effects and possible mechanism of acupuncture in CI by comparing the effects of acupuncture and sham acupuncture on the quality, efficiency, and latency of sleep, anxiety, and depression, and serum 5-HT and CORT levels. We present the following article in accordance with the CONSORT reporting checklist (available at https://dx.doi.org/10.21037/atm-21-3845).
Methods
Study design
This was a randomized, single-blind (participant), parallel, placebo-controlled trial performed according to the CONSORT guideline (18). Divided into two groups at ratio 1:1.
Randomization
To achieve the goal of random allocation and group concealment not to disturb the distribution process, this study used a random number table envelope method to hide the grouping. It is the simple randomisation method. Briefly, random numbers generated by SPSS22.0 software were written onto cards, which were sealed into opaque envelopes and kept by a designated person. After confirmation of their participation in the trial, each study participant selected an envelope containing a numbered card according to the order of enrollment. Before treatment, the envelope was handed over to the doctor and opened to reveal the randomly generated number corresponding to a treatment group.
Blinding
This clinical study followed the principle of blinding. During the implementation of blinding, the study participants, outcome assessors, and data analysts were all blinded to participants’ distribution groups. However, given the particularity of acupuncture therapy, the treating acupuncturists were not blinded to the groups.
Study participants
Study patients were recruited from the multiple clinics of the Acupuncture and Moxibustion Department, Neurology Department of the Affiliated Hospital of Nanjing University of Chinese Medicine between January 2019 and January 2020. All patients who wanted to participate in the study phoned the study coordinator, and an initial appointment for the clinical interview was made.
Diagnostic criteria
The diagnostic criteria for CI were in compliance with the International Classification of Sleep Disorders (ICSD-3), developed by the American Academy of Sleep Medicine (19).
Inclusion criteria
The inclusion criteria for study patients were as follows: (I) patients meeting the ICSD-3 diagnostic criteria for insomnia; (II) aged from 18 to 70 years old, with no restrictions on sex; (III) Pittsburgh Sleep Quality Index (PSQI) score >5 points, Hamilton Anxiety Rating Scale (HAMA) score ≥7 points, and Hamilton Depression Rating Scale (HAMD) score ≥14 points (6); (IV) no use of hypnotic medication or acupuncture treatment in the previous month; (V) no communication or cognitive impairment; and (VI) voluntarily accepted the random grouping and signed the informed consent form.
Exclusion criteria
(I) Patients diagnosed with schizophrenia or another serious mental illness; (II) patients diagnosed with obstructive sleep apnea, restless legs syndrome, or another sleep disorder; (III) patients with alcohol or any other drug abuse; (IV) pregnant or lactating women; and (V) patients who had participated in another clinical trial in the previous 3 months.
Elimination of termination criteria
(I) Patients whose insomnia symptoms worsened during the trial and were assessed by the researchers as needing other treatment in time, rendering them unsuitable for continuing the trial; (II) patients who experienced serious adverse events, serious complications, or special physiological changes caused by other diseases during the treatment process.
In the above cases, the participant was asked for the specific reasons for withdrawal by telephone or WeChat contact, and the reasons were recorded to retain relevant research information.
Interventions
Basic treatment
The two acupuncturists who participated in this study all had a master’s degree in Acupuncture and Massage from Nanjing University of Chinese Medicine, 8 years of professional training in acupuncture, and a doctor’s qualification certificate . The Information Collection System of Chinese Medicine Diagnosis and Treatment of Insomnia (software copyright, Registration No. 2019SR0900086) was used to conduct unified sleep hygiene education for the two groups of CI patients.
Acupuncture group
For the acupuncture group, Baihui (GV20), Yintang (GV29), Shenmen (HT7, bilateral), and Sanyinjiao (SP6, bilateral) were selected as the acupoints (Figure 1). The positions of the above acupoints are strictly in accordance with the National Standard of the People’s Republic of China: Acupoints Location (GB12346-90). After the insertion of the needles (size: 0.30×25 mm) to a certain depth, equal manipulations involving twirling, lifting, and thrusting were implemented to elicit ‘De-qi’, a sensation of soreness numbness, heaviness, and distention. The electroacupuncture stimulation lasted for 30 minutes with a dilatational wave of 2 Hz at GV20 and GV29, with continuous wave stimulation, and a current intensity of 0.1 to 1 mA depending on the participant’s comfort level (preferably with the skin around the acupoints shivering mildly without pain) (Table 1).
Figure 1.
Acupoints locations.
Table 1. Treatment parameters.
| Interventions | Acupuncture group | Sham Acupuncture group |
|---|---|---|
| Points | Baihui (GV-20), Yintang (GV-29), Shenmen (HT-7, bilateral), Sanyinjiao (SP-6, bilateral) | Jianyu (LI15, bilateral), Binao (LI14, bilateral), Futu (ST32, bilateral) |
| Depth description | GV-20, GV-24 and GV-29 being inserted 10 mm obliquely. HT-7 being penetrated 10 mm straightly, while SP-6 being perpendicularly punctured 15 mm | All acupoints were inserted 1–2 mm |
| Needle retention time | 30 min | 30 min |
| Needle type | 0.30×25 mm (Huatuo, Suzhou, China) | 0.30×25 mm (Huatuo, Suzhou, China) |
| Needle stimulation | By thrusting and twirling to achieve the sensation of ‘De-qi’ | Without twirling, lifting, and thrusting to minimize the placebo effect by avoiding manual stimulation and sensation of ‘De-qi’ |
| Frequency and duration of treatment sessions | Three times a week for 4 weeks | Three times a week for 4 weeks |
Sham acupuncture group
According to previous research (20), the non-disorder-related acupoints Jianyu (LI15, bilateral), Binao (LI14, bilateral), and Futu (ST32, bilateral) were selected for the sham acupuncture group. Disposable sterile needles (size: 0.30×25 mm) were inserted 1–2 mm into the acupoints without twirling, lifting, or thrusting to avoid manual stimulation and ‘De-qi’ and minimize the placebo effect. Then, the low-frequency pulsed electroacupuncture therapeutic instrument (the same instrument used in the acupuncture group) was placed next to the patients, connected to LI15 and LI14 on one side, and turned on for 30 minutes, while we did not open the stimulus intensity button to ensure the normal display of the power supply and the timer (Table 1).
The course of treatment: treatment was given 3 times a week (once every other day) for 4 weeks (12 sessions in total).
Regarding the purpose of the study, the study patients were informed as follows: ‘In this study, we will compare different types of acupuncture treatments, which have been proven effective in the previous clinical practices’ (21). During the study, the prescriptions of any sedative or hypnotic drugs, including Chinese medicine, Chinese patent medicine, and Western medicine (e.g., benzodiazepines, non-benzodiazepines, antidepressants, and anxiety drugs), were not permitted.
Observation indexes and methods
All CI patients were assessed online within 1 week before and after treatment and at follow-up 3 months after treatment. The assessment was conducted by the same nurse from the Acupuncture and Rehabilitation Department Ward, using the Information Collection System of Chinese Medicine Diagnosis and Treatment of Insomnia to guide the patients to complete the scale assessment online. The nurse did not participate in the treatment and did not know the participants’ grouping.
Sleep index
The PSQI, which can be used to evaluate an individual’s sleep quality in the past one month and its correlation with their mental and physical health, was adopted. The higher an individual’s score, the poorer their sleep quality. Most previous studies used a PSQI score of >5 points as the threshold for diagnosing insomnia limit (22). This study used the total score of PSQI, sleep efficiency, sleep quality, and sleep latency as a statistical analysis indicator.
Psychiatric symptom rating scale
The HAMA scale was adopted for the assessment of participants’ anxiety state. The scale comprises 14 items and uses a 5-level scoring system (0 to 4 points) to assess both physical and mental aspects: the higher an individual’s score, the more severe their anxiety symptoms (23).
The HAMD scale was adopted for the assessment of participants’ depression state. We used the 17-item version for the assessment, including 7 factors (despair, anxiety, sleep disorders, weight, cognitive impairment, day and night change, and retardation). The higher an individual’s score, the more severe their depression symptoms (24).
Serum 5-HT and CORT
All patients were required to take a fasting blood test at 8 A.M. before and after treatment and were instructed to avoid vigorous activities before blood was drawn. The concentrations of serum 5-HT and CORT were detected by enzyme-linked immunosorbent assay (ELISA). Briefly, after collecting 4 mL of venous blood, the serum was isolated by centrifugation at 3,000·rev/min for 5 minutes and placed in a refrigerator (−80 °C). Venous blood was taken twice in total, before and after treatment. All specimens were dealt with in strict accordance with the instructions supplied with the ELISA kit.
Sample size
We hypothesized that the acupuncture group in our study could reduce the PSQI score by 5.13 points compared with the sham acupuncture group, and the standard deviation (SD) of 3.42 was taken from the results of previous research. According to the needs of this study, α=0.05 and 1−β=0.90, based on the following formula (25):
| [1] |
Calculating the sample size of each group: n=25.7≈26; considering the loss factor (according to a 15% loss rate), the number of samples in each group was 30 cases, and the total number of samples in the two groups was 60 cases.
Safety evaluation
Adverse reactions that occurred during treatment and their extent and duration were timely recorded, including local hematoma, needle syncope, stuck needle, and infections. In the occurrence of adverse reactions, the cause was determined, its relevance to acupuncture treatment was analyzed, and symptomatic treatment was given. All CI patients were evaluated for safety before and at the end of treatment according to the level of adverse reactions, as follows: level 1: safe, without any adverse reactions to acupuncture; level 2: relatively safe, with adverse reactions not requiring any treatment and able to continue acupuncture; level 3: safety problems, with moderate adverse reactions (such as dizziness, etc.) but able to continue acupuncture after treatment; and level 4: withdrawal from the trial due to an adverse reaction(s).
Statistical analyses
Data were expressed as the mean ± standard deviation and analyzed using SPSS22.0 software and GraphPad Prism. Comparisons between the acupuncture and sham acupuncture groups were performed using t-tests. The PSQI, HAMA, HAMD scores, serum 5-HT, and CORT levels were compared between the two groups using independent-samples t-tests. Paired-samples t-tests were used to compare the indicators at different time points (before vs. after treatment, before treatment vs. at the follow-up, and after treatment vs. at the follow-up). P values of less than 0.05 were assumed to indicate a significant difference.
Medical ethics and clinical registration
This clinical trial was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and Chinese Clinical Trial Research Specifications. Ethical approval was obtained from the Institutional Review Board of the Affiliated Hospital of Nanjing University of Chinese Medicine (Nanjing, Jiangsu, China) (approval number: 2018NL-142-02), and the trial was registered in the Chinese Clinical Trial Registry (ChiCTR1800020298). Informed consent was taken from all the patients.
Results
Demographic characteristics
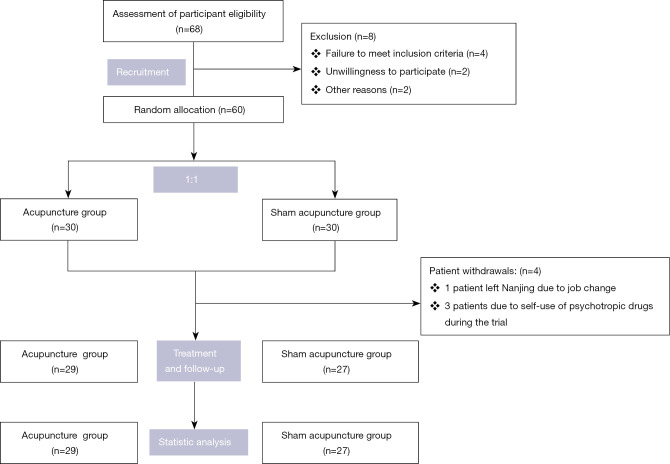
The study period lasted from January 2019 and January 2020. A total of 60 CI patients were enrolled in the trial, of whom 4 patients dropped out during the study period (1 patient in the acupuncture group left Nanjing due to a job change, and 3 patients in the sham acupuncture group were withdrawn due to self-use of psychotropic drugs during the trial). Therefore, 56 patients were included in the full analysis set (Figure 2).
Figure 2.
Flow diagram.
There were no statistically significant differences in the general information (sex, age, course of disease, and degree of illness) of the patients in the two groups (Table 2).
Table 2. General information of CI patients in the two treatment groups.
| Groups | Cases | Sex (cases) | Age (years) | Disease duration (months) | PQSI (score) | |
|---|---|---|---|---|---|---|
| Male | Female | |||||
| Acupuncture group | 29 | 13 | 16 | 47.17±14.08 | 2.71±3.22 | 14.17±2.30 |
| Sham acupuncture group | 27 | 10 | 17 | 45.59±12.65 | 2.90±3.55 | 14.78±2.28 |
CI, chronic insomnia.
Scale evaluation
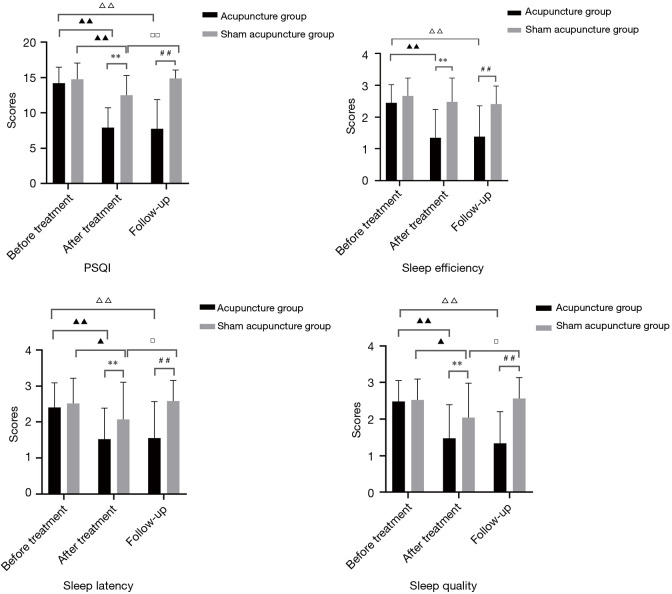
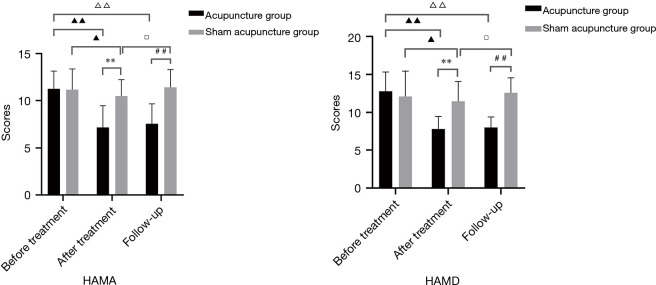
After treatment, the PSQI, HAMA, and HAMD scores in the acupuncture group were significantly lower than those before treatment. At follow-up, the scores in the acupuncture group showed no significant differences compared with those after treatment. After treatment and follow-up, the scores in the sham acupuncture group all increased, showing no significant difference from those before treatment. At follow-up, the PSQI, HAMA, and HAMD scores in the acupuncture group were significantly lower than those in the sham acupuncture group (Table 3 and Figures 3,4).
Table 3. Comparison of various evaluation indexes between the two groups.
| PSQI | Acupuncture group (n=29) | Sham acupuncture group (n=27) | |||||
|---|---|---|---|---|---|---|---|
| Before treatment | After treatment | Follow-up | Before treatment | After treatment | Follow-up | ||
| Sleep quality | 2.48±0.57 | 1.48±0.91▲▲** | 1.34±0.86ΔΔ## | 2.52±0.58 | 2.04±0.94▲□ | 2.56±0.58 | |
| Sleep latency | 2.41±0.68 | 1.52±0.87▲▲** | 1.55±1.02ΔΔ## | 2.52±0.7 | 2.07±1.04▲□ | 2.59±0.57 | |
| Sleep efficiency | 2.45±0.57 | 1.34±0.90▲▲** | 1.38±0.98ΔΔ## | 2.67±0.56 | 2.48±0.75 | 2.41±0.57 | |
| Total score | 14.17±2.30 | 7.93±2.77▲▲** | 7.76±4.10ΔΔ## | 14.78±2.28 | 12.48±2.82▲▲□□ | 14.89±1.18 | |
| HAMA | 11.24±1.92 | 7.17±2.29▲▲** | 7.55±2.11ΔΔ## | 11.15±2.23 | 10.48±1.72▲□ | 11.41±1.89 | |
| HAMD | 12.79±2.54 | 7.83±1.65▲▲** | 8.03±1.38ΔΔ## | 12.11±3.33 | 11.48±2.60▲□ | 12.59±1.97 | |
| CORT | 441.90±72.87 | 360.38±72.22▲▲** | – | 430.22±67.89 | 409.11±64.91▲ | – | |
| 5-HT | 439.55±121.14 | 540.79±86.59▲▲** | – | 455.67±89.12 | 476.24±92.23 | – | |
(I) Comparison within the groups: before vs. after treatment, ▲, P<0.05, ▲▲, P<0.01; during follow-up vs. before treatment, ΔΔ, P<0.01; during follow-up vs. after treatment, □, P<0.05, □□, P<0.01; (II) comparison between the acupuncture group and the sham acupuncture group: after treatment, **, P<0.01; and during follow-up, ##, P<0.01. PSQI, Pittsburgh Sleep Quality Index; HAMA, Hamilton Anxiety Rating Scale; HAMD, Hamilton Depression Rating Scale; CORT, corticosterone; 5-HT, 5-hydroxytryptamine.
Figure 3.
Comparisons of the scores of each PSQI category between the two groups of CI patients. Comparison between before-treatment and after-treatment: ▲, P<0.05; ▲▲, P<0.01; Comparison between before-treatment and at follow-up: △△, P<0.01; comparison between after-treatment and at follow-up: □, P<0.05, □□, P<0.01; Comparison between the two groups after treatment: **, P<0.01; At follow-up, acupuncture group was compared with the control group: ##, P<0.01. PSQI, Pittsburgh Sleep Quality Index; CI, chronic insomnia.
Figure 4.
Comparison of the HAMA and HAMD scores between the two groups of CI patients. (I) Comparison within the groups: before vs. after treatment, ▲, P<0.05, ▲▲, P<0.01; during follow-up vs. before treatment, △△, P<0.01; during follow-up vs. after treatment, □, P<0.05; (II) comparison between the acupuncture group and the sham acupuncture group: after treatment, **, P<0.01; and during follow-up, ##, P<0.01. HAMA, Hamilton Anxiety Rating Scale; HAMD, Hamilton Depression Rating Scale; CI, chronic insomnia.
Serum 5-HT and CORT concentrations
After treatment, the increase in serum 5-HT levels and the decrease in serum CORT levels were greater in the acupuncture group than in the sham acupuncture group (Table 3 and Figure 5).
Figure 5.
Comparison of serum 5-HT and CORT levels between the two groups of CI patients. (I) Comparison within the groups: before vs. after treatment, ▲, P<0.05, ▲▲, P<0.01; (II) comparison between the acupuncture group and the sham acupuncture group after treatment, **, P<0.01. 5-HT, 5-hydroxytryptamine; CORT, corticosterone; CI, chronic insomnia.
Safety evaluation
One patient suffered a mild subcutaneous hematoma in the acupuncture group. In the sham acupuncture group, one patient experienced mild fatigue, which was evaluated as level 2 in terms of safety.
Discussion
There are many records in Internal Classic that state acupuncture can regulate the spirit. Later generations of physicians have pointed out that the theory that acupuncture can regulate the spirit has unique advantages in treating insomnia. According to the classic theory of Chinese medicine, regarding the relationship between the Du meridian and spirit, the Du meridian dominates Yang Qi, communicates with the brain upward, connects the viscera internally, and links the meridians externally. The key pathogenesis of insomnia is “restless brain spirit, irritable mind, and disorder of the spirit of five zang organs.” Therefore, clinical practitioners often regulate the brain, spirit, mind, and five zang organs spirit through the Du meridian to treat insomnia. In summary, the application of Tiaoshen acupuncture to the Baihui (GV20), Yintang (GV29), Shenmen (HT7), and Sanyinjiao (SP6) can invigorate Yang qi, balance Yin and Yang, regulate the Du meridian, and calm the mind to promote peaceful sleep and a good mood.
According to the present study results, acupuncture was more effective than sham acupuncture in improving sleep efficiency and quality and decreasing sleep latency, anxiety, and depression in CI patients. A good medical environment, communication between the physicians and patients, and basic sleep health education during the diagnosis and acupuncture treatment process could alleviate the patient’s bad mood to some extent. Thus, sham acupuncture could also improve the sleep state and anxiety, and depression of CI patients. A follow-up assessment was carried out for all patients 3 months after the end of treatment using an online scale. The results showed that the acupuncture group exhibited a sustained and relatively stable improvement in sleep assessment parameters and reduced anxiety and depression scores compared to the sham acupuncture group, which was consistent with the conclusion of previous studies (26).
The HAMA and HAMD are currently widely used to evaluate the anxiety and depression state of CI patients with high reliability and validity (27). Good-quality sleep plays a vital role in regulating and stabilizing emotions, while long-term insomnia can cause anxiety, depression, and other emotional disorders. Modern research has confirmed that anxiety, depression, and insomnia have mutual causal relations, promote and coexist with each other, and have a bi-directional relationship (28). In this study, acupuncture significantly decreased the HAMA and HAMD scores of patients with CI and relieved their anxiety and depression to some extent, which was consistent with the conclusion of previous studies (29).
As a major inhibitory neurotransmitter, 5-HT is involved in the brain’s regulation of emotion and memory and is closely related to insomnia . Studies have shown that CI patients accompanied by anxiety and depression generally have a low 5-HT content and low function, which leads to reduced excitability of neural activity in the body and induces anxiety and depression symptoms (30). Research has also shown that acupuncture can increase the tryptophan content in the peripheral system, increase the level of 5-HT in the blood, and accelerate tryptophan transport in the blood, thereby promoting the synthesis of 5-HT in the brain and ultimately improving the sleep of patients (31). CORT, as an important stress hormone, plays a key role in neuroendocrine regulation. CI patients are often in a certain state of stress, which activates HPA and causes an increase in glucocorticoid and catecwholamine content, eventually causing an increase in cortisol levels (32). The increase in cortisol can also inhibit the activity of 5-HT neurons in the mesenteric nucleus-hippocampus system (33), aggravating the patients’ condition. Studies have shown that excessive CORT results in abnormal structural and functional connections in brain regions related to mood regulation, such as the temporal lobe cortex and anterior wedge, by binding to glucocorticoid receptors (GR) and mineralocorticoid receptors (MR), resulting in insomnia, anxiety, and depression symptoms (34). A previous study performed acupuncture on 29 CI patients for 2 weeks. After treatment, CORT and the GR, MR in the above-mentioned brain regions were down-regulated, which improved patients’ anxiety and depression to some extent (35). Based on the research findings of relevant scholars on the effects of acupuncture on 5-HT, its receptors, and HPA axis-related hormones in rats with sleep deprivation, together with the preliminary results of this trial, we speculated that acupuncture might regulate insomnia, anxiety, and depression symptoms in CI patients by reducing the level of serum CORT while increasing those of 5-HT (36).
There are several limitations to this study. Firstly, this study mainly used subjective scales to evaluate the efficacy of acupuncture on CI patients resulting in a lack of objectivity. Polysomnography(PSG) should be used to monitor sleep and verify our results in a larger sample size. Secondly, the etiology and pathogenesis of CI are complex, and it has various clinical classifications, so whether acupuncture applies to all characteristics of CI is worthy to further clinical trials. Lastly, insomnia has a complex relationship with mental disorders and the understanding of how insomnia causes anxiety and depression are still limited. This study focused on the neuroendocrine aspects of the common pathogenesis of insomnia and anxiety, and depression; however, more studies on the effects of acupuncture on CI patients with anxiety and depression take into account other aspects, such as sleep electrophysiology and brain function imaging, are still needed.
Supplementary
The article’s supplementary files as
Acknowledgments
Funding: The Science and Technology Project of Jiangsu Provincial Administration of Chinese Medicine (JD201810), Key R&D Program of Jiangsu Province (Social Development) (BE2021751), Six Talent Peaks ‘High-Level Talents’ Program of Jiangsu Province (WSN-015), Scientific Research Project of Jiangsu Academy of Chinese Medicine (BM2018024-2019017).
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This clinical trial was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and Chinese Clinical Trial Research Specifications. Ethical approval was obtained from the Institutional Review Board of the Affiliated Hospital of Nanjing University of Chinese Medicine (Nanjing, Jiangsu, China) (approval number: 2018NL-142-02). Informed consent was taken from all the patients.
Reporting Checklist: The authors have completed the CONSORT reporting checklist. Available at https://dx.doi.org/10.21037/atm-21-3845
Trial Protocol: Available at https://dx.doi.org/10.21037/atm-21-3845
Data Sharing Statement: Available at https://dx.doi.org/10.21037/atm-21-3845
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/atm-21-3845). The authors have no conflicts of interest to declare.
(English Language Editors: J. Reynolds and J. Chapnick)
References
- 1.Chung KF, Yeung WF, Ho FY, et al. Cross-cultural and comparative epidemiology of insomnia: the Diagnostic and statistical manual (DSM), International classification of diseases (ICD) and International classification of sleep disorders (ICSD). Sleep Med 2015;16:477-82. 10.1016/j.sleep.2014.10.018 [DOI] [PubMed] [Google Scholar]
- 2.Geoffroy PA, Hoertel N, Etain B, et al. Insomnia and hypersomnia in major depressive episode: Prevalence, sociodemographic characteristics and psychiatric comorbidity in a population-based study. J Affect Disord 2018;226:132-41. 10.1016/j.jad.2017.09.032 [DOI] [PubMed] [Google Scholar]
- 3.Ohayon MM. Observation of the natural evolution of insomnia in the American general population cohort. Sleep Med Clin 2009;4:87-92. 10.1016/j.jsmc.2008.12.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Christodoulou C, Efstathiou V, Ferentinos P, et al. Comparative study of hostility in depressive patients with and without a suicide attempt history. Psychol Health Med 2017;22:866-71. 10.1080/13548506.2016.1238491 [DOI] [PubMed] [Google Scholar]
- 5.Wu W, Lin C, Chen S, et al. Research progress of serum inflammatory markers in patients with chronic insomnia with anxiety and depression. Medicine and Philosophy 2017;38:18-21. [Google Scholar]
- 6.Gu X, Gu P, Liu Y, et al. Correlation between anxiety, depression and sympathetic skin response in patients with chronic insomnia. Chinese Journal of Neurology 2017;50:665-70. [Google Scholar]
- 7.Buysse DJ. Insomnia. JAMA 2013;309:706-16. 10.1001/jama.2013.193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Edinger JD, Wyatt JK, Stepanski EJ, et al. Testing the reliability and validity of DSM-IV-TR and ICSD-2 insomnia diagnoses. Results of a multitrait-multimethod analysis. Arch Gen Psychiatry 2011;68:992-1002. 10.1001/archgenpsychiatry.2011.64 [DOI] [PubMed] [Google Scholar]
- 9.Becker NB, Jesus SN, João KADR, et al. Depression and sleep quality in older adults: a meta-analysis. Psychol Health Med 2017;22:889-95. 10.1080/13548506.2016.1274042 [DOI] [PubMed] [Google Scholar]
- 10.Chen PJ, Huang CL, Weng SF, et al. Relapse insomnia increases greater risk of anxiety and depression: evidence from a population-based 4-year cohort study. Sleep Med 2017;38:122-9. 10.1016/j.sleep.2017.07.016 [DOI] [PubMed] [Google Scholar]
- 11.McCall WV, Black CG. The link between suicide and insomnia: theoretical mechanisms. Curr Psychiatry Rep 2013;15:389. 10.1007/s11920-013-0389-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mysliwiec V, Martin JL, Ulmer CS, et al. The Management of Chronic Insomnia Disorder and Obstructive Sleep Apnea: Synopsis of the 2019 U.S. Department of Veterans Affairs and U.S. Department of Defense Clinical Practice Guidelines. Ann Intern Med 2020;172:325-36. 10.7326/M19-3575 [DOI] [PubMed] [Google Scholar]
- 13.Liu C, Xi H, Wu W, et al. Placebo effect of acupuncture on insomnia: a systematic review and meta-analysis. Ann Palliat Med 2020;9:19-29. 10.21037/apm.2019.11.15 [DOI] [PubMed] [Google Scholar]
- 14.He W, Li M, Zuo L, et al. Acupuncture for treatment of insomnia: An overview of systematic reviews. Complement Ther Med 2019;42:407-16. 10.1016/j.ctim.2018.12.020 [DOI] [PubMed] [Google Scholar]
- 15.Wu X, Zheng X, Guo X, et al. Research Progress of Acupuncture and moxibustion interfering with HPA Axis related hormones to improve Sleep. Journal of Clinical Acupuncture and Moxibustion 2017;33:69-71. [Google Scholar]
- 16.Owens M, Herbert J, Jones PB, et al. Elevated morning cortisol is a stratified population-level biomarker for major depression in boys only with high depressive symptoms. Proc Natl Acad Sci U S A 2014;111:3638-43. 10.1073/pnas.1318786111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gao X, He X, Lan Z, et al. Correlation between plasma serotonin and cortisol levels and severity of depression. Prevention and Control of chronic Diseases in China 2017;25:129-30.
- 18.Moher D, Hopewell S, Schulz KF, et al. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. Int J Surg 2012;10:28-55. 10.1016/j.ijsu.2011.10.001 [DOI] [PubMed] [Google Scholar]
- 19.American Academy of Sleep Medicine. International Classification of Sleep Disorders (3rd ed.). 2014; Darien, IL: American Academy of Sleep Medicine. [Google Scholar]
- 20.Yang HY, Wang DY, Dong X, et al. Status of placebo acupuncture control research. Zhongguo Zhen Jiu 2020;40:337-41. [DOI] [PubMed] [Google Scholar]
- 21.Wang C, Yang WJ, Yu XT, et al. Acupuncture for insomnia with short sleep duration: protocol for a randomised controlled trial. BMJ Open 2020;10:e033731. 10.1136/bmjopen-2019-033731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Manzar MD, BaHammam AS, Hameed UA, et al. Dimensionality of the Pittsburgh Sleep Quality Index: a systematic review. Health Qual Life Outcomes 2018;16:89. 10.1186/s12955-018-0915-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Riemann D, Baglioni C, Bassetti C, et al. European guideline for the diagnosis and treatment of insomnia. J Sleep Res 2017;26:675-700. 10.1111/jsr.12594 [DOI] [PubMed] [Google Scholar]
- 24.Broen MP, Moonen AJ, Kuijf ML, et al. Factor analysis of the Hamilton Depression Rating Scale in Parkinson's disease. Parkinsonism Relat Disord 2015;21:142-6. 10.1016/j.parkreldis.2014.11.016 [DOI] [PubMed] [Google Scholar]
- 25.Sakpal TV. Sample size estimation in clinical trial. Perspect Clin Res 2010;1:67-9. [PMC free article] [PubMed] [Google Scholar]
- 26.Luo D, Wu Y, Cai L, et al. Clinical efficacy of soothing the liver and regulating mind acupuncture in the treatment of depression-related insomnia. Chinese Journal of Gerontology 2017;37:3837-9. [Google Scholar]
- 27.Rohan KJ, Rough JN, Evans M, et al. A protocol for the Hamilton Rating Scale for Depression: Item scoring rules, Rater training, and outcome accuracy with data on its application in a clinical trial. J Affect Disord 2016;200:111-8. 10.1016/j.jad.2016.01.051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zeng T, Tan H. Correlation between sleep disorder and cognitive executive function impairment and anxiety and depression in asymptomatic cerebral infarction. Journal of Practical Medicine 2019;35:3522-6. [Google Scholar]
- 29.Guo J, Huang W, Tang CY, et al. Effect of acupuncture on sleep quality and hyperarousal state in patients with primary insomnia: study protocol for a randomised controlled trial. BMJ Open 2016;6:e009594. 10.1136/bmjopen-2015-009594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Peng H, Li L, He Z. Hydrogen proton spectroscopy study on metabolic characteristics of anterior cingulate gyrus and activity level of hypothalamus-pituitary-adrenal axis in patients with depression. Chinese Journal of Mental Health 2013;27:624-8. [Google Scholar]
- 31.Luo B, Wang Y, Zhang Y, et al. Effects of three acupuncture methods on the contents of 5-HT and 5-HIAA in hippocampus of rats with PCPA insomnia . Chinese Journal of basic Medicine of traditional Chinese Medicine 2016;22:1517-9. [Google Scholar]
- 32.Cui L, Cui W, Ma X, et al. Study on the relationship between the changes of hair and plasma cortisol levels and depression. Chinese Journal of Neuropsychiatric Disorders 2017;43:43-7. [Google Scholar]
- 33.Salacz P, Csukly G, Haller J, et al. Association between subjective feelings of distress, plasma cortisol, anxiety, and depression in pregnant women. Eur J Obstet Gynecol Reprod Biol 2012;165:225-30. 10.1016/j.ejogrb.2012.08.017 [DOI] [PubMed] [Google Scholar]
- 34.Sharpley CF, Bitsika V. Joining the dots: neurobiological links in a functional analysis of depression. Behav Brain Funct 2010;6:73. 10.1186/1744-9081-6-73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Xu X, Wang S, Lu R, et al. To observe the change of whole brain degree and centrality after acupuncture treatment in patients with primary insomnia by voxel-based resting state fMRI. Journal of Sun Yat-sen University (Medical Science Edition) 2017;38:296-300. [Google Scholar]
- 36.Wu X, Zheng X, Guo X, et al. Research progress on the effects of acupuncture on 5-HT, its receptor and HPA axis related hormones in insomniac rats. Chinese Journal of traditional Chinese Medicine 2018;36:127-9. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The article’s supplementary files as