Abstract
Objective: This study was designed to investigate the application value of humanistic care interventions in patients with lower extremity arteriosclerosis obliterans (LEASO). Methods: We enrolled 98 LEASO patients undergoing interventional therapy in our hospital into this study, among whom 47 cases received conventional care interventions (the regular group) while the other 51 received humanistic care interventions based on conventional care interventions (the research group). The two groups were compared in negative emotions, complications, and quality of life of patients. Results: Scores of negative emotions were lower in the research group than in the regular group after care (P < 0.05). The pain intensity decreased in both groups after care, with a sharper decrease in the research group (P < 0.05). The incidence of complications was lower in the research group than in the regular group after care (P < 0.05). The pain-free walking distance (PFWD) increased remarkably in both groups after care, with a longer PFWD in the research group than in the regular group (P < 0.05). Scores of the 36-Item Short-Form Health Survey (SF-36) increased after care in both groups (P < 0.05), with higher SF-36 scores in the research group than in the regular group (P < 0.05). SF-36 reflects the quality of life of patients from four aspects including vitality, emotional state, social function, and role-emotional. The care compliance and satisfaction level with care of patients were higher in the research group than in the regular group (P < 0.05). The care compliance rate and patient satisfaction level with care were higher in the research group than in the regular group (P < 0.05). Conclusion: Humanistic care interventions can reduce postoperative pain intensity and improve the quality of life in patients with LEASO.
Keywords: Humanistic care interventions, lower extremity arteriosclerosis obliterans, application value
Introduction
Lower extremity arteriosclerosis obliterans (LEASO), a chronic and progressive disease, is caused by insufficient blood supply for limbs affected by thickened arterial intima and artery stenosis and occlusion resulted from atherosclerosis, which triggers a series of symptoms and signs of the affected limb [1,2]. Mainly affecting middle-aged and elderly people, LEAOS has risen as a public health problem due to the aging of population and the changing dietary structure of people [3]. Limb ischemia caused by LEASO leads to surging disability and mortality, which seriously impairs the prognosis of patients [4]. At present, surgery and interventional therapy are effective in relieving arterial occlusion. Interventional therapy is a common treatment for LEASO patients, characterized by simple operations, small trauma, and high safety [5,6]; however, its long-term efficacy remains controversial. Therefore, it is highly significant to design scientific and standardized perioperative care interventions to enhance treatment efficacy, reduce the risk of complications, and improve the treatment services.
Continuous developments of social economy have increased people’s health awareness and requirements for nursing [7]. Care interventions have shown good application value in the treatment of various diseases [7,8]. For example, high-quality perioperative care can effectively relieve negative emotions and improve the quality of life in patients with lung cancer [8]. Personalized care can improve the perception of care and enhance the satisfaction level with care in patients undergoing orthopedic surgery [9]. So care interventions are crucial during disease treatment. Humanistic care interventions are guided by knowledge of multiple disciplines, which can enhance the subjectivity of nurses, foster a good nurse-patient relationship, and improve the overall quality of the nursing team, aiming to provide patients with more systematic and comprehensive high-quality services [10,11]. In view that only a few studies have investigated the application of humanistic care interventions, here we compared the clinical performances of humanistic care interventions and conventional care interventions to assess the application value of humanistic care interventions in LEASO patients undergoing interventional therapy.
Materials and methods
We analyzed the medical records of 98 LEASO patients undergoing interventional therapy in The First Hospital of Changsha. Among them, 47 cases (30 males and 17 females) receiving conventional care interventions were assigned to the regular group, with an average age of 62.01 ± 9.01 years; the other 51 cases (33 males and 18 females) receiving humanistic care interventions based on conventional care interventions were assigned to the research group, with an average age of 61.98 ± 8.77 years. This study has obtained ethical approval from the ethics committee of our hospital. All research participants signed the written informed consent. Inclusion criteria: Patients meeting the diagnostic criteria of LEASO [12]; patients with no drug treatment prior to hospital admission; patients with normal liver and kidney functions; patients with no genetic history of mental illness; patients capable of verbal communication; patients with clear consciousness. Exclusion criteria: Patients with comorbid systemic diseases such as infectious diseases and hematopoietic dysfunction; patients with surgical contraindications; patients with incomplete clinical data; patients unwilling to cooperate with treatment; patients with no family accompany at the time of admission.
Nursing methods
Patients in the regular group received conventional care interventions. The introduction of health knowledge to patients was arranged immediately after admission. The condition of patients was monitored closely. Before surgery, nurses provided guidance about diet, medication, daily routine, and care of the affected limb and ordered patients to quit smoking and drinking. Also, nurses instructed patients to soak their feet in warm water every day and take daily foot care. After surgery, patients were given necessary anticoagulation treatment. Nurses instructed patients to do appropriate physical exercises when patients’ physical condition allowed and gave certain nursing guidance when patients were discharged from the hospital.
Patients from the research group received humanistic care interventions based on conventional care interventions. All nurses were trained about humanistic care knowledge to improve their nursing skills, responsibility, patience, and compassion. Humanistic care interventions were patient-centered and aimed to meet the needs of patients as much as possible. Specific care interventions were tailored to patients’ educational backgrounds and personality characteristics. For psychological interventions, nurses actively communicated with patients, answered various questions raised by them with enthusiasm and patience, and listened to the inner voice of patients to build trust. Nurses also encouraged the families of patients to show care, love, and support for patients to reduce their psychological burden, making joint efforts to provide patients with humanistic care. The ward was comfortable, quiet, and well-equipped to improve the patient’s sense of belonging and facilitate the implementation of care inventions. Health knowledge was regularly introduced. Before surgery, patients were informed about knowledge on the disease and treatment, as well as possible postoperative complications and related countermeasures. Nurses shared some successful treatment cases with patients to correct their perception of the disease and enhance their self-confidence. Also, nurses evaluated the pain intensity of patients and designed pain interventions to increase patients’ pain threshold. Patients were distracted from pain by things they were interested in or took analgesics in severe cases. Nurses stressed the importance of foot care during the hospitalization and instructed patients to wash their feet gently with warm water every day without damaging their skin. Patients were also recommended to wear soft and comfortable socks and shoes. Nurses also provided appropriate dietary guidance. Patients with comorbid diabetes received interventions to control blood sugar, and those with comorbid hypertension were instructed about standard medication to effectively control their blood pressure.
Outcome measures
1. The efficacy of interventional therapy in LEASO patients receiving different care interventions was evaluated, which was divided into marked response, moderate response, and no response [3].
2. The degree of anxiety and depression was assessed by the Self-Rating Anxiety Scale (SAS) and Self-Rating Depression Scale (SDS) designed by W. K. Zung [13,14]. A higher SAS/SDS score indicates a higher degree of negative emotions.
3. Pain intensity was evaluated by the Visual Analogue Scale (VAS) [15]. A higher VAS score indicates higher pain intensity.
4. Postoperative complications, care compliance rate, and pain-free walking distance (PFWD) of all patients were recorded.
5. The quality of life of patients was assessed by the 36-Item Short-Form Health Survey (SF-36) [16]. A higher SF-36 score indicates a better quality of life. Patient satisfaction with care was evaluated by the self-made questionnaire.
Statistical analysis
Data analysis and visualization were performed using Graphpad prism 6. Count data were expressed as n [%] and the comparison was analyzed by the chi-square test. Measurement data were expressed as mean ± standard deviation and the comparison was analyzed by the t-test. The difference between before care and after care was analyzed by the ANOVA and LSD-t post-hoc test. P < 0.05 indicates the difference was statistically significant.
Results
Comparison of clinical data of patients
Details of clinical data of all patients are shown in Table 1. Differences between the research and the regular groups in sex, average age, body mass index (BMI), smoking, hypertension, diabetes, and number of affected limbs are not statistically significant (P > 0.05).
Table 1.
Clinical data of patients [n (%)/(mean ± SD)]
| Research group (n = 51) | Regular group (n = 47) | X2/t | P | |
|---|---|---|---|---|
| Sex | 0.009 | 0.928 | ||
| Male | 33 (64.71) | 30 (63.83) | ||
| Female | 18 (35.29) | 17 (36.17) | ||
| Average age (year) | 61.98 ± 8.77 | 62.01 ± 9.01 | 0.017 | 0.987 |
| BMI (kg/m2) | 26.01 ± 4.23 | 25.79 ± 4.37 | 0.252 | 0.802 |
| Smoking | 0.056 | 0.813 | ||
| Yes | 27 (52.94) | 26 (55.32) | ||
| No | 24 (47.06) | 21 (44.68) | ||
| Comorbid hypertension | 0.085 | 0.771 | ||
| Yes | 30 (58.82) | 29 (61.70) | ||
| No | 21 (41.18) | 18 (38.30) | ||
| Comorbid diabetes | 0.022 | 0.881 | ||
| Yes | 17 (33.33) | 15 (31.91) | ||
| No | 34 (66.67) | 32 (68.09) | ||
| Number of affected limbs | 0.037 | 0.848 | ||
| One | 36 (70.59) | 34 (72.34) | ||
| Two | 15 (29.41) | 13 (27.66) |
Comparison of treatment efficacy in patients
Details of treatment responses in the two groups are shown in Table 2. Overall response rate = the percentage of cases with marked responses + cases with moderate responses. The overall response rate was slightly higher in the research group than in the regular group (90.20% vs. 80.85%), but the difference was not significant (P > 0.05).
Table 2.
Treatment responses in the two groups [n (%)]
| Marked response | Moderate response | No response | Overall response rate | |
|---|---|---|---|---|
| Research group (n = 51) | 28 (54.91) | 18 (35.29) | 5 (9.80) | 46 (90.20) |
| Regular group (n = 47) | 18 (38.30) | 20 (42.55) | 9 (19.15) | 38 (80.85) |
| X2 | 1.744 | |||
| P | 0.187 |
Comparison of scores of negative emotions
The degree of anxiety and depression was reflected by the SAS and SDS designed by W. K. Zung (Figure 1). Differences in anxiety and depression scores between the two groups before care were not marked (P > 0.05). Scores of anxiety and depression decreased remarkably in both groups after care, with lower anxiety and depression scores in the research group than in the regular group (P < 0.05).
Figure 1.

Comparison of scores of negative emotions. A. Comparison of the anxiety score. B. Comparison of the depression score. Note: “a” indicates P < 0.05 when compared with data before care within the same group; “b” indicates P < 0.05 when compared with data in the regular group after care.
Comparison of pain intensity
Pain intensity of patients was reflected by the VAS (Figure 2). Differences in the pain sore between the two groups before care were not marked (P > 0.05). The pain score decreased remarkably in both groups after care, with a lower pain score in the research group than in the regular group (P < 0.05).
Figure 2.

Comparison of the pain score between the two groups before and after care. Note: “a” indicates P < 0.05 when compared with data before care within the same group; “b” indicates P < 0.05 when compared with data in the regular group after care.
Comparison of postoperative complications
Details of postoperative complications in the two groups are shown in Table 3. The overall incidence of postoperative complications was remarkably lower in the research group than in the regular group (9.80% vs. 25.54%, P < 0.05).
Table 3.
Postoperative complications in the two groups [n (%)]
| Infection | Hematoma | Pressure ulcer | Constipation | Arterial thrombosis | Incidence rate | |
|---|---|---|---|---|---|---|
| Research group (n = 51) | 1 (1.96) | 2 (3.92) | 0 (0.00) | 2 (3.92) | 0 (0.00) | 5 (9.80) |
| Regular group (n = 47) | 2 (4.26) | 3 (6.38) | 2 (4.26) | 4 (8.51) | 1 (2.13) | 12 (25.54) |
| X2 | 4.220 | |||||
| P | 0.040 |
Care compliance of patients
Care compliance was assessed from four dimensions: medication compliance, positive changes in living habits, self-monitoring, and regular review, as shown in Table 4. According to data statistics, the number of cases with good compliance in medication, positive changes in living habits, self-monitoring, and regular review was higher in the research group than in the regular group (P < 0.05).
Table 4.
Care compliance of patients
| Case number | Medication compliance | Positive changes in living habits | Self-monitoring | regular review | |
|---|---|---|---|---|---|
| Research group | 51 | 42 (82.35) | 33 (64.71) | 26 (50.98) | 35 (68.63) |
| Regular group | 47 | 30 (63.83) | 21 (44.68) | 14 (29.79) | 23 (48.94) |
| X2 | 4.305 | 3.965 | 4.548 | 3.926 | |
| P | 0.038 | 0.047 | 0.033 | 0.048 |
Comparison of walking capacity of patients
Details of PFWD of patients in the two groups are shown in Figure 3. The difference between the two groups in PFWD was not significant before care (P > 0.05). PFWD increased remarkably after care in both groups, with longer PFWD in the research group than in the regular group (489.10 ± 97.11 vs. 443.29 ± 93.39, P < 0.05).
Figure 3.
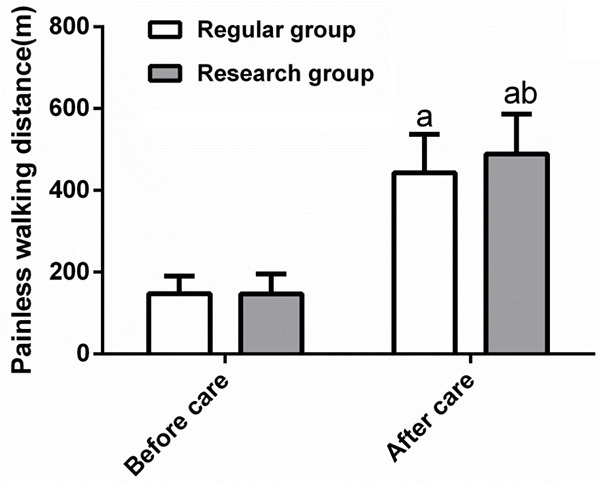
Comparison of the painless walking distance of patients between the two groups before and after care. Note: “a” indicates P < 0.05 when compared with data before care within the same group; “b” indicates P < 0.05 when compared with data in the regular group after care.
Comparison of quality of life of patients
The quality of life of patients was reflected by the SF-36 from four aspects including vitality, emotional state, social function, and role-emotional (Figure 4). Differences between the two groups in scores of the SF-36 were not notable before care. Scores of four aspects of the SF-36 increased in both groups after care (P < 0.05), with higher scores of four aspects of the SF-36 in the research group than in the regular group (P < 0.05).
Figure 4.
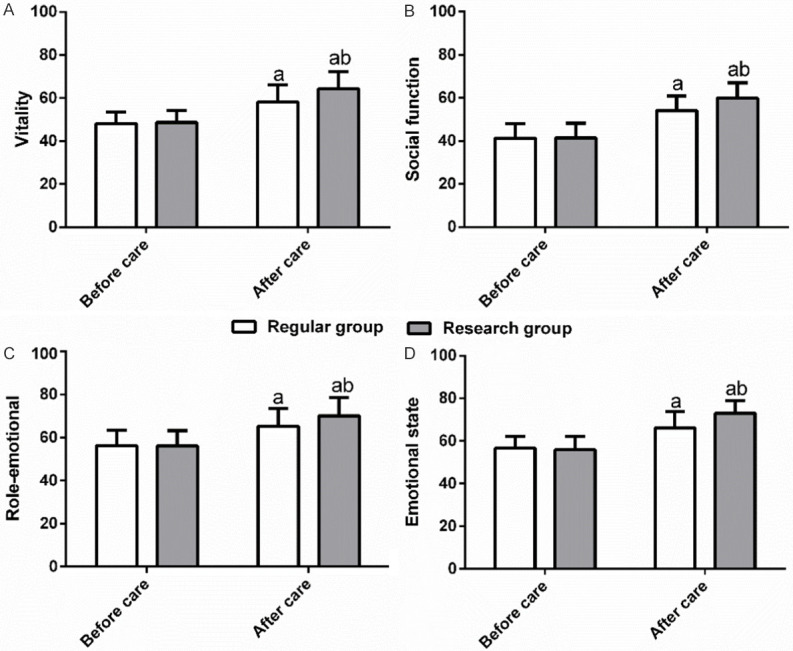
Comparison of quality of life of patients. A. Comparison of the score of viability between the two groups before and after care. B. Comparison of the score of social function between the two groups before and after care. C. Comparison of the score of role-emotional between the two groups before and after care. D. Comparison of the score of emotional state between the two groups before and after care. Note: “a” indicates P < 0.05 when compared with data before care within the same group; “b” indicates P < 0.05 when compared with data in the regular group after care.
Comparison of patient satisfaction with care
Patient satisfaction level was reflected by the self-made questionnaire, ranging from great satisfaction, partial satisfaction, moderate satisfaction, and dissatisfaction (Table 5). The care satisfaction rate was higher in the research group than in the regular group (94.12% vs. 80.85%, P < 0.05).
Table 5.
Patient satisfaction with care in the two groups [n (%)]
| Great satisfaction | Partial satisfaction | Moderate satisfaction | Dissatisfaction | Satisfaction level | |
|---|---|---|---|---|---|
| Research group (n = 51) | 15 (29.41) | 21 (41.18) | 12 (23.53) | 3 (5.88) | 48 (94.12) |
| Regular group (n = 47) | 7 (14.89) | 14 (29.79) | 17 (36.17) | 9 (19.15) | 38 (80.85) |
| X2 | 6.133 | ||||
| P | 0.013 |
Discussion
LEASO is a common life-threatening systemic peripheral vascular disease, manifesting as limb numbness, coldness, pain, and intermittent claudication in its early stage and developing into gangrene and even severe conditions requiring amputation [4,17]. Conventional care for LEASO is basic and can meet the needs of most hospitalized patients; however, it can hardly meet the needs of some patients due to the increasing requirements for care interventions, prompting the need for novel care interventions that can cooperate with treatment interventions to the greatest extent [18,19].
The main targets of existing care interventions are patient-centered to provide traditional medical care and give humanistic care to help patients find their own life value [20]. The humanistic care ability of medical staff can affect the treatment efficacy, psychological condition, and rehabilitation ability of patients [21]. The importance of humanistic care interventions in modern medicine has been acknowledged, but the application of humanistic care interventions in patients with LEASO has not been fully studied. Here we trained medical staff responsible for LEASO patients undergoing interventional therapy with relevant knowledge and skills on humanistic care interventions and assessed the treatment efficacy after care. The overall response rate was higher in patients receiving humanistic care interventions than in patients receiving conventional care interventions, but the difference was not statistically significant. Here we only assessed the short-term treatment efficacy in patients, so the effects of different care interventions on the long-term treatment efficacy need to be further studied. Suffering from long-lasting illness, LEASO patients, mostly the elderly, have weakened psychological defense and poor coping ability, thereby at high risks of negative emotions. A large number of studies abroad have revealed that care interventions for cognitive behavior, home care, and other care modes can effectively relieve the anxiety and depression of inpatients and reduce the psychological burden [22,23]. Then we scored negative emotions (anxiety and depression) in patients and noted a sharper reduction in scores of negative emotions in patients receiving humanistic care interventions than in patients receiving conventional care interventions. This is because nurses of humanistic care interventions mainly guide the ASO patients from the psychological level, listen carefully to the main complaints of the patients, assess their psychological state in time, and encourage families to give joint care to patients. A previous study has demonstrated that rapid rehabilitation care can effectively reduce pain intensity and the postoperative VAS score in patients with colorectal cancer [24], suggesting that care interventions can relieve pain to a certain extent. Insufficient blood supply to the lower limbs often causes severe and long-lasting pain in patients with LEASO [3,25], which decreases the quality of life of patients. The pain intensity is generally measured by the VAS score in clinic trials. In this study, nurses gave humanistic care based on conventional care interventions to distract patients from pain by exposing patients to the music they were interested in and instructing them to exercise for physical relaxation, thereby reducing the pain intensity.
LUAN et al. [26] suggested that comprehensive care interventions can reduce the risk of postoperative complications in patients with otorhinolaryngologic diseases. Clinical studies have shown that LEASO patients are susceptible to various complications after treatment, which attenuate treatment efficacy and impair recovery [27]. Here we found that humanistic care interventions efficiently reduced risks of complications after interventional therapy and improved the condition of patients by understanding the complications in advance and taking adequate preventive measures. It is generally believed that care interventions can reduce the incidence of postoperative complications, enhance the quality of life, increase the treatment compliance, and strengthen the self-care ability of patients, thereby improving prognosis. In this study, we assessed the care compliance of patients from four dimensions: medication compliance, positive changes in living habits, self-monitoring, and regular review. We noted better care compliance in patients receiving humanistic care interventions because nurses communicated friendly and frequently with patients to build mutual trust. A previous study [28] suggested that among diabetic patients with peripheral arterial disorder of the lower extremities, the walking distance was longer in patients relying on diet to control disease progression than in patients relying on drugs to control disease progression. In this study, the walking distance was longer in patients receiving humanistic care interventions than in patients receiving conventional care interventions alone. We speculate that this is because nurses of humanistic care interventions strictly controlled the diet of patients and instructed patients to do functional exercises to control blood sugar and blood pressure and increase walking distance. Assessment of the quality of life can effectively reflect the recovery of patients after treatment [29]. Care interventions can affect the quality of life of patients after treatment [30]. In this study, we evaluated the quality of life of patients with the SF-36 survey and found that humanistic care interventions enhanced knowledge and skills of medical staff, increased the communication efficiency, and hence improved the quality of life of LEASO patients after treatment. The humanistic care model requires medical staff to be decent, compassionate, and dedicated so that medical staff and patients can forge a harmonious and friendly relationship with mutual understanding [31]. Here we also assessed the patient satisfaction level with care. In this study, patients receiving humanistic care interventions showed higher satisfaction with care because nurses enhanced mutual trust and the nurse-patient relationship and improved the medical experience of patients.
In summary, this study illustrates that humanistic care interventions can effectively relieve negative emotions, reduce risks of complications, and improve the quality of life in LEASO patients undergoing interventional therapy. However, as the prognosis of patients is affected by many factors such as complications, hospital environment and family factors, the design of this study has certain limitations. In future studies, prognostic risk factors of LEASO patients will be explored, so as to better improve the treatment efficacy and the quality of life of patients.
Disclosure of conflict of interest
None.
References
- 1.Bai J, Wang F, Wang X, Mutu E, Duan C, Qi Y, Hu L, Gao Z. Expression and clinical significance of HSP27 and its phosphorylation in lower extremity arteriosclerosis obliterans. PeerJ. 2020;8:e9305. doi: 10.7717/peerj.9305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhuang JM, Li X, Li TR, Zhao J, Luan JY, Wang CM. Randomized controlled trial to superficial femoral artery recanalization for lower extremity arteriosclerosis obliterans. Beijing Da Xue Xue Bao Yi Xue Ban. 2017;49:153–157. [PubMed] [Google Scholar]
- 3.Yong J, Wang Y, Xing S, Bi Y, Li N, Zhao S. Efficacy of trimetazidine and plasmin combined with alprostadil in treatment of lower extremity arteriosclerosis obliterans. Exp Ther Med. 2019;17:4554–4560. doi: 10.3892/etm.2019.7476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Koshikawa M, Ikeda U. Arteriosclerosis obliterans (ASO) Nihon Rinsho. 2010;68:926–929. [PubMed] [Google Scholar]
- 5.Yao W, Wang L, Chen Q, Wang F, Feng N. Effects of valsartan on restenosis in patients with arteriosclerosis obliterans of the lower extremities undergoing interventional therapy: a prospective, randomized, single-blind trial. Med Sci Monit. 2020;26:e919977. doi: 10.12659/MSM.919977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li H, Gui H, Yuan G, Zheng X, Gao C, Yuan H. Increased plasma olfactomedin 2 after interventional therapy is a predictor for restenosis in lower extremity arteriosclerosis obliterans patients. Scand J Clin Lab Invest. 2018;78:269–274. doi: 10.1080/00365513.2018.1452287. [DOI] [PubMed] [Google Scholar]
- 7.Haahr A, Østergaard K, Kirkevold M. “It is hard work, but it is worth it”: patients and spouses’ experiences of a nursing intervention to promote adjustment to deep brain stimulation for parkinson’s disease-a feasibility study. ANS Adv Nurs Sci. 2018;41:174–187. doi: 10.1097/ANS.0000000000000208. [DOI] [PubMed] [Google Scholar]
- 8.Yu X, Liu J. Effects of high-quality nursing care for patients with lung cancer during the perioperative period: a protocol of systematic review of randomized controlled trials. Medicine (Baltimore) 2019;98:e18132. doi: 10.1097/MD.0000000000018132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tekin F, Findik UY. Level of perception of individualized care and satisfaction with nursing in orthopaedic surgery patients. Orthop Nurs. 2015;34:371–374. doi: 10.1097/NOR.0000000000000194. [DOI] [PubMed] [Google Scholar]
- 10.Chiang HH, Liaw JJ. Correspondence in humanistic care. Hu Li Za Zhi. 2017;64:50–58. doi: 10.6224/JN.000068. [DOI] [PubMed] [Google Scholar]
- 11.Mu PF. Discourse on humanistic clinical care and nurse healing. Hu Li Za Zhi. 2011;58:5–11. [PubMed] [Google Scholar]
- 12.Lian W, Nie H, Yuan Y, Wang K, Chen W, Ding L. Clinical significance of endothelin-1 and c reaction protein in restenosis after the intervention of lower extremity arteriosclerosis obliterans. J Invest Surg. 2021;34:765–770. doi: 10.1080/08941939.2019.1690600. [DOI] [PubMed] [Google Scholar]
- 13.Samakouri M, Bouhos G, Kadoglou M, Giantzelidou A, Tsolaki K, Livaditis M. Standardization of the Greek version of Zung’s Self-rating Anxiety Scale (SAS) Psychiatriki. 2012;23:212–220. [PubMed] [Google Scholar]
- 14.Kanda F, Oishi K, Sekiguchi K, Kuga A, Kobessho H, Shirafuji T, Higuchi M, Ishihara H. Characteristics of depression in Parkinson’s disease: evaluating with Zung’s self-rating depression scale. Parkinsonism Relat Disord. 2008;14:19–23. doi: 10.1016/j.parkreldis.2007.05.004. [DOI] [PubMed] [Google Scholar]
- 15.Rauh KH, Andersen RS, Rosenberg J. Visual analogue scale for measuring post-operative pain. Ugeskr Laeger. 2013;175:1712–1716. [PubMed] [Google Scholar]
- 16.Hepinstall MS, Rutledge JR, Bornstein LJ, Mazumdar M, Westrich GH. Factors that impact expectations before total knee arthroplasty. J Arthroplasty. 2011;26:870–876. doi: 10.1016/j.arth.2010.09.010. [DOI] [PubMed] [Google Scholar]
- 17.Han B, Ge CQ, Wang LP, Zhang SF, Li HZ, Zhang HG, Zhou CG, Ji GH, Yang Z, Zhang L. Leihong granule intervened in-stent restenosis after endovascular therapy for lower extremity arterial occlusive diseases: a clinical observation. Zhongguo Zhong Xi Yi Jie He Za Zhi. 2014;34:153–156. [PubMed] [Google Scholar]
- 18.Qiu LR, Zhou LJ, Wang BY. Clinical effect of nursing intervention for patients undergoing laparoscopic cholecystectomy. J Biol Regul Homeost Agents. 2019;33:231–235. [PubMed] [Google Scholar]
- 19.Fu SL, Sun CH, Shang XX, Liu XS. High quality nursing of children with pneumonia complicated with heart failure. J Biol Regul Homeost Agents. 2019;33:905–910. [PubMed] [Google Scholar]
- 20.Watson J. Love and caring. Ethics of face and hand--an invitation to return to the heart and soul of nursing and our deep humanity. Nurs Adm Q. 2003;27:197–202. doi: 10.1097/00006216-200307000-00005. [DOI] [PubMed] [Google Scholar]
- 21.Wu HL, Volker DL. Humanistic nursing theory: application to hospice and palliative care. J Adv Nurs. 2012;68:471–479. doi: 10.1111/j.1365-2648.2011.05770.x. [DOI] [PubMed] [Google Scholar]
- 22.Davidson JR, Dawson S, Krsmanovic A. Effectiveness of group cognitive behavioral therapy for insomnia (CBT-I) in a primary care setting. Behav Sleep Med. 2019;17:191–201. doi: 10.1080/15402002.2017.1318753. [DOI] [PubMed] [Google Scholar]
- 23.Shi RC, Meng AF, Zhou WL, Yu XY, Huang XE, Ji AJ, Chen L. Effects of home nursing intervention on the quality of life of patients with nasopharyngeal carcinoma after radiotherapy and chemotherapy. Asian Pac J Cancer Prev. 2015;16:7117–7121. doi: 10.7314/apjcp.2015.16.16.7117. [DOI] [PubMed] [Google Scholar]
- 24.Xu F, Yu P, Li L. Rapid rehabilitation nursing in postoperative patients with colorectal cancer and quality of life. Oncol Lett. 2019;18:651–658. doi: 10.3892/ol.2019.10379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang B, Liu W, Huo Y, Gong Z, Wang W, Hao R, Fang J, Zhang J, Jiang W. Application of femoral-femoral artery bypass grafting combined with transverse tibial bone transporting for lower extremity arteriosclerosis obliterans or combined with diabetic foot. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2018;32:1576–1580. doi: 10.7507/1002-1892.201806124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Luan RL, Zhu MX, Sun HY. Effect of comprehensive nursing intervention in preventing postoperative pain, complications, and psychological pressure in the otolaryngology department. Medicine (Baltimore) 2019;98:e15923. doi: 10.1097/MD.0000000000015923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hu M, Wang D, He T. Comparison of efficacy between trimetazidine and cilostazol in the treatment of arteriosclerosis obliterans in lower extremity. Exp Ther Med. 2019;17:4427–4434. doi: 10.3892/etm.2019.7472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dolan NC, Liu K, Criqui MH, Greenland P, Guralnik JM, Chan C, Schneider JR, Mandapat AL, Martin G, McDermott MM. Peripheral artery disease, diabetes, and reduced lower extremity functioning. Diabetes Care. 2002;25:113–120. doi: 10.2337/diacare.25.1.113. [DOI] [PubMed] [Google Scholar]
- 29.Hall A. Quality of life and value assessment in health care. Health Care Anal. 2020;28:45–61. doi: 10.1007/s10728-019-00382-w. [DOI] [PubMed] [Google Scholar]
- 30.Singh JA. Quality of life and quality of care for patients with gout. Curr Rheumatol Rep. 2009;11:154–160. doi: 10.1007/s11926-009-0022-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Deng J, Lei L, Zhang HL, Luo Y. The current status and the influencing factors of humanistic care ability among a group of medical professionals in Western China. Technol Health Care. 2019;27:195–208. doi: 10.3233/THC-181389. [DOI] [PMC free article] [PubMed] [Google Scholar]


