Abstract
Objective: This study aimed to investigate the value of Gensini score and interleukin-1 receptor antagonist (IL-1ra) in assessing the condition and prognosis of patients with coronary heart disease (CHD). Methods: According to their condition, 175 patients were divided into stable angina group (SA, 60 cases), unstable angina group (UA, 60 cases) and acute myocardial infarction group (AMI, 55 cases). The Gensini score, GRACE score, IL-1ra and troponin (Tn) were compared in the three groups. The correlation between Gensini score and GRACE score, IL-1ra and Tn, were explored. The patients were divided into death group (21 cases), adverse cardiovascular events group (MACE, 50 cases) and good prognosis group (104 cases) according to clinical outcomes. The ROC curve with regard to Gensini score, IL-1ra and the clinical outcome was plotted. Results: With the exacerbation of the disease, the Gensini score, GRACE score, IL-1ra and Tn were significantly higher in patients with CHD (P<0.05). Correlation analysis showed a positive association between Gensini score and GRACE score (r=0.9751, P<0.05). IL-1ra showed a positive association with Tn level (r=0.9731, P<0.05); Gensini score and IL-1ra had an area under the curve (AUC) of 0.9350 and 0.9499 for adverse CHD outcome, respectively (P<0.001). Conclusion: Gensini score and IL-1ra reflect better the severity of CHD in patients with CHD, and also the AUC of 0.9350 and 0.9499 (P<0.001). It can be used in the prognostic evaluation of patients with CHD.
Keywords: Gensini score, IL-1ra, coronary heart disease, condition assessment, prognosis, applied value
Introduction
Coronary heart disease (CHD) is a kind of comprehensive disease caused by carotid artery atherosclerosis. It is characterized by luminal narrowing or blockage, resulting in a series of lesions such as ischemia and hypoxia and then injury and necrosis, which is also known clinically as ischemic heart disease [1,2]. CHD is a common and frequently-occurred cardiovascular diseases. Rheology has shown that the number of deaths from CHD worldwide is as high as 17 million cases each year. With the improvement of the living standards of Chinese residents and the adjustment of dietary structure, the morbidity and mortality of cerebrovascular diseases have been significantly increased. Reports showed that CHD was a leading cause of death in 2009 [3,4]. CHD is usually with rapid onset, critical condition, and poor prognosis, which brings a serious burden to the patients and their families. Patients with CHD require long-term follow-up and regular re-examination, which also brings great medical pressure to society [5].
Accurate diagnosis and prognosis assessment are important measures to improve the quality of life of CHD patients. Currently, the common examination methods for CHD include routine examination, echocardiography, nuclear cardiac imaging, and coronary CT imaging, etc. However, nuclear cardiac imaging is suitable for the detection of myocardial metabolism and myocardial contractility, which makes it difficult to assess the degree of coronary artery stenosis visually. Performing imaging procedures requires a high level of experience and is difficult to perform in primary hospitals. Coronary angiography remains the gold standard for the evaluation of CHD and could not be replaced by any noninvasive test [6-8].
The Gensini score is a common method for evaluating the degree of coronary artery disease in clinical practice. Studies have confirmed that the score is of good value in the assessment of condition in CHD patients [9]. A retrospective analysis of 180 patients with CHD showed that the Gensini score was significantly different from that of individuals, and further analysis showed a correlation between Gensini score and patient prognosis [10]. Interleukin-1 receptor antagonist (IL-1ra) is a receptor that binds to cytokines and exerts biological effects. A study has shown that IL-1ra can promote endothelial cell activation, increase the secretion of adhesion factor and enhance leukocyte adhesion, and has been shown to be closely related to atherosclerosis [11]. The study aimed to investigate the feasibility of the Gensini score and IL-1ra in prognosis assessment of CDH patients, so as to provide a theoretical reference for improving the outcomes of CHD patients.
Materials and methods
Baseline data
One hundred and seventy-five patients with CHD from May 2019 to January 2020 were enrolled, and they were divided into stable angina group (SA, 60 cases), unstable angina group (UA, 60 cases) and acute myocardial infarction group (AMI, 55 cases) according to their conditions.
Inclusion criteria: (1) subjects met the diagnostic criteria for CHD in the American Guidelines for the Diagnosis and Treatment of Coronary Heart Disease [12] and showed obvious symptoms; (2) the subjects were clearly conscious and had no difficulties in communication; (3) the medical records were complete; (4) the study had been approved by the Ethics Committee of Taihe Hospital; (5) the subjects had signed the informed consent form; (6) ≥18 years old.
Exclusion criteria: (1) those combined with mental disorders or mental retardation; (2) those who had been diagnosed with other cardiovascular diseases (congenital heart disease, cardiomyopathy, etc.); (3) those who had undergone heart transplantation; (4) those with other serious medical conditions (heart failure, respiratory failure, etc.); (5) those with systemic immune system diseases or infections; (6) those who were pregnant or breastfeeding.
Elimination criteria: (1) those who were lost to follow-up; (2) those who volunteered to withdraw.
Intervention methods
Coronary artery score
Coronary angiography was performed in all subjects, and the stenosis of the left main coronary artery, left anterior descending, left circumflex and right coronary arteries was evaluated in conjunction with the imaging findings. The lesion was considered normal if there was no abnormality or <50% stenosis; A single lesion was confirmed if there was ≥50% stenosis in any of the above arteries, and a multi-branch lesion was confirmed if there was ≥50% stenosis in two or three arteries. According to the American Heart Association’s Gensini score, a score of 1 is assigned for stenosis ≤25%, 2 for 26%-50%, 4 for 51%-75%, 8 for 76%-90%, 16 for stenosis 91%-99%, and 32 for complete occlusion [13], and the final Gensini score is obtained by multiplying the stenosis score of the evaluated artery by the correlation coefficient.
GRACE score
GRACE score is a tool that can evaluate the risk and prognosis of ischemic adverse events in CHD patients, covering age, systolic blood pressure, pulse, blood creatinine and other indicators. The sum of the scores of each indicator is the GRACE score. Scores of 0-109 points represent low-risk, scores of 110-140 represent intermediate-risk, and scores of 141 and above represent high-risk [14].
Laboratory indices
Blood samples were retrieved from the cubital veins of the enrolled subjects, centrifuged, and reserved for later use. The IL-1ra levels of the blood samples are detected by enzyme-linked immunosorbent assay (ELISA). The application kits are all purchased from Shanghai Jingkang Biological Engineering Co., Ltd. The operation was carried out in strict accordance with the kit instructions. The troponin (Tn) level was analyzed with an automatic analyzer, and the average value of each index was tested 3 times, and the average value was the final result.
Statistical method
Collected data were entered into the EXCEL form with SPSS 22.0 as the data analysis tool. If the data conformed to the normal distribution, the count data were expressed as [n (%)]. Chi-square test was used for difference analysis. Measurement data were expressed as (mean ± standard deviation), t test was used for difference analysis between groups, and Spearman was used for correlation analysis. P<0.05 indicated that the difference was significant.
Results
Comparison of baseline data
General data such as sex, age, weight, BMI, etc. of patients in SA, UA and AMI groups were measured separately, and the comparison between the groups showed that there was no significant difference in the above indices among the three groups, which was comparable (P>0.05) (Table 1).
Table 1.
Comparison of baseline data (x̅ ± s)/[n (%)]
| Baseline data | SA (n=60) | UA (n=60) | AMI (n=55) | t/X2 | P | |
|---|---|---|---|---|---|---|
| Gender | Male | 37 | 34 | 32 | 0.547 | 0.362 |
| Female | 23 | 26 | 23 | |||
| Average age (years) | 49.19±3.22 | 49.35±3.41 | 48.98±3.51 | 0.036 | 0.987 | |
| Average weight (kg) | 63.38±3.43 | 63.87±3.61 | 64.01±2.87 | 0.066 | 0.917 | |
| Average BMI (kg/m2) | 23.22±2.11 | 23.19±2.01 | 23.41±2.03 | 0.871 | 0.317 | |
Comparison of the differences between Gensini score and GRACE score in patients with different conditions
As the disease condition worsened, the Gensini score and GRACE score of CHD patients showed a gradual increase, and between-group comparisons showed that the Gensini and GRACE scores in AMI group was higher than that in UA group (P<0.05). The Gensini score and GRACE score of patients in UA group was higher than that of patients in SA group (P<0.05) (Figure 1).
Figure 1.

Comparison of the differences between Gensini score and GRACE score in patients with different conditions. #Means P<0.05 in comparison with SA group, and *means P<0.05 in comparison with UA group.
Comparison of IL-1ra and Tn levels
Blood samples were collected from patients in SA, UA and AMI groups and laboratory tests were performed, and it was found that the IL-1ra and Tn levels in blood samples from CHD patients showed a gradual increase as the disease worsened. IL-1ra and Tn levels were higher in AMI group than in UA group (P<0.05), and IL-1ra and Tn levels were higher in UA group than in SA group (P<0.05) (Figure 2).
Figure 2.

Comparison of IL-1ra and Tn levels in patients with different conditions. #Means P<0.05 in comparison with SA group, and *means P<0.05 in comparison with UA group.
Comparison of Gensini score and GRACE score in CHD patients with different outcomes
The enrolled CHD patients were divided into death group (21 cases), adverse cardiovascular event group (MACE, 50 cases) and good prognosis group (104 cases) according to the clinical outcome after 30 days of follow-up. The Gensini score and GRACE score of death group were significantly higher than MACE group, and the Gensini score and GRACE score of MACE group were significantly higher than good prognosis group (P<0.05) (Figure 3).
Figure 3.

Comparison of the differences between Gensini score and GRACE score in CHD patients with different clinical outcomes. #Means P<0.05 in comparison with death group, and *means P<0.05 in comparison with MACE group.
Comparison of IL-1ra and Tn levels in CHD patients with different clinical outcomes
Patients with CHD were grouped according to clinical outcomes and laboratory tests were performed to compare the serum IL-1ra as well as Tn levels between groups (P<0.05). The IL-1ra and Tn levels were higher in death group than in MACE group, and higher in MACE group than in good prognosis group (P<0.05) (Figure 4).
Figure 4.

Comparison of IL-1ra and Tn levels in patients with different clinical outcomes. #Means P<0.05 in comparison with death group, and *means P<0.05 in comparison with MACE group.
Correlation analysis of Gensini score and GRACE score, IL-1ra and Tn levels in CHD patients
Gensini score showed a positive relationship with GRACE score (r=0.9751, P<0.05) and IL-1ra was positively correlated with the Tn level (r=0.9731, P<0.05) (Figure 5).
Figure 5.

Correlation analysis between Gensini score and GRACE score, IL-1ra and Tn level in CHD patients. Gensini score showed a positive correlation with GRACE score (r=0.9751, P<0.05) and IL-1ra showed a positive correlation with Tn level (r=0.9731, P<0.05).
The value of Gensini score and IL-1ra for poor prognosis of CHD
The area under the curve (AUC) of Gensini score was 0.9305 with 95% CI=0.8528-1.0000 (P<0.001) and of IL-1ra was 0.9499 with 95% CI=0.8942-1.0000 (P<0.001) for poor prognosis (Figure 6).
Figure 6.
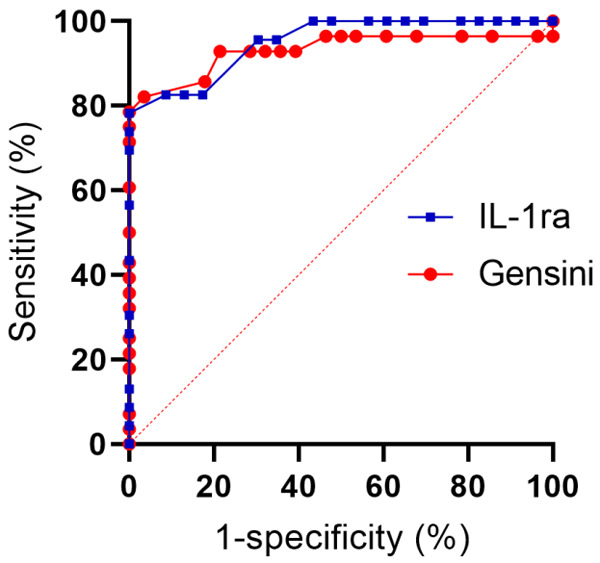
The AUC of Gensini score and IL-1ra for poor prognosis. AUC of Gensini score for poor prognosis was 0.9305 with 95% CI=0.8528-1.0000 (P<0.001) and AUC of IL-1ra for poor prognosis is 0.9499 with 95% CI=0.8942-1.0000 (P<0.001).
Discussion
CHD is a common chronic disease and its incidence will continue to rise with the aging of Chinese society and the adjustment of dietary and living patterns. Studies have shown that with the progression of individual atherosclerotic disease, CHD patients may develop various pathological symptoms such as angina, myocardial infarction, arrhythmias, and in some patients, sudden death may occur as a result of cardiac arrest. Therefore, it is important to perform early diagnosis and evaluation of CHD patients, and provide targeted clinical interventions to reduce the mortality rate [15].
There are many clinical studies on the diagnosis and prognosis evaluation of CHD patients, but the diagnostic methods may exhibite some limitations. For example, although coronary CT is a non-invasive assessment tool for CHD, it is seldom applied due to its complex procedures for operators; MRI or nuclear cardiac imaging provides myocardial metabolism, activity and the function of each chamber of the heart, it is not intuitive enough to assess coronary stenosis and is expensive as well, thus its applicability is limited [16]. Cardiac function score is a simple tool for evaluating CHD condition, with high accuracy. The clinical scales include GRACE, TIMI, ACUITY, Duke, Gensini, etc., all of which have different scope of application [16]. The Gensini score is a scale that can reflect the degree of coronary artery stenosis in subjects. It has a wide range of clinical applications. A study on the correlation between cystatin C and Gensini score found that the level of cystatin C in patients with CHD was positively correlated with Gensini score. The Gensini score of non-CHD patients is significantly lower than that of CHD patients. Gensini score, therefore, could be used to assess the condition of CHD [17,18]. Laboratory indicators are also references for the assessment of CHD patients’ condition. Tn is one marker of myocardial injury and necrosis, which has important significance for the diagnosis of acute myocardial infarction and risk stratification, with a diagnostic sensitivity of 100% and a specificity of 91% [19]. IL-1ra, a high-affinity cell receptor, has been shown to be extensively involved in inflammatory processes and is closely related to the development of CHD [20]. However, to best of our knowledge, no studies had examined the role of IL-1ra in the assessment of CHD condition and prognosis.
In this study, we found that as the condition of CHD patients worsened, the levels of Gensini score, GRACE score, IL-1ra and Tn showed a gradual increase trend, and there were significant differences between CHD patients with different conditions. A multicenter, retrospective study indicated that CHD is induced by myocardial ischemia caused by atherosclerosis. The lesion is characterized by damage or necrosis of cardiomyocytes, and as the disease worsens in patients with CHD, the symptoms of coronary artery occlusion become more prominent, which directly affects the Gensini score and GRACE score [21]. Another study conducted on CHD patients showed that the pathological process of CHD is actually closely related to the inflammatory response. The stronger the inflammatory response, the faster the disease progresses. That study believed that the level of serum inflammatory factors could also be used to assess the condition of patients with CHD [22]. We believed the IL-1ra and Tn levels have a theoretical basis for evaluating the condition of CHD patients.
There was a significant positive correlation between the above indicators (r=0.9751, r=0.9731, P<0.05), and it was pointed out that GRACE score is a clinical tool for risk stratification of CHD, which is useful in guiding treatment strategies as well as the timing of interventions. Several clinical treatment guidelines, including the 2015 ESC NSTE-ACS Management Guidelines and the NSTE-ACS Diagnosis and Treatment Guidelines (2016), have now used GRACE score as a tool for risk stratification and assessment of CHD [23,24]. The positive correlation between the Gensini score and the GRACE score suggests that the Gensini score also has good application value in the assessment of CHD condition and prognosis, and we found that the AUC of the Gensini score for poor prognosis of CHD was 0.9305, suggesting its high sensitivity. Tn is now widely used in clinical practice as a marker of myocardial injury and necrosis, and a study of 90 patients with asymptomatic CHD showed that tracking Tn levels in patients with CHD can help assess the disease condition, facilitate revision of clinical measures, and improve patient outcomes [25]. We speculated that Tn is a kind of myocardial specific antigen, which is widely found in the cardiac and skeletal muscle of individuals, and when individuals have ischemic necrosis, Tn will enter the intercellular matrix from the myocardium and could be used as a specific indicator for assessing myocardial injury [26], which is evidenced by the Tn levels in CHD patients with different conditions and clinical outcomes.
In summary, Gensini score and IL-1ra indicated the severity of CHD and can be used in the prognosis prediction of CHD patients, which is worthy of clinical promotion and application. The innovation of this study, the demonstration of the feasibility of Gensini score and IL-1ra on the assessment of CHD patients’ condition and prognosis provides a clinical reference for the subsequent studies on CHD patients. The shortcoming of this study is that the effects of Gensini score and IL-1ra on the long-term prognosis of patients with CHD was not analyzed, and need further investigation.
Disclosure of conflict of interest
None.
References
- 1.Anderson JL, Morrow DA. Acute myocardial infarction. N Engl J Med. 2017;376:2053–2064. doi: 10.1056/NEJMra1606915. [DOI] [PubMed] [Google Scholar]
- 2.Thiele H, Akin I, Sandri M, Fuernau G, de Waha S, Meyer-Saraei R, Nordbeck P, Geisler T, Landmesser U, Skurk C, Fach A, Lapp H, Piek JJ, Noc M, Goslar T, Felix SB, Maier LS, Stepinska J, Oldroyd K, Serpytis P, Montalescot G, Barthelemy O, Huber K, Windecker S, Savonitto S, Torremante P, Vrints C, Schneider S, Desch S, Zeymer U. PCI strategies in patients with acute myocardial infarction and cardiogenic shock. N Engl J Med. 2017;377:2419–2432. doi: 10.1056/NEJMoa1710261. [DOI] [PubMed] [Google Scholar]
- 3.Wongcharoen W, Sutthiwutthichai S, Gunaparn S, Phrommintikul A. Is non-HDL-cholesterol a better predictor of long-term outcome in patients after acute myocardial infarction compared to LDL-cholesterol? A retrospective study. BMC Cardiovasc Disord. 2017;17:10. doi: 10.1186/s12872-016-0450-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cafagna G, Seghieri C. Educational level and 30-day outcomes after hospitalization for acute myocardial infarction in Italy. BMC Health Serv Res. 2017;17:18. doi: 10.1186/s12913-016-1966-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Smolderen KG, Spertus JA, Gosch K, Dreyer RP, D’Onofrio G, Lichtman JH, Geda M, Beltrame J, Safdar B, Bueno H, Krumholz HM. Depression treatment and health status outcomes in young patients with acute myocardial infarction: insights from the VIRGO study (variation in recovery: role of gender on outcomes of young AMI patients) Circulation. 2017;135:1762–1764. doi: 10.1161/CIRCULATIONAHA.116.027042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Krumholz HM, Hennen J, Ridker PM, Murillo JE, Wang Y, Vaccarino V, Ellerbeck EF, Radford MJ. Use and effectiveness of intravenous heparin therapy for treatment of acute myocardial infarction in the elderly. J Am Coll Cardiol. 1998;31:973–979. doi: 10.1016/s0735-1097(98)00022-9. [DOI] [PubMed] [Google Scholar]
- 7.Lellouche F, Simon M, L’Her E. Oxygen therapy in suspected acute myocardial infarction. N Engl J Med. 2018;378:201. doi: 10.1056/NEJMc1714937. [DOI] [PubMed] [Google Scholar]
- 8.Hofmann R, Svensson L, James SK. Oxygen therapy in suspected acute myocardial infarction. N Engl J Med. 2018;378:201–202. doi: 10.1056/NEJMc1714937. [DOI] [PubMed] [Google Scholar]
- 9.Mohammadi R, Khodakarim S, Alipour A, Bitaraf E, Soori H. Association between air temperature and acute myocardial infarction hospitalizations in Tehran, Iran: a time-stratified case-crossover. Int J Occup Environ Med. 2017;8:143–152. doi: 10.15171/ijoem.2017.1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tung YC, Chang GM, Chang HY, Yu TH. Relationship between early physician follow-up and 30-day readmission after acute myocardial infarction and heart failure. PLoS One. 2017;12:e0170061. doi: 10.1371/journal.pone.0170061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Al-Lamee R, Thompson D, Dehbi HM, Sen S, Tang K, Davies J, Keeble T, Mielewczik M, Kaprielian R, Malik IS, Nijjer SS, Petraco R, Cook C, Ahmad Y, Howard J, Baker C, Sharp A, Gerber R, Talwar S, Assomull R, Mayet J, Wensel R, Collier D, Shun-Shin M, Thom SA, Davies JE, Francis DP. Percutaneous coronary intervention in stable angina (ORBITA): a double-blind, randomised controlled trial. Lancet. 2018;391:31–40. doi: 10.1016/S0140-6736(17)32714-9. [DOI] [PubMed] [Google Scholar]
- 12.Lassen JF, Burzotta F, Banning AP, Lefèvre T, Darremont O, Hildick-Smith D, Chieffo A, Pan M, Holm NR, Louvard Y, Stankovic G. Percutaneous coronary intervention for the left main stem and other bifurcation lesions: 12th consensus document from the European Bifurcation Club. EuroIntervention. 2018;13:1540–1553. doi: 10.4244/EIJ-D-17-00622. [DOI] [PubMed] [Google Scholar]
- 13.Metz L, Thivel D, Peirrera B, Richard R, Julian V, Duclos M. A new equation based on the 6-min walking test to predict VO2peak in women with obesity. Disabil Rehabil. 2018;40:1702–1707. doi: 10.1080/09638288.2017.1304582. [DOI] [PubMed] [Google Scholar]
- 14.Zannad F, Ferreira JP. Reply: cardiopulmonary exercise testing versus 6-min walk test as clinically meaningful endpoints in HF trials. J Am Coll Cardiol. 2017;69:2252. doi: 10.1016/j.jacc.2017.01.065. [DOI] [PubMed] [Google Scholar]
- 15.Wang Z, Wang L, Su X, Pu J, Jiang M, He B. Rational transplant timing and dose of mesenchymal stromal cells in patients with acute myocardial infarction: a meta-analysis of randomized controlled trials. Stem Cell Res Ther. 2017;8:21. doi: 10.1186/s13287-016-0450-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gao L, Liu Y, Guo S, Yao R, Wu L, Xiao L, Wang Z, Liu Y, Zhang Y. Circulating long noncoding RNA HOTAIR is an essential mediator of acute myocardial infarction. Cell Physiol Biochem. 2017;44:1497–1508. doi: 10.1159/000485588. [DOI] [PubMed] [Google Scholar]
- 17.Ambavane A, Lindahl B, Giannitsis E, Roiz J, Mendivil J, Frankenstein L, Body R, Christ M, Bingisser R, Alquezar A, Mueller C TRAPID-AMI investigators. Correction: economic evaluation of the one-hour rule-out and rule-in algorithm for acute myocardial infarction using the high-sensitivity cardiac troponin T assay in the emergency department. PLoS One. 2018;13:e0191348. doi: 10.1371/journal.pone.0191348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Burzotta F, Lassen JF, Banning AP, Lefèvre T, Hildick-Smith D, Chieffo A, Darremont O, Pan M, Chatzizisis YS, Albiero R, Louvard Y, Stankovic G. Percutaneous coronary intervention in left main coronary artery disease: the 13th consensus document from the European Bifurcation Club. EuroIntervention. 2018;14:112–120. doi: 10.4244/EIJ-D-18-00357. [DOI] [PubMed] [Google Scholar]
- 19.Lindholm D, Alfredsson J, Angerås O, Böhm F, Calais F, Koul S, Lagerqvist B, Renlund H, Sarno G, Varenhorst C. Timing of percutaneous coronary intervention in patients with non-ST-elevation myocardial infarction: a SWEDEHEART study. Eur Heart J Qual Care Clin Outcomes. 2017;3:53–60. doi: 10.1093/ehjqcco/qcw044. [DOI] [PubMed] [Google Scholar]
- 20.Papapostolou S, Andrianopoulos N, Duffy SJ, Brennan AL, Ajani AE, Clark DJ, Reid CM, Freeman M, Sebastian M, Selkrig L, Yudi MB, Noaman SQ, Chan W. Long-term clinical outcomes of transient and persistent no-reflow following percutaneous coronary intervention (PCI): a multicentre Australian registry. EuroIntervention. 2018;14:185–193. doi: 10.4244/EIJ-D-17-00269. [DOI] [PubMed] [Google Scholar]
- 21.Poder TG, Erraji J, Coulibaly LP, Koffi K. Percutaneous coronary intervention with second-generation drug-eluting stent versus bare-metal stent: systematic review and cost-benefit analysis. PLoS One. 2017;12:e0177476. doi: 10.1371/journal.pone.0177476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Psotka MA, Schiller NB, Whooley MA, Mishra RK. Association of change in 5-year N-terminal fragment of the prohormone brain-type natriuretic peptide with left ventricular structure and function in stable coronary disease. J Cardiovasc Med (Hagerstown) 2018;19:67–72. doi: 10.2459/JCM.0000000000000613. [DOI] [PubMed] [Google Scholar]
- 23.Yan W, Li RJ, Jia Q, Mu Y, Liu CL, He KL. Neutrophil-to-lymphocyte ratio compared to N-terminal pro-brain natriuretic peptide as a prognostic marker of adverse events in elderly patients with chronic heart failure. J Geriatr Cardiol. 2017;14:127–134. doi: 10.11909/j.issn.1671-5411.2017.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Khan A, Phadke M, Lokhandwala YY, Nathani PJ. A study of prehospital delay patterns in acute myocardial infarction in an urban tertiary care institute in Mumbai. J Assoc Physicians India. 2017;65:24–27. [PubMed] [Google Scholar]
- 25.Bourron O, Le Bouc Y, Berard L, Kotti S, Brunel N, Ritz B, Leclercq F, Tabone X, Drouet E, Mulak G, Danchin N, Simon T. Impact of age-adjusted insulin-like growth factor 1 on major cardiovascular events after acute myocardial infarction: results from the fast-MI registry. J Clin Endocrinol Metab. 2015;100:1879–1886. doi: 10.1210/jc.2014-3968. [DOI] [PubMed] [Google Scholar]
- 26.Westermann C, Wendeler D, Nienhaus A. Hepatitis C in healthcare personnel: secondary data analysis of therapies with direct-acting antiviral agents. J Occup Med Toxicol. 2018;13:16. doi: 10.1186/s12995-018-0197-6. [DOI] [PMC free article] [PubMed] [Google Scholar]


