Abstract
Objective: The effects of continuing nursing care under cognitive behavioral intervention on the psychological state and living quality of patients with double J catheter after ureterolithiasis surgery were analyzed in this research. Methods: The research subjects in this study were 142 patients who were discharged from our hospital with a double J tube after ureterolithiasis surgeries from June 2019 to June 2020. According to the patient care plan, the subjects were divided into the control group (n=71) and the observation group (n=71) and respectively treated with routine basic nursing measures and continuing nursing care under cognitive-behavior intervention. Subsequently, the psychological state, living quality and the complications that occurred were compared between the two groups. Results: The depression and anxiety scores of the two groups after 4 weeks of intervention, comparing to thoes before intervention, were seen with remarkably decreased significance (P<0.05). The scores of living quality and self-care quality of patients in the observation group were obviously higher than those in the control group (P<0.05). In addition, the incidence of complications in the observation group was critically lower than that in control group (P<0.05). Conclusion: Continuous nursing care under cognitive behavioral intervention can substantially improve the psychological state, living quality and self-care ability of patients with double J tube after ureterolithiasis surgery, and reduce the incidence of complications, which is worthy of clinic promotion.
Keywords: Cognitive behavior intervention, continuing nursing care, ureterolithiasis, double J catheter after ureterolithiasis surgery, psychological state, living quality
Introduction
Ureterolithiasis is a common disease in urology, and most of patients are young adults. The clinical symptoms of ureterolithiasis include lumbar and abdominal colic, nausea, and hematuria, etc., which pose serious threats to the physical and mental health of patients [1]. The basic treatment of ureterolithiasis at present is surgical treatment, and its therapeutic effect is remarkable. In order to promote urine discharge, avoid tissue adhesion, and prevent ureteral blockage, a double J catheter needs to be indwelled in the body and kept for 1 to 3 months [2,3]. However, a number of studies have found that patients with double J catheters after ureterolithiasis surgery may still encounter the irritation of the bladder, such as frequent, urgent and painful urination, and are at risk of complications such as waist pain, macroscopic hematuria, and catheter displacement. In addition, most patients with a double J tube after surgery usually are accompanied by poor mental states like depression or anxiety, and these psychological emotions may seriously affect the health and rehabilitation quality of patients [4-6]. Therefore, it is very necessary to find an effective nursing measure to reduce the risk of complications and improve the psychological state of patients during home recuperation after discharge. Cognitive behavioral intervention is a method of psychotherapy, which is widely used to treat psychiatric diseases of depression, anxiety, etc. Cognitive behavioral intervention can achieve desired therapeutic effects by changing the patients’ understanding of the disease and providing relaxation therapy [7]. In this study, the impacts of continuing nursing care under cognitive behavioral intervention on psychological state and living quality of patients with double J catheter after ureterolithiasis surgery was focused upon and researched, with the detailed report as follows.
Materials and methods
Research subjects
Retrospective analysis was used in this study. The subjects of the study were 142 patients discharged from our hospital with a double J catheter after ureterolithiasis surgery during June 2019 to June 2020. The subjects included 79 males and 63 females, with an average age of (42.37±5.51) years old. The course of disease was between 3-11 d, with an average course of (7.26±2.13) d. The position of the catheter was left in 80 patients and right in 62 patients. According to the patient care plan, the patients were divided into an observation group (n=71) and a control group (n=71). The study was carried out with the approval of our hospital ethics committee.
Inclusion and exclusion criteria
Inclusion criteria: (1) All the subjects included met the diagnostic criteria in The Chinese Guidelines for The Diagnosis and Treatment of Urological Diseases, and were confirmed as having ureteral calculus by imaging examinations of color Doppler ultrasound and CT [8], which was consistent with the indications of surgical treatment; (2) All patients successfully completed the surgery and were placed with the double J catheter; (3) No tube infection or other complications occurred before the patients were discharged from the hospital; and (4) Patients and their family members voluntarily participated in this study and signed the informed consent.
Exclusion criteria: (1) Patients with multiple or complex ureterolithiasis were excluded; (2) Patients with ureteral complications were excluded; (3) Those who were accompanied by mental illness, disturbance of consciousness or cognitive function were excluded; or (4) Patients unable to cooperate with medical staff for intervention treatment were excluded.
Methods
The control-group patients were treated with conventional nursing measures, and were informed in detail of nursing measures, precautions, follow-up time, and the estimated extubation time before they were discharged. The observation-group patients received continuing nursing care under cognitive behavior intervention, and the specific methods were as follows: (1) Under the cognitive behavior intervention, a continuing nursing group that consisting of 1 head nurse, 2 in charge nurses, 3 nurses, 3 health instructors and 2 follow-up personnel was established. The head nurse was responsible for the training of team members, and developed a scientific and standardized nursing process in line with the patients’ individual conditions. The team members implemented the scientific and standardized division of labor to ensure the standardization of the whole workflow. (2) The personal information file of patients was established to record the basic information of patient’s name, disease condition and contact information. We informed the patients of the importance of post-discharge care, kept in close contact with them, and reported their situation to the hospital in real time. (3) A WeChat group of patients was established, and health instructors and follow-up personnel were arranged to take turns to answer patients’ questions online. At the same time, we regularly introduced to patients the causes and nursing measures of complications that may occur after surgery through WeChat groups, thus to prevent patients from encountering negative emotions such as fear, tension, and anxiety that may affect their confidence in treatment due to complications. (4) Cognitive intervention. Through active communication with the patients before discharge, we can mastered their cognition and psychological state of the disease. We designed intervention programs for patients with different problems, and actively answered their questions to eliminate doubts to enhance their confidence in conquering the disease. (5) When patients were discharged from the hospital, we informed them of the predictive nursing measures and precautions for various complications through oral instruction and manuals, which included: a. Predictive care measures for bladder irritation: patients should keep good living habit, increase drinking water, eat more fresh vegetables and fruits, and maintain good urinary habit by a standing position. Patients should avoid holding back urine to prevent reflux. If the patient has urination pain, frequent urination and urgency during recuperation, it is necessary to increase the amount of water and reduce the activity, so that the symptoms can be alleviated or eliminated. If the symptoms persist, seek medical treatment right away. b. Nursing care of swelling and pain of the waist. The predictive nursing measures should be taken in view of the possibility of swelling and pain of the waist in patients. We recommended patients to drink and urinate reasonably to keep the urethra unobstructed, avoid holding urine, compression or twisting of the pipeline. In the case of back pain, patients should avoid bending the waist, but can rest in lateral position instead. c. The predictive nursing measures for hematuria were as follows: We encouraged the patients to drink plenty of water to dilute the urine, flush the urethra, and observe their urine volume and urine color. Patients should increase the amount of water if the urine is red. If the symptoms were not alleviated or even worsened after measures were taken, they should seek medical advice immediately. d. Predictive nursing measures for double J catheter displacement. We instructed the patients to avoid heavy physical activity or sudden squatting during the recovery period. Meanwhile, they were not to extend the limbs and waist to avoid the displacement of double J catheter caused by body movements. They were also informed to conduct follow-ups regularly, and seek medical treatment in time in case of accident. e. The predictive nursing measures of urinary tract infection were as follows: We informed the patients to keep the dressing dry and clean, and instructed them on skin cleaning and the judgement of urinary tract infection. If this situation happens, the patients should seek medical attention immediately. (7) A telephone follow-up was conducted 4 weeks after discharge. We comprehensively recorded the patients’ psychological state, living quality and complications to fully understand the patients’ recovery, and promptly informed them to seek medical treatment once there was any situation.
Observation of indexes
Psychological state: We adopted the self-rating depression Scale (SDS) [9] and self-rating anxiety scale (SAS) [10], and evaluated the psychological states of depression and anxiety before and 4 weeks after the intervention in discharged patients with double J catheter after ureterolithiasis surgery. A higher score of patient represented a worse psychological state.
Quality of life: We followed up the patients’ quality of life with SF-36 [11] via telephone four weeks after discharge. The scale contained 8 dimensions, including physiological function (PF), physiological function (RP), physical pain (BP), general health status (GH), energy (VT), social function (SF), emotional function (RE), mental health (MH), with a total of 36 items. A higher score in the 8 dimensions represented a better the quality of life of patients, and the average score was used as the overall quality of life.
Self-care quality. We conducted telephone follow-ups at 4 weeks after the patients’ discharge and applied the self-designed self-care quality rating scale for evaluation. The scale included three aspects of daily nursing procedures, basic knowledge of catheter care and preventive measures for complications, with a full score of 100 points. A higher score of the patients revealed a higher quality of self-care of discharged patients.
The complications of the two groups of patients were compared.
We applied our self-developed nursing satisfaction scale to score the patients’ satisfaction with nursing 4 weeks after discharge. The scale consisted of 20 items, each of which was scored from 1 to 5 points with a total score of 100 points. A higher score of the scale referred to a higher satisfaction of patients with nursing care.
Statistical analysis
The handling and processing of data was conducted by statistical tool SPSS 25.0. The measurement data were expressed by (x̅±s), the comparison between groups was by t-test of independent samples, the count data was expressed by percentage, and the result was expressed by χ2 test. P<0.05 was regarded as a statistically significant difference.
Results
Clinical materials
There was no statistically significant difference between the two groups in terms of gender, age, course of disease or other general data (P>0.05), as shown in Table 1.
Table 1.
Comparison of general data between the two groups
| Item | Control group (n=71) | Observation group (n=71) | χ2/t | P |
|---|---|---|---|---|
| Gender (M/F, cases) | 38/33 | 41/30 | 0.2568 | 0.6123 |
| Age (x̅±s, years old) | 41.59±4.96 | 43.15±6.06 | 1.6786 | 0.0955 |
| Courses of disease | 7.04±2.05 | 6.58±2.21 | 1.2858 | 0.2006 |
| Position of catheter (L/R, number of cases) | 42/29 | 38/33 | 0.4581 | 0.4985 |
Comparison of changes in psychological state of the two groups of patients before and after intervention
The depression and anxiety scores of the two groups after 4 weeks of intervention, compared to before intervention, were seen with a remarkable decrease (P<0.05), and the decrease in the observation group was remarkably greater than that in the control group (P<0.05) (Table 2 and Figure 1).
Table 2.
Comparison of changes in psychological state in two groups of patients before and after intervention (x̅±s, points)
| Group | SDS | SAS | ||||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| Before intervention | After intervention | t | P | Before intervention | After intervention | t | P | |
| Control group (n=71) | 52.33±5.24 | 49.15±4.72 | 3.7995 | <0.001 | 55.01±6.23 | 50.13±5.51 | 4.9440 | 0.0000 |
| Observation group (n=71) | 52.41±5.76 | 44.34±3.17 | 10.3246 | <0.001 | 55.12±6.14 | 47.88±3.75 | 8.4793 | 0.0000 |
| T | 0.0866 | 7.1284 | - | - | 0.1060 | 2.8445 | - | - |
| P | 0.9311 | 0.0000 | - | - | 0.9158 | 0.0051 | - | - |
Figure 1.
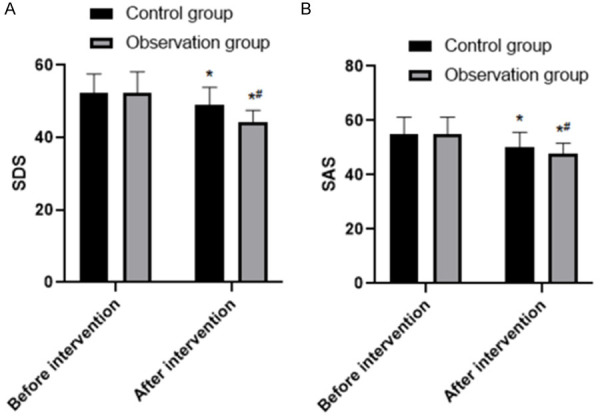
Comparison of SDS and SAS scores between the two groups before and after treatment. Note: Compare with before intervention, *P<0.05; Compare with control group, #P<0.05. A: SDS scores; B: SAS sores.
Comparison of living quality scores and self-care quality scores of both groups of patients 4 weeks after discharge
The score of living quality in the observation group was obviously higher than that in the control group [(108.22±6.84) points, (91.48±5.76) points, t=15.7739, P=0.0000]. The score of self-care quality in the observation group was substantially higher than which in the control group [(92.77±3.63) points, (84.52±3.15) points, t=14.4638, P=0.0000], and each dimension score of SF-36 in observation group was also substantially higher than that in control group (P<0.05), with details listed in Table 3 and Figure 2.
Table 3.
Comparison of living quality and self-care quality of the two groups of patients 4 weeks after discharge
| Group | Score of living quality | Self-care quality |
|---|---|---|
| Control group (n=71) | 64.48±5.76 | 84.52±3.15 |
| Observation group (n=71) | 71.22±6.84 | 92.77±3.63 |
| t | 6.3510 | 14.4638 |
| P | <0.001 | <0.001 |
Figure 2.
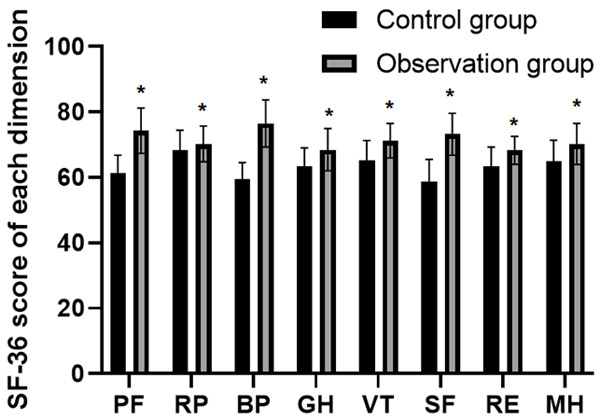
Comparison of SF-36 scores between the two groups 4 weeks after discharge. Note: Compare with control group, *P<0.05.
Comparison of complications between the two groups
The incidence of complications in the observation group was critically lower than that in control group, and the difference was statistically significant (11.27%, 29.58%, χ2=7.3232, P=0.0068), as shown in Table 4.
Table 4.
Comparison of complications between the two groups [number of cases, (%)]
| Group | Bladder irritation | Swelling and pain of waist | Hematuria | Displacement of Double J catheter | Urinary tract infection | Overall incidence |
|---|---|---|---|---|---|---|
| Control group (n=71) | 4 (5.63) | 5 (7.04) | 4 (5.63) | 2 (2.82) | 6 (8.45) | 21 (29.58) |
| Observation group (n=71) | 2 (2.82) | 1 (1.41) | 2 (2.82) | 0 (0) | 3 (4.22) | 8 (11.27) |
| χ2 | - | - | - | - | - | 7.3232 |
| P | - | - | - | - | - | 0.0068 |
Comparison of satisfaction with nursing
The score of nursing satisfaction in the observation group 4 weeks after discharge was obviously higher than that in control group [(91.27±6.31) points, (85.47±9.32) points, t=4.3422, P=0.000].
Discussion
Most ureteral calculi, which caused by the falling of breakstones in the renal calculi or the extracorporeal ultrastructure, coming from the kidney [12]. According to the epidemiological statistics, the high incidence of ureterolithiasis is in young adults aged between 20 and 40, and the prone site is the lower ureter, accounting for about 50% to 60% of the total cases [13,14]. Patients with ureteral calculi often seek out medical treatment due to symptoms of macroscopic hematuria or pain, and those who go untreated may experience renal obstruction or dilation. For severe cases, it may even cause the gradual loss of renal function. Therefore, it is of huge importance for a prompt and effective treatment. At present, the primary methods for ureteral calculi include symptomatic treatment, traditional Chinese medicine treatment, extracorporeal ultrastructure, ureteroscopy and laparotomy [15]. The periods of postoperative recovery and hospitalization of patients with ureterolithiasis have been greatly shortened. However, with the shortening of hospital stay, the probability of patients with bladder irritation, swelling and pain of waist, hematuria, displacement of double-J catheter, urinary tract infection and other related complications has increased [16,17]. The main reason is that in traditional nursing care, patients receive corresponding nursing intervention only when they are hospitalized. However, the lack of self-care awareness after discharge and the failure to perform nursing care as required will result in complications for the patient [18]. In addition, some discharged patients with double J catheter after ureterolithiasis surgery may suffer from adverse psychological states of depression or anxiety due to the appearance of the indwelling tube [19]. Studies have confirmed that these adverse psychological states may lead to the decline of the bodily immunity, and greatly affects the clinical results of patients, which is not conducive to the recovery of disease [20]. Meanwhile, such psychological burdens are largely related to economic pressure, family and social responsibilities, and suffering from the disease by patients. Therefore, it is of particular importance to conduct continuing nursing care with cognitive behavior to such patients, as it provides a more comprehensive and regular nursing intervention for them during home rehabilitation.
Cognitive behavioral intervention is a kind of psychological intervention used to solve various physical and psychological problems of patients. It improves the patient’s negative mood by correcting their wrong cognition of disease and behavior. The Guidelines of American Psychiatric Association clearly point out the need for cognitive behavior intervention, which has a significant effect on patients with anxiety and depression [22,23]. At present, cognitive behavioral intervention has been widely extended in patients with hemodialysis [24] and malignant tumors [25,26], which has significantly improved their negative psychological state and living quality. Continuing nursing care is a type of new nursing model that effectively extends the inpatient nursing care to the discharged period. The continuing nursing care under cognitive behavioral intervention is a combination of psychological intervention and physiological nursing measures. It ensures the patients receive enough continuing nursing care during recuperation at home, thus accelerating the recovery progress and reducing the probability of disease deterioration and the incidence of complications [27]. In this study, the depression and anxiety scores of the two groups after 4 weeks of intervention were apparently lower than in prior-intervention, and the decline in the observation group was greater than in the control group, indicating that continuing nursing care under cognitive behavioral intervention can evidently improve the adverse psychological states of patients. We analyzed this and found that the possible reason was that the continuing nursing care under cognitive behavior intervention was helpful for medical staff to establish a good relationship with patients. By communicating with patients, we helped them adjust their negative psychology and timely correct their misunderstandings of disease. The scores of living quality and self-care quality of patients in the observation group were obviously higher than those in the control group, and the incidence of complications in the observation group was critically lower than that in the control group, suggesting that continuing nursing care under cognitive behavioral intervention can dramatically improve the living and self-care quality of patients, and in the meantime reduce their incidence of complications. We have analyzed the reason for the improvement, and found that it lies in the enhanced mastering of patients’ knowledge of post-operative care on catheters and the prevention and treatment of possible complications through a number of ways.
However, there may be a certain deviations in the research results due to the limited sample size. In addition, due to the relatively short observation period, its long-term effects on patients are unclear. It is suggested to further expand the sample size and observe the long-term effects on patients after surgery in later studies.
To conclude, the continuing nursing care under cognitive behavioral intervention can dramatically improve the psychological state, living quality and self-care ability of discharged patients with double J tube after ureterolithiasis surgery, and reduce the incidence of complications, which is worthy of clinic promotion.
Disclosure of conflict of interest
None.
References
- 1.Liu XJ, Wen JG, Wan YD, Hu BW, Wang QW, Wang Y. Role of silodosin as medical expulsive therapy in ureteral calculi: a meta-analysis of randomized controlled trials. Urolithiasis. 2018;46:211–218. doi: 10.1007/s00240-017-0974-1. [DOI] [PubMed] [Google Scholar]
- 2.Bercovich E, Leiderman M, Beck-Razi N, Gaitini D, Javitt M. Ultrasound-unenhanced CT fusion for detection and localization of ureteral stones. AJR Am J Roentgenol. 2018;210:W8–W11. doi: 10.2214/AJR.17.17840. [DOI] [PubMed] [Google Scholar]
- 3.Alevizopoulos A, Zosimas D, Piha L, Hanna M, Charitopoulos K. Managing small ureteral stones: a retrospective study on follow-up, clinical outcomes and cost-effectiveness of conservative management vs. early surgery. Curr Urol. 2016;9:36–43. doi: 10.1159/000442849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Faw C, Wan J, Hollingsworth JM, Ambani SN, Ghani KR, Roberts WW, Dauw CA. Impact of the timing of ureteral stent placement on outcomes in patients with obstructing ureteral calculi and presumed infection. J Endourol. 2019;33:736–740. doi: 10.1089/end.2019.0138. [DOI] [PubMed] [Google Scholar]
- 5.Dell’Atti L, Papa S. Ten-year experience in the management of distal ureteral stones greater than 10 mm in size. G Chir. 2016;37:27–30. doi: 10.11138/gchir/2016.37.1.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chertack N, Jain R, Monga M, Noble M, Sivalingam S. Two are no different than one: ureteral duplication appears to have no effect on ureteroscopy outcomes. J Endourol. 2018;32:692–697. doi: 10.1089/end.2018.0041. [DOI] [PubMed] [Google Scholar]
- 7.Ellison JS, Merguerian PA, Fu BC, Holt SK, Lendvay TS, Gore JL, Shnorhavorian M. Follow-up imaging after acute evaluations for pediatric nephrolithiasis: trends from a National database. J Pediatr Urol. 2018;14:525–531. doi: 10.1016/j.jpurol.2018.04.019. [DOI] [PubMed] [Google Scholar]
- 8.Yadav SS, Aggarwal SP, Mathur R, Sharma KK, Yadav RG, Tomar V, Teli RD, Jain D. Pediatric percutaneous nephrolithotomy-experience of a tertiary care center. J Endourol. 2017;31:246–254. doi: 10.1089/end.2015.0842. [DOI] [PubMed] [Google Scholar]
- 9.May PC, Hsi RS, Tran H, Stoller ML, Chew BH, Chi T, Usawachintachit M, Duty BD, Gore JL, Harper JD. The morbidity of ureteral strictures in patients with prior ureteroscopic stone surgery: multi-institutional outcomes. J Endourol. 2018;32:309–314. doi: 10.1089/end.2017.0657. [DOI] [PubMed] [Google Scholar]
- 10.Farrell MR, Papagiannopoulos D, Ebersole J, White G, Deane LA. Perinephric fat stranding is associated with elevated creatinine among patients with acutely obstructing ureterolithiasis. J Endourol. 2018;32:891–895. doi: 10.1089/end.2018.0252. [DOI] [PubMed] [Google Scholar]
- 11.Tran TY, Bamberger JN, Blum KA, Parkhomenko E, Thai J, Chandhoke RA, Gupta M. Predicting the impacted ureteral stone with computed tomography. Urology. 2019;130:43–47. doi: 10.1016/j.urology.2019.04.020. [DOI] [PubMed] [Google Scholar]
- 12.Marchini GS, Torricelli FC, Batagello CA, Monga M, Vicentini FC, Danilovic A, Srougi M, Nahas WC, Mazzucchi E. A comprehensive literature-based equation to compare cost-effectiveness of a flexible ureteroscopy program with single-use versus reusable devices. Int Braz J Urol. 2019;45:658–670. doi: 10.1590/S1677-5538.IBJU.2018.0880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Scotland KB, Hubosky SG, Tanimoto R, Cooper R, Healy KA, Bagley DH. Simultaneous bilateral ureteral calculi: a new paradigm for management. Urology. 2018;118:30–35. doi: 10.1016/j.urology.2018.03.052. [DOI] [PubMed] [Google Scholar]
- 14.Portis JL, Neises SM, Portis AJ. Pain is independent of stone burden and predicts surgical intervention in patients with ureteral stones. J Urol. 2018;200:597–603. doi: 10.1016/j.juro.2018.04.075. [DOI] [PubMed] [Google Scholar]
- 15.Lee MH, Lee IJ, Kim TJ, Lee SC, Jeong CW, Hong SK, Byun SS, Oh JJ. The effect of short-term preoperative ureteral stenting on the outcomes of retrograde intrarenal surgery for renal stones. World J Urol. 2019;37:1435–1440. doi: 10.1007/s00345-018-2519-9. [DOI] [PubMed] [Google Scholar]
- 16.Khatami A, Rosengren K. Reduced time from diagnosis to stone-free status in patients with ureteral calculi. Int J Health Care Qual Assur. 2016;29:276–287. doi: 10.1108/IJHCQA-03-2015-0028. [DOI] [PubMed] [Google Scholar]
- 17.Boulalas I, De Dominicis M, Defidio L. Semirigid ureteroscopy prior retrograde intrarenal surgery (RIRS) helps to select the right ureteral access sheath. Arch Ital Urol Androl. 2018;90:20–24. doi: 10.4081/aiua.2018.1.20. [DOI] [PubMed] [Google Scholar]
- 18.Fani P, Patlas MN, Monteiro S, Katz DS. Non-contrast MDCT for ureteral calculi and alternative diagnoses: yield in adult women vs in adult men. Curr Probl Diagn Radiol. 2019;48:148–151. doi: 10.1067/j.cpradiol.2018.01.009. [DOI] [PubMed] [Google Scholar]
- 19.Kaler KS, Safiullah S, Lama DJ, Parkhomenko E, Okhunov Z, Ko YH, Huynh L, Patel RM, Landman J, Clayman RV. Medical impulsive therapy (MIT): the impact of 1 week of preoperative tamsulosin on deployment of 16-French ureteral access sheaths without preoperative ureteral stent placement. World J Urol. 2018;36:2065–2071. doi: 10.1007/s00345-018-2336-1. [DOI] [PubMed] [Google Scholar]
- 20.Picozzi SC, Marenghi C, Casellato S, Ricci C, Gaeta M, Carmignani L. Management of ureteral calculi and medical expulsive therapy in emergency departments. J Emerg Trauma Shock. 2011;4:70–76. doi: 10.4103/0974-2700.76840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sridharan K, Sivaramakrishnan G. Efficacy and safety of alpha blockers in medical expulsive therapy for ureteral stones: a mixed treatment network meta-analysis and trial sequential analysis of randomized controlled clinical trials. Expert Rev Clin Pharmacol. 2018;11:291–307. doi: 10.1080/17512433.2018.1424537. [DOI] [PubMed] [Google Scholar]
- 22.Koo KC, Yoon JH, Park NC, Lee HS, Ahn HK, Lee KS, Kim DK, Cho KS, Chung BH, Hong CH. The impact of preoperative alpha-adrenergic antagonists on ureteral access sheath insertion force and the upper limit of force required to avoid ureteral mucosal injury: a randomized controlled study. J Urol. 2018;199:1622–1630. doi: 10.1016/j.juro.2017.09.173. [DOI] [PubMed] [Google Scholar]
- 23.Modi PK, Kwon YS, Davis RB, Elsamra SE, Dombrovskiy V, Olweny EO. Pediatric hospitalizations for upper urinary tract calculi: epidemiological and treatment trends in the United States, 2001-2014. J Pediatr Urol. 2018;14:13. doi: 10.1016/j.jpurol.2017.09.001. [DOI] [PubMed] [Google Scholar]
- 24.Silay MS, Ellison JS, Tailly T, Caione P. Update on urinary stones in children: current and future concepts in surgical treatment and shockwave lithotripsy. Eur Urol Focus. 2017;3:164–171. doi: 10.1016/j.euf.2017.07.005. [DOI] [PubMed] [Google Scholar]
- 25.Mohey A, Alhefnawy M, Mahmoud M, Gomaa R, Soliman T, Ahmed S, Noureldin YA. Fluoroless-ureteroscopy for definitive management of distal ureteral calculi: randomized controlled trial. Can J Urol. 2018;25:9205–9209. [PubMed] [Google Scholar]
- 26.Kane TD. Ureteroscopy for urinary calculi with or without ureteral stents. Am J Nurs. 2020;120:69. doi: 10.1097/01.NAJ.0000662840.58258.75. [DOI] [PubMed] [Google Scholar]
- 27.Hernandez N, Song Y, Noble VE, Eisner BH. Predicting ureteral stones in emergency department patients with flank pain: an external validation of the STONE score. World J Urol. 2016;34:1443–1446. doi: 10.1007/s00345-016-1760-3. [DOI] [PubMed] [Google Scholar]


