Abstract
Objective: To investigate the clinical application of perioperative nursing care for patients with osteosarcoma of the distal femur who received artificial knee replacement. Methods: A total of 80 patients with osteosarcoma of the distal femur admitted to our hospital from March 2019 to March 2020 were selected as research subjects and divided into the control group and the study group according to their admission sequence. The control group was given routine nursing care, while the study group was given perioperative nursing care. The negative emotions, sleep quality, limb function, pain, complication rate, and nursing satisfaction of the two groups of patients after nursing care were analyzed. Results: After nursing care, (1) the Hamilton depression rating scale (HAMD) and Hamilton anxiety scale (HAMA) scores of the study group were both lower than those of the control group; (2) the sleep quality score of the study group was lower than that of the control group (P < 0.001); (3) the study group obtained higher limb function score and excellent-and-good rate than the control group (P < 0.05); (4) the pain score of the study group was lower than that of the control group (P < 0.05), and the time to functional exercise and length of hospital stay of the study group were shorter than those of the control group (P < 0.05); (5) patients in the study group had a lower complication rate than those in the control group (P=0.02); (6) the nursing satisfaction rating of the study group was higher than that of the control group (P < 0.001). Conclusion: For patients with osteosarcoma of the distal femur treated by artificial knee replacement, in addition to the amelioration of negative emotions and sleep quality, perioperative nursing also improves the patients’ limb function and satisfaction and mitigates pain and complications.
Keywords: Total knee arthroplasty, perioperative period, nursing, femur, distal, osteosarcoma, effect
Introduction
The incidence of osteosarcoma is increasing over the years [1-3]. It has been reported that the 5-year survival rate of patients with osteosarcoma of the distal femoral is only 5%, which poses a serious threat to the health and life of patients [4]. Osteosarcoma of the distal femur is most common in male adolescents. In addition to malignant tumors, patients with the disease may suffer symptoms such as dysfunction, pain, and even pathological fractures in severe cases [5]. In recent years, the common clinical treatment for the osteosarcoma is artificial knee replacement, which is accompanied by adverse reactions such as postoperative infection, bringing more challenges to perioperative nursing and treatment. Effective nursing methods are contributory to the improvement of the recovery of knee joint function, postoperative quality of life, and muscle tension around the knee joint for patients undergoing artificial knee replacement during the perioperative period [6]. Therefore, this study explored the clinical application of perioperative nursing care for patients with osteosarcoma of the distal femur who received artificial knee replacement, with the goal of providing a theoretical basis for clinical nursing care.
Materials and methods
General information
This is a prospective study, in which a total of 80 patients admitted to our hospital for treatment of osteosarcoma of the distal femur from March 2019 to March 2020 were selected as research subjects and divided into the control group (n=40) and the study group (n=40) according to their admission order. The protocol was approved by the Ethics Committee of the First Hospital of Cangzhou Central Hospital (Approved No. CL2018DT224).
Inclusion/exclusion criteria
Inclusion criteria
(1) All study subjects met the diagnostic criteria for osteosarcoma of the distal femur [7]; (2) No metastatic lesions and pathological fractures were found preoperatively; (3) The patients and their families signed a consent form after being informed of the purpose and process of the treatment.
Exclusion criteria
(1) Patients with knee joint diseases or malignant tumors other than osteosarcoma of the distal femur; (2) Patients with behavioral, language, or mental disorders; (3) Patients with primary liver, kidney, brain, or other tissue or organ diseases.
Methods
Treatment
After general anesthesia, tumor-type artificial knee replacement, distal femoral osteosarcoma segment amputation, and negative pressure drainage were performed. After the operation, each patient was given anti-infective treatment and 14 days of radiotherapy with high-dose cisplatin (NMPA approval number: H53021678; Manufacturer: Yunnan Gejiu Biopharmaceutical), methotrexate (NMPA approval number: H31020644; Manufacturer: Shanghai Shangyao Xinyi Pharmaceutical Factory), and vincristine (NMPA approval number: H20065857; Manufacturer: Guangdong Lingnan Pharmaceutical), and they were also given 7 days of chemotherapy with vincristine and methotrexate according to the patient’s specific condition.
Nursing methods
Patients in the control group were given routine nursing care, including vital signs detection, wound care, drainage tube care, functional exercise, prevention of deep embolism, etc.
Patients in the study group were given perioperative nursing intervention for artificial knee replacement: (1) Preoperative nursing care. Timely psychological counseling was provided to the patients according to the patients’ psychological state to build up their confidence in treatment by active communication, the elimination of patients’ worries, and education of disease-related knowledge. In addition, A preoperative evaluation of the patient’s overall condition is required for the formulation of corresponding nursing plans, and the implementation of preoperative antibiotic therapy was used to prevent postoperative infection. Moreover, the patients were instructed in terms of coughing, expectoration, and bowel movements, and the necessity of early functional training before surgery was underlined for prevention of complications. (2) Postoperative care. The patient’s vital signs were closely observed to analyze the changes in urine volume and color. Any abnormality required the prompt intervention of the chief physician. The bed of the patient was raised by 15° within 6 hours after the operation, helping the patient lie on the back without a pillow. The patient’s lower limbs were wrapped with elastic bandages, with a soft pillow 30 cm below the patient’s knee joint to maintain an angle of 25° over the heart to prevent the patient from developing deep vein thrombosis in the lower limbs and promote venous blood flow. Additionally, the patient’s foot sensation, dorsal pulsation, affected limb skin, the bleeding from the wound, and the drainage tube patency after fixation required close monitoring during nursing, with the character, color, and volume of the drainage fluid recorded. 24 hours after the operation, the patients’ affected limbs were raised to activate the blood circulation, once every two days. After the recovery from anesthesia, the patients were given exercise instruction accordingly, which included contraction training and functional training. Extubation was conducted 4 days after the operation. The patients were guided to perform knee bending (0°-5° was the starting angle, and it was increased by 10° every day), and the speed and frequency of functional training were adjusted in time according to the patients’ recovery. 21 days after the operation, the patients started to receive walking training with a crutch, and after another 28 days, independent walking training was performed.
Evaluation indexes
Negative emotions
The Hamilton Depression Scale (HAMD) and Hamilton Anxiety Scale (HAMA) [8] were adopted for the analysis of the patients’ negative emotions. There are 24 items on the HAMD scale. Normal: total score < 8 points; possible depression: 8 points ≤ total score < 20 points; depression: 20 points ≤ total score < 35 points; severe depression: 35 points ≤ total score. There are 14 items on the HAMA scale. Normal: total score < 7 points; possible anxiety: 7 points s total score < 14 points; anxiety: 14 points ≤ total score < 21 points; marked anxiety: 21 points ≤ total score < 29 points; severe anxiety: 29 points ≤ total score.
Sleep quality
The sleep quality was analyzed using the Pittsburgh Sleep Quality Index (PSQI) [9]. The full score of the PSQI is 21 points, and the score is negatively correlated with sleep quality.
Limb function and therapeutic efficiency
The patient’s limb function was evaluated by the Harris knee joint function scale [9]. The scale covers four parts, including pain, function, joint range of motion, and limb deformity, with a total score of 100 points. The score is positively correlated with the knee joint function. The limb function is classified into four levels by Harris score: ≥ 90 points are excellent; 80-89 points are good, 70-79 points are acceptable, and < 70 points are poor. The excellent-and-good rate of treatment = the rate of patients’ excellent limb function + the rate of those with good limb function.
Perioperative observation indexes
The patient’s pain was rated by the visual analogue scale (VAS) [11], with a maximum score of 10 points. A higher score indicates stronger pain. The time to functional exercise and length of hospital stay were recorded and compared between the two groups.
Complications and nursing satisfaction
The postoperative complications such as constipation, muscle atrophy, deep vein thrombosis, and pulmonary infection were statistically analyzed. Patient satisfaction with nursing care was analyzed by using a self-made nursing satisfaction questionnaire, which was divided into very satisfied, satisfied, and dissatisfied, and the nursing satisfaction = the rate of patients very satisfied with nursing care + that of those satisfied with nursing care.
Statistical methods
The software SPSS20.0 was used to process and analyze the research data. Measurement data were represented by mean ± standard deviation (x̅±sd) and analyzed by t-test. Count data were represented by [n (%)] and analyzed by X2 test. P < 0.05 represented that the difference was statistically significant.
Results
General data
The control group consisted of 28 males and 12 females, aged 13-65 years, with an average age of 38.48±6.32 years, lesion diameter of about 3.0-8.0 cm, and an average lesion diameter of 4.18±1.05 cm. The study group consisted of 29 males and 11 females, aged 12-64 years, with an average age of 38.41±6.12 years, lesion diameters of 3.0-8.0 cm, and an average lesion diameter of 4.18±1.05 cm. As shown in Table 1, the general clinical data such as age and lesion diameter of the two groups were comparable (P>0.05).
Table 1.
Comparison of general data
| Groups | n | Male/Female | Age (x̅ ± sd, years) | lesion diameter (x̅ ± sd, cm) |
|---|---|---|---|---|
| Study group | 40 | 28/12 | 38.48±6.32 | 4.78±2.11 |
| Control group | 40 | 29/11 | 36.71±7.12 | 5.12±1.75 |
| χ2/t | 0.061 | 1.176 | 0.784 | |
| P | 0.805 | 0.243 | 0.435 |
Negative emotions, sleep quality, and self-care ability
After nursing care, the HAMD and HAMA scores of the study group were both lower than those of the control group (both P < 0.001), as shown in Table 2.
Table 2.
Comparison of negative emotions (x̅±sd, points)
| Groups | n | HAMD | HAMA | ||
|---|---|---|---|---|---|
|
|
|
||||
| Before nursing | After nursing | Before nursing | After nursing | ||
| Study group | 40 | 27.56±6.65 | 10.21±2.04 | 23.78±5.22 | 8.41±2.11 |
| Control group | 40 | 27.51±6.58 | 17.33±3.46 | 23.74±5.38 | 15.76±3.62 |
| t | 0.03 | 2.58 | 0.03 | 11.09 | |
| P | 0.97 | 0.01 | 0.97 | < 0.001 | |
Before nursing care, no significant difference was found in the sleep quality score between the two groups (13.46±3.02 vs. 14.02±3.80) (t=0.730, P=0.468), while after nursing care, the sleep quality score of the study group was lower than that of the control group (5.22±1.62 vs. 7.59±2.88) (t=4.54, P < 0.001), as shown in Figure 1.
Figure 1.
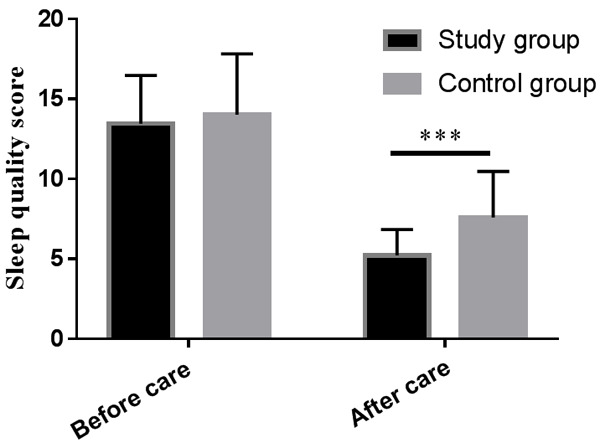
Sleep quality scores of the two groups of patients. ***P < 0.001.
Evaluation of the limb function and therapeutic efficiency
Before nursing care, no significant difference was found in the limb function score between the two groups (64.67±11.38 vs. 66.03±14.02) (t=0.476, P=0.635), while after nursing care, a higher limb function score in the study group than that of the control group was observed (82.58±14.66 vs. 72.62±16.21) (t=2.887, P=0.005), as shown in Figure 2. The excellent-and-good rate of treatment of the study group was significantly higher than that of the control group (82.5% vs. 52.5%, P=0.004), as shown in Table 3.
Figure 2.
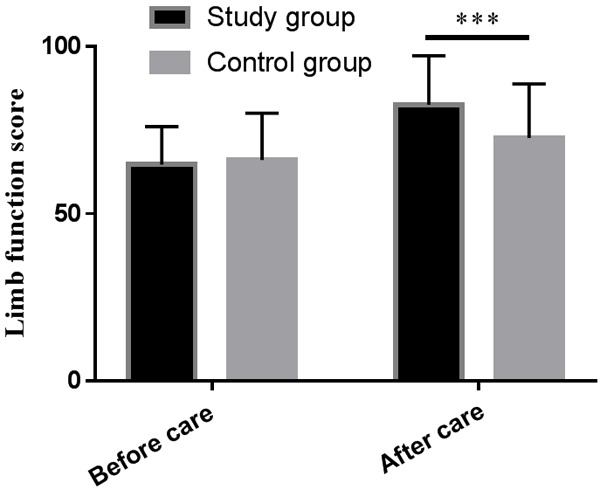
Limb function scores of the two groups of patients. ***P < 0.001.
Table 3.
Comparison of therapeutic efficiency
| Groups | n | Excellent | Good | Acceptable | Poor | Excellent-and-good rate |
|---|---|---|---|---|---|---|
| Study group | 40 | 21 | 12 | 4 | 3 | 82.5% (33) |
| Control group | 40 | 15 | 6 | 14 | 5 | 52.5% (21) |
| χ2 | 8.205 | |||||
| P | 0.004 |
Perioperative observation indexes
Before nursing care, no remarkable difference was seen between the two groups in the pain score (6.45±2.03 vs. 6.98±2.35) (t=1.079, P=0.284), while after nursing care, the pain score of the study group was lower than that of the control group (3.09±1.23 vs. 4.95±2.52) (t=4.195, P < 0.001), as shown in Figure 3. The time to functional exercise and length of hospital stay in the study group were shorter than those in the control group, respectively, as shown in Table 4.
Figure 3.
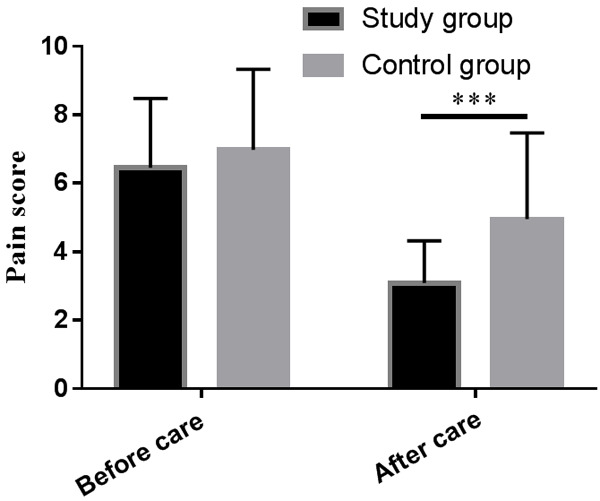
Pain scores of the two groups of patients. ***P < 0.001.
Table 4.
Comparison of the time to functional exercise and length of hospital stay (x̅±sd, d)
| Groups | n | Time to functional exercise | Length of hospital stay |
|---|---|---|---|
| Study group | 40 | 13.66±3.76 | 16.46±3.05 |
| Control group | 40 | 17.24ol gr | 20.75ol gr |
| t | 3.658 | 3.792 | |
| P | < 0.001 | < 0.001 |
Incidence of complications
After nursing care, the complication rate of the study group was lower than that of the control group (5% vs. 22.5%) (t=5.16, P=0.02), as shown in Table 5.
Table 5.
Comparison of complications
| Groups | n | muscle atrophy | pulmonary infection | deep vein thrombosis | constipation | Comparison rate |
|---|---|---|---|---|---|---|
| Study group | 40 | 0 | 0 | 0 | 2 | 5% (2/40) |
| Control group | 40 | 1 | 1 | 3 | 4 | 22.5% (9/40) |
| χ2 | 5.16 | |||||
| P | 0.02 |
Patients’ satisfaction
After nursing care, patients in the study group were more satisfied with the intervention than those in the control group [97.5% (39/40) vs. 75% (30/40)] (t=8.54, P ≤ 0.001), as shown in Table 6.
Table 6.
Comparison of satisfactory rate
| Groups | n | Very satisfied | satisfied | Unsatisfied | Satisfactory rate |
|---|---|---|---|---|---|
| Study group | 40 | 33 | 6 | 1 | 97.5% (39/40) |
| Control group | 40 | 25 | 5 | 10 | 75% (30/40) |
| χ2 | 8.54 | ||||
| P | < 0.001 |
Discussion
Artificial knee replacement is the most common clinical treatment for osteosarcoma of the distal femur, which can alleviate patients’ clinical symptoms, enhance the stability and mobility of their joints, and correct the deformed joints, to improve joint function [12]. To ensure an uneventful artificial knee joint placement, both surgical factors and perioperative nursing are of equal importance. Given the patients’ worries and fear of the surgery, the relevant knowledge of the disease was introduced to the patients and their families prior to the surgical treatment, to ensure the alleviation of clinical symptoms after negative emotions, which further helped restore the knee joint function of patients in postoperative training and thus improved their prognostic quality.
This study explored the clinical application of perioperative nursing care for patients with osteosarcoma of the distal femoral who underwent artificial knee replacement. The results showed that the limb function score and the excellent-and-good rate of the study group were both higher than those of the control group, which proves the effective promotion of perioperative nursing care for artificial knee replacement on the postoperative limb function recovery of the patients. Perioperative nursing emphasizes the importance of nurses as the main participants in the treatment process, which enhances nurses’ sense of responsibility and identity in nursing and plays the role of medical groups to improve treatment effects [13].
Relevant studies have pointed out that most patients with osteosarcoma of the distal femur suffer severe negative emotions, which seriously hinders their sleep quality and recovery. Perioperative nursing requires active communication with patients to reduce their negative emotions and establish confidence in treatment [14]. This study found that the study group given perioperative nursing care showed significantly milder negative emotions and higher sleep quality than the control group given conventional nursing care, which is consistent with the conclusions of Nakajima et al. [15]. The results further verify the promising effect of perioperative nursing care for artificial knee replacement on ameliorating patients’ negative emotions and sleep quality. Given the wide recognization of the role of early functional exercises in promoting the recovery of patients, perioperative nursing care, being regarded as a form of passive exercise, gives greater play to the advantages of early functional exercise and shortens the recovery time of patients by specifying exercise strategies based on the patient’s recovery in real-time.
Preoperative training of sputum, coughing, and deep breathing for patients is beneficial to promoting their lung capacity and reducing the incidence of lung infections after surgery [16]. Guidance on out-of-bed activities and eating habits before surgery for patients can effectively reduce postoperative constipation and other conditions [17,18]. In addition, early functional training plays an essential role in preventing thrombosis. Patients with osteosarcoma of the distal femur are prone to chronic pain, and postoperative training for ankle and knee joints can effectively reduce muscle atrophy [19,20]. In this study, the results showed that the complication rate of the study group was lower than that of the control group, which verifies the efficacy of perioperative nursing care on reducing the incidence of complications in patients. The management of patient catheters was strengthened in this study. In post-operative care, the evidence level for improving the treatment effect is moderate, and the recommendation grade is strong [21].
Perioperative nursing is an important nursing method, which is widely used in the artificial knee joint replacement, but its application in patients with distal femoral osteosarcoma is less reported. This study introduced the perioperative nursing methods of patients with osteosarcoma of the distal femur undergoing knee joint replacement and analyzed its clinical efficacy, which provides evidence-based medicine for the development of nursing work. However, this study also has the following limitations: In the development of nursing work, the individual differences, including education level, professional ability, and training time of nurses, require further unification, and the steps of nursing work need to be further standardized. In addition, individualized care needs to be carried out to meet the needs of different patients, which poses higher requirements for the development of nursing work.
In summary, for patients with osteosarcoma of the distal femur treated by artificial knee joint replacement, in addition to the amelioration of negative emotions and sleep quality, perioperative nursing also improves the patients’ limb function and satisfaction and mitigates pain and complications.
Disclosure of conflict of interest
None.
References
- 1.Thomas T, Coombs NC, Mullette EJ, Bick T, Brant JM. Bilateral total knee arthroplasty: predictors of discharge disposition. Orthop Nurs. 2020;39:92–96. doi: 10.1097/NOR.0000000000000639. [DOI] [PubMed] [Google Scholar]
- 2.Patterson JT, Tillinghast K, Ward D. Dialysis dependence predicts complications, intensive care unit care, length of stay, and skilled nursing needs in elective primary total knee and hip arthroplasty. J Arthroplasty. 2018;33:2263–2267. doi: 10.1016/j.arth.2018.02.035. [DOI] [PubMed] [Google Scholar]
- 3.Donahue RE, Bradbury GR, Zychowicz ME, Muckler VC. Multimodal perioperative analgesia regimen to improve patient outcomes after total knee arthroplasty: a multidisciplinary quality improvement project. J Perianesth Nurs. 2018;33:138–152. doi: 10.1016/j.jopan.2016.07.007. [DOI] [PubMed] [Google Scholar]
- 4.Hughes CG, Boncyk CS, Culley DJ, Fleisher LA, Leung JM, McDonagh DL, Gan TJ, McEvoy MD, Miller TE Perioperative Quality Initiative (POQI) 6 Workgroup. American society for enhanced recovery and perioperative quality initiative joint consensus statement on postoperative delirium prevention. Anesth Analg. 2020;130:1572–1590. doi: 10.1213/ANE.0000000000004641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res. 2010;468:57–63. doi: 10.1007/s11999-009-1119-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hohler SE. Walk patients through total hip arthroplasty. Nursing. 2018;48:24–30. doi: 10.1097/01.NURSE.0000544209.08536.d1. [DOI] [PubMed] [Google Scholar]
- 7.Davicioni E, Wai DH, Anderson MJ. Diagnostic and prognostic sarcoma signatures. Mol Diagn Ther. 2008;12:359–74. doi: 10.1007/BF03256302. [DOI] [PubMed] [Google Scholar]
- 8.Zimmerman M, Martin J, Clark H, McGonigal P, Harris L, Holst CG. Measuring anxiety in depressed patients: a comparison of the Hamilton anxiety rating scale and the DSM-5 anxious distress specifier interview. J Psychiatr Res. 2017;93:59–63. doi: 10.1016/j.jpsychires.2017.05.014. [DOI] [PubMed] [Google Scholar]
- 9.Del Rio João KA, Becker NB, de Neves Jesus S, Isabel Santos Martins R. Validation of the portuguese version of the pittsburgh sleep quality index (PSQI-PT) Psychiatry Res. 2017;247:225–229. doi: 10.1016/j.psychres.2016.11.042. [DOI] [PubMed] [Google Scholar]
- 10.Wright RW MARS Group. Osteoarthritis classification scales: interobserver reliability and arthroscopic correlation. J Bone Joint Surg Am. 2014;96:1145–1151. doi: 10.2106/JBJS.M.00929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zdzieblik D, Oesser S, Gollhofer A, König D. Improvement of activity-related knee joint discomfort following supplementation of specific collagen peptides. Appl Physiol Nutr Metab. 2017;42:588–595. doi: 10.1139/apnm-2016-0390. [DOI] [PubMed] [Google Scholar]
- 12.Yao JJ, Maradit Kremers H, Kremers WK, Lewallen DG, Berry DJ. Perioperative inpatient use of selective serotonin reuptake inhibitors is associated with a reduced risk of THA and TKA revision. Clin Orthop Relat Res. 2018;476:1191–1197. doi: 10.1007/s11999.0000000000000098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Salt E, Wiggins AT, Rayens MK, Morris BJ, Mannino D, Hoellein A, Donegan RP, Crofford LJ. Moderating effects of immunosuppressive medications and risk factors for post-operative joint infection following total joint arthroplasty in patients with rheumatoid arthritis or osteoarthritis. Semin Arthritis Rheum. 2017;46:423–429. doi: 10.1016/j.semarthrit.2016.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hohler SE. Providing evidence-based practices for patients with hip fractures. Nursing. 2018;48:52–57. doi: 10.1097/01.NURSE.0000531895.31558.55. [DOI] [PubMed] [Google Scholar]
- 15.Nakajima A, Sonobe M, Akatsu Y, Aoki Y, Takahashi H, Suguro T, Nakagawa K. Association between limb alignment and patient-reported outcomes after total knee arthroplasty using an implant that reproduces anatomical geometry. J Orthop Surg Res. 2018;13:320. doi: 10.1186/s13018-018-1030-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sappey-Marinier E, Pauvert A, Batailler C, Swan J, Cheze L, Servien E, Lustig S. Kinematic versus mechanical alignment for primary total knee arthroplasty with minimum 2 years follow-up: a systematic review. SICOT J. 2020;6:18. doi: 10.1051/sicotj/2020014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.El-Galaly A, Nielsen PT, Kappel A, Jensen SL. Reduced survival of total knee arthroplasty after previous unicompartmental knee arthroplasty compared with previous high tibial osteotomy: a propensity-score weighted mid-term cohort study based on 2,133 observations from the Danish knee arthroplasty registry. Acta Orthop. 2020;91:177–183. doi: 10.1080/17453674.2019.1709711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Matharu GS, Mouchti S, Twigg S, Delmestri A, Murray DW, Judge A, Pandit HG. The effect of smoking on outcomes following primary total hip and knee arthroplasty: a population-based cohort study of 117,024 patients. Acta Orthop. 2019;90:559–567. doi: 10.1080/17453674.2019.1649510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Scholten R, Leijtens B, Hannink G, Kamphuis ET, Somford MP, van Susante JLC. General anesthesia might be associated with early periprosthetic joint infection: an observational study of 3,909 arthroplasties. Acta Orthop. 2019;90:554–558. doi: 10.1080/17453674.2019.1644069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Katarincic JA, Fantry A, DePasse JM, Feller R. Local modalities for preventing surgical site infections: an evidence-based review. J Am Acad Orthop Surg. 2018;26:14–25. doi: 10.5435/JAAOS-D-16-00033. [DOI] [PubMed] [Google Scholar]
- 21.Wainwright TW, Gill M, McDonald DA, Middleton RG, Reed M, Sahota O, Yates P, Ljungqvist O. Consensus statement for perioperative care in total hip replacement and total knee replacement surgery: enhanced recovery after surgery (ERAS®) society recommendations. Acta Orthop. 2020;91:3–19. doi: 10.1080/17453674.2019.1683790. [DOI] [PMC free article] [PubMed] [Google Scholar]


