Abstract
Growing evidence suggests dementia incidence can be reduced through prevention programs targeting risk factors. To accelerate the implementation of such prevention programs, a new generation of brain health services (BHS) is envisioned, involving risk profiling, risk communication, risk reduction, and cognitive enhancement. The purpose of risk communication is to enable individuals at risk to make informed decisions and take action to protect themselves and is thus a crucial step in tailored prevention strategies of the dementia incidence. However, communicating about dementia risk is complex and challenging.
In this paper, we provide an overview of (i) perspectives on communicating dementia risk from an ethical, clinical, and societal viewpoint; (ii) insights gained from memory clinical practice; (iii) available evidence on the impact of disclosing APOE and Alzheimer’s disease biomarker test results gathered from clinical trials and observational studies; (iv) the value of established registries in light of BHS; and (v) practical recommendations regarding effective strategies for communicating about dementia risk.
In addition, we identify challenges, i.e., the current lack of evidence on what to tell on an individual level—the actual risk—and on how to optimally communicate about dementia risk, especially concerning worried yet cognitively unimpaired individuals. Ideally, dementia risk communication strategies should maximize the desired impact of risk information on individuals’ understanding of their health/disease status and risk perception and minimize potential harms. More research is thus warranted on the impact of dementia risk communication, to (1) evaluate the merits of different approaches to risk communication on outcomes in the cognitive, affective and behavioral domains, (2) develop an evidence-based, harmonized dementia risk communication protocol, and (3) develop e-tools to support and promote adherence to this protocol in BHSs.
Based on the research reviewed, we recommend that dementia risk communication should be precise; include the use of absolute risks, visual displays, and time frames; based on a process of shared decision-making; and address the inherent uncertainty that comes with any probability.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13195-021-00840-5.
Keywords: Brain Health Services, Dementia, Aging, Alzheimer’s disease, Prevention, Risk communication
Background
Encouraging evidence suggests dementia incidence can be reduced by means of precision prevention programs targeting risk factors [1, 2]. This entails tailoring risk reduction to the clinical, biological, genetic, and psychosocial characteristics of each patient. To accelerate the implementation of such a precision approach in dementia prevention, a new generation of Brain Health Services (BHSs) can be envisioned [3], guided by risk profiling [4], and risk communication (the present paper), with the general goal of personalized risk reduction [5] and cognitive enhancement [6], in an ethical and equitable context [7].
The recently proposed diagnostic framework for Alzheimer’s disease (AD) sets the biologically defined disease (by amyloid-β and tau) apart from the clinical staging [8]. This underlines that it is pivotal to define which risk one is referring to, since “risk” may refer to an individual’s likelihood of getting a disease such as AD, which does not immediately imply a clinical outcome (here, cognitive impairment or dementia). Yet, “risk” may also refer to the likelihood of developing the adverse clinical outcome (i.e., dementia). Here, we focus mainly on the dementia risk.
The World Health Organization defines risk communication as “an exchange of real-time information, advice and opinions between experts and people facing threats to their health, economic or social well-being” [9]. The purpose of risk communication is to enable individuals to make informed decisions and take action to protect themselves. Because of the influence that perceptions of individualized risk are expected to have on people’s health- and disease-related behavior, the provision of risk information is an essential aspect of any health prevention effort [10]. Thus, risk communication is a crucial step in tailored prevention strategies of dementia incidence.
However, communicating risk is complex and therefore challenging for clinicians [11, 12]. First, the concept of risk is difficult for patients to comprehend and for physicians to explain [12–17]. Second, risk disclosure is an intervention by itself, because of its potential impact on psychological and mental health of the individual [18] and on decisions that are made for example about the future, employment, and living arrangements, and about who to share these results with. Still, knowing your individual potential for prevention and being able to take action through personalized, multi-domain, risk reduction prevention programs are considered important benefits [19, 20]. In addition, there is currently no single risk prediction tool that is fully validated or recommended as the golden standard for clinical practice.
How to communicate dementia risk depends on the context. Within the context of trial enrollment, disclosure of biomarker evidence and hence dementia risk can be warranted and risk disclosure is then embedded in the protocol [17]. In the clinical context, increasing numbers of individuals without cognitive impairment are seeking care [21, 22], and express a need for information, guidance, and practical advice, although they vary in specific information needs and preferences [23–26]. The envisioned BHSs are aimed at providing meaningful answers to this growing demand. These individuals experience a subjective cognitive decline (SCD) [27] or functional cognitive disorders [22] or are just concerned about cognitive decline and/or their brain health and want to preserve their cognitive performance as long as possible. These individuals represent the target population of BHSs (Altomare et al., [3]) and could be subjected to prediction modeling to inform their individualized dementia risk, although these models are not perfect and risk communication remains challenging [28].
To this background, communication strategies should maximize the desired impact of risk information on individuals’ understanding of their health/disease status and dementia risk perception and minimize potential harms. This paper aims to provide an overview of different perspectives, available evidence, and practice recommendations regarding optimal strategies for communicating dementia risk and identify the next steps in the development of an evidence-based risk communication protocol.
Perspectives on communicating dementia risk
Ethical perspective
Individuals have a right to know or not know their dementia risk [29]. Whether someone wants to know and how it impacts them is very personal [30]. Among potential personal benefits are a reduction in feelings of uncertainty and anxiety, enhanced preparedness for the future, and improved quality of life [31–34]. On the other hand, facing a high probability to develop dementia can have negative psychological effects, including stress, depression or even suicidal ideation, and affect sense of self, future, and perception of memory [31, 35]. In addition, sharing personal risk information with others could lead to stigmatization as well as social, professional, and legal discrimination. While (inter)national agreements protect genetic privacy and prohibit discrimination, these may not apply to biomarker-based risk, nor address protections for long-term care insurance [36]. Nonetheless, from an ethical perspective, it is questionable whether these are reasons not to communicate dementia risk, especially when individuals prefer to know.
Another important argument in the context of provision of dementia risk information is actionability. While some argue that there may be a lack of actionability in the absence of a disease-modifying treatment for AD [18, 37], others point out that learning their likelihood of developing dementia empowers individuals to shift priorities or try to reduce risk through (other) preventive actions, for example controlling modifiable risk factors such as hypertension [1], or adopting a healthier lifestyle [31, 38]. Knowing ones’ risk could thus meaningfully contribute to a worthwhile set of options. It is important to educate, prepare and counsel individuals on all that is known and still uncertain [39], so they can make informed decisions about knowing their dementia risk and utilize their right to self-determination, while they still can.
Clinician perspective
When facing a risk, proper decision-making by the individual about preventive/protective action requires proper understanding and conceptualization of this risk. Clinicians must explain the medical problem (i.e., dementia), the magnitude of the risk, and its implications in a way that is readily understandable by lay people. Here, we can learn from cancer genetics, with a longer history in risk communication.
In Mendelian, autosomal dominant conditions with full penetrance, the risk of developing the disease corresponds to the risk of inheriting the mutation, i.e., 50% for each child of an affected patient, which is easily understood as the outcome of flipping a coin. This applies to some Mendelian forms of AD (e.g., Presenilin mutations). Conveying a risk becomes slightly more complex when penetrance is incomplete (e.g., BRCA mutations), say 70%, producing a disease risk of 35%. Here, geneticists will convey a finer analogy, like picking one out of a hundred marbles from a bag, 65 being green (no disease) and 35 red (disease). Next are moderate-penetrance genes like CHEK2, causing a significant but limited increase in breast cancer risk. This compares with some moderately penetrant Alzheimer’s genes, including APOE-ε4. In families with many affected, other factors than the CHEK2 mutation are also at play. Hence, pre-symptomatic testing in unaffected at-risk relatives might carry false alarm if the mutation is found to be present (because the associated cancer risk is limited), and false reassurance if the mutation is found to be absent (because the residual risk remains increased over population risk) [40]. The analogy of picking one out of a hundred marbles with different colors could also be used to explain the risk of developing dementia associated with moderately penetrant Alzheimer’s genes, including these false cases.
In hereditary breast and ovarian cancer, pre-symptomatic genetic testing allows for targeted prevention [41]. However, depending on the magnitude of the risk, one might weigh the potential benefits and harms of preventive options differently. For example, considering preventive mastectomy with a BRCA1 mutation versus CHEK2. This highlights how effective risk communication is essential, especially when weighing pros and cons of preventive options. With the advent of effective pre-symptomatic strategies in AD, we should learn from the experience learned in genetic counseling in cancer.
Societal/public perspective
AD is a major healthcare concern for many people [42]. Having been asked to choose the one disease they were most afraid of from a list of seven, respondents in a public opinion survey most frequently identified cancer, followed by AD (about one quarter). Interestingly, there was a considerable public interest in pre-symptomatic diagnostic testing. Asked individuals whether they want to take a medical test which would tell them whether they would develop AD, a plurality in all countries responded that they would be “very likely” or “somewhat likely” to get such test, ranging from 51% in Germany to 78% in Poland. However, there’s also evidence that people’s preferences for knowing their AD status or dementia risk decrease when they have had the possibility to think about the consequences of receiving such information [43].
In light of the changing definitions of AD, which could lead to differences in understanding and miscommunication [44], special attention should be paid to raise awareness in the general public about the spectrum of AD from the asymptomatic to the dementia stage. Similarly, prevention messages should be included in campaigns targeting the general public and at-risk populations. depending on the structure of local health care provision and local opportunities.
Evidence on communicating dementia risk
Pending evidence on (the effects of different) strategies for dementia risk communication from the envisioned BHSs, we can learn from evidence gathered within the memory clinic setting, the research setting including clinical trials and prospective studies, and the context of brain research registries.
Memory clinic setting
People present at memory clinics with symptoms or problems in daily life. This is different from the envisioned BHSs mainly aimed at asymptomatic individuals. Yet, memory clinic experience, particularly with regards to MCI, is informative for BHSs [45]. A recent randomized clinical trial (RCT) among individuals with mild cognitive impairment (MCI), showed that receiving information on one’s amyloid-PET status did not improve understanding of the MCI diagnosis nor the capacity to cope with the uncertainty inherent to that diagnosis [46]. Still, the recently published practice guideline by the American Academy of Neurology (AAN) states that an accurate diagnosis of MCI is important, especially to discuss the prognostic possibilities, i.e., risk of dementia [47]. In addition, recommendations were published on how to communicate about amyloid positron emission tomography (PET) results and prognostic information with MCI patients [48]. Nonetheless, communicating the MCI label remains challenging for clinicians [11], and few provide specific or personalized information on the dementia risk to MCI patients [12].
One of the reasons for being reluctant to sharing prognostic information is the apparent lack of individualized risk information for MCI patients, leaving clinicians at best to provide patients with a “fifty-fifty probability.” Recent evidence however illustrates that in MCI, prediction models with good accuracy, calibration, and generalization allow an individualized prognosis based on biomarker evidence [49]. Even when these models still warrant prospective clinical validation, their clinical applicability is at the horizon. On a group level, biomarkers are also predictive of incident dementia in cognitively unimpaired individuals who present with subjective cognitive decline (SCD) at the memory clinic, although it should be noted that at least half of biomarker positive individuals with SCD does not progress to dementia within 5 years [50]. For this population, individualized risk models are not yet ready for implementation, since their external validation is suboptimal [28]. In short, it is not easy to convert biomarker findings to an actual specific and personalized dementia risk. Clinicians’ reluctance in sharing this information is therefore appropriate. To this background, considering the BHS target group of cognitively unimpaired individuals, it is questionable whether we currently have the data available to derive reliable dementia risk estimates. Risk communication can only be as good as the models it is based on, and clearly more work needs to be done.
Research setting
To identify individuals at higher risk of developing AD or dementia, APOLIPOPROTEIN (APOE) and amyloid PET testing are being incorporated in clinical (drug) trials and prospective studies as screening tools (e.g., Alzheimer’s Prevention Initiative Generation Program [51]; Anti-Amyloid Treatment in Asymptomatic Alzheimer’s Disease (A4) Study [52]; AMYPAD Diagnostic and Patient Management Study [53]). Although the disclosure of APOE-ε4 carriership and amyloid PET positivity have distinct implications, trial protocols have adopted similar recommendations regarding the disclosure of APOE and amyloid PET test results (Supplement A in Supplementary Material).
A number of studies have been carried out to assess the safety of disclosing such AD biomarker test results to cognitively unimpaired individuals in the context of trials (Table 1) [31, 32, 54–61]. Most research has shown that disclosure of Alzheimer biomarker results (after pre-test education and psychological screening) does not lead to short-term negative psychological consequences (Table 1). However, it may not always be possible to extrapolate results from highly motivated individuals taking part in research to a more general population. Furthermore, none of the existing disclosure protocols have dealt with actual risk communication, which would imply the provision of the precise magnitude of the risk of developing dementia, considering a specific timeframe (e.g., risk within a number of years). Moreover, additional research is needed to examine the broader implications, both beneficial and harmful, of living with risk, and the impact over longer periods of time.
Table 1.
An overview of studies investigating the impact of disclosure of APOE and Amyloid PET test results to research participants
| Publication | Project/study name | Type of study | Disclosure of | Main finding(s) |
|---|---|---|---|---|
| Green et al. 2009 [54] | The Risk Evaluation and Education for Alzheimer’s Disease (REVEAL) Study | RCT | APOE |
No differences between the two groups (disclosure vs no disclosure) in changes in time-averaged measures of anxiety, depression, or test-related distress (measured at 6 weeks, 6 months, and 1 year). The ε4-negative subgroup had a significantly lower level of test-related distress than did the ε4-positive one. |
| Chao et al. 2008 [55] | REVEAL | RCT | APOE | Participants who learned they were ε4 positive were significantly more likely than ε4 negative participants to report AD-specific health behavioral change 1 year after disclosure. |
| Bemelmans et al. 2016 [31] | N/A | Systematic review | APOE |
In cognitively unimpaired research participants with a first-degree relative with AD, disclosure of APOE-ε4 positivity does not lead to elevated anxiety and depression levels. It does increase test-related distress. It results in behavioral changes concerning insurance and health. |
| Langlois et al. 2019 [56] | Alzheimer’s Prevention Initiative Generation Program | RCT | APOE |
Standard protocol for disclosure is reported. Analyses have not been published yet. |
| Harkins et al. 2015 [57] | Anti-Amyloid Treatment in Asymptomatic Alzheimer’s Disease (A4) Study. | Modified Delphi study to develop consensus on best practices | Amyloid PET | Standard protocol for disclosure is reported. |
| Burns et al. 2017 [58] | University of Kansas Alzheimer’s Prevention through Exercise [APEX] | RCT | Amyloid PET |
Depressive symptoms were stable throughout the visits and not different between groups (elevated vs non-elevated amyloid). Anxiety symptoms peaked at a low level on the day of disclosure in the “elevated” group but were not sustained at 6 weeks or 6 months. Individuals with elevated amyloid had slightly higher total levels of test-related distress compared with the non-elevated amyloid group at 6 weeks and 6 months post-disclosure. |
| Largent et al. 2020 [32] | Study of Knowledge and Reactions to Amyloid Testing (SOKRATES) recruiting participants from the A4 and Longitudinal Evaluation of Amyloid Risk and Neurodegeneration (LEARN) trials | Observational study | Amyloid PET |
Participants generally understood that an “elevated” amyloid PET scan result means increased but presently unquantifiable risk of developing AD dementia. Participants who received an “elevated” result often wanted more information regarding the result. An “elevated” result sparked negative emotions that decreased but did not entirely dissipate with time, but did not lead to extreme distress. Support the safety of disclosing amyloid imaging results to cognitively unimpaired persons following pre-test assessments of knowledge and psychological well-being. Participants who received an “elevated” result reported contemplating and making changes to health behaviors and future plans to a greater extent. Participants with elevated brain amyloid viewed the amyloid PET scan result as a serious, sensitive piece of health information. Irrespective of their brain amyloid status, participants were mindful that their amyloid PET scan result had implications for themselves and also for others. |
| Grill et al. 2020 [59] | A4 study and LEARN trials | Observational study | Amyloid PET | Participants in the elevated amyloid group, compared with participants who learned that they had a not elevated amyloid result, were not more likely to experience short-term increases in depression, anxiety, or suicidality |
| Wilde et al. 2018 [60] | N/A | Systematic review | Amyloid PET |
The sparse data available suggest that disclosure of amyloid PET results has a low risk of psychological harm in the context of clinical trials, whereas both participants and professionals seem to support disclosure. More research is needed about the psychological impact of PET disclosure, and the predictive value of results at an individual level. Communication materials and strategies to support disclosure of amyloid PET results should be further developed and prospectively evaluated. |
| Kim and Lingler 2019 [61] | N/A | Systematic review | Amyloid PET |
Provides important early insights into the psychological safety of disclosing amyloid imaging results to cognitively normal persons. Highlights the need for rigorously designed studies that address social and behavioral outcomes and extend to symptomatic populations. |
Brain research registries
Here, we present three examples of brain research registries, aiming to catalyze trial enrolment of individuals in the earliest disease stages. The success of these registries reflects the high interest in brain research, prevention, and brain health in the general community.
The “BBDPS Study: a study on risk factor disclosure” and its associated registry
The registry associated with the Barcelonaβeta Dementia Prevention Study (BBDPS) aims to recruit individuals with SCD or MCI from the general population (Supplement B in Supplementary Material). People were invited to register if they “were feeling changes in their memory or cognitive status.” The study’s schematic is shown in Figure B1 in Supplementary Material. The registry contributes to a highly efficient recruitment strategy, with screening failure rates much lower than standard rates. Moreover, the BBDPS-registry shows value in light of BHSs since ongoing (prevention) studies can be offered to more than 50% of the registered individuals.
In a first evaluation of the emotional impact of disclosing personal risk estimates, the BBDPS-study showed that disclosing the 5-year dementia risk to cognitively unimpaired participants in a research setting increases neither feelings of depression nor anxiety, hence can be considered safe (Table B1 and Figure B2 in Supplementary Material).
The Swiss Brain Health Registry
The Swiss Brain Health Registry (www.bhr-suisse.org) aims to facilitate access to research programs to persons who wish to contribute to research on AD and memory-related diseases. The registry is open to all persons aged 50 and over. Once participants sign the informed consent, they are in the registry and can be contacted by researchers from one of the participating Swiss memory clinics (Geneva, Lausanne, Fribourg, St. Gallen or Lugano) and offered the opportunity to participate in a study. The website offers generic advice on lifestyles for a healthy brain, but the Swiss Brain Health Registry does not provide registrants with information on their personal dementia risk.
The Dutch Brain Research Registry
The Dutch Brain Research Registry (Hersenonderzoek.nl in Dutch) [62] was set up in 2017 with the aim to accelerate recruitment of participants for current and future clinical brain disease studies in the Netherlands. To date, over 20.000 participants signed up (58±11 years old, 78% female). Using their personal online portal, registrants provide demographic information, medical history, family history of dementia, medication and substance use, and lifestyle information. Prescreening of registrants for studies/trials is solely based on this self-reported information. For this reason, the Dutch Brain Research Registry chose not to provide registrants with any information on their personal risk for developing AD and/or dementia.
Between January and June 2019, five focus groups were organized (each 3 to 8 participants, total n = 28) to explore registrant experiences, including motivations for registration. In addition to altruistic reasons (contribute to science/society) and family-related reasons (brain disease runs in family), registrants often reported that receiving information about their brain health and gaining insight in improving or maintaining their own brain health were important reasons for registration. These findings indicate that many of the registrants of a low-threshold, online research registry like the Dutch Brain Research Registry are representative of the target population for the envisioned BHSs.
Practical recommendations on risk communication
How to communicate risk
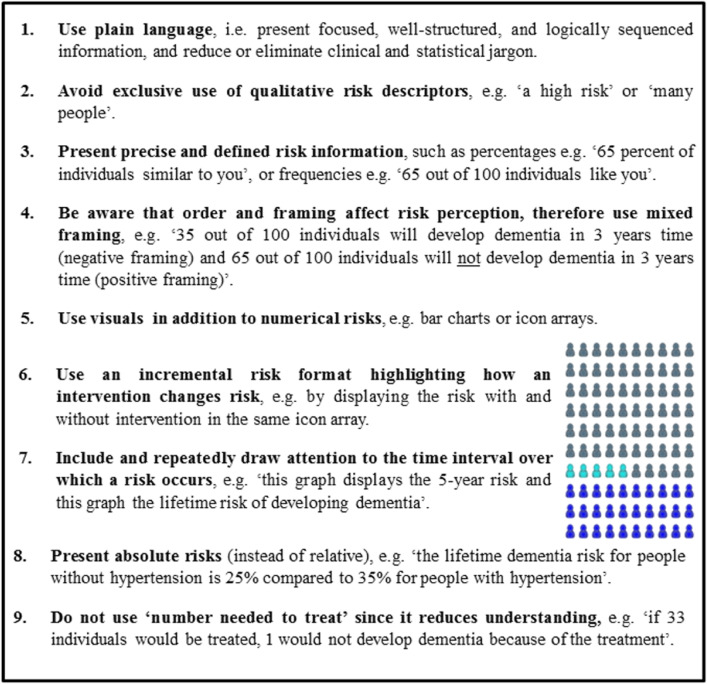
Table 2 displays nine practical recommendations on how to communicate about dementia risk, as synthesized from available guidelines and evidence in the oncology field [14, 63, 64]. The online tool ADappt (www.ADappt.health) encompasses a dementia risk calculation tool, including a communication sheet taking into account these recommendations [65].
Table 2.
Practice recommendations for communicating risk in BHSs
Managing expectations: communicating uncertainty and shared decision-making
Risk profiling is about probabilistic statements regarding the individual's future, and therefore uncertainty is inherent [66]. Even when biomarker testing confirms a disease diagnosis, it often does not provide certainty about disease severity or its course [67]. Moreover, high-quality data are sometimes not available and even when they are, these data can have multiple interpretations or be contradictory, and risk models are never perfect [28]. Hence, communication about uncertainty is an integral aspect of risk disclosure, and managing expectations beforehand is important to inform individuals that this process will not necessarily result in a reduction of uncertainty [48, 68]. An approach for uncertainty communication has been proposed [69], which comprises three steps: (1) normalizing uncertainty, by acknowledging individuals' wish for more certainty while explaining that uncertainty is unfortunately inherent to the situation; (2) addressing the individual’s emotions regarding uncertainty by acknowledging that it is unpleasant not to know things; and (3) stimulating individuals to focus on living in the here and now instead of dwelling on the uncertainty, thereby helping them to cope with uncertainty.
Thus, risk communication is not simply about disclosing test results (i.e., one-way information provision), but also about what individuals and their relatives want to know and when (i.e., a two-way information exchange). Especially since individuals might weigh the potential harms and benefits of knowing their dementia risk differently, depending on their values, needs, and situation [25]. A process of shared decision-making (SDM) [70] offers a way to incorporate evidence and the health care professional’s expertise, as well as the individual’s preferences into decision-making about pursuing biomarker testing for AD and/or knowing their dementia risk [71, 72]. Four steps are proposed: (1) informing the individual that a preference-sensitive decision is to be made; (2) explaining the options including pros and cons; (3) discussing what is important for the individual in his/her situation; and (4) discussing the individual’s preferred role in decision-making and make a decision. In general, the SDM approach has been shown to encourage health-promoting behaviors, reduce inappropriate or unnecessary use of care, and improve patient and clinician satisfaction [73, 74].
Discussion
We reviewed and synthesized current evidence to formulate practice recommendations for communicating dementia risk. Based on evidence in the field of oncology, risk communication should be based on a process of shared decision-making, taking into account that risk implies, by definition, uncertainty. Best practice recommendations for risk communication include the use of absolute risks, visual displays, and time frames.
In memory clinics, patients present with signs and symptoms. Still, even in that context, there is room for improvement in risk communication [24]. Some experience is also gained in the trial setting, where protocols for disclosure of APOE and amyloid test results and dementia risk have been developed, and studies show that biomarker disclosure is not harmful in the short term [32, 59, 60]. But often this disclosure only infers the explanation that these biomarker findings can be viewed as a risk factor for dementia. They do not specify the time frame or the precise magnitude of the risk, nor do they relate this risk to the general risk of dementia (without knowledge on biomarkers) or the risk based on the individual’s full risk profile (e.g., incorporating cardiovascular factors). Yet, an increasing number of individuals want to know their risk and specifically its meaning [25, 75, 76].
In other fields, such as oncology, quite a lot of research has been done on the optimal way to convey risks. A first attempt to integrate these recommendations in risk communication based on biomarker-findings in patients presenting at a memory clinic with MCI is www.ADappt.health [65]. However, risk communication is not only about how to communicate, but also about what to tell. The step to executing this type of risk communication in cognitively unimpaired individuals, the target population of BHSs, is quite large. Although findings at group level clearly endorse the predictive value of biomarker findings, these same findings also illustrate large heterogeneity in disease course, and therefore translation to the individual level is limited. It takes a long time from biomarker abnormality to onset of dementia, and this explains why large cohorts with long duration of follow-up are needed.
Challenges
Evidence about the effectivity of specific risk communication strategies mainly stems from data collected in other medical settings, such as oncology. Some important differences warrant caution when translating that evidence to the field of AD and dementia. In oncology, patients with a given cancer diagnosis are presented with evidence-based treatment options and accompanying known probabilities of survival and other harms and benefits. In comparison, in AD, we are talking about evidence of disease, based on biomarkers, to predict likelihood of developing dementia in the future. These differences emphasize the need for more specific research on risk communication in the context of AD and the implementation of a precision approach to dementia prevention.
In general, risk information is difficult to convey, and for at-risk individuals to understand [77, 78]. It may be even more difficult in dementia, as no fixed events define its onset [79]. As an additional barrier, the cognitive impairment that is inherent to a neurodegenerative disease such as AD could hamper communication and understanding. A particular challenge at this stage is that a lot of people in the general public use the terms AD and dementia interchangeably and are not aware of the new definition of AD as the underlying disease which may cause dementia at a later stage [44, 80]. There is a lot of (linguistic) confusion -also among professionals- making it harder to define optimal strategies to clearly communicate risk.
Finally, decisions about whether and how to pursue diagnostic testing and communicate risk estimates as part of a nation's package of healthcare benefits might also depend on the national structure of health care provision and local opportunities, since there is a wide variety in healthcare benefits/reimbursement systems among countries.
Future research directions
More evidence is warranted about the impact of dementia risk communication, to be able to adequately inform, make (shared) decisions, and manage expectations. More specifically, we need to systematically evaluate the relative merits of different approaches/strategies to risk communication on outcomes in three domains: (i) the cognitive domain, reflecting peoples’ risk perception and understanding, such as accuracy in answering questions related to probabilistic information; (ii) the affective domain, concerning the psychosocial impact, including stigma, and individuals’ preferences for or satisfaction with the communication strategy; and (iii) the behavioral domain, people’s intentions to change behavior, or their actual actions, such as lifestyle modifications.
Furthermore, research should be directed at identifying those factors that influence individuals’ reactions to getting to know their dementia risk, since differences between individuals may moderate the relation between risk communication and relevant outcomes. Hence, a one-size-fits-all approach does not work. This is especially relevant in light of cultural differences and minority groups, and one's educational background. Insight into moderating factors and individual differences could stimulate the adoption of a truly personalized, tailored approach to dementia prevention, taking into account the individual’s characteristics and personal needs, preferences, values, and situation.
Next, based on that evidence, we should develop an evidence-based dementia risk communication protocol. Although evidence about the impact of different strategies on relevant outcomes could form a strong base, input from health care professionals and the target population will be necessary to align perspectives and gain acceptance among stakeholders, which support the implementation of risk communication best-practices. Finally, (e-)tools are warranted to support professionals in communication and promote adherence to the communication protocol.
Conclusion
With the growing knowledge of AD and availability of biomarkers on the one hand, and the increasing focus on prevention strategies on the other hand, there is a growing demand to know one’s risk of dementia in very early stages. This demand will even further increase with the upcoming of blood-based biomarkers and disease-modifying treatments. Communicating about the risk of developing dementia is thus crucial, yet challenging, because of the current lack of evidence on what to tell on an individual level (i.e., the actual risk), and on how to optimally communicate about risk in a way that maximizes the desired impact of this information and minimize its harms. Available evidence suggests that risk communication should be precise and include the use of absolute risks, visual displays, and time frames, be based on a process of shared decision-making, and address the uncertainty inherent to any probability. Next steps required for the development of an evidence-based BHS protocol for dementia risk communication include the systematic evaluation of the relative merits of different strategies to risk communication on affective, cognitive, and behavioral outcomes, with a special focus on individual differences.
Supplementary Information
Additional file 1. Supplement A. Summary of recommendations on how to disclose test results for dementia risk assessment in context of clinical trials. Supplement B. The Barcelonaβeta Dementia Prevention Study (BBDPS) and its associated registry. Figure B1. Schematic representation of the BBDPS. Table B1. Sample characteristics of the BBDPS participants at baseline visit. Figure B2. Impact of dementia risk disclosure on 69 low-risk versus 20 high-risk individuals with SCD from the BBDPS.
Acknowledgements
European Task Force for Brain Health Services (in alphabetical order): Marc ABRAMOWICZ, Daniele ALTOMARE, Frederik BARKHOF, Marcelo BERTHIER, Melanie BIELER, Kaj BLENNOW, Carol BRAYNE, Andrea BRIOSCHI, Emmanuel CARRERA, Gael CHÉTELAT, Chantal CSAJKA, Jean-François DEMONET, Alessandra DODICH, Bruno DUBOIS, Giovanni B. FRISONI, Valentina GARIBOTTO, Jean GEORGES, Samia HURST, Frank JESSEN, Miia KIVIPELTO, David LLEWELLYN, Laura McWHIRTER, Richard MILNE, Carolina MINGUILLÓN, Carlo MINIUSSI, José Luis MOLINUEVO, Peter M NILSSON, Janice RANSON, Federica RIBALDI, Craig RITCHIE, Philip SCHELTENS, Alina SOLOMON, Wiesje VAN DER FLIER, Cornelia VAN DUIJN, Bruno VELLAS, Leonie VISSER.
The authors would like to express their gratitude to BBDPS participants.
Abbreviations
- AAN
American Academy of Neurology
- AD
Alzheimer’s disease
- APOE
APOLIPOPROTEIN
- A4
Anti-Amyloid Treatment in Asymptomatic Alzheimer’s Disease Study
- BBDPS
Barcelonaβeta Dementia Prevention Study
- BHS
Brain Health Services
- CES-D
Center for Epidemiologic Studies Depression Scale
- MCI
Mild cognitive impairment
- PET
Positron emission tomography
- SCD
Subjective cognitive decline
- SDM
Shared decision-making
- STAI
State-Trait Anxiety Inventory
Authors’ contributions
Leonie N.C. Visser, Carolina Minguillon, Wiesje M. van der Flier, and José Luis Molinuevo conceptualized this Paper, drafted the manuscript for intellectual content, and approved the manuscript. Gonzalo Sánchez-Benavides, Marc Abramowicz, Karine Fauria, Jean Georges, Philip Scheltens, Jetske van der Schaar, and Marissa Zwan drafted specific parts of the manuscript, revised the manuscript for intellectual content, and approved the manuscript. Daniele Altomare, Giovanni B. Frisoni, and Federica Ribaldi conceived and organized the workshop whence the Papers of the BHS series in this issue of Alzheimer’s Research & Therapy originated, conceived the related editorial initiative, revised this manuscript for intellectual content, harmonized the manuscript with the other Papers of the BHS series, and approved the manuscript.
Funding
This paper was the product of a workshop funded by the Swiss National Science Foundation entitled “Dementia Prevention Services” (grant number: IZSEZ0_193593).
Additional funding was obtained from EURO-FINGERS, an EU Joint Programme - Neurodegenerative Disease Research (JPND) project. The EURO-FINGERS project is supported through the following funding organizations under the aegis of JPND - www.jpnd.eu: Finland, Academy of Finland; Germany, Federal Ministry of Education and Research; Spain, National Institute of Health Carlos III; Luxembourg, National Research Fund; Hungary, National Research, Development and Innovation Office; The Netherlands, Netherlands Organisation for Health Research and Development (ZonMW-Memorabel #733051102); Sweden, Swedish Research Council.
LNCV is funded by an Alzheimer Nederland fellowship (WE.15-2019-05).
The Barcelonaβeta Dementia Prevention Study and its registry have received funding from the Barcelona City Council (20190454), the Health Department of the Catalan Government, the Catalan Agency for Health Quality and Evaluation, and Biogen.
Hersenonderzoek.nl is supported by ZonMw-Memorabel (#73305095003), Gieskes-Strijbis Foundation, Alzheimer Nederland and Hersenstichting.
GBF received funding by the EU-EFPIA Innovative Medicines Initiatives 2 Joint Undertaking (IMI 2 JU) “European Prevention of Alzheimer’s Dementia consortium” (EPAD, grant agreement number: 115736) and “Amyloid Imaging to Prevent Alzheimer’s Disease” (AMYPAD, grant agreement number: 115952); the Swiss National Science Foundation: “Brain connectivity and metacognition in persons with subjective cognitive decline (COSCODE): correlation with clinical features and in vivo neuropathology” (grant number: 320030_182772).
WF, LNCV, and PS are recipients of ABOARD, which is a public-private partnership receiving funding from ZonMW (#73305095007) and Health~Holland, Topsector Life Sciences & Health (PPP-allowance; #LSHM20106).
Availability of data and materials
The data that support the findings of the BBDPS of are available from the corresponding author Carolina Minguillon, upon reasonable request.
Declarations
Ethics approvals and consent to participate
The BBDPS was approved by the Independent Ethics Committee “Parc de Salut Mar”, Barcelona, and registered at Clinicaltrials.gov (Identifier: NCT03847038). All participating subjects and signed the study’s informed consent form that had also been approved by the Independent Ethics Committee “Parc de Salut Mar”, Barcelona.
Consent for publication
Not applicable.
Competing interests
GBF reports grants from Alzheimer Forum Suisse, Académie Suisse des Sciences Médicales, Avid Radiopharmaceuticals, Biogen, GE International, Guerbert, Association Suisse pour la Recherche sur l’Alzheimer, IXICO, Merz Pharma, Nestlé, Novartis, Piramal, Roche, Siemens, Teva Pharmaceutical Industries, Vifor Pharma, and Alzheimer’s Association; he has received personal fees from AstraZeneca, Avid Radiopharmaceuticals, Elan Pharmaceuticals, GE International, Lundbeck, Pfizer, and TauRx Therapeutics.
PS has received consultancy fees (paid to the institution) from AC Immune, Alkermes, Alnylam, Anavex, Biogen, Brainstorm Cell, Cortexyme, Denali, EIP, ImmunoBrain Checkpoint, GemVax, Genentech, Green Valley, Novartis, Novo Noridisk, PeopleBio, Renew LLC, Roche. He is PI of studies with AC Immune, CogRx, FUJI-film/Toyama, IONIS, UCB, Vivoryon. He serves on the board of the Brain Research Center.
WF has received consultancy fees (paid to the institution) from Oxford Health Policy Forum CIC, Roche BV. She has been an invited speaker at Boehringer Ingelheim, Biogen MA Inc, and WebMD Neurology (Medscape). She has performed contract research for Biogen MA Inc and Boehringer Ingelheim. All funding is paid to her institution. WF is associate editor at Alzheimer’s, Research & Therapy.
JLM is currently a full-time employee of Lundbeck and has previously served as a consultant or at advisory boards for the following for-profit companies, or has given lectures in symposia sponsored by the following for-profit companies: Roche Diagnostics, Genentech, Novartis, Lundbeck, Oryzon, Biogen, Lilly, Janssen, Green Valley, MSD, Eisai, Alector, BioCross, GE Healthcare, ProMIS Neurosciences.
The other co-authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Leonie N.C. Visser and Carolina Minguillon contributed equally to this work (shared first author).
Wiesje M. van der Flier and José Luis Molinuevo contributed equally to this work (shared last author).
Contributor Information
Leonie N. C. Visser, Email: leonie.visser@ki.se
Carolina Minguillon, Email: cminguillon@barcelonabeta.org.
References
- 1.Livingston G, Huntley J, Sommerlad A, Ames D, Ballard C, Banerjee S, et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. The Lancet. 2020;396(10248):413–46. [DOI] [PMC free article] [PubMed]
- 2.Frisoni GB, Molinuevo JL, Altomare D, Carrera E, Barkhof F, Berkhof J, Delrieu J, Dubois B, Kivipelto M, Nordberg A, et al. Precision prevention of Alzheimer's and other dementias: Anticipating future needs in the control of risk factors and implementation of disease-modifying therapies. Alzheimers Dementia. 2020;16(10):1457–1468. doi: 10.1002/alz.12132. [DOI] [PubMed] [Google Scholar]
- 3.Altomare D, Molinuevo JL, Ritchie C, Ribaldi F, Carrera E, Dubois B, Jessen F, McWhirter L, Scheltens P, van der Flier WM, Vellas B, Démonet JF, Frisoni GB. Brain Health Services: Organization, structure and challenges for implementation. A user manual for Brain Health Services – Part 1 of 6. Alzheimer's Research & Therapy. 2021. [DOI] [PMC free article] [PubMed]
- 4.Ranson JM, Rittman T, Hayat S, Brayne C, Jessen F, Blennow K, van Duijn C, Barkhof F, Tang E, Mummery CJ, Stephan BCM, Altomare D, Frisoni GB, Ribaldi F, Molinuevo JL, Scheltens P, Llewellyn, DJ. Modifiable risk factors for dementia and dementia risk profiling. A user manual for Brain Health Services – Part 2 of 6. Alzheimer's Research & Therapy. 2021. [DOI] [PMC free article] [PubMed]
- 5.Solomon A, Stephen R, Altomare D, Carrera E, Frisoni GB, Kulmala J, Molinuevo JL, Nilsson P, Ngandu T, Ribaldi F, Vellas B, Scheltens P, Kivipelto M. Multidomain interventions: state-of-the-art and future directions for protocols to implement precision dementia risk reduction. A user manual for Brain Health Services – Part 4 of 6. Alzheimer's Research & Therapy. 2021. [DOI] [PMC free article] [PubMed]
- 6.Brioschi Guevara A, Bieler M, Altomare D, Berthier M, Csajka C, Dautricourt S, Démonet JF, Dodich A, Frisoni GB, Miniussi C, Molinuevo JL, Ribaldi F, Scheltens P, Chételat G. Protocols for cognitive enhancement. A user manual for Brain Health Services – Part 5 of 6. Alzheimer's Research & Therapy. 2021. [DOI] [PMC free article] [PubMed]
- 7.Milne R, Altomare D, Ribaldi F, Molinuevo JL, Frisoni GB, Brayne C. Societal and equity challenges for Brain Health Services. A user manual for Brain Health Services – Part 6 of 6. Alzheimer's Research & Therapy. 2021. [DOI] [PMC free article] [PubMed]
- 8.Jack CR, Jr, Bennett DA, Blennow K, Carrillo MC, Dunn B, Haeberlein SB, Holtzman DM, Jagust W, Jessen F, Karlawish J, et al. NIA-AA Research Framework: Toward a biological definition of Alzheimer's disease. Alzheimers Dementia. 2018;14(4):535–562. doi: 10.1016/j.jalz.2018.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization: General information on risk communication. Retrieved from: https://www.who.int/riskcommunication/background/en/. Accessed 14 Dec 2020
- 10.Rothman AJ, Kiviniemi MT. Treating people with information: an analysis and review of approaches to communicating health risk information. J Natl Cancer Inst Monogr. 1999;25:44–51. doi: 10.1093/oxfordjournals.jncimonographs.a024207. [DOI] [PubMed] [Google Scholar]
- 11.Kunneman M, Smets EMA, Bouwman FH, Schoonenboom NSM, Zwan MD, Pel-Littel R, van der Flier WM. Clinicians' views on conversations and shared decision making in diagnostic testing for Alzheimer's disease: The ABIDE project. Alzheimers Dement (N Y) 2017;3(3):305–313. doi: 10.1016/j.trci.2017.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Visser LNC, van Maurik IS, Bouwman FH, Staekenborg S, Vreeswijk R, Hempenius L, de Beer MH, Roks G, Boelaarts L, Kleijer M, et al. Clinicians' communication with patients receiving a MCI diagnosis: The ABIDE project. PLoS One. 2020;15(1):e0227282. doi: 10.1371/journal.pone.0227282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bell NR, Dickinson JA, Grad R, Singh H, Kasperavicius D, Thombs BD. Understanding and communicating risk: Measures of outcome and the magnitude of benefits and harms. Can Fam Physician. 2018;64(3):181–185. [PMC free article] [PubMed] [Google Scholar]
- 14.Zipkin DA, Umscheid CA, Keating NL, Allen E, Aung K, Beyth R, Kaatz S, Mann DM, Sussman JB, Korenstein D, et al. Evidence-based risk communication: a systematic review. Ann Intern Med. 2014;161(4):270–280. doi: 10.7326/M14-0295. [DOI] [PubMed] [Google Scholar]
- 15.Gigerenzer G, Gaissmaier W, Kurz-Milcke E, Schwartz LM, Woloshin S. Helping Doctors and Patients Make Sense of Health Statistics. Psychol Sci Public Interest. 2007;8(2):53–96. doi: 10.1111/j.1539-6053.2008.00033.x. [DOI] [PubMed] [Google Scholar]
- 16.Peters E, Hibbard J, Slovic P, Dieckmann N. Numeracy skill and the communication, comprehension, and use of risk-benefit information. Health Affairs (Project Hope) 2007;26(3):741–748. doi: 10.1377/hlthaff.26.3.741. [DOI] [PubMed] [Google Scholar]
- 17.Peters KR, Lynn Beattie B, Feldman HH, Illes J. A conceptual framework and ethics analysis for prevention trials of Alzheimer Disease. Prog Neurobiol. 2013;110:114–123. doi: 10.1016/j.pneurobio.2012.12.001. [DOI] [PubMed] [Google Scholar]
- 18.Schermer MHN, Richard E. On the reconceptualization of Alzheimer's disease. Bioethics. 2019;33(1):138–145. doi: 10.1111/bioe.12516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kostoff RN. Actionable Causes of Alzheimer's disease. J Sci Res. 2017;6:51–53. doi: 10.5530/jscires.6.1.7. [DOI] [Google Scholar]
- 20.Imtiaz B, Tolppanen AM, Kivipelto M, Soininen H. Future directions in Alzheimer's disease from risk factors to prevention. Biochem Pharmacol. 2014;88(4):661–670. doi: 10.1016/j.bcp.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 21.van der Flier WM, Scheltens P. Amsterdam Dementia Cohort: Performing Research to Optimize Care. J Alzheimers Dis. 2018;62(3):1091–1111. doi: 10.3233/JAD-170850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McWhirter L, Ritchie C, Stone J, Carson A. Functional cognitive disorders: a systematic review. Lancet Psychiatry. 2020;7(2):191–207. doi: 10.1016/S2215-0366(19)30405-5. [DOI] [PubMed] [Google Scholar]
- 23.Fruijtier AD, Visser LNC, van Maurik IS, Zwan MD, Bouwman FH, van der Flier WM, Smets EMA. ABIDE Delphi study: topics to discuss in diagnostic consultations in memory clinics. Alzheimers Res Ther. 2019;11(1):77. doi: 10.1186/s13195-019-0531-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Visser LNC, Kunneman M, Murugesu L, van Maurik I, Zwan M, Bouwman FH, Schuur J, Wind HA, Blaauw MSJ, Kragt JJ, et al. Clinician-patient communication during the diagnostic workup: The ABIDE project. Alzheimers Dementia. 2019;11:520–528. doi: 10.1016/j.dadm.2019.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kunneman M, Pel-Littel R, Bouwman FH, Gillissen F, Schoonenboom NSM, Claus JJ, van der Flier WM, Smets EMA. Patients' and caregivers' views on conversations and shared decision making in diagnostic testing for Alzheimer's disease: The ABIDE project. Alzheimers Dement (N Y) 2017;3(3):314–322. doi: 10.1016/j.trci.2017.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tochel C, Smith M, Baldwin H, Gustavsson A, Ly A, Bexelius C, Nelson M, Bintener C, Fantoni E, Garre-Olmo J, et al. What outcomes are important to patients with mild cognitive impairment or Alzheimer's disease, their caregivers, and health-care professionals? A systematic review. Alzheimers Dement (Amst) 2019;11:231–247. doi: 10.1016/j.dadm.2018.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jessen F, Amariglio RE, Buckley RF, van der Flier WM, Han Y, Molinuevo JL, Rabin L, Rentz DM, Rodriguez-Gomez O, Saykin AJ, et al. The characterisation of subjective cognitive decline. Lancet Neurol. 2020;19(3):271–278. doi: 10.1016/S1474-4422(19)30368-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.van Maurik IS, Slot RER, Verfaillie SCJ, Zwan MD, Bouwman FH, Prins ND, Teunissen CE, Scheltens P, Barkhof F, Wattjes MP, et al. Personalized risk for clinical progression in cognitively normal subjects-the ABIDE project. Alzheimers Res Ther. 2019;11(1):33. doi: 10.1186/s13195-019-0487-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Smedinga M, Tromp K, Schermer MHN, Richard E. Ethical Arguments Concerning the Use of Alzheimer's Disease Biomarkers in Individuals with No or Mild Cognitive Impairment: A Systematic Review and Framework for Discussion. J Alzheimers Dis. 2018;66(4):1309–1322. doi: 10.3233/JAD-180638. [DOI] [PubMed] [Google Scholar]
- 30.Arias JJ, Cummings J, Grant AR, Ford PJ. Stakeholders' Perspectives on Preclinical Testing for Alzheimer's Disease. J Clin Ethics. 2015;26(4):297–305. [PubMed] [Google Scholar]
- 31.Bemelmans SA, Tromp K, Bunnik EM, Milne RJ, Badger S, Brayne C, Schermer MH, Richard E. Psychological, behavioral and social effects of disclosing Alzheimer's disease biomarkers to research participants: a systematic review. Alzheimers Res Ther. 2016;8(1):46. doi: 10.1186/s13195-016-0212-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Largent EA, Harkins K, van Dyck CH, Hachey S, Sankar P, Karlawish J. Cognitively unimpaired adults' reactions to disclosure of amyloid PET scan results. PLoS One. 2020;15(2):e0229137. doi: 10.1371/journal.pone.0229137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Christensen KD, Karlawish J, Roberts JS, Uhlmann WR, Harkins K, Wood EM, Obisesan TO. Le LQ, Cupples LA, Zoltick ES, et al. Disclosing genetic risk for Alzheimer's dementia to individuals with mild cognitive impairment. Alzheimers Dement (N Y) 2020;6(1):e12002. doi: 10.1002/trc2.12002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ott BR, Pelosi MA, Tremont G, Snyder PJ. A Survey of Knowledge and Views Concerning Genetic and Amyloid PET Status Disclosure. Alzheimers Dement (N Y) 2016;2(1):23–29. doi: 10.1016/j.trci.2015.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Karlawish J. Addressing the ethical, policy, and social challenges of preclinical Alzheimer disease. Neurology. 2011;77(15):1487–1493. doi: 10.1212/WNL.0b013e318232ac1a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Stites SD, Milne R, Karlawish J. Advances in Alzheimer's imaging are changing the experience of Alzheimer's disease. Alzheimers Dement (Amst) 2018;10:285–300. doi: 10.1016/j.dadm.2018.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bunnik EM, Richard E, Milne R, Schermer MHN. On the personal utility of Alzheimer's disease-related biomarker testing in the research context. J Med Ethics. 2018;44(12):830–834. doi: 10.1136/medethics-2018-104772. [DOI] [PubMed] [Google Scholar]
- 38.Seiffert DJ, McCarthy Veach P, LeRoy B, Guan W, Zierhut H. Beyond medical actionability: Public perceptions of important actions in response to hypothetical genetic testing results. J Genet Couns. 2019;28(2):355–366. doi: 10.1002/jgc4.1048. [DOI] [PubMed] [Google Scholar]
- 39.Vanderschaeghe G, Dierickx K, Vandenberghe R. Review of the Ethical Issues of a Biomarker-Based Diagnoses in the Early Stage of Alzheimer's Disease. J Bioeth Inq. 2018;15(2):219–230. doi: 10.1007/s11673-018-9844-y. [DOI] [PubMed] [Google Scholar]
- 40.Lee AJ, Cunningham AP, Tischkowitz M, Simard J, Pharoah PD, Easton DF, Antoniou AC. Incorporating truncating variants in PALB2, CHEK2, and ATM into the BOADICEA breast cancer risk model. Genet Med. 2016;18(12):1190–1198. doi: 10.1038/gim.2016.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hartmann LC, Lindor NM. The Role of Risk-Reducing Surgery in Hereditary Breast and Ovarian Cancer. N Engl J Med. 2016;374(5):454–468. doi: 10.1056/NEJMra1503523. [DOI] [PubMed] [Google Scholar]
- 42.AlzheimerEurope: The Value of Knowing. Findings of Alzheimer Europe’s five country survey on public perceptions of Alzheimer’s disease and views on the value of diagnosis. In. Luxembourg: Alzheimer Europe; 2011. Retrieved on 13 September 2021 from https://www.alzheimer-europe.org/Research/Value-of-Knowing.
- 43.Robinson SM, Canavan M, O'Keeffe ST. Preferences of older people for early diagnosis and disclosure of Alzheimer's disease (AD) before and after considering potential risks and benefits. Arch Gerontol Geriatr. 2014;59(3):607–612. doi: 10.1016/j.archger.2014.07.010. [DOI] [PubMed] [Google Scholar]
- 44.Smedinga M, Bunnik EM, Richard E, Schermer MHN. The Framing of "Alzheimer's Disease": Differences Between Scientific and Lay Literature and Their Ethical Implications. Gerontologist. 2021;61(5):746–55. [DOI] [PMC free article] [PubMed]
- 45.Petersen RC. Mild cognitive impairment as a diagnostic entity. J Intern Med. 2004;256(3):183–194. doi: 10.1111/j.1365-2796.2004.01388.x. [DOI] [PubMed] [Google Scholar]
- 46.Lingler JH, Sereika SM, Butters MA, Cohen AD, Klunk WE, Knox ML, McDade E, Nadkarni NK, Roberts JS, Tamres LK, et al. A randomized controlled trial of amyloid positron emission tomography results disclosure in mild cognitive impairment. Alzheimers Dementia. 2020;16(9):1330–1337. doi: 10.1002/alz.12129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Petersen RC, Lopez O, Armstrong MJ, Getchius TSD, Ganguli M, Gloss D, Gronseth GS, Marson D, Pringsheim T, Day GS, et al. Practice guideline update summary: Mild cognitive impairment: Report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology. Neurology. 2018;90(3):126–135. doi: 10.1212/WNL.0000000000004826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Grill JD, Apostolova LG, Bullain S, Burns JM, Cox CG, Dick M, Hartley D, Kawas C, Kremen S, Lingler J, et al. Communicating mild cognitive impairment diagnoses with and without amyloid imaging. Alzheimers Res Ther. 2017;9(1):35. doi: 10.1186/s13195-017-0261-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.van Maurik IS, Vos SJ, Bos I, Bouwman FH, Teunissen CE, Scheltens P, Barkhof F, Frolich L, Kornhuber J, Wiltfang J, et al. Biomarker-based prognosis for people with mild cognitive impairment (ABIDE): a modelling study. Lancet Neurol. 2019;18(11):1034–1044. doi: 10.1016/S1474-4422(19)30283-2. [DOI] [PubMed] [Google Scholar]
- 50.Ebenau JL, Timmers T, Wesselman LMP, Verberk IMW, Verfaillie SCJ, Slot RER, van Harten AC, Teunissen CE, Barkhof F, van den Bosch KA, et al. ATN classification and clinical progression in subjective cognitive decline: The SCIENCe project. Neurology. 2020;95(1):e46–e58. doi: 10.1212/WNL.0000000000009724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lopez Lopez C, Tariot PN, Caputo A, Langbaum JB, Liu F, Riviere ME, Langlois C, Rouzade-Dominguez ML, Zalesak M, Hendrix S, et al. The Alzheimer's Prevention Initiative Generation Program: Study design of two randomized controlled trials for individuals at risk for clinical onset of Alzheimer's disease. Alzheimers Dement (N Y) 2019;5:216–227. doi: 10.1016/j.trci.2019.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sperling RA, Rentz DM, Johnson KA, Karlawish J, Donohue M, Salmon DP, Aisen P. The A4 study: stopping AD before symptoms begin? Sci Transl Med. 2014;6(228):228 fs213. doi: 10.1126/scitranslmed.3007941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Frisoni GB, Barkhof F, Altomare D, Berkhof J, Boccardi M, Canzoneri E, Collij L, Drzezga A, Farrar G, Garibotto V, et al. AMYPAD Diagnostic and Patient Management Study: Rationale and design. Alzheimers Dementia. 2019;15(3):388–399. doi: 10.1016/j.jalz.2018.09.003. [DOI] [PubMed] [Google Scholar]
- 54.Green RC, Roberts JS, Cupples LA, Relkin NR, Whitehouse PJ, Brown T, Eckert SL, Butson M, Sadovnick AD, Quaid KA, et al. Disclosure of APOE genotype for risk of Alzheimer's disease. N Engl J Med. 2009;361(3):245–254. doi: 10.1056/NEJMoa0809578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Chao S, Roberts JS, Marteau TM, Silliman R, Cupples LA, Green RC. Health behavior changes after genetic risk assessment for Alzheimer disease: The REVEAL Study. Alzheimer Dis Assoc Disord. 2008;22(1):94–97. doi: 10.1097/WAD.0b013e31815a9dcc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Langlois CM, Bradbury A, Wood EM, Roberts JS, Kim SYH, Riviere ME, Liu F, Reiman EM, Tariot PN, Karlawish J, et al. Alzheimer's Prevention Initiative Generation Program: Development of an APOE genetic counseling and disclosure process in the context of clinical trials. Alzheimers Dement (N Y) 2019;5:705–716. doi: 10.1016/j.trci.2019.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Harkins K, Sankar P, Sperling R, Grill JD, Green RC, Johnson KA, Healy M, Karlawish J. Development of a process to disclose amyloid imaging results to cognitively normal older adult research participants. Alzheimers Res Ther. 2015;7(1):26. doi: 10.1186/s13195-015-0112-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Burns JM, Johnson DK, Liebmann EP, Bothwell RJ, Morris JK, Vidoni ED. Safety of disclosing amyloid status in cognitively normal older adults. Alzheimers Dementia. 2017;13(9):1024–1030. doi: 10.1016/j.jalz.2017.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Grill JD, Raman R, Ernstrom K, Sultzer DL, Burns JM, Donohue MC, Johnson KA, Aisen PS, Sperling RA, Karlawish J, et al. Short-term Psychological Outcomes of Disclosing Amyloid Imaging Results to Research Participants Who Do Not Have Cognitive Impairment. JAMA Neurol. 2020;77(12):1504-13. [DOI] [PMC free article] [PubMed]
- 60.de Wilde A, van Buchem MM, Otten RHJ, Bouwman F, Stephens A, Barkhof F, Scheltens P, van der Flier WM. Disclosure of amyloid positron emission tomography results to individuals without dementia: a systematic review. Alzheimers Res Ther. 2018;10(1):72. doi: 10.1186/s13195-018-0398-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kim H, Lingler JH. Disclosure of amyloid PET scan results: A systematic review. Prog Mol Biol Transl Sci. 2019;165:401–414. doi: 10.1016/bs.pmbts.2019.05.002. [DOI] [PubMed] [Google Scholar]
- 62.Zwan MD, van der Flier WM, Cleutjens S, Schouten TC, Vermunt L, Jutten RJ, van Maurik IS, Sikkes SAM, Flenniken D, Howell T, et al. Dutch Brain Research Registry for study participant recruitment: Design and first results. Alzheimers Dement (N Y) 2021;7(1):e12132. doi: 10.1002/trc2.12132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Fagerlin A, Zikmund-Fisher BJ, Ubel PA. Helping patients decide: ten steps to better risk communication. J Natl Cancer Inst. 2011;103(19):1436–1443. doi: 10.1093/jnci/djr318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.van de Water LF, van Kleef JJ, Dijksterhuis WPM, Henselmans I, van den Boorn HG, Vaarzon Morel NM, Schut KF, Daams JG, Smets EMA, van Laarhoven HWM. Communicating treatment risks and benefits to cancer patients: a systematic review of communication methods. Qual Life Res. 2020;29(7):1747–1766. doi: 10.1007/s11136-020-02503-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.van Maurik IS, Visser LN, Pel-Littel RE, van Buchem MM, Zwan MD, Kunneman M, Pelkmans W, Bouwman FH, Minkman M, Schoonenboom N, et al. Development and Usability of ADappt: Web-Based Tool to Support Clinicians, Patients, and Caregivers in the Diagnosis of Mild Cognitive Impairment and Alzheimer Disease. JMIR Form Res. 2019;3(3):e13417. doi: 10.2196/13417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Koenig BA, Silverberg HL. Understanding probabilistic risk in predisposition genetic testing for Alzheimer disease. Genet Test. 1999;3(1):55–63. doi: 10.1089/gte.1999.3.55. [DOI] [PubMed] [Google Scholar]
- 67.Visser LNC, Pelt SAR, Kunneman M, Bouwman FH, Claus JJ, Kalisvaart KJ, Hempenius L, de Beer MH, Roks G, Boelaarts L, et al. Communicating uncertainties when disclosing diagnostic test results for (Alzheimer's) dementia in the memory clinic: The ABIDE project. Health Expect. 2019;23(1):52–62. doi: 10.1111/hex.12964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Campbell S, Manthorpe J, Samsi K, Abley C, Robinson L, Watts S, Bond J, Keady J. Living with uncertainty: Mapping the transition from pre-diagnosis to a diagnosis of dementia. J Aging Stud. 2016;37:40–47. doi: 10.1016/j.jaging.2016.03.001. [DOI] [PubMed] [Google Scholar]
- 69.Smith AK, White DB, Arnold RM. Uncertainty--the other side of prognosis. N Engl J Med. 2013;368(26):2448–2450. doi: 10.1056/NEJMp1303295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Stiggelbout AM, Pieterse AH, De Haes JC. Shared decision making: Concepts, evidence, and practice. Patient Educ Couns. 2015;98(10):1172–1179. doi: 10.1016/j.pec.2015.06.022. [DOI] [PubMed] [Google Scholar]
- 71.van der Flier WM, Kunneman M, Bouwman FH, Petersen RC, Smets EMA. Diagnostic dilemmas in Alzheimer's disease: Room for shared decision making. Alzheimers Dement (N Y) 2017;3(3):301–304. doi: 10.1016/j.trci.2017.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Grad R, Legare F, Bell NR, Dickinson JA, Singh H, Moore AE, Kasperavicius D, Kretschmer KL. Shared decision making in preventive health care: What it is; what it is not. Can Fam Physician. 2017;63(9):682–684. [PMC free article] [PubMed] [Google Scholar]
- 73.Berger ZD, Brito JP, Ospina NS, Kannan S, Hinson JS, Hess EP, Haskell H, Montori VM, Newman-Toker DE. Patient centred diagnosis: sharing diagnostic decisions with patients in clinical practice. BMJ. 2017;359:j4218. doi: 10.1136/bmj.j4218. [DOI] [PubMed] [Google Scholar]
- 74.Stiggelbout AM, van der Weijden T, De Wit MP, Frosch D, Legare F, Montori VM, Trevena L, Elwyn G. Shared decision making: really putting patients at the centre of healthcare. BMJ. 2012;344:e256. doi: 10.1136/bmj.e256. [DOI] [PubMed] [Google Scholar]
- 75.Millard FB, Kennedy RL, Baune BT. Dementia: opportunities for risk reduction and early detection in general practice. Aust J Prim Health. 2011;17(1):89–94. doi: 10.1071/PY10037. [DOI] [PubMed] [Google Scholar]
- 76.Robinson L, Dickinson C, Magklara E, Newton L, Prato L, Bamford C. Proactive approaches to identifying dementia and dementia risk; a qualitative study of public attitudes and preferences. BMJ Open. 2018;8(2):e018677. doi: 10.1136/bmjopen-2017-018677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Bogardus ST, Jr, Holmboe E, Jekel JF. Perils, pitfalls, and possibilities in talking about medical risk. JAMA. 1999;281(11):1037–1041. doi: 10.1001/jama.281.11.1037. [DOI] [PubMed] [Google Scholar]
- 78.Lipkus IM. Numeric, verbal, and visual formats of conveying health risks: suggested best practices and future recommendations. Med Decis Mak. 2007;27(5):696–713. doi: 10.1177/0272989X07307271. [DOI] [PubMed] [Google Scholar]
- 79.Petersen RC, Doody R, Kurz A, Mohs RC, Morris JC, Rabins PV, Ritchie K, Rossor M, Thal L, Winblad B. Current concepts in mild cognitive impairment. Arch Neurol. 2001;58(12):1985–1992. doi: 10.1001/archneur.58.12.1985. [DOI] [PubMed] [Google Scholar]
- 80.Frisoni GB, Ritchie C, Carrera E, Nilsson P, Ousset PJ, Molinuevo JL, Dubois B, Scheltens P, Minoshima S. Re-aligning scientific and lay narratives of Alzheimer's disease. Lancet Neurol. 2019;18(10):918–919. doi: 10.1016/S1474-4422(19)30323-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Supplement A. Summary of recommendations on how to disclose test results for dementia risk assessment in context of clinical trials. Supplement B. The Barcelonaβeta Dementia Prevention Study (BBDPS) and its associated registry. Figure B1. Schematic representation of the BBDPS. Table B1. Sample characteristics of the BBDPS participants at baseline visit. Figure B2. Impact of dementia risk disclosure on 69 low-risk versus 20 high-risk individuals with SCD from the BBDPS.
Data Availability Statement
The data that support the findings of the BBDPS of are available from the corresponding author Carolina Minguillon, upon reasonable request.