Abstract
Objectives
We aimed to investigate whether the implementation of personal protective measures against COVID-19 reduced the transmission of influenza-like illnesses.
Methods
We followed 758 international students from 95 countries located in 5 continents from October 2020 to March 2021. Their frequency of wearing masks, physical distancing, washing hands, and avoiding crowded places, as well as their reported cases of influenza-like illnesses, were examined. We used Kaplan-Meier analysis to compare the occurrence of symptoms of influenza-like illnesses among participants who adhered with those who did not adhere to the personal protective measures.
Results
From October 2020 to March 2021, 139 (18%) students reported symptoms of influenza-like illnesses. The survival analysis showed that students who frequently wore face masks, exercised physical distancing, and disinfected their hands had a reduced risk of influenza-like illnesses. We found a two-fold increased risk of influenza-like illnesses among participants who did not implement all the personal protective measures compared with those who adhered to the measures (hazard ratio=2.16, 95% CI=1.53-3.05, P<0.001).
Conclusions
Our findings suggest that personal protective measures with high feasibility and acceptability could be implemented during influenza epidemics to reduce transmission.
INTRODUCTION
After the widespread implementation of measures to mitigate COVID-19, influenza activity and influenza-like illnesses declined sharply (Olsen et al., 2020). The observed decline was attributed to artifactual changes related to hospital-seeking behaviors for respiratory illnesses and real changes related to a reduction in circulating respiratory viruses because of the implementation of non-pharmaceutical interventions against COVID-19. Influenza data reported to the World Health Organization's (WHO) FluNet platform in 2021 showed a continued decline in most countries and regions in the Northern Hemisphere, temperate zones, and Southern Hemisphere in influenza-positive results and outpatient visits for influenza-like illnesses (WHO 2021a). The transmissibility of the SARS-CoV-2 (R0=2–6.1) (Ke et al., 2021) is higher than that of influenza (R0=1.28) (Biggerstaff et al., 2014), which suggests that the coronavirus may have played a role in interrupting transmission of circulating influenza.
SARS-CoV-2, like other viruses that cause acute respiratory infections, spreads primarily by respiratory droplets. Thus, the practice of personal protective measures to protect against COVID-19 may have resulted in the decline in influenza-like illnesses during the 2020–2021 flu season. The WHO recommended the following protective measures against COVID-19 transmission: washing hands; keeping physical distance; avoiding touching eyes, nose and mouth; staying at home if you are sick; wearing masks; disinfecting frequently touched objects and surfaces; and avoiding the 3Cs (crowded places, close contacts, and closed spaces) (WHO 2021b). Evidence supports that wearing facemasks, protecting the eyes, physical distancing (Chu et al., 2020), and hand hygiene (Alzyood et al., 2020) can protect against the transmission of SARS-CoV-2. However, data on the effectiveness of these measures in preventing community transmission of influenza-like illnesses are lacking (Olsen et al., 2020; Cowling et al., 2020). We aimed to investigate the association between the implementation of personal protective measures and cases of influenza-like illnesses in the general population by following a group of international students from 95 countries located in 5 continents from October 2020 to March 2021.
METHODS
Data collection
We conducted a longitudinal observational study to assess cases of influenza-like illnesses among international students during the 2020–2021 flu season. Data collection commenced in October 2020 and concluded at the end of March 2021. Participants of this study comprised international students aged ≥18 years enrolled in undergraduate or postgraduate programs in universities in Turkey. The participants were identified from a database of international students on the Turkish Scholarship at the Presidency for Turks Abroad and Related Communities. We collected data through monthly online surveys delivered to the participants through their students’ information systems. We explained the purpose of the study and the confidentiality of responses to the students. The students gave informed consent before participating in the study. Potential participants were screened based on the responses given in the baseline questionnaire to determine whether they met the study's inclusion criteria. Participants enrolled answered questions about their frequency of implementing personal protective measures and if they experienced symptoms of influenza-like illnesses in the previous month.
We assessed respondents’ level of personal protective measures using 5 items recommended by the WHO: the frequency of wearing facemasks, physical distancing, hand hygiene, surface disinfection, and avoiding crowded places. Participants reported their frequency of implementing the measures using a 5-Likert scale. The scale reliability was examined because it had not been validated previously in the context of this research. Cronbach's alpha test was calculated for all participants. Results indicated that the scale had good reliability (α=0.81, 95% CI 0.79–0.83). The survey forms were also pretested on a convenience sample of 50 male and 50 female international students (n=100) outside the target group to ensure clarity of interpretation and improve the validity of responses. We assessed influenza-like illnesses by symptoms of an acute respiratory infection with an onset within 10 days, fever of >38°C, and persistent cough in the absence of an alternative causative agent (Stellrecht, 2017). Students who reported symptoms of fever, sore throat, and persistent cough and did not receive any confirmatory tests were regarded as having symptoms of influenza-like illnesses, consistent with the WHO's case definition of influenza-like illnesses. Ethical approval for this study was obtained from the Non-Interventional Clinical Research Ethics Committee of Hacettepe University (No. GO 20/885), and all participants gave informed consent. Moreover, approval for the study was obtained from the Ministry of Health of the Republic of Turkey.
Statistical analysis
We first grouped categorical variables with ordinal response scales, including the level of personal protective measures. We grouped responses to the frequency of wearing facemasks, washing hands, physical distancing, avoiding crowded places, and disinfecting surfaces into 3 groups: 2 (Frequently or Always), 1 (Sometimes) and 0 (Never). All participants implemented some of the measures to some extent to protect themselves from coronavirus infection. The personal protective measures scores (0, 1 or 2) were added for each student to give the overall implementation of personal protective measures, with 0 and 10 being the lowest and highest possible score, respectively. We compared the frequency of practicing personal protective measures among students who had influenza-like illnesses with those who did not.
We estimated the first occurrence of influenza-like illnesses over the 2020–2021 flu season using Kaplan-Meier analysis. Before conducting the survival analysis, the assumption of homogeneity of variances was tested and satisfied based on Levene's F-test (F=1.43, P=0.49). We compared the 6-month survival of the students who implemented all the personal protective measures with those who did not, with the event of interest determined as experiencing symptoms of influenza-like illnesses or censoring. We used a log rank test to compare and understand the differences between the survival distributions. Using a multivariate Cox regression (proportional hazards) analysis, we examined the association between students’ level of implementing personal protective measures against COVID-19 and the occurrence of influenza-like illnesses, factoring in the time of observation or censoring (loss to follow-up). The first regression analysis included covariates such as gender, age, country of origin, and current smoking status, in addition to the implementation of personal protective measures. The initial results showed that gender (P=0.71), age (P=0.59), country of origin (P=0.65), and smoking (P=0.26) did not significantly affect the symptoms of influenza-like illnesses. Therefore, the covariates were removed from the regression model, and the analysis was rerun with only the 6 personal protective measures against COVID-19 (wearing facemasks, hand hygiene, physical distancing, surface disinfection, and avoiding crowded places) set as the covariates. All statistical analyses were done with R version 4.3.3.
Results
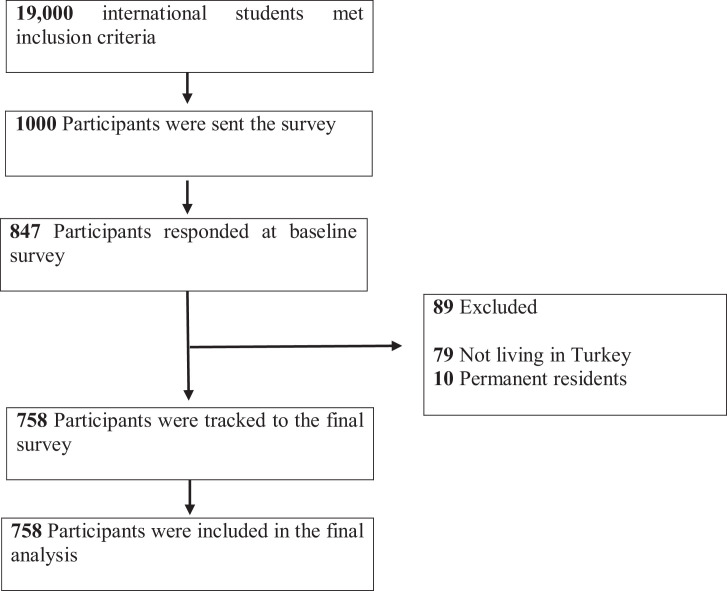
Of the total students who received the survey (n=1000), 847 students agreed to participate and took part in the baseline survey (response rate 84.7%) Figure 1 . We excluded 79 students from the study because they were not enrolled in universities in Turkey at the time of the study. An additional 10 students were excluded because they reported being permanent residents in Turkey, thus, did not meet the classification of an international student. Therefore, we sent monthly follow-up surveys to 758 students who met the inclusion criteria (Table 1 ) at the beginning of every month, from November 2020 to March 2021, and a reminder in the middle of every month to maximize the response rate.
Figure 1.
Participant enrollment.
Table 1.
Demographic characteristics of study population
| Characteristic | Male (n=383) |
Female (n=365) |
Total (n=758) |
|||
| N | % | N | % | N | % | |
| Age | ||||||
| ≤20 | 65 | 17.0 | 64 | 17.1 | 129 | 17.0 |
| 21–25 | 120 | 31.3 | 160 | 42.7 | 280 | 36.9 |
| 26–30 | 114 | 29.8 | 102 | 27.2 | 216 | 28.5 |
| 31–35 | 70 | 18.3 | 38 | 10.2 | 108 | 14.2 |
| 36–40 |
14 | 3.7 | 11 | 2.9 | 25 | 3.3 |
| Country | ||||||
| Asia | 178 | 46.5 | 191 | 50.9 | 369 | 48.7 |
| Africa | 182 | 47.5 | 123 | 32.8 | 305 | 40.3 |
| Europe | 22 | 5.7 | 55 | 14.7 | 77 | 10.1 |
| North and South America |
1 | 0.3 | 6 | 1.6 | 7 | 0.9 |
| Residence | ||||||
| Apartment / House | 198 | 51.7 | 174 | 46.4 | 372 | 49.1 |
| Dormitory |
185 | 48.3 | 201 | 53.6 | 386 | 50.9 |
| Chronic disease | ||||||
| Yes | 13 | 3.4 | 19 | 5.1 | 32 | 4.2 |
| No |
370 | 96.6 | 356 | 94.9 | 726 | 95.8 |
| Smoking | ||||||
| Yes | 52 | 13.6 | 26 | 6.9 | 78 | 10.3 |
| No | 331 | 86.4 | 349 | 93.1 | 680 | 89.7 |
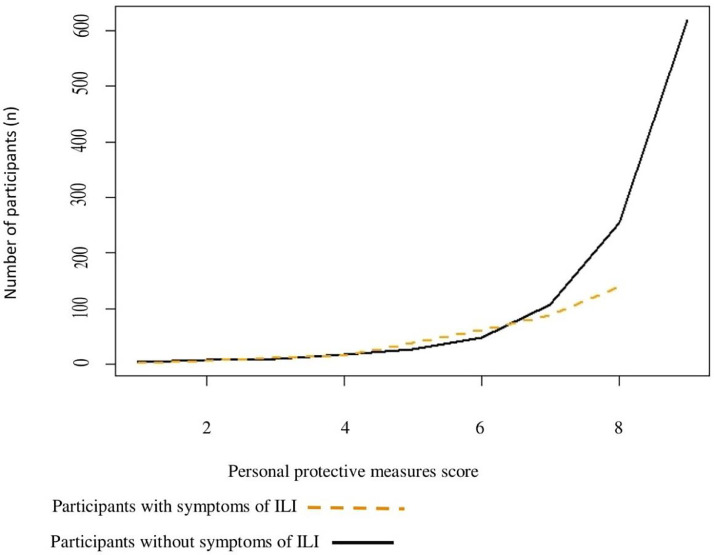
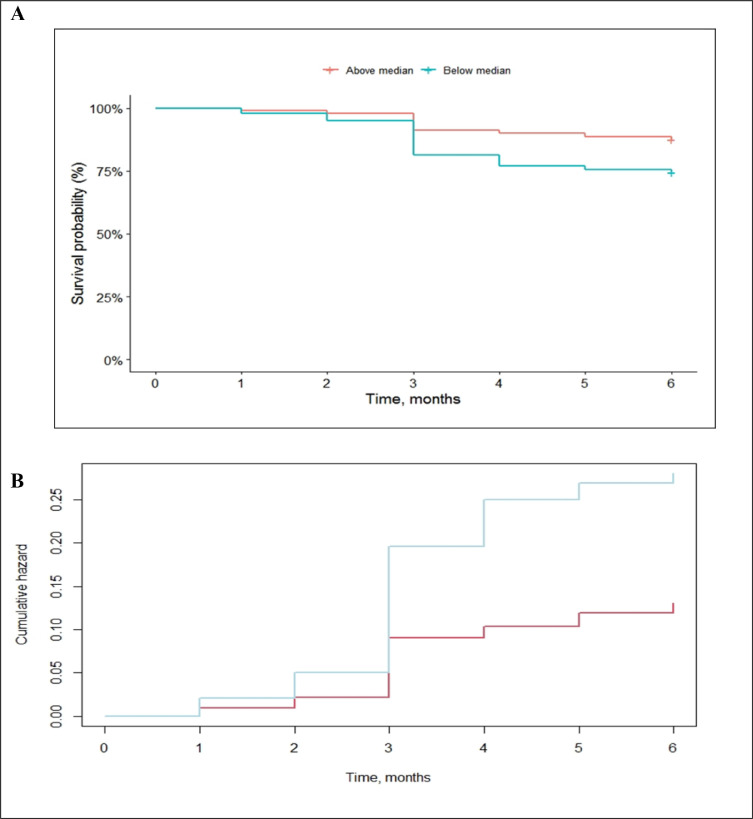
A total of 139 (18%) international students reported symptoms of acute respiratory infections between October 2020 and March 2021 (Figure 2 ). Table 2 shows the implementation of personal protective measures by the students. We found that participants who did not have symptoms of influenza-like illnesses reported higher implementation of all the personal protective measures than those who experienced symptoms. We observed that the level of personal protection against COVID-19 was higher among students who did not have influenza-like illnesses (Figure 3 ), further indicating a link between implementation of the measures against coronavirus and cases of influenza-like illnesses. Of the students who had influenza-like illnesses, 62.6% (n=87) had scores below the median and 37.4% (n=52) had scores above the median person protective measure. Results of the survival analysis showed that the overall probability of being event-free among students with personal protective measure scores above the median was higher than students who had scores below the median (Figure 4 ). There was a significant difference in survival distribution between participants who scored below the median and those who scored above the median, log-rank χ2=23, P<0.001. The results from the Kaplan Meier method showed that international students who adhered to implementing the personal protective measures had a reduced risk of acquiring respiratory infections.
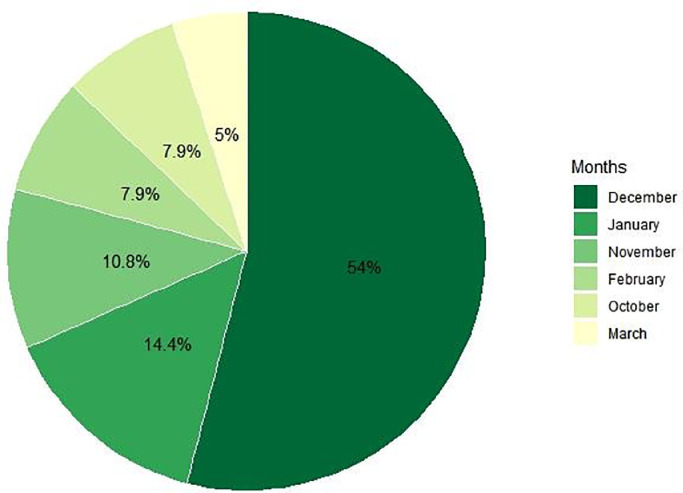
Figure 2.
Percentage of participants who reported symptoms of influenza-like illnesses by month between October 2020 and March 2021
More than half of reported cases of influenza-like illnesses (54.0%) occurred in December 2020. The least reported cases of influenza-like illnesses occurred in March 2021 (5.0%).
Table 2.
The percentage of participants for each frequency of personal protective measure recommended by the World Health Organization
| N | 1. Never |
1. Sometimes |
2. Always/Frequently |
||||
| N | % | N | % | N | % | ||
| Participants with influenza-like illnesses Facemask |
139 |
- |
- |
6 |
4.3 |
133 |
95.7 |
| Physical distancing | 139 | - | - | 56 | 40.3 | 83 | 59.7 |
| Hand hygiene | 139 | 5 | 3.6 | 20 | 14.4 | 114 | 82.0 |
| Surface disinfection | 139 | 14 | 10.1 | 43 | 30.9 | 82 | 59.0 |
| Avoiding crowds | 139 | 3 | 2.2 | 48 | 34.5 | 88 | 63.3 |
|
Participants without influenza-like illnesses Facemask |
619 |
1 |
0.2 |
8 |
1.3 |
610 |
98.5 |
| Physical distancing | 619 | 8 | 1.3 | 72 | 11.6 | 539 | 87.1 |
| Hand hygiene | 619 | 8 | 1.3 | 46 | 7.4 | 565 | 91.3 |
| Surface disinfection | 619 | 18 | 2.9 | 165 | 26.7 | 436 | 70.4 |
| Avoiding crowds | 619 | 10 | 1.6 | 92 | 14.9 | 517 | 83.5 |
Chi square (with Fisher's exact test) was used to compare the implementation of personal protective measures between participants who had influenza-like illnesses and those who did not. There was a significant difference in the use of facemask (P=0.006), physical distancing (P<0.001), hand hygiene (P=0.004), surface disinfection (P=0.0002), and avoiding crowded places (P<0.001).
Figure 3.
Personal protective measure score (PPMS) among students with and without symptoms of influenza-like illnesses PPMS was calculated from students’ frequency of wearing facemasks, physical distancing, hand hygiene, surface disinfection, and avoiding crowded places. We assigned scores of 2, 1 and 0 to students who always/frequently, sometimes, and never implemented a specific measure. We then calculated the PPMS by adding the sum of the scores for each of the 5 measures; therefore, the highest potential PPMS was 10, and the lowest was 0.
Figure 4.
A Survival probability of students with personal protective measures above the median (red) and below the median (blue) score. B Cumulative hazard plot of students with personal protective measures above the median (red) and below the median (blue) score.
Having identified that students’ implementation of personal protective measures played a role in the observed decline in influenza-like illnesses cases, we conducted a Cox proportional hazard regression analysis to determine the measure that offered the highest protection. The regression analysis showed that at a given point in time, students who wore facemasks were 33.6% less likely to show symptoms of influenza-like illnesses than students who did not wear a facemask, adjusting for all the other personal protective measures (hazard ratio=0.664, 95% CI=0.494–0.893, P=0.006) Table 3. Similarly, students who exercised physical distancing measures were 23.5% less likely to report symptoms of influenza-like illnesses when compared with those who did not adhere to physical distancing adjusting for the other measures (hazard ratio=0.765, 95% CI=0.610–0.960, P=0.020). Furthermore, international students who frequently disinfected their hands were 17.1 % less likely to report symptoms of influenza-like illnesses than those who did not frequently disinfect their hands (hazard ratio=0.821, 95% CI=0.793–0.915, P=0.029). We found a two-fold increased risk of influenza-like illnesses among students who did not implement every personal protective measures compared with those who adhered to all the measures (HR=2.16, 95% CI=1.53–3.05, P<0.001). There was no significant association between surface disinfection (P=0.298) and avoiding crowded places (P=0.730) with the reported symptoms of influenza-like illnesses among the participants.
Table 3.
Associations between personal protective measures recommended by the World Health Organization and the cases of influenza-like illnesses
| Covariates | Hazard ratio (HR) | 95% CI of HR | P-value |
| Facemask | 0.664 | 0.494 - 0.893 | 0.006* |
| Physical distancing | 0.765 | 0.610 - 0.960 | 0.020* |
| Hand hygiene | 0.829 | 0.793 - 0.915 | 0.029* |
| Surface disinfection | 0.895 | 0.724 - 1.104 | 0.298 |
| Avoiding crowded places | 0.964 | 0.781 - 1.189 | 0.730 |
Shown is the P-value <0.05, which indicated a significant relationship. The analysis included all 758 international students.
Discussion
Our findings suggest that in addition to the public health measures (including curfews, restrictions on mass gatherings, quarantine measures, and border entry restrictions), personal measures against COVID-19 protect people from acute respiratory infections. Given that international students hesitate to visit healthcare services and often delay accessing healthcare (Masai et al., 2021 Apr 7), the findings of this study provide important information on these students’ reported cases of influenza-like illnesses, which may not be captured in hospital visits. The current study showed that the overall probability of being free of influenza-like illnesses between October 2020 and March 2021 among participants who adhered to the personal protective measures was higher than those who did not adhere to the measures. This finding supports the consensus that personal COVID-19 measures prevented transmission of acute respiratory infections, including influenza-like illnesses.
Influenza data reported to the WHO's FluNet platform in 2021 showed a continued decline in confirmed influenza-positive results and outpatient visits for influenza-like illnesses (WHO 2021a). The findings of our study suggest that although personal COVID-19 measures prevented transmission of respiratory infections in the community, changes in hospital-seeking behavior could potentially have resulted in much lower consultations for influenza-like illnesses . Our findings provide wider evidence of cases of acute respiratory infections in the community during the 2020–2021 flu season, as well as the impact of personal measures (including wearing facemasks, washing hands, physical distancing, disinfecting surfaces, and avoiding crowded places) on the transmission of respiratory infections among students.
Cox proportional hazard regression analysis showed that students who wore facemasks were 33.6% less likely to show symptoms of influenza-like illnesses than students who did not after adjusting for all the other personal protective measures (hazard ratio=0.664, 95% CI=0.494–0.893, P=0.006). The current study did not distinguish between cloth, surgical and N95 masks. Thus, study results showed the effectiveness of wearing masks in general among the international student population. Previous studies have shown that facemasks effectively prevent the transmission of respiratory infections (Leung et al., 2020). The present study investigated the impact of personal protective measures in influenza-like illnesses by observing a group of international students from 95 countries over 6 months. Additionally, our study found that the compliance rate of mask-wearing among international students was high (97.87%). Therefore, the results of this study provide a reliable estimate of the impact of wearing masks in preventing acute respiratory infections among students in a context where facemasks are widely adopted.
We also identified an association between students’ practice of physical distancing measures and cases of influenza-like illnesses. The percentage of students with symptoms of influenza-like illnesses who always or frequently implemented physical distancing measures was significantly lower when compared with students without symptoms of influenza-like illnesses (P<0.001). Furthermore, students who adhered to physical distancing measures were 23.5% less likely to report symptoms of influenza-like illnesses when compared with those who did not, adjusting for the other measures (hazard ratio= 0.765, 95% CI=0.610–0.960, P=0.020). The study finding is consistent with findings from previous studies, which have shown that physical distancing measures effectively interrupt the transmission of respiratory viruses (Chu et al., 2020; Poole et al., 2020). For example, one study showed that influenza transmissibility declined by 44% after implementing physical distancing measures and changes in population behavior (Cowling et al., 2020).
Previous studies have shown that hand hygiene reduces respiratory infections by 16%–21% (Aiello et al., 2008). The present study also showed a significant association between the frequency of handwashing/disinfection and reported cases of influenza-like illnesses among international students. In particular, students who frequently disinfected their hands were 17.1% less likely to report symptoms of influenza-like illnesses than those who did not frequently disinfect their hands (hazard ratio=0.821, 95% CI=0.793–0.915, P=0.029). Since the compliance rate among study participants was high, with 91.56% (n=694) of the students reporting always or frequently disinfecting their hands, the results of this study provide a reliable estimate of the impact of hand hygiene in preventing influenza-like illnesses in the context of a pandemic.
We did not find any significant association between cases of influenza-like illnesses and avoiding crowded places. Evidence exists in the literature on the benefits of reducing social mixing (e.g., Prem et al., 2020); however, evidence on the direct impact of avoiding crowded places in preventing respiratory virus infection in individuals remains scarce. Additionally, our study did not find a significant association between surface disinfection and reported cases of influenza-like illnesses among international students. This non-significant finding may be due to the study setting and the target population. A previous study has shown that surface disinfection effectively reduces secondary COVID-19 transmission in households (Wang et al., 2020). In the present study, we observed the international students’ practice of personal COVID-19 measures in the community.
Overall, adherence to the 5 personal protective measures recommended by the WHO prevented cases of influenza-like illnesses among international students enrolled in this study. We found that participants who did not implement every measure were 2 times more likely to have influenza-like illnesses than students who frequently implemented all the measures (hazard ratio=2.16, 95% CI=1.53–3.05). This finding demonstrates that the personal protective measures worked synergistically with the implementation of all measures offering higher protection to international students compared with single measures.
Our study has some limitations. First, participants in the study gave a self-reported evaluation of their implementation of personal protective measures against COVID-19, which may have led to a possible overestimation of their implementation. To resolve any potential social desirability bias, we used anonymous online surveys and assured them of the confidentiality of their responses at the introductory part of every survey. Second, the study evaluated the preventive effects of 5 personal protective measures; other measures may have contributed to suppressing transmission of respiratory infections. Third, the study was conducted on students, limiting the findings' generalizability to the general population. Despite these limitations, to the best of our knowledge, this is the first study to explore the practice of personal protection measures and the risk of influenza-like illnesses during the 2020–2021 flu season.
In conclusion, our study found that personal measures to protect against COVID-19 (including wearing facemasks, hand hygiene and physical distancing) prevented the transmission of acute respiratory infections during the 2020–2021 flu season. Our findings suggest that personal protective measures with high feasibility and acceptability could be implemented during influenza epidemics to reduce transmission, particularly in populations at the highest risk of developing severe complications. Therefore, future studies should investigate the utility of these measures in people who are at risk of severe complications.
Contributors
ANM designed the study, collected and analyzed the data, and prepared and revised the manuscript. LA designed and supervised the study, analyzed the data, and revised the manuscript.
Declaration of Competing Interests
All authors declare no competing interests.
Acknowledgments
Data sharing
The datasets supporting the conclusions of this article are available from the corresponding author and can be shared upon request.
Acknowledgments
The authors wish to thank all international students who gave their time to participate in the study.
Funding
We did not receive any funding for this research.
References
- Aiello AE, Coulborn RM, Perez V, Larson EL. Effect of hand hygiene on infectious disease risk in the community setting: a meta-analysis. Am J Public Health. 2008;98(8):1372–1381. doi: 10.2105/AJPH.2007.124610. Aug. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alzyood M, Jackson D, Aveyard H, Brooke J. COVID-19 reinforces the importance of handwashing. J Clin Nurs. 2020;29(15-16):2760–2761. doi: 10.1111/jocn.15313. Aug. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biggerstaff M, Cauchemez S, Reed C, Gambhir M, Finelli L. Estimates of the reproduction number for seasonal, pandemic, and zoonotic influenza: a systematic review of the literature. BMC Infect Dis. 2014 Sep 4;14:480. doi: 10.1186/1471-2334-14-480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu DK, Akl EA, Duda S, Solo K, Yaacoub S, Schünemann HJ. COVID-19 Systematic Urgent Review Group Effort (SURGE) study authors. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. 2020 Jun 27;395(10242):1973–1987. doi: 10.1016/S0140-6736(20)31142-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cowling BJ, Ali ST, Ng TWY, Tsang TK, Li JCM, Fong MW, et al. Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: an observational study. Lancet Public Health. 2020;5(5):e279–e288. doi: 10.1016/S2468-2667(20)30090-6. May. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stellrecht KA, Chapter 11 - Molecular Testing for Respiratory Viruses, Editor(s): William B. Coleman, Gregory J. Tsongalis, Diagnostic Molecular Pathology, Academic Press, 2017, Pages 123-137, ISBN 9780128008867, https://doi.org/ 10.1016/B978-0-12-800886-7.00011-X.
- Ke R, Romero-Severson E, Sanche S, Hengartner N. Estimating the reproductive number R0 of SARS-CoV-2 in the United States and eight European countries and implications for vaccination. J Theor Biol. 2021 May 21;517 doi: 10.1016/j.jtbi.2021.110621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung NHL, Chu DKW, Shiu EYC, Chan KH, McDevitt JJ, Hau BJP. Author Correction: Respiratory virus shedding in exhaled breath and efficacy of face masks. Nat Med. 2020;26(6):981. doi: 10.1038/s41591-020-0946-9. Jun. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masai AN, Güçiz-Doğan B, Ouma PN, Nyadera IN, Ruto VK. Healthcare services utilization among international students in Ankara, Turkey: a cross-sectional study. BMC Health Serv Res. 2021 Apr 7;21(1):311. doi: 10.1186/s12913-021-06301-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olsen SJ, Azziz-Baumgartner E, Budd AP, Brammer L, Sullivan S, Pineda RF, Cohen C, Fry AM. Decreased Influenza Activity During the COVID-19 Pandemic - United States, Australia, Chile, and South Africa, 2020. MMWR Morb Mortal Wkly Rep. 2020 Sep 18;69(37):1305–1309. doi: 10.15585/mmwr.mm6937a6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poole S, Brendish NJ, Tanner AR, Clark TW. Physical distancing in schools for SARS-CoV-2 and the resurgence of rhinovirus. Lancet Respir Med. 2020;8(12):e92–e93. doi: 10.1016/S2213-2600(20)30502-6. Dec. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prem K, Liu Y, Russell TW, Kucharski AJ, Eggo RM, Davies N, Jit M, Klepac P., Centre for the Mathematical Modelling of Infectious Diseases COVID-19 Working Group The effect of control strategies to reduce social mixing on outcomes of the COVID-19 epidemic in Wuhan, China: a modelling study. Lancet Public Health. 2020;5(5):e261–e270. doi: 10.1016/S2468-2667(20)30073-6. May. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y, Tian H, Zhang L, Zhang M, Guo D, Wu W, et al. Reduction of secondary transmission of SARS-CoV-2 in households by face mask use, disinfection and social distancing: a cohort study in Beijing, China. BMJ Glob Health. 2020;5(5) doi: 10.1136/bmjgh-2020-002794. May. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. 2021a. FluNet summary Available at: https://www.who.int/tools/flunet/flunet-summary. (Accessed 10 April 2021)
- World Health Organization. 2021b. Coronavirus disease (COVID-19) advice to the public. Available at. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public. (Accessed 25 July 2021)