Abstract
This paper conducts a comparative review of the (curative) health systems’ response taken by Cyprus, Greece, Israel, Italy, Malta, Portugal, and Spain during the first six months of the COVID-19 pandemic. Prior to the COVID-19 pandemic, these Mediterranean countries shared similarities in terms of health system resources, which were low compared to the EU/OECD average. We distill key policy insights regarding the governance tools adopted to manage the pandemic, the means to secure sufficient physical infrastructure and workforce capacity and some financing and coverage aspects.
We performed a qualitative analysis of the evidence reported to the ‘Health System Response Monitor’ platform of the European Observatory by country experts. We found that governance in the early stages of the pandemic was undertaken centrally in all the Mediterranean countries, even in Italy and Spain where regional authorities usually have autonomy over health matters. Stretched public resources prompted countries to deploy “flexible” intensive care unit capacity and health workforce resources as agile solutions. The private sector was also utilized to expand resources and health workforce capacity, through special public-private partnerships. Countries ensured universal coverage for COVID-19-related services, even for groups not usually entitled to free publicly financed health care, such as undocumented migrants.
We conclude that flexibility, speed and adaptive management in health policy responses were key to responding to immediate needs during the COVID-19 pandemic. Financial barriers to accessing care as well as potentially higher mortality rates were avoided in most of the countries during the first wave. Yet it is still early to assess to what extent countries were able to maintain essential services without undermining equitable access to high quality care.
Keywords: COVID-19, health system responses, governance, Mediterranean countries
1. Introduction
Mediterranean European countries, which are the focus of this paper, were impacted in similar ways by the COVID-19 pandemic in spring 2020, albeit with different intensities. The seven countries included in this article (Cyprus, Greece, Israel, Italy, Malta, Portugal and Spain) are geographically linked in that they surround or are situated within the Mediterranean Sea. It is important to note upfront, that while these countries share some important similarities, they have different sizes, populations, wealth and culture, as well as different political structures and health systems. The most obvious differences relate to geographical and population sizes, with Italy and Spain having large territories and populations (60 and 47 million residents, respectively) that rank within the top five among European Union (EU) countries, whereas Greece, Israel and Portugal all have populations around 8 – 10 million and Malta and Cyprus are small island states of half a million and 900 0001 people, respectively [1].
Politically, Italy and Spain have quasi-federal, de-centralized governance arrangements with significant powers delegated to their regional governments, including for running regional health systems and services. In contrast, the other five countries have much more centralized governance structures for their national health systems. Regarding the health system, the majority of the countries in this group (Cyprus, Italy, Malta, Portugal, Spain) have National Health Service type systems that are predominantly tax-financed, while Cyprus, Israel and Greece (since 2011 reforms) have a mixed model combining contributions by residents and taxes through the state budget. While Greece has a single insurer, Israel has a National Health Insurance with four insurers. Population coverage for health care is universal in all the countries, and except in Greece, general practitioners (GPs) are gatekeepers for specialist care [2], [3], [4], [5], [6], [7], [8], [9].
Different levels of resources may facilitate different types of responses to COVID-19; hence a cross-country comparison should attempt to hold the baseline of resources constant and compare among similar countries. Prior to the pandemic, Mediterranean countries shared important similarities in terms of health system resources, which were low when compared to the EU/OECD average. We argue that the similar level of resources (see below) represented a similar starting point when responding to the COVID-19 pandemic, which makes this cross-country comparison possible and meaningful. Thus, when analyzing the health systems’ response among this group of countries, we were able to identify strategies that are related to the level of resources at their disposal and differentiate these from those related to other considerations.
In particular, all seven countries have lower than average health spending (and shares of public funding) for their health systems. Health expenditure as a share of GDP ranged from a low of 6.8% in Cyprus to a high of 9.5% in Portugal in 2018 (the EU27 average was 7%). Yet, the levels of public funding for health care is much lower than the EU average (79.4%) in all of the countries, and in the cases of Cyprus (43%), Greece (59%), Israel (65%) and Malta (64%), significantly lower. Conversely, the share of health spending paid out- of-pocket in all seven countries is substantially higher than the EU average (15.9%), ranging from 21-27% in Italy, Israel, Spain and Portugal, 35% in Malta, 37% in Greece and 45% in Cyprus [1,10].
Infrastructure and personnel resources were important in providing health services (both COVID-19 related and unrelated) during the initial phase of the pandemic. In this respect, the physical resources available to each country's health system vary, but one similarity is notable: all have lower numbers of curative care hospital beds than the average across EU or OECD countries. Relatedly, one of the most important resources to treat COVID-19 patients is ICU beds. The rate of ICU beds per population prior to the pandemic varied among Mediterranean countries, ranging from 11.5 beds per 100,000 population in Cyprus to 5.2 in Greece (see Table 1 ).
Table 1.
Selected health resources indicators per 100,000 population before the pandemic
| Physicians per 100,000 population | Nurses per 100,000 population | Curative care beds per 100,000 population | ICU beds per 100,000 population | |
|---|---|---|---|---|
| Cyprus | 407.32 | 542.10 | 330.09 | 11.5 (public hospitals) |
| Greece | 610.40 | 336.52 | 363.47 | 5.2 |
| Israel | 322.00 | 589.00 | 218 | 8 |
| Italy | 397.71 | 574.21 | 258.54 | 8.42 |
| Malta (including Gozo) | 397.21 | 778.33 | 319.01 | 5.4 |
| Portugal | 515.04 | 688.01 | 329.16 | 4.4 |
| Spain | 402.08 | 586.85 | 249.67 | 9.7 |
| EU27 average (excludes Israel) | 350 | 880 | 450 | 11.5 (2010) |
The health workforce, in particular, is the foundation for ensuring accessibility of services; it represented one of the main bottlenecks in the health systems’ response during upsurges of COVID-19 cases. All the countries covered here record significantly lower numbers of nurses per 100 000 population than the average across EU countries (880), with Greece recording the lowest (336) and Malta the highest (778). On the other hand, Mediterranean countries have above-the-average physician ratios [1,10]. But in some, the average age of physicians is high. Italy and Israel have the oldest medical practitioners among OECD countries, with 55% and 50% over the age of 55, respectively, in 2017, compared to an OECD average of 34% [10]. An older medical staff might have been one of the critical issues during the emergency phase of the pandemic: given the high incidence of complications of the disease in older individuals, many of the physicians treating COVID-19 patients became severely ill themselves, reducing even further the available workforce, while other doctors might have refrained from being in direct contact with COVID-19 patients [18] (I-COM, 2020).
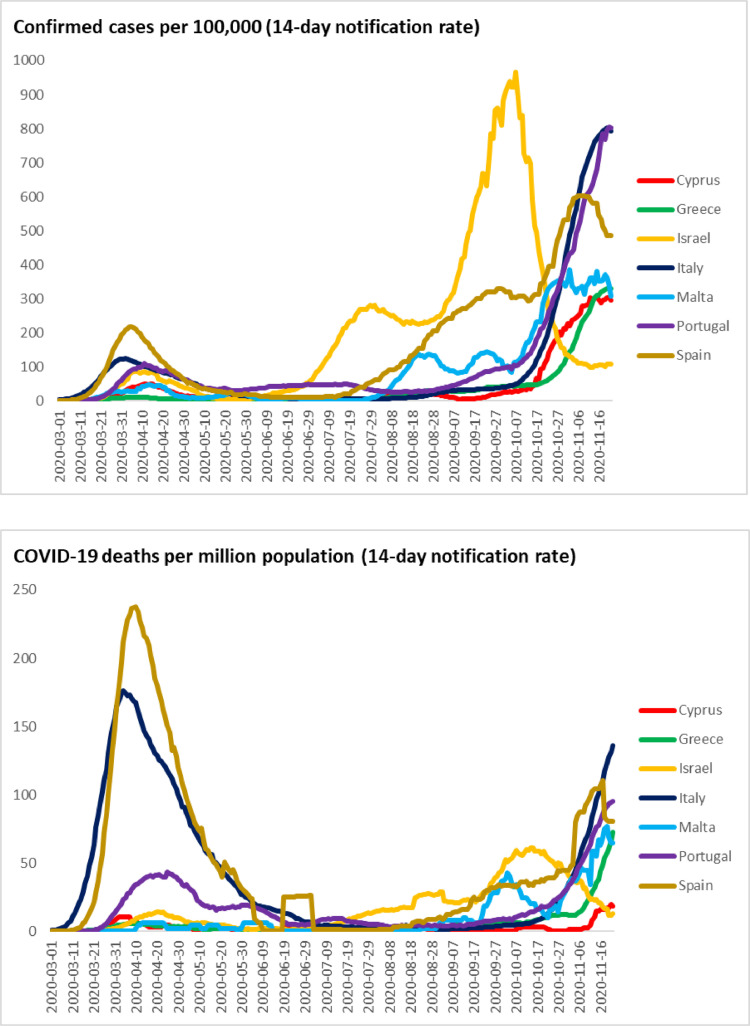
Among the Mediterranean countries, Italy and Spain reported their first cases on 30-31 January 2020. COVID-19 cases were then reported in February in Israel and Greece, finally reaching Portugal, Malta, and Cyprus as late as early March (see Fig. 1 ). Italy and Spain were severely impacted by the first wave of the pandemic, both in terms of recorded cases and number of deaths. By 22 April, both Spain and Italy had nearly 200 000 cases [19,21] with the first and second highest COVID-19 mortality burden in Europe [20]. Following the significant decline in the number of daily cases in May2 2020 and the relaxation of lockdown measures, as well as the reopening of borders for tourism over the 2020 summer, infection rates subsequently surged and by mid-October 2020 all of the countries had re-imposed stricter virus mitigation measures, including local lockdowns.
Fig. 1.
Overview of COVID-19 14-day incidence rates and crude deaths in Mediterranean group countries, March – November 2020.
Source: [20].
This article compares the initial health systems’ response to COVID-19 implemented by Cyprus, Greece, Israel, Italy, Malta, Portugal and Spain in the first six months of the COVID-19 pandemic and identifies some key lessons. The article does not try to assign causality between any measure and outcomes or assess whether countries have dealt better with the pandemic than others. Rather, the analysis intends to draw out common patterns, key contrasts, and innovative approaches in the early responses aimed at addressing similar challenges. We focus on health systems’ response related to the (curative) health system, excluding public health measures. The main period of analysis corresponds to the initial outbreak in Europe (February-May, 2020; defined as the ‘first wave’), with some reflections addressing the subsequent months until the end of September 2020. The “second wave” of the pandemic had different timings in the different countries, and we define it as the period between August and October 2020. We focus on the first six months of the pandemic because it was the period that we could most identify changes compared to the starting point in terms of resources, workforce, and governance.
2. Methods
This analysis builds on the methodology and content compiled in the COVID-19 Health System Response Monitor (HSRM). The HSRM was a tool established in March 2020 and designed in response to the COVID-19 outbreak to collect and disseminate up-to-date information on how countries, mainly in the WHO European Region, are responding to the crisis, focused primarily on the responses of health systems (see www.covid19healthsystem.org). It was a joint initiative by the European Observatory on Health Systems and Policies, the WHO Regional Office for Europe and the European Commission.
The information was collected and regularly updated by country experts, by way of an evolving set of questions that serve as prompts for the country health policy experts contributing to the platform. By following a structured questionnaire and having a team of Observatory staff editing the responses, information was collected in a way that enables broad comparisons across countries. The aim of this paper is to distil some key policy insights emerging from policy responses in the seven selected Mediterranean countries by focusing on responses at the health system level, namely on the governance tools adopted to manage the pandemic, the means to secure sufficient physical infrastructure and workforce capacity and some financing and coverage aspects.
The identification of key policy insights from country experiences followed a deliberative process that included extensive review of the HSRM materials and structured discussions among article co-authors, Observatory editors, and other experts. Where relevant, other country material, key documents, and literature were used to inform the paper. The results of the paper were structured along the identified main areas of policy insights related to the (curative) health system.
3. Results
3.1. Governance
3.1.1. Governance was mainly centralized to co-ordinate national policy responses
Mediterranean countries employed similar governance structures regarding their COVID-19 responses (see Table 2 ). It is notable in Table 2 that, initially, the head of country emergency responses were the higher authorities (in government), such as prime ministers or presidents, with the Ministry of Health as the lead authority for the health system response in all countries. All countries appointed an authority for emergency response. In some countries, these authorities were in place before the pandemic (e.g., the National Security Council in Israel, the Superintendence of Public Health in Malta, the Centre for the coordination of Alerts and Health Emergencies in Spain3 ). In others, these were assembled specially to handle the pandemic. All Mediterranean countries also established committees of COVID-19 Scientific Advisors. Finally, all countries had pre-existing emergency legislation or preparedness plans for pandemics, but the extent to which these plans were applicable to the COVID-19 pandemic and whether these plans were followed varied across countries.
Table 2.
Responsibilities for COVID-19 emergency response4
| Cyprus | Greece | Israel | Italy | Malta | Portugal | Spain | |
|---|---|---|---|---|---|---|---|
| Head of country emergency response | President of the Republic and the Council of Ministers | Prime Minister | Prime Minister | Prime Minister | Superintendent of Public Health | President of the Republic and Prime-Minister | Prime Minister |
| Authority for emergency response | Council of Ministers | General Secretariat for Civil Protection | Initially the National Security Council.4 From July 2020 authority was handed to the Corona Cabinet in the Parliament | Department of Civil Protection, Extraordinary commissioner (nominated on 18th March) | Superintendent of Public Health | National Authority for Civil Protection | 1st State of Alarm Ministry of Health |
| Authority for health system response | Ministry of Health and the State Health Services Organization | Ministry of Health; National Committee for Public Health | Ministry of Health | Ministry of Health, Regional Governments | Ministry for Health | Ministry of Health | 1st State of Alarm Ministry of Health |
| COVID-19 Scientific Advisors | Scientific Advisory Committee | Public Health Emergency Committee for Infectious Diseases | “Professional Corona Cabinet” and the National Security Council | National Scientific and Technical Committee; National Health Institute | Senior Advisory Group, COVID-19 Response Team | Academics and National Public Health Council | Centre for the Coordination of Alerts and Health Emergencies |
| Pre-existing emergency legislation or preparedness plan | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
Source: Authors based on Covid-19 Health Systems Reform Monitor.
Early on, responses to the pandemic were formulated centrally in all seven countries, even Italy and Spain, where regional authorities are responsible for the planning and provision of health services in their own territories (see Box 1 ). In Cyprus, Israel, Malta, Greece and Portugal, which already have highly centralized health systems, concentrating governance arrangements for the pandemic response within national-level institutions facilitated rapid decision-making, co-ordination of specific measures and effective mobilisation of resources, e.g. building a national reserve of personal protective equipment (PPE), procurement of diagnostic testing kits and their rapid distribution across national territories.
Box 1.
In Spain and Italy, the powers of regional governments were curtailed to allow for nationally coordinated responses
| Spain has a decentralized National Health System but after declaring a ‘state of alarm’ on 14 March 2020, a Royal Decree conferred on the national government full responsibility to decide and implement measures to deal with the COVID-19 crisis, either directly or through harmonized policies across all the regions (known as Autonomous Communities) [22]. The Prime Minister delegated competences to the national Ministers of Health (who acted as the principal authority), Defense, Internal Affairs, Transport, Mobility and Urban Matters, in their respective areas of responsibility. |
| Although regional authorities and municipalities retained operational management of health and social care services, all were put under the direct orders of the Minister for Health, who had to guarantee territorial cohesion and equity in the provision of services [23]. Nevertheless, all decisions were discussed within the Interterritorial Council for the National Health System - the highest governance body of the health system comprising the Ministry of Health and the regional ministers of health. After the expiration of the state of alarm (21 June 2020), autonomous communities and municipalities recovered their competences in the areas of health and social care, although action is coordinated along with the Ministry of Health. |
| Similarly, Italian regions usually enjoy a great deal of autonomy in decision-making, and are responsible, among other things, for planning and delivery of health services. However, the urgent nature of the pandemic crisis legitimized central government intervention and activated the national Department of Civil Protection to support regions in the procurement of pharmaceuticals, medical devices, human resources and infrastructure. The national response came in the form of a series of decrees from the Presidency of the Council of Ministers (Italy's equivalent of the Prime Minister's Office), containing measures based on the recommendations of the national Scientific and Technical Committee to deal with the pandemic, including decisions on transmission prevention measures and imposing national or regionalized lockdowns (following nationally set criteria). While regional leaders increasingly put forward their views on the direction that policies should take, unlike in Spain, the key elements of the COVID-19 response were decided by the national government. |
After the first wave, Spain, and Israel (to some extent) reverted to decentralized governance structures. In Spain, on 16 July 2020, the Ministry of Health and the regions agreed an ‘Early Response Plan to Control the COVID-19 pandemic’. According to this Plan, the COVID-19 direction committee (created by the Ministry of Health) and the Interterritorial Council (CISNS), jointly decided on the strategic management for preparedness and response to health threats and decided the measures to be implemented in tandem [22]. The actual implementation of the measures was directly run by the regions. In Israel, the Prime Minister (PM) moved authority from the Prime Minister's Office to the Government, the Parliament, and the Ministry of Health. A “Corona project manager” was appointed, and created a “traffic light” plan, that sets four severity scenarios based on COVID-19 morbidity, positivity rate of tests, and rate of increase of transmission, and determines the responses needed for each scenario. The Ministry of Health classified municipalities into a “colour” on a weekly basis. Municipalities could voluntarily implement different public health measures according to their “colour” and their population's needs. For example, some cities imposed upon themselves night curfews and managed to move from “red” to “green” cities.
3.1.2. Evolving evidence for decision-making was marshalled by pandemic committees and public health bodies
At the beginning of the pandemic, in line with other EU member states, Mediterranean countries had to respond to the pandemic in a situation of information scarcity and high uncertainty. Pre-existing pandemic preparedness plans, based on influenza models and WHO recommendations were in place, but their usefulness varied. In Cyprus, Portugal and Malta, the plans turned out to be robust and, with some adaptations, were converted to guide initial responses and contingency measures. In the other countries, plans that were found to be outdated or simply not fit for purpose, were reformulated based on evolving knowledge, to the specific challenges presented by the COVID-19 pandemic. For example, Spain established a more comprehensive early response plan by collecting governance measures for the early detection of new outbreaks, the provision of health care and the planning of strategic resources, after developing an initial early response plan in the first wave that adopted fast-track measures in response to epidemiological changes in the incidence of COVID-19 [22].
Generally, countries relied on advice and data provided by public health or pandemic committees, and assembled scientific teams of experts such as public health physicians, epidemiologists, statisticians and mathematical modellers, and infectious disease specialists to advise the government, the Ministry of Health and other ministries involved with co-ordinating the responses to COVID-19 (see Table 2). Italian policymaking took urgent action, using the little knowledge available at the time. The Head of the Department of Civil Protection established a Scientific and Technical Committee in early February 2020, assembling executive experts to provide technical support and data for decision making regarding the adoption of the most appropriate preventive and protective measures. In Italy's case, this did not always lead to harmonised responses in all areas; despite the centralization of the pandemic response at the national level, the Italian regions still retained decision-making autonomy on, for example, whether to conduct extensive testing of their populations as part of their efforts to mitigate transmission of the virus. As an example, despite being the two most affected regions and sharing similar socioeconomic profiles, Lombardy and the Veneto regions selected different paths, with the latter pursuing an overtly proactive strategy, which involved also performing tests on asymptomatic individuals at a very early stage and then tracing potential positives, while Lombardy conducted half the number of tests with a focus on hospitalized, symptomatic individuals [21].
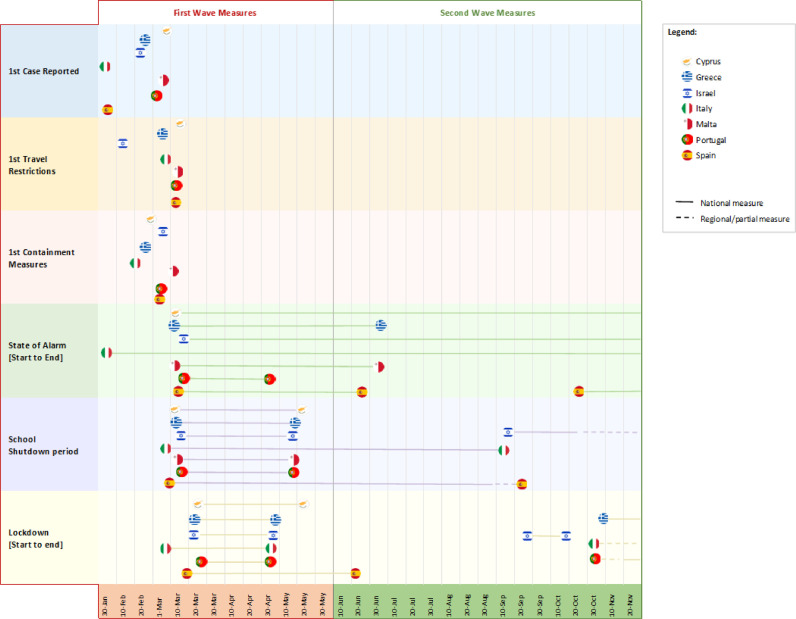
A high degree of convergence around the declaration of states of alarm or emergency is evident in the seven countries (see Fig. 2 ), including the start of school closures and the imposition of national lockdowns; although, it is noteworthy that Malta chose to implement a raft of prevention measures without resorting to a lockdown. Israel implemented travel restrictions as early as 2nd February 2020, even before any case was recorded, and its first containment measures, such as physical distancing requirements, followed fairly swiftly once positive cases were identified. In Cyprus, Greece, Malta, and Portugal, the decision to close schools and impose a lockdown was based on the actions taken by other European countries, particularly Italy and Spain, as the initial epicentres of the virus on the continent. In fact, when the State of Emergency was declared in these countries, their health systems were by no means near to collapse, and although the number of new infections was rising, the growth trend was far from exponential.
Fig. 2.
Timeline of selected Mediterranean country responses.
Note: 'travel restrictions' include any kind of travel limitation, such as the requirement to quarantine when returning from a risk area, or requiring a negative test result to disembark; the closures of airports; and cancellation of flights.
Source: Authors own elaboration, based on Covid-19 Health Systems Response Monitor.
States of Emergency were enacted in all countries as the legal prerequisite to enable implementation of other legislation that might become needed. For example, in Malta the declaration of a public health emergency, as authorised under the Public Health Act [24] gave the Superintendent of Public Health and Minister for Health the power, including emergency powers, to pass a series of laws as appropriate, 'in order to reduce, remove or eliminate the threat to public health'. In Spain it was critical, since as a quasi-federal country, the government needed special powers to centralize control of the COVID-19 response during the first wave. The delayed start of the pandemic in countries such as Cyprus, Israel, Malta and Portugal gained them valuable time to prepare their countries’ responses by planning the expansion of testing and laboratory capacity and ICU beds, and the acquisition of PPE and ventilators.
3.1.3. Ensuring sufficient physical infrastructure and workforce capacity
The unexpected and dramatic surge of COVID-19 cases in a short period of time exceeded the usual resource capacities that had been planned for 2020. Mediterranean countries entered the COVID-19 pandemic with relatively tight health budgets and lower than average human and physical resources compared to other EU countries, particularly in primary care, which meant that they had to be even more adaptative, creative, responsive, and agile when mobilizing resources and boosting capacity to cope with the actual or potential demands of treating COVID-19 patients. Here we look at some of the strategies employed by the seven countries to ensure adequate supplies of PPE and ICU beds, as well as health care professionals.
3.1.4. Adaptive management means were used to secure PPE and medical supplies
As the first two countries having to deal with a pandemic emergency, both Italy and Spain faced significant shortages of PPE, especially masks and gowns [25]. Cyprus and Israel had national reserves of PPE, which had been accumulated based on the needs of pre-pandemic times [26]. Nevertheless, none of the reserves were enough to cope with the scale up required during the initial months of the pandemic. Governments from all the countries in this group faced unprecedented difficulties in finding and purchasing PPE and test kits, both in national and international markets due to the global shortage of PPE, along with other required medical supplies such test kits and pharmaceuticals between January and March, 2020.
Prior to the pandemic, countries varied in the level and body responsible for procuring supplies of PPE. Israel, Malta, and Cyprus had centralized procurement, and continued to procure and purchase PPE centrally during the pandemic. Greece, Portugal, and Spain also recurred (temporally, in March 2020) to centralized procurement and purchase of PPE and testing kits by the government, the Ministry of Health (or other ministries). As a second step, from April 2020, countries started producing PPE domestically or organized big shipments of medical supplies needed for the pandemic. For example, in Greece publicly owned companies, acting on behalf of Greek health authorities, were responsible for procurement and purchasing. In Spain, from June 2020, procurement mechanisms were transferred back to the regions, although with the backup of the Ministry of Health in case of need, eg. if regions were unable to keep strategic stocks of PPE. To allocate these consumables in an efficient and equitable way across regions and providers, Greece and Spain developed digital registries which monitor stock and utilization of equipment, and even hospital beds, which Israel also monitors.
Some countries loosened regulations and allowed special “fast-track” licenses for domestic production of COVID-19 related material (PPE) and medical supplies such as diagnostic equipment (Greece, Israel, Italy, Spain). Italy's NHS even purchased material from private hospitals and clinics to allocate it to public hospitals treating COVID-19 patients. Cyprus, Greece, and Italy also attracted monetary and in-kind donations of medical consumables such as PPE, ICU beds, monitors and ventilators from companies, NGOs and individuals.
3.1.5. ICU beds were deployed from a variety of sources to create new COVID-19 treatment wards
Mediterranean countries rapidly converted ICU beds from other wards (e.g. post-surgical awakening units, neonatal intensive care units, operating and resuscitation rooms in cardiac surgery departments and neurosurgery clinics) into COVID-19 treatment wards (Spain, Greece, Israel, Malta). Spain also adapted “regular” beds with monitoring equipment and high-flow ventilators to enable their use by COVID-19 patients, while Greece and Italy were also able to utilize ICU beds provided by military hospitals.
Another strategy was to opt for “flexible” ICU capacity, which could be adapted as needs arose. Greece built “flexible” ICU wards while Israel increased the number of ICU beds four-fold from 1,500 beds before the pandemic to about 6,000 with “flexible beds”, that can be assembled and disassembled easily according to needs. In Israel, entire COVID-19 wards were built during the second wave in September and October 2020, and then disassembled in November when they were no longer needed, meaning that no excess capacity had to be carried by the hospital system but that no patients remained without treatment [27]. In Spain, in addition to bed conversions, after the first wave, regions had to demonstrate the ability to increase ICU beds if they were aiming to alleviate restrictions; specifically, the increase of 1.5 and 2 beds per 10,000 inhabitants within 5 days after the surge of new cases. The strategy did not mean increasing the number of settled ICUs beds, but being able to deploy them in case of need.
The use of private-sector capacity also has been particularly notable among Mediterranean countries. Although for most countries private hospitals usually do not provide services to the NHS, in Italy, for example, COVID-19 patients were temporally sent to be treated in ICU beds in private hospitals during the first wave. Another strategy employed by Cyprus, Italy and Greece was to send all non-COVID-19 cases to private hospitals while publicly funding them, releasing ICU beds from public hospitals, and converting them into COVID-19 ICU beds. In Greece, public-private partnerships to purchase ICU services from the private sector were established to be utilized whenever deemed necessary, to cater for possible future COVID-19 hospitalizations. More controversially, a contingency plan was put in place that included the mandatory requisition of private facilities and beds, which was activated for two weeks in November 2020 for two private clinics in northern Greece following the private hospitals’ refusal to voluntarily provide the 200 beds requested for the public health system to treat COVID-19 patients. In Spain, where the public and private systems regularly complement one another (mainly for elective surgery waiting lists reduction programs and early discharge programs), [6] private hospitals were considered a strategic reserve of regular and ICU beds, and these were used to ease patient flows within public hospitals, particularly in some regions where public hospitals were overwhelmed in the first wave. Portugal and Cyprus even received donations and loans of ventilators to expand ICU bed capacity from private companies. For example, with donation from a large betting company Cyprus managed in record time to set up a 21-bed ICU in a space inside the public Nicosia General Hospital.
3.1.6. Surge capacity for health workers was boosted quickly
All the seven countries pursued a variety of strategies to secure and boost the necessary numbers of health care workers to meet the increased demands of treating COVID-19 patients, including in hospital ICU settings, and to support the reorganization of health services during the pandemic (Table 3 ). The urgency of surge capacity differed among the countries according to the number and severity of COVID-19 cases that they had to deal with, and with changes in patient pathways that they implemented once more was learned about the disease and how non-severe cases could be managed through community settings and home care. All the countries shared similar challenges like starting with pre-existing low numbers of doctors and nurses working in the public sector (that is, below the average across EU countries), and the fact that health care workers themselves constituted one of the groups with a higher likelihood of being infected or having to be quarantined [28].
Table 3.
Country strategies to maintain or scale up the supply of health professionals
| Cyprus | Greece | Israel | Italy | Malta | Portugal | Spain | |
|---|---|---|---|---|---|---|---|
| Reallocation of health professionals within the public sector | x | x | x | x | x | x | |
| Extra hours, moving part-time to full-time, cancelling leave | x | x | x | x | x | x | x |
| Recruitment of new staff (short-term, freelance or temporary contracts) | x | x | x | x | x | x | |
| Recruitment of medical students and student nurses (accelerated end of training) | x | x | x | x | x | ||
| Recruitment of retired and previously inactive health professionals | x | x | |||||
| Deploying private sector health professionals to the public sector | x | x | x | x | |||
| Use of military medical personnel | x | x | x | x | |||
| Volunteers (any background) | x | x | x | x |
Source: Authors based on Covid-19 Health Systems Reform Monitor.
The most common strategies during the first wave of responses included temporarily reallocating health care professionals already working within the public sector from regular hospital wards to specially designated COVID-19 wards, and from primary care settings to hospitals (Greece, Israel, Malta, Spain). The hours of existing staff were extended, and it was not uncommon for doctors and nurses to report working longer or back-to-back shifts. Cyprus, Israel, Italy, Portugal and Spain loosened hiring requirements to enable the fast recruitment of additional staff on short-term, freelance or temporary contracts. For example, Portugal used an exceptional procedure to hire an extra 137 doctors and 1100 nurses by the end of July 2020.
Several of the countries (Cyprus, Israel, Italy, Malta and Spain) also recruited medical and nursing students to support health professionals, for instance by allowing final year students to join the workforce. Other strategies involved bringing retired or inactive health professionals back to the workforce (Italy, Portugal), recruiting medical, nursing and paramedical professions students (Cyprus) and temporarily enrolling professionals from the armed forces (Greece, Israel, Italy, Spain). Malta used temporary staff from the tourism and business sector (whose usual jobs were stopped or curtailed) for non-medical roles such as joining contact tracing teams [29].
Special recruitment drives were effective. As one of its first solutions, Italy launched an online recruitment drive to establish a Specialist Medical Unit and a Technical-Nursing Unit. From around 7 000 doctors and 10 000 nurses who applied as candidates, 300 physicians and 500 nurses (from the National Health Service, private clinics as well as freelancers) were recruited and sent to areas most affected by the COVID-19 emergency. In addition to their normal salary, each professional received a flat-rate solidarity premium of €200 for each day of work, paid by the Italian Department of Civil Protection, while the hosting regions were responsible for reimbursing transfer and accommodation. Similarly, Greece strengthened its health system with more than 6 800 new recruitments, including medical (745), nursing (3867), paramedical and other staff, far exceeding the initial provision for 2 000 recruitments. Public hospitals still suffered staff shortages, prompting legislation in April 2020 to allow for the employment of private physicians in public hospitals. In addition, to address regional staffing needs, an online platform was launched for health care workers from public hospitals to apply for transfers to areas most heavily affected by COVID-19; the financial incentive included doubling their remuneration. Several of the countries (including Greece, Cyprus, Italy and Malta) also enlisted the help of significant numbers of volunteers to help with basic support roles such as manning helplines or delivering medication and food to vulnerable people needing to self-isolate.
3.1.7. Financing and coverage
The additional physical and human resources incurred extra costs that represented a heavy burden on regular health budgets. While the overall impact of the COVID-19 pandemic on the countries’ health budgets for 2020 needs to be assessed (e.g., underspends in hospital services due to the cancellations of surgeries may have offset increased spending in other areas of the COVID-response), Table 4 presents some examples of how Mediterranean countries’ governments made available new or emergency budgets and where these funds were mobilized. Additionally, some of the countries (Cyprus, Greece and Italy) received private donations from companies, NGOs and individuals for these purposes.
Table 4.
Additional central government COVID-19 health expenditure commitments, 2020
| Country | Additional commitment (millions, national currency) | Additional commitment (per capita, Euro PPPs) | Main expenditure areas | Date of latest available official announcement |
|---|---|---|---|---|
| Cyprus | 100 | 114 per capita | Purchase and distribution of PPE, testing kits and other medical goods and equipment, hiring additional health workforce, payments to hotels and other quarantine areas | 15 March 2020 |
| Greece | 610 | 67 | Purchase and distribution of PPE and medical goods, hiring additional health workforce, enhance laboratory capacities | 21 Sep 2020 |
| Israel | 3800 | 420 (not PPP) | Opening ICU beds and COVID-19 wards, hiring more personnel, complying with stricter hygiene and isolation regulations | Jul 2020 |
| Italy | 6312 | 101 | Hiring of medical and nursing personnel, expanded private hospital capacity, purchase of medical equipment | 17 Mar 2020 |
| Malta | 100 | Health system COVID-related support only. Does not include rest of 1.8 billion Euro economic package to support businesses, employment, quarantine etc. | 18 March 2020 | |
| Portugal | 504 | 57 | Health personnel expenditures, acquisition of medical equipment | 18 Jun 2020 |
| Spain | 10 030 | 220 | Ministry of Health support, transfer to regions, research on drugs and vaccine development | 12 Jul 2020 |
3.1.8. Universal coverage was maintained and sometimes expanded throughout the crisis
One of the most important findings is that in all the Mediterranean countries, health coverage was universal, enabling access to COVID-19 and non-COVID-19 care during emergency times. In fact, in most of the countries, coverage was expanded to new populations that were previously uninsured. In particular, undocumented immigrants were, at least temporarily, covered by the government for COVID-19 services (Cyprus, Israel, Portugal, Greece, Malta, Spain). For example, the Portuguese Government granted temporary residency rights to all immigrants and asylum seekers who applied for residency before 18 March 2020. When the State of Emergency was announced, these individuals were fully entitled to health and social care benefits, until at least 1 July 2020 [34]. In terms of coverage of services, all population groups were eligible for all COVID-19 related services, including diagnostic tests, isolation settings for those who could not self-isolate at home, and treatment of the disease and its symptoms. Regarding covering costs, the seven countries chose to publicly fund all COVID-19 services without user charges.
4. Discussion
4.1. Centralized governance helped to co-ordinate national policy responses, but the impetus for localized responses has also been an important development
The approach to governance in the early stages of the pandemic was undertaken centrally in all the Mediterranean countries, even Italy and Spain, where regional authorities normally have autonomy over health matters. It is clear that operationally, centralization facilitated decision making and the rapid and homogenous implementation of measures not only for containment policies, but also in building a national reserve of PPEs and diagnosis tests, and rapid distribution to providers, as well as increasing workforce surge capacity. However, the two examples of Spain and Israel, which switched to decentralized models in the second wave, are also instructive. In Spain, the regions reclaimed their political jurisdiction for the pandemic response, albeit involving consultation and co-ordination processes with the national government. No doubt this development reflected the country's strong semi-federalist political structure and the regions’ insistence that any ceding of powers in the early stage of the nationally co-ordinated response would only be temporary. But it also means that after the State of Alarm expired, Spanish regions were able to implement pandemic response measures that cater to the specific epidemiological situation in their territories and to take responsibility for balancing public health objectives with social and economic impacts [36]. Similarly, in Israel, although the ‘traffic light’ severity scenario plan is set centrally by the Ministry of Health, municipalities are allowed to tailor mitigation measures to match local conditions and objectives, with decision-making being close to localised needs. Locally tailored public health responses boosted compliance with mitigation measures in Israel, as these were deemed more appropriate. In terms of learning more generalized lessons, whether this subsidiarity approach leads to greater legitimacy to pandemic response measures and/or boosted the compliance of local populations requires further analysis, particularly with regard to local lockdowns and quarantining/isolation regimes.
4.2. Learning from the experiences of ‘first movers’ was important to informing pandemic responses, especially in conditions of uncertainty
In the quickly evolving situation at the start of the pandemic, there was a generalized concern among this group of Mediterranean countries that their health systems, with stretched resources, would not have the capacity to treat patients if infection rates were to reach high magnitudes. In Italy and Spain, the first countries to experience a rapid increase in the number of cases, their health systems, and their hospitals, in particular, experienced ever-growing difficulties in coping with the number of patients requiring treatment [35], [36], [37]. The sudden outbreak of cases in Italy and Spain led to a “domino effect” among the other countries, which imposed physical distancing restrictions, lockdowns, travel restrictions and rapid mobilization of resources comparatively early given their relatively low COVID-19 morbidity rates, to try and anticipate potential spreader situations and avoid similar scenarios. The experiences of Italy and Spain as ‘first movers’ in terms of policy responses became a reference point for some of the other countries. Cyprus implemented mitigation measures before the first case was recorded while in Greece, the authorities started testing promptly to identify asymptomatic cases. In retrospect, such pre-emptive actions cushioned the impact on health systems as they mustered resources and organized capacity.
4.3. Surge planning has highlighted the benefits of flexible capacity
Over time, the seven countries analyzed here continuously built-up ICU bed stocks, significantly increasing ICU bed capacity, even though, with the exception of Italy and Spain, this extra capacity was not needed during the first wave of the pandemic. For example, Greece utilized only one third of its ICU capacity in the first wave; however, during the second wave, occupancy rates increased dramatically, and in some regions, it reached more than 100%. Similarly, in Cyprus and Malta, there was minimal utilization of ICU bed stock in the first wave but utilization rates rose constantly after the summer of 2020 [38]. As mentioned above, surge planning for crucial infrastructure like ICU beds was no doubt spurred on by the worst-case scenarios presented by Italy and Spain, even if the achieved capacity was not always needed immediately during the first wave. Interestingly, the situation prompted the innovative design and deployment of “flexible” ICU capacity as an agile solution to avoid the potential misallocation of resources through excess capacity. The models from Greece, Israel and Spain provide valuable blueprints and may become a mainstay of future hospital bed contingency planning in the future.
A similar reflection can be made about measures to boost health workforce capacity: flexibility in being able to utilize a range of potential sources to recruit additional personnel to deliver COVID-19-related services has been a notable success in the Mediterranean countries, and one that is sure to be employed again in similar crises. In particular, boosting appropriate health workforce capacity was a (crucial) prerequisite for operating ICU beds. Increasing ICU bed capacity had to be done in coordination with the deployment of adequate and qualified staff in order to be able to use these beds. When preparing for future health-related shocks, countries will have to plan strategies that coordinate the rapid increase of medical equipment, treatment settings and workforce capacity concomitantly. Otherwise, there is the risk that patients might be undertreated and equipment might be underused due to lack of qualified professionals.
4.4. The usual lines between public funding and private provision have been (temporarily) redrawn
One relevant feature of many Mediterranean countries is the divide between public and private providers, where the latter either usually do not provide services to publicly funded patients or the provision is essentially subsidiary to public provision extra needs. During the pandemic, added reliance on the private sector in order to expand resources and health workforce capacity to treat patients has led to special public-private partnerships (PPPs) and agreements. While this was common practice in Spain, for some of the other countries it was more of a novelty. For example, in Cyprus, during the first wave, patients who could not be treated in public hospitals due to the closure of wards, could be treated by private providers, with the costs of care reimbursed by the Ministry of Health [39]. In Italy, public funding regularly reimburses services only to private providers which are accredited with the NHS and meet specific requirements [3]. However, as part of COVID-19 response measures, non-accredited private providers could also be extraordinarily reimbursed through public funding in order to gain additional capacity during the emergency. In Greece, notwithstanding the reticence of some private hospital facilities to enter into agreements for public provision of services for COVID-19 patients, where this did occur, patients directed to private hospitals to alleviate public hospitals have been exempted from the very high co-payments that would normally apply in cases where contracted private providers supply services to publicly-funded patients [8]; under the PPP agreements, these costs are fully covered by the state. It is too early to tell whether these agreements will be regarded as only temporary solutions to be employed in contingency circumstances or whether the greater experimentation with PPP agreements may lead to longer term readiness in some of the countries in the group to contract more with private providers for the supply of publicly funded services to meet specific objectives, such as to reduce waiting times for elective surgery.
It is acknowledged that while PPPs were crucial in many countries in the early responses to the pandemic, facilitating the surge in capacity, resources and strengthened public health activities, the speedy manner with which they were established may have resulted in lack of transparency and inefficiencies [40]. There are various models of good governance for PPPs that can build health systems’ resilience in the context of COVID-19. However, drawbacks of PPPs might include unbalanced risk sharing – and thus a high risk for wasting public money, while still being profitable for the private sector (and which may create public debts), corruption, distortion of public policy priorities, and weakening of institutions within the public health system. In this case, resilience is undermined, and negative impacts may override the benefits of PPPs. Going forward, Mediterranean countries will need to assess whether, and to what extent, the introduction of such partnerships supported the resilience of their health systems in responding to the shock of the pandemic.
4.5. Covering everyone for COVID-19 services is instrumental to mitigation efforts
In the Mediterranean countries, universal health coverage was key not only to providing care for those in need and to reduce inequalities among population groups, but also in curbing the potential spread of the virus. The instrumental basis to this policy decision lies in the fact that any individuals who were not covered by public services for COVID-19, be it access to testing or to required treatment, would face greater barriers in being diagnosed and would continue the transmission to others in the community. Similarly, the policy of ensuring coverage for the resident population at large, even for groups such as undocumented migrants, meant that financial barriers to accessing care as well as potentially higher mortality rates were avoided. Although this expansion of coverage may be only temporary, it was nevertheless a reflection of the values of solidarity and equity that underline these health systems, as well as an extraordinary example of the positive pay-offs of ensuring universal coverage to successfully respond to public health crises.
5. Conclusions
Mediterranean countries had universal health coverage that ensured good foundations for their health systems to respond to the COVID-19 pandemic. Nevertheless, their resource-endowments entering the pandemic were stretched compared to other European countries. The preparedness of governance tools varied among the countries and centralization of decision making was a common reaction. These countries developed adaptative solutions that allowed them to deploy resources from other sectors, overcoming the unexpected and rising requirements of the pandemic. Some countries received extraordinary monetary and in-kind donations to boost national resources, but the bulk of the health systems’ response to the pandemic has been financed through the national coffers, even when private facilities or personnel were deployed. For countries with coverage limitations, these responses were accompanied by a temporary expansion of coverage of COVID-19 related services to populations not previously covered, such as undocumented immigrants. Speed and creativity were key for Mediterranean countries to respond to the immediate pressing needs of the pandemic, yet it is still early to know if the different health systems were truly resilient and will be able to maintain essential services without undermining equitable access to high quality care.
Declaration of Competing Interests
The authors declare no competing interests
Acknowledgments
Acknowledgements
The manuscript benefitted from comments received on the presentation at the HSPM network members during the annual (virtual) meeting on 29th October, 2020.
We thank Nathan Shuftan for the research assistance, and Prof. Bruce Rosen for the valuable comments that helped improve this paper.
Funding
N/A
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Footnotes
Cyprus has been a divided island since 1974. Consequently, all data and discussions in this paper refer to those areas of the Republic of Cyprus in which the government of Cyprus exercises effective control.
It is important to note that morbidity rates are highly correlated to testing policies and rates, and therefore should be compared with caution.
Centre for the coordination of Alerts and Health Emergencies, DG of Public Health, Ministry of Health (CCAES)
Israel's central body for coordination, integration, analysis and monitoring in the field of national security and is the staff forum on national security for the Israeli Prime Minister and Government.
References
- 1.European Commission B. Eurostat. Health Statistics. 2020 [Google Scholar]
- 2.OECD; 2019. Cyprus: Country Health Profile 2019. [Google Scholar]
- 3.Ferré F, de Belvis AG, Valerio L, Longhi S, Lazzari A, Fattore G, et al. Italy: Health System Review. Health Systems in Transition. 2014;16(4) [PubMed] [Google Scholar]
- 4.Azzopardi-Muscat N, Buttigieg S, Calleja N, Malta Merkur S. Health System Review. Health Systems in Transition. 2017;19(1) [PubMed] [Google Scholar]
- 5.de Almeida Simoes J, GF Augusto, Fronteira I, Hernandez-Quevedo C. Portugal: Health System Review. Health Systems in Transition. 2017;19(2) [PubMed] [Google Scholar]
- 6.Bernal-Delgado E, Garcia-Armesto S, Oliva J, Sanchez Martinez FI, Repullo JR, Pena-Longobardo LM, et al. Spain: Health System Review. Health Systems in Transition. 2018;20(2) [PubMed] [Google Scholar]
- 7.Rosen B, Waitzberg R, Merkur S. Israel: health system review. Health Systems in Transition. 2015;17(6) [PubMed] [Google Scholar]
- 8.Economou C, Kaitelidou D, Karanikolos M, Maresso A. Greece: Health System Review. Health Systems in Transition. 2017;19(5) [PubMed] [Google Scholar]
- 9.The General Health System (Personal Doctors) Internal Regulations of 2019. 2019.
- 10.OECD; 2020. OECD Health Statistics 2020. [Google Scholar]
- 11.Israeli Ministry of Health. Hospital beds and licensing stations 2020. Available at: https://www.health.gov.il/PublicationsFiles/beds2020.pdf.
- 12.Boldrini R, Di Cesare M, Basili F, Giannetti A, Messia I. Ministry of Health; Italy: 2017. Statistical SSN Yearbook – Organisational framework, activities and productive factors of the SSN. [Google Scholar]
- 13.Press release . Initial statement of the Minister of Health Mr. Konstantinos Ioannou in COVID-19 press conference. March 2020. [Google Scholar]
- 14.Cuschieri S, Grech P, Farrugia IK, Gauci C, Grech V. One of COVID-19’s many costs: Malta's expenditure in consumables and non-consumables, a population-based study. Early Hum Dev. 2020 doi: 10.1016/j.earlhumdev.2020.105260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.OECD . OECD Publishing; Paris: 2019. Health at a Glance 2019: OECD Indicators. [DOI] [Google Scholar]
- 16.Ministério da Saúde, República Portuguesa. [Ministry of Health, Portugal]. 2021 Apr 23 [cited 2021 May 12]; Available from: https://www.sns.gov.pt/institucional/ministerio-da-saude/.
- 17.Rhodes A, Ferdinande P, Flaatten H, Guidet B, Metnitz PG, Moreno RP. The variability of critical care bed numbers in Europe. Intensive care medicine. 2012;38(10):1647–1653. doi: 10.1007/s00134-012-2627-8. [DOI] [PubMed] [Google Scholar]
- 18.Della Porta MR, Mazzoni E, Salerno D, Tani G. Bringing health back to the centre. From the health emergency to the hoped-for revolution in NHS governance. 2020 Sep.
- 19.OECD . OECD; Paris: 2020. Beyond Containment: Health systems responses to COVID 19 in the OECD. [Google Scholar]
- 20.WHO. WHO Coronavirus (COVID-19) Dashboard; 2020.
- 21.Kozlakidis Z, Zammarchi L, Boccia S, Cascini F, Mckee M, Ricciardi W. How the Italian NHS Is Fighting Against the COVID-19 Emergency. Front Public Health. 2020;1:167. doi: 10.3389/fpubh.2020.00167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.PLAN DE RESPUESTA TEMPRANA EN UN ESCENARIO DE CONTROL DE LA PANDEMIA POR COVID-19. 2020.
- 23.The Ministry of the Presidency. Royal Decree 463/2020. Declaration of the state of emergency due to the COVID-19 pandemic; March 2020.
- 24.Public Health Act. Chapter 465. Laws of Malta; 2007.
- 25.Civil Protection Department. Analisi Distribuzione Aiuti (ADA) Dashboard. Italy; 2020.
- 26.Walla! news. Staff protection; 2020.
- 27.Haaretz Journal. Senior Doctors on COVID-19 Response. Israel; 2020.
- 28.Williams GA, Maier CB, Scarpetti G, Giulio De Belvis A, Fattore G, Morsella A, et al. What strategies are countries using to expand health workforce surge capacity during the COVID-19 pandemic? Eurohealth. 2020;26(2) [Google Scholar]
- 29.The Malta Independent. Over 900 tourism workers apply to join the contact tracing team in MTA scheme; 2020.
- 30.Filut, A. Ministry of Finance to the Ministry of Health: Forget about the additional funds for Corona until June next year. 2020 Nov 4 [cited 2021 May 12]; Available from: https://www.calcalist.co.il/local/articles/0,7340,L-3868376,00.html.
- 31.STQARRIJA MILL-UFFIĊĊJU TAL-PRIM MINISTRU - Pakkett finanzjarju ta’ €1.81biljun sabiex tkun mgħejjuna l-ekonomija [STATEMENT BY THE OFFICE OF THE PRIME MINISTER - € 1.81 billion financial envelope to help the economy]. 2020 Mar 18 [cited 2021 May 12]; Available from: https://www.gov.mt/en/Government/DOI/PressReleases/Pages/2020/March/18/pr200520.aspx.
- 32.Government Services and Information . Government Services and Information Malta; Malta: 2020. Press release. € 1.81 billion financial package released to boost the economy recovery. [Google Scholar]
- 33.Diário da República. 2.a série PARTE C PRESIDÊNCIA DO CONSELHO DE MINISTROS, ADMINISTRAÇÃO INTERNA, TRABALHO, SOLIDARIEDADE E SEGURANÇA SOCIAL E SAÚDE Gabinetes da Ministra de Estado e da Presidência, do Ministro da Administração Interna e das Ministras do Trabalho, Solidariedade e Segurança Social e Saúde [Republic Diary. 2nd series PART C PRESIDENCY OF THE COUNCIL OF MINISTERS, INTERNAL ADMINISTRATION, LABOR, SOLIDARITY AND SOCIAL SECURITY AND HEALTH Offices of the Minister of State and Presidency, of the Minister of Internal Administration and of the Ministers of Labour, Solidarity and Social Security and Health]; March 2020.
- 34.The Ministry of the Presidency. Royal Decree 555/2020. Extension the state of emergency due to the COVID-19 pandemic, declared in the royal decree 463/2020; June 2020.
- 35.Boccia S, Ricciardi W, Ioannidis J. What Other Countries Can Learn From Italy During the COVID-19 Pandemic. JAMA. April 7 2020 doi: 10.1001/jamainternmed.2020.1447. [DOI] [PubMed] [Google Scholar]
- 36.Sisó-Almirall A. Blog of Spanish Health Economics Association; 2020. COVID-19 challenges primary and community care. [Google Scholar]
- 37.Pane Mena O, Santos JP. Blog of Spain Health Economics Association; 2020. The challenge of COVID-19 for specialized care. [Google Scholar]
- 38.ECDC . European Centre for Disease Prevention and Control; Stockholm: 2021. Data on hospital and ICU admission rates and current occupancy for COVID-19 [Internet] ( https://www.ecdc.europa.eu/en/publications-data/download-data-hospital-and-icu-admission-rates-and-current-occupancy-covid-19 accessed April 2021) [Google Scholar]
- 39.Quentin W, Albreht T, Bezzina A, Bryndova L, Dimova A, Gerkens S, et al. Adjusting hospital inpatient payment systems for COVID-19. Eurohealth. 2020;26(2) [Google Scholar]
- 40.Tille F Panteli, Fahy D, Waitzberg N, Davidovitch R, Degelsegger-Márquez N. Governing the Public-Private-Partnerships of the Future: Learnings from the Experiences in Pandemic Times. Eurohealth. 2021;27(3) [Google Scholar]