Abstract
Simple Summary
Dysbiosis of the gut microbiome may contribute to the heterogeneity of colorectal cancer from phenotypic, prognostic and response to treatment perspectives. We analysed CRC microbiome by 16S rRNA gene sequencing of paired tumour mucosa, adjacent visually normal mucosa and stool swabs of 178 patients with stage 0–IV CRC. We observed that tumour mucosa is dominated by pathogenic bacteria of oral origin and proposed a CRC tumour microbiome subtyping system. The subtypes and tumour mucosa genera were associated with prognostic clinical covariates (tumour grade, localisation, TNM, BRAF mutation and MSI). In contrast, changes in the stool microbiome were associated with lymph node involvement and the presence of synchronous metastases. We discovered new associations between microorganisms and CRC and clinical parameters. Our study represents a step forward in understanding the role of the microbiome and its interactions with factors involved in tumour progression, and it opens novel avenues for exploring new treatments and biomarkers.
Abstract
Long-term dysbiosis of the gut microbiome has a significant impact on colorectal cancer (CRC) progression and explains part of the observed heterogeneity of the disease. Even though the shifts in gut microbiome in the normal-adenoma-carcinoma sequence were described, the landscape of the microbiome within CRC and its associations with clinical variables remain under-explored. We performed 16S rRNA gene sequencing of paired tumour tissue, adjacent visually normal mucosa and stool swabs of 178 patients with stage 0–IV CRC to describe the tumour microbiome and its association with clinical variables. We identified new genera associated either with CRC tumour mucosa or CRC in general. The tumour mucosa was dominated by genera belonging to oral pathogens. Based on the tumour microbiome, we stratified CRC patients into three subtypes, significantly associated with prognostic factors such as tumour grade, sidedness and TNM staging, BRAF mutation and MSI status. We found that the CRC microbiome is strongly correlated with the grade, location and stage, but these associations are dependent on the microbial environment. Our study opens new research avenues in the microbiome CRC biomarker detection of disease progression while identifying its limitations, suggesting the need for combining several sampling sites (e.g., stool and tumour swabs).
Keywords: colorectal cancer, 16S rRNA gene, tumour microbiome, microbial subtypes
1. Introduction
Colorectal cancer (CRC) is the third most frequent cancer worldwide and the second leading cause of cancer mortality in Europe [1]. It is a heterogeneous disease, both from a phenotypic and a prognostic and response to treatment perspective. The current standard treatments are limited and remain ineffective for many CRC patients due to inadequate patient selection, resulting in unneeded toxicity and high cost resulting from over-treating of patients that do not benefit [2,3]. Recent research shows that gut microbiota may significantly influence colorectal tumour initiation and progression [4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22].
Several studies showed that bacteria adherent to colorectal adenomas or carcinomas were different from bacteria adherent to healthy gut mucosa [8,11,12] due to the altered tumour environment with decreased pH and modified metabolic conditions resulting from hypoxia and onset of necrosis [23]. Gut microbiota can promote colon cancer development or change the tumour invasion potential through (i) immunomodulation [10,24,25,26] or (ii) metabolic activity—via the production of specific toxins inducing DNA damage responses. Overall, the evidence of microbiome importance in colon cancer development is so overwhelming that a bacterial driver-passenger model for colorectal cancer development and progression has been suggested [27] as an alternative to the universally accepted driver-passenger mutational adenoma-carcinoma model. Additionally, gut microbiota seems to play a crucial role also in response to anti-cancer therapy [28].
Previous studies associating gut dysbiosis with CRC were focused on comparing the gut microbiome in the normal-adenoma-carcinoma sequence [4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,29,30,31,32]. It is the landscape of the microbiome within the ongoing disease and its associations with clinical variables that remain under-explored. The published studies vary in techniques employed, specimen origin and sample size, thus hampering any integrative analysis. Most studies compared diseased and healthy subjects, and the few that tried to characterise microbial composition within the CRC patients suffered from a small sample size. The specimens used in most studies were stool [4,6,7,15,17,18,20,21,22] or mucosa samples from colonoscopy biopsies [11,13,15] or post-resection [6,12,16,19]. Stool microbiota sampling has the advantage of being non-invasive, allowing its use for screening and follow-up studies. Some efforts combined information about the tumour-associated microbiome with existing prognostic scores in an attempt to improve the prediction accuracy [18] or to develop a new screening/prognostic model [33]. The results of two different meta-analyses showed that the accuracy of predicting diseased state was about 0.8, such as occult blood test results, the main non-invasive clinical test for this type of cancer [34,35]. However, the microbial composition in stool only partially reflects the situation in tumour mucosa, a trend consistent across different nationalities of the patients, sampling techniques or sequencing methodology [36].
The microbiota adherent to the mucosal tissue differs from the faecal microbiota in its needs for oxygen and nutrient types [37,38]. Therefore, the information derived from stool may be insufficient for capturing tumour-microbe interactions consistent with the disease prognosis. The relevance of the tumour mucosa microbiome assessment for screening purposes is dependent not only on the co-presence of the bacteria in both tumour mucosa and stool but also on its association with relevant clinical parameters in both sample types. Additionally, studying the (dis)similarity of bacterial composition between tumour and visually normal mucosa from the same individual may provide hints regarding the changes in microenvironment which have occurred favouring the growth of certain species and shed some light on the underlying tumour-immune system-microbe interactions and metabolic pathways.
Recently, two studies provided a comparison of bacterial composition in both tumour tissue and visually normal tissue and the bacterial composition of stool samples from the same patients [34,35]. Liu et al. [34] showed that the bacterial communities in both tumour tissue and visually normal tissue were similar. Still, the study was vastly underpowered (n = 8 individuals) and did not explore the clinical relevance of this similarity. Other studies associated microbiome on tumour or in stool with clinical variables [35,39,40] but had a similar disadvantage in terms of statistical power (n = 25, n = 30, n = 53, individuals, respectively).
The studies mentioned were species-centric because they compared the abundance of individual microbial species between the groups of interest. However, a broader view is needed to account for lesser-known species coupled with a larger sample size allowing for capturing enough inter-tumour heterogeneity, thus better understanding the possible effects of bacteria on tumour growth, aggressiveness or response to therapy. Our study takes a microbial community-centric approach to provide a comprehensive description of the CRC tumour microbiome based on 16S rRNA sequencing. We analyse three sample types (tumour mucosa, visually normal mucosa, stool) from n = 178 individuals with stage 0–IV colorectal cancer.
Our study has a dual nature, both exploratory and confirmatory. We explore and interpret the landscape of the tumour mucosa-associated microbiome with respect to clinical variables and microbial composition of paired adjacent visually normal mucosa and paired stool samples. Benefitting from a larger sample size, we advance the state-of-the-art knowledge by reporting previously unseen associations. Most importantly, we capture the tumour microbial heterogeneity and derive CRC tumour microbiome subtypes.
2. Materials and Methods
2.1. Patients and Specimens
All specimens were collected at Masaryk Memorial Cancer Institute (Brno, Czech Republic) from 2015 to 2019. Patient inclusion criteria were (i) scheduled for resection based on preliminary screening (such as a colonoscopy), (ii) no neoadjuvant treatment, (iii) no previous CRC diagnosis (iv) with confirmed stage 0–IV CRC without multiplicities (single tumour). The stool samples were collected from untreated patients before the scheduled surgery. Patients performed the collection at home, the morning of their hospitalisation for the surgery and brought the samples to the hospital, where they were immediately frozen at −80 °C until further processing. Swabs from the tumour and visually normal mucosa were collected within 30 minutes of the tumour resection at the pathology department. Whenever possible, the swab from visually normal tissue was taken at least 20 cm proximally to the tumour. The swabs were then stored immediately in a freezer at −20 °C and, without unnecessary delay, transferred to −80 °C until further processing. All samples, including stool, were collected using DNA free cotton swabs (Deltalab, Barcelona, Spain).
Overall, we analysed n = 483 samples from n = 178 CRC patients. There were 127 triplets (all three sample types from the same patient) and 51 mucosa duplets (swabs from tumour and visually normal mucosa from the same patient).
The study was approved by the ethical committee of Masaryk Memorial Cancer Institute. All patients gave written informed consent following the Declaration of Helsinki prior to participating in the study.
2.2. DNA Extraction, PCR Amplification and Sequencing of 16S rRNA Gene
According to the manufacturer’s instructions, the DNA extraction was performed using DNeasy® PowerSoil® Isolation kit (QIAGEN, Düsseldorf, Germany). Extracted DNA was used as a template in amplicon PCR to target the V4 hypervariable region of the bacterial 16S rRNA gene. The 16S metagenomics library was prepared according to the 16S Metagenomic Sequencing Library Preparation protocol (Illumina, San Diego, CA, USA), with some deviations described below. Each PCR was performed with HotStarTaq Master Mix Kit (QIAGEN, Hilden, Germany) in triplicate, with the primer pair consisting of Illumina overhang nucleotide sequences, an inner tag, and gene-specific sequences [41,42]. The Illumina overhang served to ligate the Illumina index and adapter. Each inner tag, i.e., a unique sequence of 7–9 bp, was designed to differentiate samples into groups. Primer sequences and PCR cycling conditions are summarised in Table S3. After PCR amplification, triplicates were pooled, and the amplified PCR products were determined by gel electrophoresis. PCR clean-up was performed with Agencourt AMPure XP beads (Beckman Coulter Genomics, Danvers, MA, USA). Samples with different inner tags were equimolarly pooled based on fluorometrically measured concentration using Qubit® dsDNA HS Assay Kit (Invitrogen™, Carlsbad, CA, USA) and microplate reader (Synergy Mx, BioTek, Winooski, VT, USA). Pools were used as a template for a second PCR with Nextera XT indexes (Illumina, USA). Differently indexed samples were quantified using the qPCR kit KAPA Library Quantification Complete Kit (Roche, Indianapolis-Marion County, IN, USA) and LightCycler 480 Instrument (Roche, USA) and equimolarly pooled according to the measured concentration. The prepared libraries were checked with a 2100 Bioanalyzer Instrument using the High Sensitivity D5000 Screen tape (Agilent Technologies, Santa Clara, CA, USA), and concentration was measured with qPCR shortly prior to sequencing. The final library was diluted to a concentration of 8 pM, and 20% of PhiX DNA (Illumina, USA) was added. According to the manufacturer’s instructions, sequencing was performed with the Miseq reagent kit V2 (500 cycles) using a MiSeq instrument (Illumina, USA).
2.3. Data Analysis
2.3.1. Preprocessing and Quality Control
Forward and reverse pair-end reads were demultiplexed, and barcodes and primers were trimmed. Denoising algorithm with DADA2 [43] was applied separately on forward and reverse reads that passed the quality and length filter and did not contain N’s. Reads were merged using the fastq-join method [44]. In the next step, chimaeras were detected with the function removeBimeraDenovo in DADA2. Chimaera sequences were subsequently excluded from the analysis, and Amplicon Sequence Variant (ASV) table was created.
After quality filtering and chimaeras removing, the number of reads ranged from 2968 to 239,116, with a median of 44,371 and a mean of 53,074 reads per sample. The number of reads did not differ between the sample types (paired Wilcoxon test, Figure S1).
2.3.2. Taxonomy Assignment and Metabolic Potential Prediction
Taxonomy was assigned to each ASV based on SILVA 123 reference database [45] using the algorithm UCLUST [46] in QIIME [47]. BLAST algorithm [48] was used to identify the species, and all taxa with the maximum identity and minimum e-value were selected for each ASV. The observed species metric and the Chao1 and Shannon index were used to estimate alpha diversity for each sample in QIIME. Beta diversity was computed in QIIME using both weighted and unweighted UniFrac metrics [49].
We filtered out the ASVs unassigned at the phylum level and all the ASVs belonging to the phylum Cyanobacteria. Only the taxa present in at least three samples of the same sample type and at the same time represented by at least nine reads were kept for further analysis to account for possible contaminations. The threshold of 9 reads represents 0.3% taxa abundance in the sample with the least number of reads (2968).
This filtering step discarded 46–55% of taxa at each taxa level (Table S4).
Picrust 2 [50] was used to predict hypothetical abundances of KEGG orthologs in each sample and to summarise them into higher functional processes.
2.3.3. Statistical Analysis and Data Mining
All comparisons between the three sample types were performed on triplet samples from 127 patients, totalling n = 381 samples for the analysis. For the analysis of tumour-visually normal mucosa pairs, we used paired tumour and visually normal mucosa swabs from 178 patients (totalling 356 samples). We used all the available samples for analyses performed within each sample type (178 for tumour mucosa swabs, n = 178 for visually normal tissue mucosa swabs and n = 127 for stool).
Data were analysed using appropriate corrections and approaches for compositional data [51,52,53,54]. Zero multiplicative replacement [53] was applied prior to the centred log-ratio (clr) transformation.
Non-metric Multidimensional Scaling (R vegan package [55]) over Aitchinson distance matrices (R coda.base package [56]) was used to analyse tumour microbial heterogeneity and β-diversity. To estimate the contribution of clinical traits in the microbiome, β-diversity permutational multivariate analysis of variance for distance matrices (R adonis function of vegan 2.5.4 package [55]) with 999 permutations were used. To assess the differences between the sample types in alpha diversity, we used a paired non-parametric two-way Mann-Whitney U test. We applied a non-parametric approach to identify differences in microbial composition between sample types and the associations between relative microbial abundance and clinical variables. For non-parametric analysis, the Friedman test with paired Wilcoxon test and rank regression was used (R package Rfit [57]). A drop in dispersion test was used to produce overall p-values for rank regression models. The Cochran Q test was used to analyse differences in the presence of genera across sample types (analysis of triplets). Benjamini-Hochberg correction for multiple hypothesis testing was applied [58]. Results were considered significant at FDR <0.1. The adjusted p-values are referred to as q-values. Visualisation was performed with gplots 3.0.1.1, ggplot2, ComplexHeatmap 1.17.and circlize 0.4.8 packages [59,60,61,62].
For each clinical variable (or a combination thereof), we only tested genera present in at least 10 samples in one clinical group (or a combination thereof). We do emphasise that we approached this statistical testing from the point of view of a pilot discovery study.
Due to the known association between tumour grade and location [63] (also confirmed in our data, p < 0.001, Fisher’s exact test), we investigated the associations of the microbiome with grade and tumour location in a model with the interaction between covariates compared to a model without interaction. To ensure a more balanced design, we considered three locations: right and transverse, left, rectosigmoid and rectum, respectively.
The threshold of false discovery rate was set to 0.1, as is customary in similar studies, with the aim to identify potential candidates for further research. While we consider only associations with FDR <0.1 to be statistically significant, we also report the unadjusted results p < 0.05 for hypothesis confirmation by other studies.
2.4. Data Access
The data were uploaded to the European Nucleotide Archive under accession number PRJEB35990.
2.5. Validation
We performed partial validation of our results on three publicly available datasets. The association of the tumour microbiome with tumour localisation was validated in the dataset of Dejea et al. [31], n = 23. No grade information was available, and hence in the validation we did not use the grade*localisation interaction term. Publicly available fastq files were analysed with QIIME pipeline with the appropriate approach for 454 Roche sequencing. Taxonomy was assigned using SILVA 123 database to have comparable results with our dataset.
The association of stool microbiome with AJCC staging and TNM staging was validated in two datasets (Zeller et al. [32] and Feng et al. [30]). The processed datasets with taxonomic information were used as available in R package curatedMetagenomicData [64] and were normalised using the clr transformation before the analysis.
All associations were tested using rank regression (R package Rfit [57]). The dataset of Feng et al. only contained one M1 sample; hence we only analysed associations with AJCC staging, T stage and N stage.
3. Results
In our effort to describe tumour microbial landscape, we explored the differences in microbiome abundance, diversity, the presence/absence of the species and the proportion of samples with the respective genera in different sample types across patient groups defined by clinical variables (Table 1).
Table 1.
Table of clinical variables and their distribution in the complete set of 178 patients, the subset of 127 patients and in the CRC tumour microbial subtypes, respectively. (For categorical variable, Fisher exact test was performed and for continuous data, Kruskal-Wallis test was used.).
| Clinical Variables | Data Subset Comparison | Tumour Microbiome Subtypes | |||||
|---|---|---|---|---|---|---|---|
| All Tumours (n = 178) | Triplets (n = 127) | p-Value | TMS1 (n = 46) | TMS2 (n = 55) | TMS3 (n = 77) | p-Value | |
| age at diagnosis | Mean (SD) | Mean (SD) | 0.804 | Mean (SD) | Mean (SD) | Mean (SD) | 0.887 |
| 66.92 (10.66) | 66.61 (10.61) | - | 66.89 (9.88) | 67.47 (11.39) | 66.55 (10.69) | - | |
| gender | n (%) | n (%) | 1 | n (%) | n (%) | n (%) | 0.729 |
| male | 99 (55.6) | 70 (55.1) | - | 25 (54.3) | 33 (60.0) | 41 (53.2) | - |
| female | 79 (44.4) | 57 (44.9) | - | 21 (45.7) | 22 (40.0) | 36 (46.8) | - |
| tumour localisation | n (%) | n (%) | 0.597 | n (%) | n (%) | n (%) | <0.001 |
| right | 64 (36.0) | 48 (37.8) | - | 28 (60.9) | 11 (20.0) | 25 (32.5) | - |
| transverse | 19 (10.7) | 13 (10.2) | - | 6 (13.0) | 5 (9.1) | 8 (10.4) | - |
| left | 44 (24.7) | 36 (28.3) | - | 4 (8.7) | 17 (30.9) | 23 (29.9) | - |
| rectosigmoideum | 32 (18.0) | 23 (18.1) | - | 6 (13.0) | 10 (18.2) | 16 (20.8) | - |
| rectum | 19 (10.7) | 7 (5.5) | - | 2 (4.3) | 12 (21.8) | 5 (6.5) | - |
| grade | n (%) | n (%) | 0.998 | n (%) | n (%) | n (%) | <0.001 |
| NA, in situ | 7 (3.9) | 5 (3.9) | - | 0 (0.0) | 3 (5.5) | 4 (5.2) | - |
| 1 | 18 (10.1) | 12 (9.4) | - | 1 (2.2) | 5 (9.1) | 12 (15.6) | - |
| 2 | 102 (57.3) | 73 (57.5) | - | 18 (39.1) | 37 (67.3) | 47 (61.0) | - |
| 3 | 51 (28.7) | 37 (29.1) | - | 27 (58.7) | 10 (18.2) | 14 (18.2) | - |
| AJCC stage | n (%) | n (%) | 0.968 | n (%) | n (%) | n (%) | 0.136 |
| 0 | 8 (4.5) | 6 (4.7) | - | 0 (0.0) | 3 (5.5) | 5 (6.5) | - |
| I | 31 (17.4) | 26 (20.5) | - | 2 (4.3) | 12 (21.8) | 17 (22.1) | - |
| II | 66 (37.1) | 45 (35.4) | - | 21 (45.7) | 19 (34.5) | 26 (33.8) | - |
| III | 48 (27.0) | 34 (26.8) | - | 16 (34.8) | 12 (21.8) | 20 (26.0) | - |
| IV | 25 (14.0) | 16 (12.6) | - | 7 (15.2) | 9 (16.4) | 9 (11.7) | - |
| tumour pathologic stage | n (%) | n (%) | 0.979 | n (%) | n (%) | n (%) | 0.007 |
| pTis | 8 (4.5) | 6 (4.7) | - | 0 (0.0) | 3 (5.5) | 5 (6.5) | - |
| pT1 | 11 (6.2) | 10 (7.9) | - | 0 (0.0) | 5 (9.1) | 6 (7.8) | - |
| pT2 | 32 (18.0) | 24 (18.9) | - | 2 (4.3) | 12 (21.8) | 18 (23.4) | - |
| pT3 | 115 (64.6) | 79 (62.2) | - | 42 (91.3) | 30 (54.5) | 43 (55.8) | - |
| pT4 | 12 (6.7) | 8 (6.3) | - | 2 (4.3) | 5 (9.1) | 5 (6.5) | - |
| regional lymph nodes pathologic stage | n (%) | n (%) | 0.618 | n (%) | n (%) | n (%) | 0.041 |
| pN0 | 109 (61.2) | 79 (62.2) | - | 23 (50.0) | 36 (65.5) | 50 (64.9) | - |
| pN1 | 46 (25.8) | 36 (28.3) | - | 13 (28.3) | 10 (18.2) | 23 (29.9) | - |
| pN2 | 23 (12.9) | 12 (9.4) | - | 10 (21.7) | 9 (16.4) | 4 (5.2) | - |
| synchronous distant metastasis | n (%) | n (%) | 0.846 | n (%) | n (%) | n (%) | 0.722 |
| M0 | 153 (86.0) | 111 (87.4) | - | 39 (84.8) | 46 (83.6) | 68 (88.3) | - |
| M1 | 25 (14.0) | 16 (12.6) | - | 7 (15.2) | 9 (16.4) | 9 (11.7) | - |
| MSI/MSS | n (%) | n (%) | 1 | n (%) | n (%) | n (%) | <0.001 |
| MSI | 27 (15.2) | 19 (15.0) | - | 16 (34.8) | 4 (7.3) | 7 (9.1) | - |
| MSS | 110 (61.8) | 81 (63.8) | - | 22 (47.8) | 37 (67.3) | 51 (66.2) | - |
| NA | 41 (23.0) | 27 (21.2) | - | 8 (17.4) | 14 (25.4) | 19 (24.7) | - |
| BRAF | n (%) | n (%) | 1 | n (%) | n (%) | n (%) | 0.022 |
| BRAF wt | 77 (43.3) | 53 (41.7) | - | 17 (37.0) | 27 (49.1) | 33 (42.9) | - |
| BRAF mut | 12 (6.7) | 9 (7.1) | - | 7 (15.2) | 1 (1.8) | 4 (5.2) | - |
| NA | 89 (50.0) | 65 (51.2) | - | 22 (47.8) | 27 (49.1) | 40 (51.9) | - |
| KRAS | n (%) | n (%) | 1 | n (%) | n (%) | n (%) | 0.839 |
| KRAS wt | 24 (13.5) | 17 (13.4) | - | 7 (15.2) | 8 (14.5) | 9 (11.7) | - |
| KRAS mut | 13 (7.3) | 9 (7.1) | - | 5 (10.9) | 4 (7.3) | 4 (5.2) | - |
| NA | 141 (79.2) | 101 (79.5) | - | 34 (73.9) | 43 (78.2) | 64 (83.1) | - |
| NRAS | n (%) | n (%) | 1 | n (%) | n (%) | n (%) | 0.553 |
| NRAS wt | 37 (20.8) | 26 (20.5) | - | 11 (23.9) | 12 (21.8) | 14 (18.2) | - |
| NRAS mut | 2 (1.1) | 1 (0.8) | - | 1 (2.2) | 1 (1.8) | 0 (0.0) | - |
| NA | 139 (78.1) | 100 (78.7) | - | 34 (73.9) | 42 (76.4) | 63 (81.8) | - |
CRC—colorectal cancer, TMS—tumour microbial subtypes, SD—standard deviation, NA—not available, pT—tumour pathologic stage, pTis—tumour in situ, pN—regional lymph nodes pathologic stage, M—synchronous distant metastasis, MSI—microsatellite instability MSS—microsatellite stable, wt—wild type, mut—mutation.
3.1. Microbial Categorisation According to Sample Type
There was no significant difference between the read counts across different sample types (paired analysis of sample triplets, see Methods).
The analysis of the 127 triplet samples revealed that the microbial diversity was significantly decreased in mucosal samples (both tumour mucosa and visually normal mucosa swabs) compared to stool, as measured by the number of observed species, Chao 1 and Shannon index (Figure S1). No differences were found between the tumour mucosa swabs and visually normal mucosa swabs.
Overall, in all the 483 samples, we identified 5449 ASVs: of these, 4800 ASVs in the 127 triplet samples. The QIIME assigned species only to 48 ASVs. Hence, we also performed a manual BLAST search to the SILVA database (Table S5).
For further analysis, however, we operated on higher taxonomic levels. After the taxa filtering step (Table S4), 13 phyla, 25 classes, 43 orders, 75 families and 264 genera were identified in the 127 triplets, most of which in all three sample types (Table S6). Inclusion of the additional 51 duplets (tumour mucosa and visually normal mucosa swabs) resulted only in slight differences at the genus level—the identified taxa remained the same. What changed was their unique presence in some sample types (Text S1).
While most of the genera were found in all three sample types, their incidence and abundance across sample types varied greatly between mucosal samples and stool, both in overall and pairwise comparisons (Text S1, Figure S16). In this case, 14 genera (Stomatobaculum, Pseudoramibacter, Pelomonas, Pasteurella, Mycoplasma, Kingella, Johnsonella, Helicobacter, Deinococcus, Centipeda, Bergeyella, Actinobacillus, Abiotrophia and an unassigned genus from order Comamonadaceae) were detected only in mucosal (tumour and visually normal) samples (Figure S2).
We further analysed the pairwise incidence of the 264 genera across sample types. We found that 104 genera varied significantly across sample types (analysis of 127 triplets, Text S1, Table S7).
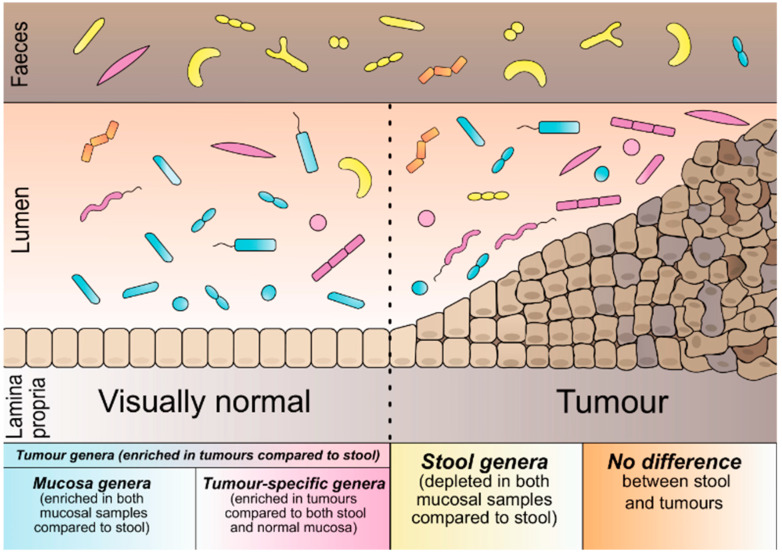
To categorise the microbial genera based on their preferred environment: we compared their abundance across sample types. Of the 264 genera, 121 differed significantly in abundance across the sample types (Tables S8 and S9, Figure S3). Based on these results, we defined five microbial categories (Figure 1). The first is based solely on the results of tumour vs stool comparison: tumour genera (57 genera, more abundant in tumours than stool). Additionally, within the category of tumour genera, we defined mucosa genera (52 genera, also enriched in visually normal mucosa compared to stool) and tumour-specific genera (16 genera of tumour category, additionally enriched in tumours compared to visually normal mucosa). In this case, 49 genera were significantly more abundant in stool than tumours and visually normal mucosa from the group of stool genera. The fifth category was defined as the no-difference genera (143 genera, no difference across any of the sample types) (Text S1).
Figure 1.
Schematic representation of bacterial categories according to their preferred environment.
3.2. The Landscape of CRC Tumour Microbiome
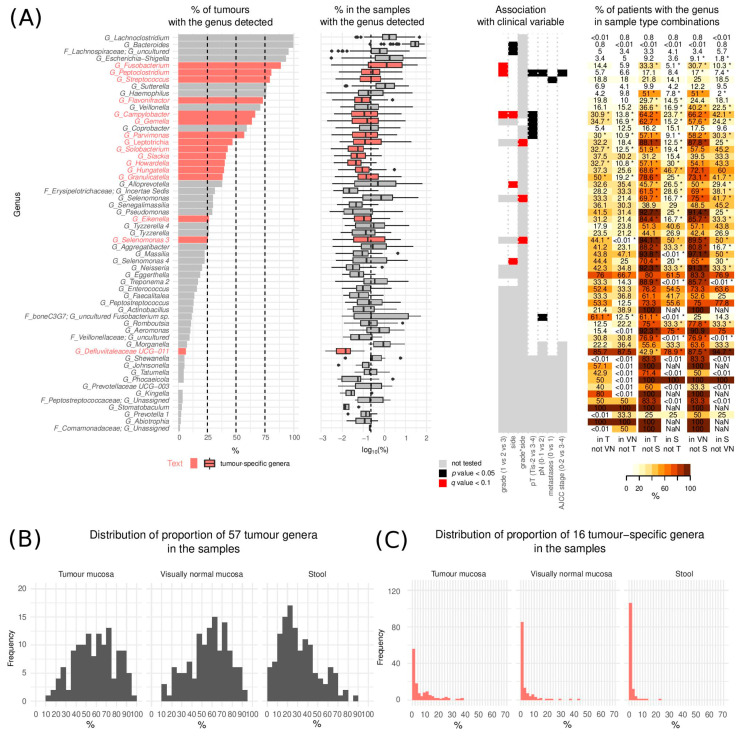
For the description of tumour mucosa microbial heterogeneity without stool contaminants, we only considered species that were statistically significantly enriched in tumour mucosa compared to stool. We hence investigated the group of 57 tumour genera with a special focus on the subgroup of 16 tumour-specific genera (Gemella, Granulicatella, Parvimonas, Hungatella, Peptoclostridium, Flavonifractor, Selenomonas 3, Fusobacterium, Leptotrichia, Eikenella, Campylobacter, Slackia, Streptococcus, Howardella, Solobacterium, Defluviitaleaceae UCG-011, Figure 2A).
Figure 2.
Tumour genera. (A) (left) Proportion of tumours with the genera detected and distribution of their respective relative abundances (in %) in the samples where they were detected (middle) and association of the bacteria with clinical variables (right). The vertical dashed line represents the median relative abundance of all 264 detected genera (median = 0.24%). The boxplot middle vertical line represents median, the box represents the interquartile range (IQR), the whiskers extend to +/−1.5 IQR. The black dots refer to outliers. (B) Overall proportion of the 57 tumour genera in the three sample types (n = 127) (C) Overall proportion of the 16 tumour-specific genera in the three sample types (n = 127). (Tis—Tumour in situ, pT—tumour pathologic stage, pN—regional lymph nodes pathologic, T—tumour swabs, VN—visually normal mucosa swabs, S—stool, NaN—not a number). * p < 0.05.
We performed the analysis of co-occurrence and observed significantly increased co-occurences between 20 tumour genera (of which 13 tumour-specific) (Text S1, Figure S4, Table S10). We also observed 14 significantly decreased co-occurrences between genera (Text S1, Figure S4, Table S10).
Tumour genera incidence ranged from 1.1% to 99.4% (median 26.4%) of tumours with the median abundance of the individual genera in the samples with the genus detected ranging from 0.01% to 29.8% (median 0.15%) (Figure 2A). Overall, tumour genera constituted 1.1% to 97% (median 59.6%) while the tumour-specific genera constituted between 0.0–62.3% (median 3.1%) of the microbiome found on tumour mucosa (Figure 2C).
We performed a detailed literature search (Table S11) which revealed that tumour genera consisted predominantly of oral bacteria, many known as oral pathogens.
Some of the tumour genera of (possible) oral origin identified in our study, while previously associated with CRC, were never reported on tumour mucosa, namely Solobacterium (increased in CRC faecal samples [35]), Slackia and Pseudomonas (decreased [12,19] in CRC faecal samples), and Treponema (the presence of which in the oral cavity was associated with increased risk of CRC [33]).
We newly identified many genera of both oral and gut origin, not previously associated with CRC, with increased abundance in the tumour lesions: Selenomonas 3, Selenomonas 4, Aggregatibacter, Actinobacillus, Bergeyella, Phocaeiola, Defluviitaleaceae UCG-011, Abiotrophia, Johnsonella, Stomatobaculum, Kingella, Shewanella, Tatumella, Senegalimassilia, Aeromonas, Prevotellaceae UCG-003, Incertae Sedis genus from family Erysipelotrichaceae, an uncultured species from Veillonelaceae family, and an uncultured species from boneC3G7 at the family level (BLAST hit Fusobacterium necrophorum) (oral origin) and Tyzzerella 4, Massilia and an unassigned genus from Peptostreptococcaceae family (gut origin).
Amongst tumour genera of gut origin, Lachnoclostridium, Flavonifractor [65,66], Sutterella and Hungatella (ex-Clostridium hathewayi) [67] were previously only reported increased in the stool of patients with CRC.
3.3. Microbiome and Clinical Variables
Prior to the subtype derivation, we assessed the association of bacterial genera from all the sampled environments with the clinical parameters and interpreted the results based on our microbial categorisation. We performed partial validation on three publicly available datasets.
β-diversity analysis by NMDS performed on each sample type separately showed that tumour location was the factor with the highest influence on total microbiome composition for all sample types, while tumour histological grade affected only tumour samples (Text S1, Table S12, Figures S5 and S6).
The results of regression analysis for each clinical variable are summarised in Table 2 and Table S13, and Figures S7–S10; the detailed results of partial validation are presented in Text S2, Tables S1, S2 and S14.
Table 2.
Summary of rank regression results (p < 0.05) associating microbiome of the three different sample types with the clinical variables. Bold text denotes genera significant at FDR < 0.1, text underlined by a solid line denotes that the association was validated in an independent dataset, marked by the superscript number (1 Feng et al. [30]; 2 Dejea et al. [31], * previously published association [40,66,68,69,70,71,72], see Discussion and Table S11). Up and down arrows denote increase or decrease in abundance, respectively.
| Regression Covariate | Effect/Contrast | Tumour Mucosa | Visually Normal Mucosa | Stool |
|---|---|---|---|---|
| grade | increasing grade | ↑ Fusobacterium *,Campylobacter*, Leptotrichia, Peptoclostridium, Mogibacterium * | - | - |
| - | ↓ Unassigned genus from order Opitutae vadin HA64 | - | ||
| location | right-sided/transverse vs left-sided and rectum/rectosigmoid | ↑ Holdemania, Selenomonas 4, Clostridium sensu stricto 1, Alloprevotella | ↑ Selenomonas 3, Selenomonas, Treponema 2 | - |
| ↓ Bifidobacterium *, Christensenellaceae R-7 group2, Ruminococcaceae UCG-013, Fusicatenibacter | ↓ Lachnospira, Bifidobacterium, Coprococcus 1, Christensenellaceae R-7 group | - | ||
| right-sided/transverse vs left-sided | ↑ Campylobacter, Alloprevotella | - | - | |
| ↓ Family XIII AD3011 group, Coprococcus 1 | - | |||
| right-sided/transverse vs rectosigmoid/rectum | ↑ Oribacterium, Fretibacterium | - | - | |
| - | ↓ [Eubacterium] ventriosum group | |||
| grade*location interaction | low-graded; right-sided/transverse | ↑Ruminococcaceae UCG-010, uncultured bacterium from Clostridiales vadinBB60 group | - | ↑ Unassigned genus from order Opitutae vadin HA64, Porphyromonas |
| grade 2; left-sided | ↓Coprococcus 2, Ruminiclostridium 6, [Eubacterium] ventriosum group, Incertae Sedis from Lachnospiraceae family | ↓ Gemella, Corynebacterium 1 | ↓ Ruminiclostridium 6, Coprococcus 2 | |
| grade 2; rectosigmoid/rectum | - | ↑ Veillonella | ↑ Veillonella | |
| ↓ Methanobrevibacter, Dielma, Victivallis | ↓ Methanobrevibacter, an uncultured genus from the Peptococcaceae family | ↓ Victivallis, Ruminiclosridium 6, Lachnospiraceae UCG-005, an unassigned genus from order Mollicutes RF9 | ||
| grade 3; right-sided/transverse | ↑ Prevotella, Selenomonas, Selenomonas 3 | - | - | |
| grade 3; left-sided | - | ↑ Eisenbergiella, Leptotrichia, Escherichia-Shigella, Veillonella | ↑ Veillonella, Prevotella 7 | |
| ↓ Coprococcus 2, Ruminiclostridium 6, [Eubacterium] ventriosum group, Incertae Sedis from Lachnospiraceae family, Odoribacter | ↓ Gemella, Corynebacterium 1 | ↓ Coprococcus 2 | ||
| grade 3; rectosigmoid/rectum | ↑ Lachnospira | ↑ Veillonella | ↑ Prevotella, Prevotella 7 | |
| ↓ Methanobrevibacter, Dielma, Victivallis | ↓ Methanobrevibacter, Eisenbergiella, an uncultured genus from the Peptococcaceae family | ↓ Lachnospiraceae UCG-005, unassigned genus from order Mollicutes RF9 | ||
| AJCC stage | III–IV vs 0–II | ↑ Peptoclostridium | - | ↑ Akkermansia |
| - | ↓ Gelria | - | ||
| Tumour pathologic stage | pT 3–4 vs pTis-2 | ↑ Peptoclostridium, Gemella, Campylobacter, Parvimonas | ↑ Peptoclostridium, Escherichia-Shigella, an unassigned species from Ruminococcaceae | ↑ Escherichia-Shigella |
| ↓ Coprobacter, Intestinimonas, Ruminococcaceae UCG-009, Oscillospira, Cloacibacillus | ↓ Intestinimonas, Ruminococcaceae UCG-009, Holdemanella, Coprobacter, Gelria, an uncultured genus from the Christensenellaceae family | ↓ Prevotella 6, Ruminococcaceae UCG-011 1 | ||
| Regional lymph nodes stage | N1–2 vs N0 | ↑ Peptoclostridium | - | ↑ Peptococcus, Campylobacter, Akkermansia *, Selenomonas, Porphyromonas *, Streptococcus, Oscillospira |
| ↓ Prevotellaceae UCG-001, uncultured Fusobacterium sp. from family boneC3G7 | ↓ [Eubacterium] hallii group | ↓ Faecalibacterium, Ruminiclostridium, Dorea 1, Lachnospiraceae FCS020 group | ||
| Synchronous distant metastasis | present vs absent | ↑ Porphyromonas, Streptococcus, Ruminococcaceae UCG-005 | ↑ Akkermansia | ↑ uncultured genus from Erysipelotrichaceae family, Akkermansia, Coprococcus 1, Solobacterium |
| - | ↓ Gelria, [Eubacterium] brachy group, uncultured genera from Christensenellaceae family, Gordonibacter, Fretibacterium | ↓ Selenomonas, Ruminococcaceae UCG-004 |
FDR-false discovery rate.
Increased abundance of Fusobacterium, Campylobacter and Leptotrichia in tumour mucosa appeared to be independent predictors of tumour’s higher grade (p < 0.01, FDR < 0.1). Leptotrichia was significantly increased on visually normal mucosa adjacent to grade 3 left-sided tumours (p < 0.05, FDR < 0.1).
The mucosa of grade 3 right-sided tumours was enriched in Prevotella, Selenomonas and Selenomonas 3 (p < 0.01, FDR < 0.1). Prevotella was also increased in the stool of patients with grade 3 rectosigmoid/rectum tumours (p < 0.01, FDR < 0.1). The mucosa of grade 3 tumours of the rectosigmoid/rectum and visually normal mucosa adjacent to left, rectosigmoid and rectal tumours, regardless of the grade, were enriched in Lachnospira (p < 0.05, FDR < 0.1).
The mucosa of left-sided (for some including rectosigmoid/rectum) low-grade tumours was enriched in Ruminiclostridium 6, Coprococcus 2, [Eubacterium] ventriosum group, Clostridiales Vadin BB60 group, Ruminococcaceae UCG-010 and an uncultured species and an Incertae Sedis genus from the Lachnospiraceae family (p < 0.01, FDR < 0.1). Ruminoclostridium 6 remained enriched also in the stool of patients with grade 2 left-sided, rectosigmoid and rectal tumours (p < 0.01, FDR < 0.1). Methanobrevibacter, Victivallis were significantly enriched in the mucosa of low-grade tumours of rectosigmoid and rectum (both p < 0.01, FDR < 0.1).
Christensenellaceae R-7 group, Bifidobacterium and Ruminococcaceae UCG-013 were increased in mucosa of the left-sided, rectosigmoid and rectal tumours (p < 0.01, FDR < 0.1). Similar associations were found for visually normal mucosa for Christensenellaceae R-7 group, Coprococcus 1, Lachnospira and Bifidobacterium (p < 0.01, FDR < 0.1). The increased abundance of the Christensenellaceae R-7 group in tumour mucosa of left-sided tumours was also validated in an independent dataset (p = 0.0047) (Text S2, Table S14). When comparing early (0–II) and advanced (III–IV) stages, we identified an increased abundance of Akkermansia in the stool of advanced stage tumours (p < 0.01, FDR < 0.1) (Table S13, Figures S11 and S12).
Patients with advanced T stages (pT 3–4) were characterised by a significant increase in abundance of Gemella, Campylobacter, Peptoclostridium and Parvimonas (p < 0.01, FDR < 0.1) on tumour mucosa, and increased Peptoclostridium, Escherichia-Shigella (p < 0.01, FDR < 0.1) in the adjacent visually normal mucosa. Early T stage tumours (pTis-2) were associated with an increase in Coprobacter, on tumour mucosa, increased Intestinimonas, Ruminococcaceae UCG-009, Holdemanella and Coprobacter on the adjacent visually normal tissue (p < 0.05, FDR < 0.1) and Prevotella 6 (p < 0.01, FDR < 0.1) and Ruminococcaceae UCG-011 (p < 0.05, FDR > 0.1) in the stool (Table S13, Figures S11 and S13). We validated the decrease of Ruminococcaceae in the stool of patients with pT 3–4 stage (p = 0.00113, Feng et al.) (Text S2, Table S14).
The presence of metastases (local or distant) at the time of diagnosis was predominantly associated with changes in the stool microbiome. Except for the increased abundance of Akkermansia in stool of patients with N1–2 stage tumours (p < 0.01, FDR < 0.1) and of the uncultured genus from the Erysipelotrichaceae family in the stool of patients with synchronous distant metastases (p < 0.01, FDR < 0.1), none of these associations were significant after FDR correction (Table S13, Figures S11, S14 and S15). Nevertheless, we validated the decrease of Dorea in the stool of patients with N1–2 stage tumours (p = 0.00011) in an independent dataset (Feng et al.) (Text S2, Table S14).
3.4. Tumour CRC Microbial Subtypes
We continued our characterisation of tumour microbial heterogeneity by performing hierarchical clustering of patients based on the relative abundance of the 57 tumour genera in the tumour mucosa samples (See Methods). Once the subtypes were identified, we performed between-subtype differential abundance analyses of microbiome profiles in all three sampling environments.
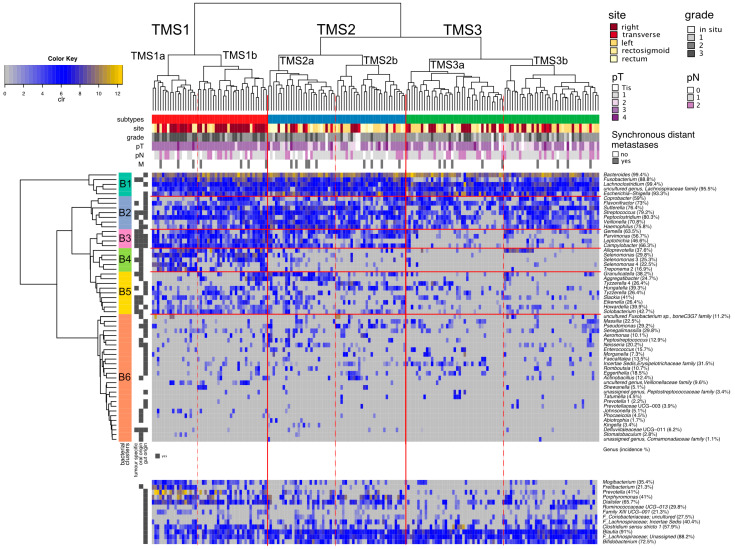
Based on the tumour genera profiles, we observed three major subtypes of tumours (TMS1–TMS3), that could further be divided into two groups each (Figure 3 and Figure 4). The bacteria were clustered into six groups B1–B6 (Figure 3, Table S12).
Figure 3.
Tumour microbial subtypes. Hierarchical clustering of tumours (Aitchinson distance) and genera (Euclidean distance) based on the clr-transformed abundances of 57 tumour genera. Clinical variables of individual patients are shown. Proportions right to the genera name denote incidence of the genus in 178 tumour-mucosa samples. (TMS—tumour microbial subtypes, clr—centered log—ratio transformation, pT—tumour pathologic stage, pN—regional lymph nodes pathologic, M—synchronous distant metastasis, Tis—tumour in situ).
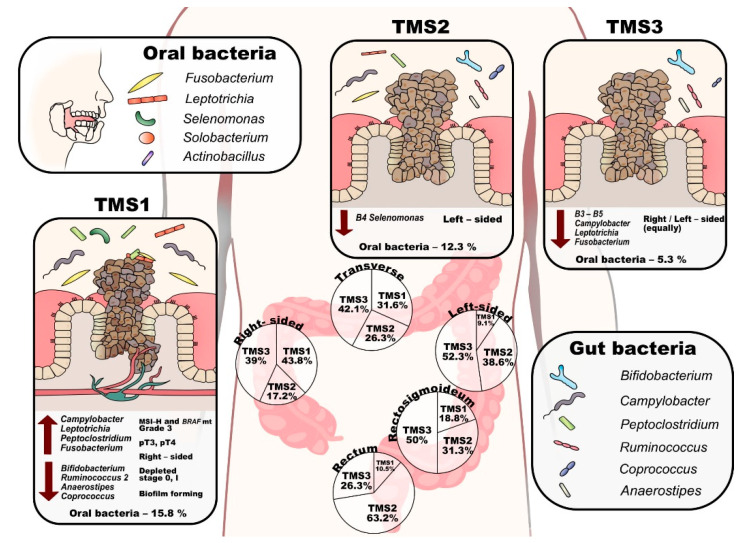
Figure 4.
Scheme of the tumour microbial subtypes. (TMS—tumour microbial subtypes, pT—tumour pathologic stage, MSI-H— microsatellite instability-high).
The B1 group and B2 group are represented by typical gut microbiome members. The B1 group consists of the five most common and most abundant genera Fusobacterium, Lachnoclostridium, Bacteroides, Escherichia-Shigella and one uncultured genus from the family Lachnospiraceae. All tumours contain at least three of these bacteria, most tumours (78.7%) all five. These bacteria have high co-occurrence across the sampled environments (Figure 2A, fourth panel), except for Fusobacterium, predominantly found in mucosa samples. The B4 group contains exclusively oral microbiome genera, and we named it the Selenomonas group due to its enrichment in the Selenomonas genera. B3 and B5 groups include mostly oral microbiome genera. These genera have significantly different incidence across the sampled environments, with 45.7–94.1% of patients missing these genera in the stool if present on tumour mucosa. Group B6 consists of 27 less common species with incidence ranging from 0% to 37% (median 11.1%).
Tumour microbial subtype 1 (TMS1) represents 26% (46) of tumours and is defined by the presence of B1–B4 microbial groups, and overall contains most of the high-grade associated genera (Fusobacterium, Campylobacter, Leptotrichia, Peptoclostridium and Selenomonas, see Table 2). This subtype is enriched in right-sided (60.9%), grade 3 (58.7%), pT3 or pT4 stage (95.6%) tumours and is depleted of stage 0 and stage I tumours (0% and 4.3%, respectively) (Table 1, Figure 4). In addition, TMS1 contains significantly more tumours with MSI-H (34.8%) and BRAF mutation (15.2%) compared to other tumour microbial subtypes. TMS1 differs from TMS2 and TMS3 by the presence of the Selenomonas group (B4), Solobacterium and Howardella species, and Clostridium sensu stricto 1. In contrast to other subtypes, this subtype shows a significantly decreased abundance of typical faecal commensals such as Bifidobacterium, Ruminococcus 2, Anaerostipes and Coprococcus 1 on tumour mucosa (Table S15). In stool samples, we observed a higher abundance of Prevotella and Clostridium sensu stricto 1 (Table S16).
Tumour microbial subtype 2 (TMS2) comprises 31% (55) of tumours and is defined mainly by the absence of B4 bacteria (the Selenomonas group). This subtype can be further divided into two groups by the increased incidence of Leptotrichia, Granulicatella, Aggregatibacter and Neisseria (TMS2a) or Tyzzerella 4, Hungatella (ex-Clostridium hathewayi), Solobacterium, Pseudomonas and Porphyromonas (TMS2b). TMS2 tumours are predominantly from the left side, rectosigmoid or rectum (70.9%) (Table 1, Figure 4). The mucosa of TMS2 tumours shows a significantly higher abundance of Haemophilus, Sutterella, Veillonella and Streptococcus and a lower abundance of Alloprevotella (Table S15). Alloprevotella was also significantly decreased in stool samples (Table S16).
Finally, the largest subtype, TMS3, represents 43% (77) of tumours and is mostly missing the B3–5 bacterial groups and most of the high-grade related species. TMS3 is characteristic by an increased proportion of grade 1 tumours (15.6%). In the TMS3 microbial subtype, right-sided and left-sided tumours are equally represented (Table 1, Figure 4). The subtype can be further divided by increased incidence of Incertae sedis from the Erysipelotrichaceae family and Tyzzerella 4 (TMS3a) or Clostridium sensu stricto 1, Ruminococcaceae UCG-013 and Incertae sedis from Lachnospiraceae family (TMS3b). Interestingly, subtype TMS3 contains all the tumours that lack Fusobacterium species (most of them in TMS3a) both in their mucosa and in the patients’ stool.
Most importantly, the subtypes differed significantly in the proportion of the oral genera with TMS1 median of 15.8%, TMS2 median of 12.3% and TMS3 median of 5.3% (p < 0.001). We then explored the estimated metabolic potential of the microbial communities specific to the tumour subtypes (Table S17). TMS1 is characterised by functional shifts in bacterial composition, including the increase in gene content specific for nucleotide metabolism, metabolism of terpenoids and polyketides and energy metabolism (p < 0.05, FDR < 0.1), reduction in lipid metabolism and xenobiotics biodegradation and metabolism (p < 0.05, FDR < 0.1). At the lower functional level, TMS1 subtype was characterised by increased peptidoglycan biosynthesis, novobiocin biosynthesis and ansamycin biosynthesis (p < 0.05, FDR < 0.1). The TMS2 subtype exhibited the highest score of xenobiotics biodegradation and metabolism. TMS3 subtype showed enhanced biosynthesis of other secondary metabolites, carbohydrate metabolism and amino acid metabolism and reduced metabolism of other amino acids (p < 0.05, FDR < 0.1).
4. Discussion
Carcinogenesis of colorectal cancer is a complex process with a unique set of somatic molecular changes. Considerable efforts have been dedicated to understanding the heterogeneity of CRC and deriving clinically applicable molecular markers of the disease progression and patients’ response to therapy. Approaching the problem from the molecular perspective in supervised analyses led to identifying several molecular markers and signatures with limited clinical use [73]. The unsupervised approach led to the definition of four consensus molecular subtypes [74], which, surprisingly, bear some prognostic value. The CRC heterogeneity puzzle, however, is far from being solved. One of the reasons is that the tumour microenvironment, especially the microbiome, seems to play a much more critical role than imagined. Many studies correlated the dysbiosis of the gut microbiome with the development of colorectal cancer in the healthy mucous-adenoma-carcinoma sequence or focused on elucidating the concrete role of selected bacterial species in the gut (colorectal) pathogenesis progression [4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22].
In contrast, our study aimed to use an unsupervised approach to characterise the heterogeneity of the CRC gut microbiome in the ongoing disease to discover unforeseen patterns. The comparison of microbial communities of stool, tumour mucosa and adjacent visually normal mucosa provided us with insights into the preferred environment of the observed species. The resulting microbial categorisation served to focus downstream analyses and to interpret our findings. We based the characterisation of the CRC tumour microbial landscape by performing subtyping of patients on bacteria with increased abundance in tumour mucosa compared to the stool to filter out potential stool contaminants. With a median of 59.6%, the tumour genera represented an essential fraction of the total microbiome found on tumour mucosa. Interestingly, the tumours of different microbial subtypes differed in the on-mucosa abundance of typical faecal genera (both pathogenic and commensal) that were not used for their definition. The analysis of microbial composition between sample types confirmed previously reported observations [8,11,34] that mucosa-associated bacteria dominate the tumour mucosal microbiome and that these species are associated also with visually normal mucosa. It is debatable to what extent the non-cancerous tissue (however distant from the tumour) from the surgically removed segment is already influenced by the bacteria initiating CRC development. Consistent with the bacterial driver-passenger model as proposed by Tjalsman et al. [27] our mucosa genera could be bacterial drivers, while tumour-specific genera could be bacterial passengers. We observed that tumours harbour a diverse community of opportunistic pathogens of oral origin (31 of 57 tumour genera) as previously reported [29,31,75].
Multiple factors make the CRC tumour niche a favourable environment for oral bacteria, in particular, for oral pathogens. Some of the bacteria can bind to specific proteins overexpressed on tumour cells [76,77,78]. Inflammation in the oral tissue niche selects for those species that are most adapted to the new environment, producing specific molecules such as microbial proteolytic enzymes [79] that break down the host’s extracellular matrix and soluble factors to get nutrients and invade the tissue. In the digestive tract, some oral bacteria can change their oxygen requirements from facultative anaerobic to strict anaerobic and their metabolism from asaccharolytic to proteolytic [80]. Oral pathogens gaining a more favourable niche on colon tissue may shift the balance on their behalf, producing proteins playing a key role in biofilm formation [81]. Some of the oral genera detected in our study were previously never associated with CRC tumour mucosa (e.g., Selenomonas 3, Selenomonas 4, Aggregatibacter, Johnsonella, Abiotrophia, Defluviitaleaceae UCG-011). Most importantly, we newly associate 22 genera of both oral and gut origin with CRC overall. Some of these genera contain species that are known human pathogens causing infections of mucosal or other tissues such as: periodontal disease (Selenomonas, Phocaeiola Aggregatibacter) [82,83,84] infections in humans through animal bites (Bergeyella and Actinobacillus) [85,86]; endocarditis (B. cardium) or respiratory infections (A. hominis) [87,88]. For other genera, their potential involvement in CRC is not so obvious. The tumour-specific genera of Defluviitaleaceae might influence CRC through the metabolism of butyrate [89]. The association of Tyzzerella 4 from the Lachnospiraceae family with CRC may be due to its increased occurrence in patients with higher cardiovascular risk (CVR) factor scores [90], which are also associated with CRC [91]. Massilia was detected in patients with pancreatic cancer [92].
Correlating the tumour microbiome with clinical variables of tumour progression, such as grade or stage, bears the promise of offering viable hypotheses on the role of bacteria in the progression of the disease. Currently, the associations between clinical variables and gut microbial composition in an ongoing disease are understudied, and only a few efforts addressed the topic on limited cohorts.
The sample size of our study allowed for the study of the interaction of grade and tumour location, thus providing a finer estimation of the differences in the microbiome composition. We report 59 associations of 43 genera with tumour grade and/or location for all sample types studied. We confirmed previously reported high-grade tumour associations of Fusobacterium, Campylobacter and Mogibacterium, in CRC tumour mucosa [40,68]. We newly observed potentially beneficial effects of the increased abundance of 13 stool genera significantly associated with left location, namely decreasing tumour grade with increasing abundance, e.g., of Bifidobacterium, Ruminococcaceae UCG-010 and Victivallis in tumour mucosa; and of Porphyromonas and Lachnospiraceae UCG-005, in the stool. Bifidobacterium was previously shown to have anti-cancerogenic effects [66,69,70,71,72].
We also found location-dependent grade-predictive genera. Remarkably, while in the right colon a higher grade was associated with an increase in pathogenic genera (Prevotella, Selenomonas) on tumour mucosa, in the left colon a higher grade was associated with a depletion in possibly beneficial (commensal) genera (Methanobrevibacter, Coprococcus 2, Ruminiclostridium 6, Odoribacter, Dielma, Victivallis) on tumour mucosa or in the stool. We can only speculate whether the prolonged exposure of tumour mucosa to predominantly stool bacteria that is mechanistically related to tumours in a distant part of the colon (left-sided or with onset in rectosigmoid and rectum) can have potentially harmful or beneficial effects or whether any associations are mostly due to the well-known molecular differences in the right vs left-sided tumours [36,93,94]. The increased abundance of pathogens on the high-grade right-sided tumours might be the result of increased permeability of proximal gut mucosa [95], but the relevance of the animal models was questioned [96].
We confirmed a previously published increase of Akkermansia and Porphyromonas in the stool of patients with local metastases [72], and newly associated increased Akkermansia in stool in patients with stage III–IV CRC. We noted that the occurrence of synchronous local and distant metastases was mainly associated with shifts in stool microbiome, while tumour specific variables such as grade or location were associated with changes in tumour microbiome. On one side, this observation raises the possibility of microbiome-based non-invasive metastasis diagnostics in colorectal cancer or monitoring the patients at risk. On the other hand, the alteration of the stool microbial community might only reflect changes in the overall health status in the presence of metastasis and cancer progression itself similarly to non-colonic malignancies [97,98,99].
Pairwise analysis of the incidence of all genera across sample types helped us to assess their screening potential. On-tumour microbes with significant clinical associations and no difference in incidence across sample types are perfect candidates for stool-based screening studies or stool-based prognostic and predictive classifiers. Most of the tumour-specific genera, if present on tumour mucosa, were not identified in stool of the same patients in more than 50% of cases. Given that these genera prefer the mucosal environment over the stool, such associations are not entirely surprising. Consequently, these genera are better candidates for colonoscopy biopsy sample screening.
We then compared how the previously suggested stool-based predictive microbial markers of CRC (compared to healthy and adenomas) [29] behave with respect to the progression of an ongoing disease (associations with grade or stage) as a result of tumour microenvironment changes. Some retained their predictive potential of progression of the disease as stool predictors of the presence of local metastases (increase in Campylobacter, Porphyromonas, Streptococcus and decrease in Lachnospiraceae and Faecalibacterium). Some showed no significant clinical associations in stool, but their increased abundance on tumour mucosa was predictive of high pT stage (Parvimonas) or grade (Fusobacterium).
The three tumour–mucosa-based microbial subtypes we derived on patterns of similarity of the abundance of the tumour genera represent the first attempt to systematically describe microbial heterogeneity of CRC tumour environment. We were intrigued to see that compared to subtyping efforts based on gene expression [74,100], also microbial profiling identified one subtype (TMS1) enriched in BRAF mutant, MSI-H, right-sided tumours. An interesting observation was that the tumour microbial subtypes differ not only in the type of the tumour genera they host but also in the count of potentially pathogenic microbiome correlated with high grade and stage and the proportion of oral pathogens within the tumour genera. Of the 10 high grade or high stage-related genera, TMS1 tumours had a median of 8 (80%), TMS2 of 6 (60%) and TMS3 of 4 (40%), differing thus in what we could call “microbial pathogens burden”. This subtyping could reflect differences in tumour biological properties linked with cancer progression: malignant tumours with active growth, cell and tissue atypia because of disruption of the mucus layer and dysregulation of local immunity provide more comfortable conditions to aggressive microbial consortia expansion and unconventional (oral) species homing. Moreover, with respect to the bacteria-supported model of carcinogenesis, proved in animal models [10,101], the pathogenic bacteria growth leads to additional dedifferentiation of tumour cells forming the pathogenetic loop. The differences in the proportion of oral pathogens and metabolic potential lead us to the hypothesis that the TMS1 subtype is enriched in tumours with microbial biofilms. This subtype is enriched in right-sided tumours and compared with the other two subtypes, is enriched in the presence of oral bacteria. Recently, biofilms have been associated with right-sided CRC [31]. Drewes et al. [102] identified several biofilm-associated shifts, including the functional alteration in peptidoglycan biosynthesis, novobiocin biosynthesis and ansamycin biosynthesis, which were significantly increased in the TMS1 subtype. Studies show that the commensal and the pathogenic periodontal bacteria (Fusobacterium, Porphypomonas) produce proteins such as gingipains [81] and RadD [103], which can play a key role in biofilm formation. Koliarakis et al. [75] proposed a new outlook on CRC pathogenesis driven by gut mucosa biofilm created by periodontopathic bacteria translocated into the colorectum. Tomkovich et al. [104] successfully demonstrated that polymicrobial biofilms are carcinogenic. Transcriptomic studies of periodontal tissues show that many organisms can fulfil gaps in metabolism, therefore the pathogenic community is more important as one unit than the virulence of one species [105].
It remains to be investigated whether the microbial subtypes could improve the prediction of patients’ survival and prognosis. We can speculate that the high microbial pathogen burden could worsen not only the tumour progression but also potentially the patient’s condition after the surgical resection and during and after the chemotherapy treatment. Given the fact that tumour-related genera reside also on visually normal mucosa, they could initiate CRC tissue dysplastic changes and malignisation. There is limited evidence of linkage between mucosal microbiota and metachronous adenomas growing demonstrated by Liu et al. [106]. On the other side, it is shown that the microbiome could interact and metabolise chemotherapeutic medicine, which leads to modulation of its activity and toxicity [107]. In the light of the above, modification of gut microbiome after colorectal cancer surgical removal might be considered as an additional step of treatment to prevent tumour recurrence and modulate chemotherapy effectiveness and toxicity.
The probable presence of biofilm in the TMS1 subtype might make this subtype of interest to potential prevention and treatment strategies. Importantly, although TMS1 is enriched in proximal tumours, it occurs in 9.1–18.8% of left, rectosigmoid and rectal tumours. Remarkably, biofilm communities from the colon biopsies of healthy individuals were as potent in inducing colon inflammation as the biofilm communities from CRC hosts [104]. The inhibition or removal of such biofilms from patients with CRC could represent a promising strategy for secondary CRC prevention and treatment but remains an uneasy task due to inefficiency of traditional antimicrobial strategies such as antibiotic treatment [108]. A recent study associated periodontitis with increased risk of high-grade proximal colorectal cancer [109]. Based on this, our results suggest an intriguing hypothesis: whether improving oral hygiene would impact the incidence of TMS1 tumours, or, more importantly, would lower the recurrence rate or development of secondary tumours in the TMS1 patients.
Another clinically relevant observation is the association of left-sided high-grade tumours with the depletion in protective species rather than increase in bacterial pathogens. This suggests that antibiotic treatment of patients with distal tumours may have a detrimental effect on their prognosis. Coadministration of probiotics in this case could be highly beneficial.
We believe that for certain patient populations, the inclusion of tumour mucosa sampling during colonoscopy for analysis of microbial composition could help to efficiently steer pre- and post-operative treatment decisions.
5. Conclusions
In our study, by analysis of 483 samples from n = 178 patients, we extended the current characterisation of the colorectal cancer microbiome in several directions. Thanks to the large sample size, we identified bacterial genera that were not previously associated with CRC tumour mucosa, clinical variables or with colorectal carcinoma at all. These genera should be studied in more detail to describe their mechanism of interaction with the disease.
By focusing on microbial community analysis, in contrast to classical microbiome-centred approaches, we were able to identify co-occurring species and three major tumour-microbial subtypes that correlate with clinical variables, such as grade, location and TNM staging. The subtypes also differ in what we describe as microbial pathogens burden—the number of pathogenic species correlated with increased grade and stage present on tumour mucosa, although the concept can be defined with respect to all three environments (tumour mucosa, visually normal mucosa and stool).
An important limitation of our study is the lack of proper validation of all the results since adequate data is unavailable, hence these results must be taken cautiously. Additionally, it is well known that the gut microbial composition changes with dietary patterns and lifestyle, which could be region-based [98]. More studies of similar sample size or larger from different geographical locations, are needed to derive robust and generalisable patterns. We make the full data available, including clinical variables, as a first step towards building a data corpus that could support such investigations. The nature of the samples (mucosa) prohibited us from using more advanced whole-metagenomic sequencing due to severe human DNA contamination issues [110,111,112]. The technology chosen was high throughput, fitting the purpose of microbial community-based analysis. We did perform the sequence matching for the identified ASVs against the SILVA database, however, being aware of the limitations, we provide these results solely as supplementary information without discussing them here in detail.
Having sampled the microbiome at three different complementary sites allowed the study of several environments leading to the definition of novel microbial categories with multiple implications. Our study shows that the associations with clinical variables found for the tumour mucosal or adjacent visually normal mucosa microbiome are rarely preserved in the microbial composition of stool and vice versa. While tumour histological grade, stage and location are reflected in the corresponding mucosal microbiome, the presence of lymph nodes or distant metastases influences mainly the stool microbiome. It seems that the mucosa and stool microbiome are complementary with respect to the modulation of their effects on disease progression. Tumour-mucosa biopsies from colonoscopy might need to be coupled with stool sampling for efficient screening or diagnostic purposes.
Understanding the role of tumour-subtype specific microbial communities could lead to tailored strategies of CRC patient gut microbiome management through lifestyle and diet recommendations including probiotic and antimicrobial interventions.
Our study is a step forward in understanding the role of the microbiome and its interactions with other factors involved in oncogenesis and tumour progression. Rather than providing definite answers it opens new avenues for exploring new treatments and biomarkers.
Acknowledgments
The authors acknowledge the help of the volunteers enrolled in this study. We thank the ONCOBIOME researchers for their insight and suggestions.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/cancers13194799/s1, Figure S1: Number of reads and diversity comparison of three sample types on 127 triplets, Figure S2: Genera which were detected only in some of the three sample types, Figure S3: Differences in microbiome composition across the sample types, Figure S4: Co-occurrence analysis of 57 tumour genera, Figure S5: Microbial β-diversity analysis by NMDS on 178 tumour tissue swab, Figure S6: Microbial β-diversity analysis by NMDS performed on 127 triplets, Figure S7: Side-dependent associations between tumour histological grade and microbiota composition, Figure S8: Boxplots of distribution of clr transformed abundance of genera associated with tumour grade and/or location in 178 tumour mucosa samples in models with or without interaction at p-value < 0.05, Figure S9: Boxplots of distribution of clr transformed abundance of genera associated with tumour grade and/or location in 178 visually normal mucosa samples in models with or without interaction at p-value < 0.05, Figure S10: Boxplots of distribution of clr transformed abundance of genera associated with tumour grade and/or location in 127 stool samples in models with or without interaction at p-value < 0.05, Figure S11: Associations between tumour stage, including TNM staging separately, gender and microbiota composition in all sample types and sample sizes, Figure S12: Boxplots of distribution of clr transformed abundance of genera associated with tumour stage in 178 tumour mucosa samples, 178 adjacent visually normal mucosa samples and 127 stool samples at p-value < 0.05, Figure S13: Boxplots of distribution of clr transformed abundance of genera associated with tumour pathologic stage in 178 tumour mucosa samples, 178 adjacent visually normal mucosa samples and 127 stool samples at p-value < 0.05, Figure S14: Boxplots of distribution of clr transformed abundance of genera associated with the presence of lymph-node metastases in 178 tumour mucosa samples, 178 adjacent visually normal mucosa samples and 127 stool samples at p-value < 0.05, Figure S15: Boxplots of distribution of clr transformed abundance of genera associated with the presence of distance metastases in 178 tumour mucosa samples, 178 adjacent visually normal mucosa samples and 127 stool samples at p-value < 0.05, Figure S16: Results of pairwise coincidence analysis of genera across sample types within the same patient, Table S1: Results of validation of associations of microbiome with tumour location on the Dejea et al. dataset, Table S2: Results of validation of associations of microbiome with tumour location on the Dejea et al., Zeller et al. and Feng et al. datasets, Table S3: List of primers and the length of PCR products, Table S4: Results of the filtering steps based on ASV abundance and type of taxonomic assignment, Table S5: Table of identified ASV’s in the three sample types (127 triplets) with taxonomy assigned by BLAST and QIIME, Table S6: Number of taxa identified at respective taxonomic levels after the filtering steps in 127 triplets (381 samples) and overall (483), in different sample types and their combinations, Table S7: Results of Cochran’s Q test and McNemar’s test including the report of the results as the co-occurence of specific event pairs: genera present in one sample type but not in the second sample type and vice versa, Table S8: Total counts of genera found significantly differentially abundant across the three sample types (127 triplets), divided into categories according to their enrichment in different sample types (TtoS—tumour to stool, VNtoS—visually-normal to stool, TtoVN—tumour to visually-normal.), Table S9: Results of the Friedman test across the three sample types (127 triplets), Table S10: Results of microbial co-occurrence analysis, Table S11. Summary of the 57 tumour genera. Overview of the current knowledge about the genera that we categorise as associated with tumour mucosa, Table S12: Results of adonis testing of the associations between β-diversity and clinical variables, Table S13: Results of rank regression associating microbiome with the clinical variables, Table S14: Results of rank regression on publicly available validation datasets, Table S15: Results of rank regression associating tumour microbiome abundance with tumour microbiome subtypes, Table S16: Results of rank regression associating stool microbiome abundance with tumour microbiome subtypes, Table S17: Results of rank regression of differences between tumour microbiome subtypes in metabolic potential of the microbial communities, Text S1: Extended results of differences in microbiome diversity and incidence across the sample type, Text S2: Validation of results on publicly available data.
Author Contributions
E.B., R.Š., R.N., B.B. and L.Z.-D. designed the study; B.Z. and S.S. performed bioinformatic analysis; B.Z., V.A.P., V.P. and E.B. performed statistical data analysis; M.H., L.M., N.K. and V.B. performed the sample processing, DNA isolation and sequencing; B.Z., M.H., V.A.P., L.M., E.B., P.V., L.Z.-D., B.B. and R.H. interpreted the results; B.Z. drafted the first version of the manuscript. M.H. designed Figure 1 and Figure 4. All authors participated in writing or editing of the manuscript and approved the final manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
Authors thanks to Research Infrastructure RECETOX RI (No LM2018121) financed by the Ministry of Education, Youth and Sports, and Operational Programme Research, Development and Innovation—project CETOCOEN EXCELLENCE (No CZ.02.1.01/0.0/0.0/17_043/0009632) for supportive background. This work received funding from the Ministry of Health of the Czech Republic (project AZV 16-31966A) and the European Union’s Horizon 2020 research and innovation programme under grant agreement No 825410. This publication reflects only the author’s view and the European Commission is not responsible for any use that may be made of the information it contains. Computational resources were supplied by the project “e-Infrastruktura CZ” (e-INFRA LM2018140) provided within the program Projects of Large Research, Development, and Innovations Infrastructures. The work was supported by the project BBMRI-CZ no. LM2018125.
Institutional Review Board Statement
The study was approved by the ethical committee of Masaryk Memorial Cancer Institute. Ethical code: Č.J. 2015/1721/MOU, JID: MOU 73 866.
Informed Consent Statement
All patients gave written informed consent in accordance with the Declaration of Helsinki prior to participating in the study.
Data Availability Statement
Sequencing data were uploaded to the European Nucleotide Archive under accession number PRJEB35990.
Conflicts of Interest
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ferlay J., Colombet M., Soerjomataram I., Dyba T., Randi G., Bettio M., Gavin A., Visser O., Bray F. Cancer incidence and mortality patterns in Europe: Estimates for 40 countries and 25 major cancers in 2018. Eur. J. Cancer. 2018;103:356–387. doi: 10.1016/j.ejca.2018.07.005. [DOI] [PubMed] [Google Scholar]
- 2.Punt C.J.A., Koopman M., Vermeulen L. From tumour heterogeneity to advances in precision treatment of colorectal cancer. Nat. Rev. Clin. Oncol. 2017;14:235–246. doi: 10.1038/nrclinonc.2016.171. [DOI] [PubMed] [Google Scholar]
- 3.Van Der Jeught K., Xu H.-C., Li Y.-J., Lu X.-B., Ji G. Drug resistance and new therapies in colorectal cancer. World J. Gastroenterol. 2018;24:3834–3848. doi: 10.3748/wjg.v24.i34.3834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ahn J., Sinha R., Pei Z., Dominianni C., Wu J., Shi J., Goedert J.J., Hayes R., Yang L. Human Gut Microbiome and Risk for Colorectal Cancer. J. Natl. Cancer Inst. 2013;105:1907–1911. doi: 10.1093/jnci/djt300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arthur J., Perez-Chanona E., Mühlbauer M., Tomkovich S., Uronis J.M., Fan T.-J., Campbell B.J., Abujamel T., Dogan B., Rogers A.B., et al. Intestinal Inflammation Targets Cancer-Inducing Activity of the Microbiota. Science. 2012;338:120–123. doi: 10.1126/science.1224820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Balamurugan R., Rajendiran E., George S., Samuel G.V., Ramakrishna B. Real-time polymerase chain reaction quantification of specific butyrate-producing bacteria, DesulfovibrioandEnterococcus faecalisin the feces of patients with colorectal cancer. J. Gastroenterol. Hepatol. 2008;23:1298–1303. doi: 10.1111/j.1440-1746.2008.05490.x. [DOI] [PubMed] [Google Scholar]
- 7.Chen J., Young S.M., Allen C., Seeber A., Péli-Gulli M.-P., Panchaud N., Waller A., Ursu O., Yao T., Golden J.E., et al. Identification of a Small Molecule Yeast TORC1 Inhibitor with a Multiplex Screen Based on Flow Cytometry. ACS Chem. Biol. 2012;7:715–722. doi: 10.1021/cb200452r. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen W., Liu F., Ling Z., Tong X., Xiang C. Human Intestinal Lumen and Mucosa-Associated Microbiota in Patients with Colorectal Cancer. PLoS ONE. 2012;7:e39743. doi: 10.1371/journal.pone.0039743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cipe G., Idiz U.O., Firat D., Bektasoglu H. Relationship between intestinal microbiota and colorectal cancer. World J. Gastrointest. Oncol. 2015;7:233–240. doi: 10.4251/wjgo.v7.i10.233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kostic A., Chun E., Robertson L., Glickman J.N., Gallini C.A., Michaud M., Clancy T.E., Chung D.C., Lochhead P., Hold G., et al. Fusobacterium nucleatum Potentiates Intestinal Tumorigenesis and Modulates the Tumor-Immune Microenvironment. Cell Host Microbe. 2013;14:207–215. doi: 10.1016/j.chom.2013.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lu Y., Chen J., Zheng J., Hu G., Wang J., Huang C., Lou L., Wang X., Zeng Y. Mucosal adherent bacterial dysbiosis in patients with colorectal adenomas. Sci. Rep. 2016;6:26337. doi: 10.1038/srep26337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Marchesi J.R., Dutilh B.E., Hall N., Peters W.H.M., Roelofs R., Boleij A., Tjalsma H. Towards the Human Colorectal Cancer Microbiome. PLoS ONE. 2011;6:e20447. doi: 10.1371/journal.pone.0020447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nakatsu G., Li X., Zhou H., Sheng J., Wong S.H., Wu W.K.K., Ng S.C., Tsoi H., Dong Y., Zhang N., et al. Gut mucosal microbiome across stages of colorectal carcinogenesis. Nat. Commun. 2015;6:8727. doi: 10.1038/ncomms9727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rubinstein M.R., Wang X., Liu W., Hao Y., Cai G., Han Y.W. Fusobacterium nucleatum Promotes Colorectal Carcinogenesis by Modulating E-Cadherin/β-Catenin Signaling via its FadA Adhesin. Cell Host Microbe. 2013;14:195–206. doi: 10.1016/j.chom.2013.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sobhani I., Tap J., Roudot-Thoraval F., Roperch J.P., Letulle S., Langella P., Corthier G., Van Nhieu J.T., Furet J.-P. Microbial Dysbiosis in Colorectal Cancer (CRC) Patients. PLoS ONE. 2011;6:e16393. doi: 10.1371/journal.pone.0016393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Viljoen K.S., Dakshinamurthy A., Goldberg P., Blackburn J.M. Quantitative Profiling of Colorectal Cancer-Associated Bacteria Reveals Associations between Fusobacterium spp., Enterotoxigenic Bacteroides fragilis (ETBF) and Clinicopathological Features of Colorectal Cancer. PLoS ONE. 2015;10:e0119462. doi: 10.1371/journal.pone.0119462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang T., Cai G., Qiu Y., Fei N., Zhang M., Pang X., Jia W., Cai S., Zhao L. Structural segregation of gut microbiota between colorectal cancer patients and healthy volunteers. ISME J. 2011;6:320–329. doi: 10.1038/ismej.2011.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wu N., Yang X., Zhang R., Li J., Xiao X., Hu Y., Chen Y., Yang F., Lu N., Wang Z., et al. Dysbiosis Signature of Fecal Microbiota in Colorectal Cancer Patients. Microb. Ecol. 2013;66:462–470. doi: 10.1007/s00248-013-0245-9. [DOI] [PubMed] [Google Scholar]
- 19.Yang J., McDowell A., Kim E.K., Seo H., Lee W.H., Moon C.-M., Kym S.-M., Lee D.H., Park Y.S., Jee Y.-K., et al. Development of a colorectal cancer diagnostic model and dietary risk assessment through gut microbiome analysis. Exp. Mol. Med. 2019;51:1–15. doi: 10.1038/s12276-019-0313-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yu J., Feng Q., Wong S.H., Zhang D., Liang Q.Y., Qin Y., Tang L., Zhao H., Stenvang J., Li Y., et al. Metagenomic analysis of faecal microbiome as a tool towards targeted non-invasive biomarkers for colorectal cancer. Gut. 2017;66:70–78. doi: 10.1136/gutjnl-2015-309800. [DOI] [PubMed] [Google Scholar]
- 21.Zackular J.P., Baxter N., Iverson K.D., Sadler W.D., Petrosino J.F., Chen G.Y., Schloss P.D. The Gut Microbiome Modulates Colon Tumorigenesis. mBio. 2013;4:e00692-13. doi: 10.1128/mBio.00692-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zackular J., Rogers M., Ruffin M., Schloss P.D. The Human Gut Microbiome as a Screening Tool for Colorectal Cancer. Cancer Prev. Res. 2014;7:1112–1121. doi: 10.1158/1940-6207.CAPR-14-0129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vaupel P., Harrison L. Tumor Hypoxia: Causative Factors, Compensatory Mechanisms, and Cellular Response. Oncologist. 2004;9((Suppl. S5)):4–9. doi: 10.1634/theoncologist.9-90005-4. [DOI] [PubMed] [Google Scholar]
- 24.Louis P., Hold G., Flint H.J. The gut microbiota, bacterial metabolites and colorectal cancer. Nat. Rev. Microbiol. 2014;12:661–672. doi: 10.1038/nrmicro3344. [DOI] [PubMed] [Google Scholar]
- 25.Tlaskalova-Hogenova H., Vannucci L., Klimesova K., Stepankova R., Krizan J., Kverka M. Microbiome and Colorectal Carcinoma. Cancer J. 2014;20:217–224. doi: 10.1097/PPO.0000000000000052. [DOI] [PubMed] [Google Scholar]
- 26.Xiao Y., Freeman G.J. The Microsatellite Instable Subset of Colorectal Cancer Is a Particularly Good Candidate for Checkpoint Blockade Immunotherapy. Cancer Discov. 2015;5:16–18. doi: 10.1158/2159-8290.CD-14-1397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tjalsma H., Boleij A., Marchesi J.R., Dutilh B.E. A bacterial driver–passenger model for colorectal cancer: Beyond the usual suspects. Nat. Rev. Genet. 2012;10:575–582. doi: 10.1038/nrmicro2819. [DOI] [PubMed] [Google Scholar]
- 28.Pennisi E. Cancer Therapies Use a Little Help from Microbial Friends. Science. 2013;342:921. doi: 10.1126/science.342.6161.921. [DOI] [PubMed] [Google Scholar]
- 29.Thomas A.M., Manghi P., Asnicar F., Pasolli E., Armanini F., Zolfo M., Beghini F., Manara S., Karcher N., Pozzi C., et al. Metagenomic analysis of colorectal cancer datasets identifies cross-cohort microbial diagnostic signatures and a link with choline degradation. Nat. Med. 2019;25:667–678. doi: 10.1038/s41591-019-0405-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Feng Q., Liang S., Jia H., Stadlmayr A., Tang L., Lan Z., Zhang D., Xia H., Xu X., Jie Z., et al. Gut microbiome development along the colorectal adenoma–carcinoma sequence. Nat. Commun. 2015;6:6528. doi: 10.1038/ncomms7528. [DOI] [PubMed] [Google Scholar]
- 31.Dejea C.M., Wick E.C., Hechenbleikner E.M., White J.R., Welch J.L.M., Rossetti B.J., Peterson S.N., Snesrud E.C., Borisy G.G., Lazarev M., et al. Microbiota organization is a distinct feature of proximal colorectal cancers. Proc. Natl. Acad. Sci. USA. 2014;111:18321–18326. doi: 10.1073/pnas.1406199111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zeller G., Tap J., Voigt A.Y., Sunagawa S., Kultima J.R., Costea P.I., Amiot A., Böhm J., Brunetti F., Habermann N., et al. Potential of fecal microbiota for early-stage detection of colorectal cancer. Mol. Syst. Biol. 2014;10:766. doi: 10.15252/msb.20145645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yang Y., Cai Q., Shu X., Steinwandel M.D., Blot W.J., Zheng W., Long J. Prospective study of oral microbiome and colorectal cancer risk in low-income and African American populations. Int. J. Cancer. 2019;144:2381–2389. doi: 10.1002/ijc.31941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Liu C., Zhang Y., Shang Y., Wu B., Yang E., Luo Y.-Y., Li X. Intestinal bacteria detected in cancer and adjacent tissue from patients with colorectal cancer. Oncol. Lett. 2018;17:1115–1127. doi: 10.3892/ol.2018.9714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pu L.Z.C.T., Yamamoto K., Honda T., Nakamura M., Yamamura T., Hattori S., Burt A.D., Singh R., Hirooka Y., Fujishiro M. Microbiota profile is different for early and invasive colorectal cancer and is consistent throughout the colon. J. Gastroenterol. Hepatol. 2020;35:433–437. doi: 10.1111/jgh.14868. [DOI] [PubMed] [Google Scholar]
- 36.Flemer B., Lynch D.B., Brown J.M.R., Jeffery I., Ryan F., Claesson M., O’Riordain M., Shanahan F., O’Toole P.W. Tumour-associated and non-tumour-associated microbiota in colorectal cancer. Gut. 2017;66:633–643. doi: 10.1136/gutjnl-2015-309595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Egao Z., Eguo B., Egao R., Ezhu Q., Eqin H. Microbiota disbiosis is associated with colorectal cancer. Front. Microbiol. 2015;6:20. doi: 10.3389/fmicb.2015.00020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Li E., Hamm C.M., Gulati A.S., Sartor R.B., Chen H., Wu X., Zhang T., Rohlf F.J., Zhu W., Gu C., et al. Inflammatory Bowel Diseases Phenotype, C. difficile and NOD2 Genotype Are Associated with Shifts in Human Ileum Associated Microbial Composition. PLoS ONE. 2012;7:e26284. doi: 10.1371/journal.pone.0026284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Han S., Wu W., Da M., Xu J., Zhuang J., Zhang L., Zhang X., Yang X. Adequate Lymph Node Assessments and Investigation of Gut Microorganisms and Microbial Metabolites in Colorectal Cancer. OTT. 2020;13:1893–1906. doi: 10.2147/OTT.S242017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wu Y., Shi L., Li Q., Wu J., Peng W., Li H., Chen K., Ren Y., Fu X. Microbiota Diversity in Human Colorectal Cancer Tissues Is Associated with Clinicopathological Features. Nutr. Cancer. 2019;71:214–222. doi: 10.1080/01635581.2019.1578394. [DOI] [PubMed] [Google Scholar]
- 41.Apprill A., McNally S., Parsons R., Weber L. Minor revision to V4 region SSU rRNA 806R gene primer greatly increases detection of SAR11 bacterioplankton. Aquat. Microb. Ecol. 2015;75:129–137. doi: 10.3354/ame01753. [DOI] [Google Scholar]
- 42.Caporaso J.G., Lauber C.L., Walters W.A., Berg-Lyons D., Lozupone C.A., Turnbaugh P.J., Fierer N., Knight R. Global patterns of 16S rRNA diversity at a depth of millions of sequences per sample. Proc. Natl. Acad. Sci. USA. 2011;108:4516–4522. doi: 10.1073/pnas.1000080107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Callahan B.J., McMurdie P., Rosen M.J., Han A.W., Johnson A.J.A., Holmes S. DADA2: High-resolution sample inference from Illumina amplicon data. Nat. Methods. 2016;13:581–583. doi: 10.1038/nmeth.3869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Aronesty E. Comparison of Sequencing Utility Programs. TOBIOIJ. 2013;7:1–8. doi: 10.2174/1875036201307010001. [DOI] [Google Scholar]
- 45.Pruesse E., Quast C., Knittel K., Fuchs B.M., Ludwig W., Peplies J., Glöckner F.O. SILVA: A comprehensive online resource for quality checked and aligned ribosomal RNA sequence data compatible with ARB. Nucleic Acids Res. 2007;35:7188–7196. doi: 10.1093/nar/gkm864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Edgar R.C. Search and clustering orders of magnitude faster than BLAST. Bioinformatics. 2010;26:2460–2461. doi: 10.1093/bioinformatics/btq461. [DOI] [PubMed] [Google Scholar]
- 47.Caporaso J.G., Kuczynski J., Stombaugh J., Bittinger K., Bushman F., Costello E.K., Fierer N., Peña A.G., Goodrich J.K., Gordon J.I., et al. QIIME allows analysis of high-throughput community sequencing data. Nat. Methods. 2010;7:335–336. doi: 10.1038/nmeth.f.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Altschul S.F., Gish W., Miller W., Myers E.W., Lipman D.J. Basic local alignment search tool. J. Mol. Biol. 1990;215:403–410. doi: 10.1016/S0022-2836(05)80360-2. [DOI] [PubMed] [Google Scholar]
- 49.Lozupone C., Knight R. UniFrac: A New Phylogenetic Method for Comparing Microbial Communities. Appl. Environ. Microbiol. 2005;71:8228–8235. doi: 10.1128/AEM.71.12.8228-8235.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Douglas G.M., Maffei V.J., Zaneveld J.R., Yurgel S.N., Brown J.R., Taylor C.M., Huttenhower C., Langille M.G.I. PICRUSt2 for prediction of metagenome functions. Nat. Biotechnol. 2020;38:685–688. doi: 10.1038/s41587-020-0548-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Aitchison J. The Statistical Analysis of Compositional Data. J. R. Stat. Soc. Ser. B Methodol. 1982;44:139–160. doi: 10.1111/j.2517-6161.1982.tb01195.x. [DOI] [Google Scholar]
- 52.Gloor G.B., Wu J.R., Pawlowsky-Glahn V., Egozcue J.J. It’s all relative: Analyzing microbiome data as compositions. Ann. Epidemiol. 2016;26:322–329. doi: 10.1016/j.annepidem.2016.03.003. [DOI] [PubMed] [Google Scholar]
- 53.Martín-Fernández J.-A., Hron K., Templ M., Filzmoser P., Palarea-Albaladejo J. Bayesian-multiplicative treatment of count zeros in compositional data sets. Stat. Model. Int. J. 2015;15:134–158. doi: 10.1177/1471082X14535524. [DOI] [Google Scholar]
- 54.Tsilimigras M.C., Fodor A.A. Compositional data analysis of the microbiome: Fundamentals, tools, and challenges. Ann. Epidemiol. 2016;26:330–335. doi: 10.1016/j.annepidem.2016.03.002. [DOI] [PubMed] [Google Scholar]
- 55.Oaksen J., Blanchet F.G., Friendly M., Kindt R., Legendre P., McGlinn D., Minchin P.R., O’Hara R.B., Simpson G.L., Solymos P., et al. Vegan: Community Ecology Package. R Package. 2019. [(accessed on 4 July 2020)]. Available online: http://cran.rproject.org/package=vegan.
- 56.Comas-Cufí M. R Package. coda.base: A Basic Set of Functions for Compositional Data Analysis. 2020. [(accessed on 4 July 2020)]. Available online: https://rdrr.io/cran/coda.base/
- 57.Kloke J.D., McKean J.W. Rfit: Rank-Based Estimation for Linear Models. R J. 2012;4:57–64. doi: 10.32614/RJ-2012-014. [DOI] [Google Scholar]
- 58.Benjamini Y., Hochberg Y. Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. J. R. Stat. Soc. Ser. B Methodol. 1995;57:289–300. doi: 10.1111/j.2517-6161.1995.tb02031.x. [DOI] [Google Scholar]
- 59.Gu Z., Gu L., Eils R., Schlesner M., Brors B. circlize implements and enhances circular visualization in R. Bioinformatics. 2014;30:2811–2812. doi: 10.1093/bioinformatics/btu393. [DOI] [PubMed] [Google Scholar]
- 60.Gu Z., Eils R., Schlesner M. Complex heatmaps reveal patterns and correlations in multidimensional genomic data. Bioinformatics. 2016;32:2847–2849. doi: 10.1093/bioinformatics/btw313. [DOI] [PubMed] [Google Scholar]
- 61.Warnes G.R., Bolker B., Bonebakker L., Gentleman R., Liaw W.H.A., Lumley T., Maechler M., Magnusson A., Moeller S., Schwartz M., et al. Gplots: Various R Programming Tools for Plotting Data; R Package. 2020. [(accessed on 4 July 2020)]. Available online: https://rdrr.io/cran/gplots/
- 62.Wickham H. Ggplot2: Elegant Graphics for Data Analysis. 2nd ed. Springer; Cham, Switzerland: 2016. [Google Scholar]
- 63.Wray C.M., Ziogas A., Hinojosa M.W., Le H., Stamos M.J., Zell J.A. Tumor Subsite Location Within the Colon Is Prognostic for Survival After Colon Cancer Diagnosis. Dis. Colon Rectum. 2009;52:1359–1366. doi: 10.1007/DCR.0b013e3181a7b7de. [DOI] [PubMed] [Google Scholar]
- 64.Pasolli E., Schiffer L., Manghi P., Renson A., Obenchain V., Truong D.T., Beghini F., Malik F., Ramos M., Dowd J., et al. Accessible, curated metagenomic data through ExperimentHub. Nat. Methods. 2017;14:1023–1024. doi: 10.1038/nmeth.4468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.De Almeida C.V., Lulli M., Di Pilato V., Schiavone N., Russo E., Nannini G., Baldi S., Borrelli R., Bartolucci G., Menicatti M., et al. Differential Responses of Colorectal Cancer Cell Lines to Enterococcus faecalis’ Strains Isolated from Healthy Donors and Colorectal Cancer Patients. JCM. 2019;8:388. doi: 10.3390/jcm8030388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Gupta A., Dhakan D.B., Maji A., Saxena R., Visnu Prasoodanan P.K., Mahajan S., Pulikkan J., Kurian J., Gomez A.M., Scaria J., et al. Association of Flavonifractor plautii, a Flavonoid-Degrading Bacterium, with the Gut Microbiome of Colorectal Cancer Patients in India. mSystems. 2019;4 doi: 10.1128/mSystems.00438-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ai D., Pan H., Li X., Gao Y., Liu G., Xia L.C. Identifying Gut Microbiota Associated with Colorectal Cancer Using a Zero-Inflated Lognormal Model. Front. Microbiol. 2019;10:826. doi: 10.3389/fmicb.2019.00826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ito M., Kanno S., Nosho K., Sukawa Y., Mitsuhashi K., Kurihara H., Igarashi H., Takahashi T., Tachibana M., Takahashi H., et al. Association ofFusobacterium nucleatumwith clinical and molecular features in colorectal serrated pathway. Int. J. Cancer. 2015;137:1258–1268. doi: 10.1002/ijc.29488. [DOI] [PubMed] [Google Scholar]
- 69.Bahmani S., Azarpira N., Moazamian E. Anti-colon cancer activity of Bifidobacterium metabolites on colon cancer cell line SW742. Turk. J. Gastroenterol. 2019;30:835–842. doi: 10.5152/tjg.2019.18451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Mangifesta M., Mancabelli L., Milani C., Gaiani F., De’Angelis N., De’Angelis G.L., Van Sinderen D., Ventura M., Turroni F. Mucosal microbiota of intestinal polyps reveals putative biomarkers of colorectal cancer. Sci. Rep. 2018;8:1–9. doi: 10.1038/s41598-018-32413-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Parisa A., Roya G., Mahdi R., Shabnam R., Maryam E., Malihe T. Anti-cancer effects of Bifidobacterium species in colon cancer cells and a mouse model of carcinogenesis. PLoS ONE. 2020;15:e0232930. doi: 10.1371/journal.pone.0232930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Sivan A., Corrales L., Hubert N., Williams J.B., Aquino-Michaels K., Earley Z.M., Benyamin F.W., Lei Y.M., Jabri B., Alegre M.-L., et al. Commensal Bifidobacterium promotes antitumor immunity and facilitates anti-PD-L1 efficacy. Science. 2015;350:1084–1089. doi: 10.1126/science.aac4255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Koncina E., Haan S., Rauh S., Letellier E. Prognostic and Predictive Molecular Biomarkers for Colorectal Cancer: Updates and Challenges. Cancers. 2020;12:319. doi: 10.3390/cancers12020319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Guinney J., Dienstmann R., Wang X., De Reyniès A., Schlicker A., Soneson C., Marisa L., Roepman P., Nyamundanda G., Angelino P., et al. The consensus molecular subtypes of colorectal cancer. Nat. Med. 2015;21:1350–1356. doi: 10.1038/nm.3967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Koliarakis I., Messaritakis I., Nikolouzakis T.K., Hamilos G., Souglakos J., Tsiaoussis J. Oral Bacteria and Intestinal Dysbiosis in Colorectal Cancer. Int. J. Mol. Sci. 2019;20:4146. doi: 10.3390/ijms20174146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Long X., Wong C.C., Tong L., Chu E.S.H., Szeto C.H., Go M.Y.Y., Coker O.O., Chan A.W.H., Chan F.K., Sung J.J.Y., et al. Peptostreptococcus anaerobius promotes colorectal carcinogenesis and modulates tumour immunity. Nat. Microbiol. 2019;4:2319–2330. doi: 10.1038/s41564-019-0541-3. [DOI] [PubMed] [Google Scholar]
- 77.Abed J., Emgård J.E., Zamir G., Faroja M., Almogy G., Grenov A., Sol A., Naor R., Pikarsky E., Atlan K.A., et al. Fap2 Mediates Fusobacterium nucleatum Colorectal Adenocarcinoma Enrichment by Binding to Tumor-Expressed Gal-GalNAc. Cell Host Microbe. 2016;20:215–225. doi: 10.1016/j.chom.2016.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Zou X., Feng B., Dong T., Yan G., Tan B., Shen H., Huang A., Zhang X., Zhang M., Yang P., et al. Up-regulation of type I collagen during tumorigenesis of colorectal cancer revealed by quantitative proteomic analysis. J. Proteom. 2013;94:473–485. doi: 10.1016/j.jprot.2013.10.020. [DOI] [PubMed] [Google Scholar]
- 79.Takahashi N. Microbial ecosystem in the oral cavity: Metabolic diversity in an ecological niche and its relationship with oral diseases. Int. Congr. Ser. 2005;1284:103–112. doi: 10.1016/j.ics.2005.06.071. [DOI] [Google Scholar]
- 80.Eley B.M., Cox S.W. Proteolytic and hydrolytic enzymes from putative periodontal pathogens: Characterization, molecular genetics, effects on host defenses and tissues and detection in gingival crevice fluid. Periodontol. 2000. 2003;31:105–124. doi: 10.1034/j.1600-0757.2003.03107.x. [DOI] [PubMed] [Google Scholar]
- 81.Potempa J., Sroka A., Imamura T., Travis J. Gingipains, the major cysteine proteinases and virulence factors of Porphyromonas gingivalis: Structure, function and assembly of multidomain protein complexes. Curr. Protein Pept. Sci. 2003;4:397–407. doi: 10.2174/1389203033487036. [DOI] [PubMed] [Google Scholar]
- 82.Gonçalves L.F.H., Fermiano D., Feres M., Figueiredo L.C., Teles F.R.P., Mayer M.P.A., Faveri M. Levels ofSelenomonasspecies in generalized aggressive periodontitis. J. Periodontal Res. 2012;47:711–718. doi: 10.1111/j.1600-0765.2012.01485.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Scher J.U., Ubeda C., Equinda M., Khanin R., Buischi Y., Viale A., Lipuma L., Attur M., Pillinger M., Weissmann G., et al. Periodontal disease and the oral microbiota in new-onset rheumatoid arthritis. Arthritis Rheum. 2012;64:3083–3094. doi: 10.1002/art.34539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Herbert B.A., Novince C.M., Kirkwood K.L. Aggregatibacter actinomycetemcomitans, a potent immunoregulator of the periodontal host defense system and alveolar bone homeostasis. Mol. Oral Microbiol. 2016;31:207–227. doi: 10.1111/omi.12119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Lin W.-R., Chen Y.-S., Liu Y.-C. Cellulitis and Bacteremia Caused by Bergeyella zoohelcum. J. Formos. Med. Assoc. 2007;106:573–576. doi: 10.1016/S0929-6646(07)60008-4. [DOI] [PubMed] [Google Scholar]
- 86.Peel M.M., Hornidge K.A., Luppino M., Stacpoole A.M., Weaver R.E. Actinobacillus spp. and related bacteria in infected wounds of humans bitten by horses and sheep. J. Clin. Microbiol. 1991;29:2535–2538. doi: 10.1128/jcm.29.11.2535-2538.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Sohn K.M., Huh K., Baek J.-Y., Kim Y.-S., Kang C.-I., Peck K.R., Lee N.Y., Song J.-H., Ko K.S., Chung D.R. A new causative bacteria of infective endocarditis, Bergeyella cardium sp. nov. Diagn. Microbiol. Infect. Dis. 2015;81:213–216. doi: 10.1016/j.diagmicrobio.2014.12.001. [DOI] [PubMed] [Google Scholar]
- 88.Friis-Møller A., Christensen J.J., Fussing V., Hesselbjerg A., Christiansen J., Bruun B. Clinical Significance and Taxonomy of Actinobacillus hominis. J. Clin. Microbiol. 2001;39:930–935. doi: 10.1128/JCM.39.3.930-935.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Zha Z., Lv Y., Tang H., Li T., Miao Y., Cheng J., Wang G., Tan Y., Zhu Y., Xing X., et al. An orally administered butyrate-releasing xylan derivative reduces inflammation in dextran sulphate sodium-induced murine colitis. Int. J. Biol. Macromol. 2020;156:1217–1233. doi: 10.1016/j.ijbiomac.2019.11.159. [DOI] [PubMed] [Google Scholar]
- 90.Kelly T.N., Bazzano L.A., Ajami N.J., He H., Zhao J., Petrosino J.F., Correa A., He J. Gut Microbiome Associates with Lifetime Cardiovascular Disease Risk Profile Among Bogalusa Heart Study Participants. Circ. Res. 2016;119:956–964. doi: 10.1161/CIRCRESAHA.116.309219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Niederseer D., Bracher I., Stadlmayr A., Huber-Schönauer U., Plöderl M., Obeid S., Schmied C., Hammerl S., Stickel F., Lederer D., et al. Association between Cardiovascular Risk and Diabetes with Colorectal Neoplasia: A Site-Specific Analysis. J. Clin. Med. 2018;7:484. doi: 10.3390/jcm7120484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Mei Q.-X., Huang C.-L., Luo S.-Z., Zhang X.-M., Zeng Y., Lu Y.-Y. Characterization of the duodenal bacterial microbiota in patients with pancreatic head cancer vs. healthy controls. Pancreatology. 2018;18:438–445. doi: 10.1016/j.pan.2018.03.005. [DOI] [PubMed] [Google Scholar]
- 93.Gao R., Kong C., Huang L., Li H., Qu X., Liu Z., Lan P., Wang J., Qin H. Mucosa-associated microbiota signature in colorectal cancer. Eur. J. Clin. Microbiol. Infect. Dis. 2017;36:2073–2083. doi: 10.1007/s10096-017-3026-4. [DOI] [PubMed] [Google Scholar]
- 94.Xi Y., Yuefen P., Wei W., Quan Q., Jing Z., Jiamin X., Shuwen H. Analysis of prognosis, genome, microbiome, and microbial metabolome in different sites of colorectal cancer. J. Transl. Med. 2019;17:1–22. doi: 10.1186/s12967-019-2102-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Kamphuis J., Mercier-Bonin M., Eutamène H., Théodorou V. Mucus organisation is shaped by colonic content; a new view. Sci. Rep. 2017;7:1–13. doi: 10.1038/s41598-017-08938-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Paone P., Cani P.D. Mucus barrier, mucins and gut microbiota: The expected slimy partners? Gut. 2020;69:2232–2243. doi: 10.1136/gutjnl-2020-322260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Luu T.H., Michel C., Bard J.-M., Dravet F., Nazih H., Bobin-Dubigeon C. Intestinal Proportion ofBlautiasp. is Associated with Clinical Stage and Histoprognostic Grade in Patients with Early-Stage Breast Cancer. Nutr. Cancer. 2017;69:267–275. doi: 10.1080/01635581.2017.1263750. [DOI] [PubMed] [Google Scholar]
- 98.Wu A.H., Tseng C., Vigen C., Yu Y., Cozen W., Garcia A.A., Spicer D. Gut microbiome associations with breast cancer risk factors and tumor characteristics: A pilot study. Breast Cancer Res. Treat. 2020;182:451–463. doi: 10.1007/s10549-020-05702-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Zhuang H., Cheng L., Wang Y., Zhang Y.-K., Zhao M.-F., Liang G.-D., Zhang M.-C., Li Y.-G., Zhao J.-B., Gao Y.-N., et al. Dysbiosis of the Gut Microbiome in Lung Cancer. Front. Cell. Infect. Microbiol. 2019;9:112. doi: 10.3389/fcimb.2019.00112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Budinska E., Popovici V., Tejpar S., D’Ario G., Lapique N., Sikora K.O., Di Narzo A.F., Yan P., Hodgson J.G., Weinrich S., et al. Gene expression patterns unveil a new level of molecular heterogeneity in colorectal cancer. J. Pathol. 2013;231:63–76. doi: 10.1002/path.4212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.He Z., Gharaibeh R.Z., Newsome R.C., Pope J.L., Dougherty M., Tomkovich S., Pons B., Mirey G., Vignard J., Hendrixson D.R., et al. Campylobacter jejuni promotes colorectal tumorigenesis through the action of cytolethal distending toxin. Gut. 2019;68:289–300. doi: 10.1136/gutjnl-2018-317200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Drewes J.L., White J.R., Dejea C.M., Fathi P., Iyadorai T., Vadivelu J., Roslani A.C., Wick E.C., Mongodin E.F., Loke M.F., et al. High-resolution bacterial 16S rRNA gene profile meta-analysis and biofilm status reveal common colorectal cancer consortia. Npj Biofilms Microbiomes. 2017;3:1–12. doi: 10.1038/s41522-017-0040-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Kaplan C.W., Lux R., Haake S.K., Shi W. TheFusobacterium nucleatumouter membrane protein RadD is an arginine-inhibitable adhesin required for inter-species adherence and the structured architecture of multispecies biofilm. Mol. Microbiol. 2009;71:35–47. doi: 10.1111/j.1365-2958.2008.06503.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Tomkovich S., Dejea C.M., Winglee K., Drewes J.L., Chung L., Housseau F., Pope J.L., Gauthier J., Sun X., Mühlbauer M., et al. Human colon mucosal biofilms from healthy or colon cancer hosts are carcinogenic. J. Clin. Investig. 2019;129:1699–1712. doi: 10.1172/JCI124196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Jorth P., Turner K.H., Gumus P., Nizam N., Buduneli N., Whiteley M. Metatranscriptomics of the Human Oral Microbiome during Health and Disease. mBio. 2014;5:e01012-14. doi: 10.1128/mBio.01012-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Liu Y., Geng R., Liu L., Jin X., Yan W., Zhao F., Wang S., Guo X., Ghimire G., Wei Y. Gut Microbiota-Based Algorithms in the Prediction of Metachronous Adenoma in Colorectal Cancer Patients Following Surgery. Front. Microbiol. 2020;11:1106. doi: 10.3389/fmicb.2020.01106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Alexander J.L., Wilson I.D., Teare J., Marchesi J., Nicholson J.K., Kinross J. Gut microbiota modulation of chemotherapy efficacy and toxicity. Nat. Rev. Gastroenterol. Hepatol. 2017;14:356–365. doi: 10.1038/nrgastro.2017.20. [DOI] [PubMed] [Google Scholar]
- 108.Chew S.-S., Tan L.T.-H., Law J.W.-F., Pusparajah P., Goh B.-H., Ab Mutalib N.S., Lee L.-H. Targeting Gut Microbial Biofilms—A Key to Hinder Colon Carcinogenesis? Cancers. 2020;12:2272. doi: 10.3390/cancers12082272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Kim G.W., Kim Y.-S., Lee S.H., Park S.G., Kim D.H., Cho J.Y., Hahm K.B., Hong S.P., Yoo J.-H. Periodontitis is associated with an increased risk for proximal colorectal neoplasms. Sci. Rep. 2019;9:7528. doi: 10.1038/s41598-019-44014-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Horz H.-P., Scheer S., Huenger F., Vianna M.E., Conrads G. Selective isolation of bacterial DNA from human clinical specimens. J. Microbiol. Methods. 2008;72:98–102. doi: 10.1016/j.mimet.2007.10.007. [DOI] [PubMed] [Google Scholar]
- 111.Walker S.P., Tangney M., Claesson M. Sequence-Based Characterization of Intratumoral Bacteria—A Guide to Best Practice. Front. Oncol. 2020;10:179. doi: 10.3389/fonc.2020.00179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Heravi F.S., Zakrzewski M., Vickery K., Hu H. Host DNA depletion efficiency of microbiome DNA enrichment methods in infected tissue samples. J. Microbiol. Methods. 2020;170:105856. doi: 10.1016/j.mimet.2020.105856. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Sequencing data were uploaded to the European Nucleotide Archive under accession number PRJEB35990.