Abstract
This study primarily aimed to develop a shorter version of the self-reported adherence to patient-centered physical therapy (s-SAPCPTS) by using Rasch analysis and secondarily aimed to preliminarily investigate the relationship between the s-SAPCPTS scores and demographics (i.e., age, sex, final academic degree (non-postgraduate degrees or postgraduate degrees), and practice environment). In an online anonymous survey, 110 Japanese physical therapists completed the self-reported adherence to patient-centered physical therapy and provided data on their demographics. Through the Rasch analysis, items were excluded in a stepwise manner, until certain pre-established criteria of the unidimensionality were satisfied. Subsequently, a conversion table for the Rasch score was developed. Furthermore, multiple regression analysis was conducted by using the independent variables age, sex, and final academic degree. Using the Kruskal–Wallis test, we compared the Rasch s-SAPCPTS scores among four practice environments. Consequently, the seven-item s-SAPCPTS was developed by excluding seven items through the Rasch analysis. Postgraduate degree was a statistically significant contributing factor for Rasch s-SAPCPTS scores (p = 0.038, β = 0.20). The Kruskal–Wallis test demonstrated statistically significant differences in the Rasch s-SAPCPTS scores among the four practice environments (p = 0.006). In conclusion, the seven-item s-SAPCPTS was developed with the preliminary evidence of construct validity. It was also found that the final academic degree and practice environment could be the contributing factors of s-SAPCPTS scores.
Keywords: adherence, patient-centered approach, physical therapy, Rasch analysis, unidimensionality
1. Introduction
Person-centered approaches, where persons (patients) actively participate in their health service, increase patient satisfaction and exercise adherence [1,2,3,4]. The importance of person-centered approaches has been recognized among guideline developers [5] and included in one of six core concepts to improve a health care system [6]. However, in physical therapy practice, person-centered approaches have not always been provided, due to their preference for a biomedical approach that limits the person-centered approach [7,8,9]. One of the initial steps in the facilitation of a person-centered approach in physical therapy is to develop a simple self-reporting measure for adherence to person-centered approaches to allow us to investigate the effect of educational interventions.
In 2019, Shand, et al. [10] developed the Healthcare Providers Patient-Activation Scale (HP-PAS) to evaluate attitudes toward patient-activation; the items in the scale were generated from ecological perspectives of patient self-management proposed by Fisher et al. [11]. In the HP-PAS, 20 items relevant to person-centered approaches were selected to evaluate the importance toward the person-centered approach. Subsequently, it was found that 14 out of the 20 items in the Japanese version of the HP-PAS [12] demonstrated content validity with adequate test–retest reliability, when the response scale was changed from a five-point Likert scale for the importance to an 11-point numerical rating scale (NRS) (i.e., 0–100%) for the adherence [13]. Consequently, the 14-item questionnaire was proposed to evaluate the self-reported adherence to patient-centered physical therapy (SAPCPTS). However, evaluation of the use of the 11-point NRS is required as Simms, et al. [14] suggested that the choice of response scale was important and there was no advantage for any response scales beyond six options. Further, the construct validity of the SAPCPTS has not been examined till date. To allow therapists to calculate sum scores for comparing the magnitude of the SAPCPTS, the unidimensionality of the scale needs to be investigated. The appropriateness of the scale and the unidimensionality can be assessed by using the Rasch analysis.
Furthermore, it was considered important to investigate whether the demographics correlate with the magnitude of the SAPCPTS to consider future strategies of facilitating PCA in physical therapy. Apart from the basic demographics including age and sex, the final academic degree was suspected to be a relevant factor, as final academic degrees influence adherence to the clinical practice guideline [15]. The practice environment was also suspected as a relevant factor for the SAPCPTS, because the working environment can be a relevant factor for evidence-based practice [16,17].
The primary aim of the current study was to develop a shorter version of the SAPCPTS (s-SAPCPTS) by assessing appropriateness of the response scale and unidimensionality. The secondary aim was to investigate the relationship between s-SAPCPTS scores and demographics.
2. Materials and Methods
2.1. Design
The s-SAPCPTS was developed by reducing items that affect unidimensionality, using the Rasch analysis. Furthermore, test–retest reliability of the total score of s-SAPCPTS and its minimum detectable changes (MDCs) were calculated by using shared datasets of 53 participants from a previous study [13] who were recruited by using the same inclusion criteria as those in the current study. This study was approved by the institutional research ethics committee (Saitama Prefectural University; protocol code: #20011).
2.2. Participants
Data were collected between July and September 2020 via an anonymous online survey posted on the author’s personal webpage (https://physicaltherapytak.wixsite.com/mysite, accessed on 30 August 2021). An online link to the survey was posted on Facebook. The inclusion criteria were (1) possession of Japanese physical therapist credentials and (2) knowledge of Japanese as the native language.
2.3. Outcomes
The primary outcome was the 14-item SAPCPTS (Supplementary Materials Table S1). Respondents rated self-reporting adherence to each item in their clinical practice in percentage, using an 11-point NRS from 0% (never) to 100% (always) with 10% intervals. Higher total scores indicated greater adherence to patient-centered physical therapy.
The secondary outcomes were demographics, including age, sex, final academic degree (non-postgraduate degrees including diploma and bachelor degrees or postgraduate degrees including master’s and doctorate degrees), practice environment (hospital; clinic; long-term care health facilities, nursing home, or others; or educational institute).
2.4. Procedures
Data collection was continued until a minimum sample of 100 was obtained, which is considered acceptable to run Rasch analysis [18], adequate to construct validity in the Consensus-Based Standards for the Selection of Health Measurement Instruments [19,20], and acceptable to perform multiple regression analysis with three dependent variables (i.e., n = 15–30 per dependent variable [21]).
In the 14-item SAPCPTS, Rasch analysis was conducted by using the Andrich’s Rating Scale Model with the Winsteps version 3.93 (Winsteps.com, Beaverton, Oregon). Unidimensionality was assessed by using the criteria reported in previous studies [22,23,24,25]. Briefly, the response format was considered appropriate when (1) all response options had >10 counts, (2) average measures of person abilities increased with response options, (3) outfit mean square (MnSq) values of each response option were <2, and (4) there was no disordering step calibration [22,24]. The response options were modified when the criteria were not satisfied. Subsequently, unidimensionality was considered when all following criteria were satisfied: (1) the eigenvalue was <2 in the first contrast, and (3) infit/outfit MnSq statistics was <1.4 and standard Z-values were <2. An item with a MnSq of >1.4 and a standard Z-value of >2 indicated a construct different from other items and thus was excluded in a stepwise manner until the criteria of unidimensionality were satisfied. Consequently, the s-SAPCPTS was developed.
The response distribution of the s-SAPCPTS was also assessed by visualizing an item–person map and assessing floor and ceiling effects. A threshold of 15% was used for the assessment of floor and ceiling effects [22,23]. Furthermore, the Rasch score of 0–100 was established.
Internal consistency, test–retest reliability, multiple regression analysis, and comparison among practice environments were assessed by using SPSS version 21.0 (IBM Corp, Armonk, New York), with a statistical significance of 5%. Internal consistency was assessed with Cronbach’s α, where α > 0.7 was considered acceptable [26]. Regarding test–retest reliability, the total Rasch s-SAPCPTS scores that were extracted from the datasets of 53 participants in a previous study [13] were used to obtain intra-class correlation coefficients (ICC), where the criteria for ICC value were as follows: ≤0.40 = weak, 0.41–0.74 = moderate, and ≥0.75 = strong [26]. Subsequently, the MDC in the Rasch s-SAPCPTS scores were calculated by using the following formulas:
| (1) |
| (2) |
To investigate relationships between the demographics of age, sex, and final academic degree and the Rasch s-SAPCPTS scores, multiple regression analysis was conducted by using the enter method. For data on sex and final academic degree, a 0/1 dummy code was used. For comparing the four practice environments, the Kruskal–Wallis test was performed by using the Rasch s-SAPCPTS scores, considering the uncertainty of normal distribution in each practice environment.
3. Results
In total, 110 participants completed the survey. Demographics of all patients are summarized in Table 1. The criteria were satisfied with the 11-point NRS in the seven-item s-SAPCPTS. To satisfy the criteria of unidimensionality, seven items were excluded, and consequently, a seven-item s-SAPCPTS was developed. The items in the original English version of s-SAPCPTS, as well as its Japanese version, are presented in Supplementary Materials Table S2. In the s-SAPCPTS, the eigenvalue of the first contrast was 1.78, and 66.2% of the raw variance was explained by the measure. Table 2 presents fit statistics in the s-SAPCPTS.
Table 1.
Demographics of the participants.
| Variables | Rasch Analysis (n = 110) | Regression Modeling (n = 85) |
|---|---|---|
| Age (years), mean ± SD | 32.5 ± 7.2 | 32.7 ± 7.1 |
| Sex (no. of males to no. of females) | 85:25 | 68:17 |
| Final academic degree (n), [%] | ||
| Doctorate | 3 [2.7] | 3 [3.5] |
| Master’s | 17 [15.5] | 15 [17.6] |
| Bachelor | 53 [48.2] | 38 [44.7] |
| Diploma | 37 [33.6] | 29 [34.1] |
| Years since the acquisition of the physical therapy license (years), mean ± SD | 9.4 ± 6.0 | 9.8 ± 6.0 |
Table 2.
Fit statistics in the seven-item Self-Reported Adherence to Patient-Centered Physical Therapy Scale.
| Item No.1 | Measure | SE | Infit MnSq | Infit Zstd | Outfit MsSq | Outfit Zstd |
|---|---|---|---|---|---|---|
| Item 20 | 0.42 | 0.07 | 1.03 | 0.3 | 1.05 | 0.4 |
| Item 38 | 0.24 | 0.07 | 1.14 | 1.0 | 1.08 | 0.6 |
| Item 11 | 0.01 | 0.07 | 1.04 | 0.4 | 1.05 | 0.4 |
| Item 9 | −0.07 | 0.07 | 0.90 | −0.7 | 0.87 | −0.9 |
| Item 5 | −0.15 | 0.07 | 0.82 | −1.3 | 0.86 | −1.0 |
| Item 34 | −0.15 | 0.07 | 1.05 | 0.4 | 0.96 | −0.2 |
| Item 8 | −0.30 | 0.07 | 1.07 | 0.5 | 0.95 | −0.3 |
1 Correspond with the 40-item Healthcare Providers Patient-Activation Scale [10]. Abbreviations: SE, standard error of measurement; MnSq, mean square; Zstd, standardized Z value.
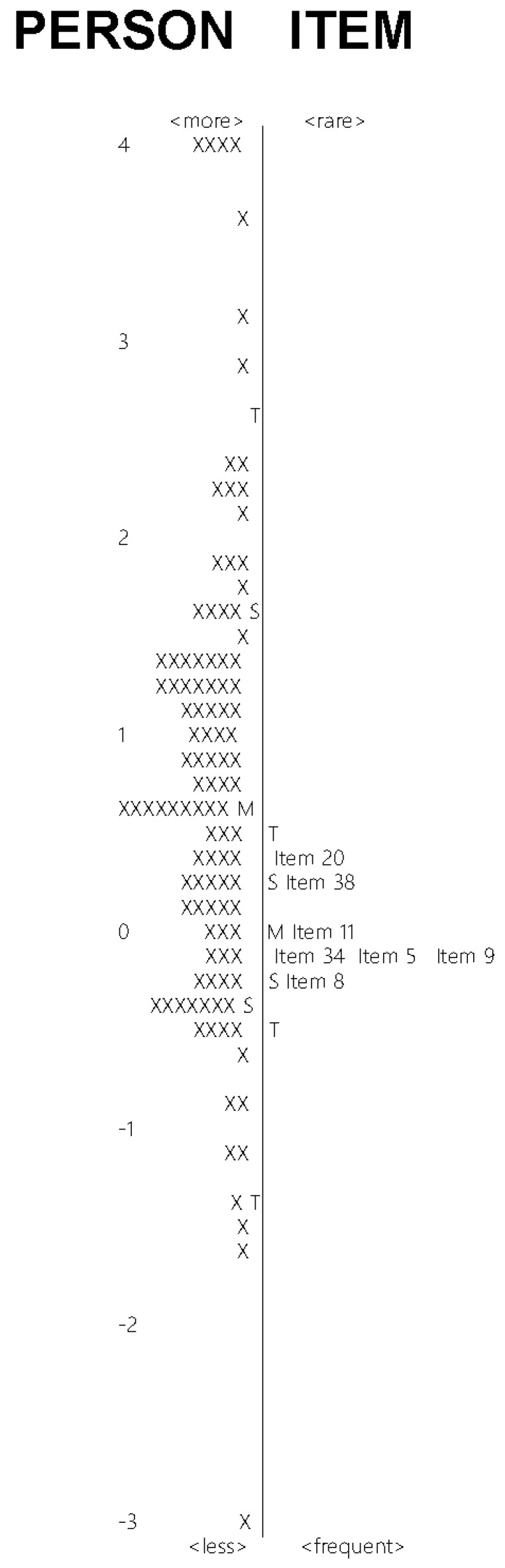
Neither ceiling (5.7%) nor flooring effects (1.4%) were observed. Figure 1 demonstrates the Rasch item–person map. The mean of person ability appeared close to the mean of item difficulty; however, the distribution of item difficulty did not cover that of person ability. The conversion from the raw total score to the 0–100 Rasch score of the s-SAPCPTS is presented in Supplementary Materials Table S3.
Figure 1.
Rasch item–person map.
The Cronbach-α was 0.93, indicating acceptable internal consistency. The ICC (95 confidence interval) of the s-SAPCPTS was 0.82 (0.71–0.89) and the MDC was 17.21.
As demonstrated by the multiple regression modeling, the final academic degree was a statistically significant contributing factor for Rasch s-SAPCPTS scores (Table 3). There were two outliers for which the predicted value of the measured value was above ±3 standard deviations.
Table 3.
Results of multiple regression modeling for the Rasch score of the seven-item Self-Reported Adherence to Patient-Centered Physical Therapy Scale.
| Model | Unstandardized Coefficients (B) (95% Confidence Intervals) | Standardized Coefficients (β) | p-Value |
|---|---|---|---|
| (Constant) | 50.63 (36.14–65.12) | <0.001 | |
| Sex 1 | −5.16 (−11.72–1.42) | −0.15 | 0.123 |
| Final academic degree 2 | 7.58 (0.43–14.74) | 0.20 | 0.038 |
| Age | 0.28 (−0.11–0.67) | 0.14 | 0.154 |
R2 = 0.09, ANOVA p = 0.017, Durbin–Watson = 1.91; 1 0 = female, and 1 = male; 2 0 = non-postgraduate degrees, including diploma and bachelor degrees, and 1 = postgraduate degrees, including master’s and doctorate degrees.
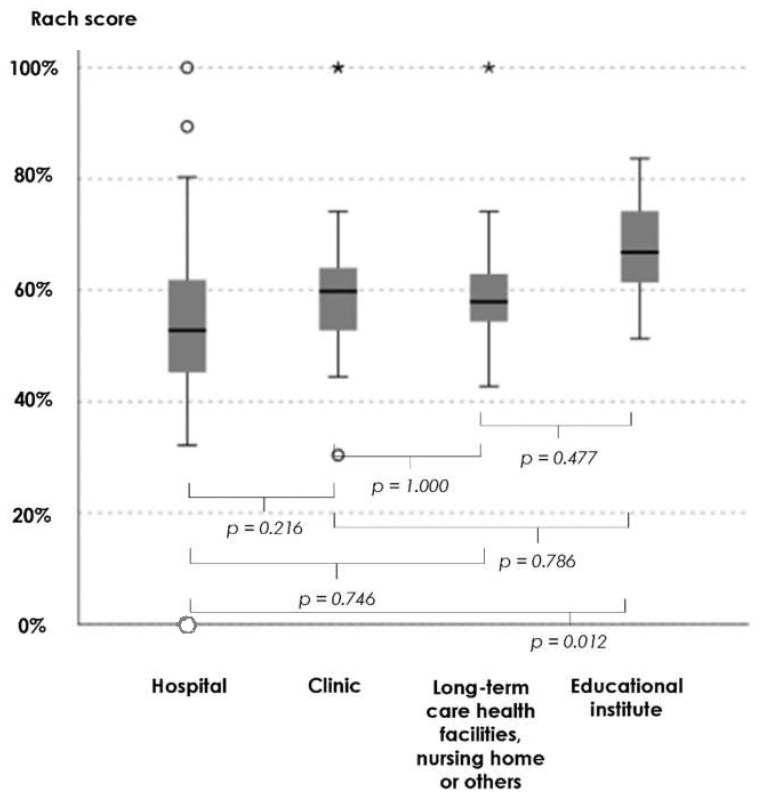
The Kruskal–Wallis test demonstrated statistically significant differences in the Rasch s-SAPCPTS scores among the four practice environments (p = 0.006). Pairwise multiple comparison test with Bonferroni correction demonstrated a statistically significant difference only between the practice environments of hospital and educational institute (p = 0.012) (Figure 2).
Figure 2.
Kruskal–Wallis test for the Rasch score of the seven-item Self-Reported Adherence to Patient-Centered Physical Therapy Scale among the four practice environments. ◯ outliers and * extreme outliers.
4. Discussion
In the current study, we developed the s-SAPCPTS for Japanese physical therapists via the confirmation of appropriateness of the 11-point NRS and unidimensionality. The s-SAPCPTS also demonstrated acceptable internal consistency, test–retest reliability, and neither ceiling nor flooring effect. The Rasch item–person map showed relatively matched mean person ability and item difficulty, and limited distribution of item difficulty. These characteristics are not surprising, because the included items were limited to only seven. Although it is optimal that the distribution of item difficulty completely covers the distribution of person ability, it would be difficult to deny the construct validity of the s-SAPCPTS by using the biased item–person map only, considering the relatively matched mean person ability and item difficulty. Thus, the current study demonstrated preliminary evidence of validity and reliability of the s-SAPCPTS and suggests clinical use of the scale in the future.
Interestingly, neither age nor sex, but instead, the final academic degree and practice environment were the contributing factors for the Rasch s-SAPCPTS score. Physical therapists in the education institute had the highest Rasch s-SAPCPTS score, which is not surprising, considering that physical therapists in the education institute often have postgraduate degrees. These findings correspond to those of a previous study conducted among Japanese physical therapists [15], in which postgraduate education in the Mechanical Diagnosis and Therapy (MDT) was a factor contributing to biopsychosocially oriented approaches. Similarly, among Japanese physical therapists, clinical experience and sex were not the contributing factors for identifying the psychological status of the patient through physical evaluation without a questionnaire [27], which was possible in therapists with the highest MDT training [28]. Thus, in Japanese physical therapists, post-graduate training is considered useful for increasing s-SAPCPTS scores, which may result in the implementation of person-centered approaches.
4.1. Research Agenda
This study found that the final academic degree was a statistically significant contributing factor for s-SAPCPTS scores, but the effect size of R2 = 0.09 can be interpreted as a none-to-very weak effect size [29]. These findings indicate that other factors that are relevant to the final academic degree may better influence the s-SAPCPTS scores, for example, pain neurophysiology knowledge [30,31] and adherence to evidence-based practice [16,32]. Further, skills for behavioral modifications, which can be enhanced in post-graduate clinical training, for example, skills to enhance patient’s attitude toward self-management [33] and communication skills to enhance patient autonomy [34], may better influence the s-SAPCPTS scores than the academic degree. Further studies are required to identify important factors to facilitate the implementation of person-centered approaches.
4.2. Limitations
A limitation of the current study is the generalizability of the scale. Educational levels influence the magnitude of the self-reported adherence of the person-centered approach; thus, s-SAPCTPRS scores of Japanese physical therapists could be different from those of physical therapists in other countries, considering differences in database use [35]. Another limitation is a potential bias in sampling. The data used in this study were not collected by all physical therapists in a certain community, such as the Japanese Physical Therapy Association; thus, there could have been self-selection bias and self-presentation bias. Furthermore, the effect size in the multiple regression analysis can be interpreted as a none-to-very weak effect size [29]. Although robust contributing factors should be determined by using a more comprehensive sampling method with a far larger sample size and other promising dependent variables, the findings in the current study will be a foundation for future studies.
5. Conclusions
In this study, the seven-item s-SAPCPTS was developed by using preliminary evidence of construct validity. It was also found that the final academic degree and practice environment could be the contributing factors of s-SAPCPTS scores. The developed s-SAPCPTS has possible applications among Japanese physical therapists in future studies.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/ijerph181910282/s1. Table S1: Descriptions of the 14-item Self-Reported Adherence to Patient-Centered Physical Therapy Scale. Table S2: Seven-item Self-Reported Adherence to Patient-Centered Physical Therapy Scale. Table S3: Conversion table from raw total scores to 0–100 Rasch scores.
Funding
The author received a research grant from the Japan Society for the Promotion of Science (JSPS) KAKENHI (Grant Number 19K19912). This study is a part of the funded research, and the article processing fee of the study was covered by the research grant.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ethics Committee of the Saitama Prefectural University (protocol code #20011 and date of approval 19 June 2020).
Informed Consent Statement
This study used an anonymous online survey, where informed consent was granted by responding to the survey.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The author declares no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kinmonth A.L., Woodcock A., Griffin S., Spiegal N., Campbell M.J. Randomised controlled trial of patient centred care of diabetes in general practice: Impact on current wellbeing and future disease risk. BMJ. 1998;317:1202–1208. doi: 10.1136/bmj.317.7167.1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kinnersley P., Stott N., Peters T., Harvey I. The patient-centredness of consultations and outcome in primary care. Br. J. Gen. Pr. 1999;49:711–716. [PMC free article] [PubMed] [Google Scholar]
- 3.Rathert C., Wyrwich M.D., Boren S.A. Patient-centered care and outcomes: A systematic review of the literature. Med. Care Res. Rev. 2013;70:351–379. doi: 10.1177/1077558712465774. [DOI] [PubMed] [Google Scholar]
- 4.McMillan S.S., Kendall E., Sav A., King M.A., Whitty J.A., Kelly F., Wheeler A.J. Patient-centered approaches to health care: A systematic review of randomized controlled trials. Med. Care Res. Rev. 2013;70:567–596. doi: 10.1177/1077558713496318. [DOI] [PubMed] [Google Scholar]
- 5.Van Dulmen S.A., Lukersmith S., Muxlow J., Santa Mina E., Nijhuis-van der Sanden M.W., van der Wees P.J., on behalf of the G-I-N Allied Health Steering Group Supporting a person-centred approach in clinical guidelines. A position paper of the Allied Health Community—Guidelines International Network (G-I-N) Health Expect. 2015;18:1543–1558. doi: 10.1111/hex.12144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Committee on Quality of Health Care in America, Institute of Medicine . Crossing the Quality Chasm: A New Health System for the 21st Century. The National Academies Press; Washington, DC, USA: 2001. [Google Scholar]
- 7.Hammond R., Stenner R., Palmer S. What matters most: A qualitative study of person-centered physiotherapy practice in community rehabilitation. Physiother. Theory Pr. 2020:1–12. doi: 10.1080/09593985.2020.1825577. [DOI] [PubMed] [Google Scholar]
- 8.Mudge S., Stretton C., Kayes N. Are physiotherapists comfortable with person-centred practice? An autoethnographic insight. Disabil. Rehabil. 2014;36:457–463. doi: 10.3109/09638288.2013.797515. [DOI] [PubMed] [Google Scholar]
- 9.Hall A.J., Burrows L., Lang I.A., Endacott R., Goodwin V.A. Are physiotherapists employing person-centred care for people with dementia? An exploratory qualitative study examining the experiences of people with dementia and their carers. BMC Geriatr. 2018;18:63. doi: 10.1186/s12877-018-0756-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shand L., Higgins R., Murphy B., Jackson A. Development and validation of the healthcare providers patient-activation scale. Patient Educ. Couns. 2019;102:1550–1557. doi: 10.1016/j.pec.2019.03.005. [DOI] [PubMed] [Google Scholar]
- 11.Fisher E.B., Brownson C.A., O’Toole M.L., Shetty G., Anwuri V.V., Glasgow R.E. Ecological Approaches to Self-Management: The Case of Diabetes. Am. J. Public Health. 2005;95:1523–1535. doi: 10.2105/AJPH.2005.066084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Miyamoto S., Takasaki H. Cross-cultural adaptation to Japanese of the Healthcare Providers Patient-Activation Scale. J. Phys. Ther. Sci. 2020;32:810–815. doi: 10.1589/jpts.32.810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Takasaki H. Content validity and reliability of the modified Japanese version of the Healthcare Providers Patient-Activation Scale: Self-reported Adherence to Patient-centered Physical Therapy Scale. Physiothe Theory Pract. doi: 10.1080/09593985.2021.1987602. In press. [DOI] [PubMed] [Google Scholar]
- 14.Simms L.J., Zelazny K., Williams T.F., Bernstein L. Does the number of response options matter? Psychometric perspectives using personality questionnaire data. Psychol. Assess. 2019;31:557–566. doi: 10.1037/pas0000648. [DOI] [PubMed] [Google Scholar]
- 15.Takasaki H., Saiki T., Iwasada Y. McKenzie Therapists Adhere More to Evidence-Based Guidelines and Have a More Biopsychosocial Perspective on the Management of Patients with Low Back Pain than General Physical Therapists in Japan. Open J. Ther. Rehabil. 2014;2:173–181. doi: 10.4236/ojtr.2014.24023. [DOI] [Google Scholar]
- 16.Fernández-Domínguez J.C., De Pedro-Gómez J.E., Morales-Asencio J.M., Bennasar-Veny M., Sastre-Fullana P., Sesé-Abad A. Health Sciences-Evidence Based Practice questionnaire (HS-EBP) for measuring transprofessional evidence-based practice: Creation, development and psychometric validation. PLoS ONE. 2017;12:e0177172. doi: 10.1371/journal.pone.0177172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fernández-Domínguez J.C., Sesé-Abad A., Morales-Asencio J.M., Sastre-Fullana P., Pol-Castañeda S., De Pedro-Gómez J.E. Content validity of a health science evidence-based practice questionnaire (HS-EBP) with a web-based modified Delphi approach. Int. J. Qual. Health Care. 2016;28:764–773. doi: 10.1093/intqhc/mzw106. [DOI] [PubMed] [Google Scholar]
- 18.Bond T.G., Fox C.M. Applying the Rasch Model.: Fundamental Measurement in the Human Sciences. 2nd ed. Lawrence Erlbaum Associates, Inc.; London, UK: 2007. [Google Scholar]
- 19.Terwee C.B., Prinsen C.A.C., Chiarotto A., Westerman M.J., Patrick D.L., Alonso J., Bouter L., De Vet H.C.W., Mokkink L.B. COSMIN methodology for evaluating the content validity of patient-reported outcome measures: A Delphi study. Qual. Life Res. 2018;27:1159–1170. doi: 10.1007/s11136-018-1829-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mokkink L.B., De Vet H.C.W., Prinsen C.A.C., Patrick D.L., Alonso J., Bouter L., Terwee C.B. COSMIN Risk of Bias checklist for systematic reviews of Patient-Reported Outcome Measures. Qual. Life Res. 2018;27:1171–1179. doi: 10.1007/s11136-017-1765-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pedhazur E.J. Multiple Regression in Behavioral Research: Explanation and Prediction. 3rd ed. Harcourt Brace College Publishers; Fort Worth, TX, USA: 1997. [Google Scholar]
- 22.Takasaki H., Chien C.-W., Johnston V., Treleaven J., Jull G. Validity and Reliability of the Perceived Deficit Questionnaire to Assess Cognitive Symptoms in People With Chronic Whiplash-Associated Disorders. Arch. Phys. Med. Rehabil. 2012;93:1774–1781. doi: 10.1016/j.apmr.2012.05.013. [DOI] [PubMed] [Google Scholar]
- 23.Takasaki H., Treleaven J. Construct validity and test-retest reliability of the Fatigue Severity Scale in people with chronic neck pain. Arch. Phys. Med. Rehabil. 2013;94:1328–1334. doi: 10.1016/j.apmr.2012.12.013. [DOI] [PubMed] [Google Scholar]
- 24.Takasaki H., Johnston V., Treleaven J., Jull G. Neck Pain Driving Index: Appropriateness of the Rating Scale and Unidimensionality of the Strategic, Tactical, and Operational Levels. Arch. Phys. Med. Rehabil. 2013;94:1842–1846. doi: 10.1016/j.apmr.2013.02.017. [DOI] [PubMed] [Google Scholar]
- 25.Takasaki H., Hall T. A Japanese version of the Patient Attitudes and Beliefs Scale for patients with musculoskeletal disorders. Physiother Theory Pr. 2020;36:1438–1446. doi: 10.1080/09593985.2019.1571143. [DOI] [PubMed] [Google Scholar]
- 26.Andresen E.M. Criteria for assessing the tools of disability outcomes research. Arch. Phys. Med. Rehabil. 2000;81:S15–S20. doi: 10.1053/apmr.2000.20619. [DOI] [PubMed] [Google Scholar]
- 27.Miki T., Kondo Y., Takebayashi T., Takasaki H. Difference between physical therapist estimation and psychological patient-reported outcome measures in patients with low back pain. PLoS ONE. 2020;15:e0227999. doi: 10.1371/journal.pone.0227999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Suzuki K., Takasaki H. Ability of Therapists Trained in Mechanical Diagnosis and Therapy to Guess Pain Catastrophizing and Kinesiophobia Scores for Patients with Low Back Pain. Open J. Ther. Rehabil. 2020;08:119–130. doi: 10.4236/ojtr.2020.84011. [DOI] [Google Scholar]
- 29.Moore D.S., Notz W., Fligner M.A. The Basic Practice of Statistics. W.H. Freeman and Company; New York, NY, USA: 2013. [Google Scholar]
- 30.Beetsma A.J., Reezigt R.R., Paap D., Reneman M.F. Assessing future health care practitioners’ knowledge and attitudes of musculoskeletal pain; development and measurement properties of a new questionnaire. Musculoskelet. Sci. Pr. 2020;50:102236. doi: 10.1016/j.msksp.2020.102236. [DOI] [PubMed] [Google Scholar]
- 31.Catley M.J., O’Connell N.E., Moseley G.L. How good is the Neurophysiology of Pain Questionnaire? A Rasch analysis of psychometric properties. J. Pain. 2013;14:818–827. doi: 10.1016/j.jpain.2013.02.008. [DOI] [PubMed] [Google Scholar]
- 32.Takasaki H., Kikkawa K., Chiba H., Handa Y., Sesé-abad A., Fernández-domínguez J.C. Cross-cultural adaptation of the Health Sciences Evidence-based Practice Questionnaire into Japanese and its test–retest reliability in undergraduate students. Prog. Rehabil. Med. 2021;6:20210034. doi: 10.2490/prm.20210034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Takasaki H. Mechanical Diagnosis and Therapy enhances attitude towards self-management in people with musculoskeletal disorders: A preliminary evidence with a before-after design. SAGE Open Med. 2017;5:2050312117740986. doi: 10.1177/2050312117740986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Murray A., Hall A., Williams G.C., McDonough S.M., Ntoumanis N., Taylor I., Jackson B., Copsey B., Hurley D.A., Matthews J. Assessing physiotherapists’ communication skills for promoting patient autonomy for self-management: Reliability and validity of the communication evaluation in rehabilitation tool. Disabil. Rehabil. 2019;41:1699–1705. doi: 10.1080/09638288.2018.1443159. [DOI] [PubMed] [Google Scholar]
- 35.Takasaki H., Elkins M.R., Moseley A.M. Use of the Physiotherapy Evidence Database (PEDro) in Japan. Phys. Ther. Res. 2016;19:58–66. doi: 10.1298/ptr.E9881. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data presented in this study are available on request from the corresponding author.