Abstract
Purpose
Femur fractures are the result of high energy injury and are associated with life-threatening complications. Therefore, we studied how body mass index (BMI) contributes to complications after femoral fractures.
Methods
Using the 2016 American College of Surgeons Trauma Quality Improvement Program (ACS TQIP) database, we stratified 41,362 patients into groups based on their BMI: Normal Weight (NW), Overweight (OW), Obese (OB), Severely Obese (SO), and Morbidly Obese (MO). We compared each BMI group to the NW cohort for differences in demographic factors, comorbidities, complications, and mechanism of injury.
Results
OB, SO, and MO patients sustained higher rates of traumatic injury from high energy mechanisms, such as motor vehicle trauma, in comparison to NW patients, who sustained more injuries from falls (p < 0.05). Correspondingly, obese patients were more likely than NW patients to sustain shaft and distal end fractures (p < 0.05). At hospital admission, obese patients presented with more comorbidities, such as bleeding disorders, congestive heart failure, diabetes mellitus, and hypertension (p < 0.05). Despite these individual findings, patients with OB, SO, and MO BMI, as opposed to NW BMI, were independently associated with a higher probability of developing at least one post-trauma complication. More specifically, MO patients were associated with a 45% higher odds of developing a complication (p < 0.05).
Conclusion
Irrespective of presenting with more comorbidities and sustaining high energy injuries, OB, SO, and MO patients were independently associated with having a higher risk of developing complications following a femoral fracture. Overall, better clinical outcomes are observed among patients with no underlying conditions and normal BMI.
Keywords: Femur fracture, Obesity, Complications, Comorbidity, Injury severity score
Introduction
The femur is the strongest and heaviest tubular bone, which is primarily responsible for weight-bearing and skeletal stability [1]. Consequently, femur fractures may cause tremendous impairment and can lead to substantial complications. Fractures of this nature have been increasingly prevalent in developed nations, with an annual incidence of 4.5 distal femur fractures per 100,000 and 129.4 proximal femur fractures per 100,000 [2].
Since the incidence of femoral fractures is increasing, it has become critical to elucidate factors that may affect the risk of sustaining these fractures and developing adverse clinical outcomes. Previous publications have reported that conditions, such as osteoporosis [3], hypertension [4], diabetes [5], and several types of cancer [6], may heighten the risk of sustaining fractures. Unhealthy body mass index (BMI) (too high or too low) has also been notably cited as a risk factor for significant morbidity after sustaining a blunt traumatic injury [7, 8]. In contrast, medical literature has also reported that obese patients, in comparison to normal-weight patients, were associated with a lower risk of sustaining a hip fracture. It has been speculated that patients with obese BMIs are protected from these fractures due to their soft-tissue padding and high bone mineral density [9]. Understanding the exact role BMI plays in sustaining a femur fracture and post-trauma morbidity and mortality is critical as obesity has become a growing epidemic within the United States. For example, it has been recently reported that 63% of Americans are overweight, and 26% are obese [10]. Since the role of BMI in traumais unclear and the incidence of femur fractures is increasing, we sought to analyze the association between unhealthy BMI and the incidence of femur fractures and post-trauma morbidity and mortality using the 2016 American College of Surgeons Trauma Quality Improvement Program (ACS TQIP) database.
Methods
After obtaining approval from our Institutional Review Board, we collated all patients who sustained a femur fracture from the 2016 American College of Surgeons Trauma Quality Improvement Program (ACS TQIP). Patients ages 16 and older were then stratified into six groups according to their body mass index (BMI): Underweight (UW, BMI 10.00–18.49 kg/m2), Normal Weight (NW, BMI 18.50–24.99 kg/m2), Overweight (OW, BMI 25.00–29.99 kg/m2), Obese (OB, BMI 30.00–34.99 kg/m2), Severely Obese (SO, BMI 35.00–39.99 kg/m2), and Morbidly Obese (MO, BMI 40.0–90.00 kg/m2). Patients who sustained a femoral head/neck, trochanteric, shaft, and distal fracture were identified by abbreviated injury score (AIS) code classifications and included in our study. Patients who sustained multiple femur fractures or had fractures of an unspecified location were excluded.
Altogether, we compared each BMI cohort to the NW BMI cohort for differences in demographic factors, mechanism of injury (MOI), rates of comorbidities, and post-trauma complications. MOIs that were analyzed were falls, firearm, motor vehicle trauma (MVT) motorcyclist, MVT occupant, MVT other/unspecified, MVT pedal cyclist, MVT pedestrian, overexertion, pedal cyclist other, and pedestrian. Using Minitab 17, univariate analysis for categorical variables was completed with Chi-square test and Fischer’s exact test, and all continuous variables were analyzed with Student’s t-test. Multivariate logistic regression models comparing each BMI cohort to the NW cohort were carried out to identify risk factors for developing at least one post-trauma complication. Complications that were included in the dependent variable of the regression were ventilator-associated pneumonia, unplanned return to the operating room, unplanned admission to intensive-care unit, unplanned intubation, superficial surgical site infection, cerebrovascular accident, severe sepsis, pulmonary embolism, osteomyelitis, organ space surgical site infection, myocardial infarction, extremity compartment syndrome, drug or alcohol withdrawal syndrome, deep vein thrombosis, deep surgical site infection, decubitus ulcer, central line-associated bloodstream infection, catheter-associated urinary tract infection, cardiac arrest with cardiopulmonary resuscitation (CPR), acute respiratory distress syndrome, acute kidney injury, and others. Of note, only significant variables from univariate analyses (p < 0.05) were included in our multivariate logistic regression analyses. However, for simplicity, we only showed data for BMI.
Results
Demographics
Overall, 41,362 patients from the 2016 ACS TQIP database were collated. Analysis of demographic factors demonstrated that UW patients were the oldest, while MO patients were the youngest (70.7 ± 18.3 years vs. 55.5 ± 18.9, Table 1). In this study population, there were more female patients, especially among the UW, NW, and MO cohorts.
Table 1.
Patient characteristics
| Factor | UW (1,545) | NW (12,030) | OW (14,046) | OB (8,044) | SO (3,169) | MO (2,528) | Total (41,362) | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % | p | % | % | p | % | p | % | p | % | p | % | |
| Age ± SD | 70.7 ± 18.3 | < 0.001 | 65.4 ± 22.1 | 63.2 ± 21.2 | < 0.001 | 60.8 ± 20.6 | < 0.001 | 57.4 ± 20.0 | < 0.001 | 55.5 ± 18.9 | < 0.001 | 62.5 ± 21.2 |
| ISS ± SD | 10.2 ± 4.3 | < 0.001 | 10.9 ± 5.3 | 11.6 ± 6.5 | < 0.001 | 12.1 ± 7.0 | < 0.001 | 12.4 ± 7.2 | < 0.001 | 12.5 ± 6.9 | < 0.001 | 11.6 ± 6.3 |
| Gender | < 0.001 | < 0.001 | < 0.001 | < 0.001 | 0.744 | |||||||
| Male | 24.3% | – | 35.7% | 50.4% | – | 48.9% | – | 45.4% | – | 36.0% | – | 43.6% |
| Female | 75.7% | – | 64.3% | 49.6% | – | 51.1% | – | 54.6% | – | 64.0% | – | 56.4% |
| Fracture type | ||||||||||||
| Head and/or neck | 39.2% | 0.024 | 36.3% | 32.2% | < 0.001 | 24.9% | < 0.001 | 17.9% | < 0.001 | 14.6% | < 0.001 | 30.1% |
| Trochanter | 45.7% | 0.001 | 41.1% | 33.4% | < 0.001 | 28.0% | < 0.001 | 24.6% | < 0.001 | 17.3% | < 0.001 | 33.4% |
| Shaft | 9.4% | < 0.001 | 14.4% | 21.6% | < 0.001 | 28.1% | < 0.001 | 29.9% | < 0.001 | 32.9% | < 0.001 | 21.6% |
| Distal End | 5.6% | < 0.001 | 8.2% | 12.8% | < 0.001 | 19.0% | < 0.001 | 27.6% | < 0.001 | 35.2% | < 0.001 | 14.9% |
Boldface font indicates statistical significance (p < 0.05)
NW cohort is the control group that each BMI cohort is compared to
SD standard deviation; ISS injury severity score; UW underweight; NW normal weight; OW overweight; OB obese; SO severely obese; MO morbidly obese
Fracture classification and mechanism of injury
General analysis of femur fracture characteristics showed that the most prevalent injury type was a trochanteric fracture, while the least common injury type was a distal end fracture (33.4% vs. 14.9%, Table 1). Upon stratification by BMI classifications, head/neck and trochanter fractures were more common among UW patients, while shaft and distal end fractures were more prevalent among obese BMI cohorts (Table 1). More specifically, the rates of head/neck and trochanter femur fractures among UW patients were 39% and 45%, respectively (Table 1). In contrast, the rates of shaft and distal end fractures among UW patients were as low as 10% and 6%, respectively (Table 1).
Additional univariate analysis demonstrated that the MOI varied across all BMI categories. In general, high energy mechanisms of energy, such as MVT, were more prevalent among obese populations, while low energy mechanisms of injury, such as falls, were more prevalent among UW and NW patients. More specifically, falls were responsible for 57% of all femur fractures among MO patients, while the incidence of falls increased to 79% in NW patients (p < 0.001, Table 2) and even 90% in UW patients (Table 2). In contrast, MVT occupant-related trauma was significantly more prevalent among obese cohorts than NW cohort. For example, the rate of MVT occupant-related trauma was as high as 27.0% for MO patients and as low as 7% among NW patients (p < 0.001, Table 2). Corresponding with our findings, the average ISS was the highest among MO patients (12.5 ± 6.9, Table 1), while it was the lowest among UW patients (10.2 ± 4.3, Table 1). Although the difference may not be clinically significant, the vast differences observed in MOI between obese and NW individuals corroborate this finding.
Table 2.
Mechanism of injury
| Factor | UW (1545) | NW (12,030) | OW (14,046) | OB (8044) | SO (3169) | MO (2528) | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| % | p | % | % | p | % | p | % | p | % | p | |
| Fall | 89.6 | < 0.001 | 79.4 | 70.5 | < 0.001 | 63.5 | < 0.001 | 58.7 | < 0.001 | 57.0 | < 0.001 |
| Firearm | 1.0 | 0.001 | 2.3 | 3.4 | < 0.001 | 4.4 | < 0.001 | 4.8 | < 0.001 | 2.6 | 0.362 |
| MVT motorcyclist | 0.8 | 0.002 | 2.0 | 4.2 | < 0.001 | 4.9 | < 0.001 | 5.9 | < 0.001 | 3.5 | < 0.001 |
| MVT occupant | 2.8 | < 0.001 | 6.6 | 10.8 | < 0.001 | 16.4 | < 0.001 | 21.0 | < 0.001 | 27.0 | < 0.001 |
| MVT pedal cyclist | 0.2 | 0.863 | 0.2 | 0.1 | 0.067 | 0.1 | 0.058 | 0.0 | 0.105 | 0.0 | 0.07 |
| MVT pedestrian | 1.0 | 0.016 | 1.8 | 2.2 | 0.022 | 2.3 | 0.018 | 1.9 | 0.877 | 2.0 | 0.5 |
| Pedal cyclist, other | 0.5 | 0.003 | 1.4 | 1.1 | 0.074 | 0.6 | < 0.001 | 0.3 | < 0.001 | 0.3 | < 0.001 |
Boldface font indicates statistical significance (p < 0.05)
NW cohort is the control group that each BMI cohort is compared to
MVT motor vehicle trauma; UW underweight; NW normal weight; OW overweight; OB obese; SO severely obese; MO morbidly obese
Comorbidities and complications
Analysis of comorbidities demonstrated that despite being younger than NW patients, obese individuals were associated with higher rates of comorbidities (Table 3). For example, OB, MO, and SO patients presented with significantly more pre-existing comorbidities, such as diabetes mellitus, chronic renal failure, hypertension, and congestive heart failure (Table 3). Additionally, UW patients presented with significantly more pre-existing comorbidities than NW patients (Table 3). Examples of comorbidities that were more prevalent among UW patients are COPD, disseminated cancer, congestive heart failure, and drug use disorder (Table 3).
Table 3.
Comorbidities
| Comorbidities | UW (1545) | NW (12,030) | OW (14,046) | OB (8044) | SO (3169) | MO (2528) | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| % | p | % | % | p | % | p | % | p | % | p | |
| Alcohol use disorder | 5.6 | 0.931 | 5.6 | 4.3 | < 0.001 | 3.3 | < 0.001 | 3.6 | < 0.001 | 2.8 | < 0.001 |
| Bleeding disorder | 10.4 | 0.909 | 10.5 | 12.6 | < 0.001 | 12.7 | < 0.001 | 12.0 | 0.02 | 11.9 | 0.04 |
| Congestive heart failure | 7.5 | 0.02 | 6.0 | 6.4 | 0.206 | 7.2 | < 0.001 | 8.1 | < 0.001 | 9.3 | < 0.001 |
| Current smoker | 21.2 | 0.024 | 18.8 | 15.1 | < 0.001 | 15.5 | < 0.001 | 15.1 | < 0.001 | 15.5 | < 0.001 |
| Chronic renal failure | 2.3 | 0.467 | 2.6 | 3.4 | 0.001 | 3.5 | 0.001 | 4.2 | < 0.001 | 3.9 | 0.001 |
| Stroke/CVA | 3.9 | 0.389 | 4.4 | 4.3 | 0.982 | 4.0 | 0.177 | 3.7 | 0.098 | 3.6 | 0.07 |
| Diabetes mellitus | 9.0 | 0.002 | 11.6 | 20.5 | < 0.001 | 26.1 | < 0.001 | 31.5 | < 0.001 | 36.6 | < 0.001 |
| Disseminated cancer | 1.9 | 0.001 | 1.0 | 1.0 | 0.721 | 0.6 | 0.004 | 0.6 | 0.036 | 0.6 | 0.083 |
| Hypertension | 48.9 | 0.889 | 48.7 | 50.6 | 0.002 | 52.5 | < 0.001 | 52.3 | < 0.001 | 54.8 | < 0.001 |
| COPD | 21.6 | < 0.001 | 12.6 | 9.2 | < 0.001 | 10.5 | < 0.001 | 11.1 | 0.024 | 14.0 | 0.066 |
| Dementia | 19.4 | 0.001 | 16.0 | 9.8 | < 0.001 | 6.3 | < 0.001 | 4.2 | < 0.001 | 2.8 | < 0.001 |
| Major psychiatric illness | 15.0 | 0.046 | 13.1 | 11.7 | < 0.001 | 12.3 | 0.092 | 13.6 | 0.447 | 15.6 | 0.001 |
| Drug use disorder | 2.5 | 0.008 | 3.8 | 3.8 | 0.871 | 4.0 | 0.548 | 4.4 | 0.151 | 3.5 | 0.503 |
| ADD/ADHD | 0.6 | 0.443 | 0.5 | 0.4 | 0.193 | 0.5 | 0.728 | 0.5 | < 0.001 | 0.5 | 0.92 |
Boldface font indicates statistical significance (p < 0.05)
NW cohort is the control group that each BMI cohort is compared to
CVA cerebrovascular accident; COPD chronic obstructive pulmonary disorder; ADD attention deficit disorder; ADHD attention deficit hyperactivity disorder; UW underweight; NW normal weight; OW overweight; OB obese; SO severely obese; MO morbidly obese
After trauma, OB, SO, and MO patients developed significantly more complications, such as acute kidney injury (AKI), acute respiratory distress syndrome (ARDS), deep surgical site infection (SSI), deep vein thrombosis (DVT), and pulmonary embolism (PE) (p < 0.05, Table 4 and Fig. 1). The rate of developing at least one post-trauma complication was the highest among MO patients, and it was significantly higher than that of NW patients (20.2% vs. 14.5%, p < 0.001, Table 4). In contrast, there was no difference noted between UW and NW patients for developing at least one post-trauma complication (Table 4). Although, individual complications, such as myocardial infarction, unplanned admission to the ICU, and ventilator-associated pneumonia, were significantly more prevalent among NW patients. Interestingly, UW patients had an admission rate of 1.1% to the ICU, while this was 1.9% for NW patients (1.1% vs. 1.9%, p = 0.02, Table 4).
Table 4.
Patient complications
| Complications | UW (1545) | NW (12,030) | OW (14,046) | OB (8044) | SO (3169) | MO (2528) | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| % | p | % | % | p | % | p | % | p | % | p | |
| Acute kidney injury | 0.3 | 0.123 | 0.6 | 1.0 | 0.001 | 1.5 | < 0.001 | 1.4 | < 0.001 | 2.2 | < 0.001 |
| ARDS | 0.0 | 0.074 | 0.3 | 0.4 | 0.021 | 0.6 | < 0.001 | 0.7 | < 0.001 | 1.0 | < 0.001 |
| CAUTI | 0.3 | 0.722 | 0.4 | 0.4 | 0.632 | 0.5 | 0.142 | 0.7 | 0.019 | 0.8 | 0.002 |
| Deep SSI | 0.0 | 0.724 | 0.1 | 0.2 | 0.003 | 0.4 | < 0.001 | 0.4 | < 0.001 | 0.7 | < 0.001 |
| Deep vein thrombosis | 0.3 | 0.076 | 0.6 | 1.1 | < 0.001 | 1.4 | < 0.001 | 1.6 | < 0.001 | 2.3 | < 0.001 |
| Pulmonary embolism | 0.1 | 0.107 | 0.4 | 0.8 | < 0.001 | 1.0 | < 0.001 | 1.7 | < 0.001 | 1.5 | < 0.001 |
| Unplanned admission to the ICU | 1.0 | 0.015 | 1.9 | 2.0 | 0.757 | 2.3 | 0.044 | 3.0 | < 0.001 | 4.2 | < 0.001 |
| Unplanned return to the OR | 0.1 | 0.429 | 0.3 | 0.4 | 0.032 | 0.6 | < 0.001 | 0.9 | < 0.001 | 1.0 | < 0.001 |
| Cardiac arrest | 0.3 | 0.209 | 0.6 | 0.8 | 0.048 | 1.0 | 0.001 | 1.3 | < 0.001 | 1.6 | < 0.001 |
| Decubitus ulcer | 0.3 | 0.195 | 0.5 | 0.5 | 0.996 | 0.7 | 0.089 | 0.8 | 0.032 | 1.5 | < 0.001 |
| Drug/alcohol withdrawal syndrome | 0.7 | 0.68 | 0.6 | 0.4 | 0.006 | 0.4 | 0.011 | 0.3 | 0.022 | 0.2 | 0.018 |
| Extremity compartment syndrome | 0.0 | 0 | 0.1 | 0.1 | 0.085 | 0.2 | < 0.001 | 0.3 | < 0.001 | 0.1 | 0.386 |
| Myocardial infarction | 0.0 | 0.005 | 0.5 | 0.5 | 0.738 | 0.4 | 0.149 | 0.7 | 0.26 | 0.5 | 0.92 |
| Organ space SSI | 0.0 | 0 | 0.0 | 0.1 | 0.434 | 0.2 | 0.005 | 0.2 | 0.006 | 0.1 | 0.133 |
| Severe sepsis | 0.2 | 0.34 | 0.3 | 0.4 | 0.393 | 0.4 | 0.286 | 0.8 | 0.001 | 0.8 | 0.001 |
| Stroke/CVA | 0.2 | 0.262 | 0.4 | 0.4 | 0.82 | 0.5 | 0.092 | 0.5 | 0.428 | 0.4 | 0.873 |
| Superficial SSI | 0.0 | 0.139 | 0.1 | 0.2 | 0.211 | 0.3 | 0.056 | 0.3 | 0.016 | 0.5 | 0.001 |
| Unplanned intubation | 0.0 | < 0.001 | 1.0 | 1.0 | 0.873 | 1.2 | 0.146 | 1.3 | 0.067 | 1.7 | 0.001 |
| Ventilator associated pneumonia | 0.0 | 0.049 | 0.2 | 0.3 | 0.823 | 0.5 | 0.001 | 0.8 | < 0.001 | 0.6 | 0.002 |
| At least one complication | 14.4 | 0.989 | 14.4 | 15.5 | 0.013 | 17.6 | < 0.001 | 20.0 | < 0.001 | 21.2 | < 0.001 |
Boldface font indicates statistical significance (p < 0.05)
NW cohort is the control group that each BMI cohort is compared to
ARDS acute respiratory distress syndrome; CAUTI catheter-associated urinary tract infection; SSI surgical site infection; ICU intensive-care unit; OR operating room; CLASBI central line-associated bloodstream infection; CVA cerebrovascular accident; UW underweight; NW normal weight; OW overweight; OB obese; SO severely obese; MO morbidly obese
Fig. 1.
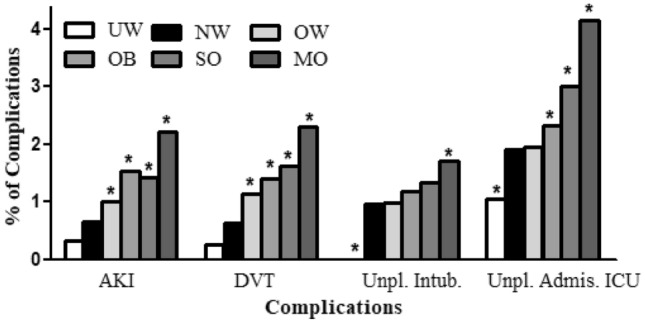
.A This figure compares the rate of complications for each BMI group to the normal weight BMI group. B (*) denotes statistical significance (p < 0.05). C Analyzed complications: acute kidney injury (AKI); deep vein thrombosis (DVT); unplanned intubation (Unpl. Intub.); unplanned admission to intensive care unit (Unpl. Admis. To ICU)
Multivariate logistic regression of independent factors associated with developing at least one complication demonstrated that, OB, SO, and MO BMI, as opposed to NW BMI, were associated with a higher risk for developing at least one complication. More specifically, MO patients were associated with about a 45.0% higher probability of developing a complication (p < 0.001, Table 5). Additionally, male gender, advanced age and ISS, and various comorbidities were risk factors for developing a complication (p < 0.05, data not shown).
Table 5.
Multivariate logistic regressions for developing at least one complication
| BMI | OR (CI) | p |
|---|---|---|
| Underweight (UW) | 0.983 (0.828, 1.168) | 0.849 |
| Overweight (OW) | 1.024 (0.947, 1.107) | 0.55 |
| Obese (OB) | 1.136 (1.039, 1.242) | 0.005 |
| Severely obese (SO) | 1.372 (1.221, 1.541) | < 0.001 |
| Morbidly obese (MO) | 1.439 (1.263, 1.639) | < 0.001 |
Six regression analyses are shown, each comparing a BMI subgroup to the NW group
Complication count: UW (233), NW (1,738), OW (2,184), OB (1,414), SO (635), and MO (536)
Boldface font indicates statistical significance (p < 0.05)
BMI body mass index; OR odds ratio; CI confidence interval
Discussion
Among all femur fracture types, patients with OB, SO, and MO BMI were associated with a higher risk of developing complications in comparison to NW patients. A previous study examining acetabular fractures reported similar observations as patients with higher than NW BMI were more susceptible to developing complications, such as DVT and wound infection [11]. This association was also prevalent among patients with pelvic ring-related injuries [12, 13]. In contrast, it was unexpected that patients with UW BMI were associated with similar and even lower rates of complications than patients with NW BMI. Previous publications have noted that there is a positive association between osteoporosis among UW populations and proximal femur fractures [14], which we even found was more common among this population. Since the UW cohort had higher rates of osteoporosis and was older and frailer than the NW cohort, we expected to observe higher rates of fractures and complications among UW patients. However, our unexpected finding can be attributed to the fact that UW patients had low rates of high energy trauma accidents. Obese patients, on the other hand, were younger, engaged in more high-energy activities, and sustained more shaft fractures. This likely contributed to their high rate of post-trauma complications.
In corroboration with our finding that OB, SO, and MO BMI, as opposed to NW BMI, are risk factors for developing at least one complication, literature suggests that high BMI is a risk factor for several negative health outcomes following injury [15–17]. Pierpont et al. reported that high adiposity, which is associated with high BMI, may lead to diminished capillary density and widespread vascular insufficiencies. These health states have also been associated with more inflammation and micro- and macronutrient deficiencies, which can worsen health and negatively affect wound healing [18].
Moreover, MO, SO, and OB patients had higher ISS than NW patients, which is in line with the finding that these patients also sustained injuries from high energy trauma accidents. For example, the rate of MVTs increased with BMI in our univariate analysis. These findings may contribute to why obese patients sustained more shaft and distal femur fractures. The shaft and distal femur, along with the knee, especially during motor vehicle trauma, may absorb most of the force from the impact of the dashboard [19]. Since patients with higher BMI were associated more high energy traumas, distal and femur fractures, and high ISS, it is comprehensable that these patients developed more complications as a result.
Additionally, male gender, advanced age and ISS, and comorbidities, like congestive heart failure, hypertension, or diabetes mellitus, were also independent risk factors for developing at least one complication. Diabetes mellitus, according to a retrospective review, was associated with a threefold higher rate of complications after ankle fracture surgery [20]. Murray et al. reported that diabetes mellitus may prolong bone healing, decrease metabolism, induce infection, and even decrease cell proliferation [21]. Furthermore, comorbidities in general are associated with being more common among populations with high BMI [22], which partially explains why we observed trends in which complications rates increased as BMI increased in our univariate analysis. Generally, having more comorbidities are indicative of worse overall health status as they may increase one’s susceptibility to post-trauma complications [23].
Interestingly, OB, SO, and MO higher rates of shaft and distal end fractures. UW on the other hand, sustained more head/neck and trochanter fractures. Previous studies reported that having a high BMI may be advantageous as there is more soft-tissue padding to protect against injury [9]. It is plausible that patients with high BMI were protected from sustaining head/neck and trochanter fractures due to having more subcutaneous tissue that can absorb more force, especially during motor vehicle accidents. Femoral shaft and distal fractures on the other hand, are one of the most common and severe fracture types [24]. These fractures are likely sustained from high energy mechanisms of injury [24], which may pre-dispose patients to developing more complications. Since patients with higher than NW BMI were associated with sustaining more shaft and distal end fractures from high energy traumas, these factors likely contributed to their high complication rate.
This study does have some limitations. Since the design is retrospective, our data analysis was dependent on strict data points collected a national database. As a result, any missing or negative values had to be excluded from our multivariate logistic regression.
Conclusion
Irrespective of presenting with more comorbidities and sustaining high energy injuries, OB, SO, and MO patients, as opposed to NW patients, were associated with having a higher risk of developing complications following a femoral fracture. Overall, better clinical outcomes are observed among patients with no underlying conditions and NW BMI.
Funding
This research did not receive funding.
Data availability
The data were from the ACS TQIP database.
Declarations
Conflict of interest
The authors of this study have no conflicts of interest.
Ethical approval
We received approval from our Institutional Review Board.
References
- 1.Chang A, Breeland G, Hubbard J. Anatomy, bony pelvis and lower limb. femur. Treasure Island: StatPearls; 2020. [PubMed] [Google Scholar]
- 2.Court-Brown CM, Caesar B. Epidemiology of adult fractures: a review. Injury. 2006;37(8):691–697. doi: 10.1016/j.injury.2006.04.130. [DOI] [PubMed] [Google Scholar]
- 3.Lane NE. Epidemiology, etiology, and diagnosis of osteoporosis. Am J Obstet Gynecol. 2006;194(2 Suppl):S3–11. doi: 10.1016/j.ajog.2005.08.047. [DOI] [PubMed] [Google Scholar]
- 4.Vestergaard P, Rejnmark L, Mosekilde L. Hypertension is a risk factor for fractures. Calcif Tissue Int. 2009;84(2):103–111. doi: 10.1007/s00223-008-9198-2. [DOI] [PubMed] [Google Scholar]
- 5.Vestergaard P, Rejnmark L, Mosekilde L. Relative fracture risk in patients with diabetes mellitus, and the impact of insulin and oral antidiabetic medication on relative fracture risk. Diabetologia. 2005;48(7):1292–1299. doi: 10.1007/s00125-005-1786-3. [DOI] [PubMed] [Google Scholar]
- 6.Body JJ. Increased fracture rate in women with breast cancer: a review of the hidden risk. BMC Cancer. 2011;11:384. doi: 10.1186/1471-2407-11-384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dhungel V, Liao J, Raut H, Lilienthal MA, Garcia LJ, Born J, et al. Obesity delays functional recovery in trauma patients. J Surg Res. 2015;193(1):415–420. doi: 10.1016/j.jss.2014.07.027. [DOI] [PubMed] [Google Scholar]
- 8.Newell MA, Bard MR, Goettler CE, Toschlog EA, Schenarts PJ, Sagraves SG, et al. Body mass index and outcomes in critically injured blunt trauma patients: weighing the impact. J Am Coll Surg. 2007;204(5):1056–1061. doi: 10.1016/j.jamcollsurg.2006.12.042. [DOI] [PubMed] [Google Scholar]
- 9.Tang X, Liu G, Kang J, Hou Y, Jiang F, Yuan W, et al. Obesity and risk of hip fracture in adults: a meta-analysis of prospective cohort studies. PLoS ONE. 2013;8(4):e55077. doi: 10.1371/journal.pone.0055077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weir C, Jan A. BMI classification percentile and cut off points. Treasure Island: StatPearls; 2020. [PubMed] [Google Scholar]
- 11.Karunakar MA, Shah SN, Jerabek S. Body mass index as a predictor of complications after operative treatment of acetabular fractures. J Bone Jt Surg Am. 2005;87(7):1498–1502. doi: 10.2106/JBJS.D.02258. [DOI] [PubMed] [Google Scholar]
- 12.Morris BJ, Richards JE, Guillamondegui OD, Sweeney KR, Mir HR, Obremskey WT, et al. Obesity increases early complications after high-energy pelvic and acetabular fractures. Orthopedics. 2015;38(10):e881–e887. doi: 10.3928/01477447-20151002-54. [DOI] [PubMed] [Google Scholar]
- 13.Sems SA, Johnson M, Cole PA, Byrd CT, Templeman DC, Group MOT Elevated body mass index increases early complications of surgical treatment of pelvic ring injuries. J Orthop Trauma. 2010;24(5):309–314. doi: 10.1097/BOT.0b013e3181caa21e. [DOI] [PubMed] [Google Scholar]
- 14.Court-Brown CM, Duckworth AD, Ralston S, McQueen MM. The relationship between obesity and fractures. Injury. 2019;50(8):1423–1428. doi: 10.1016/j.injury.2019.06.016. [DOI] [PubMed] [Google Scholar]
- 15.Bryant MK, Parrish M, Roy S, Udekwu P, Farrell M, Schinco M, et al. Inferior clinical outcomes after femur fracture in the obese are potentially preventable. Injury. 2019;50(11):2049–2054. doi: 10.1016/j.injury.2019.08.026. [DOI] [PubMed] [Google Scholar]
- 16.Kempegowda H, Richard R, Borade A, Tawari A, Graham J, Suk M, et al. Obesity is associated with high perioperative complications among surgically treated intertrochanteric fracture of the femur. J Orthop Trauma. 2017;31(7):352–357. doi: 10.1097/BOT.0000000000000825. [DOI] [PubMed] [Google Scholar]
- 17.Weinlein JC, Deaderick S, Murphy RF. Morbid obesity increases the risk for systemic complications in patients with femoral shaft fractures. J Orthop Trauma. 2015;29(3):e91–e95. doi: 10.1097/BOT.0000000000000167. [DOI] [PubMed] [Google Scholar]
- 18.Pierpont YN, Dinh TP, Salas RE, Johnson EL, Wright TG, Robson MC, et al. Obesity and surgical wound healing: a current review. ISRN Obes. 2014;2014:638936. doi: 10.1155/2014/638936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fadl SA, Sandstrom CK. Pattern recognition: a mechanism-based approach to injury detection after motor vehicle collisions. Radiographics. 2019;39(3):857–876. doi: 10.1148/rg.2019180063. [DOI] [PubMed] [Google Scholar]
- 20.Blotter RH, Connolly E, Wasan A, Chapman MW. Acute complications in the operative treatment of isolated ankle fractures in patients with diabetes mellitus. Foot Ankle Int. 1999;20(11):687–694. doi: 10.1177/107110079902001103. [DOI] [PubMed] [Google Scholar]
- 21.Murray CE, Coleman CM. Impact of diabetes mellitus on bone health. Int J Mol Sci. 2019;20(19):4873. doi: 10.3390/ijms20194873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pantalone KM, Hobbs TM, Chagin KM, Kong SX, Wells BJ, Kattan MW, et al. Prevalence and recognition of obesity and its associated comorbidities: cross-sectional analysis of electronic health record data from a large US integrated health system. BMJ Open. 2017;7(11):e017583. doi: 10.1136/bmjopen-2017-017583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kirshenbom D, Ben-Zaken Z, Albilya N, Niyibizi E, Bala M. Older age, comorbid illnesses, and injury severity affect immediate outcome in elderly trauma patients. J Emerg Trauma Shock. 2017;10(3):146–150. doi: 10.4103/JETS.JETS_62_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Denisiuk M, Afsari A. Femoral shaft fractures. Treasure Island: StatPearls; 2020. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data were from the ACS TQIP database.


