Abstract
Background:
Multiple techniques are commonly used for posterior cruciate ligament (PCL) reconstruction. However, the optimum method regarding the fixation of PCL reconstruction after PCL tears remains debatable. The purpose of this study was to compare the biomechanical properties among three different tibial fixation procedures for transtibial single-bundle PCL reconstruction.
Methods:
Thirty-six porcine tibias and porcine extensor tendons were randomized into three fixation study groups: the interference screw fixation (IS) group, the transtibial tubercle fixation (TTF) group, and TTF + IS group (n = 12 in each group). The structural properties of the three fixation groups were tested under cyclic loading and load-to-failure. The slippage after the cyclic loading test and the stiffness and ultimate failure load after load-to-failure testing were recorded.
Results:
After 1000 cycles of cyclic testing, no significant difference was observed in graft slippage among the three groups. For load-to-failure testing, the TTF + IS group showed a higher ultimate failure load than the TTF group and the IS group (876.34 ± 58.78 N vs. 660.92 ± 77.74 N [P < 0.001] vs. 556.49 ± 65.33 N [P < 0.001]). The stiffness in the TTF group was significantly lower than that in the IS group and the TTF + IS group (92.77 ± 20.16 N/mm in the TTF group vs. 120.27 ± 15.66 N/m in the IS group [P = 0.001] and 131.79 ± 17.95 N/mm in the TTF + IS group [P < 0.001]). No significant difference in the mean stiffness was found between the IS group and the TTF + IS group (P = 0.127).
Conclusions:
In this biomechanical study, supplementary fixation with transtibial tubercle sutures increased the ultimate failure load during load-to-failure testing for PCL reconstruction.
Keywords: Posterior cruciate ligament, Transtibial technique, Biomechanics, Interference screw, High-strength sutures
Introduction
Compared with the treatments used for anterior cruciate ligament (ACL) reconstruction, the optimal treatment for posterior cruciate ligament (PCL) tears has been debated because many patients develop residual posterior laxity following PCL reconstruction.[1–13] Recent studies have evaluated several PCL reconstruction techniques, including the transtibial technique or inlay technique, femoral and tibial tunnel placement, femoral and/or tibial fixation, etc.[6–9,14–17] However, the gold standard technique for PCL reconstruction has not been established.
Tibial side fixation has been the recent treatment of interest for PCL reconstruction. Numerous types of tibial fixation have been introduced for PCL reconstruction using hamstring autografts during the transtibial technique, such as interference screws, cross-pins, screws, spiked washers, and endobuttons.[6–8,11,14,18–20] The transtibial technique with a hamstring autograft is one of the most frequently employed techniques in clinical practice. However, four-stranded hamstring autografts fixed with interference screws with the transtibial technique may have short decreased pullout strength, which might lead to decreased overall graft stiffness and increased total graft deformation. Therefore, we proposed a new surgical technique for PCL reconstruction with tibial transtibial tubercle fixation (TTF) using several high-strength sutures that are not restricted by the graft length and increase the biomechanical properties of the reconstructed graft. To our knowledge, no study has compared tibial graft fixation in the transtibial technique for PCL reconstruction with TTF using several high-strength sutures with interference screws at the tibial side fixation.
The purpose of this study was to compare the biomechanical properties among three different procedures at the tibial site in terms of their ability in transtibial PCL reconstruction: the use of interference screw fixation (IS) alone, the TTF alone, and the new TTF + IS technique. The primary hypothesis is that supplementary fixation with transosseous high-strength sutures will improve the initial IS strength and stiffness under cyclic loading and load-to-failure testing. The secondary hypothesis is that the initial new TTF technique will be comparable with that achieved with IS.
Methods
Graft preparation and tunnel preparation
This study was approved by the Ethics Committee of First Affiliated Hospital of China Medical University. The availability of young cadaver knees is limited for biomechanical testing. Porcine tibias, which were used in this study, have been reported to have biomechanical properties similar to those of young human bone.[21] A randomized controlled experimental study in a porcine model was performed using 36 fresh-frozen porcine tibias and 24 porcine digital extensor tendons from healthy male pigs aged 12 to 16 months and weighing 90 kg. The bone mineral density (BMD) of the porcine tibias was assessed using dual-energy X-ray absorptiometry (Hologic QDR Whole-Body X-ray Bone Densitometer; Hologic, Bedford, MA, USA). BMD in IS group was 24.21 ± 0.85 kg/m2, in TTF group was 24.05 ± 0.62 kg/m2, and in TTF + IS group was 24.29 ± 0.53 kg/m2. Both the tibias and tendons were stored at −80°C. Before testing, all specimens were thawed at room temperature for 12 h. All of the specimens underwent one freeze-thaw cycle before biomechanical testing. The preparation procedures for the graft and tibial tunnel were similar for the three groups. The specimens were blocked and randomly divided into three groups: IS alone, TTF alone, and TTF + IS (n = 12 in each group) [Figure 1].
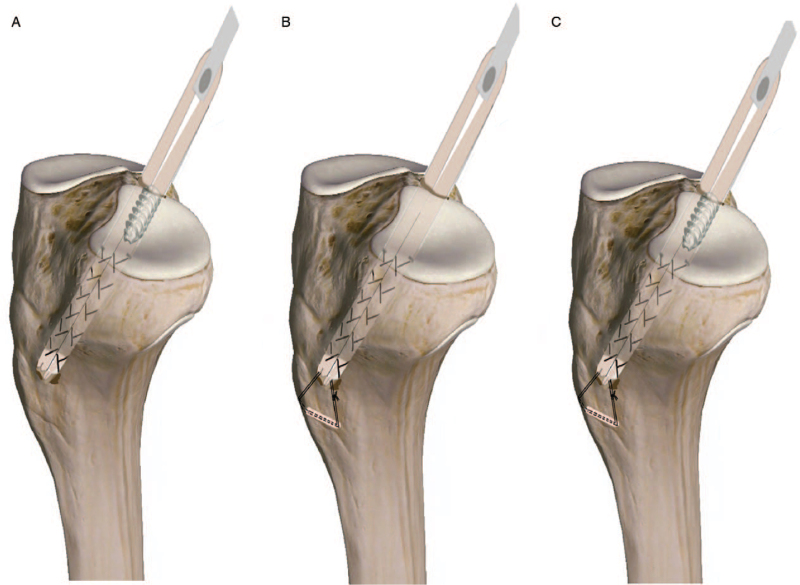
Figure 1.
Computer drawing of the three fixation groups. (A) IS; (B) TTF; (C) TTF + IS. IS: Interference screw fixation; TTF: Transtibial tubercle fixation.
For all porcine tibiae, a tunnel with a diameter of 8 mm and a length of 5 to 6 cm was prepared on the tibia by the transtibial technique. A PCL tibial drill guide (Arthrex, Naples, FL, USA) was used, and the drill guide angle of the tibia was oriented at 55° to 60°. A double-looped graft was prepared on the table, folded in half, and thinned to 8 mm in diameter and 9 to 10 mm in length. Three No. 2 Ultrabraid sutures (Smith & Nephew, Andover, MA, USA) were used to sew 3 cm of both ends of each tendon together using a crisscross stitch. Then, the grafts were wrapped in 0.9% saline solution-soaked gauze before testing. In the IS group, the graft was fixed with an 8 × 25 mm titanium interference screw (Guardsman) in the proximal tibial tunnel [Figure 2]. In the TTF + IS group, the graft was fixed with an 8 × 25 mm titanium interference screw (Guardsman) in the proximal tibial tunnel, and then the ends of the sutures were tied at the tibia. An eyelet-passing pin was drilled transversely 1 cm distal to the tibial tunnel (parallel to the tibial joint line and 1 cm posterior to the anterior tibial cortex). The sutures were passed through the transtibial tubercle with the eyelet-passing pin. All the ends of the sutures were tied at the tibia [Figure 3].
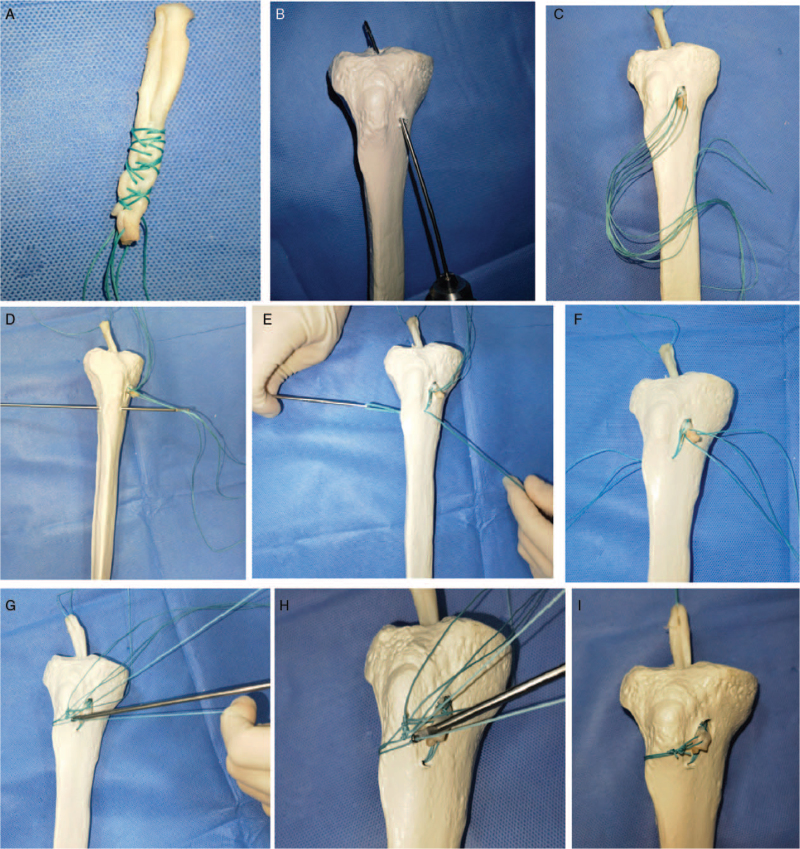
Figure 2.
Sawbone model demonstrating the TTF technique. (A–C) The graft was pulled into the tibial tunnel; an eyelet-passing pin was drilled transversely into the transtibial tubercle. (D–F) The sutures were passed to the lateral side. (G–I) The transosseous sutures were tied at the tibia with a knot pusher. TTF: Transtibial tubercle fixation.
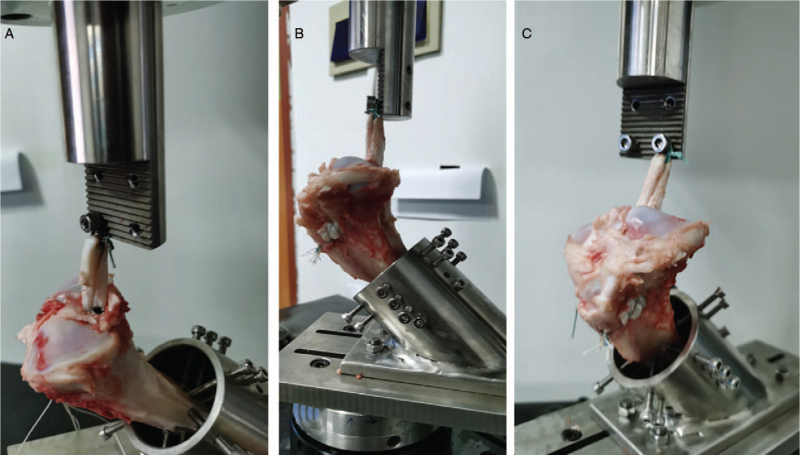
Figure 3.
(A) IS: the graft was fixed with a titanium interference screw in the proximal tibial tunnel. (B) TTF: the graft was fixed with high-strength sutures tied at the tibia. (C) TTF + IS: the graft was fixed with a titanium interference screw in the proximal tibial tunnel; the ends of the high-strength sutures were tied at the tibia. IS: Interference screw fixation; TTF: Transtibial tubercle fixation.
Biomechanical testing using animal tissue
Biomechanical testing was performed in a similar manner to the methods described by Zhang et al[20] The tibias were fixed in a custom testing jig [Figures 2 and 3]. All biomechanical tests of the graft-fixation method-tibia complexes were administered using a testing machine. The looped end of the double-looped porcine tendon graft was fixed to a bar attached to the base of the material testing machine. The free graft was kept at a length of 3 cm. The direction of the tensile force and tibial bone tunnel formed an angle of 130° in the sagittal plane. For the graft-fixation method, the tibia complex was pre-conditioned at 50 N for 5 min, and cyclic loads between 50 and 250 N were applied for 1000 cycles at a frequency of 1 Hz. Grafts were marked with links at tunnel exit points applying the pre-conditioning load and again after the cyclic loading test. Graft slippage was measured as the distance between these two lines. After clinical load testing, the constructs were pre-loaded at 20 N for 2 min; then, they underwent load-to-failure testing at a rate of 10 mm/min. The ultimate failure load (N) was determined. Pull-out stiffness (N/mm) was calculated as the slope of the linear portion of the load-elongation curve. The failure modes were noted.
Statistical analysis
Statistical analysis was performed using SPSS 21.0 (IBM, Armonk, NY, USA). We used the Kolmogorov-Smirnov test to determine the normally distributed variables within the groups. The Student's t test was used to compare the elongation, stiffness, and failure load among the three test groups. The significance level was set at P < 0.050.
Results
Cyclic testing
No failures occurred during cyclic testing. Table 1 reports the cyclic testing results (1000 cycles) in the three groups. The mean graft slippage values for the IS group, TTF group, and TTF + IS group were 1.37 ± 0.45, 1.98 ± 0.46, and 1.39 ± 0.50 mm, respectively. There were no significant differences in slippage among the three groups.
Table 1.
Cyclic testing and load-to-failure testing in the three groups.
| Items | IS | TTF | TTF + IS | P ∗ | P † | P ‡ |
| Slippage after 1000 cycles (mm) | 1.37 ± 0.45 | 1.40 ± 0.41 | 1.39 ± 0.50 | 0.883 | 0.943 | 0.039 |
| Stiffness (N/mm) | 120.27 ± 15.66 | 92.77 ± 20.16 | 131.79 ± 17.95 | 0.001 | 0.127 | <0.001 |
| Ultimate failure load (N) | 556.49 ± 65.33 | 660.92 ± 77.74 | 876.34 ± 58.78 | 0.001 | <0.001 | <0.001 |
Data are presented as mean ± standard deviation. ∗IS vs. TTF; †IS vs. TTF + IS; ‡TTF vs. TTF + IS. IS: Interference screw; TTF: Transtibial tubercle fixation.
Load-to-failure testing
The ultimate failure load in the TTF + IS group was significantly higher than those in the IS group and the TTF group (876.34 ± 58.78 N in the TTF + IS group vs. 556.49 ± 65.33 N in the IS group [P < 0.001] and 660.92 ± 77.74 N in the TTF group [P < 0.001]). The ultimate failure load in the TTF group was also significantly higher than that in the IS group (660.92 ± 77.74 N vs. 556.49 ± 65.33 N; P = 0.001).
The stiffness in the TTF group was significantly lower than those in the IS group and the TTF + IS group (92.77 ± 20.16 N/mm in the TTF group vs. 120.27 ± 15.66 N/m in the IS group [P < 0.001] and 131.79 ± 17.95 N/mm in the TTF + IS group [P < 0.001]). No significant difference in the mean stiffness was found between the IS group and the TTF + IS group [Table 1].
Discussion
The principal finding of our study was that the surgical technique for transtibial PCL reconstruction with TTF using several high-strength sutures provided a higher ultimate failure load than IS alone or TTF alone during PCL reconstruction on the tibial side in a porcine model. In the cyclic testing study, there were no significant differences in the slippage between the IS group and the TTF + IS group. In the load-to-failure testing, the TTF + IS group had a higher ultimate failure load than the IS group and the TTF group. The stiffness in the TTF group was significantly lower than that in the IS group and the TTF + IS group. No significant difference in mean stiffness was found between the IS group and the TTF + IS group (P = 0.127).
Recent studies have supported that the transtibial technique or tibial inlay technique can improve the stability of the knee in PCL-reconstructed knees.[1,13–17,19,20,22–27] However, the optimal PCL reconstruction technique has yet to be determined because PCL reconstruction has not had the same success in restoring knee stability as ACL reconstruction. Many authors have pointed out that graft fixation techniques and graft fixation levels are critical factors for successful PCL reconstruction using hamstring tendon grafts.[3]
There are some biomechanical studies supporting that supplementary tibial fixation for ACL reconstruction may be beneficial[20,28] and showing that supplementary fixation with staple or push-lock screws increases the ultimate failure load compared with interference fixation alone.[28] Multiple strands of high-strength sutures can theoretically provide a higher ultimate failure load. The transosseous suture fixation technique with high-strength sutures has been used for the repair of the rotator cuff, patellar tendon, and quadriceps tendon ruptures,[11,18,29–35] and we used transosseous suture fixation with high-strength sutures for PCL reconstruction in this biomechanical study. Another study published a similar technical note for TTF without hardware for ACL and PCL reconstruction.[13] Our study is the first to compare the biomechanics of supplementary TTF using several high-strength sutures with those of IS in transtibial PCL reconstruction. Regarding TTF + IS vs. IS alone or TTF alone, we found that supplementary TTF provided a higher ultimate failure load than IS alone or TTF alone for PCL graft-to-tibial tunnel fixation. This procedure may theoretically be recommended for supplementary fixation in cases of revision surgery with tunnel widening and graft-tunnel mismatch in PCL reconstruction. The supplementary transtibial tubercle technique does not require implants and is therefore much less expensive than other techniques, such as suspension buttons, screws or washers, and metallic anchors. Considering the decreased biomechanical properties with TTF alone (relatively lower stiffness), it might not be recommended for PCL fixation alone in a clinical setting. A longer effective length of reconstructed graft could lead to increased overall graft stiffness and decreased total graft deformation.[4] We chose to avoid the use of IS alone or TTF alone for PCL graft fixation because of the decreased pullout strength and/or decreased stiffness, which might have led to decreased overall graft stiffness and increased total graft deformation.
There were some limitations to our study. First, a main limitation of this biomechanical study was that we only focused on the time-zero outcomes. Second, we could not study the healing of the graft to bone over time. Third, human bone was not used in this study because the availability of young human bone and hamstring tendons for biomechanical testing is limited. The porcine bone model may not indicate the actual situation in human surgical repair, which limits the value of the study. However, porcine bone specimens are commonly used for biomechanical studies due to their similar structural and material properties to human hamstring tendons.[20,21] Fourth, this is another offering for knee ligament reconstruction surgeons and is a relatively non-complicated and inexpensive technique. There are no comparative data with clinical outcomes. Finally, we should provide evidence that this technique restores knee function, motion, and stability in future clinical studies.
The results of this biomechanical study suggest that supplementary TTF + IS increased the ultimate failure loads compared with conventional IS alone.
Conflicts of interest
None.
Footnotes
How to cite this article: Duan MY, Sun R, Zhuang LT, Zhang HZ. Biomechanical evaluation of a novel transtibial posterior cruciate ligament reconstruction using high-strength sutures in a porcine bone model. Chin Med J 2021;134:2316–2321. doi: 10.1097/CM9.0000000000001725
References
- 1.Chahla J, Williams BT, LaPrade RF. Posterior cruciate ligament. Arthroscopy 2020; 36:333–335. doi: 10.1016/j.arthro.2019.12.013. [DOI] [PubMed] [Google Scholar]
- 2.Christel P. Basic principles for surgical reconstruction of the PCL in chronic posterior knee instability. Knee Surg Sports Traumatol Arthrosc 2003; 11:289–296. doi: 10.1007/s00167-003-0407-2. [DOI] [PubMed] [Google Scholar]
- 3.Hiraga Y, Ishibashi Y, Tsuda E, Toh HT. Biomechanical comparison of posterior cruciate ligament reconstruction techniques using cyclic loading tests. Knee Surg Sports Traumatol Arthrosc 2006; 14:13–19. doi: 10.1007/s00167-005-0633-x. [DOI] [PubMed] [Google Scholar]
- 4.LaPrade CM, Civitarese DM, Rasmussen MT, LaPrade RF. Emerging updates on the posterior cruciate ligament: a review of the current literature. Am J Sports Med 2015; 43:3077–3092. doi: 10.1177/0363546515572770. [DOI] [PubMed] [Google Scholar]
- 5.Lee DY, Kim DH, Kim HJ, Ahn HS, Lee TH, Hwang SC. Posterior cruciate ligament reconstruction with transtibial or tibial inlay techniques: a meta-analysis of biomechanical and clinical outcomes. Am J Sports Med 2018; 46:2789–2797. doi: 10.1177/0363546517725070. [DOI] [PubMed] [Google Scholar]
- 6.Lee YS, Han SH, Kim JH. A biomechanical comparison of tibial back side fixation between suspensory and expansion mechanisms in trans-tibial posterior cruciate ligament reconstruction. Knee 2012; 19:55–59. doi: 10.1016/j.knee.2010.11.012. [DOI] [PubMed] [Google Scholar]
- 7.Lee YS, Wang JH, Bae JH, Lim HC, Park JH, Ahn JH, et al. Biomechanical evaluation of cross-pin versus interference screw tibial fixation using a soft-tissue graft during transtibial posterior cruciate ligament reconstruction. Arthroscopy 2009; 25:989–995. doi: 10.1016/j.arthro.2009.02.006. [DOI] [PubMed] [Google Scholar]
- 8.Margheritini F, Rihn JA, Mauro CS, Stabile KJ, Woo SL, Harner CD. Biomechanics of initial tibial fixation in posterior cruciate ligament reconstruction. Arthroscopy 2005; 21:1164–1171. doi: 10.1016/j.arthro.2005.06.017. [DOI] [PubMed] [Google Scholar]
- 9.Markolf KL, Zemanovic JR, McAllister DR. Cyclic loading of posterior cruciate ligament replacements fixed with tibial tunnel and tibial inlay methods. J Bone Joint Surg Am 2002; 84:518–524. doi: 10.2106/00004623-200204000-00002. [DOI] [PubMed] [Google Scholar]
- 10.May JH, Gillette BP, Morgan JA, Krych AJ, Stuart MJ, Levy BA. Transtibial versus inlay posterior cruciate ligament reconstruction: an evidence-based systematic review. J Knee Surg 2010; 23:73–79. doi: 10.1055/s-0030-1267468. [DOI] [PubMed] [Google Scholar]
- 11.McAllister DR, Hussain SM. Tibial inlay posterior cruciate ligament reconstruction: surgical technique and results. Sports Med Arthrosc Rev 2010; 18:249–253. doi: 10.1097/JSA.0b013e3181faaee1. [DOI] [PubMed] [Google Scholar]
- 12.Montgomery SR, Johnson JS, McAllister DR, Petrigliano FA. Surgical management of PCL injuries: indications, techniques, and outcomes. Curr Rev Musculoskelet Med 2013; 6:115–123. doi: 10.1007/s12178-013-9162-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pasque CB, de la Garza S. Transtibial tubercle fixation without hardware for anterior cruciate ligament and posterior cruciate ligament reconstruction:a new technique. Arthroscopy 2004; 20: (Suppl 2): 164–170. doi: 10.1016/j.arthro.2004.04.034. [DOI] [PubMed] [Google Scholar]
- 14.Nuelle CW, Milles JL, Pfeiffer FM, Stannard JP, Smith PA, Kfuri M, Jr, et al. Biomechanical comparison of five posterior cruciate ligament reconstruction techniques. J Knee Surg 2017; 30:523–531. doi: 10.1055/s-0036-1593625. [DOI] [PubMed] [Google Scholar]
- 15.Pache S, Aman ZS, Kennedy M, Nakama GY, Moatshe G, Ziegler C, et al. Posterior cruciate ligament: current concepts review. Arch Bone Jt Surg 2018; 6:8–18. [PMC free article] [PubMed] [Google Scholar]
- 16.Panchal HB, Sekiya JK. Open tibial inlay versus arthroscopic transtibial posterior cruciate ligament reconstructions. Arthroscopy 2011; 27:1289–1295. doi: 10.1016/j.arthro.2011.04.007. [DOI] [PubMed] [Google Scholar]
- 17.Wang Z, Xiong Y, Chen G, Tang X, Li Q, Zhang Z, et al. Modified tibial tunnel placement for single-bundle posterior cruciate ligament reconstruction reduces the “Killer Turn” in a biomechanical model. Medicine (Baltimore) 2019; 98:e18439.doi: 10.1097/MD.0000000000018439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim SJ, Shin JW, Lee CH, Shin HJ, Kim SH, Jeong JH, et al. Biomechanical comparisons of three different tibial tunnel directions in posterior cruciate ligament reconstruction. Arthroscopy 2005; 21:286–293. doi: 10.1016/j.arthro.2004.11.004. [DOI] [PubMed] [Google Scholar]
- 19.Zehms CT, Whiddon DR, Miller MD, Quinby JS, Montgomery SL, Campbell RB, et al. Comparison of a double bundle arthroscopic inlay and open inlay posterior cruciate ligament reconstruction using clinically relevant tools: a cadaveric study. Arthroscopy 2008; 24:472–480. doi: 10.1016/j.arthro.2007.09.012. [DOI] [PubMed] [Google Scholar]
- 20.Zhang X, Teng Y, Li R, Ma C, Yang X, Wang H, et al. Proximal, distal, and combined fixation within the tibial tunnel in transtibial posterior cruciate ligament reconstruction: a time-zero biomechanical study in vitro. Arthroscopy 2019; 35:1667–1673. doi: 10.1016/j.arthro.2019.01.017. [DOI] [PubMed] [Google Scholar]
- 21.Brown GA, Peña F, Grøntvedt T, Labadie D, Engebretsen L. Fixation strength of interference screw fixation in bovine, young human, and elderly human cadaver knees: influence of insertion torque, tunnel-bone block gap, and interference. Knee Surg Sports Traumatol Arthrosc 1996; 3:238–244. doi: 10.1007/BF01466626. [DOI] [PubMed] [Google Scholar]
- 22.Arthur JR, Haglin JM, Makovicka JL, Chhabra A. Anatomy and biomechanics of the posterior cruciate ligament and their surgical implications. Sports Med Arthrosc Rev 2020; 28:e1–e10. doi: 10.1097/JSA.0000000000000267. [DOI] [PubMed] [Google Scholar]
- 23.Benedetto KP, Hoffelner T, Osti M. The biomechanical characteristics of arthroscopic tibial inlay techniques for posterior cruciate ligament reconstruction: in vitro comparison of tibial graft tunnel placement. Int Orthop 2014; 38:2363–2368. doi: 10.1007/s00264-014-2458-z. [DOI] [PubMed] [Google Scholar]
- 24.Gill TJ, Van de Velde SK, Carroll KM, Robertson WJ, Heyworth BE. Surgical technique: aperture fixation in PCL reconstruction: applying biomechanics to surgery. Clin Orthop Relat Res 2012; 470:853–860. doi: 10.1007/s11999-011-2100-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kennedy NI, LaPrade RF, Goldsmith MT, Faucett SC, Rasmussen MT, Coatney GA, et al. Posterior cruciate ligament graft fixation angles, part 2: biomechanical evaluation for anatomic double-bundle reconstruction. Am J Sports Med 2014; 42:2346–2355. doi: 10.1177/0363546514541226. [DOI] [PubMed] [Google Scholar]
- 26.Pierce CM, O’Brien L, Griffin LW, Laprade RF. Posterior cruciate ligament tears: functional and postoperative rehabilitation. Knee Surg Sports Traumatol Arthrosc 2013; 21:1071–1084. doi: 10.1007/s00167-012-1970-1. [DOI] [PubMed] [Google Scholar]
- 27.Vellios EE, Jones KJ, McAllister DR. Open tibial inlay PCL reconstruction: surgical technique and clinical outcomes. Curr Rev Musculoskelet Med 2018; 11:316–319. doi: 10.1007/s12178-018-9490-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lee JJ, Otarodifard K, Jun BJ, McGarry MH, Hatch GF, 3rd, Lee TQ. Is supplementary fixation necessary in anterior cruciate ligament reconstructions? Am J Sports Med 2011; 39:360–365. doi: 10.1177/0363546510390434. [DOI] [PubMed] [Google Scholar]
- 29.Abellán D, Nart J, Pascual A, Cohen RE, Sanz-Moliner JD. Physical and mechanical evaluation of five suture materials on three knot configurations: an in vitro study. Polymers (Basel) 2016; 8:147.doi: 10.3390/polym8040147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Barber FA, Hapa O, Bynum JA. Comparative testing by cyclic loading of rotator cuff suture anchors containing multiple high-strength sutures. Arthroscopy 2010; 26: (9 Suppl): S134–S141. doi: 10.1016/j.arthro.2010.03.007. [DOI] [PubMed] [Google Scholar]
- 31.Barber FA, Herbert MA, Beavis RC. Cyclic load and failure behavior of arthroscopic knots and high strength sutures. Arthroscopy 2009; 25:192–199. doi: 10.1016/j.arthro.2008.09.010. [DOI] [PubMed] [Google Scholar]
- 32.Gnandt RJ, Smith JL, Nguyen-Ta K, McDonald L, LeClere LE. High-tensile strength tape versus high-tensile strength suture: a biomechanical study. Arthroscopy 2016; 32:356–363. doi: 10.1016/j.arthro.2015.08.013. [DOI] [PubMed] [Google Scholar]
- 33.Hapa O, Barber FA, Süner G, Özden R, Davul S, Bozdağ E, et al. Biomechanical comparison of tibial eminence fracture fixation with high-strength suture, EndoButton, and suture anchor. Arthroscopy 2012; 28:681–687. doi: 10.1016/j.arthro.2011.10.026. [DOI] [PubMed] [Google Scholar]
- 34.Kindya MC, Konicek J, Rizzi A, Komatsu DE, Paci JM. Knotless suture anchor with suture tape quadriceps tendon repair is biomechanically superior to transosseous and traditional suture anchor-based repairs in a cadaveric model. Arthroscopy 2017; 33:190–198. doi: 10.1016/j.arthro.2016.06.027. [DOI] [PubMed] [Google Scholar]
- 35.Meyer DC, Bachmann E, Lädermann A, Lajtai G, Jentzsch T. The best knot and suture configurations for high-strength suture material. An in vitro biomechanical study. Orthop Traumatol Surg Res 2018; 104:1277–1282. doi: 10.1016/j.otsr.2018.08.010. [DOI] [PubMed] [Google Scholar]