Abstract
Background
Shoulder injections for conditions such as adhesive capsulitis are commonly performed and can be administered through image-based or landmark-based injection approaches. Ultrasound-guided injections are widely used and accurate because ultrasound allows real-time visualization of the needle and injected contrast. Landmark-based injections would be advantageous, if they were accurate, because they would save the time and expense associated with ultrasound. However, few prospective studies have compared well-described landmark-based shoulder injection techniques without ultrasound.
Question/purpose
Using anatomic landmarks, and without using ultrasound, is the accuracy of glenohumeral injection for adhesive capsulitis greater via the posterior approach or via a new anterior approach?
Methods
Between 2018 and 2020, we treated 108 patients potentially eligible for adhesive capsulitis treatment. These patients had clinical symptoms of aggravating shoulder pain with a duration of less than 4 months and passively impaired, painful glenohumeral ROM. Due to the exclusion of patients with other shoulder conditions (full-thickness rotator cuff ruptures and posttraumatic stiffness), 95 patients received an injection in this sequential, prospective, comparative study. Between 2018 and 2019, 41 patients (17 males and 24 females; mean age 52 ± 5 years; mean BMI 24 ± 3 kg/m2) were injected through the posterior approach, with the acromion as the anatomical landmark, during the first part of the study period. After that, between 2019 and 2020, 54 patients (20 males and 34 females; mean age 54 ± 4 years; mean BMI 23 ± 3 kg/m2) received an injection through a new anterior approach, with the acromioclavicular joint as the anatomic landmark, during the second part of the study period. Injections via both approaches were administered by two experienced shoulder specialists (both with more than 10 years of experience). Both specialists had experience with the posterior approach before this study, and neither had previous training with the new anterior approach. Injections contained a corticosteroid, local anaesthetic, and contrast medium. Radiographs were taken within 20 minutes after the injection, and a radiologist blinded to the technique determined accuracy. Accurate injections were defined as having contrast fluid limited to the glenohumeral joint, while inaccurate injections displayed leakage of contrast fluid into the soft tissue or subacromial space. All of the enrolled patients were analyzed.
Results
In the group with the posterior approach, the accuracy was 78% (32 of 41) in contrast to 94% (51 of 54, odds ratio 0.21 [95% CI 0.05 to 0.83]; p = 0.03) in patients with the new anterior approach.
Conclusion
The new anterior approach without the use of ultrasound was more accurate than the posterior approach. In fact, it was nearly as accurate as previously published ultrasound-guided approaches. We recommend using the new anterior approach for intraarticular glenohumeral injections instead of ultrasound-guided injections because it will save time and costs associated with ultrasound. Still, the clinical effects (anxiety, pain, functional outcome, and adverse events) of the new anterior approach should be compared with ultrasound-guided injections in a randomized study.
Level of Evidence
Level II, therapeutic study.
Introduction
Adhesive capsulitis is painful, limiting, and common, occurring in 2% to 5% of the general population [10, 14]. Intraarticular glenohumeral steroid injections are part of the treatment for many patients with adhesive capsulitis [19] because they may reduce inflammation and provide pain relief. Injections are administered either through image-based or landmark-based injection approaches, as well as with ultrasound guidance. Ultrasound-guided injections are widely used and accurate because ultrasound allows real-time visualization of the needle and injected contrast [1, 5, 9, 11]. However, ultrasound-guided injections are more challenging as they require training to coordinate the transducer and needle at the same time [2], and not every clinician or general practitioner has the ability to use ultrasound in general practice or has access to a machine. Moreover, whether ultrasound-guided injections are more effective than injections without ultrasound remains controversial [3, 15]. A recent randomized study by Cho et al. [3] displayed no differences in pain and functional outcome between ultrasound-guided versus landmark-based corticosteroid injections for adhesive capsulitis, with accuracy rates of 100% and 71%, respectively. With regard to cost-effectiveness, the study of Gyftopoulos et al. [6] described ultrasound-guided injections as the best option for treating adhesive capsulitis. However, this conclusion was mainly based on the assumption that injected steroids have a greater effect on symptoms when administered intraarticularly than when placed extraarticularly. Even in their analysis, with the assumption of a greater effect for intraarticular injections, a landmark-based approach would become the dominant injection strategy if it were to achieve an accuracy of 91% or greater.
Landmark-based injections can be easily performed without extra costs of imaging guidance. Nevertheless, the reported accuracy of these landmark-based injection approaches varies widely (42% to 100%) [18]. Although several studies in cadavers found accurate injection approaches without using ultrasound [4, 7, 8, 12, 16, 17], there is no consensus about which approach to use. Prospective studies comparing well-described landmark-based injection approaches that can be done accurately without ultrasound are scarce [20, 21]. In 2011, Tobola et al. [20] prospectively evaluated the accuracy of three well-described glenohumeral injection approaches: the posterior, supraclavicular, and the anterior approach. Accuracy, regardless of the experience of the injection provider, was 46%, 46%, and 65%, respectively. The limited number of comparative studies that clearly describe an accurate landmark-based injection approach might be the reason why there is no standard injection approach and why most clinicians still prefer to perform expensive and time-consuming ultrasound-guided injections.
We therefore asked: Using anatomic landmarks, and without using ultrasound, is the accuracy of glenohumeral injection for adhesive capsulitis greater via the posterior approach or via a new anterior approach?
Patients and Methods
Study Design and Setting
This prospective, comparative study was performed at one outpatient clinic. Two groups of patients were treated for adhesive capsulitis. The first group received an injection through the posterior approach, and the second group received the injection through a new anterior approach. The groups were treated sequentially, and there was no overlap. Both injection approaches were performed using BD Microlance 21 Gauge x 2-inch needles and without the use of ultrasound. Injections contained a corticosteroid (1 cc methylprednisolone 40 mg), a local anaesthetic (2 cc lidocaine 10 mg/mL), and contrast medium (3 cc loxaglic acid 320 mg L/mL). Injections via both approaches were administered by two experienced shoulder specialists (EWZ, CPJV both with more than 10 years of experience). Although both specialists had experience with the posterior approach before this study, neither had any prior training with the new anterior approach. However, they were familiar with the approach because it is almost identical to the anterior portal routinely used in shoulder arthroscopy. An AP and axillary radiograph were taken within 20 minutes after the injection, and a radiologist blinded to the injection technique determined accuracy. Accurate injections were defined as having contrast fluid localized in the glenohumeral joint, while inaccurate injections displayed leakage of contrast fluid into the soft tissue or subacromial space.
Participants
Between 2018 and 2020, 108 patients with clinical symptoms of adhesive capsulitis with a duration of less than 4 months were screened for inclusion. Adhesive capsulitis was defined as shoulder pain with impaired passive glenohumeral ROM of at least 30° in two or more planes. Apart from the clinical examination, the diagnosis was further confirmed on imaging (a basic series of radiographs was made for every shoulder patient and ultrasound or MRI was performed if there was a suspicion of other shoulder conditions).
The first 54 potentially eligible patients were evaluated for inclusion in the posterior approach group and the second 54 potentially eligible patients were evaluated for inclusion in the new anterior approach group. Thirteen patients of the first group were excluded due to full-thickness rotator cuff rupture (n = 7) and posttraumatic stiffness (n = 6), while no patients were excluded in the second group (Fig. 1).
Fig. 1.
Study enrollment process.
After we obtained informed consent, 95 patients participated in this sequential, prospective, comparative study. Between 2018 and 2019, 41 patients (17 males and 24 females; mean age 52 ± 5 years; mean BMI 24 ± 3 kg/m2) received a shoulder injection through the posterior approach, with the acromion as the anatomical landmark, during the first part of the study period. Then, between 2019 and 2020, 54 patients (20 males and 34 females; mean age 54 ± 4 years; mean BMI 23 ± 3 kg/m2) received an injection through the new anterior cranial approach, with the acromioclavicular joint as anatomical landmark, during the second part of the study period (Table 1). All patients were analyzed in the groups to which they were assigned, and none were lost to follow-up.
Table 1.
Demographics of the classic posterior and new anterior approach study group.
| Parameter | Classic posterior study group (n = 41) | New anterior study group (n = 54) | p value |
| Age in years | 52 ± 5 | 54 ± 4 | 0.11 |
| BMI in kg/m2 | 24 ± 3 | 23 ± 3 | 0.15 |
| Female sex | 59 (24) | 63 (34) | 0.33 |
Data are presented as mean ± SD or % (n).
Study Interventions
Posterior Approach
During this injection procedure, the patient sat in an upright position while the forearm rested on the upper leg in internal rotation. Distally and inferior of the acromion, the soft spot at the level of the posterior glenohumeral joint was palpated, and the needle was introduced immediately lateral to the joint line. When the needle tip hit the humeral head, it was withdrawn slightly to allow fluid to be injected without resistance (Fig. 2).
Fig. 2.

This is a photograph of the posterior approach. During this approach, the patient sits upright while the forearm rests on the upper leg in internal rotation. Distally and inferior of the acromion, the soft spot at the level of the posterior glenohumeral joint is palpated, and the needle is introduced immediately lateral to the joint line.
New Anterior Approach
During this injection procedure (Fig. 3), the patient sat in an upright position while the forearm rested in maximal achievable external rotation on their upper leg, to avoid contact of the needle with the long head of the biceps. Subsequently, the injection was administered by approaching the shoulder from above. The needle was placed in the center of a line between the coracoid and anterior tip of the acromion in the soft spot, approximately 1 cm ventrally from the acromioclavicular joint and 0.5 cm laterally from the acromioclavicular joint gap. The needle was injected at a dorsocaudal angle of 30° and 10° of medial angulation. When the needle hit the humeral head, fluid was injected when there was hardly any resistance.
Fig. 3.

A-B These photographs show the new anterior approach with the AC joint as the anatomical landmark. (A) The patient sits upright, and the injection is given by approaching the shoulder from above. (B) The forearm rests in maximal achievable external rotation on the patient’s upper leg. The needle is injected 1 cm ventrally from the acromioclavicular joint and 0.5 cm laterally from the acromioclavicular joint gap, in a dorsocaudal angle of 30° and 10° of medial angulation.
Study Outcome
Our study goal was to evaluate if the accuracy of the new anterior injection approach without ultrasound was superior to the posterior approach for adhesive capsulitis of the shoulder. To achieve this, both groups received an injection that contained a mixture of a corticosteroid, an anesthetic, and contrast medium. Radiographs were taken within 20 minutes after the injection, and an experienced musculoskeletal radiologist (who had more than 10 years of experience) blinded to the injection technique determined accuracy. Accurate injections were defined as having contrast fluid localized in the glenohumeral joint, and inaccurate injections displayed the leakage of contrast fluid in the soft tissue or subacromial space.
Bias
This study was prone to selection bias because patients were included without randomization. However, patients were included sequentially according to a standard inclusion protocol. In addition, performance bias was possible because the surgeon (CPJV) who conceived of the new anterior approach performed the injections. Nevertheless, the surgeon always aimed to inject intraarticularly according to good clinical practice. In addition, a second clinician (EWZ) performed a substantial number of the patients’ injections (46% [44 of 95]). The radiologist who determined accuracy was not aware of the type of injection approach used, and so assessor bias seems unlikely.
Ethical Approval
Ethical approval for this study was obtained from the Medische Ethische Toetsingscommissie Leiden (CME Leiden, code 058), part of the Central Committee on Research Involving Human Subjects (study number NL42393.058.12).
Statistical Analysis
An a priori sample size calculation was done to determine the number of patients to include. The calculation was based on detecting a difference in the accuracy of both groups, with an overall α error (two-sided) of 5% with a statistical power of 80% (β error = 0.20). We powered the study for a difference of 30%, based on prior research showing accuracy of 50% for the posterior approach and 80% for an anterior approach [16]. Consequently, we needed a minimum of 36 patients per group. In addition, we decided to include 50% extra patients (n = 18) per group to account for potential exclusions or withdrawals. All patients who received an injection (n = 95) were analyzed. Demographics of the patients who received an injection via the posterior approach were compared with those of patients who received an injection through the new anterior approach using an independent t-test. We used a Fisher exact test to analyze the accuracy of both approaches. The statistical analysis was performed using SPSS version 24 (IBM Corp), and significance was set as a p value < 0.05.
Results
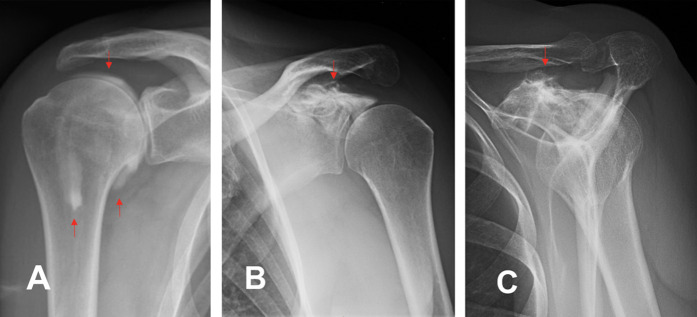
In the posterior approach group, the accuracy was 78% (32 of 41) compared with 94% (51 of 54) in the new anterior approach group (odds ratio 0.21 [95% CI 0.05 to 0.83]; p = 0.03). The bicipital groove was filled with fluid and a shortened caudal capsule was seen in patients with adhesive capsulitis who received an intraarticular injection in both groups. No fluid leakage from the glenohumeral joint was observed after the joint was infiltrated accurately through the new anterior approach (Fig. 4A). However, contrast was seen extraarticularly in three patients in the new anterior group, probably due to an incorrect injection site (Fig. 4B-C). An interesting observation in radiologic images of patients who received an inaccurate injection through the posterior approach was leakage of contrast fluid into the muscles posteriorly, with a thin layer of residual contrast fluid in the glenohumeral joint, indicating an initial adequate hit of the joint (Fig. 5A-B). This was not seen in the new anterior approach group.
Fig. 4.
A-C These radiographs show the new anterior approach. (A) This radiograph shows an accurate intraarticular injection via the new anterior approach in the right shoulder. The upper red arrow indicates intraarticular contrast medium. There was no leakage in the soft tissue. The lower left red arrow indicates the sulcus was filled with contrast. The lower right red arrow shows a restricted capsule caudally, in accordance with the diagnosis of frozen shoulder. (B-C) These radiographs show an extraarticular injection via the new anterior approach in the left shoulder. The red arrows indicate contrast medium. The needle was probably placed too medially, hitting the upper side of the glenoid. A color image accompanies the online version of this article.
Fig. 5.

A-B These radiographs show the posterior approach. (A) Injection fluid has leaked into the muscles in the right shoulder. The red arrows indicate some residual contrast in the glenohumeral joint (indicating an adequate hit of the joint). (B) Leakage of contrast is seen in the soft tissue posteriorly. A color image accompanies the online version of this article.
Discussion
Although ultrasound-guided injections are widely used because they are accurate, landmark-based shoulder injection approaches that can be performed accurately without ultrasound would be beneficial, as they would save time and expense associated with ultrasound. But prospective studies comparing well-described landmark-based shoulder injection techniques that can be done accurately without ultrasound are scarce [20, 21]. In this prospective study, we compared two landmark-based approaches: the posterior approach and a new anterior injection approach. The new anterior approach, without the use of ultrasound, is nearly as accurate as other published ultrasound-guided approaches [1, 5, 9, 11, 13]. Therefore, we recommend using the new anterior approach for intraarticular glenohumeral injections.
Limitations
A weak point of this study is the lack of randomization. We were not able to set up a randomized controlled trial due to practical issues that come with implementing randomization. Instead, the two surgeons (EWZ, CPJV) who administered the injection included eligible adhesive capsulitis patients sequentially, first in the posterior group and then in the new anterior group. More patients were included in the new anterior group than in the posterior group because 13 patients were excluded in the posterior approach due to full-thickness rotator cuff ruptures (n = 7) and posttraumatic stiffness (n = 6). Consequently, 41 patients received an injection through the posterior approach, and 54 patients received an injection via the new anterior approach. Selection bias seemed not to be prominent here, as patients in the two injection groups were comparable with regard to age, BMI, and sex.
Another limitation that could have occurred is performance bias. Although both surgeons had more than 10 years of experience, one might be concerned with the fact that one of the study surgeons (CPJV) developed the new anterior approach that was being tested; the possibility that it was being compared with an approach that he might have believed to be inferior could have influenced the results. However, as part of good clinical practice, both surgeons (EWZ, CPJV) did their best to administer accurate injections regardless of the injection approach used. This was displayed by the relatively high accuracy of the posterior injections compared with previous studies using the same posterior approach [13, 16, 18, 20]. Additionally, pooling the results of both surgeons seemed fair because they were comparably accurate using both approaches (inaccurate injections for EWZ: posterior approach 4 of 18, new anterior approach 2 of 26; inaccurate injections for CPJV: posterior approach 5 of 23, new anterior approach 1 of 28). No learning curve was observed because inaccurate injections in both study groups were seen in the beginning-, middle-, and late-injection period for both clinicians performing the injections. Nevertheless, it would be interesting to see if less experienced colleagues have a learning curve and achieve similar accuracy rates.
In addition, there is a possibility of assessment bias. Although surgeons and patients knew which injection approach was performed, the radiologist who determined accuracy did not receive information concerning the injection approach. Hence, accuracy assessment was not influenced by the radiologist’s prior knowledge of the injection approach. The lack of comparison with ultrasound-guided injections might be another limitation. However, a recent study by Cho et al. [3] showed no differences in pain and functional outcome between the 100% accurate ultrasound-guided group and the 71% accurate landmark-based injection group. Therefore, major differences with regard to pain and functional outcome between the ultrasound-guided approach and the new anterior approach are not expected.
Accuracy of the New Anterior Injection Approach
During the posterior approach, the needle was advanced until it hit the humeral head. The bevel of the needle sits exactly at the capsule. Injections of fluid are therefore likely to result in some extravasation external to the capsule and along the infraspinatus muscle belly. In contrast, injection via the anterior approach goes through the rotator interval into an open space in the joint and allows more reliable injection into the glenohumeral joint itself. This might be the reason for the superior accuracy of the new anterior injection approach (94%). This result aligns with a recent study of Shao et al. [17] (95.7% of 116 patients), where a similar (transcoracoacromial ligament) approach for intraarticular injections was used. The main difference between our anterior approach and the one in that study [17] is the reference point. In that study, the investigators identified the anterolateral corner of the acromion, superior lateral border of the coracoid tip, and curved depression of the distal clavicle. Subsequently, the needle entry site was located at the intersection between the distal third and middle third of the superior lateral border of the coracoid tip-curved depression of the distal clavicle line. We believe that our approach is less complicated because it requires only one landmark (the acromioclavicular joint). On anatomic drawings and images, the line of the acromioclavicular joint is typically in line with the glenohumeral joint and it can be used as a landmark for this technique. The acromioclavicular joint can usually be identified by palpating the small dimple of the joint line at the ventral site of the end of the clavicle. Therefore, we believe our findings can cause a shift from ultrasound-guided injections to adequate landmark-based glenohumeral shoulder injections.
Conclusion
In this sequential, prospective trial, we presented a new anterior landmark-based approach without the use of ultrasound, and found it was more accurate than the posterior approach. Moreover, the new anterior approach is nearly as accurate as other published ultrasound-guided approaches [1, 5, 9, 11, 13]. Consequently, we recommend using the new anterior approach in practice as it will save time and the cost associated with ultrasound. Future multicenter randomized studies with a larger group of less experienced clinicians performing the injections should compare the accuracy and functional outcome between ultrasound-guided injections and injections administered through the new anterior approach. This may cause a shift from ultrasound-guided injections to adequate landmark-based injections.
Acknowledgments
We thank Dr. S.R. Thoma, a radiologist at Alrijne Hospital, Leiden, the Netherlands, for his assessment of the accuracy of the administered injections.
Footnotes
Each author certifies that neither he or she, nor any member of his or her immediate family, has funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Ethical approval for this study was obtained from the Medische Ethische Toetsingscommissie Leiden (CME Leiden, code 058), part of the Central Committee on Research Involving Human Subjects (study number NL42393.058.12).
This work was performed at the Alrijne Hospital, Leiden, the Netherlands.
Contributor Information
Pieter C. J. de Groot, Email: pcjdegroot@gmail.com.
Eline W. Zwitser, Email: ewzwitser@alrijne.nl.
Cornelis P. J. Visser, Email: cpjvisser@alrijne.nl.
References
- 1.Ali AH, Said HG, Abo Elhamd E, Mahmoud MK, Qenawy OK. Shoulder MR arthrography: comparative evaluation of three different contrast injection techniques using an anterior approach. J Magn Reson Imaging. 2021;53:481-490. [DOI] [PubMed] [Google Scholar]
- 2.Bruyn GA, Schmidt WA. How to perform ultrasound-guided injections. Best Pract Res Clin Rheumatol. 2009;23:269-279. [DOI] [PubMed] [Google Scholar]
- 3.Cho CH, Min BW, Bae KC, Lee KJ, Kim DH. A prospective double-blind randomized trial on ultrasound-guided versus blind intra-articular corticosteroid injections for primary frozen shoulder. Bone Joint J. 2021;103-b:353-359. [DOI] [PubMed] [Google Scholar]
- 4.Esenyel CZ, Ozturk K, Demirhan M, et al. Accuracy of anterior glenohumeral injections: a cadaver study. Arch Orthop Trauma Surg. 2010;130:297-300. [DOI] [PubMed] [Google Scholar]
- 5.Gokalp G, Dusak A, Yazici Z. Efficacy of ultrasonography-guided shoulder MR arthrography using a posterior approach. Skeletal Radiol. 2010;39:575-579. [DOI] [PubMed] [Google Scholar]
- 6.Gyftopoulos S, Abballe V, Virk MS, Koo J, Gold HT, Subhas N. Comparison between image-guided and landmark-based glenohumeral joint injections for the treatment of adhesive capsulitis: a cost-effectiveness study. AJR Am J Roentgenol. 2018;210:1279-1287. [DOI] [PubMed] [Google Scholar]
- 7.Kim JS, Yun JS, Kim JM, et al. Accuracy of the glenohumeral injection using the superior approach: a cadaveric study of injection accuracy. Am J Phys Med Rehabil. 2010;89:755-758. [DOI] [PubMed] [Google Scholar]
- 8.Kraeutler MJ, Cohen SB, Ciccotti MG, Dodson CC. Accuracy of intra-articular injections of the glenohumeral joint through an anterior approach: arthroscopic correlation. J Shoulder Elbow Surg. 2012;21:380-383. [DOI] [PubMed] [Google Scholar]
- 9.Messina C, Banfi G, Aliprandi A, et al. Ultrasound guidance to perform intra-articular injection of gadolinium-based contrast material for magnetic resonance arthrography as an alternative to fluoroscopy: the time is now. Eur Radiol. 2016;26:1221-1225. [DOI] [PubMed] [Google Scholar]
- 10.Moren-Hybbinette I, Moritz U, Schersten B. The clinical picture of the painful diabetic shoulder--natural history, social consequences and analysis of concomitant hand syndrome. Acta Med Scand. 1987;221:73-82. [DOI] [PubMed] [Google Scholar]
- 11.Ogul H, Bayraktutan U, Ozgokce M, et al. Ultrasound-guided shoulder MR arthrography: comparison of rotator interval and posterior approach. Clin Imaging. 2014;38:11-17. [DOI] [PubMed] [Google Scholar]
- 12.Powell SE, Davis SM, Lee EH, et al. Accuracy of palpation-directed intra-articular glenohumeral injection confirmed by magnetic resonance arthrography. Arthroscopy. 2015;31:205-208. [DOI] [PubMed] [Google Scholar]
- 13.Raeissadat SA, Rayegani SM, Langroudi TF, Khoiniha M. Comparing the accuracy and efficacy of ultrasound-guided versus blind injections of steroid in the glenohumeral joint in patients with shoulder adhesive capsulitis. Clin Rheumatol. 2017;36:933-940. [DOI] [PubMed] [Google Scholar]
- 14.Reeves B. The natural history of the frozen shoulder syndrome. Scand J Rheumatol. 1975;4:193-196. [DOI] [PubMed] [Google Scholar]
- 15.Sage W, Pickup L, Smith TO, Denton ER, Toms AP. The clinical and functional outcomes of ultrasound-guided vs landmark-guided injections for adults with shoulder pathology--a systematic review and meta-analysis. Rheumatology (Oxford). 2013;52:743-751. [DOI] [PubMed] [Google Scholar]
- 16.Sethi PM, El Attrache N. Accuracy of intra-articular injection of the glenohumeral joint: a cadaveric study. Orthopedics. 2006;29:149-152. [DOI] [PubMed] [Google Scholar]
- 17.Shao X, Shi LL, Wang P, Zou F, Wang J. Transcoracoacromial ligament glenohumeral injection technique: accuracy of 116 injections in idiopathic adhesive capsulitis. Arthroscopy. 2018;34:2337-2344. [DOI] [PubMed] [Google Scholar]
- 18.Simoni P, Grumolato M, Malaise O, Preziosi M, Pasleau F, de Lemos Esteves F. Are blind injections of gleno-humeral joint (GHJ) really less accurate imaging-guided injections? A narrative systematic review considering multiple anatomical approaches. Radiol Med. 2017;122:656-675. [DOI] [PubMed] [Google Scholar]
- 19.Sun Y, Zhang P, Liu S, et al. Intra-articular steroid injection for frozen shoulder: A systematic review and meta-analysis of randomized controlled trials with trial sequential analysis. Am J Sports Med. 2017;45:2171-2179. [DOI] [PubMed] [Google Scholar]
- 20.Tobola A, Cook C, Cassas KJ, et al. Accuracy of glenohumeral joint injections: comparing approach and experience of provider. J Shoulder Elbow Surg. 2011;20:1147-1154. [DOI] [PubMed] [Google Scholar]
- 21.White AET, Tuite JD. The accuracy and efficacy of shoulder injections in restrictive capsulitis. J Orthop Rheumatol. 1996;9:37-40. [Google Scholar]