Abstract
Recent advances in electronic health records and health information technology are providing new opportunities to improve the quality of care for transgender and gender diverse people, a population that experiences significant health disparities. This article recommends changes to electronic health record systems that have the potential to optimize gender-affirming care. Specifically, we discuss the importance of creating an anatomical inventory form that captures organ diversity, and of developing clinical decision support tools and population health management systems that consider each patient’s gender identity, sex assigned at birth, and anatomy.
Keywords: transgender, anatomical inventory, electronic health records, gender identity, clinical decision support
INTRODUCTION
Transgender and gender diverse (TGD) people have a gender identity that does not correspond with their sex assigned at birth based on traditional expectations. TGD people comprise an underserved population that has significant health disparities yet is largely invisible within health care systems.1–4 Recent advances in electronic health records (EHRs) and health information technology provide opportunities for increasing the visibility of TGD patients, while also improving the management and quality of their care. In this article, we present recommendations for developing anatomical inventories, clinical decision support tools, and population health management systems within the EHR that have the potential to improve care and reduce health disparities for TGD communities. These recommendations are based on work pioneered and piloted by clinicians, researchers, informaticists, and data analysts at Fenway Health, a federally qualified health center that serves over 4200 TGD patients annually and has been recognized as a leading model in TGD health and gender identity data collection.5–8 Fenway Health has trained thousands of clinicians nationally and globally in providing state-of-the-art TGD health care.9–13 Because the systems presented in this article were developed in the United States, they will likely need to be modified for other countries; furthermore, because terminology and concepts related to gender identity differ considerably among cultures, our recommendations may not be suitable for all.
Previous publications have clarified recommended practices in collecting and entering gender identity and sex assigned at birth data into EHRs.7,8,14,15 In sum, the recommendations are for organizations to: routinely collect patient information on gender identity, sex assigned at birth, pronouns, name used, and name and sex listed on health insurance and other documents needed for billing purposes; enter these data into the EHR; give patients options to not disclose information if they have privacy concerns; update the information at least annually as well as allow patients to change their information at any point in time, such as through patient portals or by informing their provider; and ensure that names and pronouns are clearly visible to administrative staff and clinicians. The Supplementary Table provides an example of question wording for gender identity data collection systems.
The collection of these data has multiple objectives. For example, knowing pronouns and names enables clinicians to address patients in a respectful manner; having information on insurance name and sex allows organizations to bill for services more effectively; understanding a person’s gender identity and sex assigned at birth helps clinicians elicit culturally responsive and individually tailored medical, sexual, reproductive, and psychosocial histories; and cross-checking gender identity with sex assigned at birth in population health databases enables organizations to enumerate their TGD patient population and create dashboards to assess for disparities in services and health outcomes. These data, however, do not tell clinicians about a TGD patient’s anatomy, which may not match expectations based on gender identity or sex assigned at birth. Collecting data on sexual/reproductive organs in combination with gender identity and sex assigned at birth provides a more complete understanding of a person’s health needs, and can thus best drive clinical decision support for preventative screening and eliciting a sexual history.
ANATOMICAL INVENTORIES
Many TGD people undergo a diversity of medical and surgical interventions to affirm their gender identity, including but not limited to gender-affirming hormone therapies, chest reconstruction, hysterectomy, genital surgeries (eg, vaginoplasty, phalloplasty, vaginectomy/colpocleisis), and breast augmentation. There are also TGD people who have not had any gender-affirming medical or surgical interventions.16 Thus clinicians cannot know the organs a TGD person has without asking the patient and reviewing their health records. An anatomical inventory (also referred to as an organ inventory) allows clinicians to document and track the presence or absence of specific organs in the EHR along with any surgical procedures in order to guide patient-centered, preventive health screenings and post-surgical care plans. Such inventories are important for all patients, regardless of gender identity, as clinicians may be unaware of any patient’s surgical history of oophorectomy, breast augmentation, etc.
The anatomical inventory can be a structured EHR form that includes a checklist of organs and surgeries that is adaptable and expandable over time (see Table 1).15,17 Currently, anatomical inventories are available as standardized forms from some EHR vendors. Other vendors may permit health care organizations to customize their own anatomical inventory forms or templates. Unlike a review of systems form that records symptoms related to organ systems, the anatomical inventory reports the absence or presence of organs, as well as surgeries related to those organs.
Table 1.
Example of an anatomical inventory. Each data field should link to a corresponding code from the International Statistical Classification of Diseases and Related Health Problems. The format of this anatomical inventory is designed for expansion to accommodate additional variables and emerging health priorities over time.
| Breasts □ Present □ Absent |
| □ Chest reconstruction |
| □ Bilateral mastectomy |
| □ Unilateral mastectomy, R |
| □ Unilateral mastectomy, L |
| □ Breast augmentation/implants |
| Uterus □ Present □ Absent |
| □ Hysterectomy—cervix removed |
| □ Hysterectomy—cervix remains |
| Ovaries □ Present □ Absent |
| □ Bilateral salpingo-oophorectomy |
| □ Unilateral salpingo-oophorectomy, R |
| □ Unilateral salpingo-oophorectomy, L |
| Cervix □ Present □ Absent |
| Vagina □ Present □ Absent |
| □ Colpocleisis—closure of the vagina |
| □ Vaginoplasty |
| Penis □ Present □ Absent |
| □ Phalloplasty/penile implant |
| □ Metoidioplasty |
| □ Erectile device |
| □ Penectomy |
| Testes □ Present □ Absent |
| □ Testicular implant(s) |
| □ Bilateral orchiectomy |
| □ Unilateral orchiectomy, R |
| □ Unilateral orchiectomy, L |
| Urethra □ Present □ Absent |
| □ Urethral lengthening |
| Prostate □ Present □ Absent |
| □ Prostatectomy |
A provider completes the anatomical inventory in the context of a patient’s clinical history and physical exam, and then can use the inventory to guide tailored conversations around sexual history and preventive health care. One way to ask patients about their anatomy is: In order to provide you with the best clinical care, it is important for me to know if you have certain body parts. Is it okay if we talk through a list of body parts, and you can let me know whether you have these? If you use different words for parts of your body, please let me know. Clinicians ought to update inventories annually, and as needed, such as after a patient undergoes a surgery to create or remove an organ.
When possible, inventory data should link to a corresponding code from the International Statistical Classification of Diseases and Related Health Problems (ICD) which helps for billing purposes, accuracy of information, and tracking quality of care measures. Although ICD codes are somewhat limited in relation to gender-affirming care, they are currently the only codes that can be used for reimbursement claims and performance measures. As systems evolve to include other standard terminologies and nomenclatures, such as Systematized Nomenclature of Medicine (SNOMED) and Logical Observation Identifiers Names and Codes (LOINC), an inventory can be updated accordingly.
An inventory may also be expanded to capture past surgeries among people with intersex variations (also known as differences in sex development), such as clitoral reduction and repair of hypospadias. We also recommend designing EHR systems to capture anatomical inventory information in discrete data fields that are cross-linked with the problem list, medical history, and surgical history sections. Importantly, data stored in problem lists can be used in billing claims to justify why care teams did or did not perform a procedure for a patient. Anatomical inventory data in problem lists may also be used for clinical decision support, as explained in the next section.
CLINICAL DECISION SUPPORT TOOLS
Clinical decision support (CDS) tools use data from the EHR to notify care teams about a patient’s care needs, such as potential health risks and upcoming clinical services. Because CDS tools are not set up to capture all possible health-related experiences, clinicians must use CDS tools in combination with clinical judgement and other factors related to the patient’s history to make care decisions. CDS tools, which exist in every EHR, typically use demographic data and laboratory and problem ICD codes to make recommendations. Because some clinical recommendations are based solely on the sex recorded for the patient, clinicians may receive inconsistent and incorrect recommendations from CDS tools for TGD patients. Take the example of a 30-year-old transgender man who had a total hysterectomy 2 years ago for gender affirmation purposes. During the patient’s annual checkup with a new provider, the CDS prompts the clinician to recommend a Pap test based on the patient’s female sex assigned at birth. Mistakes like this could increase a TGD patient’s mistrust in the clinician and the medical system in general. Integrating anatomical inventory information about the absence of this patient’s uterus and cervix into an algorithm within the CDS system would have prevented this mistake from occurring.
Algorithms incorporated into CDS tools can also help clinicians make informed decisions based on sex assigned at birth, gender identity, and hormone therapy. For example, current standardized screening guidelines for at-risk alcohol use provide the upper limit of ranges for cisgender women and cisgender men only. In the case of a transgender woman, if the CDS recommends an upper limit of alcohol use based solely on male sex assigned at birth, the cut-off may be too high, depending on the patient’s current muscle mass, metabolism, and other body composition factors affected by hormone therapy.18 By incorporating gender identity and sex assigned at birth, as well as information on hormone therapy use, the CDS tool can provide the clinician with more information to engage in shared decision-making with the patient about alcohol use.
Although there have yet to be studies that measure the outcomes of CDS tools that incorporate information relevant for TGD people, our health center’s use of these systems for 2 years has anecdotally reduced burden on clinicians and improved integration of patient information within the EHR system. The CDS could also support clinicians in safely and effectively prescribing gender-affirming hormone therapy for TGD patients. For example, CDS systems could remind clinicians to consider ordering certain laboratory tests prior to initiating a hormone regimen and during routine monitoring of hormone therapy. Finally, CDS systems should not apply rules to guide preventative screening based on an assumption that patients have binary sexual/reproductive anatomy. Increasingly, patients receive surgeries to affirm non-binary gender identities, such as penis-preserving vaginoplasty and vagina-preserving phalloplasty. In addition, patients with intersex variations may have non-binary anatomies.
POPULATION HEALTH MANAGEMENT
Many health care organizations use pay-for-performance or value-based program policies to improve quality and reduce costs. These programs are based on nationally recognized quality measures, such as the Healthcare Effectiveness Data and Information Set (HEDIS), which currently defines some population measures by binary sex without consideration of diversity in anatomy or TGD identities. Because some TGD people are excluded by this definition, health care organizations with large TGD populations may appear to be underperforming. For example, the national quality measure for cervical cancer screening defines the risk cohort as “women 21–64 years of age”; thus, the EHR would flag the cervical cancer screening record as being out of compliance for a transgender woman whose sex designation has been changed to female, even if this patient does not have a cervix. Meanwhile, a transgender man with a cervix whose sex designation has been changed to male would be excluded from this measure. A clinician could appear to be non-compliant on a particular quality measure when, in fact, the measure itself is not clinically relevant for a subset of patients.
Clinical care teams increasingly rely on population health management tools to help them follow the requirements of quality measures, federal initiatives, and global contracts. They also use these tools to monitor outcomes and provide actionable steps for care delivery. Similar to CDS tools, most population health management tools do not incorporate gender identity, sex assigned at birth, or an anatomical inventory. Some EHR vendors, however, allow customers the flexibility to include or create a customized field in their tools in order to identify and serve TGD patients more accurately.
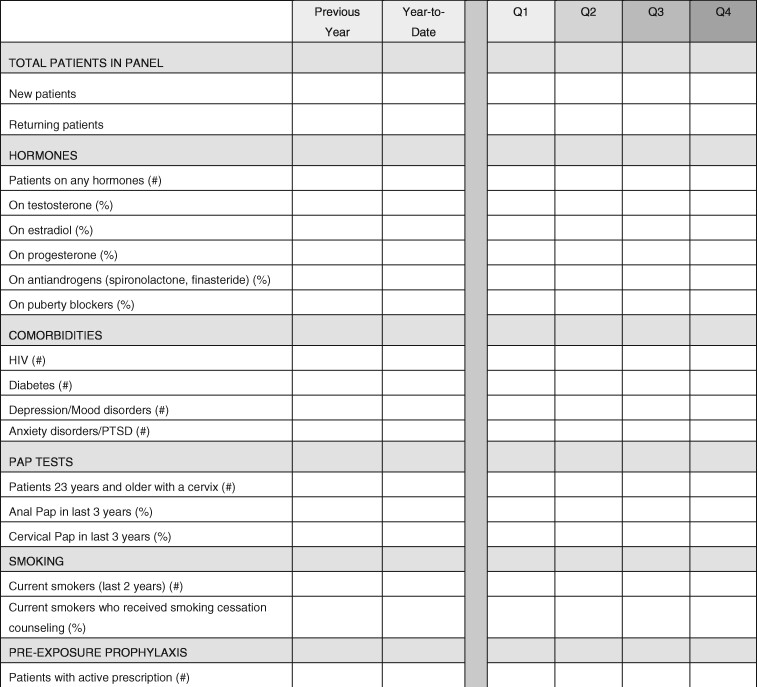
Given the limitations of some population health management tools, health care teams may benefit from developing clinical dashboards specifically for TGD patients. Dashboards present aggregate population data on key metrics in easy-to-understand graphic layouts. To identify TGD patients, information analysts can cross-check the gender identity field with the sex assigned at birth field. Suggested metrics for TGD dashboards include: (1) number of new patients; (2) number and percentage of returning patients; (3) demographics (e.g., age, race, ethnicity, gender identity, sexual orientation); (4) number of patients by service and provider panel; (5) percentage of patients taking gender-affirming hormones; (6) percentage of patients receiving recommended behavioral health screenings (e.g., depression, anxiety, substance use, tobacco); (7) percentage of patients receiving recommended preventative screenings (e.g., cervical cancer, breast/chest cancer, colon cancer); and (8) percentage of patients with common health concerns (e.g., diabetes, hypertension, HIV). See Figure 1 for an excerpt from a sample dashboard.
Figure 1.
An example clinical question and answer for a study formulated from Liu et al.22
The development of internal dashboards enables the customization of queries to include additional data fields like an anatomical inventory. For example, the cervical cancer screening measure shown in Figure 1 includes all patients ages 23 years and older who have a cervix, regardless of their sex assigned at birth or gender identity. Care teams and organizational leaders can use these metrics to observe TGD health outcomes and potential disparities at 1 point in time, and to track changes over longer periods of time. The information from dashboards may enable quality improvement projects to address disparities among all TGD patients, as well as discrepancies between care teams within the organization. For example, a dashboard may show that in the last year, only 60% of TGD patients received depression screening in primary care, compared to 85% of cisgender women and men. In this case, the team could investigate the reasons for the disparity by speaking with providers and reviewing records. Perhaps providers were prioritizing hormone therapies over screening; perhaps a higher percentage of TGD patients were already being screened by behavioral health providers; or perhaps cultural stigma played a role. Once the reasons are uncovered, the team can move forward in addressing the issues that led to inequitable screening rates among TGD patients.
CONSIDERATIONS FOR ELECTRONIC INFORMATION EXCHANGE
TGD patients may access care and services from multiple institutions, such as clinics, hospitals, and pharmacies. To ensure a smooth exchange of data across different systems, it is important for organizations, such as Health Level Seven International (HL7), to develop standardized terminology and fields for gender identity and related information. We recommend the implementation of uniform fields that capture gender identity, sex assigned at birth, name and sex on insurance, name used, pronouns, and the anatomical inventory. Organizations can look up options for terms through standards development organizations such as LOINC, a widely used health terminology standard. Interoperability of such data would, for example, enable clinical specialists seeing a patient for the first time to be able to communicate with the patient using the patient’s correct name and pronouns without the burden of collecting the data again. A current drawback with information exchange systems is a lack of privacy controls for patients who do not want to share their surgical history or sex assigned at birth with external providers. Future EHR and HL7 enhancements should allow patients to choose which information can be shared externally. In the absence of such controls, clinicians should explicitly tell patients who will have access to this information.
CONCLUSION
Advances in EHR systems present opportunities for improving clinical care for TGD patients, many of whom face numerous barriers to accessing and receiving medically necessary care. EHR systems that integrate gender identity, sex assigned at birth, and anatomical inventories, and reference those fields and forms to produce clinical recommendations, identify health disparities, and promote culturally responsive communication, will allow for more tailored, gender-affirming, and timely care for patients.
FUNDING
This work was supported by the Patient-Centered Outcomes Research Institute (AD-2017C1- 6271). The funder was not involved in the writing of the article or in the decision to submit the article for publication.
AUTHOR CONTRIBUTIONS
CG and AK conceived of the structure of the manuscript. CG, JT, and AK designed the concepts described in the article. HG drafted and edited the manuscript. All authors provided critical review and approved the final version.
DATA AVAILABILITY
No new data were generated or analyzed in support of this manuscript.
SUPPLEMENTARY MATERIAL
Supplementary material is available at Journal of the American Medical Informatics Association online.
CONFLICT OF INTEREST STATEMENT
Dr. A.S. Keuroghlian stands to receive future royalties as editor of a forthcoming McGraw-Hill Education textbook on transgender and gender diverse care. The authors have no financial conflicts to report.
Supplementary Material
REFERENCES
- 1. Reisner SL, Greytak EA, Parsons JT, Ybarra ML.. Gender minority social stress in adolescence: disparities in adolescent bullying and substance use by gender identity. J Sex Res 2015; 52 (3): 243–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Reisner SL, White Hughto JM, Gamarel KE, Keuroghlian AS, Mizock L, Pachankis JE.. Discriminatory experiences associated with posttraumatic stress disorder symptoms among transgender adults. J Couns Psychol 2016; 63 (5): 509–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Gilbert PA, Pass LE, Keuroghlian AS, Greenfield TK, Reisner SL.. Alcohol research with transgender populations: a systematic review and recommendations to strengthen future studies. Drug Alcohol Depend 2018; 186: 138–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Frank J, Restar A, Kuhns L, et al. Unmet health care needs among young transgender women at risk for HIV transmission and acquisition in two urban U.S. cities: the lifeskills study. Transgend Health 2019; 4 (1): 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Morenz AM, Goldhammer H, Lambert CA, Hopwood R, Keuroghlian AS.. A blueprint for planning and implementing a transgender health program. Ann Fam Med 2020; 18 (1): 73–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cahill S, Singal R, Grasso C, et al. Do ask, do tell: high levels of acceptability by patients of routine collection of sexual orientation and gender identity data in four diverse American community health centers. PLoS One 2014; 9 (9): e107104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Grasso C, Goldhammer H, Funk D, et al. Required sexual orientation and gender identity reporting by US health centers: first-year data. Am J Public Health 2019; 109 (8): 1111–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Grasso C, McDowell MJ, Goldhammer H, Keuroghlian AS.. Planning and implementing sexual orientation and gender identity data collection in electronic health records. J Am Med Inform Assoc 2019;26 (1): 66–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ard KL, Keuroghlian AS.. Training in sexual and gender minority health: expanding education to reach all clinicians. N Engl J Med 2018; 379 (25): 2388–91. [DOI] [PubMed] [Google Scholar]
- 10. Furness BW, Goldhammer H, Montalvo W, et al. Transforming primary care for lesbian, gay, bisexual, and transgender people: a collaborative quality improvement initiative. Ann Fam Med 2020; 18 (4): 292–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Goldhammer H, Maston ED, Kissock LA, Davis JA, Keuroghlian AS.. National findings from an LGBT healthcare organizational needs assessment. LGBT Health 2018; 5 (8): 461–8. [DOI] [PubMed] [Google Scholar]
- 12. McDowell MJ, Goldhammer H, Potter JE, Keuroghlian AS.. Strategies to mitigate clinician implicit bias against sexual and gender minority patients. Psychosomatics 2020; 61 (6): 655–61. [DOI] [PubMed] [Google Scholar]
- 13. Grasso C, Goldhammer H, Brown RJ, Furness BW.. Using sexual orientation and gender identity data in electronic health records to assess for disparities in preventive health screening services. Int J Med Inform 2020; 142 :104245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Deutsch MB, Buchholz D.. Electronic health records and transgender patients–practical recommendations for the collection of gender identity data. J Gen Intern Med 2015; 30 (6): 843–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Deutsch MB, Green J, Keatley J, et al. Electronic medical records and the transgender patient: recommendations from the World Professional Association for Transgender Health EMR Working Group. J Am Med Inform Assoc 2013; 20 (4): 700–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. James S, Herman J, Rankin S, Keisling M, Mottet L, Anafi M.. The Report of the 2015 US Transgender Survey. Washington, DC: National Center for Transgender Equality; 2016. [Google Scholar]
- 17. Rosendale N, Goldman S, Ortiz GM, Haber LA.. Acute clinical care for transgender patients: a review. JAMA Intern Med 2018; 178 (11): 1535–43. [DOI] [PubMed] [Google Scholar]
- 18. Arellano-Anderson J, Keuroghlian AS.. Screening, counseling, and shared decision making for alcohol use with transgender and gender-diverse populations. LGBT Health 2020; 7 (8): 402–6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No new data were generated or analyzed in support of this manuscript.