Abstract
Objective
Mobile-based interventions have the potential to promote healthy aging among older adults. However, the adoption and use of mobile health applications are often low due to inappropriate designs. The aim of this systematic review is to identify, synthesize, and report interface and persuasive feature design recommendations of mobile health applications for elderly users to facilitate adoption and improve health-related outcomes.
Materials and Methods
We searched PubMed, Embase, PsycINFO, CINAHL, and Scopus databases to identify studies that discussed and evaluated elderly-friendly interface and persuasive feature designs of mobile health applications using an elderly cohort.
Results
We included 74 studies in our analysis. Our analysis revealed a total of 9 elderly-friendly interface design recommendations: 3 recommendations were targeted at perceptual capabilities of elderly users, 2 at motor coordination problems, and 4 at cognitive and memory deterioration. We also compiled and reported 5 categories of persuasive features: reminders, social features, game elements, personalized interventions, and health education.
Discussion
Only 5 studies included design elements that were based on theories. Moreover, the majority of the included studies evaluated the application as a whole without examining end-user perceptions and the effectiveness of each single design feature. Finally, most studies had methodological limitations, and better research designs are needed to quantify the effectiveness of the application designs rigorously.
Conclusions
This review synthesizes elderly-friendly interface and persuasive feature design recommendations for mobile health applications from the existing literature and provides recommendations for future research in this area and guidelines for designers.
Keywords: mobile application, user-centered design, interface design, persuasive features, healthy aging
INTRODUCTION
The aging population is increasing rapidly all over the world. The proportion of people aged 65 or above is expected to reach 12% and 23% worldwide by 2030 and 2100, respectively,1 which would put enormous pressure on health and social service systems.2 To alleviate this pressure, healthcare providers are considering designing mobile-based interventions to promote healthy lifestyles, support disease prevention and management, and improve access to health services.3 The global mobile health market was estimated at $35.1 billion in 2020 and is expected to increase to $145.7 billion by 2027.4 However, acceptance and continued use of mobile health (mHealth) applications are often low among the elderly, significantly plaguing their utility.5 One important reason is that most mHealth applications available in the market do not carefully consider the unique needs, preferences, and capabilities of elderly users, resulting in low usability.5,6
Compared with younger populations, older adults often face additional challenges in using mHealth applications due to limited perceptual, motor, and cognitive capabilities.7,8 In particular, the aging process will negatively affect visual and hearing abilities, hand-motor functions, and information processing capacity.9–12 Moreover, elderlies tend to experience reduced motivational orientation,6 further hampering the adoption and sustainable use of mHealth applications. Indeed, older adults will not adopt a technology if they do not perceive the benefits of using it.13
It is therefore essential to provide sufficient support for older adults when designing mHealth applications for them. Several review articles have focused on evaluating the benefits of mHealth applications for chronic disease management and healthy lifestyle promotion in older adults,14–17 and some have discussed practical challenges in application design.15,16,18 However, none of these reviews have compiled and reported mHealth application design recommendations for older adults. On the other hand, some articles have analyzed aging barriers for mHealth application usability and proposed several interface guidelines.6,19–21 However, these studies neither summarized the current evidence of the effectiveness of interface design nor investigated persuasive feature design. This review aims to address these gaps by identifying, synthesizing, and reporting recommended mHealth application designs that facilitate application adoption and promote healthy aging. Specifically, we seek to identify elderly-friendly interface designs that increase mHealth application acceptability and usability and persuasive features that increase adherence to the delivered mobile interventions.
METHODS
Data sources and searches
We followed the guideline of the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement.22 With the help of a librarian, 2 reviewers (JY and NL) searched PubMed, Embase, PsycINFO, CINAHL, and Scopus databases (Jan 01, 2010, to Apr 30, 2021) to identify articles with a focus on the design of mHealth applications for older adults. We chose 2010 as the start period because mHealth applications for older adults have only grown exponentially in the last decade.23
We searched the title and abstract of the articles using 3 groups of keywords that were combined using an AND operator: (a) mHealth application-related terms, (b) application design-related terms, and (c) older adult-related terms. The detailed search strategy can be seen in Supplementary Appendix A.
Study selection
We structured our inclusion and exclusion criteria based on the PICOS (Population, Interventions, Comparisons, Outcomes, Study) framework (see Table 1). Two members of the research team (JY, NL) independently screened the titles and abstracts of the retrieved articles and assessed the full texts of all potentially eligible studies against the inclusion criteria. Interrater reliability of the screening based on the title and abstract resulted in high agreement (Cohen’s kappa = 0.74), while the interrater reliability of the screening based on the full text resulted in moderate agreement (Cohen’s kappa = 0.67). Disagreements were resolved through group discussion with a third investigator (SST) until 100% agreement was achieved.
Table 1.
Inclusion and exclusion criteria based on the PICOS model
| Inclusion and exclusion criteria | |
|---|---|
| Population |
An older cohort. An older person can be defined as one whose chronological age is 60 years or above, or 65 years or above.24 In this review, we used 60 years as a more conservative threshold. |
| Interventions |
Any mHealth applications with any mobile devices, such as mobile phones and tablets. We excluded health-related interventions that only used mobile devices (eg, short messages), wearables, and smart home devices without mobile apps. |
| Comparisons | No specific comparisons were excluded. |
| Outcomes | Studies were excluded if they only described the design and development of mHealth applications without testing them using an elderly cohort. |
| Study designs | We restricted our search to English-written, peer-reviewed journal articles and excluded conference abstracts, non-human studies, theoretical articles, reviews, commentaries, editorials, proposal papers, and protocol papers. |
Data extraction and analysis
Two team members (JY, NL) extracted and synthesized information using a piloted data extraction form. Specifically, they individually extracted the following items: study characteristics (ie, participant characteristics, country, study design, mHealth application descriptions, and health domain), application design features (ie, user interfaces, persuasive features, theory), mobile interventions, comparison or control groups, evaluation outcomes (ie, end-user perceptions, health-related outcomes), and key findings. Disagreements were resolved through group discussion with another 2 investigators (HHT and KYN) until 100% agreement was achieved.
RESULTS
Study inclusion
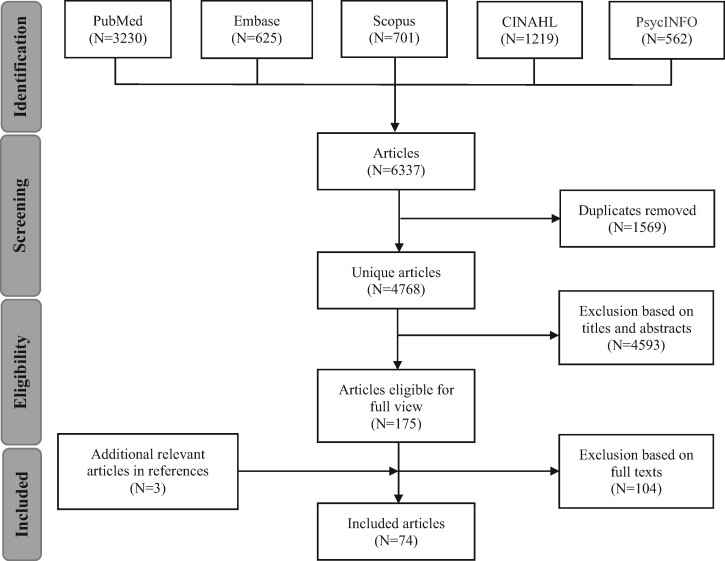
We identified a total of 6337 articles using the initial search strategy (Figure 1). We removed 1569 duplicate records using Endnote’s automatic duplication finder, leaving 4768 unique articles. After screening titles and abstracts, 175 articles were eligible for full-text review. We excluded 104 articles because the studies did not focus on mHealth applications or did not evaluate the applications with an elderly cohort, leaving 71 included articles. We included 3 studies identified through searching the reference lists of included studies. Thus, 74 articles were kept in the final analysis.
Figure 1.
Flowchart of the literature search and selection processes.
Study characteristics and quality
Table 2 presents details of study characteristics. All of the included studies enrolled participants aged 60 years or more. Four studies did not report participants’ gender. 38 studies did not reveal participants’ educational background, and 39 studies did not reveal their experience with mobile devices and digital technologies. Sample sizes ranged from 1 to 503, in which 46 studies had a sample size smaller than 30.
Table 2.
Study characteristics
| Study | Study design | Age (range, mean) | Gender (female) |
Education (college degree or higher) |
Computer-related experience | Sample size | Country | Application descriptions | Health domain |
|---|---|---|---|---|---|---|---|---|---|
| Disease prevention and self-management (N = 28) | |||||||||
| Alsswey et al25 | Quantitative research (Survey) |
60+, Mean (M): not reported. |
15.70% | 23.90% | All had at least 1 year of experience in using mobile applications. | 134 | Not reported | A mobile app designed to manage physical health needs for Arab elderly users (eg, medication-related information and instructions) | Medication adherence |
| Alvarez et al26 |
Quantitative research (Pilot study: usability study, feasibility study) |
Usability: 65+, M = 73.2; Feasibility: 65+, M = 76 |
Usability: 67.6%; Feasibility: 59.5% |
Usability: 9 years of education; Feasibility: 10.53 years of education |
Usability: 32.3% had previous experience with technology. | Usability: 34; Feasibility: 62 | Chile | A mobile app that provides interventions to prevent delirium for bedside use for hospitalized elderly patients | Delirium prevention |
| Bakogiannis et al27 | Quantitative research (Usability study, pilot study) |
Usability: M = 64.9; Pilot: M = 68.7 |
Usability: 21%; Pilot: 13% |
Not reported. | Not reported. |
Usability: 14; Pilot: 30 |
Greece | ThessHF app, a mobile app that supports heart failure self-care for elderly patients with heart failure | Heart failure self-management |
| Balsa et al28 | Quantitative research (Usability study) | 67–80, M = 70.91 | 72.2% | 63.6% | Not reported. | 11 | Portugal | VASelfCare, a mobile-based intelligent assistant (in the form of an anthropomorphic virtual assistant) that supports older adults with Type 2 Diabetes Mellitus (T2DM) in medication adherence and lifestyle changes | T2DM self-management |
| Baric et al29 |
Qualitative research (Focus groups) |
66–85, M = 73 | 45% | 40% | 55% had daily or weekly computer use; 85% had daily or weekly phone use. | 20 | Sweden | RemindMe, an interactive digital calendar that provides active reminders for senior people with cognitive impairment | Cognitive impairment self-management |
| Chen et al30 |
Qualitative research (Usability study) |
64 | 100% | Not reported. | Not reported. | 1 | China | Win-Win aSleep (WWAS), a mobile app to assist cognitive behavioral therapy for older adults with insomnia | Insomnia self-management |
| Chen et al31 |
Quantitative research (Pre-post intervention study) |
60+, M = 86.68 |
77% | Not reported. | Not reported. | 57 | Hong Kong | Lok Chi, a home-based tablet-based intervention designed to improve cognitive and emotional health for community-dwelling older adults with mild cognitive impairment (MCI) | MCI self-management |
| Chung et al32 |
Quantitative research (Pre-post intervention study) |
65–78, M = 71.56 |
100% | 0% |
38 had Android smartphones; 2 had feature phones on which mobile apps were not available. |
40 | South Korea | MIND MORE, a mobile app for insomnia self-management in community-dwelling older adults | Insomnia self-management |
| Cunningham et al33 | Quantitative research (Cohort study) | 69–97, M = 84.6 | 64% | Not reported. | Not reported. | 14 | United Kingdom | Memory Tracks, a music mobile platform that provides song-task association training for elderly people with dementia | Dementia self-management |
| Djabelkhir et al34 |
Quantitative research (RCT) |
60+, M = 79 |
60%–70% | 44.4%–60% | Not reported | 14 | France | Two tablet-based cognitive training apps (cognitive stimulation, cognitive engagement) for elderly patients with MCI | MCI self-management |
| Fortuna et al35 | Quantitative research (Feasibility study) |
60+, M = 68.8 |
87.50% | 12.50% | 62.5% had smartphones. | 8 | United States | PeerTECH, a tablet-delivered psychiatric self-management intervention for older adults with mental illnesses | Psychiatric self-management |
| Hackett et al36 |
Quantitative research (Pilot study, within-subject, cross-over experiment) |
65+, M = 80.3 |
70% | Not reported. | Participants were able to use computers and had positive attitudes toward computers. | 10 | United States | SmartPrompt, a mobile reminder app for older adults with dementia and MCI | Self-management of dementia and MCI |
| Holden et al37 | Quantitative research (Usability study) | 60–85, M = 67.6 | 61.00% | 23.00% | Some participants had never used a smartphone before. | 23 | United States | Brain Buddy, a mobile app to reduce unsafe medication use by older adults | Medication use |
| Jongstra et al38 |
Quantitative research (RCT) |
65+, M = 69 |
56% | 29% | Not reported. | 41 | Finland, France, The Netherlands | An interactive counseling platform for healthy aging (ie, cardiovascular risk profiling and prevention) | Cardiovascular diseases prevention |
| Jung et al39 |
Qualitative study (Usability study, interviews) |
65–80, M: not reported. |
78.57% | 57.14% | All participants had experience with smartphones. | 14 | United States | FRADA, a food record app that provides dietary assessments for older adults with Type 2 Diabetes | Diabetes self-management |
| Kim et al40 |
Mixed methods research (Pilot study) |
65+, M = 75.7 |
91% | 18.2% | Participants had 3.5 years of smart device usage experience on average. | 11 | South Korea | 365 Healthy Swallowing Coach, a mobile app that delivers swallowing training for elderly dysphagia patients | Swallowing training |
| Loh et al41 |
Mixed methods research (Pilot study) |
68–87, M = 76.8 | 17% | 67% | 44% (17%) had access to a mobile phone (a tablet or iPad). | 18 | United States | TouchStream, a mHealth app that provides geriatric assessment-driven interventions for older adults with cancer | Cancer treatment |
| Madill et al42 | Quantitative research (Usability study) |
60+, M = 75.5 |
23.30% | Not reported. | Not reported. | 30 | United States | “Take Back Your Back”, an iPad-based educational tool for older adults with chronic lower back pain | Back pain treatment |
| Manca et al43 | Quantitative research (Between-subject experiment) |
69–84, M = 75.3 |
64.3% | 7.14% | 50% were familiar with technologies and devices. | 14 | Italy | A music-based game (robot version and tablet version) for older adults with MCI | MCI self-management |
| Manera et al44 |
Quantitative research (Pilot study) |
60–90, M = 78.3 | 71% | Not reported. | Not reported. | 21 | Not reported. | “Kitchen and cooking”, a tablet-based serious game for elderly people with MCI and Alzheimer’s Disease (AD) | Self-management of MCI and AD |
| Mertens et al45 | Quantitative research (Crossover design) |
60+, M = 73.8 |
50% | 25% | 16.7% expert in computer literacy | 24 | Germany | Medication Plan, a mobile app designed to improve therapy adherence for elderly patients undergoing rehabilitation | Rehabilitation self-management |
| Mira et al46 |
Quantitative research (RCT) |
65+, M = 72.9 |
Not reported. | Not reported. | 45% had smartphone experience. | 99 | Spain | ALICE, a tablet-based app for medication self-management | Medication self-management |
| Portz et al47 |
Quantitative research (Pilot study) |
60+, M = 66 |
60% | Not reported. | Not reported. | 30 | United States | HF app, a mobile app that tracks heart failure symptoms in elderly users | Heart failure self-management |
| Puig et al48 |
Quantitative research (RCT) |
60+, Median = 66 |
28% | Not reported. | Not reported. | 100 | Finland | +Approp, a mobile app for HIV prevention and self-management for older HIV-infected patients | HIV prevention and self-management |
| Quinn et al49 |
Quantitative research (Pilot study) |
65+ M = 70.3 |
57% | Not reported. | 71.4% had Internet at home. | 7 | United States | Patient coaching system (PCS), a mobile software for diabetes management for older adults | Diabetes management |
| Reading Turchioe et al50 | Quantitative research (Feasibility study) |
60+, M: not reported. |
37% | 47% | 30.4% did not have a computer and 26.2% did not have the internet. | 168 | United States | mi.Symptoms, a mobile app that facilitates symptom reporting and patient outcome reporting in older adults | Chronic disease self-management |
| Scase et al51 |
Qualitative research (Focus groups) |
65–80, M = 75.0 | 88% | Not reported. | Not reported. | 25 | United Kingdom | 4 tablet-based cognitive games (ie, “Find it,” “Match it,” “Solve it,” and “Complete it”) for older adults with mild cognitive impairment | MCI self-management |
| Sun et al52 |
Quantitative research (RCT) |
66–72 M = 68 |
59.34% | Not reported. | Not reported. | 91 | China | A mobile-based telemedicine app for T2DM self-management for older adults | T2DM self-management |
| Physical and cognitive function improvement (N = 27) | |||||||||
| Albergoni et al53 |
Quantitative research (Pilot study) |
70–78, M = 73.8 |
40% | Not reported. | Not reported. | 10 | The Netherlands | PACE, a mobile app that visualizes user adherence to physical activity programs | Physical activities |
| Baez et al54 |
Quantitative research (RCT) |
65–87, M = 71.5 | 70%–75% | Not reported. | Not reported. | 40 | Italy | Gymcentral, a tablet-based app for home-based online group exercises under the supervision of a human coach | Home-based exercises |
| Bergquist et al55 |
Mixed methods research (Usability study) |
60–80, M = 66.4 | 48% | Not reported. | 83% had mobile experience. | 343 | Norway, Germany, The Netherlands | 3 mobile apps that deliver physical function self-tests (ie, Self-TUG, Self-STS, Self-Tandem) for older adults | Physical function self-tests |
| Compernolle et al56 |
Mixed methods research (Usability study) |
60–76, M = 64.3 | 54% | 57% | Not reported. | 28 | Belgium | Activator, a mobile self-monitoring tool designed to reduce older adults’ sedentary behavior | Sedentary behavior change |
| Daly et al57 |
Quantitative research (Pilot study) |
65–81, M = 70 |
50% | 60% | Not reported. | 20 | Australia | PhysiApp, a tablet-based app that delivers tailored, home-based exercise programs for community-dwelling older adults | Home-based exercises |
| Dekker-van Weering et al58 |
Quantitative research (RCT) |
65–75, M = 70.2 | 61.1% | 8.3% | Not reported. | 36 | The Netherlands | A tablet or computer-based portal that provides home-based exercise programs for pre-frail older adults | Physical activities |
| Delbaere et al59 |
Quantitative research (RCT) |
70+, M = 77.4 |
67.4% | Not reported. | 85% (88.4%) in the intervention (control) group owned computers. | 503 | Australia | StandingTall, a tablet-based mobile app that delivers home-based, balance exercises to older adults | Balance exercises |
| Geerds et al60 | Mixed methods research (Usability study) | M = 80.5 | 71.80% | Not reported. | 93.8% had more than 5 years of smartphone experience. | 48 | The Netherlands | A mobile app designed to monitor postoperative functional recovery after hip fracture | Functional recovery after hip fracture |
| Geraedts et al61 | Quantitative research (Feasibility study) |
70+, M = 81 |
62.5% | Not reported. | 62.5% had computer experience; 2.5% had a smartphone. | 21 | The Netherlands | A tablet-based app that provides home-based exercise programs for pre-frail old adults | Home-based exercises |
| Haeger et al62 | Quantitative research (Feasibility study, controlled trial) |
70+, M = 76.5 |
50% | Not reported. | Not reported. | 10 | Germany | MIT App Inventor 2, a mobile app that plans trips in hometowns to increase mobility in older adults | Mobility |
| Harte et al63 | Mixed methods research (Usability study) |
61–85, M: not reported. |
Not reported. | Not reported. | Not reported. | 12 | Ireland | A mobile app that integrates fall risk detection for older adults | Fall risk detection and fall prevention |
| Hawley-Hague et al64 | Qualitative research (Usability study, focus groups, interviews) | 64–92, M = 77.1 | Not reported. | Not reported. | Not reported. | 7 | United Kingdom | Two mobile apps that support falls rehabilitation exercises (ie, My Activity Programme for patients, Motivate Me for professionals) | Fall rehabilitation exercises |
| Hill et al65 | Mixed methods research (Feasibility study) |
60+, M = 78.8 |
78% | 56% | Not reported. | 9 | United States | A tablet-based attention training app designed to improve cognitive functioning in older adults | Cognitive training |
| Hill et al66 | Mixed methods research (Usability study) |
60+, M = 79 |
58% | 50% | Not reported. | 12 | United States | A modified tablet-based attention training app designed to improve cognitive functioning in older adults | Cognitive training |
| Hsieh et al67 | Mixed methods research (Usability study) |
70+, M = 80.3 |
81.8% | 27.2% | 54.5% used tablets and 81.1% used smartphones. | 11 | United States | Steady, a mobile app for fall risk screening for older adults | Fall risk screening and prevention |
| Kang et al68 |
Quantitative research (Pre-post experiment) |
65–75, M = 70 |
50% | Not reported. | Not reported. | 4 | South Korea | A mobile app that provides exercise suggestions for older adults with chronic disorders | Exercise suggestions |
| Kwan et al69 |
Quantitative research (RCT) |
60+, Median = 71 | 85.00% | Not reported. | Not reported. | 33 | Hong Kong | Samsung Health, a mobile app that monitors walking behaviors | Walking activities |
| Li et al70 |
Quantitative research (Pre-post between-subjects experiment) |
65+, M = 71.3 |
70% | Not reported. | Not reported. | 30 | Singapore | 5 exergames (ie, Skiing, Hiking, Pikkuli, Chinatown Race, RehaMed Volleyball) that promote physical activities in older adults | Physical activities |
| Li et al71 |
Quantitative research (RCT) |
60+, M = 79.3 |
19.4% | 4.6 years on average | Not reported. | 31 | Hong Kong | Caspar Health e-system and a mobile app designed to provide occupational therapy rehabilitation for elderly outpatients after hip fraction surgery | Physical and functional ability |
| Mehra et al72 | Mixed methods research (Usability study) |
69–99 M: not reported. |
73.3% | Not reported. | Not reported. | 15 | The Netherlands | VITAMIN app, a tablet-based app that supports older adults in home-based exercises | Exercise training |
| Pettersson et al73 | Qualitative research (Feasibility study) |
70+, M = 76 |
52.6% | Not reported. | 71% (72%) had access to tablet/smartphone (computer). | 28 | Sweden | Safe Step, a mHealth app that supports self-managed exercises and behavior changes for older adults with impaired balance | Self-managed exercises and behavior changes |
| Shake et al74 |
Quantitative research (RCT) |
65+, M = 73.4 |
86% | 20% | Not reported. | 105 | United States | Bingocize, a mobile game app designed to provide exercise and health education for older adults | Exercises and health education |
| Silveria et al75 |
Quantitative research (Pre-post intervention study) |
65+, M = 75.2 |
64% | 54.% had trades or professional diploma | 52.3% frequently used cellphones; 68.2% used computers; 59.1% used the Internet. | 44 | Switzerland | ActiveLifestyle, a tablet-based app that delivers home-based strength-balance training to independently living older adults | Strength-balance training |
| Tabak et al76 | Mixed methods research |
65–75, M = 71 |
50% | Not reported. | 40% had daily technology use. | 20 | United States | WordFit, a game-based mobile coaching app that stimulates daily physical activities among older adults | Physical activities |
| Taylor et al77 |
Quantitative research (Feasibility study) |
60+, M = 83 |
53.3% | 11 years of education on average | 33% owned a computer, 20% used a computer. | 15 | Australia | StandingTall, a tablet-based app that delivers tailored exercise programs to elderly people with dementia | Exercise programs |
| Van Het Reve et al78 |
Quantitative research (Pre-post intervention study) |
65+, M = 75 |
63.6% | 13.6% | Not reported. | 44 | Switzerland | ActiveLifestyle, a tablet-based app that delivers strength-balance training to independently living older adults | Strength-balance training |
| Zhong and Rau79 |
Quantitative research (Usability test, mixed design experiment) |
60–90, M = 69.8 | 73% | 18.9% | 73.6% had a smartphone and 60.1% had Internet access. | 148 | China | Pocket Gait, a mobile app designed to provide gait assessment and fall prevention for older adults | Fall prevention |
| Social inclusion and well-being (N = 6) | |||||||||
| Chi et al80 |
Mixed methods research (Pilot study) |
68–89, M = 78.3 |
100% | Not reported. | 70% felt comfortable using technology. | 10 | United States | Digital Pet, a tablet-based conversational agent in the form of an avatar for older adults | Social connectedness |
| Goumopoulos et al81 |
Mixed methods research (Pilot study) |
60+, M = 65.7 |
59% | Not reported. | Not reported. | 22 | Greece | Senior App Suite, a mobile app designed to improve the social well-being and independence of senior people | Social connectedness |
| Jansen-Kosterink et al82 |
Quantitative research (Usability study) |
60+, M = 73.4 |
80% | 41% | 22%, 66%, and 12% of participants had positive, neutral, and negative attitudes toward technology. | 91 | The Netherlands | GezelschApp, a mobile app that encourages social participation in community-dwelling older adults | Social connectedness |
| Judges et al83 | Mixed methods research | 68–92, M = 80.6 | 70% | Not reported. | Most of them had no experience with computers. | 10 | Canada | InTouch, a tablet-based communication app that reduces loneliness and social isolation in the elderly | Social connectedness |
| Neves et al84] | Mixed methods research (Feasibility study) | 74–95, M = 82.5 | 66.7% | Not reported. | Digital literacy: 4 (no); 3 (low); 5 (medium). | 12 | Canada | InTouch, a tablet-based communication app that reduces loneliness and social isolation in the elderly | Social connectedness |
| Similä et al85 | Mixed methods research (Feasibility study) | 66–82, M = 73 | 100% | Not reported. | 5 participants had Internet access; 4 had used a computer in the previous year; 1 had used a smartphone or tablet. | 7 | Finland | Oiva, a mobile app that provides mental wellness training for older adults | Mental wellness training |
| Healthy dieting (N = 5) | |||||||||
| Aure et al86 | Qualitative research (Interviews) | 68–95, M = 81 | 66.7% | Not reported. | 44.4% had experience with touch technology (eg, tablet, smartphone). | 18 | Norway | Appetitus, a mobile nutrition app that supports weight gain or weight maintenance for older adults | Self-monitoring of dieting |
| Aure et al87 |
Mixed methods research (Feasibility study) |
68–95, M = 79.48 |
72% | Not reported. | 40% had experience using tablet or smartphone; 48% used the Internet daily, 16% used Internet weekly, and 36% never used Internet. | 25 | Norway | Appetitus, a mobile nutrition app that supports weight gain or weight maintenance for older adults | Self-monitoring of dieting |
| Farsjø and Moen88 |
Qualitative research (Pilot study, focus group) |
69–76 M: not reported. |
100% | Not reported. | Not reported. | 4 | Norway | APPETITT, a tablet-based app designed to prevent malnutrition and weight loss in the elderly | Guidance for dieting |
| Franco et al89 | Quantitative research (Usability study) |
60–85 M: not reported. |
79.60% | 74.38% | Not reported. | 50 | United Kingdom | eNutri, a mobile app that provides graphical food frequency assessment for older adults | Healthy dieting |
| Liu et al90 |
Quantitative research (RCT) |
60–90, M = 73.9 | 79% | 58% | 68% had used mobile phones or tablets; 7% had used nutrition-related apps. | 57 | Taiwan | Two mobile apps (ie, voice-only reporting, voice-button reporting) for food intake reporting for elderly people | Food intake reporting |
| Health monitoring and health concern reporting (N = 5) | |||||||||
| Algilani et al91 |
Mixed methods research (Feasibility study) |
67–90, M = 77 |
62.50% | Not reported. | Not reported. | 8 | Sweden | A tablet-based app for early assessment and management of elderly patients’ reported concerns | Health concern reporting |
| Göransson et al92 | Qualitative research (Interviews) |
65+, M = 86 |
64.7% | 23.5% | Not reported. | 17 | Sweden | A mobile app designed to report health concerns | Health concern reporting |
| Göransson et al93 | Quantitative research (Quasi-experimental study) |
65+, M = 86 |
64.7% | 23.5% | Not reported. | 17 | Sweden | A mobile app designed to report health concerns | Health concern reporting |
| Göransson et al94 | Quantitative research (Quasi-experimental study) |
65+, M = 86 |
64.7% | 23.5% | Not reported. | 17 | Sweden | A mobile app designed to report health concerns | Health concern reporting |
| Quinn et al95 | Quantitative research (Usability study) |
65+, M = 77.8 |
66.7% | 100% | 25% are skillful with technology and electronics. | 12 | United States | A mobile app designed to improve engagement of the patient-informal caregiver team | Health recording and monitoring |
| General (provides more than 1 type of functions) (N = 3) | |||||||||
| Bott et al96 | Quantitative research (Quasi-experiment) |
65+, M: Not reported. |
54.7% | 19% had less than high school education | Not reported. | 95 | United States | A tablet-based conversational agent (embodied in the form of an animated avatar) designed to provide psychosocial and health care support for hospitalized patients | Social inclusion; delirium prevention; fall prevention |
| Stal et al97 | Quantitative research (Within-subject experiment) | 65+, M = 72.2 | 35% | 50% | Not reported. | 20 | The Netherlands | A conversational agent, which is embedded in a frailty assessment app and provides training in healthy nutrition, physical health, cognitive health for older adults | Healthy dieting; physical and cognitive function improvement |
| Steinert et al98 | Quantitative research (Usability study) | 61–76, M = 68 | Not reported. | Not reported. | None of the participants had smartphone experience. | 30 | Germany | MyTherapy, a mobile app that helps older adults achieve health-related goals | Diverse health-related goals |
Of the 74 included studies, a variety of quantitative (N = 47), qualitative (N = 9), and mixed-methods designs (N = 18) were used to evaluate mHealth applications (see Table 1 for details). We further assessed the quality of the 12 RCT studies based on the Cochrane Risk of Bias Assessment Tool (see Supplementary Appendix B for details).99 Nine studies reported random sequence generation.46,48,52,54,59,69,71,74,90 Only 3 studies explicitly stated that the allocation was concealed.54,59,69 Only 2 studies were double-blinded,54,74 and 1 study was blinded to neither researchers nor participants.71 Using 80% completed participants as a threshold, 7 studies had a low risk of incomplete outcome data.34,46,54,58,69,74,90 One study had a high risk of selective reporting bias.38 Nine studies suffered from other sources of bias, such as a small sample size,34,46,48,52,54,58,69,71 a biased sample,54,59,71,90 and a lack of baseline data.54
The mHealth applications described in the 74 included studies were mainly designed for disease prevention and self-management (N = 28), physical and cognitive function improvement (N = 27), social inclusion and well-being (N = 6), healthy dieting (N = 5), and health monitoring and reporting (N = 5). The remaining 3 articles covered more than 1 health domain, such as using a conversational agent to offer training modules for healthy dieting, physical health, and cognitive health.97
Evaluation outcomes for design effectiveness
The mHealth application designs were mainly assessed along 2 dimensions: end-user perceptions and health-related outcomes (see Supplementary Appendix C for details). Examples of end-user perceptions included usability, feasibility, acceptability, adherence, compliance, engagement, satisfaction, adoption and use, and other self-reported usage experience such as facilitators, barriers, and suggestions for future improvement. On the other hand, health-related outcomes included health-related behavior changes, physical and cognitive functions, psychosocial and emotional well-being, quality of life, and health knowledge.
Recommendations for interface designs
Our analysis identified a total of 9 elderly-friendly interface design recommendations (see Box 1). We grouped these designs into 3 categories based on the addressed needs of elderly users: perceptual limitations, motor coordination problems, and cognitive and memory deterioration.
Box 1. Recommended interface designs
Vision impairment
Font design
Large font size
Use Sans Serif family font style (eg, Arial, Verdana)
Use bold font for key points
Avoid special font styles (eg, italics, underline, all caps)
Enable users to customize the font and text properties
Color choice
-
Ensure high contrast (eg, use dark texts on a light interface background, use differentiated button color from the interface
background)
Limit number of colors
Use basic and distinctive colors
Use consistent background colors
Use culturally appropriate colors (eg, use Arabic basic colors for Arabian users)
Color coding of buttons
Provision of audio alternatives
Provide audio options
Ensure loud audio volume
Add vibrations during each auditory tone
Motor coordination problems
Gestural interactions
Use simple touchscreen gestures (eg, swiping, tapping, dragging, dropping)
Avoid complex touchscreen gestures (eg, scrolling, zooming)
Use large and structured buttons
Minimize text entry
Support voice control
Button-only interface (eg, use buttons and sliders to answer questions)
Cognitive and memory deterioration
Simple and consistent layout
Provide a simple and consistent layout
Ensure adequate white space between lines and buttons
Adaptive layout based on the screen size
Avoid large blocks of texts
Avoid texts over images
Use culturally appropriate layout (eg, use right to left reading for Arabian users)
Simple and clear navigation
Flat navigation structure
Place main functions in the home screen
Reduce menu options
Provide a clear return button and a static menu on every page
Multimedia presentation
Present information in the form of texts, pictures, and videos
Easy-to-understand content
Use labeled buttons
Organize related topics into groups
Use age-appropriate and common languages
Perceptual limitations
Font design
Fifteen studies emphasized the importance of font design to improve application readability.25,37–39,41–43,46,50,53,63,67,81,86,87 One often-mentioned design aspect is using large font size.25,38,39,41–43,46,50 For example, Goumopoulos et al81 recommended using a font size of 36 to 48 points on mobile phones. Other specific font design recommendations included using Sans Serif family font style,67,81using bold font for key points,53avoiding special font styles,53 and enabling users to customize font and text properties.53
Color choice
Designers emphasized the importance of choosing an appropriate color to cater to older adults. One suggestion is to ensure high contrast to enhance the content readability for the aging population, such as using dark texts on a light interface background.26,40,43,46,50,51,67,81,86 Another suggestion is to keep it simple, such as limiting the number of colors,29,43using basic and distinctive colors,38using consistent background colors,81 and using culturally appropriate colors.25 Finally, it is suggested to employ color-coding, such as assigning appropriate and unique colors for each button.27,33,43,50,53,63,66,88,91 For example, Harte et al63 used red for the “I have fallen” button and green for the “I am OK” button.
Audio alternatives.
Applications should provide audio alternatives to ease the burden on vision-impaired elderly users. One suggestion is to read out texts to avoid misinterpretation and ensure accessibility to elderly users.28,62,81 Designers can also use loud audio volume and add vibrations during each auditory tone for older adults with hearing difficulty.55,67
Motor coordination problems
Gestural interactions
Gestural interactions represent how elderly users interact with applications via a set of touchscreen gestures. One design guideline is to use simple gestures (eg, tapping) and avoid complex ones (eg, scrolling, zooming).26,37,39,47,63,80,84 In one study, elderly users perceived tapping to be easier than swiping and hence preferred to use a tap-only interface than an interface that supported both tapping and swiping.84 Another guideline is to use large and structured buttons to facilitate user interactions with applications.38–40,43,61,63,67,83,86,87,90 However, no study has specified appropriate button sizes. Prior human-computer interaction (HCI) studies have suggested using rectangle buttons larger than 15.9 × 9.0 mm and square buttons between 16.51 mm and 19.05 mm square to facilitate user interactions.100,101
Minimize text input
Text input can be challenging for motor-impaired elderly users. Specific strategies to reduce text input include supporting voice control,80,81,96 and using a button-only interface.27,47 For example, Goumopoulos et al81 supported voice commands to facilitate elderly users with motor skill problems to interact with the mHealth application.
Cognitive and memory deterioration
Simple and consistent layout
Layout refers to the location of data elements on the application interface. It is crucial to provide a simple and consistent layout so that elderly users could easily process and comprehend the application content.36,38,52,65,81,90 Specific layout design suggestions include ensuring adequate white space,26,40,81adapting layout based on the screen size ,89avoiding large blocks of texts,81avoiding texts over images,81 and using a culturally appropriate layout.25
Easy navigation
Navigation design describes how to guide users through an application via a set of predefined steps. Overall, designers suggested keeping the navigation structure simple and straightforward, such as using a flat navigation structure,29,40,50,55,89placing main functions in the home screen,86reducing menu options,61 and providing a clear return button and a static menu on every page.38
Multimedia presentation
Multimedia presentation describes an application interface that presents information in the form of texts, images, and videos. This practice is strongly recommended by several studies because multiple sensory cues could effectively ease the information processing for older adults by providing sensory awareness.35,46,50,55,58,66,70,85,87
Easy-to-understand content
Finally, it is important to ensure that the application content is easy to understand for elderly users. For example, designers suggested using labeled buttons so that users could easily comprehend the functionality of each button.25,40,63 Other suggestions include organizing related topics into groups,81 and using age-appropriate and common languages.25,51,70,81
Recommendations for persuasive feature designs
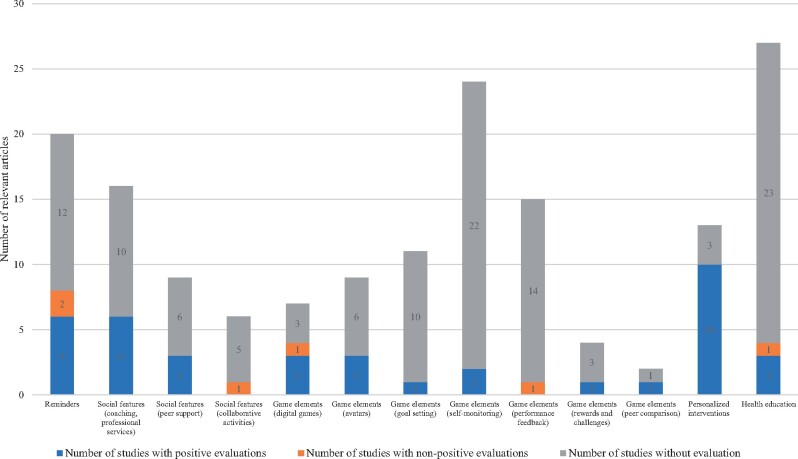
We have also identified 5 categories of persuasive features that provided motivational affordance for older adults to adhere to mobile-based interventions: reminders, social features, game elements, personalized interventions, and health education (see Figure 2 and Supplementary Appendix D).
Figure 2.
Summary of persuasive features.
Reminders
Twenty articles included reminders as part of their mobile interventions to remind elderly users to complete important daily tasks such as appointment and event scheduling, physical activities, nutrition and water intake, and medication intake.27,29,34–36,38,41,45,46,48,52,57,69,78,80,81,88,91,98,102 Among these studies, 2 studies found that older adults appreciated reminders and reported that reminders provided a sense of modernity, independence, and control in task completion.29,46 Another study examining a HIV prevention and self-care application found that medication reminder was one of the most frequently used features among elderly users.48 In contrast, Farsjø and Moen88 found that meal notifications of a nutrition application did not work as expected, and only one user paid attention to this feature. Also, Loh et al41 revealed that reminders of a mobile-based geriatric assessment-driven intervention were not useful for 3 elderly patients who already had an appointment and medication tracking system. On the other hand, 4 studies examined the impacts of reminders, and the results were mixed.36,41,45,98 Specifically, Mertens et al45 found that reminders of the Medication Plan app significantly improved medication recording adherence. Hackett et al36 showed that a reminder application improved the the completion of the Remember to Drink tasks for older adults with dementia and mild cognitive impairment.36 In contrast, the other 2 studies suggested that reminders alone may be inadequate to promote behavioral changes. Loh et al41 found that reminders were effective at improving medication adherence but not physical activities. Likewise, reminders increased medication adherence and fish and water intake, but not physical activities and social communication with friends and relatives.98
Social features
The fulfillment of psychological and social needs is essential when designing mHealth applications. The most commonly used social feature is coaching or professional care services (N = 16).34,38,41,42,54,57,58,61,62,69,72,78,81–84 Six out of the 16 studies reported positive end-user perceptions of this feature.38,42,54,61,78,86 For example, Jongstra et al38 found that elderly participants enjoyed discussing their lifestyle goals with coaches and appreciated their support. Moreover, Van Het Reve et al78 examined the messages sent and received on a strength–balance training app and found that most interactions occurred between caregivers and participants rather than between participants.
Second, 8 studies incorporated peer support by enabling users to communicate, interact and network with peer users.35,38,75,78,81–84 In particular, 1 study examining Senior App Suite showed that elderly users were satisfied with the social networking service and used it 3 times per week on average.81 Further, 2 studies evaluated the effectiveness of InTouch, a mobile application that supports multi-modality messages (ie, audio, wave, picture, and video messages) to increase social connectedness. They found that messages brought positive communication and relationship changes among elderly users.83,84 They further noted that audio messages were the easiest to use and were used most frequently, whereas wave messages were perceived as useless and were used the least.
Third, 6 studies introduced collaborative activities such as group-based online exercises,54,75,78 collaborative digital games,62,75,78 offline group discussions ,34 and offline social activities.82 Only 1 study examined the effect of collaborative activities, and the results were not encouraging.34 It designed mobile-based interventions for cognitive training that involved offline group discussions and social interactions. It showed that although elderly participants created social ties throughout the training intervention, they did not experience an improvement in cognitive and psychosocial outcomes.
Finally, 3 studies evaluated the impact of social features as a whole.54,75,78 Specifically, Baez et al54 examined the effects of tablet-based online group exercises and found that there were no significant differences in social well-being outcomes between the group training group and the individual training group. The other 2 studies compared two exercise training interventions delivered by ActiveLifestyle application (ie, an individual version and an social version) against a control group using training plans on paper sheets.75,78 Van Het Reve et al78 found that both individual and social groups had improved gait and physical performance compared with the control group. Silveira et al75 found that social features were more effective at stimulating training compliance and healthy behavior changes. They further noted that 83% of participants felt motivated by external monitoring, followed by emotional support (75%) and collaborative games (58%).
Game elements
Seven studies employed digital games to promote healthy aging.26,31,43,51,70,74,76 The evaluation results were mixed.43,51,70,74 For example, Shake et al74 evaluated Bingocize, a serious game for exercising and health education, and found that it improved quality of life in older adults by improving physical and cognitive performance. In contrast, Li et al70 designed and assessed 5 exergames among community-dwelling older adults. They found that although the exergames brought exercise enjoyment, they failed to improve self-efficacy, reduce loneliness, and improve life satisfaction.
We also analyzed specific game elements from the included articles, such as avatars (N = 9),28,38,44,51,54,74,80,96,97 goal-setting (N = 11),38,59,64,69,72,75–78,86,97 self-monitoring and tracking (N = 25),27,30,32,38,40,41,46,48–50,52,54,56,57,69,70,75,76,79,86–88,91,95,97 performance feedback (N = 16),40,43,53,54,61,62,65,66,69–71,86,87,92–94 reward and challenges (N = 6),27,36,65,66,74,75 and peer competition (N = 2).69,75 Regarding avatars, Chi et al80 examined a human-operated conversational agent embodied in a dog or cat avatar. Overall, elderly participants felt comfortable with the agent, even though they felt worried that their social interactions might be adversely affected if their emotional attachment to the avatar became too strong. Bott et al96 investigated the impact of a relational conversational agent in the form of an animated avatar and found that hospitalized patients who received the avatar had lower incidences of delirium, loneliness, depression, and falls than control patients. Finally, Stal et al97 compared user preferences of two embodied conversational agent appearances for health assessments (ie, an older male agent and a young female agent) and found that elderly users did not perceive an added value of the agent. Regarding other game elements, Aure et al86 found that the most regularly used feature of the Appetitus application was the self-monitoring dietary function. Silveira et al75 reported that 67% of elderly participants of ActiveLifestyle application felt motivated by the goal-setting and self-monitoring features, followed by positive and negative reinforcement via rewards and praises (50%), and the peer performance comparison feature (42%). Two studies examining an attention training application revealed that elderly users appreciated working through challenges and perceived negative feedback as distracting and frustrating.65,66
Personalized interventions
Thirteen studies provided personalized interventions to motivate elderly users to participate in health-promoting programs, such as physical and cognitive training, nutrition advice, therapy, and rehabilitation.34,35,41,54,57–59,64,68,71,73,77,89 Of these, 10 studies investigated the effectiveness of the personalized interventions as a whole with promising results.34,35,41,54,57–59,68,71,77 For example, Loh et al41 provided a tailored mobile intervention to support elderly cancer patients and found that the intervention was effective at decreasing symptom severity and health care utilization. The remaining 3 studies did not examine the intervention's effectiveness.64,73,89
Health education
27 studies provided education on various health topics to older adults.25–27,32,35,37,38,41,42,48,52,59,67–69,72–75,82,87,91–94,96,97 Shake et al74 examined the efficacy of a health education program that covered fall risks and osteoarthritis and found that elderly users’ health knowledge of the two topics increased over time. Hsieh et al67 reported that elderly participants perceived a fall risk mHealth application to be useful in learning their risk of falling. Sun et al52 assessed a diabetes self-management app and found that elderly users had improved self-management skills and knowledge of diabetes. In contrast, Algilani et al91 investigated the feasibility of a mHealth application for early assessment and management of patient-reported concerns. The results revealed that some users provided positive opinions regarding the self-care advice, whereas others failed to appreciate its usefulness and availability. The remaining studies did not report the benefits of their education feature.
DISCUSSION
Our review provided specific and actionable mHealth application design recommendations to develop elderly-oriented interface and persuasive features. We classified the included studies into 3 categories based on the design aspects. Category I includes 43 studies that proposed interface design recommendations to cater to the perceptual, motor, and cognitive deterioration of older adults. Category II contains 66 studies that incorporated persuasive features to provide motivational affordance toward healthy behavior changes. In contrast, Category III includes 37 studies that discussed both elderly-friendly interface and persuasive feature designs. Category III studies are particularly important because appropriate interface designs could reduce users’ confusion and frustration and thus improve application acceptability and usability, while persuasive features could motivate elderly users to adherence to mobile interventions and improve health outcomes. Future work in this field should consider both application design aspects based on our derived recommendations to assist older adults in achieving healthy aging.
We found that 6 studies focused on psychosocial well-being,80–85 and 10 studies focused on mental disease prevention and self-prevention.26,29,31,33–36,43,44,51 However, it is important to note that older adults are vulnerable to social isolation and psychological distress. They may suffer from declined functional abilities, age-related diseases, and decreased socioeconomic status after retirement.103–106 Worse still, a recent WHO report indicates that approximately 15% of older adults were suffering from mental health problems,107 and most of them were reluctant to seek professional healthcare services.108 Considering the potential of mobile-based interventions to improve the accessibility and efficacy of mental healthcare services,109 we suggest future studies should devote more effort to the design and evaluation of mHealth applications for the mental well-being of the elderly.
Our analysis also revealed that only 5 studies (6.8%) based their design elements on theories, which included social cognitive theory,38 behavior change wheel,28 technology acceptance model,25 theory of planned behavior,64 and unified theory of acceptance and use of technology.60 We recommend future research to propose theory-based application designs to provide a clearer understanding of the mechanism underlying each single design feature and, consequently, inform the theories of aging.13 For example, using the complexity literature as a theoretical basis, researchers have found that although older adults perceived a high comprehensiveness recommendation agent (that elicited detailed product attribute preferences and provided more product recommendations) to be more complex, they also perceived it as more beneficial than its counterpart.110 This contradicts the prevalent view that older adults should use simpler digital technologies.
Another important observation is that many studies proposed more than one design element and assessed the application as a whole. Consequently, our knowledge of end-user perceptions and the effectiveness of each single persuasive feature is relatively limited, particularly for peer support, collaborative activities, digital games, goal-setting, self-monitoring, performance feedback, rewards and challenges, peer comparison, and health education features (Figure 2). Moreover, elderly users who provided positive ratings on application usability may perceive specific features as difficult to use or useless.28,30,39,41,47,55,64,65,79,80,85,87,89,91,92 We thus recommend future research to investigate each design element in detail.
Finally, although 41 studies assessed the effects of mHealth applications on health-related outcomes, the strength of the evidence was limited due to poor research design. Specifically, approximately half of these studies (N = 22, 53.7%) did not have a comparison or control group. Moreover, 9 out of the 12 RCTs suffered from significant biases in study design.34,38,46,48,52,58,59,71,90 Therefore, stronger research designs are needed to rigorously quantify the effectiveness of application designs.
Limitations
We acknowledge that this review has several limitations. First, we restricted our scope to English-written, peer-reviewed journal articles. Our review could benefit from the inclusion of relevant conference publications and articles published in other languages. Second, we only included mHealth applications from the existing literature. Future research may consider conducting a more comprehensive evaluation of mHealth applications available for elderly users in the market.
CONCLUSION
This review identifies, synthesizes, and reports elderly-friendly interface and persuasive feature designs for mHealth applications from the existing literature. We derived 9 interface design recommendations that addresses the perceptual, motor, and cognitive deterioration of older adults. We also compiled 5 categories of persuasive features that may motivate older adults to achieve healthy aging. Overall, we provide specific and actionable suggestions for elderly-friendly mHealth application design and provide directions for future research in this field.
FUNDING
This research was supported by funds from the Singapore Ministry of Education Academic Research Fund Tier 1 (grant number: R-253-000-150-114) and The University of Sydney—National University of Singapore Partnership Collaboration Award 2019 Round.
AUTHOR CONTRIBUTIONS
NL and HHT designed the systematic review. JY, NL, and SST screened the title and abstracts of the included articles. JY, NL, NKY, and HHT extracted and synthesized the article information. All authors were involved in the data analysis, drafting, editing, and proofreading of the manuscript.
SUPPLEMENTARY MATERIAL
Supplementary material is available at Journal of the American Medical Informatics Association online.
Supplementary Material
DATA AVAILABILITY STATEMENT
The data underlying this article are available in the article and in its online supplementary material.
CONFLICT OF INTEREST STATEMENT
None declared.
ACKNOWLEDGMENTS
We are grateful to our librarian at the National University of Singapore, Ms. Annelissa Chin Mien Chew, for her invaluable advice on the search strategy.
REFERENCES
- 1.United Nations: Department of Economic and Social Affairs. World Population Prospects 2019: Highlights. New York, NY: United Nations Publications; 2019. https://population.un.org/wpp/Publications/Files/WPP2019_Highlights.pdf. Accessed August 23, 2021.
- 2.World Health Organization-WHO. Active Ageing: A Policy Framework. Madrid, Spain: World Health Organization; 2002. [PubMed]
- 3.Accenture. Digital Health: Primary Care is no Longer Primary. Accenture report. New York, NY: Accenture Research. 2018.https://www.accenture.com/us-en/insights/health/digital-health-primary-care. Accessed August 23, 2021.
- 4.ResearchAndMarkets. Mobile Health - Global Market Trajectory & Analytics. 2020. https://www.researchandmarkets.com/reports/5027977/mobile-health-global-market-trajectory-and?utm_source=dynamic&utm_medium=BW&utm_code=ldnh6s&utm_campaign=1412398+-+Global+Mobile+Health+Industry+(2020+to+2027)+-+Global+Market+Trajectory+%26+Analytics&utm. Accessed August 23, 2021.
- 5. Meng F, Guo X, Peng Z, et al. Investigating the adoption of mobile health services by elderly users: trust transfer model and survey study. JMIR Mhealth Uhealth 2019; 7 (1): e12269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wildenbos GA, Peute L, Jaspers M.. Aging barriers influencing mobile health usability for older adults: a literature based framework (MOLD-US). Int J Med Inform 2018; 114: 66–75. [DOI] [PubMed] [Google Scholar]
- 7. Charness N, Boot WR.. Aging and information technology use: potential and barriers. Curr Dir Psychol Sci 2009; 18 (5): 253–8. [Google Scholar]
- 8. McAlister C, Schmitter-Edgecombe M.. Naturalistic assessment of executive function and everyday multitasking in healthy older adults. Neuropsychol Dev Cogn B Aging Neuropsychol Cogn 2013; 20 (6): 735–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Luo L, Craik FIM.. Aging and memory: a cognitive approach. Can J Psychiatry 2008; 53 (6): 346–53. [DOI] [PubMed] [Google Scholar]
- 10. Wolfe B, Dobres J, Kosovicheva A, et al. Age-related differences in the legibility of degraded text. Cogn Res Princ Implic 2016; 1 (1): 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Mitzner TL, Rogers WA.. Age-related differences in reading text presented with degraded contrast. Proc Hum Factors Ergon Soc Annu Meet 2003; 47 (2): 242–6. [Google Scholar]
- 12. Luszcz MA, Bryan J.. Toward understanding age-related memory loss in late adulthood. Gerontology 1999; 45 (1): 2–9. [DOI] [PubMed] [Google Scholar]
- 13. Rogers WA, Fisk AD.. Toward a psychological science of advanced technology design for older adults. J Gerontol B Psychol Sci Soc Sci 2010; 65 (6): 645–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Yerrakalva D, Yerrakalva D, Hajna S, Griffin S.. Effects of mobile health app interventions on sedentary time, physical activity, and fitness in older adults: systematic review and meta-analysis. J Med Internet Res 2019; 21 (11): e14343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Matthew-Maich N, Harris L, Ploeg J, et al. Designing, implementing, and evaluating mobile health technologies for managing chronic conditions in older adults: a scoping review. JMIR mHealth uHealth 2016; 4 (2): e29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lee JA, Choi M, Lee SA, et al. Effective behavioral intervention strategies using mobile health applications for chronic disease management: a systematic review. BMC Med Inform Decis Mak 2018; 18 (1): 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Elavsky S, Knapova L, Klocek A, et al. Mobile health interventions for physical activity, sedentary behavior, and sleep in adults aged 50 years and older: a systematic literature review. J Aging Phys Act 2019; 27 (4): 565–93. [DOI] [PubMed] [Google Scholar]
- 18. Cornet VP, Toscos T, Bolchini D, et al. Untold stories in user-centered design of mobile health: practical challenges and strategies learned from the design and evaluation of an app for older adults with heart failure. JMIR mHealth uHealth 2020; 8 (7): e17703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kascak LR, Rebola CB, Sanford JA. Integrating Universal Design (UD) principles and mobile design guidelines to improve design of mobile health applications for older adults. In: Proceedings - 2014 IEEE International Conference on Healthcare Informatics, ICHI 2014. 2014: 343–8; Verona, Italy.
- 20. Li C, Neugroschl J, Zhu CW, et al. Design considerations for mobile health applications targeting older adults. J Alzheimers Dis 2021; 79 (1): 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Al-Razgan MS, Al-Khalifa H, Mona D, Alajmi H. Touch-based mobile phone interface guidelines and design recommendations for elderly people: A survey of the literature. In: Lecture Notes in Computer Science (including subseries Lecture Notes in Artificial Intelligence and Lecture Notes in Bioinformatics). 2012: 568–74; Heidelberg, Berlin, Germany. doi:10.1007/978-3-642-34478-7_69
- 22. Moher D, Liberati A, Tetzlaff J, et al. ; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009; 6 (7): e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.MHealth Services Market to Grow Extensively In Next Few Years: Read More to Know Why. Albany, NY: Transparency Market Research; 2018. https://www.transparencymarketresearch.com/pressrelease/mobile-health-market.htm. Accessed August 23, 2021.
- 24.United Nations: Department of Economic and Social Affairs, Population Division. World Population Ageing 2019 (ST/ESA/SER.A/444). 2020. https://www.un.org/en/development/desa/population/publications/pdf/ageing/WorldPopulationAgeing2019-Report.pdf. Accessed August 23, 2021.
- 25. Alsswey A, Bin Umar IN, Bervell B.. Investigating the acceptance of mobile health application user interface cultural-based design to assist Arab elderly users. Int J Adv Comput Sci Appl 2018; 9: 144–51. [Google Scholar]
- 26. Alvarez EA, Garrido M, Ponce DP, et al. A software to prevent delirium in hospitalised older adults: development and feasibility assessment. Age Ageing 2020; 49 (2): 239–45. [DOI] [PubMed] [Google Scholar]
- 27. Bakogiannis C, Tsarouchas A, Mouselimis D, et al. A Patient-Oriented App (ThessHF) to improve self-care quality in heart failure: from evidence-based design to pilot study. JMIR mHealth uHealth 2021; 9 (4): e24271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Balsa J, Félix I, Cláudio AP, et al. Usability of an intelligent virtual assistant for promoting behavior change and self-care in older people with type 2 diabetes. J Med Syst 2020; 44 (7): 130. [DOI] [PubMed] [Google Scholar]
- 29. Baric V, Andreassen M, Öhman A, et al. Using an interactive digital calendar with mobile phone reminders by senior people - a focus group study. BMC Geriatr 2019; 19 (1): 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Chen YX, Hung YP, Chen HC.. Mobile application-assisted cognitive behavioral therapy for insomnia in an older adult. Telemed J E Health 2016; 22 (4): 332–4. [DOI] [PubMed] [Google Scholar]
- 31. Chen K, Lou VWQ, Lo SSC.. A tablet-based volunteer-mediated intervention for cognitively impaired older people: a pretest–posttest. Res Soc Work Pract 2020; 30 (3): 288–97. [Google Scholar]
- 32. Chung K, Kim S, Lee E, et al. Mobile app use for insomnia self-management in urban community-dwelling older Korean adults: retrospective intervention study. JMIR mHealth uHealth 2020; 8 (8): e17755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Cunningham S, Brill M, Whalley JH, et al. Assessing wellbeing in people living with dementia using reminiscence music with a mobile app (Memory Tracks): a mixed methods cohort study. J Healthc Eng 2019; 2019: 8924273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Djabelkhir L, Wu YH, Vidal JS, et al. Computerized cognitive stimulation and engagement programs in older adults with mild cognitive impairment: comparing feasibility, acceptability, and cognitive and psychosocial effects. Clin Interv Aging 2017; 12: 1967–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Fortuna KL, DiMilia PR, Lohman MC, et al. Feasibility, acceptability, and preliminary effectiveness of a peer-delivered and technology supported self-management intervention for older adults with serious mental illness. Psychiatr Q 2018; 89 (2): 293–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Hackett K, Lehman S, Divers R, et al. Remind Me To Remember: A pilot study of a novel smartphone reminder application for older adults with dementia and mild cognitive impairment. Neuropsychol Rehabil 2020: 1–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Holden RJ, Campbell NL, Abebe E, et al. ; Brain Health Patient Safety Laboratory. Usability and feasibility of consumer-facing technology to reduce unsafe medication use by older adults. Res Soc Adm Pharm 2020; 16 (1): 54–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Jongstra S, Beishuizen C, Andrieu S, et al. Development and validation of an interactive Internet platform for older people: the healthy ageing through Internet counselling in the elderly study. Telemed J E Health 2017; 23 (2): 96–104. [DOI] [PubMed] [Google Scholar]
- 39. Jung H, Demiris G, Tarczy-Hornoch P, et al. A novel food record app for dietary assessments among older adults with type 2 diabetes: development and usability study. JMIR Form Res 2021; 5 (2): e14760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Kim HH, Lee SH, Cho NB, et al. User-dependent usability and feasibility of a SWALLOWING training mhealth app for older adults: mixed methods pilot study. JMIR mHealth uHealth 2020; 8 (7): e19585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Loh KP, Ramsdale E, Culakova E, et al. Novel mHealth app to deliver geriatric assessment-driven interventions for older adults with cancer: pilot feasibility and usability study. JMIR Cancer 2018; 4 (2): e10296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Madill ES, Samuels R, Newman DP, et al. Development of an evaluative, educational, and communication-facilitating app for older adults with chronic low back pain: patient perceptions of usability and utility. Pain Med 2019; 20 (11): 2120–8. [DOI] [PubMed] [Google Scholar]
- 43. Manca M, Paternò F, Santoro C, et al. The impact of serious games with humanoid robots on mild cognitive impairment older adults. Int J Hum Comput Stud 2021; 145: 102509. [Google Scholar]
- 44. Manera V, Petit PD, Derreumaux A, et al. Kitchen and cooking”, a serious game for mild cognitive impairment and Alzheimer’s disease: a pilot study. Front Aging Neurosci 2015; 7: 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Mertens A, Brandl C, Miron-Shatz T, et al. A mobile application improves therapy-adherence rates in elderly patients undergoing rehabilitation: a crossover design study comparing documentation via iPad with paper-based control. Medicine (United States) 2016; 95 (36): e4446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Mira JJ, Navarro I, Botella F, et al. A Spanish pillbox app for elderly patients taking multiple medications: randomized controlled trial. J Med Internet Res 2014; 16 (4): e99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Portz JD, Vehovec A, Dolansky MA, et al. The development and acceptability of a mobile application for tracking symptoms of heart failure among older adults. Telemed J E Health 2018; 24 (2): 161–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Puig J, Echeverría P, Lluch T, et al. A specific mobile health application for older HIV-infected patients: usability and patient’s satisfaction. Telemed e-Health 2021; 27 (4): 432–40. [DOI] [PubMed] [Google Scholar]
- 49. Quinn CC, Khokhar B, Weed K, et al. Older adult self-efficacy study of mobile phone diabetes management. Diabetes Technol Ther 2015; 17 (7): 455–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Reading Turchioe M, Grossman LV, Baik D, et al. Older adults can successfully monitor symptoms using an inclusively designed mobile application. J Am Geriatr Soc 2020; 68 (6): 1313–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Scase M, Kreiner K, Ascolese A.. Development and evaluation of cognitive games to promote health and wellbeing in elderly people with mild cognitive impairment. In: Schreier G, Hayn D, eds. Health Informatics Meets eHealth. Amsterdam, Netherlands: IOS Press; 2018: 255–62. doi:10.3233/978-1-61499-858-7-255. [PubMed] [Google Scholar]
- 52. Sun C, Sun L, Xi S, et al. Mobile phone–Based telemedicine practice in older Chinese patients with type 2 diabetes mellitus: Randomized controlled trial. JMIR mHealth uHealth 2019; 7 (1): e10664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Albergoni A, Hettinga FJ, Stut W, et al. Factors influencing walking and exercise adherence in healthy older adults using monitoring and interfacing technology: preliminary evidence. Int J Environ Res Public Health 2020; 17 (17): 6142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Baez M, Far IK, Ibarra F, et al. Effects of online group exercises for older adults on physical, psychological and social wellbeing: a randomized pilot trial. PeerJ 2017; 5: e3150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Bergquist R, Vereijken B, Mellone S, et al. App-based self-administrable clinical tests of physical function: development and usability study. JMIR Mhealth Uhealth 2020; 8 (4): e16507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Compernolle S, Cardon G, van der Ploeg HP, et al. Engagement, acceptability, usability, and preliminary efficacy of a self-monitoring mobile health intervention to reduce sedentary behavior in Belgian older adults: mixed methods study. JMIR mHealth uHealth 2020; 8 (10): e18653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Daly RM, Gianoudis J, Hall T, et al. Feasibility, usability, and enjoyment of a home-based exercise program delivered via an exercise app for musculoskeletal health in community-dwelling older adults: short-term prospective pilot study. JMIR mHealth uHealth 2021; 9 (1): e21094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Dekker-van Weering M, Jansen-Kosterink S, Frazer S, et al. User experience, actual use, and effectiveness of an information communication technology-supported home exercise program for pre-frail older adults. Front Med (Lausanne) 2017; 4: 208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Delbaere K, Valenzuela T, Lord SR, et al. E-health StandingTall balance exercise for fall prevention in older people: results of a two year randomised controlled trial. BMJ 2021; 373: n740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Geerds MAJ, Nijmeijer WS, Hegeman JH, et al. Mobile app for monitoring 3-month postoperative functional outcome after hip fracture: usability study. JMIR Hum Factors 2020; 7 (3): e16989. doi:10.2196/16989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Geraedts HAE, Zijlstra W, Zhang W, et al. A home-based exercise program driven by tablet application and mobility monitoring for frail older adults: feasibility and practical implications. Prev Chronic Dis 2017; 14: E12–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Haeger M, Bock O, Zijlstra W.. A smartphone based approach to enhance older persons’ mobility in daily life. Gerontechnology 2017; 16 (2): 109–14. [Google Scholar]
- 63. Harte R, Quinlan LR, Glynn L, et al. Human-centered design study: enhancing the usability of a mobile phone app in an integrated falls risk detection system for use by older adult users. JMIR mHealth uHealth 2017; 5 (5): e71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Hawley-Hague H, Tacconi C, Mellone S, et al. Smartphone apps to support falls rehabilitation exercise: App development and usability and acceptability study. JMIR mHealth uHealth 2020; 8 (9): e15460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Hill NL, Mogle J, Colancecco E, et al. Feasibility study of an attention training application for older adults. Int J Older People Nurs 2015; 10 (3): 241–9. [DOI] [PubMed] [Google Scholar]
- 66. Hill NL, Mogle J, Wion R, et al. App-based attention training: Incorporating older adults’ feedback to facilitate home-based use. Int J Older People Nurs 2018; 13 (1): e12163. [DOI] [PubMed] [Google Scholar]
- 67. Hsieh KL, Fanning JT, Rogers WA, et al. A fall risk mhealth app for older adults: development and usability study. JMIR Aging 2018; 1 (2): e11569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Kang GR, Kim IK, Kim WJ, et al. Promotion of adequate exercise for chronic disorders’ elderly through paced music. In: Gundlapalli AV, ed. MEDINFO 2017: Precision Healthcare through Informatics. Amsterdam, Netherlands: IOS Press; 2017: 136–40. doi:10.3233/978-1-61499-830-3-136 [PubMed] [Google Scholar]
- 69. Kwan RYC, Lee D, Lee PH, et al. Effects of an mHealth brisk walking intervention on increasing physical activity in older people with cognitive frailty: pilot randomized controlled trial. JMIR mHealth uHealth 2020; 8 (7): e16596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Li J, Xu X, Pham TP, et al. Exergames designed for older adults: a pilot evaluation on psychosocial well-being. Games Health J 2017; 6 (6): 371–8. [DOI] [PubMed] [Google Scholar]
- 71. Li CTL, Hung GKN, Fong KNK, et al. Effects of a home-based occupational therapy telerehabilitation via smartphone for outpatients after hip fracture surgery: A feasibility randomised controlled study. J Telemed Telecare 2020; 0: 1–9. doi:10.1177/1357633X20932434 [DOI] [PubMed] [Google Scholar]
- 72. Mehra S, Visser B, Cila N, et al. Supporting older adults in exercising with a tablet: a usability study. JMIR Hum Factors 2019; 6 (1): e11598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Pettersson B, Wiklund M, Janols R, et al. Managing pieces of a personal puzzle’-Older people’s experiences of self-management falls prevention exercise guided by a digital program or a booklet. BMC Geriatr 2019; 19 (1): 43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Shake MC, Crandall KJ, Mathews RP, et al. Efficacy of Bingocize®: A game-centered mobile application to improve physical and cognitive performance in older adults. Games Health J 2018; 7 (4): 253–61. [DOI] [PubMed] [Google Scholar]
- 75. Silveira P, Van De Langenberg R, Van Het Reve E, et al. Tablet-based strength-balance training to motivate and improve adherence to exercise in independently living older people: a phase II preclinical exploratory trial. J Med Internet Res 2013; 15 (8): e159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Tabak M, De Vette F, Van DIjk H, et al. A game-based, physical activity coaching application for older adults: design approach and user experience in daily life. Games Health J 2020; 9 (3): 215–26. [DOI] [PubMed] [Google Scholar]
- 77. Taylor ME, Close JCT, Lord SR, et al. Pilot feasibility study of a home-based fall prevention exercise program (StandingTall) delivered through a tablet computer (iPad) in older people with dementia. Australas J Ageing 2020; 39 (3): e278–e287. [DOI] [PubMed] [Google Scholar]
- 78. Van Het Reve E, Silveira P, Daniel F, et al. Tablet-based strength-balance training to motivate and improve adherence to exercise in independently living older people: Part 2 of a phase ii preclinical exploratory trial. J Med Internet Res 2014; 16 (6): e159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Zhong R, Rau PLP.. A mobile phone-based gait assessment app for the elderly: Development and evaluation. JMIR mHealth uHealth 2020; 8 (5): e14453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Chi NC, Sparks O, Lin SY, et al. Pilot testing a digital pet avatar for older adults. Geriatr Nurs 2017; 38 (6): 542–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Goumopoulos C, Papa I, Stavrianos A.. Development and evaluation of a mobile application suite for enhancing the social inclusion and well-being of seniors. Informatics 2017; 4 (3): 15. [Google Scholar]
- 82. Jansen-Kosterink SM, Bergsma J, Francissen A, et al. The first evaluation of a mobile application to encourage social participation for community-dwelling older adults. Health Technol 2020; 10 (5): 1107–13. [Google Scholar]
- 83. Judges RA, Laanemets C, Stern A, et al. “InTouch” with seniors: exploring adoption of a simplified interface for social communication and related socioemotional outcomes. Comput Human Behav 2017; 75: 912–21. [Google Scholar]
- 84. Neves BB, Franz R, Judges R, et al. Can digital technology enhance social connectedness among older adults? A feasibility study. J Appl Gerontol 2019; 38 (1): 49–72. [DOI] [PubMed] [Google Scholar]
- 85. Similä H, Immonen M, Toska-Tervola J, et al. Feasibility of mobile mental wellness training for older adults. Geriatr Nurs 2018; 39 (5): 499–505. [DOI] [PubMed] [Google Scholar]
- 86. Aure CF, Kluge A, Moen A.. Promoting dietary awareness: home-dwelling older adults’ perspectives on using a nutrition application. Int J Older People Nurs 2020; 15 (4): e12332. [DOI] [PubMed] [Google Scholar]
- 87. Aure CF, Kluge A, Moen A.. Older adults’ engagement in technology-mediated self-monitoring of diet: a mixed-method study. J Nurs Scholarsh 2021; 53 (1): 25–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Farsjø C, Moen A.. New app can give nutritional support to home-dwelling elderly. Sykepl Forsk 2020; 1–10. doi:10.4220/sykepleienf.2016.57821en [Google Scholar]
- 89. Franco RZ, Fallaize R, Lovegrove JA, et al. Online dietary intake assessment using a graphical food frequency app (eNutri): usability metrics from the EatWellUK study. PLoS One 2018; 13 (8): e0202006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Liu YC, Chen CH, Lin YS.. Design and usability evaluation of mobile voice-added food reporting for elderly people: randomized controlled trial. JMIR mHealth uHealth 2020; 8 (9): e20317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Algilani S, Langius-Eklöf A, Kihlgren A, et al. An interactive ICT platform for early assessment and management of patient-reported concerns among older adults living in ordinary housing – development and feasibility. J Clin Nurs 2017; 26 (11–12): 1575–83. [DOI] [PubMed] [Google Scholar]
- 92. Göransson C, Eriksson I, Ziegert K, et al. Testing an app for reporting health concerns—experiences from older people and home care nurses. Int J Older People Nurs 2018; 13 (2): e12181. [DOI] [PubMed] [Google Scholar]
- 93. Göransson C, Wengström Y, Hälleberg-Nyman M, et al. An app for supporting older people receiving home care - usage, aspects of health and health literacy: a quasi-experimental study. BMC Med Inform Decis Mak 2020; 20 (1): 226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Göransson C, Wengström Y, Ziegert K, et al. Self-care ability and sense of security among older persons when using an app as a tool for support. Scand J Caring Sci 2020; 34 (3): 772–81. [DOI] [PubMed] [Google Scholar]
- 95. Quinn CC, Staub S, Barr E, et al. Mobile support for older adults and their caregivers: dyad usability study. JMIR Aging 2019; 2 (1): e12276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Bott N, Wexler S, Drury L, et al. A protocol-driven, bedside digital conversational agent to support nurse teams and mitigate risks of hospitalization in older adults: case control pre-post study. J Med Internet Res 2019; 21 (10): e13440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Stal S, Broekhuis M, Van Velsen L, et al. Embodied conversational agent appearance for health assessment of older adults: explorative study. JMIR Hum Factors 2020; 7 (3): e19987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Steinert A, Haesner M, Tetley A, et al. Self-monitoring of health-related goals in older adults with use of a smartphone application. Act Adapt Aging 2016; 40 (2): 81–92. [Google Scholar]
- 99. Higgins J, Green S.. Cochrane Handbook for Systematic Reviews of Interventions Version. Chichester, UK: John Wiley & Sons; 2011. [Google Scholar]
- 100. Gao Q, Sun Q.. Examining the usability of touch screen gestures for older and younger adults. Hum Factors (5) 2015; 57: 835–63. [DOI] [PubMed] [Google Scholar]
- 101. Jin ZX, Piocher T, Kiff L.. Touch screen user interfaces for older adults: button size and spacing In: Stephanidis C, ed. Lecture Notes in Computer Science (Including Subseries Lecture Notes in Artificial Intelligence and Lecture Notes in Bioinformatics). Berlin, Heidelberg: Springer; 2007: 933–41. [Google Scholar]
- 102. Kim S, Chen RP, Zhang K.. Anthropomorphized helpers undermine autonomy and enjoyment in computer games. J Consum Res 2016; 43 (2): 282–302. [Google Scholar]
- 103. Lynch SM, George LK.. Interlocking trajectories of loss-related events and depressive symptoms among elders. J Gerontol B Psychol Sci Soc Sci (2) 2002; 57: S117–25. [DOI] [PubMed] [Google Scholar]
- 104. Krause N. Anticipated support, received support, and economic stress among older adults. J Gerontol - Ser B Psychol Sci Soc Sci 1997; 52: 284–93. [DOI] [PubMed] [Google Scholar]
- 105. Lang IA, Hubbard RE, Andrew MK, et al. Neighborhood deprivation, individual socioeconomic status, and frailty in older adults. J Am Geriatr Soc 2009; 57 (10): 1776–80. [DOI] [PubMed] [Google Scholar]
- 106. Ge L, Yap CW, Heng BH.. Prevalence of frailty and its association with depressive symptoms among older adults in Singapore. Aging Ment Health 2019; 23 (3): 319–24. [DOI] [PubMed] [Google Scholar]
- 107.World Health Organization. Mental health of older adults. 2017.https://www.who.int/news-room/fact-sheets/detail/mental-health-of-older-adults. Accessed August 23, 2021.
- 108. Reynolds K, Medved M, Mackenzie CS, et al. Older adults’ narratives of seeking mental health treatment: making sense of mental health challenges and “muddling through” to care. Qual Health Res (10) 2020; 30: 1517–28. [DOI] [PubMed] [Google Scholar]
- 109. Zarbo C, Brugnera A, Cipresso P, et al. E-mental health for elderly: challenges and proposals for sustainable integrated psychological interventions in primary care. Front Psychol 2017; 8: 118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Ghasemaghaei M, Hassanein K, Benbasat I.. Assessing the design choices for online recommendation agents for older adults: older does not always mean simpler information technology. MIS Q 2019; 43 (1): 329–46. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article are available in the article and in its online supplementary material.