Abstract
Objective
The study sought to summarize research literature on nursing decision support systems (DSSs ); understand which steps of the nursing care process (NCP) are supported by DSSs, and analyze effects of automated information processing on decision making, care delivery, and patient outcomes.
Materials and Methods
We conducted a systematic review in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement. PubMed, CINAHL, Cochrane, Embase, Scopus, and Web of Science were searched from January 2014 to April 2020 for studies focusing on DSSs used exclusively by nurses and their effects. Information about the stages of automation (information acquisition, information analysis, decision and action selection, and action implementation), NCP, and effects was assessed.
Results
Of 1019 articles retrieved, 28 met the inclusion criteria, each studying a unique DSS. Most DSSs were concerned with two NCP steps: assessment (82%) and intervention (86%). In terms of automation, all included DSSs automated information analysis and decision selection. Five DSSs automated information acquisition and only one automated action implementation. Effects on decision making, care delivery, and patient outcome were mixed. DSSs improved compliance with recommendations and reduced decision time, but impacts were not always sustainable. There were improvements in evidence-based practice, but impact on patient outcomes was mixed.
Conclusions
Current nursing DSSs do not adequately support the NCP and have limited automation. There remain many opportunities to enhance automation, especially at the stage of information acquisition. Further research is needed to understand how automation within the NCP can improve nurses’ decision making, care delivery, and patient outcomes.
Keywords: clinical decision support systems, nursing informatics, automation, patient safety
INTRODUCTION
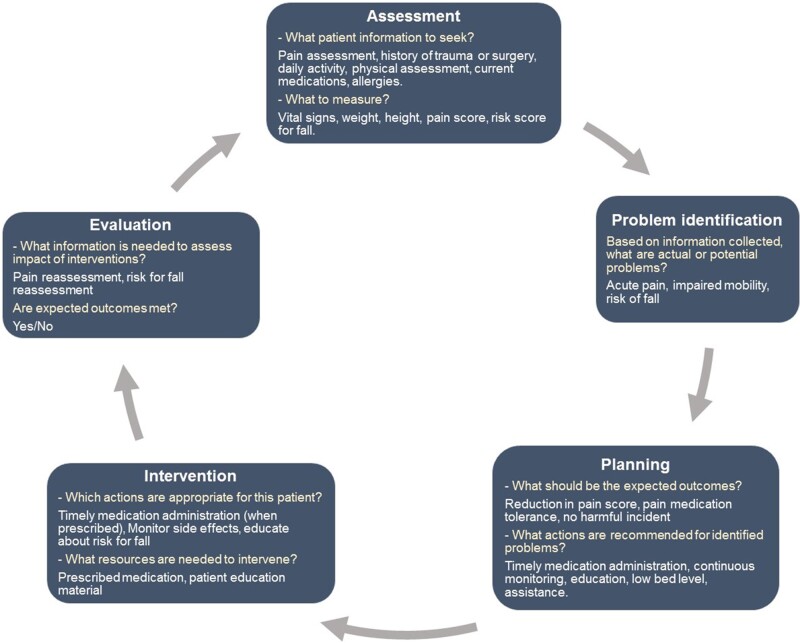
Electronic decision support systems (DSSs) are computer programs that help clinicians make informed decisions based on existing knowledge and individual patient characteristics. Their functions can vary from presenting data to users, generating alerts to implementing actions on behalf of users.1 For nurses, DSSs can play a vital role in facilitating the nursing care process (NCP), which is an important framework that helps nurses put their knowledge into practice. The NCP is a crucial care planning and problem-solving process in nursing practice that helps determine the needs of patients. It is generally taught to nursing students in early years of their education program and consists of five sequential steps: assessment, problem identification, planning, intervention, and evaluation.2,3 At each of these steps, nurses are required to use critical thinking and clinical judgment to make complex decisions about patient care. Additionally, the NCP is a dynamic process often requiring multiple iterations as the patient’s condition changes (Figure 1). For instance, a patient with knee pain may have a fluctuating pain score requiring nurses to frequently revise the care plan during their hospital stay. Failure to update care plans can lead to a mismatch between care arrangements and patient’s needs.
Figure 1.
The nursing care process with examples of decisions taken at each step for a hospitalized patient who is experiencing knee pain (after Toney-Butler and Thayer).2
Use of the NCP for continuous care planning means that nurses are constantly making decisions, and for each decision made, they go through the four distinct stages of human information processing: information acquisition, information analysis, decision selection, and action implementation.4 For example, to prevent falls, a nurse must formulate a care plan by acquiring information about the patient’s history, physical and mental health, and current functional status. Using this information, the nurse must analyze the patient’s risk for falls and select the most suitable actions. They can then implement the selected actions to ensure best patient outcomes. Within each step of NCP, nurses may be required to make multiple decisions, and for each of those decision, they may go through one or more stages of human information processing.
To make the process of care planning more robust, several DSSs such as assessment forms, risk score calculators, and risk management plans are used in nursing practice. These systems can help nurses in two ways: by facilitating one or more steps of NCP and by automating the stages of human information processing, ie, by executing information acquisition, analysis, decision and action selection, and action implementation on behalf of nurses.4 Little is known about the capabilities of existing DSSs to automate these stages and their effects on decision making, care delivery, and patient outcomes.
Previous reviews of nursing DSSs have been limited to describing system features5 or examining use patterns,6 or have been focused on specific clinical problems.7 A recent overview of systematic reviews addressed DSSs among other tools but was limited to nursing practice measures such as time, and professional satisfaction.8 To the best of our knowledge, no previous review has examined the effects of automation in nursing DSSs. To address this gap, we sought to summarize the research literature describing DSSs used by nurses, and to analyze effects of automated information processing on decision making, care delivery, and patient outcomes.
MATERIALS AND METHODS
The review was conducted in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta Analyses) statement.9 As the NCP is unique to nursing practice, we focused on electronic DSSs used solely by nurses and looked for studies about the effects of DSSs on decision making, care delivery, and patient outcomes. We chose these categories of impact using an already established framework called the information value chain, which shows that multiple steps are necessary from using DSSs to impacting patient outcomes including interacting with DSSs, receiving new information that then alters decisions, the care delivery process, and outcomes.10 For instance, a nurse may interact with a DSS to receive important new information based on which they decide to implement (decision making) an intervention (care delivery) that prevents a patient from falling during their inpatient stay (patient outcome). Thus, effects of a DSS can be measured by examining changes in decision making, care delivery, and patient outcomes.
Search strategy
We searched bibliographic databases including PubMed, CINAHL, Cochrane, Embase, Scopus, and Web of Science in October 2019 and updated the search in April 2020. Our search included the following themes based on the review objectives: decision support, nursing, care delivery, and patient outcomes. With the help of a research librarian, the authors developed search queries consisting of a comprehensive set of keywords and MeSH (Medical Subject Headings) terms relating to the chosen themes (Supplementary Appendix A). The retrieval set was limited to articles published in 2014 or later. We decided to restrict the start date of our search to 2014 because our focus was on contemporary DSSs in nursing. Previous systematic reviews published in 20075 and 201311 included similar studies and reviewed features or effects of DSSs. Moreover, the volume of nursing DSS studies has significantly increased since 2014, with an average of 154 publications indexed in PubMed per year (as compared with 70 per year from 2000 to 2013).
Study selection
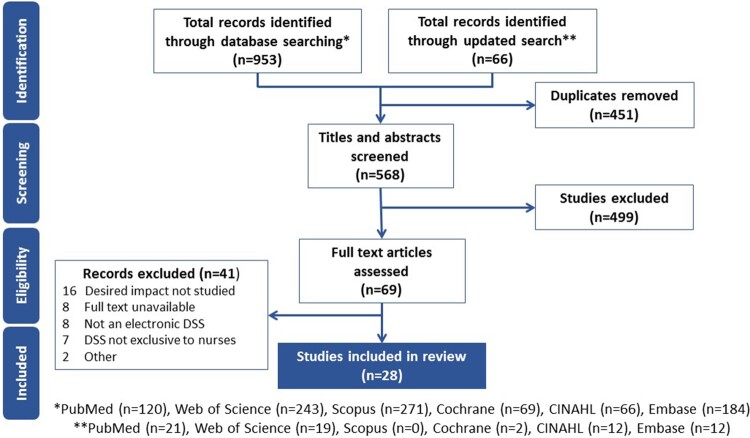
Our initial database search retrieved 1019 results (Figure 2) After duplicate entries were removed, titles and abstracts of 568 articles were screened by two reviewers (S.A. and J.A.C.). Studies about electronic DSSs used by multidisciplinary teams were excluded. Non-English articles and conference abstracts were also excluded. Full-length articles were retrieved from 69 abstracts identified for inclusion and were assessed independently against the inclusion criteria by the same reviewers. Forty-one of them were excluded because the full-text was not available, the DSS was not electronic, exclusively used by nurses, the desired impact was not studied, or the DSS was tested with undergraduate nursing students. We sought and received further information from the authors of three studies to aid eligibility assessment. Any disagreements about inclusion or exclusion were resolved by consensus. Interrater agreement was moderate (Cohen’s k = 0.565, n = 69).12
Figure 2.
Article search and retrieval process. DSS: decision support system.
Data extraction and synthesis
For each included study, descriptive information about the DSS, study design, user group, setting, implementation approach, stages of automation, nursing care process, and effects on decision making, care delivery, and patient outcomes were extracted. The quality of included studies was assessed using the Cochrane risk-of-bias tool13 for randomized controlled trials and the Joanna Briggs Institute’s checklists for nonrandomized controlled trials.14,15 Owing to heterogeneity of interventions and outcomes, a meta-analysis was not attempted. Instead, a narrative synthesis was conducted.9
User group and setting
We extracted information about participant credentials. They were mainly registered nurses, midwives, and nurse practitioners.16 While both registered nurses and nurse practitioners have a degree in nursing, and work closely with patients, nurse practitioners have further specialized training and experience. We categorized settings into short-term care in which patient encounters with the healthcare system are for a limited period of time (eg, emergency departments) and long-term care (eg, nursing homes).17
Nursing care process
DSS functions were mapped to one or more steps of the NCP: assessment, problem identification, planning, intervention, and evaluation.2
Stages of automation
DSSs were examined using a previously published framework that describes the automation of human information processing into 4 distinct stages4:
Information acquisition: Sensing or registering of data, without the user having to input information manually, eg, a telehealth DSS that collects data from home monitoring devices.
Information analysis: Cognitive functions and inferential processes, such as calculations, eg, a bedside DSS that calculates insulin dose.
Decision selection: Recommendations about possible actions, eg, a prehospital DSS that generates triage recommendations for transfer to aged care.
Action implementation: Actual execution of an action choice, eg, an oncology DSS that automatically documents nursing interventions directly in the medical record.
DSS functions could map to one or more stages of the framework.
Effects on decision making, care delivery, and patient outcomes
Using the information value chain two reviewers (S.A., F.M.) independently examined free text descriptions to identify DSS effects on decision making, care delivery, and patient outcomes. The interrater reliability for the classification was almost perfect (Cohen’s k = 0.867, n = 56).12 The effects of DSSs were then categorized as positive, negative, or no impact.
A narrative synthesis then integrated findings into descriptive summaries for each variable examined.
RESULTS
DSS users and settings
In total, 28 studies were included in our review (Table 1). Most of the DSSs studied (n = 24, 86%) were used by registered nurses (Table 2). Three (11%) were used by nurse practitioners to manage a variety of clinical conditions including obesity, tobacco use, and depression,18 back pain,19 and complex comorbidities in homebound patients.20 One DSS that guided antenatal care plans was used by both registered nurses and midwives.21
Table 1.
Studies reporting effects of nursing DSSs on decision making, care delivery, and patient outcomes (n = 28)
| Author, year | Study design | Study dates | User group | Setting | Sample size | Target population | Purpose of DSS | Stages of human information processing automated |
Steps of nursing care process |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| IA | IAn | DS | AI | A | PI | P | I | E | ||||||||
| Ajay et al, 201639 | Quasi experimental | 1 Dec 2012 to 21 Aug 2014 | RNs | Long term: community health centers |
|
Patients above the age of 30 y, who attended participating community health centers | Nursing care plan for noncommunicable diseases | Y | Y | Y | Y | Y | Y | Y | ||
| Bakken et al, 201418 | RCT | Not mentioned | NPs | Both |
|
Patients attending NP clinics | Reminds nurses to screen patients, formulate nursing care plans. | Y | Y | Y | Y | Y | Y | |||
| Barken et al, 201738 | Descriptive | Oct 2015 to Feb 2016 | RNs | Short term: telemedicine |
|
Telemedicine nurses | Triage assessment and recommendation | Y | Y | Y | Y | Y | Y | |||
| Bennett et al, 201628 | Quasi experimental |
|
RNs | Short term: emergency department | 800 patient records (400 pre and 400 post) |
|
Triage assessment and recommendation | Y | Y | Y | Y | Y | Y | |||
| Boltin et al, 201829 | Quasi experimental |
April 2017 Simulated event |
RNs | Short term: emergency department |
13 registered nurses 296 simulated patient encounters |
Mass casualty victims (all age) | Triage assessment and recommendation | Y | Y | Y | Y | Y | ||||
| Bowles et al, 201522 | Quasi experimental |
|
RNs | Short term: adult inpatient |
|
Adult patients admitted in and discharged alive from participating units | Risk assessment and recommendation for discharge outcomes | Y | Y | Y | Y | Y | Y | |||
| Chunmei et al, 201823 | Quasi experimental | Year 2017. Duration not mentioned | RNs | Short term: adult inpatient | 600 patient records (300 pre implementation, 300 post imp) | Adult inpatients | Risk assessment and management recommendations | Y | Y | Y | Y | Y | ||||
| Ciqueto Peres et al, 201524 | Descriptive | 1 Jan 2011 to 31 Dec 2012 | RNs | Short term: adult inpatient |
|
Patients admitted to medical and surgical units | Nursing problem assessment | Y | Y | Y | Y | Y | ||||
| Cortez and Wells, 201636 | RCT |
|
RNs | Short term: adult outpatient |
|
Adult oncology nurses | Recommends interventions for common symptoms | Y | Y | Y | Y | Y | ||||
| Dallaire and Cossi, 201537 | RCT |
|
RNs | Short term: ambulance | 806 patients (396 control, 410 intervention) | Older adults who called for ambulance | Triage assessment and recommendation | Y | Y | Y | Y | |||||
| Dehgani Soufi et al, 201830 | Quasi experimental | Not mentioned | RNs | Short term: emergency department |
|
Triage patients in emergency department | Triage assessment and recommendation | Y | Y | Y | Y | Y | ||||
| Febretti et al, 201443 | Quasi experimental | Not mentioned | RNs | Long term: palliative care | 24 nurses | End-of-life care patients | Recommends intervention for pain management. | Y | Y | Y | Y | Y | ||||
| Geurts et al, 201731 | RCT | May 2010 to Dec 2012 | RNs | Short term: emergency department | 222 patients (103 intervention, 109 control) | Children aged between 1 mo and 5 y, presenting in ED with acute vomiting and/or diarrhea | Assess and recommends rehydration interventions | Y | Y | Y | Y | Y | Y | Y | ||
| Harless, 201619 | Quasi experimental |
|
NPs | Short term: adult outpatient |
|
Patients over age 18 y, who presented at NP clinic with complain of nonspecific low back pain | Assessment and recommendations for functional outcomes | Y | Y | Y | Y | Y | Y | |||
| Horner and Coleman, 201421 | Quasi experimental |
|
Registered nurses and midwives | Short term: Community health centres |
|
Antenatal patients | Perinatal risk assessment and management recommendations | Y | Y | Y | Y | Y | Y | |||
| Kihlgren et al, 201632 | Quasi experimental | Not mentioned | RNs | Short term: Emergency Department | 281 patients assessed with DSS | Older people | Triage older people with health deterioration | Y | Y | Y | Y | |||||
| Lytle et al, 201525 | Quasi experimental |
|
RNs | Short term: Adult inpatient |
|
Adult inpatients in medical and surgical units | Alerts nurses to complete fall risk assessments and documentation | Y | Y | Y | Y | Y | Y | |||
| Mahabee-Gittens et al, 201833 | Quasi experimental | 3 mo starting Nov 2015 | RNs | Short term: Urgent care |
|
Pediatric urgent care nurses | Screening and counseling for caregivers who smoke | Y | Y | Y | Y | Y | ||||
| McDonald et al, 201641 | RCT | Not mentioned | RNs | Long term: home care |
|
Home health patients with high medication regimen complexity | Identify patients with high medication regimen complexity and offers management module | Y | Y | Y | Y | Y | Y | |||
| McLeod et al, 202034 | Observational |
Preimplementation: Jul to Sep 2016 Postimplementation: Jun 2017 to Dec 2018 |
RNs | Short term: Emergency Department |
7 Eds 1491 triage assessments |
Triage patients in emergency department | Triage assessment and recommendation | Y | Y | Y | Y | Y | Y | |||
| Olsho et al, 201444 | Quasi experimental | 12 mo | RNs | Long term: Nursing homes |
|
Nursing home residents | Risk assessment | Y | Y | Y | Y | Y | ||||
| Reynolds et al, 201926 | Quasi experimental | 1 y | RNs | Short term: Intensive care unit | 64 nurses, 2 sites | Pediatric nurses | Medication dose calculation | Y | Y | Y | ||||||
| Tang et al, 201945 | Quasi experimental | Jan 2017 to Jun 2017 | RNs | Long term: Nursing homes | 60 admission nurses, 30 patients. | Elderly patients with chronic diseases admitted to nursing homes | Formulate nursing care plans | Y | Y | Y | Y | Y | ||||
| Telford et al, 201827 | Observational | 1 May 2015 to 15 Dec 2015 | RNs | Short term: Intensive care unit |
|
ICU patients receiving insulin infusion | Medication dose calculation | Y | Y | Y | Y | |||||
| Thoma-Lurken et al, 201840 | RCT | Jan to May 2017 | RNs | Long term: Community | 67 nurses | Care coordinator nurses in community based dementia care | Risk assessment and management recommendations | Y | Y | Y | Y | Y | ||||
| Topaz et al, 201842 | Quasi experimental (Pilot) | Apr-May 2016 | RNs | Long term: Home care | 176 patients (90 control, 86 experimental) | Patients transitioning from hospital to home care | Generates priority score | Y | Y | Y | Y | Y | ||||
| Vetter, 201520 | Quasi experimental | 3 mo | NPs | Long term: Home care |
|
Chronically ill homebound patients with complex, comorbid conditions | Recommends diagnosis and ICD code | Y | Y | Y | Y | |||||
| Wouters et al, 202035 | Descriptive | Jul 2016 to Jul 2018 | RNs | Short term: Emergency Department | 24 nurses | Telephone triage nurses | Telephone triage assessment and recommendation | Y | Y | Y | Y | Y | Y | Y | ||
A: assessment; AI: action implementation; CHC: community health centre; DS: decision selection; dSS: decision support system; E: evaluation; I: intervention; IA: information acquisition; Ian: information analysis; ICD: International Classification of Diseases; ICU: intensive care unit; NP: nurse practitioner; P: plan; PI: problem identification; RCT: randomized controlled trial; RN: registered nurse; Y: yes.
Table 2.
Characteristics of the 28 studies reporting effects of nursing DSSs
| Characteristic | Studies |
|---|---|
| Study design | |
| Quasi-experimental | 18 (64) |
| Randomized controlled trial | 6 (21) |
| Descriptive | 3 (11) |
| Observational | 1 (4) |
| Year of publication | |
| 2014 | 3 (11) |
| 2015 | 5 (18) |
| 2016 | 7 (25) |
| 2017 | 2 (7) |
| 2018 | 7 (25) |
| 2019 | 3 (11) |
| 2020 (until March) | 1 (4) |
| DSS users | |
| Registered nurses | 24 (86) |
| Nurse practitioners | 3 (11) |
| Nurses and midwives | 1 (4) |
| Setting | |
| Short-term-care units | 19 (68) |
| Emergency or urgent care | 8 (29) |
| Inpatient wards | 4 (14) |
| Outpatient clinics | 3 (11) |
| Critical care units | 2 (7) |
| Ambulance | 1 (4) |
| Remote consultation | 1 (4) |
| Long-term-care units | 8 (29) |
| Nursing homes | 3 (11) |
| Home health care | 3 (11) |
| Community | 2 (7) |
| Both | 1 (4) |
| Nursing care process | |
| Assessment | 23 (82) |
| Problem identification | 19 (68) |
| Planning | 17 (61) |
| Intervention | 24 (86) |
| Evaluation | 3 (11) |
| Automated functions | |
| Information acquisition | 5 (18) |
| Information analysis | 28 (100) |
| Decision selection | 28 (100) |
| Action implementation | 1 (4) |
Values are n (%).
dSS: decision support system.
Categories are not mutually exclusive (ie, DSSs may have target multiple nursing care process steps and stages of automation).
Nineteen DSSs were implemented in short-term care units including inpatient wards,22–25 critical care units,26,27 emergency or urgent care,28–35 outpatient clinics,19,21,36 ambulance,37 and remote consultation.38 Eight DSSs were used in long-term-care facilities including community,39,40 home health care,20,41,42 and nursing homes.43–45 One DSS was used in both short- and long-term units.18
Nursing care process
Our mapping to the NCP showed that most DSSs were concerned with assessment, ie, they provided a list of questions or symptoms (n = 23, 82%), or supporting implementation like incident management plans (n = 24, 86%). Overall, 71% solely supported these two steps. The least commonly supported step was evaluation (n = 3, 11%). Only 2 DSSs supported all the steps of the NCP.
Automation in nursing DSSs
Our examination of stages of automation using the automation of human information processing framework showed that the stages of information analysis and decision selection were automated by all DSSs (n = 28, 100%). Examples include DSSs for triage in emergency departments29,30,32,34,35,37,38; risk management such as falls, pressure injuries, and medication errors18,21–23,25,40–42,44; dose calculation26,27; symptom management for pain, diarrhea, and fever19,31,36,39,41,43; and nursing problem identification.20,24,45 Five DSSs automated information acquisition by collecting information from medical records41,42,44 or patient input.29,38 Only one DSS automated action implementation by documenting nursing interventions directly into patients’ records.36
Effects of DSSs
The 28 included studies reported 56 outcome measures in total. Of these, baseline data to examine direction of effects were reported in 45 (Supplementary Appendix C). Twenty-two measures were related to decision making (reported in 16 unique studies), 11 were linked to care delivery (reported in seven unique studies), and 12 were related to patient outcomes (reported in seven unique studies). Overall, DSSs were demonstrated to have a positive effect on nurses’ decision making in 18 of the 22 outcome measures reported (82%, Table 3).
Table 3.
Effect of DSS on decision making, care delivery, and patient outcomes in studies that provided comparable baseline data (eg, 7 studies examined effects of DSS on care delivery reporting 11 different outcome measures demonstrating a positive effect in 8 measures)
| Number of studies | Total number of outcome measures reported | Positive effect of DSS | Negative effect of DSS | No significant effect of DSS | |
|---|---|---|---|---|---|
| Decision making 18 , 20–23 , 25 , 26 , 28 , 30 , 32–34 , 36 , 40 , 43 , 45 | 16 | 22 | 18 (82) | 0 (0) | 4 (18) |
| Care delivery 26 , 28 , 31 , 33 , 37 , 39 , 42 | 7 | 11 | 8 (73) | 1 (9) | 2 (18) |
| Patient outcomes 19 , 22 , 23 , 25 , 31 , 33 , 41 , 42 , 44 | 9 | 12 | 6 (50) | 1 (8) | 5 (42) |
| Total | 45 | 32 (71) | 2 (7) | 10 (22) |
Values are n or n (%).
dSS: decision support system.
Effects of DSSs on decision making
The effects of DSSs on decision making was reported in 23 studies (82%, n = 28). Nurses’ agreement with DSS recommendations ranged widely between 20% and 87%.21,24,25,29,31–33,39,43 Several studies reported improvements in accuracy of nursing problem identification ,18,20,23 triage prioritization,28,29,32,34 implementation of evidence-based practice,18,21,25,28,43 and nursing documentation.30,36 Reports of reduction in time required to make a decision34,45 and care plan variations among nurses19,40,45 were also found.
Other studies reported no significant effect on nursing interventions2,18,22 or cognitive load.26 One study found that documentation and plan of care compliance decreased after DSS implementation.25 Another study reported that improvement in nurses’ decision making was not consistent. While decision making was improved initially when DSS was implemented, it gradually deteriorated within three months.33 Finally, four studies found that nurses’ decisions were influenced by factors such as their work environment, experience, and clinical judgment.24,26,35,38
Effects of DSSs on care delivery
Only seven (25%) studies reported effects of DSSs on care delivery. Two RCTs reported that high risk patients received appropriate care sooner than usual when DSS was used for prioritization,37,42 while another RCT found that patients received more oral rehydration than intravenous when DSS that recommended treatment was implemented, without any effect on cost of treatment.31 An experimental study found that more patients were screened for and diagnosed with hypertension and diabetes with the use of DSSs.39 Additionally, a DSS that addressed child tobacco smoke exposure resulted in caregivers receiving education material 83.5% of the time.33 One DSS that calculated medication dose improved detection of dosage errors,26 and another study that evaluated an emergency department DSS found that the rate of appropriate analgesic administration increased but that the use of intravenous antibiotics decreased.28
Effects of DSSs on patient outcomes
Eleven (39%) studies reported effects of DSSs on patient outcomes. Four of these reported reduction in readmission when DSS was used to manage patient care.22,31,41,42 Two examined patient’s length of stay, which was increased42 or remained unchanged.31 Functional outcomes of patients with lower back pain also remained unchanged with the use of DSSs.19
Two studies that evaluated DSSs for risk management found that falls and pressure injuries decreased postimplementation.23,44 However, a similar study found that there was no effect on falls postimplementation.25 Another study of a DSS to manage intravenous insulin infusion reported one event of mild hypoglycaemia.27 A DSS that screened and managed patients with hypertension and diabetes reported significant reduction in mean systolic blood pressure and fasting blood glucose.39 Another DSS to manage patients with high medication regimen complexity reported 8% risk reduction with DSSs, as compared with 4.5% without DSSs,41 and finally, a DSS that supported caregiver education to quit smoking reported that 67% of those who were educated showed willingness to quit in the next 30 days.33
Quality of studies and risk of bias
Of the 28 studies included, most common study designs were quasi-experimental (n = 18, 64%)19–26,28–30,32,33,39,42–45 and randomized controlled trials (n = 6, 21%)18,31,36,37,40,41 (Table 2). Risk of bias assessment for the six RCTs showed some concerns (Supplementary Appendix B[i]), including not enough information about measures taken to conceal allocation sequence,31,40,41 blinding of personnel,36,37,41 and prespecified analysis plan.18,36,37,40,41 Similarly, in quasi-experimental and observational studies (Supplementary Appendices B[ii] and B[iii]), information about participants was either unclear or missing.23,28,30,39,45 Confounding factors were not addressed,27 and measurement methods and statistical analysis were limited.20,21,23,29,32,45
DISCUSSION
Main findings and implications
Despite increasing use of DSSs in clinical practice and awareness of the benefits of automation,46 their use in nursing is understudied. Previous reviews have mainly considered nursing DSSs alongside other information and communication technologies.8,47 To the best of our knowledge, ours is the first to apply the stages of human information processing4 to examine automation within nursing DSSs in relation to the NCP. We also report about DSS support for nurses’ decision making, care delivery, and patient outcomes.
Consistent with previous reviews, we found considerable heterogeneity in DSS functions, study design, and outcome measures that prevented comparative assessments.11,48,49 The majority of the included DSSs supported patient assessments and assisted nurses to identify correct interventions. However, evaluation of the efficacy of those interventions was only supported by three DSSs. These findings are consistent with a previous review that found few DSSs supported nurses to evaluate clinical interventions.5
We also found that most DSSs automated two of the four stages of human information processing stages, information analysis and decision selection. These stages are likely targeted because they allow for logical, rule-based processing, which makes them more feasible from a system design perspective. Technological feasibility is a key consideration for automation.50 Examples of tasks within these stages include risk scores calculation and recommendation of actions based on scores. The remaining two stages, information acquisition and action implementation, are more complex to automate because they require nurses’ clinical expertise and involve subjective assessment as well as actions that require physical handling. From a nursing practice perspective, information analysis and decision selection cover most of the cognitive work. However, the absence of support for the remaining stages can lead to negative outcomes. When information acquisition is manual, errors, delays, and missed data are more likely. Erroneous input can subsequently result in faulty analysis and decision selection. Similarly, manual action implementation can also be easily missed or delayed. Here, an important implication is that nurses and DSSs need to work together as they each may perform different stages of the information processing task.
In terms of the effects of DSSs on decision making, care delivery, and patient outcomes, evidence in all three outcome domains was mixed. While some DSSs were reported to have an overall positive impact on decision making in the form of improved compliance with recommendations19,28,43 and reduced time to make decisions,34,45 others had no sustainable impact. Two studies even reported negative outcomes.25,28 Interestingly, one study reported that the long term impact of DSSs was not impressive, ie, compliance and improvements in decision making and care delivery increased initially but decreased with use of DSSs over a longer period of time.33 A recent review of clinical DSSs describes in detail the long-term effect of DSS use including users’ clinical skills, education, and overreliance.51 As there was only one study that measured DSS effects over time, it was not possible to conduct a formal analysis of long-term effects in this review. Further research is required to explore whether effects are sustained or changed in the long term.
We found many reports about improvement in evidence-based practice as a result of DSS implementation, meaning that more patients were appropriately diagnosed, prioritized, educated, or treated.28,29,32–34,37,39,42 However, the impact of these improved practices on patient outcomes was mixed. While there were several reports about reduced safety incidents such as readmissions22,31,41,42 and falls,23,44 other DSSs had no effect19,31 or increased patient harm.25,27 There are four possible explanations for this disparity in impact. First, the way DSSs are integrated with existing information systems can affect outcomes. In our review, DSSs that were integrated with electronic health records (EHRs) had better outcomes,21,34,42,44,45 as compared with those that were standalone tools.26,35 Integration with existing information systems can help address gaps in automation, reduce data duplication, and improve usability.52,53 Second, most existing DSSs do not usually support more than one step of the NCP, which may affect outcomes. DSSs are mostly designed to focus on singular tasks such as medication dose or risk score calculation. It is important here to understand that these tasks are part of wider care processes. For example, dose calculation is a task within medication management and may not reduce errors if it is not directly linked to medication administration.26 Third, nurses’ decision making is a complex process with multiple variables influencing outcomes such as their clinical experience, judgment, personal values, autonomy, situation awareness, and organizational context.54–56 Their decisions are not always straightforward or mathematical in nature. Nurses often collaborate with team members, consider available resources, and prioritize tasks before coming to a decision. Therefore, the effects of DSSs may vary. Finally, we observed a wide variety of methods to implement and study DSSs. Some studies allowed time for interventions to be embedded postimplementation, and others did not. The impact of different implementation strategies is a well-understood phenomenon in the health informatics literature.57,58 We also found that evaluations were conducted in different settings and over different timeframes. Some tested DSSs in a controlled environment, eg, a computer laboratory, and others were situated in clinical settings.
Recommendations for DSS developers, nurses, and researchers
Based on our findings, we make several recommendations for DSS developers, nurses, and researchers. While DSS design is usually based on clinical tasks that must be supported, developers need to consider nursing tasks as components of the NCP where each step is interconnected. For example, a DSS that addresses knee pain management (Figure 1) should not be limited to pain assessment, but rather should support decisions about relevant potential problems, planned expected outcomes, individualized interventions, and evaluation. It is also important to realize that for many nursing care problems, DSSs alone cannot be the solution but an essential component of a group of strategies that may be needed. For example, a fall prevention toolkit combining decision support with patient and family education materials reported a significant reduction in fall rates.59 Another study implemented 2 DSSs along with training and patient education materials to improve the safety of medication use in elderly patients.60 Such use of multiple interventions is not a new concept in nursing practice. The importance of designing multisystematic models that include elements of the physical environment, culture, and technology has been highlighted in previous systematic reviews.61,62 Such an approach can conform to the way nurses perform their clinical duties, engage patients and other healthcare team members in care delivery, and address various care management factors at the same time to enhance overall impact.
There is also a need to make nursing DSSs more intelligent, ie, instead of being hard-coded, systems should be adaptive and learn from patient data and user behaviour.63 Over the last decade, advancements in artificial intelligence techniques have proven effective in disease diagnosis,64 which suggests that it is certainly possible to automate problem identification based on quantifiable data from patient medical records. Additionally, evidence suggests that using automatically deriving data from EHRs and making decisions based on those data can reduce errors and improve care quality.65 However, opportunities to incorporate such technologies within nursing DSSs and better support the NCP are yet to be realized.66
It is also important to make thoughtful decisions about which NCP steps and clinical tasks to automate. One way of doing this is through workflow analysis that nurse leaders can perform. Workflow analysis considers all physical and cognitive factors involved in decision making.67 It requires detailed documentation of each step of the decision-making process, including activities, environments, patients, organizational culture, policies, and procedures involved.68 For example, workflow analysis of resident monitoring in nursing home can capture available resources, decisions about who to monitor and when to intervene, and actions such as identifying location of harm and setting alarms.69 Another example is inpatient risk assessment, workflow that starts with initial assessment at the time of admission, and regular reassessments depending on patients’ condition. Using outcomes of workflow analysis, nurse leaders can select the system that best fits their processes. Ultimately, the decision about which NCP step and nursing tasks that can be automated should depend on added benefits to care delivery, and patient outcomes.10
Frontline staff, who are often the users of DSSs, should be involved in design and implementation processes.70 They can participate at several stages such as the needs analysis stage by sharing their perspectives, verbalizing expectations and inherent requirements of nursing practice; testing stage by providing use cases or helping developers and leaders explore effects of system prior to implementation71; and finally in the evaluation stage by offering meaningful insights about impact on decision making, care delivery, and outcomes.
Further research on the development and testing of automated nursing DSSs is required. While there are many studies examining nurses’ decision making54,72,73 and their interaction with health technology,74,75 there is a need for primary studies to examine the role of automation in nursing DSSs in relation to the NCP. Indeed, safe and effective automation of DSSs will guide the future landscape of nursing practice to improve care quality and patient safety.
Limitations
This review has several limitations. It was restricted to DSSs used solely by nurses and did not include multidisciplinary implementation studies that may involve nurses as part of a diverse user group. Moreover, our search was limited to studies published from January 2014 to March 2020. The use of DSSs is not new in nursing and several studies published before and after our search duration have evaluated their effects.59,60,62,76–78 It is thus possible that our examination of automation in nursing DSSs and its effects is not exhaustive. Heterogeneity in DSS functions, study design, and outcome measures prevented quantitative examination of effects of automation on decision making, care delivery, and patient outcomes.
CONCLUSION
This review confirms that current nursing DSSs do not adequately support the NCP and have limited automation. There remain many opportunities to enhance automation, especially at the stage of information acquisition such as by allowing DSSs to acquire data from other sources such as EHRs. Further research is required to understand how automation within the NCP can improve nurses’ decision making, care delivery, and patient outcomes.
FUNDING
This research was supported by doctoral scholarship to SA provided by Macquarie University (MQRES 20192700, 20201711); the National Health and Medical Research Council Centre for Research Excellence in Digital Health (APP1134919), and a Macquarie University Safety Net grant.
Author contributions
SA conceived this study and designed and conducted the analysis with advice and input from FM and DL. SA drafted the manuscript with input from all authors. All authors provided revisions for intellectual content. All authors have approved the final manuscript.
SUPPLEMENTARY MATERIAL
Supplementary material is available at Journal of the American Medical Informatics Association online.
Supplementary Material
ACKNOWLEDGMENTS
We wish to acknowledge the invaluable contributions of Jessica A. Chen and Jeremy Cullis.
CONFLICT OF INTEREST STATEMENT
The authors have no competing interests to declare.
DATA AVAILABILITY STATEMENT
All data relevant to the study are included in the article or uploaded as online supplemental information. All data relevant to the analysis are reported in the article.
REFERENCES
- 1. Coiera E. Guide to Health Informatics. 3rd ed.Boca Raton: CRC Press; 2015. [Google Scholar]
- 2. Toney-Butler TJ, Thayer JM.. Nursing Process. Treasure Island, FL: StatPearls; 2020. [PubMed] [Google Scholar]
- 3. Taskin Yilmaz F, Sabanciogullari S, Aldemir K.. The opinions of nursing students regarding the nursing process and their levels of proficiency in Turkey. J Caring Sci 2015; 4 (4): 265–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Parasuraman R, Sheridan TB, Wickens CD, et al. A model for types and levels of human interaction with automation. IEEE Trans Syst Man Cybern A Syst Hum 2000; 30 (3): 286–97. [DOI] [PubMed] [Google Scholar]
- 5. Lee S. Features of computerized clinical decision support systems supportive of nursing practice: a literature review. Comput Inform Nurs 2013; 31 (10): 477–95. [DOI] [PubMed] [Google Scholar]
- 6. Piscotty R, Kalisch B.. Nurses' use of clinical decision support: a literature review. Comput Inform Nurs 2014; 32 (12): 562–8. [DOI] [PubMed] [Google Scholar]
- 7. Araujo SM, Sousa P, Dutra I, et al. Clinical decision support systems for pressure ulcer management: systematic review. JMIR Med Inform 2020; 8 (10): e21621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Rouleau G, Gagnon M-P, Côté J, et al. Impact of information and communication technologies on nursing care: results of an overview of systematic reviews. J Med Internet Res 2017; 19 (4): e122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 2009; 6 (7): e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Coiera E. Assessing technology success and failure using information value chain theory. Stud Health Technol Inform 2019; 263: 35–48. [DOI] [PubMed] [Google Scholar]
- 11. Randell R, Mitchell N, Dowding D, et al. Effects of computerized decision support systems on nursing performance and patient outcomes: a systematic review. J Health Serv Res Policy 2007; 12 (4): 242–9. [DOI] [PubMed] [Google Scholar]
- 12. Landis JR, Koch GG.. The measurement of observer agreement for categorical data. Biometrics 1977; 33 (1): 159–74. [PubMed] [Google Scholar]
- 13. Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019; 366: l4898. [DOI] [PubMed] [Google Scholar]
- 14.Checklist for Quasi-Experimental Studies: Joanna Briggs Institute; 2017. https://jbi.global/critical-appraisal-tools. Accessed April 23, 2021.
- 15.Checklist for Analytical Cross-Sectional Studies: Joanna Briggs Institute; 2017. https://jbi.global/critical-appraisal-tools. Accessed April 23, 2021.
- 16.Nursing and Midwifery Board of Australia. Professional Standards; 2017.https://www.nursingmidwiferyboard.gov.au/Codes-Guidelines-Statements/Professional-standards.aspx. Accessed March 12, 2020.
- 17. Hirshon JM, Risko N, Calvello EJB, et al. ; Acute Care Research Collaborative at the University of Maryland Global Health Initiative. Health systems and services: the role of acute care. Bull World Health Organ 2013; 91 (5): 386–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bakken S, Jia H, Chen ES, et al. The Effect of a mobile health decision support system on diagnosis and management of obesity, tobacco use, and depression in adults and children. J Nurse Pract 2014; 10 (10): 774–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Harless DF. The Impact of Computer Decision Support Software by Nurse Practitioners on Functional Outcomes for Patients With Acute Lower Back Pain: A DNP Project [PhD dissertation]. Hammond, Louisiana Southeastern Louisiana University; 2016.
- 20. Vetter MJ. The influence of clinical decision support on diagnostic accuracy in nurse practitioners. Worldviews Evid Based Nurs 2015; 12 (6): 355–63. [DOI] [PubMed] [Google Scholar]
- 21. Horner V, Coleman A., Evaluation of a guidelines-based e-health decision support system for primary health care in South Africa. In: SAICSIT '14: Proceedings of the Southern African Institute for Computer Scientist and Information Technologists Annual Conference 2014 on SAICSIT 2014 Empowered by Technology; 2014: 142–7. [Google Scholar]
- 22. Bowles KH, Chittams J, Heil E, et al. Successful electronic implementation of discharge referral decision support has a positive impact on 30- and 60-day readmissions. Res Nurs Health 2015; 38 (2): 102–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Chunmei R, Hualing H, Haihua Z, et al. Design and application of nursing CDSS based on structured EMR. Stud Health Technol Inform 2018; 250: 238–9. [PubMed] [Google Scholar]
- 24. Ciqueto Peres HH, de Almeida Lopes Monteiro da Cruz D, Tellez M, et al. Usability testing of PROCEnf-USP: a clinical decision support system. Stud Health Technol Inform 2015; 216: 247–50. [PubMed] [Google Scholar]
- 25. Lytle KS, Short NM, Richesson RL, et al. Clinical decision support for nurses: A fall risk and prevention example. Comput Inform Nurs 2015; 33 (12): 530–7. quiz E1. [DOI] [PubMed] [Google Scholar]
- 26. Reynolds TL, DeLucia PR, Esquibel KA, et al. Evaluating a handheld decision support device in pediatric intensive care settings. JAMIA Open 2019; 2 (1): 49–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Telford ED, Franck AJ, Hendrickson AL, et al. A bedside computerized decision-support too for intravenous insulin infusion management in critically ill patients. Jt Comm J Qual Patient Saf 2018; 44 (5): 299–303. [DOI] [PubMed] [Google Scholar]
- 28. Bennett P, Hardiker N.. A quantitative study investigating the effects of computerised clinical decision support in the emergency department. Stud Health Technol Inform 2016; 225: 53–7. [PubMed] [Google Scholar]
- 29. Boltin N, Valdes D, Culley JM, et al. Mobile decision support tool for emergency departments and mass casualty incidents (EDIT): initial study. JMIR Mhealth Uhealth 2018; 6 (6): e10727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Dehghani Soufi M, Samad-Soltani T, Shams Vahdati S, et al. Decision support system for triage management: a hybrid approach using rule-based reasoning and fuzzy logic. Int J Med Inform 2018; 114: 35–44. [DOI] [PubMed] [Google Scholar]
- 31. Geurts D, de Vos-Kerkhof E, Polinder S, et al. Implementation of clinical decision support in young children with acute gastroenteritis: a randomized controlled trial at the emergency department. Eur J Pediatr 2017; 176 (2): 173–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kihlgren A, Svensson F, Lövbrand C, et al. A Decision support system (DSS) for municipal nurses encountering health deterioration among older people. BMC Nurs 2016; 15: 63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Mahabee-Gittens EM, Dexheimer JW, Tabangin M, et al. An electronic health record-based strategy to address child tobacco smoke exposure. Am J Prev Med 2018; 54 (1): 64–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. McLeod SL, McCarron J, Ahmed T, et al. Interrater reliability, accuracy, and triage time pre- and post-implementation of a real-time electronic triage decision-support tool. Ann Emerg Med 2020; 75 (4): 524–31. [DOI] [PubMed] [Google Scholar]
- 35. Wouters LT, Zwart DL, Erkelens DC, et al. Tinkering and overruling the computer decision support system: Working strategies of telephone triage nurses who assess the urgency of callers suspected of having an acute cardiac event. J Clin Nurs 2020; 29 (7–8): 1175–86. [DOI] [PubMed] [Google Scholar]
- 36. Cortez S, Wells N., Measuring clinical decision support influence on oncology nursing practice. Oncol Nurs Forum 2015; 42 (2): E245. [DOI] [PubMed] [Google Scholar]
- 37. Dallaire C, Cossi M-J.. Prehospital decision system supports appropriate transfer of older adults direct to a community-based hospital. Evid Based Nurs 2015; 18 (4): 127. [DOI] [PubMed] [Google Scholar]
- 38. Barken TL, Thygesen E, Söderhamn U, et al. Advancing beyond the system: telemedicine nurses' clinical reasoning using a computerised decision support system for patients with COPD - an ethnographic study. BMC Med Inform Decis Mak 2017; 17 (1): 181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Ajay VS, Jindal D, Roy A, et al. Development of a smartphone-enabled hypertension and diabetes mellitus management package to facilitate evidence-based care delivery in primary healthcare facilities in India: the mPower Heart Project. J Am Heart Assoc 2016; 5 (12): 1–10, e004343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Thoma-Lurken T, Bleijlevens MHC, Lexis MAS, Hamers JPH.. Evaluation of a decision support app for nurses and case managers to facilitate aging in place of people with dementia. A randomized controlled laboratory experiment. Geriatr Nurs 2018; 39 (6): 653–62. [DOI] [PubMed] [Google Scholar]
- 41. McDonald MV, Feldman PH, Barrón-Vayá Y, et al. Outcomes of clinical decision support (CDS) and correlates of CDS use for home care patients with high medication regimen complexity: A randomized trial. J Eval Clin Pract 2016; 22 (1): 10–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Topaz M, Trifilio M, Maloney D, et al. Improving patient prioritization during hospital-homecare transition: A pilot study of a clinical decision support tool. Res Nurs Health 2018; 41 (5): 440–7. [DOI] [PubMed] [Google Scholar]
- 43. Febretti A, Stifter J, Keenan GM, et al. Evaluating a clinical decision support interface for end-of-life nurse care. Ext Abstr Hum Factors Computing Syst 2014; 2014: 1633–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Olsho LEW, Spector WD, Williams CS, et al. Evaluation of AHRQ's on-time pressure ulcer prevention program: A facilitator-assisted clinical decision support intervention for nursing homes. Med Care 2014; 52 (3): 258–66. [DOI] [PubMed] [Google Scholar]
- 45. Tang V, Siu PKY, Choy KL, et al. An adaptive clinical decision support system for serving the elderly with chronic diseases in healthcare industry. Expert Syst 2019; 36 (2): e12369. [Google Scholar]
- 46. Soman S, Zasuwa G, Yee J, et al. Automation, decision support, and expert systems in nephrology. Adv Chronic Kidney Dis 2008; 15 (1): 42–55. [DOI] [PubMed] [Google Scholar]
- 47. Mitchell N, Randell R, Foster R, et al. A national survey of computerized decision support systems available to nurses in England. J Nurs Manag 2009; 17 (7): 772–80. [DOI] [PubMed] [Google Scholar]
- 48. Coiera E, Westbrook J, Wyatt J, et al. The safety and quality of decision support systems. Yearb Med Inform 2006; 1 (15): 20–5. [PubMed] [Google Scholar]
- 49. Bright TJ, Wong A, Dhurjati R, et al. Effect of clinical decision-support systems: a systematic review. Ann Intern Med 2012; 157 (1): 29–43. [DOI] [PubMed] [Google Scholar]
- 50. Parasuraman R, Riley V., Humans and automation: use, misuse, disuse, abuse. Hum Factors 1997; 39 (2): 230–53. [Google Scholar]
- 51. Sutton RT, Pincock D, Baumgart DC, Sadowski DC, Fedorak RN, Kroeker KI.. An overview of clinical decision support systems: benefits, risks, and strategies for success. NPJ Digit Med 2020; 3 (17): 1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Huang H-Y, Lee T-T, Hsu T-C, et al. Evaluation of the pressure injury prevention information system. Comput Inform Nurs 2020; 38 (12): 625–32. [DOI] [PubMed] [Google Scholar]
- 53. Paulsen MM, Paur I, Gjestland J, et al. Effects of using the MyFood decision support system on hospitalized patients' nutritional status and treatment: A randomized controlled trial. Clin Nutr 2020; 39 (12): 3607–17. [DOI] [PubMed] [Google Scholar]
- 54. Nibbelink CW, Brewer BB.. Decision-making in nursing practice: An integrative literature review. J Clin Nurs 2018; 27 (5–6): 917–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Bucknall T, Thomas S.. Nurses' reflections on problems associated with decision-making in critical care settings. J Adv Nurs 1997; 25 (2): 229–37. [DOI] [PubMed] [Google Scholar]
- 56. Gerdtz MF, Bucknall TK.. Triage nurses' clinical decision making. An observational study of urgency assessment. J Adv Nurs 2001; 35 (4): 550–61. [DOI] [PubMed] [Google Scholar]
- 57. Kilsdonk E, Peute LW, Jaspers MWM, et al. Factors influencing implementation success of guideline-based clinical decision support systems: a systematic review and gaps analysis. Int J Med Inform 2017; 98: 56–64. [DOI] [PubMed] [Google Scholar]
- 58. Ammenwerth E, Talmon J, Ash JS, et al. Impact of CPOE on mortality rates–contradictory findings, important messages. Methods Inf Med 2006; 45 (6): 586–93. [PubMed] [Google Scholar]
- 59. Dykes PC, Burns Z, Adelman J, et al. Evaluation of a patient-centered fall-prevention tool kit to reduce falls and injuries: a nonrandomized controlled trial. JAMA Netw Open 2020; 3 (11): e2025889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Lagerin A, Lundh L, Törnkvist L, et al. District nurses' use of a decision support and assessment tool to improve the quality and safety of medication use in older adults: a feasibility study. Prim Health Care Res Dev 2020; 21: e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Choi Y-S, Lawler E, Boenecke CA, et al. Developing a multi-systemic fall prevention model, incorporating the physical environment, the care process and technology: a systematic review. J Adv Nurs 2011; 67 (12): 2501–24. [DOI] [PubMed] [Google Scholar]
- 62. Fossum M, Ehnfors M, Svensson E, et al. Effects of a computerized decision support system on care planning for pressure ulcers and malnutrition in nursing homes: an intervention study. Int J Med Inform 2013; 82 (10): 911–21. [DOI] [PubMed] [Google Scholar]
- 63. Petersen C, Smith J, Freimuth RR, et al. Recommendations for the safe, effective use of adaptive CDS in the US healthcare system: an AMIA position paper. J Am Med Inform Assoc 2021; 28 (4): 677–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Yu K-H, Kohane IS.. Framing the challenges of artificial intelligence in medicine. BMJ Qual Saf 2019; 28 (3): 238–41. [DOI] [PubMed] [Google Scholar]
- 65. Skaret MM, Weaver TD, Humes RJ, et al. Automation of the I-PASS tool to improve transitions of care. J Healthc Qual 2019; 41 (5): 274–80. [DOI] [PubMed] [Google Scholar]
- 66. Archibald MM, Barnard A.. Futurism in nursing: technology, robotics and the fundamentals of care. J Clin Nurs 2018; 27 (11-12): 2473–80. [DOI] [PubMed] [Google Scholar]
- 67. Hummel J. Integrating Clinical Decision Support Tools into Ambulatory Care Workflows for Improved Outcomes and Patient Safety. Seattle: Qualis Health; 2013. [Google Scholar]
- 68.Agency for Healthcare Research and Quality. Workflow assessment for health IT toolkit. https://digital.ahrq.gov/health-it-tools-and-resources/evaluation-resources/workflow-assessment-health-it-toolkit/presentations. Accessed April 21, 2021.
- 69. Vandenberg AE, van Beijnum B-J, Overdevest VGP, et al. US and Dutch nurse experiences with fall prevention technology within nursing home environment and workflow: A qualitative study. Geriatr Nurs 2017; 38 (4): 276–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Hamer S, Cipriano P.. Involving nurses in developing new technology. Nurs Times 2013; 109 (47): 18–9. [PubMed] [Google Scholar]
- 71. Moen A. A nursing perspective to design and implementation of electronic patient record systems. J Biomed Inform 2003; 36 (4–5): 375–8. [DOI] [PubMed] [Google Scholar]
- 72. Hoffman K, Donoghue J, Duffield C, et al. Decision-making in clinical nursing: investigating contributing factors. J Adv Nurs 2004; 45 (1): 53–62. [DOI] [PubMed] [Google Scholar]
- 73. Reay G, Smith-MacDonald L, Then KL, et al. Triage emergency nurse decision-making: Incidental findings from a focus group study. Int Emerg Nurs 2020; 48: 100791. [DOI] [PubMed] [Google Scholar]
- 74. Ruppel H, Funk M.. Nurse-technology interactions and patient safety. Crit Care Nurs Clin North Am 2018; 30 (2): 203–13. [DOI] [PubMed] [Google Scholar]
- 75. Staggers N, Elias BL, Makar E, et al. The imperative of solving nurses' usability problems with health information technology. J Nurs Adm 2018; 48 (4): 191–6. [DOI] [PubMed] [Google Scholar]
- 76. Dykes PC, Carroll DL, Hurley A, et al. Fall prevention in acute care hospitals: a randomized trial. JAMA 2010; 304 (17): 1912–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Ruland CM. Handheld technology to improve patient care: evaluating a support system for preference-based care planning at the bedside. J Am Med Inform Assoc 2002; 9 (2): 192–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Zhu VJ, Grannis SJ, Tu W, et al. Evaluation of a clinical decision support algorithm for patient-specific childhood immunization. Artif Intell Med 2012; 56 (1): 51–7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data relevant to the study are included in the article or uploaded as online supplemental information. All data relevant to the analysis are reported in the article.