Abstract
The COVID-19 (coronavirus disease 2019) pandemic has expanded telehealth utilization in unprecedented ways and has important implications for measuring geographic access to healthcare services. Established measures of geographic access to care have focused on the spatial impedance of patients in seeking health care that pertains to specific transportation modes and do not account for the underlying broadband network that supports telemedicine and e-health. To be able to measure the impact of telehealth on healthcare access, we created a pilot augmentation of existing methods to incorporate measures of broadband accessibility to measure geographic access to telehealth. A reliable measure of telehealth accessibility is important to enable policy analysts to assess whether the increasing prevalence of telehealth may help alleviate the disparities in healthcare access in rural areas and for disadvantaged populations, or exacerbate the existing gaps as they experience “double burdens.”
Keywords: telehealth access; geographic access; health services research, 2-step virtual catchment area (2SVCA) method, 2-step floating catchment area (2SFCA) method
INTRODUCTION
Access to health care—especially equitable access—is a longstanding concern in healthcare delivery and policy.1–6 The COVID-19 (coronavirus disease 2019) pandemic has brought both renewed awareness of healthcare access and new care delivery patterns, especially related to telehealth.7–10 Typical approaches to characterizing (or measuring) access have yet to incorporate telehealth; thus, new methods to account for both physical and virtual access are urgently needed.
Healthcare access is often measured in terms of geographic access, which is one of the generally accepted components of access along with availability, affordability, acceptability, approachability, and appropriateness.11 Geographic access is generally defined as the availability of healthcare services in a given geographic area that is not inhibited by the availability of transportation or geographic or topographic barriers.12 The measurement of geographic access is typically best achieved by simultaneously evaluating the supply and demand of a particular healthcare service13 across geographic units and the transportation network connecting them. Specifically, the supply (the number of available healthcare services) and demand (the number of individuals or populations seeking the healthcare service) are typically accounted for by a series of measurements related to travel time, sometimes with the rudimentary measure of Euclidean distance, sometimes with travel time measured through spatial network analysis while estimating the decay of the influence of the density of the healthcare service available at a particular geographic locale.4 The travel time measures are typically mapped with a geographic information system (GIS) with an underlying transportation network dataset to characterize the burden of the distance to the healthcare service on populations by a transportation mode.1–3,6,14–17 This approach has been widely adopted and is appropriate for measuring geographic access to in-person healthcare utilization.
Yet, the pandemic yields a unique opportunity to better understand and mitigate geographic access barriers for some healthcare services through the inclusion of telehealth to augment or replace the use of in-person office visits. Estimating the ability to deliver telehealth services is challenging and will need to include a shift toward understanding the impact of broadband on telehealth access. Because the expanded use of telehealth to accommodate healthcare facility closures, reduced capacity, and safety measures18 during the pandemic is likely to persist based on policy shifts and patient preferences, we suggest augmenting the accepted approach to measuring geographic access by incorporating access measures specific to telehealth .
Telehealth visits, especially video visits, are fundamentally dependent on available broadband infrastructure that has consistent and reliable connectivity. Such a shift has major implications for rural communities,10,19–22 in which broadband has been slow to expand and is typically assessed by availability, not durability of connection (specifically, defined for the purposes of this proposed method is measured through broadband download and upload speeds of at least 25 and 3 mbps, respectively, which are generally considered by the Federal Communications Commission [FCC] as the adequate speeds for sustained connectivity).10,21,23 The pandemic has underscored the importance of augmenting traditional measures of healthcare access to include telehealth. This requires reimagining access measures for healthcare catchment areas that are not fully constrained by proximity and travel burden in the same way as in-person care.
Developing appropriate measurement approaches will put a focus on the underlying geography and the inherent, persistent disparities in rural communities21 that have not had resources to support high-demand digital streaming feeds from more sophisticated hospital information technology systems. Given this shift in healthcare services, we propose an approach, demonstrated from existing data, that evaluates the assessment of underlying broadband durability as well as availability in both the patient population and the healthcare system provider areas in Vermont. This approach is the first to integrate both spatial (geographic availability) and virtual accessibility, and has several unique features: (1) it addresses durability of the broadband connections for both provider and patient not simply geographic availability; (2) it accounts for the download and upload speeds for data that could determine the ability for households to support telehealth video (as well as audio), which can be important for symptom management and patient evaluation; and (3) it uses publicly available data from the FCC due to public reporting requirements for telecommunications companies.23 This proposed approach, even as a cursory visual tool, allows the overview of the availability and durability of broadband for the hospitals without the capacity to do in-depth analysis.
For researchers with the capacity and desire to do an in-depth analysis of access accommodating both broadband access and durability, we suggest an enhancement to the generally accepted standard for measuring geographic access called the 2-step floating catchment area (2SFCA) method.5,24 The 2SFCA method employs these basic steps to measure geographic access: (1) characterizing physician supply, establishing the catchment area around the physician location, summarizing the population served, and dividing the available services by population to quantify the supply’s availability; and (2) summing up the availability of supplies within a demand’s catchment area to measure its access. A more generalized version of 2SFCA method introduces a distance decay effect, captured by a continuous or a discrete function or a hybrid between the two, in place of the rigid catchment area.4 In essence, the 2SFCA measure yields an intuitive score of accessibility as the ratio of accessible supply to demand within reach such as number of physicians per 1000 residents, in which both the supply and demand discounted by their distances apart from each other.
A recommended conceptual approach and demonstration for incorporating broadband durability in geographic access methods
Given the evolution of the measurement of geographic access to health service access over the years, we focus on a modification to the popular 2SFCA method, termed the generalized 2SFCA model.4 For physical accessibility at patient location i, PAi, it is written as
| (1) |
where supply capacity at facility j is denoted by Sj, demand amount at location k (or i) is denoted by Dk (or Di), and the interactions between them is a declining function of their physical distance dkj (or dij). For simplicity in this case study, we assume that the distance decay function f(dkj) or f(dij) takes binary values 0 or 1. In other words, when (ie, within the catchment area radius d0); and when (ie, beyond the catchment area radius d0).
In the revised approach, titled the 2-step virtual catchment area (2SVCA), we propose to replace the use of distance decay measures with the download and upload speeds of the underlying geography’s broadband access for which data are available nationally, and in some cases, with better spatial resolution by state.23,25 In other words, the digital transmission speeds at the supply (service provider) and the demand (patient) locations dictate the feasibility and quality of telehealth and the strength of virtual connection between them, equivalent to the distance decay effect in the physical world. Telehealth rarely works completely independently of physical visits to service providers, and often as supplementary consultation to reduce travel burdens for patients,26 and thus takes effect within the provider’s physical catchment area.
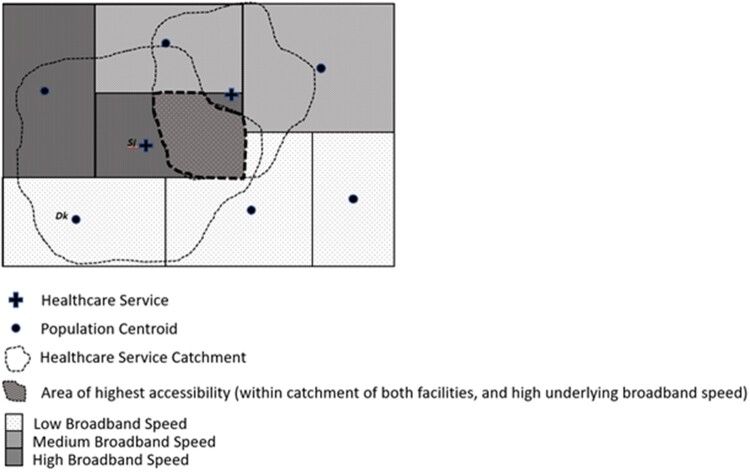
The conceptual model of 2SVCA is illustrated in Figure 1. The virtual accessibility at patient location i, VAi, is expressed as:
| (2) |
where the virtual interaction between facility j and demand location k (or i) (being apart in physical distance dkj or dij) takes place within the physical catchment area d0 and its strength is a function of their broadband strengths or , and all other notations remain the same as in equation 1.
Figure 1.
Conceptualization of the 2-step virtual catchment area method.
In equation 2, the telehealth communication strength in the 2SVCA, or ), is a function of the joint broadband qualities at both demand and supply locations (eg, a product of their durabilities or ), whereas f(dkj) or f(dij) in the 2SFCA indicates that the physical interaction between them is a declining function of their corresponding physical distance dkj or dij. In this 2SVCA model, the telehealth communication strength function is the key innovation, which can be derived from a spatial interaction model2 based on empirical data on telehealth service volume, coverage of broadband durability, and sizes of supply and demand. Here, for simplicity and illustration prior to such an empirically derived function becoming available, they take the binary values, such as = 1 if broadband Internet access is available at both supply and demand locations (ie, ), and = 0 if broadband internet access is not available at either supply or demand (ie, or ), and the same applies to ).
The new measure for telehealth access has 3 desirable properties: (1) it acknowledges the interdepence between physical and virtual access, (2) the quality of telecommunication is a joint effect of broadband durabilities at the service provider and patient locations, and (3) its result retains an intuitive and straighforward interpretation, like the 2SFCA method for geospatial accessibility, as a ratio of service supply capacity and demand volume, which interact beyond geopolitical boundaries but within a physical catchment.
To demonstrate the method, we have chosen to calculate the new telehealth accessibility by the 2SVCA and compare it with the physical accessibility by the traditional 2SFCA in Vermont. Vermont is a largley rural state with a few densely populated urban and suburban areas, and yields good comparison between the methods, and data were readily available. Using the FCC fixed broadband availability dataset,18 available at the U.S. Census Block level data for Vermont,27 and Vermont hospital locations,28 we calculate an origin-destination matrix from all Vermont U.S. Census block origins (n = 32 580) to all 14 hospital locations in Vermont to create a matrix of 456,120 records. Here, the catchment area size d0 is defined as a travel time of 60 minutes. The supply capacity S is defined by total bed size in each hospital and the demand amount D is population size in each block.
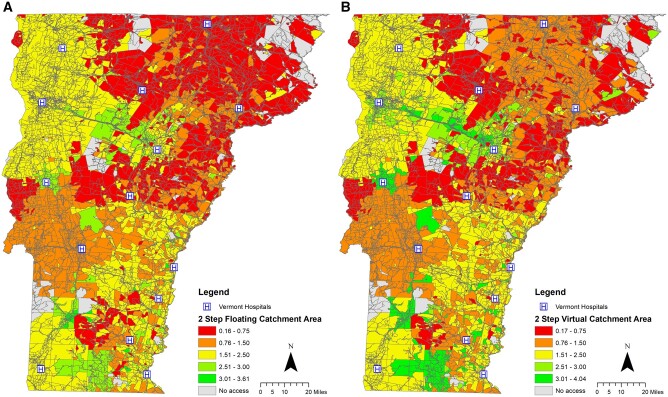
The calibration of physical accessibility by the 2SFCA in equation 1 is implemented in 2 steps: (1) for each hospital, we sum up the total population within its catchment area and calculate the ratio of hospital bed size and the summed-up population as a preliminary measure of hospital availability; and (2) for each census block, we sum up the availability ratios for hospitals, derived from the previous step, within the catchment area of that block as its physical accessibility. The result is shown in Figure 2A.
Figure 2.
Hospital accessibility in Vermont: (A) physical accessibility by 2-step floating catchment area and (B) virtual accessibility by 2-step virtual catchment area.
To calculate the 2SVCA, we follow the same steps as detailed previously with the addition of an accommodation for broadband durability. The FCC fixed broadband file contains multiple records per location due to the fact that multiple providers may service a single census block. We rationalize that an average of the download and upload speeds would give us the most appropriate estimate of the stability and durability of the connection, and calcluate an average of download and upload speeds for each Vermont census block. We consider a census block having broadband access with a minimum download and upload speed of 25 and 3 mbps (ie, ), respectively, and no access otherwise (ie, ). All 14 hospitals have broadband access (ie, ). In implementation, equation 2 is computed similarly to equation 1, while only the blocks with broadband access enter as effective terms in the dominator, and only the hospitals with broadband access (here, all hospitals) enter as effective terms in the numerator. The result is shown in Figure 2B. The spatial pattern of virtual accessibility is largely consistent with that of physical accessibility, but minor discrepancies can be detected by close look. Table 1 summarizes differences in the results by the 2 methods.
Table 1.
Summary statistics for hospital accessibility in Vermont by 2SFCA and 2SVCA
| Statistic | 2SFCA-Derived Physical Accessibility | 2SVCA-Derived Telehealth Accessibility |
|---|---|---|
| Minimum | 0.1623 | 0.1719 |
| Maximum | 3.6066 | 4.0431 |
| Mean | 1.5337 | 1.7395 |
| Standard deviation | 0.7531 | 0.8276 |
2SFCA: 2-step floating catchment area; 2SVCA: 2-step virtual catchment area.
Significance and potential impact
The modification outlined above as demonstrated in our example will provide researchers with a more appropriate measure of access that accounts for telehealth services by examining the durability of the digital infrastructure associated with telehealth delivery. From the pilot example, the overall geographic patterns of hospital accessibility measures are similar, except that with the addition of broadband, the availability scores appear to enhance access in suburban areas of hospital catchments as well as some rural hospital catchment areas. However, there remain pockets of persistent limited geographic access, suggesting an interrelationship between broadband availability and rural locations of the northern most locations of Vermont.
The increased use of telehealth has the potential to bridge some of the healthcare accessibility gaps for rural and isolated communities. To realize that potential, it is imperative that policymakers, healthcare systems, and health services researchers augment their evaluation of geographic access to health care by incorporating measures of virtual access that account for both the speed and durability of the broadband infrastructure for each health system and provider and community served—with a focus on the impact on rural communities. The underlying broadband infrastructure has become arguably as crucial to a patient’s overall healthcare access as a road network is to reaching brick-and-mortar in-person services.
The conventional wisdom seems to suggest that increasing adoption of telehealth might help alleviate the disparity of healthcare access via physical visits of healthcare facilities for rural residents.22 A recent FCC report warns of the “double burdens” for rural counties where broadband access is <50% and physician shortages are most acute.19 In other words, rural residents could face another obstacle in telehealth access due to lack of broadband infrastructure, just like their geographic challenge in making physical visits to healthcare providers. So could be the case of socioeconomically disadvantaged populations (in both rural and urban areas) because of their lack of affordability of broadband service, which has contributed to digital divides.29 With the sustained use of telehealth even after the COVID-19 pandemic, the benefits of broadband infrastructure improvement could extend across the rural-urban continuum.9,10 While this work assumes broadband availability within the healthcare system, future work should limit this assumption because all health systems may not be equipped to host both audio and video telehealth visits.30 Additionally, this example utilizes hospital locations and does not include outpatient facilities, which could alter the geographic accessibility landscape in the pilot study area. An additional important consideration is that the FCC data itself may overestimate the availability of this critical infrastructure, specifically in rural communities.31 Notwithstanding, this example demonstrates that a reliable measure of telehealth accessibility is important to enable policy analysts to assess the impact of the dramatic shift in increase of telehealth services: will it close the gaps or enlarge the divides? What policy or strategy can effectively mitigate any negative outcomes while preserving and enhancing positive gains? For these reasons, we suggest that the generally accepted approaches to measuring geographic access be updated to accommodate this significant shift in the healthcare market.
FUNDING
This work was supported by National Cancer Institute grant number P30CA023108-41S5.
AUTHOR CONTRIBUTIONS
All authors read and approved the manuscript, and each author participated sufficiently in, and stands by, the validity of this work. JA-T designed the study, directed its implementation, drafted the manuscript, and gave final approval for the submission. FW provided technical and conceptual development along with manuscript and scientific review. TO and ANAT provided conceptual development and participated in manuscript and scientific review.
DATA AVAILABILITY STATEMENT
The data underlying this article will be shared on reasonable request to the corresponding author .
CONFLICT OF INTEREST STATEMENT
The authors have no competing interests to declare.
References
- 1. Onega T, Duell EJ, Shi X, Wang D, Demidenko E, Goodman D.. Geographic access to cancer care in the U. S. Cancer 2008; 112 (4): 909–18. [DOI] [PubMed] [Google Scholar]
- 2. Onega T, Hubbard R, Hill D, et al. Geographic access to breast imaging for US women. J Am Coll Radiol 2014; 11 (9): 874–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Shi X, Alford-Teaster J, Onega T, Wang D.. Spatial access and local demand for major cancer care facilities in the United States. Ann Assoc Am Geogr 2012; 102 (5): 1125–34. [Google Scholar]
- 4. Wang F. Measurement, optimization, and impact of health care accessibility: a methodological review. Ann Assoc Am Geogr 2012; 102 (5): 1104–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wang F, Luo W.. Assessing spatial and nonspatial factors for healthcare access: towards an integrated approach to defining health professional shortage areas. Health Place 2005; 11 (2): 131–46. [DOI] [PubMed] [Google Scholar]
- 6. Xu Y, Fu C, Onega T, Shi X, Wang F.. Disparities in geographic accessibility of National Cancer Institute Cancer Centers in the United States. J Med Syst 2017; 41 (12): 203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lonergan PE, Washington SL 3rd, Branagan L, et al. Rapid utilization of telehealth in a comprehensive cancer center as a response to COVID-19: cross-sectional analysis. J Med Internet Res 2020; 22 (7): e19322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Valentino LA, Skinner MW, Pipe S.. The role of telemedicine in the delivery of healthcare in the COVID-19 pandemic. Haemophilia 2020; 26 (5): e230–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wosik J, Fudim M, Cameron B, et al. Telehealth transformation: COVID-19 and the rise of virtual care. J Am Med Inform Assoc 2020; 27 (6): 957–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Curtis K, Alford-Teaster J, Lowry M, et al. Pandemic use of telehealth by oncology at a rural academic medical center. e-Telemedicine2021. https://www.liebertpub.com/doi/10.1089/tmj.2020.0556 [DOI] [PMC free article] [PubMed]
- 11. Levesque J-F, Harris MF, Russell G.. Patient-centred access to health care: conceptualising access at the interface of health systems and populations. Int J Equity Health 2013; 12 (1): 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Primary Health Care Performance Initiative. Geographic access. 2021. https://improvingphc.org/geographic-access#:∼:text=Geographic%20access%20is%20defined%20as,equity%2C%20and%20investments%20into%20infrastructure. Accessed June 22, 2021.
- 13. Wang F, Wang C, Hu Y, Weiss J, Alford-Teaster J, Onega T.. Automated delineation of cancer service areas in northeast region of the United States: a network optimization approach. Spat Spatiotemporal Epidemiol 2020; 33: 100338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Alford-Teaster J, Lange JM, Hubbard RA, et al. Is the closest facility the one actually used? An assessment of travel time estimation based on mammography facilities. Int J Health Geogr 2016; 15 (1): 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. McGrail MR. Spatial accessibility of primary health care utilising the two step floating catchment area method: an assessment of recent improvements. Int J Health Geogr 2012; 11 (1): 50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Onega T, Alford-Teaster J, Wang F.. Population-based geographic access to parent and satellite National Cancer Institute Cancer Center Facilities. Cancer 2017; 123 (17): 3305–11. [DOI] [PubMed] [Google Scholar]
- 17. Onega T, Cook A, Kirlin B, et al. The influence of travel time on breast cancer characteristics, receipt of primary therapy, and surveillance mammography. Breast Cancer Res Treat 2011; 129 (1): 269–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Latifi R, Doarn CR.. Perspective on COVID-19: finally, telemedicine at center stage. Telemed J E Health 2020; 26 (9): 1106–9. [DOI] [PubMed] [Google Scholar]
- 19.Federal Communications Commission. Priority and rural priority. 2017. https://www.fcc.gov/health/maps/priority-and-ruralpriority-2017. Accessed June 22, 2021.
- 20. Blake KD, Croyle RT.. Rurality, rural identity, and cancer control: evidence from NCI's Population Health Assessment in Cancer Center Catchment Areas Initiative. J Rural Health 2019; 35 (2): 141–3. [DOI] [PubMed] [Google Scholar]
- 21. Levit LA, Byatt L, Lyss AP, et al. Closing the rural cancer care gap: three institutional approaches. JCO Oncol Pract 2020; 16 (7): 422–30. [DOI] [PubMed] [Google Scholar]
- 22. Thota R, Gill DM, Brant JL, Yeatman TJ, Haslem DS.. Telehealth is a sustainable population health strategy to lower costs and increase quality of health care in rural Utah. JCO Oncol Pract 2020; 16 (7): e557–62. [DOI] [PubMed] [Google Scholar]
- 23.Federal Communications Commission. Fixed Broadband Deployment. Washington, DC; 2020. https://broadbandmap.fcc.gov/#/. Accessed July 23, 2021.
- 24. Wang F. From 2SFCA to i2SFCA: integration, derivation and validation. Int J Geogr Inf Sci 2021; 35 (3): 628–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Federal Communications Commission. Mapping broadband health in America. 2017. https://www.fcc.gov/health/maps. Accessed June 22, 2021.
- 26. Sorensen MJ, Bessen S, Danford J, Fleischer C, Wong SL.. Telemedicine for surgical consultations - pandemic response or here to stay?: A report of public perceptions. Ann Surg 2020; 272 (3): e174–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.U.S. Census Block Data. Download Center. Washington, DC: U.S. Census Bureau. https://www2.census.gov/geo/tiger/TIGER2010BLKPOPHU/ Accessed July 23, 2021.
- 28.US Hospital Locations with Bed Count, 2017 - hosp geo. 2017. https://hub.arcgis.com/ Accessed July 23, 2021.
- 29. Driskell L, Wang F.. Mapping digital divide in neighborhoods: Wi-Fi access in Baton Rouge, Louisiana. Ann GIS 2009; 15 (1): 35–46. [Google Scholar]
- 30. Hong YR, Lawrence J, Williams D Jr., Mainous IA.. Population-level interest and telehealth capacity of US Hospitals in response to COVID-19: cross-sectional analysis of google search and National Hospital Survey Data. JMIR Public Health Surveill 2020; 6 (2): e18961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Busby J, Tanberk J, BroadbandNow Team. FCC reports broadband unavailable to 21.3 million Americans, BroadbandNow study indicates 42 million do not have access. 2021. https://broadbandnow.com/research/fcc-underestimates-unserved-by-50-percent. Accessed July 23, 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data underlying this article will be shared on reasonable request to the corresponding author .