Abstract
Background
This is an update of the review published on the Cochrane Library in 2016, Issue 8. Having cancer may result in extensive emotional, physical and social suffering. Music interventions have been used to alleviate symptoms and treatment side effects in people with cancer. This review includes music interventions defined as music therapy offered by trained music therapists, as well as music medicine, which was defined as listening to pre‐recorded music offered by medical staff.
Objectives
To assess and compare the effects of music therapy and music medicine interventions for psychological and physical outcomes in people with cancer.
Search methods
We searched the Cochrane Central Register of Controlled Trials (CENTRAL; 2020, Issue 3) in the Cochrane Library, MEDLINE via Ovid, Embase via Ovid, CINAHL, PsycINFO, LILACS, Science Citation Index, CancerLit, CAIRSS, Proquest Digital Dissertations, ClinicalTrials.gov, Current Controlled Trials, the RILM Abstracts of Music Literature, http://www.wfmt.info/Musictherapyworld/ and the National Research Register. We searched all databases, except for the last two, from their inception to April 2020; the other two are no longer functional, so we searched them until their termination date. We handsearched music therapy journals, reviewed reference lists and contacted experts. There was no language restriction.
Selection criteria
We included all randomized and quasi‐randomized controlled trials of music interventions for improving psychological and physical outcomes in adults and pediatric patients with cancer. We excluded patients undergoing biopsy and aspiration for diagnostic purposes.
Data collection and analysis
Two review authors independently extracted the data and assessed the risk of bias. Where possible, we presented results in meta‐analyses using mean differences and standardized mean differences. We used post‐test scores. In cases of significant baseline difference, we used change scores. We conducted separate meta‐analyses for studies with adult participants and those with pediatric participants. Primary outcomes of interest included psychological outcomes and physical symptoms and secondary outcomes included physiological responses, physical functioning, anesthetic and analgesic intake, length of hospitalization, social and spiritual support, communication, and quality of life (QoL) . We used GRADE to assess the certainty of the evidence.
Main results
We identified 29 new trials for inclusion in this update. In total, the evidence of this review rests on 81 trials with a total of 5576 participants. Of the 81 trials, 74 trials included adult (N = 5306) and seven trials included pediatric (N = 270) oncology patients. We categorized 38 trials as music therapy trials and 43 as music medicine trials. The interventions were compared to standard care.
Psychological outcomes
The results suggest that music interventions may have a large anxiety‐reducing effect in adults with cancer, with a reported average anxiety reduction of 7.73 units (17 studies, 1381 participants; 95% confidence interval (CI) ‐10.02 to ‐5.44; very low‐certainty evidence) on the Spielberger State Anxiety Inventory scale (range 20 to 80; lower values reflect lower anxiety). Results also suggested a moderately strong, positive impact of music interventions on depression in adults (12 studies, 1021 participants; standardized mean difference (SMD): −0.41, 95% CI −0.67 to −0.15; very low‐certainty evidence). We found no support for an effect of music interventions on mood (SMD 0.47, 95% CI −0.02 to 0.97; 5 studies, 236 participants; very low‐certainty evidence). Music interventions may increase hope in adults with cancer, with a reported average increase of 3.19 units (95% CI 0.12 to 6.25) on the Herth Hope Index (range 12 to 48; higher scores reflect greater hope), but this finding was based on only two studies (N = 53 participants; very low‐certainty evidence).
Physical outcomes
We found a moderate pain‐reducing effect of music interventions (SMD −0.67, 95% CI −1.07 to −0.26; 12 studies, 632 adult participants; very low‐certainty evidence). In addition, music interventions had a small treatment effect on fatigue (SMD −0.28, 95% CI −0.46 to −0.10; 10 studies, 498 adult participants; low‐certainty evidence).
The results suggest a large effect of music interventions on adult participants' QoL, but the results were highly inconsistent across studies, and the pooled effect size was accompanied by a large confidence interval (SMD 0.88, 95% CI −0.31 to 2.08; 7 studies, 573 participants; evidence is very uncertain). Removal of studies that used improper randomization methods resulted in a moderate effect size that was less heterogeneous (SMD 0.47, 95% CI 0.06 to 0.88, P = 0.02, I2 = 56%).
A small number of trials included pediatric oncology participants. The findings suggest that music interventions may reduce anxiety but this finding was based on only two studies (SMD −0.94, 95% CI −1.9 to 0.03; very low‐certainty evidence). Due to the small number of studies, we could not draw conclusions regarding the effects of music interventions on mood, depression, QoL, fatigue or pain in pediatric participants with cancer.
The majority of studies included in this review update presented a high risk of bias, and therefore the overall certainty of the evidence is low. For several outcomes (i.e. anxiety, depression, pain, fatigue, and QoL) the beneficial treatment effects were consistent across studies for music therapy interventions delivered by music therapists. In contrast, music medicine interventions resulted in inconsistent treatment effects across studies for these outcomes.
Authors' conclusions
This systematic review indicates that music interventions compared to standard care may have beneficial effects on anxiety, depression, hope, pain, and fatigue in adults with cancer. The results of two trials suggest that music interventions may have a beneficial effect on anxiety in children with cancer. Too few trials with pediatric participants were included to draw conclusions about the treatment benefits of music for other outcomes. For several outcomes, music therapy interventions delivered by a trained music therapist led to consistent results across studies and this was not the case for music medicine interventions. Moreover, evidence of effect was found for music therapy interventions for QoL and fatigue but not for music medicine interventions. Most trials were at high risk of bias and low or very low certainty of evidence; therefore, these results need to be interpreted with caution.
Plain language summary
Can music interventions benefit people with cancer?
The issue Cancer may result in extensive emotional, physical and social suffering. Music therapy and music medicine interventions have been used to alleviate symptoms and treatment side effects and address psychosocial needs in people with cancer. In music medicine interventions, patients simply listen to pre‐recorded music that is offered by a medical professional. Music therapy requires the implementation of a music intervention by a trained music therapist, the presence of a therapeutic process and the use of personally tailored music experiences.
The aim of the review This review is an update of a previous Cochrane review from 2016, which included 52 studies. For this review update, we searched for additional trials studying the effect of music interventions on psychological and physical outcomes in people with cancer. We searched for studies up to April 2020.
What are the main findings? We identified 29 new studies, so the evidence in this review update now rests on 81 studies with 5576 participants. Of the 81 studies, 74 trials included adults and 7 included children.The findings suggest that music therapy and music medicine interventions may have a beneficial effect on anxiety, depression, hope, pain, fatigue, heart rate and blood pressure in adults with cancer. Music therapy but not music medicine interventions may improve adult patients' quality of life and levels of fatigue. We did not find evidence that music interventions improve mood, distress or physical functioning, but only a few trials studied these outcomes. We could not draw any conclusions about the effect of music interventions on immunologic functioning, resilience, spiritual well‐being or communication outcomes in adults because there were not enough trials looking at these aspects. Due to the small number of trials, we could not draw conclusions for children. Therefore, more research is needed.
Overall, the treatment benefits of music therapy interventions were more consistent across trials than those of music medicine interventions, leading to greater confidence in the treatment impact of music therapy interventions delivered by a trained music therapist.
No adverse effects of music interventions were reported.
Quality of the evidence Most trials were at high risk of bias, so these results need to be interpreted with caution. We did not identify any conflicts of interests in the included studies.
What are the conclusions? We conclude that music interventions may have beneficial effects on anxiety, depression, hope, pain, and fatigue in adults with cancer. Furthermore, music may have a small positive effect on heart rate and blood pressure. Reduction of anxiety, depression, fatigue and pain are important outcomes for people with cancer, as they have an impact on health and overall quality of life.
Summary of findings
Background
Description of the condition
The lifetime risk of developing any type of cancer is 40% for men and 38% for women (Howlader 2019), and a diagnosis of cancer may result in extensive emotional, physical and social suffering. Many symptoms and treatment side effects have an impact on cancer patients' physical well‐being and quality of life (QoL), including appetite disturbance, difficulty swallowing, nausea, vomiting, constipation, diarrhea, dyspnea or difficulty breathing, fatigue, insomnia, muscle weakness and numbness (King 2003). In addition, study findings clearly indicate that people with cancer experience elevated levels of psychological distress and depression in response to diagnosis and treatment (Massie 2004; Norton 2004; Parle 1996; Raison 2003; Sellick 1999; Van't Spijker 1997). The actual experience of chemotherapy‐induced side effects, such as nausea and vomiting, and their influence on psychological well‐being varies widely in patients receiving the same cytotoxic agents. This suggests that non‐pharmacological factors possibly play an important role in how patients experience or interpret physical symptoms during the treatment phase (Montgomery 2000; Thune‐Boyle 2006). It is therefore important that cancer care incorporates services that help meet patients' psychological, social and spiritual needs.
Description of the intervention
The use of music in cancer care can be situated along a continuum of care, namely from music listening initiated by patients, to pre‐recorded music offered by medical personnel, to music psychotherapy interventions offered by a trained music therapist. Therefore, when examining the efficacy of music interventions in people with cancer, it is important to make a clear distinction between music interventions administered by medical or healthcare professionals (music medicine) and those implemented by trained music therapists (music therapy). A substantive body of evidence suggests that music therapy interventions provided by music therapists are more effective than music medicine interventions for a wide variety of outcomes (Dileo 2005). This difference might be attributed to the fact that music therapists individualize their interventions to meet patients' specific needs, more actively engage the patients in music‐making, and employ a systematic therapeutic process including assessment, treatment and evaluation. Dileo 1999 categorizes interventions as music medicine when medical personnel offer pre‐recorded music for passive listening. For example, they may offer people a compact disc (CD) for relaxation or distraction; however, no systematic therapeutic process is present, nor is there a systematic assessment of the elements and suitability of the music stimulus. In contrast, music therapy requires the implementation of a music intervention by a trained music therapist, the presence of a therapeutic process and the use of personally tailored music experiences.
These tailored music experiences include:
listening to live, improvised or pre‐recorded music;
performing music on an instrument;
improvising music spontaneously using voice, instruments or both;
composing music;
combining music with other therapeutic modalities (e.g. movement, imagery, art) (Dileo 2007).
How the intervention might work
Music interventions have been used in different medical fields to meet patients' psychological, physical, social and spiritual needs. Research on the effects of music and music therapy for medical patients has burgeoned over the past 20 years, examining a variety of outcome measures in a wide range of specialty areas (Dileo 2005). For both adult and pediatric cancer patients, music has been used to decrease anxiety prior to or during surgical procedures (Alam 2016; Burns 1999; Haun 2001), to decrease stress during chemotherapy or radiation therapy (Bradt 2015; Bro 2019; Clark 2006), to lessen treatment side effects (Bozcuk 2006; Ezzone 1998; Frank 1985), to improve mood (Barrera 2002; Burns 2001a; Cassileth 2003), to enhance pain management (Akombo 2006; Arruda 2016; Beck 1989; Verstegen 2018), to improve immune system functioning (Burns 2001a), and to improve quality of life (QoL) (Burns 2001a; Hilliard 2003; Porter 2018).
There are inherent elements of music — such as rhythm and tempo, mode, pitch, timbre, melody and harmony — that are known to influence physiological and psycho‐emotional responses in humans. For example, music has been found to arouse memory and association, stimulate imagery, evoke emotions, facilitate social interaction, and promote relaxation and distraction (Dileo 2006). In cancer settings, music therapists conduct ongoing assessments and utilize various individualized interventions in people with cancer and their families, including pertinent elements of music within the context of therapeutic relationships, to address prevailing biopsychosocial and spiritual issues, symptoms and needs (Magill 2009; McClean 2012). The following music therapy interventions are common: use of songs (singing, song writing, and lyric analysis); music improvisation (instrumental and vocal), music and imagery, music‐based reminiscence and life review, chanting and toning, music‐based relaxation, and instrumental participation (O'Callaghan 2015). Based on patient preferences and assessment outcomes, music therapists adapt and modify music interventions to address symptoms and areas of difficulty; they utilize music and verbal strategies to provide opportunities for expression and communication, reminiscence, the processing of thoughts and emotions and improvement of symptom management (Magill 2011). Therapist‐supported music therapy environments often provide the space and time through which patients and families may experience social connection, improve self fulfilment and acquire effective coping strategies (Magill 2015).
Why it is important to do this review
Several research studies on the use of music with cancer patients have reported positive results (Beck 1989; Bradt 2015; Cassileth 2003; Harper 2001; Hilliard 2003; Robb 2008). The majority of these studies, however, are compromised by small sample size and lack of statistical power. In addition, differences in factors such as methods of interventions and type and intensity of treatment have led to varying results. A systematic review is needed to more accurately gauge the efficacy of music interventions in cancer patients as well as to identify variables that may moderate its effects.
Objectives
To assess and compare the effects of music therapy and music medicine interventions for psychological and physical outcomes in people with cancer.
Methods
Criteria for considering studies for this review
Types of studies
All randomized controlled trials (RCTs) and studies with quasi‐randomized methods of treatment allocation (e.g. alternate allocation of treatments) were eligible for inclusion.
Types of participants
This review included participants diagnosed with any type of cancer. We included studies that included a few participants (< 10% of total sample size) with non‐cancer diagnoses (e.g. aplastic anemia). There were no restrictions as to age, sex, ethnicity or type of setting. We did exclude participants undergoing biopsy, bone marrow biopsy and aspiration for diagnostic purposes. This review did not include studies with cancer survivors.
Types of interventions
The review included all trials comparing standard treatment plus music therapy or music medicine interventions (as defined in the Background; Description of the intervention) with:
standard care alone;
standard care plus alternative intervention (e.g. music therapy versus music medicine);
standard care plus placebo.
Placebo treatment can involve the use of headphones for the participant without provision of music stimuli or with another type of auditory stimulus (e.g. audiobooks, white noise (hiss), pink noise (sound of ocean waves) or nature sounds).
Music therapy and music medicine interventions were pooled in the same analysis but, where possible, subgroup analyses were conducted to compare the effects of music therapy and music medicine interventions as outlined in the Subgroup analysis and investigation of heterogeneity section.
Types of outcome measures
Primary outcomes
Psychological outcomes (e.g. state anxiety, depression, distress, mood, hope, resilience)
Physical symptoms (e.g. fatigue, pain)
Secondary outcomes
Physiological outcomes (e.g. heart rate, respiratory rate, systolic blood pressure, diastolic blood pressure, mean arterial pressure, oxygen saturation, immune system functioning)
Physical functioning
Anesthetic and analgesic intake
Length of hospitalization and recovery time
Social and spiritual support (e.g. spiritual well‐being, social support)
Communication (e.g. verbalization, facial affect, gestures)
Quality of life (QoL)
We presented a 'Table 1 and Table 2 reporting the following outcomes: anxiety, depression, mood, hope, pain, fatigue, and QoL.
Summary of findings 1. Music intervention plus standard care compared to standard care alone for improving psychological and physical outcomes in adult cancer patients.
| Music intervention plus standard care compared to standard care alone for improving psychological and physical outcomes in adult cancer patients | ||||
| Patient or population: adult cancer patients (≥ 18 years) Setting: inpatient and outpatient cancer care Intervention: music intervention (music therapy or music medicine) plus standard care Comparison: standard care alone (i.e. usual cancer treatment as per the site's standard care protocol) | ||||
| Outcomes* |
Illustrative Comparative Risk
(95% CI) __________________ Corresponding Risk __________________ Music intervention |
№ of participants (studies) | Certainty of the evidence (GRADE) | Comments |
| Anxiety assessed with: Spielberger State Anxiety Index Scale (STAI) Score range: 20 to 80. A lower score represents less anxiety. Follow‐up: immediately post‐intervention |
The mean anxiety in the music intervention group was 7.73 units less (10.02 less to 5.44 less) than in the standard care group. | 1381 (17 RCTs) | ⊕⊝⊝⊝ VERY LOW 1 2 | Music intervention may result in a large reduction in anxiety. However, the evidence is very uncertain. |
| Depression Follow‐up: immediately post‐intervention |
The mean depression in the music intervention group was 0.41 standard deviations less (0.67 worse to 0.15 worse) than in the standard care group | 1021 (12 RCTs) | ⊕⊝⊝⊝ VERY LOW 1 3 | Music intervention may result in a small to moderate reduction of depression. However, the evidence is very uncertain. |
| Mood Follow‐up: immediately post‐intervention |
The mean mood in the music intervention group was 0.53 standard deviations better (0.03 worse to 1.11 better) than in the standard care group | 221 (4 RCTs) | ⊕⊝⊝⊝ VERY LOW 1 4 | Music interventions may result in a moderate improvement in mood. However, the evidence is very uncertain. |
| Hope Score range: 12 to 48. A higher score represents greater hope. Follow‐up: immediately post‐intervention |
The mean hope in the music intervention group was 3.19 units more (0.12 more to 6.25 more) than in the standard care group | 53 (2 RCTS |
⊕ ⊝ ⊝⊝ VERY LOW 1 7 |
Music intervention may result in a large increase in hope. However, the evidence is very uncertain. |
| Pain Follow‐up: immediately post‐intervention |
The mean pain in the intervention group was 0.67 standard deviations less (1.07 less to 0.26 less) than in the standard care group | 632 (12 RCTs) | ⊕⊝⊝⊝ VERY LOW 1 5 | Music interventions may result in a moderate to large improvement in pain. However, the evidence is very uncertain. |
| Fatigue Follow‐up: immediately post‐intervention |
The mean fatigue in the music intervention group was 0.28 standard deviations less (0.46 less to 0.01 less) than in the standard care group | 498 (10 RCTs) | ⊕⊕⊝⊝ LOW 1 | Music intervention may result in a slight reduction in fatigue. |
| Quality of Life Follow‐up: immediately post‐intervention |
The mean quality of life in the music intervention group was 0.88 standard deviations more (0.31 less to 2.08 more) than in the standard care group | 573 (7 RCTs) | ⊕⊝⊝⊝ VERY LOW 1 6 | Music interventions may result in a large improvement in quality of life. However, the evidence is very uncertain. |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval | ||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||
1 Downgraded two levels for high risk of bias. The majority of the trials were at high risk of bias because participants could not be blinded to the music intervention and outcome was measured using self‐report.
2 Downgraded two levels for very serious inconsistency across studies as evidenced by I2 = 93%.
3 Downgraded one level for serious inconsistency across studies as evidenced by I2 = 72%.
4 Downgraded one level for serious inconsistency across trials as evidenced by I2 = 70%.
5 Downgraded two levels for very serious inconsistency across trials as evidenced by I2 = 81%.
6 Downgraded two levels for very serious inconsistency across trials as evidenced by I2 = 97%.
7 Downgraded two level s for imprecision due to a small number of participants.
Summary of findings 2. Music intervention plus standard care compared to standard care alone for improving psychological and physical outcomes in paediatric cancer patients.
| Music intervention plus standard care compared to standard care alone for improving psychological and physical outcomes in pediatriccancer patients | ||||
| Patient or population: pediatric cancer patients (< 18 years) Setting: inpatient and outpatient cancer care Intervention: music interventions (music therapy or music medicine) plus standard care Comparison: standard care alone (i.e. usual cancer treatment as per the site's standard care protocol) | ||||
| Outcomes |
Illustrative comparative risk (95% CI) ____________________ Corresponding risk ____________________ Music intervention |
№ of participants (studies) | Certainty of the evidence (GRADE) | Comments |
| Anxiety (STAI) The score: 20 to 80. A lower score represents less anxiety. Follow‐up: immediately post‐intervention |
The mean anxiety in the music intervention group was 0.94 standard lower (1.9 lower to 0.03 higher) | 79 (2 RCTs) | ⊕⊝⊝⊝ VERY LOW 1 2 3 | Music intervention may result in a large reduction in anxiety. |
| Depression | not estimable | (0 studies) | ‐ | |
| Mood | not estimable | (0 studies) | ‐ | |
| Pain assessed with: 0 to 10 NRS. A higher score represents more pain | Listening to pre‐recorded music resulted in less pain during and after lumbar puncture (during mean: 2.35, SD 1.9; after mean: 1.2, SD 1.36) than standard care (during mean: 5.65, SD 2.5; after mean: 3.0, SD 2.0 ). | 40 (1 RCT) | ⊕ ⊝ ⊝ ⊝ LOW 1 3 |
|
| Fatigue | not estimable | (0 studies) | ‐ | |
| Quality of Life | not estimable | (0 studies) | ‐ | |
| Hope | not estimable | (0 studies) | ‐ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; OR: Odds ratio; | ||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||
1 Downgraded two levels for high risk of bias. These trials were at high risk of bias because participants could not be blinded to the music intervention and outcome was measured using self‐report.
2 Downgraded one level for serious inconsistency across studies as evidenced by I2 = 76%.
3 Downgraded two levels for imprecision due to a small number of participants.
Search methods for identification of studies
There were no language restrictions for either searching or trial inclusion.
Electronic searches
We searched the following electronic databases and trials registers for the updated review:
Cochrane Central Register of Controlled Trials (CENTRAL; 2020, Issue 3), in the Cochrane Library (Appendix 1);
MEDLINE via Ovid (January 2016 to March, week 3, 2020) (Appendix 2);
Embase via Ovid (January 2016 to 2020, week 13) (Appendix 3);
CINAHL (EbscoHost)(January 2016 to April 16 2020) (Appendix 4);
PsycINFO (OvidSp) (January 2016 to April 16 2020) (Appendix 5);
LILACS (Virtual Health Library) (2016 to April 2020) (Appendix 6).
The Science Citation Index (ISI) (2016 to April 2020) (Appendix 7).
CancerLit (2016 to 2003) (http://www.cancer.gov) (Appendix 8).
CAIRSS for Music (2016 to April 2020) (http://ucairss.utsa.edu/) (Appendix 9).
Proquest Digital Dissertations (Proquest) (to April 2020) (Appendix 10).
ClinicalTrials.gov (http://www.clinicaltrials.gov/) (to April 2020) (Appendix 11).
Current Controlled Trials (http://www.controlled-trials.com/) (to April 2020) (Appendix 12).
National Research Register (http://www.update-software.com/National/) (inception to September 2010; the NRR is no longer active) (Appendix 13).
http://www.wfmt.info/Musictherapyworld/ (database is no longer functional) (to March 2008) .
RILM Abstracts of Music Literature (EbscoHost) (to April 2020) (Appendix 14).
Searching other resources
We handsearched the following journals from first available date to December 2020:
Australian Journal of Music Therapy.
Australian Music Therapy Association Bulletin.
Canadian Journal of Music Therapy.
International Journal of the Arts in Medicine.
Journal of Music Therapy.
Musik‐,Tanz‐, und Kunsttherapie (Journal for Art Therapies in Education, Welfare and Health Care).
Musiktherapeutische Umschau.
Music Therapy.
Music Therapy Perspectives.
Nordic Journal of Music Therapy;
Music Therapy Today (online journal of music therapy).
Voices (online international journal of music therapy).
New Zealand Journal of Music Therapy.
Arts in Psychotherapy.
British Journal of Music Therapy.
Music and Medicine.
Approaches.
In an effort to identify further published, unpublished and ongoing trials, we searched the bibliographies of relevant trials and reviews, contacted experts in the field, and searched available proceedings of music therapy conferences. We consulted music therapy association websites to help identify music therapy practitioners and conference information (e.g. the American Music Therapy Association at www.musictherapy.org and the British Association for Music Therapy at http://www.bamt.org). We also handsearched the website of the Deutsches Zentrum fur Musiktherapieforschung (www.dzm-heidelberg.de/forschung/publikationen/) and the research pages of the PhD programs that are listed on the website of the European Music Therapy Confederation (emtc-eu.com/music-therapy-research/).
Data collection and analysis
Selection of studies
We divided the responsibility of the searches, as outlined in the search strategy, amongst JBr, JBi and KMC. JBr, JBi, and KMC scanned titles and abstracts of each record retrieved from the search and deleted obviously irrelevant references. When we could not reject a title or abstract with certainty, we consulted the other review author. We used an inclusion criteria form to assess the trial's eligibility for inclusion (Appendix 15). We kept a record of all excluded trials that initially appeared eligible and the reason for exclusion.
Data extraction and management
JBi and KMC independently extracted data from the selected trials using a standardized coding form. We discussed differences in data extraction until reaching a consensus. We extracted the following data.
General information
Author
Year of publication
Title
Journal (title, volume, pages)
If unpublished, source
Duplicate publications
Country
Language of publication
Intervention information
Type of intervention (e.g. singing, song‐writing, music listening, music improvisation)
Music selection (detailed information on music selection in case of music listening)
Music preference (patient‐preferred versus researcher‐selected in case of music listening)
Level of intervention (music therapy versus music medicine, as defined by the authors in the Background ; Description of the intervention)
Length of intervention
Frequency of intervention
Comparison intervention
Participant information
Total sample size
Number in experimental group
Number in control group
Sex
Age
Ethnicity
Diagnosis
Illness stage
Setting
Inclusion criteria
Outcomes
We extracted pre‐test means, post‐test means, standard deviations and sample sizes for the treatment group and the control group for the following outcomes (if applicable). For some trials, only change scores, instead of post‐test scores, were available.
Psychological outcomes (e.g. depression, anxiety, anger, hopelessness, helplessness)
Physical symptoms (e.g. fatigue, nausea, pain)
Physiological outcomes (e.g. heart rate, respiratory rate, immunoglobulin A (IgA) levels)
Social and spiritual support (e.g. family support, spirituality, social activity, isolation)
Communication (e.g. verbalization, facial affect, gestures)
Quality of life
Assessment of risk of bias in included studies
Two review authors (JBr and CD) assessed all included trials for risk of bias for the original review. New studies included in this update were assessed for risk of bias by CD, JBi and KMC (two reviewers per study). All authors were blinded to each other's assessments. JBr reviewed the reviewer authors' decisions. When there was no consensus between the two reviewer authors, JBr provided input to reach consensus. We resolved any disagreements by discussion. The authors used the following criteria for quality assessment.
Random sequence generation
Low risk
Unclear risk
High risk
We rated trials to be at low risk for random sequence generation if every participant had an equal chance to be selected for either condition, and the investigator was unable to predict which treatment the participant would be assigned to. Use of date of birth, date of admission or alternation resulted in a judgement of high risk of bias.
Allocation concealment
-
Low risk methods to conceal allocation include:
central randomization;
serially numbered, opaque, sealed envelopes;
other descriptions with convincing concealment.
Unclear risk ‐ authors did not adequately report on method of concealment
High risk (e.g. trials used alternation methods)
Blinding of participants and personnel
Low risk
Unclear risk
High risk
Since participants cannot be blinded in a music intervention trial, we did not downgrade studies for not blinding the participants. As for personnel, in music therapy studies, music therapists cannot be blinded because they are actively making music with the participants. In contrast, in music medicine studies, blinding of personnel is possible by providing control group participants with headphones but no music (e.g. blank CD). Therefore, downgrading for not blinding personnel was only applied in studies that used listening to pre‐recorded music.
Blinding of outcome assessors
Low risk
Unclear risk
High risk
When the study included no objective outcomes, we noted this in the Characteristics of included studies table, and we rated the trial as being at low risk of bias for outcome assessment of objective outcomes. The majority of the studies used self‐report measures for subjective outcomes. We rated these studies as being at high risk of bias for subjective outcomes, unless study participants were blinded to the study hypothesis (for comparative studies).
Incomplete outcome data
We recorded the proportion of participants whose outcomes were analyzed. We coded loss to follow‐up for each outcome as:
low risk: if fewer than 20% of participants were lost to follow‐up and reasons for loss to follow‐up were similar in both treatment arms;
unclear risk: if loss to follow‐up was not reported;
high risk: if more than 20% of participants were lost to follow‐up or reasons for loss to follow‐up differed between treatment arms.
Selective reporting
Low risk: reports of the study were free from suggestions of selective outcome reporting
Unclear risk
High risk: reports of the study suggested selective outcome reporting
Other sources of bias
Low risk
Unclear risk
High risk
We considered information on potential financial conflicts of interest to be a possible source of additional bias.
The above criteria were used to give each article an overall quality rating (based on section 8 of the Cochrane Handbook for Systematic Reviews of Interventions;Higgins 2021).
Low risk of bias ‐ all criteria met.
Moderate risk of bias ‐ one or more of the criteria only partly met.
High risk of bias ‐ one or more criteria not met.
Studies were not excluded based on a low quality score. We planned to use the overall quality assessment rating for sensitivity analysis. However, since most trials were at high risk of bias, we could not carry out this analysis.
Measures of treatment effect
We presented all outcomes in this review as continuous variables. We calculated standardized mean differences with 95% confidence intervals (CI) for outcome measures using results from different scales. When there were sufficient data available from various studies using the same measurement instrument, we computed a mean difference (MD) with 95% CI.
For cross‐over studies, if no carry‐over effects or period effects were apparent, we used data from the paired analyses in the meta‐analysis using a generic inverse‐variance approach. If paired analyses were not reported, we approximated the mean difference or standardized mean difference using methods outlined in Elbourne 2002. If carry‐over or period effects were present, the cross‐over trial were excluded from the meta‐analysis.
Unit of analysis issues
In all studies included in this review, participants were individually randomized to the intervention or the standard care control group. Post‐test values or change values on a single measurement for each outcome from each participant were collected and analyzed.
Dealing with missing data
We did not impute missing outcome data. We analyzed data on an endpoint basis, including only participants for whom final data point measurement was available (available case analysis). We did not assume that participants who dropped out after randomization had a negative outcome.
Assessment of heterogeneity
We investigated heterogeneity using visual inspection of the forest plots as well as the I2 statistic (Higgins 2002).
Assessment of reporting biases
We tested for publication bias visually in the form of funnel plots (Higgins 2021).
Data synthesis
We presented all outcomes in this review as continuous variables. We calculated standardized mean differences (SMD) for outcome measures using results from different scales. We used mean differences (MD) for results using the same scales. We anticipated that some individual trials would have used final scores and others change scores and even analysis of covariance (ANCOVA) in their statistical analyses of the results. We combined these different types of analyses as MDs. We calculated pooled estimates using the more conservative random‐effects model. We calculated 95% confidence intervals (CI) for each effect size estimate. We interpreted the magnitude of the SMDs using the interpretation guidelines put forth by Cohen 1988. Cohen suggested that an effect size of 0.2 be considered a small effect, an effect size of 0.5 medium, and an effect size of 0.8 large.
We made the following treatment comparisons in meta‐analyses:
Music interventions plus standard care versus standard care alone in adults.
Music interventions plus standard care versus standard care alone in children.
Music interventions plus standard care versus standard care plus placebo control in children.
Music therapy plus standard care versus music medicine plus standard care in adults.
In the update of this review, we separated pediatric studies (participants < 18 years of age) from adult clinical trials for data synthesis. In prior versions of this review, these studies were combined in meta‐analyses.
Subgroup analysis and investigation of heterogeneity
We conducted the following subgroup analyses within the music interventions plus standard care versus standard care alone comparison for outcomes with a sufficient number of available studies.
Music medicine versus music therapy.
Type of intervention (e.g. music listening alone versus music‐guided relaxation).
Music preference (patient‐preferred music versus researcher‐selected music).
We planned the following subgroup analyses a priori, but we could not carry these out because of insufficient numbers of trials per outcome for age subgroup analysis and because no separate data were available according to stage of illness.
Different age groups.
Stages of illness.
We conducted subgroup analyses as described by Deeks 2001 and recommended in section 10.10 of Higgins 2021.
Sensitivity analysis
We examined the impact of sequence generation by comparing the results of including and excluding trials that used inadequate or unclear randomization methods. We also examined whether the inclusion of studies with non‐cancer participants (< 10%) had an impact on the pooled effect size.
Summary of findings and assessment of the certainty of the evidence
We presented the overall certainty of the evidence for each outcome (see Types of outcome measures) according to the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach, which takes into account issues not only related to internal validity (risk of bias, inconsistency, imprecision, publication bias) but also to external validity such as directness of results (Langendam 2013; Schünemann 2011). We presented a summary of findings table (see Table 1) based on the methods described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2021) and using GRADEpro 2020. We used the GRADE checklist and GRADE Working Group certainty of evidence definitions (Meader 2014). We downgraded the evidence from 'high' certainty by one level for serious (or by two for very serious) concerns study for limitations for each outcome:
High‐certainty: We are very confident that the true effect lies close to that of the estimate of the effect.
Moderate‐certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different.
Low‐certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect.
Very low‐certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect
Results
Description of studies
Results of the search
For the original review, the database searches and handsearching of conference proceedings, journals and reference lists resulted in 773 unique citations. One review author (JBr) and a research assistant examined the titles and abstracts and identified 101 reports as potentially relevant, which we retrieved for further assessment. One review author (JBr) and a research assistant then independently screened them. We included 30 trials, reported in 36 records, in the original review. Where necessary, we contacted principal investigators to obtain additional details on trials and data.
The 2016 update of the search resulted in 1187 unique citations. Two review authors (JBr and AT) and one research assistant examined the titles and abstracts, retrieving full‐text articles, where necessary. This resulted in the addition of 25 references reporting on 22 trials (Figure 1) and three new ongoing trials (Mondanaro 2020; NCT02583139; NCT0258312).
1.
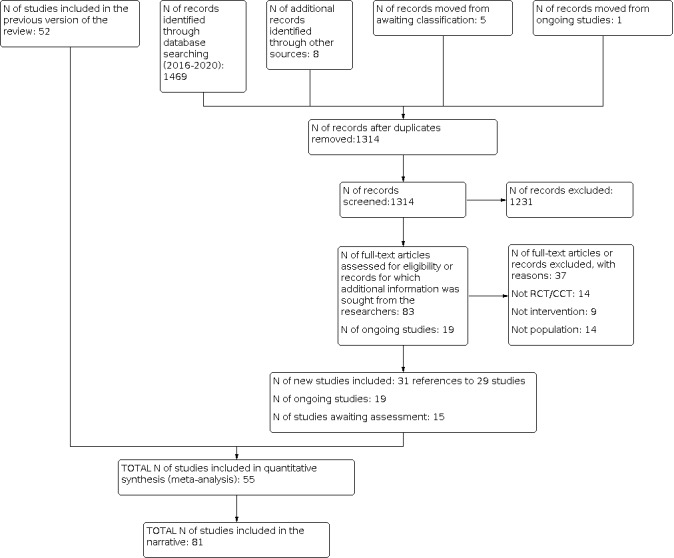
Study flow diagram.
The 2020 update of the search resulted in 1314 unique citations. Two review authors (JBi and KMC) examined the titles and abstracts, retrieving full‐text articles, where necessary. A research assistant helped with article retrieval. This resulted in the addition of 31 references reporting on 29 trials (Figure 1). In addition, we identified 19 ongoing trials (see Characteristics of ongoing studies) and 15 trials awaiting assessment (see Characteristics of ongoing studies) including Mondanaro 2020, which was an ongoing study in the 2016 update and has since been published.
Included studies
We included a total of 81 trials (74 trials with 5306 adult participants and seven trials focused on 270 pediatric oncology participants). Twenty‐six trials included participants who underwent chemotherapy or radiation therapy (Alcantara‐Silva 2018; Bradt 2015; Bro 2019; Bulfone 2009; Burns 2018; Burrai 2014; Cai 2001; Chen 2013; Chen 2020; Clark 2006; Ferrer 2005; Firmeza 2017; Gimeno 2008; Hunter 2020; Jin 2011; Karadag 2019; Lin 2011; Moradian 2015; O'Callaghan 2012; Romito 2013; Rossetti 2017; Smith 2001; Straw 1991; Tuinmann 2017; Xie 2001; Zhao 2008), 23 trials examined the effects of music during procedures or surgery (Alam 2016; Bates 2017; Binns‐Turner 2008; Burns 2009; Cassileth 2003; Danhauer 2010; Doro 2017; Fredenburg 2014a; Fredenburg 2014b; Kwekkeboom 2003; Li 2004; Li 2012; Mou 2020; Pedersen 2020; Palmer 2015; Pinto 2012; Ratcliff 2014; Rosenow 2014; Vachiramon 2013; Wang 2015; Wren 2019; Yates 2015; Zhou 2015), and 25 trials included general cancer participants (Arruda 2016; Beck 1989; Bieligmeyer 2018; Burns 2001a; Burns 2008; Chen 2004; Chen 2018; Cook 2013; Hanser 2006; Harper 2001; Hilliard 2003; Horne‐Thompson 2008; Huang 2006; Jasemi 2016; Keenan 2017; Letwin 2017; Liao 2013; Porter 2018; Ramirez 2018; Reimnitz 2018; Shaban 2006; Verstegen 2016; Verstegen 2018; Wan 2009; Warth 2015). Seven trials (N = 270) examined music interventions in pediatric participants (Bufalini 2009; Burns 2009; Duocastella 1999; Nguyen 2010; Robb 2008; Robb 2014; Robb 2017). Four trials included a few participants (< 10% of total sample size) who had a hematological disease but did not have a cancer diagnosis (e.g. aplastic anemia) (Horne‐Thompson 2008; Porter 2018; Reimnitz 2018; Verstegen 2018).
This review included 3238 adult females and 1809 adult males. The pediatric trials included 103 females and 144 males. Five trials did not provide information on the distribution between sexes (Danhauer 2010; Jin 2011; Robb 2008; Shaban 2006; Xie 2001). The average age of the participants was 54.72 years for adult trials and 11.12 years for pediatric trials.
Thirty‐one studies did not report on the ethnicity of the participants (Alam 2016; Arruda 2016; Bieligmeyer 2018; Bro 2019; Burns 2001a; Burns 2008; Burrai 2014; Cassileth 2003; Chen 2013; Chen 2018; Chen 2020; Cook 2013; Doro 2017; Duocastella 1999; Ferrer 2005; Firmeza 2017; Horne‐Thompson 2008; Jasemi 2016; Karadag 2019; Letwin 2017; Lin 2011; Moradian 2015; Mou 2020; O'Callaghan 2012; Pedersen 2020; Robb 2008; Romito 2013; Straw 1991; Vachiramon 2013; Wang 2015; Zhou 2015). For trials that did provide information on ethnicity, the distribution was as follows: 56% white, 25% Asian, 10% black, 6% Latino, and 3% other.
The trials took place in 13 different countries: the United States (Alam 2016; Bates 2017; Bradt 2015; Burns 2018; Beck 1989; Binns‐Turner 2008; Burns 2001a; Burns 2008; Burns 2009; Cassileth 2003; Clark 2006; Cook 2013; Danhauer 2010; Ferrer 2005; Fredenburg 2014a; Fredenburg 2014b; Hanser 2006; Harper 2001; Hilliard 2003; Hunter 2020; Keenan 2017; Kwekkeboom 2003; Letwin 2017; Gimeno 2008; Palmer 2015; Ratcliff 2014; Reimnitz 2018; Robb 2008; Robb 2014; Robb 2017; Rosenow 2014; Rossetti 2017; Smith 2001; Straw 1991; Vachiramon 2013; Verstegen 2016; Verstegen 2018; Wren 2019; Yates 2015), China (Cai 2001; Chen 2004; Chen 2020; Jin 2011; Li 2004; Li 2012; Liao 2013; Mou 2020; Wan 2009; Xie 2001; Zhao 2008), Denmark (Bro 2019; Pedersen 2020), Germany (Bieligmeyer 2018; Tuinmann 2017; Warth 2015), Italy (Bufalini 2009; Bulfone 2009), Iran (Jasemi 2016; Moradian 2015; Shaban 2006), Ireland (Porter 2018), Spain (Duocastella 1999; Ramirez 2018), Taiwan (Chen 2013; Chen 2018; Huang 2006; Lin 2011; Wang 2015; Zhou 2015), Brazil (Alcantara‐Silva 2018; Arruda 2016; Doro 2017; Firmeza 2017; Pinto 2012), Australia (Horne‐Thompson 2008; O'Callaghan 2012), Turkey (Karadag 2019), and Vietnam (Nguyen 2010). Trial sample size ranged from 8 to 260 participants.
We classified 39 trials as music therapy studies (Alcantara‐Silva 2018; Bates 2017; Bieligmeyer 2018; Bradt 2015; Bufalini 2009; Burns 2001a; Burns 2008; Burns 2009; Burns 2018; Cassileth 2003; Clark 2006; Cook 2013; Doro 2017; Duocastella 1999; Ferrer 2005; Fredenburg 2014a; Fredenburg 2014b; Hanser 2006; Hilliard 2003; Horne‐Thompson 2008; Letwin 2017; Gimeno 2008; Palmer 2015; Porter 2018; Ramirez 2018; Ratcliff 2014; Reimnitz 2018; Robb 2008; Robb 2014; Robb 2017; Romito 2013; Rosenow 2014; Rossetti 2017; Stordahl 2009; Tuinmann 2017; Verstegen 2016 ; Verstegen 2018; Warth 2015; Yates 2015). Of these trials, ten used interactive music‐making with the participants, five used music‐guided imagery, three used music‐guided relaxation, 10 used live patient‐selected music performed by the music therapist, two used music listening accompanied by processing of emotions evoked by the music, five studies used a combination of interactive music making and listening to live music, one study used vibro‐acoustic therapy, and two used music video‐making. We classified 43 trials as music medicine studies (Alam 2016; Arruda 2016; Beck 1989; Binns‐Turner 2008; Bro 2019; Bulfone 2009; Burrai 2014; Cai 2001; Chen 2004; Chen 2013; Chen 2018; Chen 2020; Danhauer 2010; Firmeza 2017; Harper 2001; Huang 2006; Hunter 2020; Jasemi 2016; Jin 2011; Karadag 2019; Keenan 2017; Kwekkeboom 2003; Li 2004; Li 2012; Liao 2013; Lin 2011; Moradian 2015; Mou 2020; Nguyen 2010; O'Callaghan 2012; Pedersen 2020; Pinto 2012; Shaban 2006; Smith 2001; Straw 1991; Vachiramon 2013; Wan 2009; Wang 2015; Wren 2019; Xie 2001; Zhao 2008; Zhou 2015), as defined by the authors in the background section, and used listening to pre‐recorded music as the intervention.
Frequency and duration of treatment sessions greatly varied among the trials. The total number of sessions ranged from 1 to 40 (e.g. multiple music listening sessions per day for length of hospital stay). Most sessions lasted 30 to 45 minutes. We reported details on the frequency and duration of sessions for each trial in the Characteristics of included studies table.
Seventy‐eight trials used parallel‐group designs, whereas three trials used a cross‐over design (Bradt 2015; Beck 1989; Gimeno 2008). Not all trials measured all outcomes identified for this review.
We provided details of the included trials in the review in the Characteristics of included studies table.
Excluded studies
In the original review, 27 of the 101 reports that we retrieved for further assessment were assessed not to be outcome research studies. We identified 38 experimental research studies that appeared eligible for inclusion. However, we excluded these after closer examination or after receiving additional information from the principal investigators. Reasons for exclusions were: not a randomized or quasi‐randomized controlled trial (29 studies); insufficient data reporting (2 studies); unacceptable methodological quality (3 studies); not a music intervention (1 study); not exclusively cancer participants (1 study); and article could not be located (2 studies).
For the 2016 update, we retrieved 94 reports for further assessment. We excluded 60 studies for the following reasons: not a randomized or quasi‐randomized controlled trial (36 studies), insufficient data reporting (2 studies), not a music intervention (12 studies), not population of interest (8 studies), use of healthy controls (1 study), and use of non‐standardized measurement tools (1 study).
For the current update, we retrieved 83 reports for further assessment. We excluded 37 studies for the following reasons: not a randomized or quasi‐randomized controlled trial (14 studies), not a music intervention (9 studies), and not population of interest (14 studies).
For studies with insufficient data reporting or those that could not be located, we attempted to contact the authors on multiple occasions.
Details about reasons for exclusion are provided in the Characteristics of excluded studies table.
Risk of bias in included studies
We detailed the risk of bias for each trial in the risk of bias tables included in the Characteristics of included studies table and the risk of bias summary (Figure 2). In addition, readers can consult an overall assessment of risk of bias in Figure 3.
2.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
3.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Allocation
We included 61 trials that used appropriate methods of randomization (e.g. computer‐generated table of random numbers, drawing of lots, coin flip), nine trials that used systematic methods of treatment allocation (e.g. alternate group assignment, date of birth), and 11 trials that reported using randomization but failed to state the randomization method.
Thirty‐three trials concealed allocation, whereas 16 trials did not. For the remainder of the trials, authors did not mention allocation concealment.
Blinding
Twenty‐five trials included objective outcomes, but only seven of them reported blinding of the outcome assessors. For 11 trials, the use of blinding was unclear (Bro 2019; Burrai 2014; Chen 2004; Chen 2020; Ferrer 2005; Firmeza 2017; Jin 2011; Palmer 2015; Ramirez 2018; Tuinmann 2017; Wren 2019). The other trials did not use blinding. The majority of the trials included subjective outcomes only. It is important to point out that blinding of outcome assessors is not possible in the case of self‐report measurement tools for subjective outcomes (e.g. STAI; Spielberger 1983) unless the participants are blinded to the intervention. Blinding of the participants is often not feasible in music therapy and music medicine studies. This may introduce possible bias.
Incomplete outcome data
The dropout rate was small for most trials, falling between 0% and 17%. Fifteen trials reported dropout rates of more than 20%. For 21 trials, it was unclear whether there were any participant withdrawals. Most trials reported reasons for dropout. Detailed information on dropout rate and reasons is included in the Characteristics of included studies table.
Selective reporting
We found evidence of selective reporting in three trials (Burns 2008; Hunter 2020; Ratcliff 2014).
We examined publication bias visually in the form of funnel plots for several of the included outcomes. Visual inspection suggested that there was no publication bias for anxiety (Figure 4), depression (Figure 5), pain (Figure 6),
4.

Funnel plot of comparison: 1 Music intervention plus standard care versus standard care alone with adults, outcome: 1.1 Anxiety (STAI).
5.

Funnel plot of comparison: 1 Music intervention plus standard care versus standard care alone with adults, outcome: 1.6 Depression.
6.

Funnel plot of comparison: 1 Music intervention plus standard care versus standard care alone with adults, outcome: 1.13 Pain.
Other potential sources of bias
For ten trials, it was unclear if there were other potential sources of bias because no explicit declaration of interest statement was included in the publication..
Overall risk of bias
As a result, only one trial was at overall low risk of bias (Bradt 2015). Three additional trials were at low risk of bias for objective outcomes, as they satisfied all criteria used to assess risk of bias (Alam 2016; Duocastella 1999; Nguyen 2010). Five trials were at moderate risk of bias for objective outcomes (Binns‐Turner 2008; Bro 2019; Burrai 2014; Hilliard 2003; Palmer 2015). Seventy‐two trials were at high risk of bias. The main reason for receiving a high risk of bias rating was the lack of blinding. As pointed out above, blinding is often impossible in music therapy and music medicine studies that use subjective outcomes, unless the studies compare the music intervention with another active treatment intervention (e.g. progressive muscle relaxation). This is especially true for music therapy studies that use active music‐making. Therefore, it appears impossible for these types of studies to receive a low or even moderate risk of bias even if they have adequately addressed all other risk factors (e.g. randomization, allocation concealment, etc.).
Effects of interventions
Comparison 1: Music intervention plus standard care versus standard care alone in adults
Primary outcomes
Psychological outcomes
State anxiety
Thirty‐three trials examined the effects of music interventions plus standard care compared to standard care alone for anxiety in adult participants with cancer. Nineteen trials measured anxiety by means of the Spielberger State‐Trait Anxiety Inventory ‐ State Anxiety form (STAI‐S) (Alam 2016; Binns‐Turner 2008; Bro 2019; Bulfone 2009; Chen 2013; Danhauer 2010; Firmeza 2017; Harper 2001; Jin 2011; Kwekkeboom 2003; Li 2012; Lin 2011; O'Callaghan 2012; Rossetti 2017; Smith 2001; Vachiramon 2013; Wan 2009; Wren 2019; Zhou 2015); and fourteen trials reported mean anxiety measured by other scales, such as a numeric rating scale (NRS) or a visual analogue scale (VAS) (Cai 2001; Chen 2020; Cassileth 2003; Doro 2017; Ferrer 2005; Hanser 2006; Karadag 2019; Li 2004; Mou 2020; Palmer 2015; Tuinmann 2017; Verstegen 2018; Yates 2015; Zhao 2008). We could not include the data from Burns 2008 because it did not report post‐test or follow‐up scores. The author did provide follow‐up scores (four weeks post‐intervention), but we could not combine these with the post‐test scores of the other trials. Moreover, Burns 2008 reported a large moderating effect of pre‐intervention affect state scores on post‐test scores and follow‐up scores. We also did not include the data from Kwekkeboom 2003 in the meta‐analysis because this study was affected by a serious flaw in the implementation of the intervention. Participants in this trial listened to music while undergoing painful medical procedures. However, they reported that the use of headphones prevented them from hearing the surgeon, increasing their anxiety. Finally, we reported the data from Hanser 2006 narratively and did not include them in the meta‐analysis because of the high attrition rate (40%). In addition, the researchers experienced serious issues with intervention implementation within the predetermined implementation timeframe (three sessions were implemented over a 15‐week period), and the authors concluded that the intervention was significantly diluted because of this.
A meta‐analysis of 17 trials (N = 1381) that used the full STAI‐S (score range: 20 to 80) to examine state anxiety in 1381 participants indicated a lower state of anxiety in participants who received standard care combined with music interventions than those who received standard care alone (MD −7.73, 95% CI −10.02 to −5.44, P < 0.00001; very low‐certainty evidence; Analysis 1.1). Statistical heterogeneity was high across the trials (I2 = 93%). Removal of outliers (Binns‐Turner 2008; Harper 2001; Wan 2009) did not reduce heterogeneity much (I2 = 80%) . In Kwekkeboom 2003, participants in the music listening group reported higher levels of anxiety at post‐test (mean: 33.45, standard deviation (SD) 1.77) than those in the standard care group (mean: 30.59, SD 1.93). A sensitivity analysis excluding the trials that used inadequate methods of randomization (Bulfone 2009; Chen 2013) had minimal impact on the pooled effect size (MD −7.83, 95% CI −10.91 to −4.76, P < 0.00001, I2 = 92%; Analysis 1.1).
1.1. Analysis.

Comparison 1: Music intervention plus standard care versus standard care alone in adults, Outcome 1: Anxiety (STAI)
The standardized mean difference (SMD) of trials that reported post‐test anxiety scores on measures other than the full‐form STAI‐S (N = 882) also suggested a moderate to large anxiety‐reducing effect of music (SMD −0.76, 95% CI −1.28 to −0.25, P = 0.004; Analysis 1.2; 9 trials (Cai 2001; Chen 2020; Ferrer 2005; Karadag 2019; Li 2004; Mou 2020; Verstegen 2018; Zhao 2008; Yates 2015)). The results were not consistent across the trials (I2 = 91%) with one trial reporting a much larger effect size than other trials (Mou 2020) and one trial favoring the standard care control condition (Chen 2020). We did not include the data of four trials in the meta‐analysis because change scores and final scores should not be combined for the computation of a SMD (Alam 2016; Cassileth 2003; Doro 2017; Palmer 2015) or because only effect sizes were reported (Tuinmann 2017). However, the data by Cassileth 2003 were consistent with the results of the meta‐analysis, reporting a greater effect of music therapy on anxiety (mean change score: −2.6, SD 2.5) than standard care alone (mean change score: −0.9, SD 3.0) on the POMS‐anxiety subscale (score range: 0 to 36). Likewise, the data from Palmer 2015 indicated a beneficial effect of music therapy (mean change score: −30.9, SD 36.3) versus standard care (mean change score: 0, SD 22.7) on the Global Anxiety‐VAS (score range: 0 to 100 mm). The findings from Tuinmann 2017 also supported a greater treatment benefit of music therapy than standard care control (MD = −0.3, 95% CI −1.8 to −1.2). Finally, Alam 2016 reported similar change scores for the music intervention treatment arm (mean change score: −9.94, SD 2.42) and the control treatment arm (mean change score: −9.35, SD = 2.71), whereas Doro 2017 reported negligible change in anxiety for both treatment arms. A sensitivity analysis to examine the impact of randomization method, excluding the data of Cai 2001, Ferrer 2005 and Li 2004, had a minimal impact on the pooled effect size (SMD −0.72; 95% CI −1.67 to 0.23, P = 0.14; Analysis 1.2 ). A sensitivity analysis removing studies that included some participants without a cancer diagnosis (Verstegen 2018) did not impact the effect size estimate (SMD −0.75, 95% CI −1.3 to −0.21, P = 0.007, I2 = 92%; Analysis 1.2).
1.2. Analysis.

Comparison 1: Music intervention plus standard care versus standard care alone in adults, Outcome 2: Anxiety (non‐STAI (full version) measures)
Based on these findings, we can conclude that music interventions may have a large anxiety‐reducing effect. However, because participants could not be blinded to the music intervention and anxiety was measured using self‐report, there is a potential for biased reporting by the participants. Due to this potential bias combined with the high heterogeneity associated with the pooled effect, the finding is low‐certainty evidence (Table 1).
We conducted several a priori‐determined subgroup analyses, as outlined in the Methods.
Firstly, we compared the treatment benefits of music therapy versus music medicine studies for anxiety. We only included studies that reported post‐test scores in this analysis to allow for computation of a standardized mean difference across studies. The pooled effect of four music therapy studies (SMD −0.81, 95% CI −1.16 to −0.46, P < 0.00001, I2 = 0%; Ferrer 2005; Rossetti 2017; Verstegen 2018; Yates 2015) was similar to that of the music medicine studies (SMD −0.87, 95% CI −1.28 to −0.47, P < 0.0001, I2 = 94%; Binns‐Turner 2008; Bro 2019; Bulfone 2009; Cai 2001; Chen 2020; Danhauer 2010; Jin 2011; Karadag 2019; Li 2004; Li 2012; Lin 2011; Mou 2020; O'Callaghan 2012; Smith 2001; Vachiramon 2013; Wan 2009; Wren 2019; Zhao 2008; Zhou 2015). Although there was no evidence of a difference in effect between the music therapy studies and the music medicine studies (P = 0.83), it is worth noting that the results of the music therapy studies were consistent across studies, whereas the results of the music medicine studies were highly heterogeneous (Analysis 1.3). Because the results of the music therapy studies were consistent across studies, we can have greater confidence that music therapy interventions offered by a trained music therapist will result in large reductions in anxiety in adults with cancer.
1.3. Analysis.

Comparison 1: Music intervention plus standard care versus standard care alone in adults, Outcome 3: Anxiety (intervention subgroup)
Secondly, we compared studies that used patient‐preferred music with studies that used researcher‐selected music. For this comparison, we only included studies that used listening to pre‐recorded music as the intervention. Music preference did not appear to impact the treatment benefits for anxiety. The use of patient‐preferred music resulted in a SMD of −0.81 (95% CI −1.3 to −0.32, P = 0.001, I2 = 94%), whereas researcher‐selected music resulted in a SMD of −0.79 (95% CI −1.19 to −0.39, P = 0.0001, I2 = 56%) (Analysis 1.4).
1.4. Analysis.

Comparison 1: Music intervention plus standard care versus standard care alone in adults, Outcome 4: Anxiety (music preference)
Finally, we compared the music medicine studies by type of intervention (e.g. music‐guided relaxation, music listening alone, etc.). We could not conduct this subgroup analysis for music therapy studies because of an insufficient number of trials. The majority of the music medicine studies used listening to pre‐recorded music. Four studies, however, embedded relaxation or imagery instructions within the pre‐recorded music (Jin 2011; Lin 2011; Wan 2009; Zhou 2015). The pooled effect of these four studies (SMD −1.61, 95% CI −2.56 to −0.65, P = 0.0009, I2 = 95%) was much larger than that of music listening only studies (SMD −0.71, 95% CI −1.16 to −0.26, P = 0.002, I2 = 89%), but because of the large heterogeneity, there was no evidence of a difference in effect between these two types of interventions (P = 0.10) (Analysis 1.5).
1.5. Analysis.

Comparison 1: Music intervention plus standard care versus standard care alone in adults, Outcome 5: Anxiety (music‐guided relaxation)
Depression
Twelve trials (N = 1021) examined the effects of music plus standard care compared to standard care alone on depression in 1021 participants (Arruda 2016; Bates 2017; Cai 2001; Cassileth 2003; Chen 2020; Clark 2006; Karadag 2019; Li 2012; Verstegen 2018; Wan 2009; Yates 2015; Zhou 2015). Their pooled estimate indicated a moderate treatment effect of music (SMD −0.41, 95% CI −0.67 to −0.15, P = 0.002; very low‐certainty evidence; Analysis 1.6), but the results were inconsistent across trials (I2 = 72%). When we removed two outliers (Karadag 2019; Li 2012), heterogeneity was greatly reduced (I2 = 13%), but there was no identifiable reason why these studies acted like an outlier. At first sight, it appeared that the outlier values might be explained by the fact that both of these studies used a large number of sessions (i.e. up to 25‐60 sessions compared to 1‐5 sessions in other studies). However, Cai 2001 used 30 sessions and this study did not act as an outlier.
1.6. Analysis.

Comparison 1: Music intervention plus standard care versus standard care alone in adults, Outcome 6: Depression
A sensitivity analysis examining the impact of randomization method resulted in a smaller pooled effect size (SMD −0.32, 95% CI −0.59 to −0.04, P = 0.03, I2 = 70%; Analysis 1.6). A sensitivity analysis excluding one study that included some participants who did not have a cancer diagnosis (Verstegen 2018) did not impact the pooled effect size (SMD −0.41, 95% CI −0.68 to −0.15, P = 0.002, I2 = 75%; Analysis 1.6). Because participants could not be blinded to the music intervention and self‐report was used to measure depression, there is a potential for bias. This, as well as the fact that results were inconsistent across trials, makes this very‐low certainty evidence (Table 1).
Subgroup analyses revealed that there was no evidence of a difference in effect between music therapy and music medicine studies for the outcome of depression (P = 0.14) (Analysis 1.7) or between patient‐preferred versus researcher‐selected music (Analysis 1.8).
1.7. Analysis.

Comparison 1: Music intervention plus standard care versus standard care alone in adults, Outcome 7: Depression (intervention subgroup)
1.8. Analysis.

Comparison 1: Music intervention plus standard care versus standard care alone in adults, Outcome 8: Depression (music preference)
Distress
Two trials (N = 127) examined the effects of music interventions on distress during radiation therapy (Clark 2006; Rossetti 2017). Their pooled estimate did not find support for an effect of music (SMD −0.38, 95% CI −1.43 to 0.66, I2 = 88%, P = 0.47).
Mood
The pooled estimate of five trials (N = 221) resulted in little effect of music interventions for mood in participants with cancer (SMD 0.53, 95% CI −0.03 to 1.11, P = 0.07; very low‐certainty evidence) Analysis 1.10; Burrai 2014; Cassileth 2003; Moradian 2015; Ratcliff 2014). The results were inconsistent across studies (I2 = 76%), with Burrai 2014 reporting much larger treatment benefits than the other studies. Removal of this outlier greatly reduced the heterogeneity (I2 = 0%). Although Burrai 2014 was the only study that used live saxophone music played by a nursing staff member, other studies included in this analysis used live music offered by music therapists. Therefore, it is unclear if the use of live music may have accounted for the large treatment benefit in the Burrai 2014 study. The potential bias stemming from participants not being blinded to the music intervention and the high heterogeneity associated with the pooled effect makes this very low‐certainty evidence (Table 1).
1.10. Analysis.

Comparison 1: Music intervention plus standard care versus standard care alone in adults, Outcome 10: Mood
A sensitivity analysis based on randomization method slightly increased the pooled effect (SMD 0.68, 95% CI −0.04 to 1.39, P = 0.06, I2 = 81%; Analysis 1.10) but the evidence concerning the impact of music interventions on mood is very uncertain.. We could not include the data from Burns 2001a in the meta‐analysis because the authors did not use a constant in the computation of their scores, as recommended in the Profile of Mood States (POMS) scoring guide (McNair 1971). The results of the meta‐analysis were robust compared to Burns 2001a, which reported a mean post‐test score of −48.25 (SD 32.96) for the music therapy group and a mean post‐test score of 20.75 (SD 30.87) for the control group. Due to a large baseline difference between the music and control treatment arms in Doro 2017, the post‐test values of this trial could not be included in the meta‐analysis. The results by Bieligmeyer 2018 are reported separately because this study used vibro‐acoustic therapy as the intervention. The authors reported larger mood‐enhancing effects in the vibro‐acoustic treatment arm (pretest scores: 71.8 SD 19.67; post‐test scores: 81, SD 16.26) than the control group (pre‐test scores: 73.52, SD 20.62; post‐test scores: 72.75, SD 20.63).
A subgroup analysis comparing music therapy (SMD 0.37, 95% CI −0.13 to 0.87, P = 0.15) with music medicine (SMD 0.73, 95% CI −0.54 to 1.99, P = 0.26) found no evidence of a difference in effect between the two types of studies (SMD 0.53, 95% CI ‐0.03 to 1.10, P = 0.6), but the results of the music therapy studies were consistent across studies (I2 = 37%), whereas the music medicine studies were inconsistent across studies (I2 = 90%) (Analysis 1.11).
1.11. Analysis.

Comparison 1: Music intervention plus standard care versus standard care alone in adults, Outcome 11: Mood (intervention subgroup)
Hope
Two studies examined the treatment benefits of music interventions for hope (Arruda 2016; Verstegen 2018) (Analysis 1.12). The pooled effect size indicated an increase of 3.19 on the Herth Hope Index with music interventions compared to control (MD, 95% CI 0.12 to 6.25, I2 = 48%, P = 0.04; very low‐certainty evidence).
1.12. Analysis.

Comparison 1: Music intervention plus standard care versus standard care alone in adults, Outcome 12: Hope
Resilience
One music therapy trial with adult cancer participants (N = 15) (Letwin 2017) reported greater improvements in resilience in the music therapy treatment arm (pre‐test scores: 74.13, SD 11.29; post‐test scores: 81.88, SD 7.55) than in the control arm (pre‐test scores: 75.29, SD 13.29; post‐test scores: 78.57, SD 9.14) as measured on the The Response to Stressful Events Scale (RSES) (range: 0 to 88) (Johnson 2011).
Physical symptoms
Pain
Twenty trials compared the effects of music versus standard care on pain (Alam 2016; Arruda 2016; Bieligmeyer 2018; Binns‐Turner 2008; Clark 2006; Danhauer 2010; Doro 2017; Fredenburg 2014a; Huang 2006; Kwekkeboom 2003; Letwin 2017; Li 2012; Moradian 2015; Reimnitz 2018; Tuinmann 2017; Verstegen 2016; Verstegen 2018; Wan 2009; Wren 2019).
We could not include the data from Alam 2016, Clark 2006 or Moradian 2015 in the meta‐analysis because of the use of change scores. We could not include the post‐test scores from Doro 2017 due to large baseline differences between the treatment arms. Tuinmann 2017 only reported effect sizes which could not be included in this meta‐analysis. Kwekkeboom 2003 compared the effects of music listening, audiotape and standard care on procedural pain and anxiety, finding that participants did not like wearing the headsets as it prevented them from hearing the surgeon, causing greater anxiety. The literature suggests that increased anxiety leads to increased pain perception (McCracken 2009); therefore, we excluded these data from the meta‐analysis. We did not include the data from Bieligmeyer 2018 in the meta‐analysis because this study examined the effects of vibro‐acoustic therapy which combines music with vibrations to affect the body.
The pooled effect of the remaining twelve studies with 632 participants resulted in a moderate effect for music on pain perception (SMD −0.67, 95% CI −1.07 to −0.26, P = 0.001; very low‐certainty evidence; Analysis 1.13). There was disagreement between the trials on the size of the effect (I2 = 81%), but this was due to Li 2012 reporting much larger treatment benefits than the other trials. Removal of this outlier reduced the heterogeneity to 23%. As this was the only study with a large number of sessions (up to 60 sessions), frequency of sessions may be a potential explanation for this outlier. As with other outcomes in this review, there is a potential for bias because the participants could not be blinded and self‐report outcome measures were used. In addition, the large heterogeneity lowered the certainty of the evidence for this outcome. A sensitivity analysis excluding those studies that included some participants who did not have a cancer diagnosis (Reimnitz 2018; Verstegen 2016; Verstegen 2018) resulted in a larger effect size (SMD −0.77, 95% CI −1.25 to −0.29, P = 0.002, I2 = 85%; Analysis 1.13).
1.13. Analysis.

Comparison 1: Music intervention plus standard care versus standard care alone in adults, Outcome 13: Pain
Using a 0 to 10 numeric rating scale, Clark 2006 found that music therapy resulted in greater pain reduction (mean change score: −0.44, SD 2.55) than standard care (mean change score: 0.45, SD 1.87). In contrast, Moradian 2015 reported similar improvements in pain for the treatment (mean change score: −12.96, SD 24.16) and the control group (mean change score: −13.58, SD 28.51). Tuinmann 2017 reported a greater treatment benefit for music compared to standard care for pain (MD = ‐10, 95% CI ‐18.9 to ‐1.2) on the pain subscale of the European Organization for Research and Treatment on Cancer scale (EORTC). In contrast, Alam 2016 reported minimal pain reduction in participants who listened to pre‐recorded music (mean change score: ‐0.41, SD = 1.69) versus those who did not (mean change score: ‐0.23, SD = 1.57) during cutaneous surgery. Finally, Bieligmeyer 2018 reported greater pain‐reducing effects in participants who underwent vibro‐acoustic therapy (pre‐test scores: 12.88, SD 19.59; post‐test scores: 10, SD 16.3) than those in the control group (pre‐test scores: 12.75, SD 18.62; post‐test scores: 15.36, SD 21.56).
For this outcome, we were able to compare the treatment benefits of music therapy versus music medicine studies (Analysis 1.14). The pooled effect of five music therapy trials suggested a moderate pain‐reducing effect of music therapy. This effect was consistent across trials and therefore enhanced our confidence in this evidence (SMD −0.47, 95% CI −0.86 to −0.07, P = 0.02, I2 = 0%; Fredenburg 2014a; Letwin 2017; Reimnitz 2018; Verstegen 2016; Verstegen 2018). The pooled effect of music medicine studies was larger but was highly inconsistent across studies (SMD −0.81, 95% CI −1.38 to −0.24, P = 0.005, I2 = 89%; (Arruda 2016; Binns‐Turner 2008; Danhauer 2010; Huang 2006; Li 2012; Wan 2009; Xie 2001).
1.14. Analysis.

Comparison 1: Music intervention plus standard care versus standard care alone in adults, Outcome 14: Pain (intervention subgroup)
We were also able to examine the impact of music preference on treatment effect (SMD −0.84, 95% CI −1.34 to −0.33, P = 0.001, I2 = 87%; Analysis 1.15). Although there was no evidence of a difference in effect between the use of patient‐preferred music and researcher‐selected music (P = 0.78), the use of patient‐preferred music led to a larger pooled effect (SMD −0.87, 95% CI −1.65 to −0.1, P = 0.03, I2 = 90%) than the use of researcher‐selected music (SMD −0.74, 95% CI −1.33 to 0.14, P = 0.02, I2 = 73%). The large heterogeneity was due to some studies reporting a much larger beneficial effect than others.
Fatigue
Ten trials examined the effects of music interventions on fatigue in 498 participants (Bates 2017; Cassileth 2003; Chen 2020; Clark 2006; Ferrer 2005; Fredenburg 2014b; Moradian 2015; Reimnitz 2018; Rosenow 2014; Wren 2019). The pooled estimate of their change scores indicated a small effect for music interventions (SMD −0.28, 95% CI −0.46 to −0.10, P = 0.002; low‐certainty evidence, Analysis 1.16), with consistent results across studies (I2 = 0%). Burns 2008 also collected data on fatigue; however, investigators did not report post‐intervention data; the study provided us with four‐week post‐intervention follow‐up scores, but could not provide the immediate post‐test scores. This prevented us from pooling their data with data from the other three studies. A sensitivity analysis excluding one study due to inadequate randomization methods (Ferrer 2005) had minimal impact on the pooled effect (SMD −0.26, 95% CI −0.45 to ‐0.07, P = 0.007, I2 = 0%; Analysis 1.16). A sensitivity analysis excluding one study that included some participants who did not have a cancer diagnosis (Reimnitz 2018) also had minimal impact on the pooled effect (SMD −0.26, 95% −0.44 to −.0.07, P = 0.007, I2 = 0%; Analysis 1.16).
1.16. Analysis.

Comparison 1: Music intervention plus standard care versus standard care alone in adults, Outcome 16: Fatigue
A comparison between music therapy and music medicine trials suggested a small to moderate effect for music therapy trials that was consistent across trials (SMD −0.36, 95% CI −0.61 to −0.12, P = 0.004, I2 = 0%; Bates 2017; Cassileth 2003; Ferrer 2005; Fredenburg 2014b; Reimnitz 2018; Rosenow 2014), whereas there was no evidence of an effect for music medicine trials (SMD −0.15, 95% CI −0.43 to 0.14, P = 0.31, I2 = 0%; Chen 2020; Moradian 2015; Wren 2019) (Analysis 1.17).
1.17. Analysis.

Comparison 1: Music intervention plus standard care versus standard care alone in adults, Outcome 17: Fatigue (intervention subgroup)
Secondary outcomes
Physiological outcomes
Heart rate
Twelve trials examined the effects of music on heart rate in 1165 participants (Alam 2016; Binns‐Turner 2008; Bro 2019; Burrai 2014; Chen 2013; Ferrer 2005; Firmeza 2017; Harper 2001; Jin 2011; Mou 2020; Wren 2019; Zhao 2008). All of the studies except for Ferrer 2005 were music medicine studies. Since Bro 2019 only reported effect sizes, the findings of that study were not included in this meta‐analysis. The pooled estimate of the remaining 11 studies (N = 1022) showed a decrease in heart rate, favoring music interventions over standard care (MD −3.4, 95% CI −5.58 to −1.23, P = 0.002; Analysis 1.19). However, the results were inconsistent across studies (I2 = 82%). A sensitivity analysis excluding Ferrer 2005 and Chen 2013 because of an unknown randomization method and a lack of proper randomization, respectively, resulted in a larger effect with less heterogeneity (MD −4.37, 95% CI −6.29 to −2.44, P < 0.00001, I2 = 51%; Analysis 1.19).
1.19. Analysis.

Comparison 1: Music intervention plus standard care versus standard care alone in adults, Outcome 19: Heart rate
Bro 2019 reported a greater decrease in heart rate for participants who listened to live music during chemotherapy versus those in the control group (MD ‐1.8, 95% CI ‐3.9 to 0.2, P = 0.08).
A subgroup analysis for music preference indicated that there was no evidence of a difference in effect (P = 0.62) for heart rate between researcher‐selected music (MD −4.47, 95% CI −8.02 to −0.91, P = 0.01, I2 = 61%) and patient‐preferred music (MD −3.34, 95% CI −6.06 to −0.62, P = 0.02, I2 = 80%; Analysis 1.20).
1.20. Analysis.

Comparison 1: Music intervention plus standard care versus standard care alone in adults, Outcome 20: Heart rate (music preference)
One cross‐over trial compared the effect of music and imagery with imagery alone (Gimeno 2008). Both interventions resulted in similar decreases in heart rate from pre‐test to post‐test (P = 0.9): the music and imagery group's mean heart rate dropped from 89.58 beats per minute (bpm) (SD 17.32) at pre‐test to 78.84 bpm (SD 13.46) at post‐test; the imagery only group's mean heart rate dropped from 93.31 bpm (SD 15.76) to 81.05 bpm (SD 13.96).
Respiratory rate
The pooled estimate of five trials (N = 437) suggested a very small, beneficial effect for music interventions on respiratory rate (MD −0.71, 95% CI −1.18 to −0.23, P = 0.004; Analysis 1.21; Chen 2013; Firmeza 2017; Jin 2011; Mou 2020; Zhao 2008), and the studies did not agree on the size of effect (I2 = 86%). A sensitivity analysis excluding Chen 2013 because of failure to use a proper method of randomization resulted in a larger pooled effect (MD −1.18, 95% CI −2.46 to 0.11, P = 0.07, I2 = 88%; Analysis 1.21).
1.21. Analysis.

Comparison 1: Music intervention plus standard care versus standard care alone in adults, Outcome 21: Respiratory rate
We could not conduct a subgroup analysis based on music preference for this outcome due to an insufficient number of trials differentiating music type.
Systolic blood pressure
We found a pooled estimate of −4.18 mmHg (95% CI −6.7 to −1.66, P = 0.001; N = 992; Analysis 1.22) for systolic blood pressure (SBP), favoring music interventions (Alam 2016; Burrai 2014; Chen 2013; Ferrer 2005; Firmeza 2017; Harper 2001; Jin 2011; ; Mou 2020; Wren 2019; Zhao 2008). The results were inconsistent across studies (I2 = 70%). Excluding Chen 2013 and Ferrer 2005 because of lack of proper randomization had minimal impact on the pooled effect size (MD −4.5 mmHg, 95% CI −8.36 to −0.64, P = 0.02, I2 = 73%; Analysis 1.22). All of the studies except for Ferrer 2005 were music medicine studies. Bro 2019 reported a minimal effect on SBP of listening to live music compared to standard care (MD −0.7, 95% CI −4.3 to 2.9, P = 0.7)).
1.22. Analysis.

Comparison 1: Music intervention plus standard care versus standard care alone in adults, Outcome 22: Systolic blood pressure
We conducted a subgroup analysis based on music preference (Analysis 1.23), but no significant difference was found between the effect of patient‐preferred music (MD −4.82, 95% CI −7.9 to −1.75, P = 0.002, I2 = 70%) compared to researcher‐selected music (MD −4.71, 95% CI −12.04 to 2.63, P = 0.21, I2 = 78%) (P = 0.98).
1.23. Analysis.

Comparison 1: Music intervention plus standard care versus standard care alone in adults, Outcome 23: Systolic blood pressure (music preference)
Diastolic blood pressure
We found a pooled estimate of −2.34 mmHg (95% CI −4.7 to 0.01; Analysis 1.24) for diastolic blood pressure (DBP) in 992 participants (Alam 2016; Burrai 2014; Chen 2013; Ferrer 2005; Firmeza 2017; Harper 2001; Jin 2011; Mou 2020; Wren 2019; Zhao 2008).The results were inconsistent across studies (I2 = 88%). Excluding Chen 2013 and Ferrer 2005 in a sensitivity analysis resulted in a larger MD of −3.86 mmHg (95% CI −6.01 to −1.71, P = 0.0004) that was less heterogeneous (I2 = 65%; Analysis 1.24). All of the studies except for Ferrer 2005 were music medicine studies.
1.24. Analysis.

Comparison 1: Music intervention plus standard care versus standard care alone in adults, Outcome 24: Diastolic blood pressure
Bro 2019 reported a minimal effect of listening to live music on DBP (MD = 0.7, 95% CI ‐2.2 to 3.5, P = 0.63).
Patient‐preferred music resulted in somewhat greater reductions in DBP (MD −3.36, 95% CI −6.46 to −0.27, P = 0.03, I2 = 92%; Analysis 1.25) than researcher‐selected music (MD −2.51, 95% CI −5.03 to 0.02, P = 0.05, I2 = 0%) (P = 0.67).
1.25. Analysis.

Comparison 1: Music intervention plus standard care versus standard care alone in adults, Outcome 25: Diastolic blood pressure (music preference)
Mean arterial pressure
Binns‐Turner 2008 reported on the effects of music on mean arterial pressure (MAP) in 30 participants and found a large decrease in MAP for the music group (mean change score: −15.1 mmHg, SD 17.1, 95% CI −23.76 to −6.44). In contrast, participants in the standard care group experienced an increase in MAP (mean change score: 4.5 mmHg, SD 15.3, 95% CI −3.25 to 12.25).
Oxygen saturation level
Two trials with 252 participants reported no effect for music listening on oxygen saturation levels (MD 0.59, 95% CI −0.62 to 1.8, P = 0.34, I2 = 86%; Analysis 1.26; Burrai 2014; Chen 2013; ).
1.26. Analysis.

Comparison 1: Music intervention plus standard care versus standard care alone in adults, Outcome 26: Oxygen saturation
Immune system functioning
Two trials examined the effects of music on immune system functioning. Chen 2004 compared music listening to standard care in 46 participants and found post‐test differences for the following indicators of immune system functioning: CD3 (music: mean 44, SD 12.62; control: mean 36.73, SD 11.01), CD4/CD8 (music: mean 1.67, SD 0.76; control: mean 1.32, SD 1.01), and natural killer (NK) cell activity (music: mean 25.23, SD 15.20; control: mean 21.36, SD 12.86), indicating a positive effect of music listening on the immune system in women with breast cancer. CD3 and CD4/CD8 are proteins that play a role in immune system functioning. Tuinmann 2017 investigated the effects of music listening in addition to standard care in patients undergoing high‐dose chemotherapy after autologous stem cell transplantation. No evidence of treatment effect was found for IgA (MD = −0.5, 95% CI −1.3 to 0.2), IgG (MD = −0.4, 95% CI −2.9 to 2.1), T4 (MD = 0.1, 95% CI −1.6 to 1.7), T8 (MD = −0.2, 95% CI −1.5 to 1.1), and NK (MD = −0.5, 95% CI −1.3 to 0.3) cell activity.
Physical functioning
Six trials examined the effects of music on participants' physical functioning (Hanser 2006; Hilliard 2003; Liao 2013; Moradian 2015; Tuinmann 2017; Xie 2001). We could not include the results of Hanser 2006 in the pooled estimate because of the use of change scores and the high attrition rate. The results of Tuinmann 2017 are reported separately because the authors only reported an effect size. The pooled estimate of the remaining studies indicated no evidence for an effect of music on physical status in 493 participants with cancer (SMD 0.78, 95% CI −0.74 to 2.31, P = 0.31; Analysis 1.18). The results were highly inconsistent (I2 = 98%), with Xie 2001 reporting a much larger beneficial effect. In Hanser 2006, music therapy led to a greater improvement in physical well‐being (FACT‐G Physical Well‐Being Subscale, score range: 0 to 28) (mean change score: 2.0, SD 4.6) than standard care (mean change score: −0.4, SD 3.7). In the study by Tuinmann 2017 with cancer patients during high‐dose chemotherapy and stem cell support, physical functioning as measured by the Karnofsky Performance Scale deteriorated in both the music listening and the control group. A smaller decline was found in the music listening group (MD = 0.8, 95% CI ‐2.2 to 3.9). Removing Xie 2001 because of an improper randomization method resulted in a small effect that was consistent across studies (SMD 0.08, 95% CI −0.18 to 0.34, P = 0.54, I2 = 0%; Analysis 1.18).
1.18. Analysis.

Comparison 1: Music intervention plus standard care versus standard care alone in adults, Outcome 18: Physical functioning
Anesthetic and analgesic intake
Two studies included use of anesthesia and analgesics as an outcome. Palmer 2015 examined the amount of propofol needed to reach a sedation score of 70 on the Bispectral Index (BIS) in women undergoing breast surgery. A BIS reading of 70 represents moderate sedation. The average propofol needed in the live music group (N = 67) was 67.2 mg (SD 53.7), 61.9 mg (SD 34.1) in the recorded music group (N = 65), and 70.5 mg (SD 35.2) in the usual care group (N = 62). Wang 2015 examined the impact of music‐guided relaxation compared to standard care on postoperative consumption of the sufentanil, a narcotic medicine, and use of a patient‐controlled analgesia (PCA) pump. Participants in the music treatment arm consumed a smaller amount of sufentanil (52.68 µg, SD 7.07) than the standard care treatment arm (82.65 µg, SD 6.19). PCA use was also lower in the music treatment arm (19.06, SD 3.49) than in the control group (30.96, SD 4.0).
Length of hospital stay and recovery time
Palmer 2015 also examined the effect of music on recovery time following breast surgery. Recovery time was defined as the interval between surgery end time and the time when the participant had met all discharge criteria determined by the recovery nurse. The results indicated that there was no difference in recovery time between the two types of music interventions (live music by a music therapist and listening to pre‐recorded music) and the usual care group, suggesting that the addition of a music intervention did not increase participant time commitment. A difference was found between the live music group (52.4 minutes, SD 21.6) and the recorded music group (64.8 minutes, SD 35.3), with the live music group getting discharged approximately 12 minutes faster than the recorded music group. However, the authors suggest a careful interpretation of these results as other factors could have contributed to this difference.
Li 2012 tracked the length of women's hospital stay after radical mastectomy. Women in the music listening treatment arm stayed an average of 13.62 days (SD 2.04), whereas women in the usual care control arm stayed an average of 15.53 days (SD 2.75) (P < 0.001).
Social and spiritual support
Spiritual well‐being
Two trials under this comparison assessed spiritual well‐being (Cook 2013; Hanser 2006). One trial compared music therapy to usual care using the Functional Assessment of Chronic Illness Therapy‐Spiritual Well‐Being subscale (FACIT‐Sp, score range: 0 to 48) (Hanser 2006). Results indicated that participants in the music therapy treatment arm reported a slightly greater increase in spiritual well‐being (mean change score: 2.5, SD 8.56) than those in the control group (mean change score: 0.7, SD 6.95). Cook 2013 compared music therapy with standard care and reported a greater improvement in the music therapy treatment arm (mean change score: 4.4, SD 4.84) than the control arm (mean change score: 2.0, SD 6.08) on the FACIT‐Sp.
Quality of life
Eleven trials compared the impact of music interventions to standard care on QoL (Bieligmeyer 2018; Bro 2019; Burns 2001a; Hanser 2006; Hilliard 2003; Liao 2013; Moradian 2015; Porter 2018; Ratcliff 2014; Tuinmann 2017; Xie 2001). We did not include Bieligmeyer 2018; Bro 2019; Hanser 2006; Tuinmann 2017 in the meta‐analysis for reasons discussed above. Meta‐analysis of the remaining seven trials (N = 573) resulted in a heterogeneous SMD of 0.88 (95% CI −0.31 to 2.08, P = 0.15, I2 = 97%; Analysis 1.27; Burns 2001a; Hilliard 2003; Liao 2013; Moradian 2015; Porter 2018; Ratcliff 2014; Xie 2001), with Xie 2001 reporting a much larger beneficial effect than the other trials. Removal of this outlier resulted in a small effect size that was homogeneous (SMD 0.29, 95% CI 0.07 to 0.52, P = 0.01, I2 = 0%).
1.27. Analysis.

Comparison 1: Music intervention plus standard care versus standard care alone in adults, Outcome 27: Quality of life
We conducted a sensitivity analysis removing all studies that used improper methods of randomization. This resulted in a moderate effect size (SMD 0.47, 95% CI 0.06 to 0.88, P = 0.02, I2 = 56%; Analysis 1.27). Overall, the lack of blinding of participants to the music intervention and the use of self‐report measures, makes this very low‐certainty evidence.
A subgroup analysis per intervention type resulted in a homogenous, moderate effect of music therapy on QoL (SMD 0.40, 95% CI 0.08 to 0.71, P = 0.01, I2 = 0%; Analysis 1.28) that was consistent across studies. In Hanser 2006, music therapy resulted in a greater improvement in QoL (FACT‐G, 0‐108) (mean change score: 3.5, SD 13.75) than standard care (mean change score: 0.9, SD 15.8). For the music medicine studies, there was no evidence of an effect and the pooled effect was very heterogeneous (SMD 1.32, 95% CI −1.02 to 3.67, P = 0.21, I2 = 99%). The large heterogeneity was due to the outlying values of Xie 2001; removing it from the analysis resulted a pooled effect that was consistent across studies but the conclusion of no evidence of effect remained (SMD 0.18, 95% CI −0.14 to 0.51, P = 0.27, I2 = 0%). There was no evidence of a difference in treatment effect between the music therapy studies and the music medicine studies (P = 0.44). Because there was only evidence of an effect for music therapy interventions and the results were consistent across trials, we can be more certain that music therapy interventions delivered by a trained music therapist will result in improvements in quality of life of adults with cancer.
1.28. Analysis.

Comparison 1: Music intervention plus standard care versus standard care alone in adults, Outcome 28: Quality of life (intervention subgroup)
Comparison 2: Music intervention plus standard care versus standard care alone in children
Seven trials included pediatric participants (N = 270). Two trials compared music interventions with standard care (Bufalini 2009; Nguyen 2010), one trial compared music therapy with an activities session (Duocastella 1999), three trials compared music therapy with an audiobook control (Burns 2009; Robb 2008; Robb 2014), and one trial compared a parent‐delivered music intervention with an audiobook control condition (Robb 2017). In this comparison, we reported on the two trials that compared a music intervention with standard care. In comparison 3, we reported on the remainder of the pediatric trials.
Primary outcomes
Psychological outcomes
State anxiety
Two trials (Bufalini 2009; Nguyen 2010) examined the effects of music on state anxiety. Whereas Bufalini 2009 used the full STAI form, Nguyen 2010 used the STAI‐short form. Therefore a standardized mean difference was computed. The pooled effect size suggested a large treatment effect for music (SMD −0.94, 95% CI −1.9 to 0.03, P = 0.06, I2 =76%; Analysis 2.1; very low‐certainty evidence ).
2.1. Analysis.

Comparison 2: Music interventions plus standard care versus standard care alone in children, Outcome 1: Anxiety (STAI)
Depression
We identified no studies for this outcome.
Distress
We identified no studies for this outcome.
Mood
We identified no studies for this outcome.
Hope
We identified no studies for this outcome.
Resilience
We identified no studies for this outcome.
Physical symptoms
Pain
Nguyen 2010 examined the effects of listening of pre‐recorded music on children's pain during and after lumbar puncture (LP). Children who listened to music reported significantly less pain during LP (mean: 2.35, SD 1.9) than children in the standard care condition (mean: 5.65, SD 2.5). Children in the music condition continued to report less pain after the LP (mean: 1.2, SD 1.36) compared to children in the control condition (mean: 3.0, SD 2.0).
Fatigue
We identified no studies for this outcome.
Secondary outcomes
Physiological outcomes
Nguyen 2010 also found beneficial effects of listening to pre‐recorded music on physiological responses during and after LP. Children in the music group exhibited an average heart rate of 102.7 (SD 9.24) during and 100.8 (SD 11.4) after LP compared to children in the control group (during: 117.7, SD 19.49; after: 111.1, SD 17.23); an average respiratory rate of 25.1 (SD 3.6) during and 24.5 (SD 3.49) after LP compared to 28.5 (SD 3.86) during and 28.2 (3.72) after LP in the control group; an average oxygen saturation level of 99.2 (SD 1.14) during and 99.7 (SD 0.49) after LP compared to 98 (SD 2.77) during and 99.2 (1.47) after LP in the control group; an average SBP of 97.1 (SD 8.57) during and 98.5 (SD 10.13) after LP compared to 105.6 (SD 15.97) during and 102.4 (SD 11.26) after LP in the control group; and an average DBP of 65.2 (SD 6.83) during and 62.75 (4.82) after compared to 69.8 (11.67) during and 64.2 (SD 9.4) after LP in the control group.
Comparison 3: Music interventions plus standard care versus standard care plus placebo control in children
Primary outcomes
Psychological outcomes
State Anxiety
We identified no studies for this outcome.
Depression
We identified no studies for this outcome.
Distress
Two trials examined the effects of music therapy on reduction of distress, comparing a music video intervention with an audiobook control condition in adolescents and young adults during stem cell transplantation (Burns 2009; Robb 2014). In the music video, participants wrote songs and created accompanying music videos in collaboration with a music therapist. The pooled effect of the two trials did not provide support for an effect of music therapy (SMD −0.07, 95% CI −0.39 to 0.26, P = 0.69, I2 = 0%; Analysis 3.1). In Burns 2009, both groups reported an increase in distress post‐intervention scores, which were used in the meta‐analysis. However, follow‐up measures at 100 days after the stem‐cell transplantation indicated a lower mean distress score for the music therapy group (mean: 1.67, SD 0.55) than the audiobook group (mean: 2.00, SD 0.64).
3.1. Analysis.

Comparison 3: Music interventions plus standard care versus standard care plus placebo control in children, Outcome 1: Distress
Robb 2017 examined the feasibility and acceptability of a parent‐delivered music intervention in the care of young children. Even though emotional distress was lower for children who received the parent‐delivered intervention compared to children with the audiobook control condition, parents found the parent delivery format not acceptable.
Mood
Duocastella 1999 compared the effects of music therapy with an activities session on mood in children but did not find significant differences between the two treatment arms. Children in the music therapy treatment arm reported post‐intervention scores of 4.67 (SD 0.62) versus 4.47 (SD 0.51) reported by children in the activities treatment arm.
Hope
We identified no studies for this outcome.
Resilience
One music therapy study in 80 adolescents and young adults undergoing hematopoietic stem cell transplant (HSCT) included resilience as an outcome and and found no evidence of an effect (SMD 0.21, P = 0.35) (Robb 2014). The authors reported that the study was underpowered to detect medium and small effect sizes.
Coping
Robb 2014 examined the effect of music therapy on coping. They reported a moderate effect size for courageous coping immediately post‐transplant. At the same time, they found no change in the use of defensive coping strategies, suggesting that adolescents and youth in the music therapy treatment arm increased their use of positive coping strategies.
Physical outcomes
Pain
We identified no studies for this outcome.
Fatigue
We identified no studies for this outcome.
Secondary outcomes
Physiological outcomes
Immune system functioning
In one trial with 30 children, Duocastella 1999 found no evidence of an effect on Immunoglobin A (IgA) levels of live music‐making (mean change score: 7.07 mg/L, SD 34.52) compared to engaging children in activities that did not involve music (mean change score: 4.13 mg/L, SD 41.02).
Social and spiritual support
Spiritual well‐being
Burns 2009 and Robb 2014 also examined the effect of a music video intervention versus audiobook control condition on spiritual well‐being in adolescents and young adults. Their pooled estimate did not find support for an effect of music therapy on spiritual well‐being (SMD 0.31, 95% CI −0.11 to 0.73, P = 0.15, I2 = 0%; Analysis 3.2).
3.2. Analysis.

Comparison 3: Music interventions plus standard care versus standard care plus placebo control in children, Outcome 2: Spiritual well‐being
Social support
Robb 2014 examined the effect of music therapy on perceived social support in adolescents and young adults during stem cell transplant. At 100 days post‐transplant, participants in the music therapy treatment arm reported greater improvements in perceived social support (SMD 0.54, P = 0.028) and family environment (i.e. family cohesion, family adaptation, family communication, and family strength) (SMD 0.66, P = 0.008) than participants in the audiobook control group. Qualitative analysis of the music videos that accompanied the songs written by the participants revealed that study participants were "identifying peers (i.e. social integration), family members (i.e. family environment), and faith/spirituality (i.e. spiritual perspective) as important sources of support" (p. 916).
Communication
One trial in children with cancer compared the effects of one session of active music‐making to music listening and audio storybooks on levels of active engagement and initiation in 55 children (Robb 2008). Active music therapy sessions led to higher active engagement (post‐test mean: 26.03, SD 4.1) than music listening (post‐test mean: 15.65, SD 6.2, P < 0.0001) or audio storybooks (post‐test mean: 15.17, SD 4.9, P < 0.0001). Active music‐making (post‐test mean: 14.19, SD 8.3) and music listening (post‐test mean: 15.89, SD 11.2) also increased the child's initiation behaviour compared to the audio storybooks (post‐test mean: 7.43, SD 6.6) (P = 0.04 and P = 0.002, respectively).
Quality of life
Burns 2009 compared music therapy to an audiobook control, finding a small increase in QoL in the music therapy group (Index of Well‐Being, score range 9 ‐ 63) (mean change score: 0.31, SD 1.73, N = 7) and a small decrease in the control group (mean change score: −0.22, SD 1.24, N = 3). However, the sample size was too small to draw any meaningful conclusions.
Comparison 4: Music therapy plus standard care versus music medicine plus standard care in adults
Only two studies reported on the direct comparison between music therapy and music medicine interventions. Both studies were with adult participants.
Primary outcomes
Psychological outcomes
State Anxiety
Two trials directly compared the effects of music therapy with music medicine on cancer participants' anxiety using a 100 mm visual analogue scale (Bradt 2015; Palmer 2015). Music therapy resulted in greater anxiety reduction than music medicine (MD −3.55, 95% CI −7.13 to 0.02, P = 0.05, I2 = 0%; Analysis 4.1). A total of 77.4% of the participants in the cross‐over trial by Bradt 2015 expressed a preference for receiving music therapy sessions for the remainder of their cancer treatment or future treatments. The main reasons cited by participants for this preferences were that they felt cared for by the music therapist, enjoyed the interactive and creative music‐making, and valued the opportunity for emotional expression and processing.
4.1. Analysis.

Comparison 4: Music therapy plus standard care versus music medicine plus standard care in adults, Outcome 1: Anxiety
Depression
We identified no studies for this outcome.
Distress
We identified no studies for this outcome.
Mood
We identified no studies for this outcome.
Hope
We identified no studies for this outcome.
Resilience
We identified no studies for this outcome.
Physical outcomes
Pain
We identified no studies for this outcome.
Fatigue
We identified no studies for this outcome.
Comparison 5: Music interventions plus standard care versus standard care plus alternative relaxation interventions in adults
Several studies compared music interventions with other relaxation interventions such as progressive muscle relaxation, guided imagery and relaxation, and verbal relaxation instructions. At this time, only single studies were identified per outcome. This precluded meta‐analysis of the results.
Primary outcomes
Psychological outcomes
State Anxiety
Straw 1991 compared music listening to guided imagery and relaxation training and found that both interventions reduced state anxiety as measured by the STAI‐S (score range 20 to 80) (guided imagery post‐test mean: 38.6, SD 10.01; music listening post‐test mean: 34.22, SD 10.12).
Depression
Stordahl 2009 compared music‐assisted relaxation with verbal relaxation instructions in 20 women with breast cancer and reported a lower level of depression on the Center for Epidimiologic Diseases ‐ Depression Scale (CES‐D, score range 0 to 60) following treatment in the music‐assisted relaxation treatment arm (N = 10; post‐test mean: 6.6, SD 5.02) than in the verbal relaxation treatment arm (N = 10; post‐test mean: 9.20, SD 10.96).
Mood
Stordahl 2009 also compared the impact of music‐assisted relaxation with verbal relaxation instructions on mood in women with breast cancer and found that music‐assisted relaxation resulted in lower scores (i.e. better mood) on the POMS‐SF (score range 14 to 70 as reported in this thesis) (post‐test mean: 6.5, SD 5.19) than verbal relaxation instructions (post‐test mean = 8.64, SD 6.42).
Distress
We identified no studies for this outcome.
Mood
We identified no studies for this outcome.
Hope
We identified no studies for this outcome.
Resilience
We identified no studies for this outcome.
Physical symptoms
Pain
Shaban 2006 compared the effects of progressive muscle relaxation (PMR) to music listening and found that PMR was more effective in reducing pain (100 mm VAS) (mean post‐test score: 6.22, SD 2.45) than listening to pre‐recorded music (mean post‐test score: 4.96, SD 2.76) in 100 participants.
Warth 2015 compared live‐music based relaxation provided by a trained music therapist with listening to a pre‐recorded mindfulness‐based stress reduction (MBSR) programme. Both resulted in similar pain reductions, namely from 2.95 (SD 2.3) at pretest to 2.45 (SD 2.1) at post‐test for music and from 2.89 (SD 2.17) to 2.57 (SD 2.16) for MBSR.
Fatigue
We identified no studies for this outcome.
Secondary outcomes
Quality of life
Straw 1991 compared a guided imagery and relaxation intervention to music listening and found that music listening led to a greater increase in QoL (Functional Living Index, score range 22 to 154) (mean change score: 16.33, SD 20.73) than the guided imagery and relaxation group (mean change score: 4.6, SD 20.49).
Warth 2015 reported a greater increase in QoL (EORTC‐QLQ‐C15) in the live‐music based relaxation treatment arm (mean change score: 10.6, SD 19.6) than in the MBSR treatment arm (mean change score: 7.54, SD 23.0).
Discussion
Summary of main results
The results of 26 trials (Table 3) suggest that music therapy and music medicine interventions may have a beneficial effect on anxiety in adults with cancer, with a reported anxiety reduction of 7.73 units, on average, on the STAI‐S (score range: 20 to 80) scale and −0.76 standardized units on other anxiety scales (which is considered a moderate to large effect). Although the magnitude of the effect differed across the studies, all but two trials (Chen 2020; O'Callaghan 2012) agreed on the direction of the point estimates. These anxiety‐reducing results are consistent with the findings of three other Cochrane systematic reviews on the use of music with coronary heart disease patients (Bradt 2013a), with mechanically ventilated patients (Bradt 2014), and for preoperative anxiety (Bradt 2013b). A comparison of music therapy with music medicine trials for anxiety reduction in people with cancer suggest a large treatment effect for music therapy studies (SMD −0.81) that was consistent across studies. Music medicine trials resulted in a similar treatment effect (SMD −0.87) but results were highly inconsistent across studies. Cohen 1988 suggested that an effect size of 0.20 could be considered a small effect, an effect size of 0.50 medium, and an effect size of 0.80 large. A direct comparison of music therapy with music medicine interventions for anxiety reduction in two studies indicated greater anxiety reduction of music therapy interventions. It is noteworthy that a large majority of the participants in one of the comparative studies expressed a preference for the music therapy intervention. The results of two trials suggest that music interventions may have a beneficial effect on anxiety in children with cancer with a reported reduction of ‐0.94 standardized units.
1. Studies per primary outcomes.
| Outcome | Studies included in the meta‐analyses |
| State Anxiety | Binns‐Turner 2008; Bro 2019; Bulfone 2009; Cai 2001; Chen 2013; Chen 2020; Danhauer 2010; Ferrer 2005; Firmeza 2017; Harper 2001; Jin 2011; Karadag 2019; Li 2004; Li 2012; Lin 2011; Mou 2020; O'Callaghan 2012; Rossetti 2017; Smith 2001; Vachiramon 2013; Verstegen 2018; Wan 2009; Wren 2019; Yates 2015; Zhao 2008; Zhou 2015 |
| Depression | Arruda 2016; Bates 2017; Cai 2001; Cassileth 2003; Chen 2020; Karadag 2019; Li 2012; Verstegen 2018; Wan 2009; Yates 2015; Zhou 2015 |
| Distress | Clark 2006; Rossetti 2017 |
| Mood | Beck 1989; Burrai 2014; Cassileth 2003; Moradian 2015; Ratcliff 2014 |
| Hope | Arruda 2016; Verstegen 2016 |
| Pain | Arruda 2016; Binns‐Turner 2008; Danhauer 2010; Fredenburg 2014a; Huang 2006; Letwin 2017; Li 2012; Reimnitz 2018; Verstegen 2016; Verstegen 2018; Wan 2009; Wren 2019 |
| Fatigue | Bates 2017; Cassileth 2003; Chen 2020; Clark 2006; Ferrer 2005; Fredenburg 2014b; Moradian 2015; Reimnitz 2018; Rosenow 2014; Wren 2019 |
The results of 12 studies (Table 3) suggest that music interventions may reduce depression in adults with cancer. The results of a single study (Robb 2014) suggest that music therapy may help adolescents and young adults employ positive coping strategies during stem cell transplant, a high‐risk and high‐intensity treatment. We found no evidence of effect for distress or mood.
The results of two studies (Table 3) suggest that music interventions may increase hope in adult cancer patients by an average of 3.19 units on the Herth Hope Index (score range: 12 to 48).
As for the effect of music on physical symptoms in adults, the results of 12 trials (Table 3) suggest that music has a moderate pain‐reducing effect of −0.67 standardized units. Music interventions also had a small effect on fatigue (−0.28 standardized units). We found no evidence for an effect of music on physical status. The results of a single study with pediatric oncology participants also found pain‐reducing effects of music. Reduction of anxiety, depression, fatigue and pain are important outcomes for people with cancer, as they have an impact on health and overall QoL.
It is important that careful consideration is given to the implementation of music listening interventions. The results of Kwekkeboom 2003 indicate that listening to music through headphones may be contraindicated during painful procedures because it prevents the patient from hearing the surgeon's instructions and comments. This may greatly increase patients' anxiety and, consequently, their perceived pain. In this case, it is better to listen to music without headphones.
Furthermore, results suggest that music interventions may have a beneficial effect on several physiological responses in adult patients with cancer. Listening to music may reduce heart rate by an average of three to four beats per minute. These results are consistent with the findings of a Cochrane systematic review on the use of music with coronary heart disease patients (Bradt 2013a), which reported a heart rate reduction of 3.4 bpm. Similar results were reported in a Cochrane review on music interventions for mechanically ventilated patients (Bradt 2014), namely a mean heart rate reduction of 3.95 bpm. In the case of a resting heart rate within normal range, a reduction of 4 bpm may not be clinically significant. However, it might be in the case of a tachycardiac rate. In a study examining the quantitative relationship between resting heart rate reduction and clinical benefit, Cucherat 2007 found that each 10 bpm reduction in heart rate was estimated to reduce the relative risk of cardiac death by 30%. The findings of this review suggest that music listening may have minimal impact on respiratory rate (less than 1 breath per minute), yet the findings of other systematic reviews suggest that listening to music may help reduce respiratory rate by 2 to 3 breaths per minute (Bradt 2013a; Bradt 2014). The results of this review also indicate that listening to music may have a beneficial effect on SBP and DBP. Trials on music listening with cardiac patients and mechanically ventilated patients have also reported reductions in systolic blood pressure (Bradt 2013a; Bradt 2014). The reduction of heart rate and blood pressure corresponds with the anxiety‐reducing effects found by subjective outcome measures in this review.
Only one study in this review examined the effects of music on physiological responses in children and reported beneficial treatment effects of music for heart rate, respiratory rate, oxygen saturation level and blood pressure during lumbar puncture (Nguyen 2010).
No evidence of support was found for an effect of music interventions on oxygen saturation level in adult patients. Single trials included in this review found support for a beneficial effect of music on mean arterial pressure .
Music therapy interventions had a moderate effect of 0.4 standardized units on quality of life in adults, whereas we found no support for an effect for music medicine studies. Two studies that compared music therapy with audiobook control in adolescents and young adults did not find support for spiritual well‐being (Burns 2009; Robb 2014). Two music therapy studies with adults reported conflicting results for this outcome. Finally, a single study with adolescents and young adults during stem cell transplant reported beneficial effects of music therapy on perceived social support and the family environment.
Subgroup analyses of treatment effects between music therapy and music medicine studies was possible for six outcomes, namely anxiety, depression, mood, pain, fatigue and quality of life. There was a difference for quality of life and fatigue, with music therapy studies contributing to a larger pooled treatment effect, whereas no evidence of effect was found for music medicine studies; we found no difference between music therapy and music medicine studies for the other outcomes. However, it is worth noting that, for all outcomes, music therapy interventions resulted in consistent findings across studies whereas the results of music medicine studies were highly heterogeneous for these outcomes. As a result, there is greater confidence in the treatment effects of music therapy interventions delivered by a trained music therapist than in the treatment effects of music medicine interventions.
We could examine the impact of music preference for anxiety, depression, pain, heart rate, systolic and diastolic blood pressure. Music preference did not impact on the treatment effect of music.
For all outcomes, the sensitivity analyses were robust to the original conclusions.
The Table 1 and Table 2 provide a summary of the main results of this review with associated risks. Because participants could not be blinded to music interventions and subjective outcomes are measured by self‐report measures, there was a high risk of bias for most studies. As a result, the evidence ranged from uncertain to very uncertain for most outcomes.
It is important to note that the included studies compared music interventions with standard care (except for Analysis 3.1 and Analysis 3.2). Therefore, it is unclear how much of the treatment effect is attributable to the specific effect of music‐based interventions versus how much is due to contextual effects (e.g. participant‐therapist relationship) (Rossettini 2018).
Overall completeness and applicability of evidence
This review included 81 randomized controlled trials and quasi‐randomized trials. Seventy‐four trials enrolled adult oncology participants whereas seven trials enrolled pediatric participants with cancer.
Forty‐three trials used listening to pre‐recorded music, and 38 trials used music therapy interventions that actively engaged the participants (Characteristics of included studies). We were able to compare the treatment effects of music therapy studies with music medicine studies for six outcomes. For the other outcomes, this was not possible due to an insufficient number of music therapy and music medicine studies per outcome.
This review included both music therapy and music medicine studies, as defined in the Background. Music therapists who work with cancer patients do not limit their interventions to offering music listening for relaxation purposes. Music therapists are specially trained clinically and academically to carefully select music interventions to offer emotional and spiritual support, support communication with loved ones, enhance a sense of control, and improve physical well‐being in patients with cancer. Comparative analyses suggest that music therapy interventions are more effective than music medicine interventions in improving quality of life and fatigue. We found no differences between music therapy and music medicine interventions for other outcomes, but it is worth noting that the results of music therapy studies were consistent across trials whereas the results of music medicine studies were highly inconsistent across studies. This is likely due to the fact that music therapists are trained to meet the individual needs of patients through music interventions (e.g. meeting the patient's in‐the‐moment needs when offering live music) rather than offering a limited selection of pre‐recorded music, which may not be suitable for all patients. Participants in a cross‐over trial who experienced both music therapy and music medicine interventions overwhelmingly preferred the music therapy sessions because of the personal attention and care, the creativity of the interactive music‐making, and the opportunity for emotional expression through singing and playing instruments.
In general, the trials that used listening to pre‐recorded music provided little information about the music selections used, except for mentioning general music styles (e.g. new age, classical music, easy listening, etc). Music within each of these styles can vary widely, and more detailed information would help clinicians make well‐informed decisions regarding music selections.
The frequency and duration of the interventions varied widely across the trials. Twenty‐four trials offered a single music session. We would like to suggest that offering multiple music listening sessions allows for the participant to give feedback about the music, select different music if needed, and become more skilled in using music for relaxation purposes. In the case of music therapy interventions, multiple sessions allow for the development of a therapeutic relationship and deepening of the therapeutic process through the music. This may lead to greater health benefits. At this time, however, the relationship between the frequency and duration of treatment and treatment effect remains unclear. Further investigation into the optimal frequency and duration of music interventions for specific outcomes in people with cancer is needed.
Presently, we cannot provide data regarding cost or cost‐effectiveness of music therapy or music medicine applications in the care of cancer patients, as the reviewed trials did not provide these data.
Quality of the evidence
Because of the large number of trials at high risk of bias, readers should interpret the findings of this review with caution. Often blinding of participants is not possible in music medicine or music therapy studies unless a comparative design is used (e.g. Bradt 2015). Many of the trials in this review included subjective outcomes, such as anxiety, pain, mood and quality of life. When participants cannot be blinded to the intervention, there is definitely an opportunity for bias when they are asked to report on these subjective outcomes.
For many trials, the principal investigators needed to be contacted to provide additional methodological and statistical information, which improved the quality of evidence in the review.
For anxiety and quality of life, there were large effects across studies. The trials did not agree on the size of effect, with some reporting much larger beneficial effects than others, resulting in large confidence intervals. For both outcomes, the certainty of the evidence was low and very low, respectively . For pain and mood, the pooled effect sizes were moderate to large but the evidence was very uncertain. For depression, the pooled effect was small to moderate but here too, there was very low‐certainty evidence. Finally, the pooled effect for fatigue was small and the evidence was of low certainty (Table 1; Table 2).
Potential biases in the review process
The strength of our review is that we searched all available databases and a large number of music therapy journals (English, German, and French language), checked reference lists of all relevant trials, contacted relevant experts for identification of unpublished trials, and included publications without restricting language. We requested additional data, where necessary, for all trials we considered for inclusion. This allowed us to get accurate information on the trial quality and data for most trials and helped us make well‐informed trial selection decisions. The database searches were completed more than one year ago. Due to the COVID 19 pandemic, we experienced delays in data extraction and analyses. We decided not to update the searches closer to the time of publication as to not further delay the publication of this updated review.
Although we cannot completely rule out the possibility that we missed some published and unpublished trials, we are confident that our detailed search strategy combined with extensive handsearching identified all relevant trials. It is possible that we did not identify some grey literature; however, it is doubtful that this would have had a significant impact on our results. Grey literature tends to include trials with relatively small numbers of participants and inconclusive results (McAuley 2000).
One of the included trials (Bradt 2015) was conducted by the lead author of this review. As for all new studies included in this update, the risk of bias was independently assessed by JBi, CD, and KMC. Data extraction was completed independently by JBr, JBi, and KMC.
Agreements and disagreements with other studies or reviews
The findings of this review are consistent with the results of a review (32 RCTs and controlled clinical trials) assessing the effect of music interventions on psychological and physical outcomes in cancer patients (Zhang 2012). Zhang and colleagues reported a mean difference of −12.3 for anxiety (STAI‐S, score range 20 to 80), −6.23 for depression (Self‐Rating Depression Scale, score range 20 to 80), −0.52 for pain (0 to 10 numeric rating scale) and 13.32 for quality of life (Quality of Life ‐ Cancer, score range 0‐100). The authors also reported that the effects of music on vital signs, especially blood pressure, were small. In contrast, Nightingale 2013 (a review of four RCT studies) evaluated the effects of music on anxiety in adult cancer patients, reporting no evidence of an effect for music on anxiety. This was likely due to the small number of studies included in this review. In addition, reviewers included Kwekkeboom 2003 in the meta‐analysis, which was a quite problematic trial in terms of the implementation of the music listening interventions, as discussed in the Results section of our review. Study participants reported that the use of headphones while undergoing painful medical procedures was anxiety‐provoking because it prevented them from hearing the surgeon. In addition, Nightingale 2013 included Hanser 2006 in the meta‐analysis, whereas we included this study in the narrative only. Our decision was based on a very high attrition rate (40%) and the inability to implement the music therapy intervention within the a priori set time frame, thereby highly diluting the intervention, as reported by the authors.
Kohler 2020 conducted a systematic review of music therapy studies with adult oncology patients. The authors reported a pooled effect size for psychological well‐being (mood, anxiety, depression), physical symptom distress (pain, fatigue, physical symptom scales) and quality of life. The reported pooled effect size for quality of life (d = 0.36, 95% 0.07 to 0.65, P = 0.023, I2 = 0%) was similar to the findings in our review for music therapy studies (Analysis 1.28).
Authors' conclusions
Implications for practice.
This systematic review indicates that music interventions may have beneficial effects on anxiety, depression, hope, pain, and fatigue in adults with cancer. Music therapy interventions had a moderate effect on QoL in adults, whereas we found no support for an effect for music medicine studies. Furthermore, the results suggest that music may reduce heart rate and blood pressure, though this reduction is rather small and therefore may not be clinically significant. Results from single trials suggest that music listening in cancer patients undergoing surgery may reduce anesthetic and analgesic consumption and reduce the length of hospital stay, but more research is needed before drawing solid conclusions. Results from a single study furthermore suggest that post‐surgery recovery time may be shortened when a music therapist offers live, individualized music before and during surgery. Overall, evidence of the trials included in this review suggest that music interventions may be offered as a complementary treatment to adults with cancer and that music therapy interventions delivered by a trained music therapist may lead to more consistent results.
No evidence of effect was found for distress, mood, physical functioning, or oxygen saturation. However, only a small number of trials investigated the effects of music on these outcomes. More research is needed. We cannot draw any conclusions at this time regarding the effects of music interventions on resilience, spiritual well‐being, mean arterial pressure, immunologic functioning or communication behaviours in adults because the results of the studies that included these outcomes could not be pooled or because we could only identify one trial.
A small number of trials included pediatric oncology participants. Not all trials included the same outcomes, therefore, we could only compute pooled effect sizes for a small number of outcomes. Those findings suggest that music interventions may reduce anxiety, but no evidence of an effect was found for distress or spiritual well‐being. However, there were only two trials included for each of these outcomes, thus more research is needed. At this time, we cannot draw conclusions regarding the effects of music interventions on mood, resilience, coping, QoL, communication behaviors, pain, or physiological responses in pediatric patients with cancer, because the results of the studies that included these outcomes could not be pooled or because we could only identify one trial.
Because participants cannot be blinded to music interventions and subjective outcomes are measured by self‐report measures, there was a high risk of bias for most studies. Therefore, the findings of this review need to be interpreted with caution.
Implications for research.
This systematic review provides evidence that music interventions may have beneficial effects on anxiety, depression, hope, pain, fatigue, heart rate and blood pressure in adults with cancer. Only a few trials with pediatric participants were included and therefore no conclusions can be drawn at this time regarding the impact of music interventions on pediatric oncology patients. Comparative analyses between music therapy and music medicine interventions indicate that music therapy is more effective in improving QoL and fatigue than music medicine interventions. Moreover, the treatment effects of music therapy interventions show greater consistency across studies than music medicine interventions for anxiety, depression, and pain. At this time, more RCTs are needed to determine the effectiveness of music medicine versus music therapy for other outcomes in this review. This can be achieved by including more music medicine as well as music therapy RCTs in future reviews, when these become available or, alternatively, future trials could directly compare the effects of these two types of interventions. It is important to note that Bradt 2015 undertook such a comparative study based on the recommendation of the original systematic review, concluding that both music therapy and music medicine interventions were similarly effective for symptom management. However, the results of their mixed methods research study clearly indicated that even listening to pre‐recorded music can evoke strong emotions and existential issues in people with cancer and that the participants in this study were grateful for the presence of a music therapist to process these emotions and fears. Participants furthermore emphasized the importance of interactive music‐making, as it allowed them to access their creativity; this is considered an important resource for the facilitation of resilience in the face of life's challenges. Future research should explore patient characteristics as moderators of treatment benefits of music therapy interventions versus listening to pre‐recorded music. For example, Bradt 2015 suggested that listening to music may cause distress in patients who have a negative outlook on life. It is possible that these patients are at greater risk for music's powerful capacity to access sad and traumatic memories, and such patients may be better served by listening to music in the presence of a music therapist who can help them process their emotions. On the other hand, Bradt and colleagues emphasized that some patients have a great need for stability and emotional security during this challenging time in their life and may therefore prefer the familiarity of their own music. Self‐selected music presents predictable musical and emotional content and may, therefore, provide a much needed holding environment for the patient.
We recommend that future research efforts aim to enhance understanding of how music therapy and music medicine interventions can be optimized for symptom management, how music interventions can best serve patients along the cancer treatment trajectory, and what unique aspects of music therapy and music medicine interventions contribute to the care of patients (Bradt 2015).
As stated in other reviews, it is important that investigators consider qualitative and mixed methods research, as these enhance understanding of the qualitative aspects of a patient's experience and identify factors that may contribute to or limit the effectiveness of music therapy or music medicine interventions (Bradt 2010; Bradt 2013a; Bradt 2014).
Future trials that use listening to pre‐recorded music should report more details related to the music selections made available to participants and exercise greater care in selecting music that reflects the patient's true preference (rather than just giving the patient the option to select from four or five general genres). It is recommended that reporting guidelines for music‐based interventions as outlined by Robb 2010 are used in clinical trial reports. In addition, researchers need to carefully consider the potential negative impact of the use of headphones during procedures because of hampered communication between the patient and medical personnel.
More research is needed that examines the relationship between frequency and duration of music interventions and treatment effects.
Many trials used small sample sizes and did not indicate the use of power calculations. Future trials need to include power calculations in order to use adequate sample sizes.
More studies are needed on the use of music interventions in pediatric patients with cancer. Of the 81 trials in this review, only seven studies focused on outcomes in children and adolescents.
Many studies examined the effects of music interventions on anxiety. Given that the findings regarding anxiety‐reducing effects of music are quite robust, it is important that future studies focus on other outcomes included in this review.
Formal cost‐benefit evaluations of music medicine and music therapy are needed.
What's new
| Date | Event | Description |
|---|---|---|
| 12 August 2022 | Amended | Correction to analyses order made. |
History
Protocol first published: Issue 1, 2008 Review first published: Issue 8, 2011
| Date | Event | Description |
|---|---|---|
| 7 October 2021 | New citation required and conclusions have changed | This review is the second update of the previously published Cochrane reviews (Bradt 2011; Bradt 2016), The prior update (Bradt 2016) included 52 studies. This second update includes 29 new trials. In total, the evidence rests on 81 trials with a total of 5592 participants. In this update, we separated clinical trials with adults from those with pediatric patients in the meta‐analyses. Because few trials with pediatric patients were available, we could not yet draw conclusions about the impact of music interventions on pediatric patients. Our conclusions about the impact of music interventions on state anxiety, depression, pain, and quality of life in adults with cancer remain similar to those in Bradt 2016 but with the addition of new trials, the estimate is more precise. For fatigue, the pooled effect was slightly lower but the precision of the estimate greatly improved compared to Bradt 2016. The conclusions for physical functioning remained the same. No new studies were added to the meta‐analysis for mood. The conclusions remain unchanged. This review included hope as a new outcome. The pooled effect of two studies suggested that music may improve hope in adults with cancer. The conclusions for the effects of music interventions on vital signs remained similar to those of the previous review. Because of the addition of many trials in this update, we were able to conduct a priori determined subanalyses comparing music therapy with music medicine studies and comparing patient‐preferred music with researcher‐selected music for more outcomes. |
| 7 October 2021 | New search has been performed | In the previous version of this review (Bradt 2016), we searched the databases until January 2016. In this updated version, we reran the searches until April 2020. |
| 29 April 2016 | New citation required and conclusions have changed | This review is an update of the previous Cochrane review that included 30 studies (Bradt 2011). This updated review includes 22 new trials. One of the previous authors, Dr Denise Grocke, decided not to participate in the update of this review, and we added a new co‐author, Aaron Teague. Our conclusions about the impact of music interventions on state anxiety in people with cancer remain similar to those in Bradt 2011. Although the pooled effect of the studies that used the Spielberger State Anxiety Inventory (STAI) was slightly lower than in the previous review, the addition of trials examining this outcome resulted in a more precise estimate. The pooled effect of studies that used measurement tools other than the STAI was higher than in the previous review. The conclusions for the effect of music interventions on depression changed. Whereas the previous review did not find support for an effect, this review update found a moderate effect for depression. We also found a similar effect size (moderate) as the previous review for mood, but the pooled effect was no longer statistically significant in this update. The conclusions for the effect of music interventions on pain changed. Whereas the previous review reported a moderate effect, this review update found a large effect for pain. The conclusions for the effect of music interventions on fatigue also changed. Whereas the previous review did not find evidence of an effect, this review update found a small to moderate effect for music interventions on fatigue. The conclusions for physical functioning remained the same. The conclusion for the effect of music interventions on quality of life remained similar, that is, there was a large pooled effect size that was not statistically significant. However, a subgroup analysis revealed that music therapy interventions resulted in a moderate and statistically significant effect that was consistent across trials, whereas music medicine studies resulted in a large but heterogeneous effect size that was not statistically significant. The conclusions for the effects of music interventions on vital signs remained similar to those of the previous review. This review update included additional outcomes such as resilience, coping, and anesthetic and analgesic intake, but no meta‐analysis was possible because we only identified one study per outcome. Because of the addition of many trials in this update, we were able to conduct a priori determined sub‐analyses comparing music therapy with music medicine studies and comparing patient‐preferred music with researcher‐selected music for several of the outcomes. |
| 29 April 2016 | New search has been performed | In the previous version of this review, we searched the databases until September 2010 (Bradt 2011). In this updated version we reran the searches until January 2016. We also extended our handsearching to include two additional journals, namely Music Medicine and Approaches. In this updated review we have revised the 'Risk of bias' tables for all studies according to the new Cochrane 'Risk of bias' tool. |
| 15 July 2011 | Amended | Label revision in forest plot of 'distress' outcome. |
| 24 June 2008 | Amended | Converted to new review format. |
Acknowledgements
We would like to thank and acknowledge Clare Jess (Managing Editor), Jo Platt (Information Specialist) and Jo Morrison (Co‐ordinating Editor ) of Cochrane Gynaecological, Neuro‐oncology and Orphan Cancers (GNOC). We would also like to acknowledge the following research assistants for their help with screening, article retrieval, handsearching, data extraction, and data input: Patricia Gonzalez, Andi McGraw Hunt, and Patricia Winters, graduate assistants at Temple University, for their help with the original review; Minjung Shim, Kelly L By, Johanna Dwinells, and Karolina Bryl, research assistants at Drexel University, for their help with the 2016 update of the review; Brigette Schneible, research fellow at Drexel University, for her help with the current review; and Denise Grocke, Lucanne Magill and Aaron Teague for their contributions as authors on previous versions of this review.
The authors and Cochrane GNOC Team, are grateful to the following peer reviewers for their time and comments: Katja Boehm and Barbara Wheeler.
We would like to thank the Cystic Fibrosis Group for permission to modify their data extraction form.
This project was supported by the National Institute for Health Research, via Cochrane Infrastructure funding to the Cochrane Gynaecological, Neuro‐oncology and Orphan Cancer Group. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health.
Appendices
Appendix 1. CENTRAL search strategy
#1 MeSH descriptor Neoplasms explode all trees #2 malignan* or neoplasm* or cancer or carcinoma* or tumo* #3 (#1 OR #2) #4 MeSH descriptor Music explode all trees #5 MeSH descriptor Music Therapy explode all trees #6 music* or melod* #7 sing or sings or singing or song* or compose or composing or improvis* #8 (#4 OR #5 OR #6 OR #7) #9 (#3 AND #8)
Appendix 2. MEDLINE search strategy (OvidSp)
1 exp neoplasms/ 2 (malignan* or neoplas* or cancer* or carcinoma* or tumo*).mp. 3 1 or 2 4 music/ or music therapy/ 5 (sing or sings or singing or song* or improvis*).mp. 6 (music* or melod*).mp. 7 4 or 5 or 6 8 3 and 7 9 randomized controlled trial.pt. 10 controlled clinical trial.pt. 11 randomized.ab. 12 placebo.ab. 13 clinical trials as topic.sh. 14 randomly.ab. 15 trial.ti. 16 9 or 10 or 11 or 12 or 13 or 14 or 15 17 8 and 16
key: mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept, rare disease supplementary concept, unique identifier; pt=publication type; ab=abstract; ti=title
Appendix 3. Embase search strategy (OvidSp)
1 exp neoplasm/ 2 (malignan* or neoplasm* or cancer* or carcinom* or tumo*).mp. 3 1 or 2 4 music therapy/ or music/ 5 (sing or sings or singing or song* or improvis*).mp. 6 (music* or melod*).mp. 7 4 or 5 or 6 8 3 and 7 9 crossover procedure/ 10 double‐blind procedure/ 11 randomized controlled trial/ 12 single‐blind procedure/ 13 random*.mp. 14 factorial*.mp. 15 (crossover* or cross over* or cross‐over*).mp. 16 placebo*.mp. 17 (double* adj blind*).mp. 18 (singl* adj blind*).mp. 19 assign*.mp. 20 allocat*.mp. 21 volunteer*.mp. 22 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 23 8 and 22
key: [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword]
Appendix 4. CINAHL search strategy (EbscoHost)
S22 S21 and S7 and S4 S21 S20 or S19 or S18 or S17 or S16 or S15 or S14 or S13 or S12 or S11 or S10 or S9 or S8 S20 TI ( (singl* or doubl* or treb* or tripl*) ) and TI ( (blind* or mask*) ) S19 AB ( (singl* or doubl* or treb* or tripl*) ) and AB ( (blind* or mask*) ) S18 Randomized controlled trials/ S17 evaluation studies/ S16 comparative study/ S15 prospective studies/ S14 clinical trial/ S13 study design/ S12 AB ( (control$ or prospectiv$ or volunteer$) ) or TI ( (control$ or prospectiv$ or volunteer$) ) S11 AB random$ or TI random$ S10 AB placebo$ or TI placebo$ S9 placebos/ S8 AB (clin$ N25 trial$) or TI (clin$ N25 trial$) S7 S5 OR S6 S6 TX (malignan$ or neoplasm$ or cancer or carcinoma$ or tumo$) S5 neoplasms/ S4 S3 OR S2 OR S1 S3 TX (music$ OR melod$ OR sing OR singing OR sings OR song$ OR improvis$) S2 music therapy/ S1 music/
Appendix 5. PsycInfo search strategy (OvidSp)
1 exp Neoplasms/ 2 (malignan$ or neoplasm$ or cancer or carcinoma$ or tumo$).tw. 3 1 or 2 4 music/ or music therapy/ 5 (music$ or melod$).tw. 6 (sing or sings or singing or song$ or improvis$).tw. 7 or/4‐6 8 3 and 7 9 empirical study.md. 10 followup study.md. 11 longitudinal study.md. 12 prospective study.md. 13 quantitative study.md. 14 "2000".md. 15 treatment effectiveness evaluation/ 16 exp hypothesis testing/ 17 repeated measures/ 18 exp experimental design/ 19 placebo$.ti,ab. 20 random$.ti,ab. 21 (clin$ adj25 trial$).ti,ab. 22 ((singl$ or doubl$ or trebl$ or tripl$) adj (blind$ or mask$)).ti,ab. 23 or/9‐22 24 8 and 23 25 limit 24 to human
Appendix 6. LILACS search strategy (Virtual Health Library)
((music$)) and ((((malignan$ or neoplasm$ or cancer or carcinoma$ or tumo$)) or (("cancer"))))
Appendix 7. Social Science Citation Index search strategy (ISI)
#1 Topic=(music*) #2 TopiC= (music therapy) #3 Topic=(singing or sings or song* or improvis* or melod*) #4 #1 OR #2 OR #3 #5 Topic=(neoplasm*) #6 Topic=(malignan* or neoplasm* or cancer or carcinoma* or tumo*) #7 #5 OR #6 #8 Topic=(random allocation) #9 Topic=(controlled clinical trial*) #10 Topic=(randomized controlled trial*) #11Topic=(double blind method*) #12 Topic=(single blind method*) #13 Topic=(clinical trial*) #14 Topic=(placebo*) #15 Topic=(random*) #16 #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 #17 #4 AND #7 AND # 16
Appendix 8. CancerLit search strategy
music OR (music therapy)
Appendix 9. CAIRSS search strategy
Cancer OR neoplasm OR neoplasms Malignant OR carcinoma OR carcinomas Tumor OR tumour
Appendix 10. Proquest Digital Dissertations search strategy (Proquest)
Music and (cancer or tumor or malignant or neoplasm)
Appendix 11. clinicaltrials.gov search strategy
music OR "music therapy"
Appendix 12. Current Controlled Trials search strategy
music OR "music therapy"
Appendix 13. National Research Register search strategy
music
Appendix 14. RILM Abstracts of Music Literature search strategy (EbscoHost)
Cancer or tumor or malignant or neoplasm
Appendix 15. Study Selection, Quality Assessment & Data Extraction Form
Review:Music interventions for improving psychological and physical outcomes in cancer patients
Name Coder:
Date:
Paper Code:
| First author | Title | Journal/Conference Proceedings etc | Year | Language |
Appendix 16. Original search strategies
MEDLINE search strategy (OvidSp)
1 exp Neoplasms/ 2 (malignan$ or neoplasm$ or cancer or carcinoma$ or tumo$).tw. 3 1 or 2 4 music/ or music therapy/ 5 (sing or sings or singing or song$ or improvis$).tw. 6 (music$ or melod$).tw. 7 or/4‐6 8 Randomized Controlled Trials/ 9 random allocation/ 10 Controlled Clinical Trials/ 11 control groups/ 12 clinical trials/ 13 double‐blind method/ 14 single‐blind method/ 15 Placebos/ 16 placebo effect/ 17 cross‐over studies/ 18 Multicenter Studies/ 19 Therapies, Investigational/ 20 Research Design/ 21 Program Evaluation/ 22 evaluation studies/ 23 randomized controlled trial.pt. 24 controlled clinical trial.pt. 25 clinical trial.pt. 26 multicenter study.pt. 27 evaluation studies.pt. 28 random$.tw. 29 (controlled adj5 (trial$ or stud$)).tw. 30 (clinical$ adj5 trial$).tw. 31 ((control or treatment or experiment$ or intervention) adj5 (group$ or subject$ or patient$)).tw. 32 (quasi‐random$ or quasi random$ or pseudo‐random$ or pseudo random$).tw. 33 ((multicenter or multicentre or therapeutic) adj5 (trial$ or stud$)).tw. 34 ((control or experiment$ or conservative) adj5 (treatment or therapy or procedure or manage$)).tw. 35 ((singl$ or doubl$ or tripl$ or trebl$) adj5 (blind$ or mask$)).tw. 36 (coin adj5 (flip or flipped or toss$)).tw. 37 latin square.tw. 38 (cross‐over or cross over or crossover).tw. 39 placebo$.tw. 40 sham.tw. 41 (assign$ or alternate or allocat$ or counterbalance$ or multiple baseline).tw. 42 controls.tw. 43 (treatment$ adj6 order).tw. 44 or/8‐43 45 3 and 7 and 44 46 limit 45 to humans
Embase search strategy (OvidSp)
1 exp Neoplasm/ 2 (malignan* or neoplasm* or cancer or carcinom* or tumo*).mp. [mp = title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] 3 1 or 2 4 exp music therapy/ or exp music/ 5 (music* or melod*).mp. [mp = title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] 6 (sing or sings or singing or song* or compose or composing or improvis*).mp. [mp = title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] 7 6 or 4 or 5 8 Randomized Controlled Trial/ 9 Randomization/ 10 exp Controlled Clinical Trial/ 11 Control Group/ 12 Clinical Trial/ 13 Double Blind Procedure/ 14 Single Blind Procedure/ 15 Placebo/ 16 Crossover Procedure/ 17 Multicenter Study/ 18 Experimental Therapy/ 19 Methodology/ 20 exp Health Care Quality/ 21 exp Evaluation/ 22 random*.mp. [mp = title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] 23 (controlled adj5 (trial* or stud*)).mp. [mp = title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] 24 (clinical* adj5 trial*).mp. [mp = title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] 25 ((control or treatment or experiment* or intervention) adj5 (group* or subject* or patient*)).mp. [mp = title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] 26 (quasi‐random* or quasi random* or pseudo‐random* or pseudo random*).mp. [mp = title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] 27 ((multicenter or multicentre or therapeutic) adj5 (trial* or stud*)).mp. [mp = title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] 28 ((control or experiment* or conservative) adj5 (treatment or therapy or procedure or manage*)).mp. [mp = title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] 29 ((single* or double* or tripl* or trebl*) adj5 (blind* or mask*)).mp. [mp = title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] 30 (coin adj5 (flip or flipped or toss*)).mp. [mp = title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] 31 latin square.mp. [mp = title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] 32 (cross‐over or cross over or crossover).mp. [mp = title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] 33 placebo*.mp. [mp = title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] 34 sham.mp. [mp = title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] 35 (assign* or alternate or allocat* or counterbalance* or multiple baseline).mp. [mp = title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] 36 controls.mp. [mp = title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] 37 (treatment* adj6 order).mp. [mp = title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] 38 35 or 33 or 32 or 11 or 21 or 26 or 17 or 22 or 18 or 30 or 23 or 16 or 13 or 29 or 27 or 25 or 28 or 36 or 9 or 12 or 14 or 15 or 20 or 8 or 34 or 37 or 24 or 10 or 19 or 31 39 38 and 3 and 7 40 39
CancerLit Search Strategy (CancerLit was searched in the original review but is no longer available)
music OR (music therapy)
Musictherapyworld.de (was searched in the original review but is no longer functional)
The site's research register, dissertation archive, and bibliography were searched in 2008 for the following terms: cancer or tumor or tumour or malignant or neoplasm or neoplasms or carcinoma or carcinomas
Data and analyses
Comparison 1. Music intervention plus standard care versus standard care alone in adults.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Anxiety (STAI) | 17 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1.1 All studies | 17 | 1381 | Mean Difference (IV, Random, 95% CI) | ‐7.73 [‐10.02, ‐5.44] |
| 1.1.2 Sensitivity analysis (randomization method) | 15 | 1121 | Mean Difference (IV, Random, 95% CI) | ‐7.83 [‐10.91, ‐4.76] |
| 1.2 Anxiety (non‐STAI (full version) measures) | 9 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.2.1 All studies | 9 | 882 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.76 [‐1.28, ‐0.25] |
| 1.2.2 Sensitivity analysis (randomization method) | 5 | 530 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.72 [‐1.67, 0.23] |
| 1.2.3 Sensitivity analysis (< 10% non‐cancer excluded) | 8 | 869 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.75 [‐1.30, ‐0.21] |
| 1.3 Anxiety (intervention subgroup) | 23 | 2003 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.86 [‐1.22, ‐0.50] |
| 1.3.1 Music therapy studies | 4 | 144 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.81 [‐1.16, ‐0.46] |
| 1.3.2 Music medicine studies | 19 | 1859 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.87 [‐1.28, ‐0.47] |
| 1.4 Anxiety (music preference) | 16 | 1590 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.82 [‐1.22, ‐0.41] |
| 1.4.1 Patient‐preferred music | 13 | 1288 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.81 [‐1.30, ‐0.32] |
| 1.4.2 Researcher‐selected music | 3 | 302 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.79 [‐1.19, ‐0.39] |
| 1.5 Anxiety (music‐guided relaxation) | 15 | 1334 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.93 [‐1.38, ‐0.47] |
| 1.5.1 Music‐guided relaxation studies | 4 | 476 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.61 [‐2.56, ‐0.65] |
| 1.5.2 Listening to music only | 11 | 858 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.67 [‐1.09, ‐0.24] |
| 1.6 Depression | 12 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.6.1 All studies | 12 | 1021 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.41 [‐0.67, ‐0.15] |
| 1.6.2 Sensitivity analysis (randomization method) | 10 | 779 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.32 [‐0.59, ‐0.04] |
| 1.6.3 Sensitivity analysis (< 10% non‐cancer studies excluded) | 11 | 1008 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.41 [‐0.68, ‐0.15] |
| 1.6.4 Sensitivity analysis (outliers removed) | 9 | 674 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.36, ‐0.05] |
| 1.7 Depression (intervention subgroup) | 12 | 1021 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.41 [‐0.67, ‐0.15] |
| 1.7.1 Music therapy studies | 5 | 225 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.19 [‐0.46, 0.07] |
| 1.7.2 Music medicine studies | 7 | 796 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.53 [‐0.90, ‐0.17] |
| 1.8 Depression (music preference) | 7 | 708 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.55 [‐0.91, ‐0.19] |
| 1.8.1 Patient‐preferred music | 3 | 375 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.59 [‐1.26, 0.09] |
| 1.8.2 Researcher‐selected music | 4 | 333 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.53 [‐0.98, ‐0.07] |
| 1.9 Distress | 2 | 127 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.38 [‐1.43, 0.66] |
| 1.10 Mood | 4 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.10.1 All studies | 4 | 221 | Std. Mean Difference (IV, Random, 95% CI) | 0.53 [‐0.03, 1.10] |
| 1.10.2 Sensitivity analysis (randomization method) | 3 | 177 | Std. Mean Difference (IV, Random, 95% CI) | 0.68 [‐0.04, 1.39] |
| 1.11 Mood (intervention subgroup) | 4 | 221 | Std. Mean Difference (IV, Random, 95% CI) | 0.53 [‐0.03, 1.10] |
| 1.11.1 Music therapy studies | 2 | 104 | Std. Mean Difference (IV, Random, 95% CI) | 0.37 [‐0.13, 0.87] |
| 1.11.2 Music medicine studies | 2 | 117 | Std. Mean Difference (IV, Random, 95% CI) | 0.73 [‐0.54, 1.99] |
| 1.12 Hope | 2 | 53 | Mean Difference (IV, Random, 95% CI) | 3.19 [0.12, 6.25] |
| 1.13 Pain | 12 | 1206 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.72 [‐1.01, ‐0.42] |
| 1.13.1 All studies | 12 | 632 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.67 [‐1.07, ‐0.26] |
| 1.13.2 Sensitivity analysis (< 10% non‐cancer studies excluded) | 9 | 574 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.77 [‐1.25, ‐0.29] |
| 1.14 Pain (intervention subgroup) | 12 | 632 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.67 [‐1.07, ‐0.26] |
| 1.14.1 Music therapy studies | 5 | 105 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.47 [‐0.86, ‐0.07] |
| 1.14.2 Music medicine studies | 7 | 527 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.81 [‐1.38, ‐0.24] |
| 1.15 Pain (music preference) | 8 | 567 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.84 [‐1.34, ‐0.33] |
| 1.15.1 Patient‐preferred music | 5 | 348 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.87 [‐1.65, ‐0.10] |
| 1.15.2 Researcher‐selected music | 3 | 219 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.74 [‐1.33, ‐0.14] |
| 1.16 Fatigue | 10 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.16.1 All studies | 10 | 498 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.28 [‐0.46, ‐0.10] |
| 1.16.2 Sensitivity analysis (randomization method) | 9 | 448 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.26 [‐0.45, ‐0.07] |
| 1.16.3 Sensitivity analysis (< 10% non‐cancer studies excluded) | 9 | 463 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.26 [‐0.44, ‐0.07] |
| 1.17 Fatigue (intervention subgroup) | 9 | 449 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.27 [‐0.46, ‐0.08] |
| 1.17.1 Music therapy studies | 6 | 256 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.36 [‐0.61, ‐0.12] |
| 1.17.2 Music medicine studies | 3 | 193 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.15 [‐0.43, 0.14] |
| 1.18 Physical functioning | 4 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.18.1 All studies | 4 | 493 | Std. Mean Difference (IV, Random, 95% CI) | 0.78 [‐0.74, 2.31] |
| 1.18.2 Sensitivity analysis (randomization method) | 3 | 233 | Std. Mean Difference (IV, Random, 95% CI) | 0.08 [‐0.18, 0.34] |
| 1.19 Heart rate | 11 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.19.1 All studies | 11 | 1022 | Mean Difference (IV, Random, 95% CI) | ‐3.40 [‐5.58, ‐1.23] |
| 1.19.2 Sensitivity analysis (randomization method) | 9 | 772 | Mean Difference (IV, Random, 95% CI) | ‐4.37 [‐6.29, ‐2.44] |
| 1.20 Heart rate (music preference) | 10 | 972 | Mean Difference (IV, Random, 95% CI) | ‐3.65 [‐5.94, ‐1.35] |
| 1.20.1 Patient‐preferred music | 7 | 807 | Mean Difference (IV, Random, 95% CI) | ‐3.34 [‐6.06, ‐0.62] |
| 1.20.2 Researcher‐selected music | 3 | 165 | Mean Difference (IV, Random, 95% CI) | ‐4.47 [‐8.02, ‐0.91] |
| 1.21 Respiratory rate | 5 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.21.1 All studies | 5 | 737 | Mean Difference (IV, Random, 95% CI) | ‐0.71 [‐1.18, ‐0.23] |
| 1.21.2 Sensitivity analysis (randomization method) | 4 | 537 | Mean Difference (IV, Random, 95% CI) | ‐1.18 [‐2.46, 0.11] |
| 1.22 Systolic blood pressure | 10 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.22.1 All studies | 10 | 992 | Mean Difference (IV, Random, 95% CI) | ‐4.18 [‐6.70, ‐1.66] |
| 1.22.2 Sensitivity analysis (randomization method) | 8 | 742 | Mean Difference (IV, Random, 95% CI) | ‐4.50 [‐8.36, ‐0.64] |
| 1.23 Systolic blood pressure (music preference) | 9 | 942 | Mean Difference (IV, Random, 95% CI) | ‐4.76 [‐7.25, ‐2.26] |
| 1.23.1 Patient‐preferred music | 6 | 777 | Mean Difference (IV, Random, 95% CI) | ‐4.82 [‐7.90, ‐1.75] |
| 1.23.2 Researcher‐selected music | 3 | 165 | Mean Difference (IV, Random, 95% CI) | ‐4.71 [‐12.04, 2.63] |
| 1.24 Diastolic blood pressure | 10 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.24.1 All studies | 10 | 992 | Mean Difference (IV, Random, 95% CI) | ‐2.34 [‐4.70, 0.01] |
| 1.24.2 Sensitivity analysis (randomization method) | 8 | 742 | Mean Difference (IV, Random, 95% CI) | ‐3.86 [‐6.01, ‐1.71] |
| 1.25 Diastolic blood pressure (music preference) | 9 | 942 | Mean Difference (IV, Random, 95% CI) | ‐3.21 [‐5.63, ‐0.80] |
| 1.25.1 Patient‐preferred music | 6 | 777 | Mean Difference (IV, Random, 95% CI) | ‐3.36 [‐6.46, ‐0.27] |
| 1.25.2 Researcher‐selected music | 3 | 165 | Mean Difference (IV, Random, 95% CI) | ‐2.51 [‐5.03, 0.02] |
| 1.26 Oxygen saturation | 2 | 252 | Mean Difference (IV, Random, 95% CI) | 0.59 [‐0.62, 1.80] |
| 1.27 Quality of life | 7 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.27.1 All studies | 7 | 573 | Std. Mean Difference (IV, Random, 95% CI) | 0.88 [‐0.31, 2.08] |
| 1.27.2 Sensitivity analysis (randomization method) | 5 | 269 | Std. Mean Difference (IV, Random, 95% CI) | 0.47 [0.06, 0.88] |
| 1.28 Quality of life (intervention subgroup) | 7 | 573 | Std. Mean Difference (IV, Random, 95% CI) | 0.88 [‐0.31, 2.08] |
| 1.28.1 Music therapy studies | 4 | 160 | Std. Mean Difference (IV, Random, 95% CI) | 0.40 [0.08, 0.71] |
| 1.28.2 Music medicine studies | 3 | 413 | Std. Mean Difference (IV, Random, 95% CI) | 1.32 [‐1.02, 3.67] |
1.9. Analysis.

Comparison 1: Music intervention plus standard care versus standard care alone in adults, Outcome 9: Distress
1.15. Analysis.

Comparison 1: Music intervention plus standard care versus standard care alone in adults, Outcome 15: Pain (music preference)
Comparison 2. Music interventions plus standard care versus standard care alone in children.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Anxiety (STAI) | 2 | 79 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.94 [‐1.90, 0.03] |
Comparison 3. Music interventions plus standard care versus standard care plus placebo control in children.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 Distress | 2 | Mean Difference (IV, Random, 95% CI) | ‐0.07 [‐0.39, 0.26] | |
| 3.2 Spiritual well‐being | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.31 [‐0.11, 0.73] |
Comparison 4. Music therapy plus standard care versus music medicine plus standard care in adults.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 4.1 Anxiety | 2 | 194 | Mean Difference (IV, Fixed, 95% CI) | ‐3.55 [‐7.13, 0.02] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Alam 2016.
| Study characteristics | ||
| Methods | Randomized controlled trial (RCT) 3‐arm parallel‐group design |
|
| Participants | Adults pending staged excisional surgery Type of cancer: basal or cutaneous squamous cell carcinoma of the face Total N randomized: 155 Total N analyzed: 155 N randomized to music group: 54 N randomized to guided imagery group: 50 (not included in this review) N randomized to control group: 51 N analyzed in music group: 54 N analyzed in guided imagery group: 50 (not included in this review) N analyzed in control group: 51 Mean age: 63.1 years Sex: 65 (42%) females, 90 (58%) males Ethnicity: not reported Setting: procedural/surgical Country: USA |
|
| Interventions | 2 study groups: 1. Music group: listening to pre‐recorded music through headphones during surgery 2. Control group: standard care. Participants wore headphones with no music or sound. Music selections provided: Soothing music and nature sounds such as falling water and chirping bird, 60‐70 bpm Number of sessions: 1 Length of sessions: for duration of the surgery Categorized as music medicine |
|
| Outcomes | Pain (0‐10 NRS): change score Anxiety (STAI ‐ 6‐item short form): change score Systolic blood pressure (SBP): change score Diastolic blood pressure (DBP): change score Heart rate (HR): change score |
|
| Notes | Only SEM were reported. SD for the change scores were computed by JB. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "This was a randomized controlled study with an allocation ratio of 1:1:1, using a random block size of 9" (p. 586) |
| Allocation concealment (selection bias) | Low risk | "The randomization allocation sequence was generated by a separate investigator (S. Y.) from those who enrolled subjects and assigned participants to their groups (N. A. K., M. P.)" (p. 587). "Assignments were sealed in opaque envelopes and numbered consecutively" (p. 586). |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | "During the period when subjects were undergoing surgery (e.g. surgical preparation, injection of local anesthesia, excision procedure, repair procedure, and application of bandage), subjects wore earphones attached to a playback device. Playback was looped to be continuous, and was either of guided imagery or standardized relaxing music, as per randomization. In the control group, participants wore earphones without any sound" (p. 587). |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | "Those applying and removing the earphones with the appropriate recording intraoperatively (N. A. K., J. H. S.) were different from those recording blood pressures, pain scores, and responses to subject and surgeon questionnaires (M. P., N. A. K., R. T. B.). The surgeon was blinded as to subject assignment" (p. 587). |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. Even though participants in the control condition wore headphones as well to blind study personnel, participants knew whether or not they were listening to music. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No report of conflict of interest |
Alcantara‐Silva 2018.
| Study characteristics | ||
| Methods | RCT 2‐arm parallel‐group design |
|
| Participants | Adults attending outpatient radiotherapy Type of cancer: breast (n = 90, 77%), gynaecological (n = 27, 23%) Total N randomized: 164 Total N analyzed: 106 analyzed pre‐ and post; 94 analyzed midpoint N randomized to music group: 82 N randomized to control group: 82 N analyzed in music group: 53 analyzed pre‐ and post; 47 analyzed midpoint N analyzed in control group: 53 analyzed pre‐ and post; 47 analyzed midpoint Mean age: 52.37 years Sex: 164 (100%) females, (0%) males Ethnicity: Caucasian 42 (39.3%), African 9 (8.4%), Asian 8 (7.5%), Indian 1 (0.9%), Mulatto 47( 43.9%) Setting: outpatient Country: Brazil |
|
| Interventions | 2 study groups: 1. Music group: conducted according to the following protocol: (1) welcoming the participant (5 minutes); (2) first listening (5 minutes); (3) second listening (5 minutes); (4) processing participant's feelings (5 to 15 minutes); (5) third listening (5 minutes); and (6) session closure (5 minutes). 2. Control group: standard care Music selections provided: The selection of songs for the first and third listening was performed by the music therapist based on her own repertoire of the baroque, classical, and romantic periods. For the first listening, 12 instrumental songs with a slow tempo, a tone, and regular pulse were chosen. These features generate a consonant melody, leading to more pleasure during listening because of the activation of the cortical region of the brain, related to pleasurable responses to consonant musical stimuli. Number of sessions: 10 on average, offered twice per week Length of sessions: 30‐40 min Categorized as music therapy |
|
| Outcomes | Quality of life (QoL), fatigue and physical functioning: only post‐test scores and P values were reported. No standard deviations or standard errors were reported. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "To carry out the randomization, 164 sealed envelopes containing the names of the groups (control group [CG] and music therapy group [MTG]) in identical proportions were used" (p. 629). |
| Allocation concealment (selection bias) | Low risk | "To carry out the randomization, 164 sealed envelopes containing the names of the groups (control group [CG] and music therapy group [MTG]) in identical proportions were used" (p. 629). |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The music therapist and the participants could not be blinded. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | No objective outcomes were included in this study. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Loss of subjects of 19 in control group (23%) and 29 (35%) in music therapy group. Higher attrition in music therapy group was due to fact that participants who did not complete 75% of sessions were excluded. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | The author(s) received no financial support for the research, authorship, and/or publication of this article. |
Arruda 2016.
| Study characteristics | ||
| Methods | RCT 3‐arm parallel‐group design |
|
| Participants | Adult oncology Type of cancer: genitourinary (n = 26, 40%), gastrointestinal (n = 14, 21%), breast (n = 6, 9%), hematological (n = 3, 5%), other (n = 16, 25%) Total N randomized: 75 Total N randomized: 65 N randomized to music group: 25 N randomized to poetry group: 25 (not analyzed in this review) N randomized to control group: 25 N analyzed in music group: 22 N analyzed in poetry group: 22 (not analyzed in this review) N analyzed in control group: 21 Mean age: not reported Sex: 47 (72%) females, 18 (28%) males Ethnicity: not reported Setting: inpatient Country: Brazil |
|
| Interventions | 3 study groups: 1. Music group: music listening 2. Experimental group 2: poetry (not analysed in this review) 3. Control group: standard care Music selections provided: a series of 30‐minute instrumental songs by the artists Yasunori Mitsuda and Vic Mignona, which were used in the video game Chrono Cross and the Japanese animation Fullmetal Alchemist. The choice of musical repertoire took into consideration the following aspects: instrumental quality, rhythm regularity, and constant intensity. Number of sessions: 3 Length of sessions: 30 min Categorized as music medicine |
|
| Outcomes | Pain (Visual Analogue Scale (VAS)): post‐test scores Depression (Beck Depression Inventory (BDI)): post‐test scores Hope (Herth Hope Scale): post‐test scores |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Preselection of patients was made by a random selection of their records. A numeric selection was then conducted for choice of beds to be evaluated across eligible subjects, and another selection was conducted for allocation into the three groups using simple randomization" (p. 944). |
| Allocation concealment (selection bias) | Unclear risk | No allocation concealment information was provided. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | "Awareness of patients as to what they were hearing prevented blinding" (p. 945). |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | No objective outcomes were included in this study. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition rate: 19.7%. Attrition rate was greater in the control group. However, because the participant flow chart referenced in the publication was actually not included in the publication, the exact attrition per treatment arm and reasons for attrition could not be identified. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | "No competing financial interests exist" (p. 947). |
Bates 2017.
| Study characteristics | ||
| Methods | RCT 2‐arm parallel‐group design |
|
| Participants | Adults undergoing first autologous stem cell transplant (ASCT) Type of cancer: multiple myeloma (n = 40, 49%), non‐Hodgkin lymphoma (n = 34, 41%), Hodgkin lymphoma (n = 8, 10%) Total N randomized: 108 Total N randomized: 82 N randomized to music group: 55 N randomized to control group: 53 N analyzed in music group: 45 N analyzed in control group: 37 Mean age: 58 years Sex: 37 (45%) females, 45 (55%) males Ethnicity: Caucasian 75 (91%), African‐American 7 (9%) Setting: inpatient Country: USA |
|
| Interventions | 2 study groups: 1. Music therapy group: The initial session included a brief assessment of the participant’s concerns, including symptoms to help identify music therapy session goals, music background and preferences, and possible music therapy intervention options. When songs were chosen, these were primarily presented live, sung by the music therapist, who used a keyboard or acoustic guitar for accompaniment, with the participant engaging in the music experience to the extent to which he or she was able. Receptive (e.g. music listening, song choices, music and imagery, music‐assisted relaxation) and recreative (e.g. singing, instrument playing) music therapy methods were used most frequently. Music‐assisted relaxation also incorporated live music, with the music therapist simultaneously providing verbal prompts. 2. Control group: standard care Music selections provided: not reported Number of sessions: 2 Length of sessions: 30 min Categorized as music therapy |
|
| Outcomes | Pain (10 cm VAS): only P value reported Nausea (10 cm VAS): no means per data point reported Mood disturbance (Profile of Mood States (POMS)): total mood disturbance score not reported Depression (POMS): post‐test scores Fatigue (POMS): post‐test scores; changes scores computed by JB Narcotic pain medication use (morphine equivalent dose): only P value reported |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Consented patients underwent computer‐generated randomization and were assigned to either the experimental arm (music therapy with standard supportive care) or the standard care arm (standard supportive care). Randomization was stratified according to disease (lymphoma, myeloma) and used random block sizes. The randomization list was generated before the study began and was kept in a secured location accessible only to the protocol coordinator" (p. 1568). |
| Allocation concealment (selection bias) | Low risk | Allocation concealment was used (personal communication with author). |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The music therapist and the participants could not be blinded. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | No objective measures included |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition rate: n = 26 (24%) |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | "This research was supported by the listed affiliated institution and a grant from the Prentiss Foundation. No products were used or created as result of this research study, and there was no financial support from any commercial companies. No financial relationships or interests exist or were created as a result of this study" (p. 1572). |
Beck 1989.
| Study characteristics | ||
| Methods | RCT Cross‐over trial |
|
| Participants | Adults with documented cancer‐related pain Type of cancer: breast (n = 7, 46.5%), multiple myeloma (n = 4, 26.5%), rectal (n = 1, 6.75%), prostate (n = 1, 6.75%), sarcoma (n = 1, 6.75%), lymphoma (n = 1, 6.75%) Total N randomized: 15 Total N analyzed: 15 Mean age: 55.6 years Sex: 12 (80%) females, 3 (20%) males Ethnicity: 15 (100%) white Setting: participants' home Country: USA |
|
| Interventions | 2 study groups
Music provided: the researcher asked a registered music therapist to select relaxing music in 7 categories including classical, jazz, folk, rock, country and western, easy listening and new age. Participants were asked to select from these music options. Number of sessions: 3 Length of sessions: 45 min Categorized as music medicine trial |
|
| Outcomes | Mood (VAS), pain (VAS): change scores | |
| Notes | Because of significant pre‐test differences, JB used data provided in Beck's dissertation to compute change scores. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Using a coin flip for a random start, assignment was alternated between the 2 groups which differed on the order of the intervention". |
| Allocation concealment (selection bias) | Low risk | Cross‐over trial; all participants received both conditions. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | It was unclear whether personnel were blinded. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | The study did not address objective outcomes. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 6 dropouts (28.6%) because of hospitalisation (n = 1), deterioration (n = 2), inadequate baseline (n = 2), or withdrawal during baseline (n = 1) |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No conflict of interest reported |
Bieligmeyer 2018.
| Study characteristics | ||
| Methods | RCT Cross‐over design |
|
| Participants | Adult inpatients Type of cancer: breast (n = 12, 27.3%), colorectal (n = 6, 13.6%), bronchial (n = 4, 9.1%), lymphoma (n = 4, 9.2%), other (n = 18, 40.3%) Total N randomized: 44 Total N analyzed: 44 Mean age: 54.35 years Sex: 31 (70.5%) females, 13 (29.5%) males Ethnicity: not reported Setting: inpatient Country: Germany |
|
| Interventions | 2 study conditions: 1. Music therapy condition: vibro‐acoustic therapy 2. Control condition: standard care Music selections provided: The 48 strings of the sound‐bed were tuned in a TAO tuning as a precursor of pentatonics (tones D, E, A, B) over four octaves. Number of sessions: 1 Length of sessions: 10 min Categorized as music therapy |
|
| Outcomes | Mood (Berlin Mood Questionnaire (BMQ)): post‐test scores Pain (VAS): post‐test scores Quality of Life (European Organization Research & Treatment of Cancer QOL Questionnaire (EORT‐QLQ)): insufficient data |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Using opaque envelopes for the randomization procedure, participants were randomly assigned to either music intervention followed by control intervention or control intervention followed by music intervention. For every block of four participants, two envelopes were allocated to each arm of the trial to ensure groups of approximately the same size. Block size was unknown to the participants so that the schedule was not predictable. The participants opened the envelopes immediately before the first intervention so that at this moment the author was informed about the actual sequence for the respective participant. Randomization was carried out by the author" (p. 172). |
| Allocation concealment (selection bias) | Low risk | "Using opaque envelopes for the randomization procedure, participants were randomly assigned to either music intervention followed by control intervention or control intervention followed by music intervention" (p. 172). |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants and MT could not be blinded in active music interventions. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | No objective outcomes were included in this study. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rate: N = 2 (4%) |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | The study was financed by the ARCIM Institute. The authors indicated no potential conflicts of interest. |
Binns‐Turner 2008.
| Study characteristics | ||
| Methods | RCT 2‐arm parallel‐group design |
|
| Participants | Women undergoing mastectomy Type of cancer: breast cancer Total N randomized: 30 N randomized to music group: 15 N randomized to control group: 15 N analyzed in music group: 15 N analyzed in control group: 15 Mean age: 56.63 years Sex: 30 (100%) females, 0 (0%) males Ethnicity: 24 (80%) white, 6 (20%) black Setting: inpatient Country: USA |
|
| Interventions | 2 study groups
(Note: iPod case concealed the function status of the iPod to ensure blinding of medical personnel) Music selections provided: 4 h of continuous non‐repeating music in genre selected by the participant from the following genres: classical, easy listening, inspirational or new age Number of sessions: 1 Length of sessions: duration of mastectomy (music was begun after the participant received midazolam preoperatively) Categorized as music medicine |
|
| Outcomes | Anxiety (Spielberger State‐Trait Anxiety Inventory ‐ State Anxiety form, STAI‐S), pain (VAS): post‐test scores Heart rate (HR), mean arterial pressure (MAP): change scores |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "[T]he participants were assigned by the investigator to experimental or control groups by selecting numbers from an envelope which contained papers numbered 1 to 30 (odd numbers were assigned to the experimental group and even numbers to the control group)" (p. 53). |
| Allocation concealment (selection bias) | Low risk | Not reported. We assumed that the participants were present when the lot was drawn therefore assuring allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Personnel were blinded. Quote: "The iPOD was placed in a carrying case which concealed the function of the player; participants were not blinded." We decided to assign 'unclear risk' because it was unlikely that the participants' knowledge of group allocation influenced their physiological responses (objective outcome measures). However, this knowledge may have influenced their reporting on subjective outcomes. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | Outcome assessors were blinded for HR and MAP (iPod function was concealed from medical personnel who obtained the HR and MAP data). |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No report of conflict of interest |
Bradt 2015.
| Study characteristics | ||
| Methods | RCT Cross‐over design |
|
| Participants | Adults receiving cancer treatment Type of cancer: breast (n = 6, 19.4%), head and neck (n = 3, 9.7%), gastrointestinal (n = 3, 9.7%), gynaecological (n = 3, 9.7%), hematologic (n = 7, 22.6%), lung (n = 4, 12.9%), other (n = 5, 16%) Total N randomized: 39 with 5 participants lost prior to initiation of treatment Total N analyzed: 31 Age: 53.8 years Sex: 21 (67.7%) females, 10 (32.3%) males Ethnicity: 23 (74.2%) black, 1 (3.2%) Asian, 6 (19.4%) white, 1 (3.2%) other Setting: inpatient and outpatient Country: USA |
|
| Interventions | 2 study conditions:
Number of sessions: 2 of each condition Length of sessions: 30‐45 min Categorized as music therapy |
|
| Outcomes | Anxiety (VAS), mood (VAS), relaxation (VAS), pain (NRS): post‐test scores | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Using a list of random numbers, participants were randomized to one of two treatment sequences consisting of two MT sessions followed by two MM sessions or vice versa" (p. 1262). |
| Allocation concealment (selection bias) | Low risk | "The use of sequentially numbered, opaque, sealed envelopes ensured allocation concealment" (p. 1262). |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Study participants were blinded: "We minimized expectation effects of participants throughout the study by referring to both treatment conditions as music sessions rather than referring to one intervention as music therapy" (p. 1263). The music therapist could not be blinded. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | No objective outcomes were included in this study. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | Low risk | Self‐report measures were used for subjective outcomes but participants were blinded to the study hypotheses. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rate: 13% (p. 1264) |
| Selective reporting (reporting bias) | Low risk | No indication of selective reporting |
| Other bias | Low risk | Study was funded by Drexel University's College of Medicine. |
Bro 2019.
| Study characteristics | ||
| Methods | RCT 3‐arm parallel‐group design |
|
| Participants | Adults undergoing chemotherapy Type of cancer: Hodgkin (n = 42, 29%), non‐Hodgkin (n = 101, 71%) Total N randomized: 143 Total N analyzed: 125 N randomized to live music group: 47 N randomized to recorded music group: 47 (not included in this review) N randomized to control group: 49 N analyzed in live music group: 44 N analyzed in recorded music group: 40 N analyzed in control group: 41 Mean age: 60 years Sex: 63 (44%) females, 80 (56%) males Ethnicity: not reported Setting: outpatient Country: Denmark |
|
| Interventions | 2 study groups: 1. Music group: listening to live music 2. Control group: standard care Music selections provided: Based on the participant's oral and written feedback on musical preference, musical background, wishes for specific music pieces/genres, and constellation of musicians, the PI chose musicians for the first treatment. Subsequently, one to three musician(s) planned a suitable repertoire, and the sound level was considered. Number of sessions: Numbers of planned treatments varied across participants; the musicians played music starting in the second and up to the third to sixth chemotherapy sessions. Length of sessions: 25‐30 min Categorized as music medicine |
|
| Outcomes | Anxiety (STAI): post‐test (after 6 sessions) Quality of Life (EORTC‐QLQ‐30): effect size |
|
| Notes | The published article only included effect sizes and did not include any means or standard deviations for the outcomes. However, the dissertation included a table for means and SDs per time point for STAI. Therefore, only the STAI data were included in the meta‐analysis. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Randomization was made by calling an independent research unit, who had a computer‐generated randomization list" (p. 3888). |
| Allocation concealment (selection bias) | Low risk | "Randomization was made by calling an independent research unit, who had a computer‐generated randomization list" (p. 3888). |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants and personnel could not be blinded due to live music intervention. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Unclear risk | Unclear whether the research nurse was blinded prior to measuring objective outcomes |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition: n = 18 (12.6%) |
| Selective reporting (reporting bias) | Low risk | Outcomes reported in the dissertation and the published article were the same. |
| Other bias | Low risk | "The authors have no financial relationships to disclose" and "Funding: The Hospital of Southwest Jutland, The Danish National Academy of Music, Region of Southern Denmark, The Danish Cancer Society Research Center, The Danish National Research Foundation (DNRF 117), Familien Hede Nielsens Fond, Karola Joergensens Forskningsfond, Roche.dk, HiFi‐Klubben, Juhl‐Soerensen A/S, Sønderjyllands Symphony Orchestra, Aarhus Symphony Orchestra, and Copenhagen Phil supported this study". |
Bufalini 2009.
| Study characteristics | ||
| Methods | Controlled clinical trial (CCT) (randomisation method unclear) 2‐arm parallel‐group design |
|
| Participants | Children with cancer who had previously undergone more than 2 painful, invasive procedures (e.g. osteomedullar biopsy, lumbar puncture) and who were scheduled to undergo a painful medical procedure Type of cancer: acute lympathic leukemia (n = 18, 47% of music group, n = 25, 65% of control group), non‐Hodgkin's lymphoma (n = 12, 32% of music group, n = 8, 20% of control group), neuroblastoma (n = 4, 11% of music group, n = 4, 10% of control group), osteosarcoma (n = 2, 5% of music group, n = 2, 5% of control group), medulloblastoma (n = 2, 5% of music group, 0% of control group) Total N randomized: unclear N analyzed in music group: 20 N analyzed in control group: 19 Mean age: 6.72 years Sex: 15 (38%) females, 24 (72%) males Ethnicity: 39 (100%) white (Italian) Setting: inpatient Country: Italy |
|
| Interventions | 2 study groups:
Music selections provided: during the initial music listening phase, the following music was used: lullabies (e.g. Brahms); children's songs (Walt Disney); folk songs (Italian/non‐Italian), ethnic songs (Albania, Romania, Latin America), pop (Italian/non‐Italian), classical music (e.g. Bach), other music (Celtic music, Simon and Garfunkel, etc.). This phase was followed by active music‐making with the child using small percussion instruments and vocal and body percussion. Number of sessions: 1 Length of sessions: 15 min for phase 1 (music listening); length of active music making was not specified. Categorized as music therapy |
|
| Outcomes | Anxiety (STAI‐S): post‐test scores Induction compliance (not used in this review) |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Music therapist and participants could not be blinded as this trial used an interactive music therapy intervention. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | The study did not address objective outcomes. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | It was unclear whether the number of participants analyzed equalled the number of participants recruited. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No conflict of interest reported |
Bulfone 2009.
| Study characteristics | ||
| Methods | CCT 2‐arm parallel‐group design |
|
| Participants | Women with breast cancer waiting for adjuvant chemotherapy Type of cancer: breast (n = 60, 100%) Total N randomized: 60 N randomized to music group: 30 N randomized to control group: 30 N analyzed in music group: 30 N analyzed in control group: 30 Mean age: 50.95 years Sex: 60 (100%) females Ethnicity: 60 (100%) white (Italian) Setting: inpatient Country: Italy |
|
| Interventions | 2 study groups:
Music selections provided: participants were asked to select from new age music, nature music, film soundtracks, Celtic melodies, or classical music. Number of sessions: 1 Length of sessions: 15 min Categorized as music medicine |
|
| Outcomes | Anxiety (STAI‐S): post‐test scores | |
| Notes | The principal investigator provided us with standard deviations as these were not given in the study report. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Alternate assignment using order of admission (personal communication with principal investigator) |
| Allocation concealment (selection bias) | High risk | Alternate assignment prohibited allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | It was unclear whether personnel were blinded; participants were not blinded. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | The study did not address objective outcomes. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No attrition |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No conflict of interest reported |
Burns 2001a.
| Study characteristics | ||
| Methods | RCT 2‐arm parallel‐group design |
|
| Participants | Adult patients with cancer Diagnosis: ovarian (n = 1, 13%), breast (n = 7, 87%) Total N randomized: 8 N randomized to music group: 4 N randomized to control group: 4 N analyzed in music group: 4 N analyzed in control group: 4 Mean age: 48 (SD 6.56) years Sex: 8 (100%) females Ethnicity: no information provided Setting: outpatient Country: USA |
|
| Interventions | 2 study groups:
Music selections provided: Quote from study report (p. 55): "The Bonny Method of Guided Imagery and Music is an in depth music psychotherapy that utilizes specially sequenced Western Art music to elicit imagery and emotional expression." Number of sessions: 10 Length of sessions: 90‐120 min Categorized as music therapy |
|
| Outcomes | Mood (POMS): could not be included because constant of 100 was not used in total score computation by the authors. Quality of Life (QoL‐Cancer Scale): change scores were computed by JB to allow for computation of pooled effect size (SMD) with other studies that reported change scores. |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated number list (personal communication with principal investigator) |
| Allocation concealment (selection bias) | Low risk | Statistical program Aleator (personal communication with principal investigator) |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding of participants and music therapist was not possible given the interactive nature of the music therapy sessions. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | The study did not address objective outcomes. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No subject loss |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | Study was supported by Trustees of the Paul Jenkins fund. |
Burns 2008.
| Study characteristics | ||
| Methods | CCT 2‐arm parallel‐group design |
|
| Participants | Adults with acute leukemia Diagnosis: acute leukemia, high‐grade non‐Hodgkin's lymphoma Total N randomized: 49 N randomized to music group: 25 N randomized to control group: 24 N analyzed in music group: 15 N analyzed in control group: 15 Mean age: 54 years Sex: 30 (61%) females, 19 (39%) males Ethnicity: not provided Setting: inpatient Country: USA |
|
| Interventions | 2 study groups:
Music selections provided: classical music and new age music based on participant preference was used. Number of sessions: 8 Length of sessions: 45 min Categorized as music therapy |
|
| Outcomes | Anxiety (STAI‐S): 4‐week post‐intervention scores Fatigue (the Functional Assessment of Chronic Illness Therapy—Fatigue scale, FACIT‐F): 4‐week post‐intervention scores Positive and negative affect (Affect and Negative Affect Schedule, PANAS): 4‐week post‐intervention scores (not used in this review) |
|
| Notes | Post‐test scores were not reported in this study report. Values were obtained from the principal investigator. However, she could only provide us with the 4‐week post‐intervention scores. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding of participants and music therapist was not possible given the interactive nature of the music therapy sessions. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | This study did not address objective outcomes. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition rate was 38.8%. There were 10 withdrawals in the experimental group, 9 in the control group for the following reasons: too sick to complete the measures or carry out the intervention (n = 6), voluntary withdrawal (n = 4), transfer to ICU (n = 4), death (n = 3), did not complete follow‐up questionnaires (n = 2) |
| Selective reporting (reporting bias) | High risk | Only feasibility data were reported. No post‐test or follow‐up scores were reported. Follow‐up scores (4‐weeks post‐intervention) were received from the author. |
| Other bias | Low risk | Supported by a grant from the National Center for Complementary and Alternative Medicine 5F32AT001144‐02, and Bardett‐Kenkel award from the Walter Cancer Institute |
Burns 2009.
| Study characteristics | ||
| Methods | RCT 2‐arm parallel‐group design |
|
| Participants | Adolescents and young adults with cancer during stem‐cell transplantation (SCT) Diagnosis: no further diagnosis details reported Total N randomized: 12 N randomized to music group: 7 N randomized to control group: 5 N analyzed in music group: 7 N analyzed in control group: 2 Mean age: 17.5 years Sex: 5 (42%) females, 7 (58%) males (at the onset of the trial) Ethnicity: 8 (66%) white, other information not provided Setting: inpatient Country: USA |
|
| Interventions | 2 study groups:
Music selections provided: music videos of 10 songs from 5 music styles including pop, rock, rap, country, and rhythm and blues Number of sessions: 6 Length of sessions: 60 min Categorized as music therapy |
|
| Outcomes | Distress (McCorkle Symptom Distress Scale): post‐test scores QoL (Index of Well‐Being): post‐test scores Spiritual beliefs (Reed Spiritual Perspective Scale): change scores Hope (Herth Hope index): not included in this review Mood (Mental Health Scale of the Child Health Questionnaire), pain (Child Health Questionnaire): could not be included because of high attrition. |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated number list (personal communication with principal investigator) |
| Allocation concealment (selection bias) | Unclear risk | Central randomization was used, but author was unsure how information was transferred to field investigators (personal communication with principal investigator). |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Music therapist could not be blinded because of the interactive nature of the music therapy sessions; participants were blinded to the purpose of the study (personal communication with principal investigator). |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | This study did not address objective outcomes. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 2 participants (16.6%) were dropped from the study when they became very ill and were transferred to the intensive care unit; 1 of these 2 participants eventually died. 1 participant withdrew from the study after learning randomization status. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | Supported by American Cancer Society IRG‐84‐002‐19 |
Burns 2018.
| Study characteristics | ||
| Methods | RCT 2‐arm parallel‐group design |
|
| Participants | Adults undergoing chemotherapy infusion Type of cancer: breast/gynecological (n = 33, 43.4%), hematologic (n = 12, 15.8%), lung (n = 8, 10.5%), genitourinary (n = 5, 6.6%), gastrointestinal (n = 6, 7.9%), and missing data (n = 12, 15.8%) Total N randomized: 86 Total N analyzed: 76 N randomized to music and imagery group: 43 N randomized to music listening group: 43 N analyzed in music and imagery group: 40 N analyzed in music listening group: 36 Mean age: 47.45 years Sex: 48 (63.2%) females, 28 (36.8%) males Ethnicity: 57 (75%) white, 16 (21%) black or African‐American, 3 (4%) other Setting: outpatient Country: USA |
|
| Interventions | 2 study groups: 1. Music and imagery group: delivered by board‐certified music therapist according to the following protocol: 1) discussion of issues (5‐10 min) to develop a session focus; 2) transition (1‐2 min) to relaxed seating position; 3) music and imagery (30‐35 min): a guided visualization, accompanied by recorded music, in which the music therapist helped the participant focus on one or more of the following: a) relaxing the body, b) changing breathing rhythm and depth, c) visualization, and d) connecting with the participant's spiritual or religious world. Visualizations could take a number of forms such as: a) images related to one's breathing, b) images of nature, c) supportive, nurturing images, d) images related to the effects of the chemotherapy on the participant's body, and e) positive images of personal importance to the participant; 4) review of the experience (5 min). 2. Music listening group: participants listened to preferred music genre as facilitated by a board‐certified music therapist following this format: 1) discussion of music preferences (5‐10 min); 2) participant selection of playlist based on preferred genre (1‐2 min); 3) preferred music listening (30‐35 min); 4) review of experiences (5 min). Music selections provided for music and imagery group: consisted of Western Art Music and new age genres and was selected by the music therapist from a list based on assessment of participant's need for structure and energy level. Music selections provided for music listening group: Music playlists were compiled by a research assistant by examining the Billboard charts for popular recordings and including the genres: country, new age, 2000s, Christian, jazz, 60s/70s, 80s/90s, classical (Western art music), Broadway, and spiritual. Number of sessions: 1 Length of sessions: 45‐50 min, during chemotherapy Categorized as music therapy |
|
| Outcomes | Depression (Hospital Anxiety and Depression Scale (HADS): Mean, SE, and effect size Anxiety (HADS): Mean, SE, and effect size Locus of control (Multidimensional Health Locus of Control): Mean, SE, and effect size Coherence (Sense of Coherence Scale): Mean, SE, and effect size Distress (Impact of Events Scale (IES)): Mean, SE, and effect size Benefits finding ‐ Benefit Finding Scale: Mean, SE, and effect size |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Participants received their group assignment after pretest data collection, based on a simple 1:1 randomization scheme calculated by the Statistical Package for Social Sciences (SPSS v.10). A randomization scheme was created for each site" (p. 88). |
| Allocation concealment (selection bias) | Low risk | "Participants received their group assignment after pretest data collection, based on a simple 1:1 randomization scheme calculated by the Statistical Package for Social Sciences (SPSS v.10). A randomization scheme was created for each site. The site Principal Investigator (PI) provided the site music therapist the participant’s group assignment after pretest measures were collected" (p. 88). |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants were blinded to study hypothesis but music therapists could not be blinded. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | No objective outcomes included |
| Blinding of outcome assessment (detection bias) Subjective outcomes | Low risk | Participants were blinded to study hypothesis therefore self‐report measure outcome assessment could be rated as low risk. Moreover, the research assistants who collected the self‐report measures were blinded to group allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition rate: 9%. However, 3 people in the music listening and 6 people in the music imagery treatment arm withdrew. Reasons for withdrawal were unclear. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective outcome reporting |
| Other bias | Low risk | This research was supported in part by the Arthur Flagler Fultz Research Fund awarded to Burns and Meadows (co‐PIs). |
Burrai 2014.
| Study characteristics | ||
| Methods | RCT 2‐arm parallel‐group design |
|
| Participants | Adults with cancer receiving chemotherapy treatment Type of cancer: metastatic cancer (n = 45, 86.6%), non‐metastatic cancer (n = 7, 13.4%) Total N randomized: 52 Total N analyzed: 52 N randomized to music group: 26 N randomized to control group: 26 N analyzed in music group: 26 N analyzed in control group: 26 Mean age: 64.5 years Sex: 43 (82.7%) females, 9 (17.3%) males Ethnicity: not reported Setting: inpatient Country: Italy |
|
| Interventions | 2 study groups:
Music selections provided: participant was asked to select 5 or 6 musical pieces from a playlist that included music from a wide variety of styles Number of sessions: 3 Length of sessions: 30 min Categorized as music medicine |
|
| Outcomes | SBP, DBP: change score HR, oxygen saturation: post‐test scores Mood (VAS): post‐test scores Glycemia: not included in this review Pain (VAS): not included in this review. Baseline levels indicated that participants were barely experiencing pain. |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "For the randomisation sequence generation for allocation of the participants, a computer‐generated list of random numbers was used. For the randomisation type, participants were randomly assigned following simple randomisation procedures (computerized random numbers) to 1 of 2 groups" (p. 304). |
| Allocation concealment (selection bias) | Low risk | "As for the allocation concealment mechanism, the allocation sequence was concealed from the researcher enrolling and assessing participants in sequentially numbered, opaque, sealed, and stapled envelopes. Envelopes were opened only after the enrolled participants completed all baseline assessments, and it was time to allocate the intervention" (p. 304). |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Live music was used; therefore blinding was not possible. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Flow chart (p. 305) indicated 0% dropouts. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | "The authors have disclosed that they have no significant relationships with, or financial interest in, any commercial companies pertaining to this article" (p. 301). |
Cai 2001.
| Study characteristics | ||
| Methods | CCT 2‐arm parallel‐group design |
|
| Participants | Adults with cancer receiving chemotherapy or radiation therapy Diagnosis: lung cancer (n = 25, 14%), gastric carcinoma (n = 45, 25%), intestinal carcinoma (n = 28, 15%), breast cancer (n = 84, 46%) Total N randomized: unclear N randomized to music group: unclear N randomized to control group: unclear N analyzed in music group: 128 N analyzed control group: 54 Mean age: 51 years Sex: 107 (59%) females, 75 (41%) males Ethnicity: 182 (100%) Chinese Setting: inpatient Country: China |
|
| Interventions | 2 study groups:
Music selections provided: Chinese classical music Number of sessions: 30 Length of sessions: 30 min Categorized as music medicine |
|
| Outcomes | Depression (Zung Self Rating Depression Scale): post‐test scores Anxiety (Zung Self Rating Anxiety Scale): post‐test scores |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not provided in the translation of the study report |
| Allocation concealment (selection bias) | Unclear risk | Not provided in the translation of the study report |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel were not blinded. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | This study did not address objective outcomes. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | It was unclear whether the number of participants randomized equalled the number of participants analysed. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No conflict of interest reported |
Cassileth 2003.
| Study characteristics | ||
| Methods | RCT 2‐arm parallel‐group design |
|
| Participants | Adults with hematologic malignancy admitted for high dose therapy with autologous stem cell transplantation Diagnosis: Hodgkin's (n = 8, 12%), non‐Hodgkin's lymphoma (n = 31, 45%), myeloma/amyloidosis (n = 30, 43%) Total N randomized: 69 Total N analyzed: 60 N randomized to music group: 36 N randomized to control group: 33 N analyzed in music group: 34 N analyzed in control group: 26 Mean age: 52 years Sex: 37 (54%) females, 32 (46%) males Ethnicity: not provided Setting: inpatient Country: USA |
|
| Interventions | 2 study groups:
Music selections provided: each music therapy session was individualized according to the needs of the participant. Number of sessions: the treatment group received a median of 5 sessions during a median of 10 days. Length of sessions: 20‐30 min Categorized as music therapy |
|
| Outcomes | Depression (POMS): post‐test scores (after 1 session) Anxiety (POMS): change scores (after 1 session) Mood (POMS total score): change scores (after 1 session) Fatigue (POMS): post‐test scores (after 1 session) |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "[R]andomized by telephone using the MSKCC clinical research database" (p. 2724) and "randomly permuted blocks with the following strata: whole body/whole lymphatic irradiation (yes/no); diagnosis (lymphoma, Hodgkin disease, myeloma/amyloidosis); and center (MSKCC/ICC)" (p. 2724). |
| Allocation concealment (selection bias) | Low risk | Quote: "[T]he use of telephone registration and randomization ensured concealment of treatment allocation". |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Music therapist and participants could not be blinded given the interactive nature of the music therapy session. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | This study did not address objective outcomes. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rate = 9 (13%) Withdrew before learning allocation (n = 7); discharged before post‐test (n = 2) |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | Supported in part, by the Memorial Sloan‐Kettering Cancer Center Translational/Integrative Medicine Research Fund |
Chen 2004.
| Study characteristics | ||
| Methods | RCT 2‐arm parallel‐group design |
|
| Participants | Adults who were ready to receive adjuvant chemotherapy after mastectomy Diagnosis: breast cancer Total N randomized: unclear N randomized to music group: unclear N randomized to control group: unclear N analyzed in music group: 42 N analyzed in control group: 44 Mean age: not provided Sex: 86 (100%) females Ethnicity: 86 (100%) Chinese Setting: inpatient Country: China |
|
| Interventions | 2 study groups:
Music selections provided: music selection was based on the participant's psychological status (excited or inhibited), but no further details were provided. Number of sessions: 36 Length of sessions: 60 min Categorized as music medicine |
|
| Outcomes | CD3, CD4, CD8, CD4/CD8, NK cell activity: post‐test scores | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Translation sheet: "Table of random numbers" |
| Allocation concealment (selection bias) | High risk | No allocation concealment was used. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Personnel and participants were not blinded. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Unclear risk | Information regarding blinding of outcome assessors was not provided in the translation of the report. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | Low risk | This study did not address subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | It was unclear whether the number of participants analyzed equalled the number of participants recruited. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No conflict of interest reported |
Chen 2013.
| Study characteristics | ||
| Methods | CCT 2‐arm parallel‐group design |
|
| Participants | Adult oncology patients Type of cancer: head and neck (n = 67, 33.5%), gynecological (n = 23, 11.5%), breast (n = 38, 19%), digestive tract (n = 37, 18.5%), lung (n = 12, 6%), prostate (n = 18, 9%) (numbers do not add up to total N of 200 but are reported as such in the published article) Total N randomized: 200 Total N analyzed: 200 N randomized to music group: 100 N randomized to control group: 100 N analyzed in music group: 100 N analyzed in control group: 100 Mean age: 55.4 years Sex: 79 (39.5%) females, 121 (60.5%) males Ethnicity: not reported Setting: outpatient Country: Taiwan |
|
| Interventions | 2 study groups:
Music selections provided: slow‐paced, soft, melodic music at low volume with consistent tempo and dynamics and an average 60‐80 beats per minute. Subjects chose their own music tracks from a selection of songs in Mandarin, Mandarin pop, traditional Taiwanese songs, Western music (country and western), and classical music (e.g. chamber music with string instruments). Number of sessions: 1 Length of sessions: 15 min Categorized as music medicine |
|
| Outcomes | Anxiety (STAI): change scores HR, RR, SBP, DBP, oxygen saturation: change scores |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "The 200 patients were randomly assigned by simple random sampling (every other patient) into two groups" (p. 437). |
| Allocation concealment (selection bias) | High risk | Alternate assignment prohibited allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were blinded to the study hypothesis. Personnel were not blinded. |
| Blinding of outcome assessment (detection bias) Objective outcomes | High risk | Outcome assessors were not blinded. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "A total of 209 patients who met the inclusion criteria were enrolled. Nine of these patients withdrew at the early stage for reasons of severe clinical condition or personal reasons, and 200 patients were retained for analysis" (p. 437). Attrition rate: 4.4% |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No conflict of interest reported |
Chen 2018.
| Study characteristics | ||
| Methods | CCT 3‐arm parallel‐group design |
|
| Participants | Adult women with breast cancer Type of cancer: breast cancer Total N randomized: 60 Total N analyzed: 36 N randomized to group music intervention: 20 N randomized to self‐directed music intervention: 20 (not included in this review) N randomized to control: 20 N analyzed in group music intervention: 20 N analyzed in control group: 16 Mean age: not reported Sex: 60 (100 %) females Ethnicity: not reported Setting: outpatient Country: Taiwan |
|
| Interventions | 2 study groups: 1. Music group: group sessions consisted of three stages: relaxation (10 min), music listening (40 min), and experience‐sharing (10 min). 2. Control group: standard care Music selections provided: combination of participant‐selected music and researcher‐selected music Number of sessions: 8 Length of sessions: 60 min Categorized as music medicine |
|
| Outcomes | Anxiety (HADS): mean rank Depression (HADS): mean rank |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "Subjects were sequentially assigned to GMI, SMI, or control group based on study enrollment" (p. 463). |
| Allocation concealment (selection bias) | High risk | Sequential assignment prevented allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants and personnel could not be blinded due to active music intervention. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | No objective outcomes included in this study |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition: 13.3% |
| Selective reporting (reporting bias) | Low risk | No suggestions of selective outcome reporting |
| Other bias | Low risk | "The authors declare that they have no conflict of interest. We have full control of all primary data and agree to allow the journal to review our data. Funding Funding support from the Minister of Science Technology, Taiwan, R.O.C. (NSC 102‐2410‐H‐006‐013)" (p. 468). |
Chen 2020.
| Study characteristics | ||
| Methods | RCT 2‐arm parallel‐group design |
|
| Participants | Women undergoing chemotherapy Type of cancer: breast (n = 100, 100%) Total N randomized: 100 Total N analyzed: 100 N randomized to music group: 50 N randomized to control group: 50 N analyzed in music group: 50 N analyzed in control group: 50 Mean age: 50.36 years Sex: 100 (100%) females, (0%) males Ethnicity: not reported Setting: outpatient Country: China |
|
| Interventions | 2 study groups: 1. Music group: listening to pre‐recorded music 2. Control group: standard care Music selections provided: 7‐8 pieces of recorded music including light music, sounds of nature, folk songs, pop songs, and classical music was given. The first two or three tracks were chosen according to participants’ music preference. Number of sessions: 1 Length of sessions: 45 min Categorized as music medicine |
|
| Outcomes | Depression (HADS‐D): post‐test scores, change scores computed by JB Anxiety (HADS‐A): post‐test scores Sleep quality (Pittsburgh Sleep quality index (PSQI)): post‐test scores Fatigue (Multidimensional Fatigue Symptom Inventory): post‐test scores, change scores computed by JB |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Eligible participants were randomly allocated to the experimental and control group using a computer‐generated sequence" (p. 353). |
| Allocation concealment (selection bias) | Unclear risk | No information was reported about allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Control group participants were not offered headset and blank CD. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Unclear risk | It was not reported who collected the objective outcomes. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts |
| Selective reporting (reporting bias) | Low risk | No evidence of selective outcome reporting |
| Other bias | Low risk | "Funding Funding support from the Minister of Science Technology, Taiwan, R.O.C. (MOST 102‐2410‐H‐006 ‐013). The authors declare that there is no conflict of interest" (p. 359). |
Clark 2006.
| Study characteristics | ||
| Methods | RCT 2‐arm parallel‐group design |
|
| Participants | Adults with cancer undergoing radiation therapy Diagnosis: prostate (n = 8, 13%), breast (n = 13, 21%), lung (n = 8, 13%), head and neck (n = 14, 22%), gastrointestinal (n = 9, 14%), gynecological (n = 5, 8%), other (n = 6, 10%) Total N randomized: 63 N randomized to music group: 35 N randomized to control group: 28 Total N analyzed: 59 N analyzed in music group: 18‐28 (depending on outcome) N analyzed in control group: 14‐21 (depending on outcome) Mean age: 57.59 years Sex: 24 (38%) females, 39 (62%) males Ethnicity: 54 (86%) white, 7 (11%) black, 2 (3%) other Setting: not stated in study report Country: USA |
|
| Interventions | 2 study groups:
Music selections provided: a personalized tape was created for each participant to use at any time during the course of therapy. Number of sessions: 2‐4 times per week for approximately 4‐5 weeks Length of sessions: unknown Categorized as music therapy |
|
| Outcomes | Anxiety (Hospital Anxiety and Depression Scale, HADS): post‐test scores, change scores computed due to large baseline differences. Depression (HADS): post‐test scores Fatigue (POMS): post‐test scores, change scores computed. Pain (Numeric Rating Scale, NRS): post‐test scores, change scores computed due to large baseline differences. Distress (NRS): change scores |
|
| Notes | No standard deviations were reported for post‐test scores in the publication. Standard deviations were obtained from the author. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Patients were randomized using a minimization procedure in which the first subject is assigned to a group with a coin toss. Subsequent subjects were assigned based upon covariate (tumor site, gender and pain) and assignment of previous subjects using a computer program." (p. 251). |
| Allocation concealment (selection bias) | Low risk | Minimization procedure as described above |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The music therapist and participants could not be blinded. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | This study did not address objective outcomes. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rate: 8%. Participants did not meet inclusion criteria (n = 4) or did not return for radiation therapy treatment (n = 1). |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No conflict of interest reported |
Cook 2013.
| Study characteristics | ||
| Methods | RCT 2‐arm parallel‐group design |
|
| Participants | Adult oncology patients Type of cancer: leukemia (n = 7, 41.2%), unspecified or other (n = 10, 58.8%) Total N randomized: 34 Total N analyzed: 17 N randomized to music group: 21 N randomized to control group: 13 N analyzed in music group: 10 N analyzed in control group: 7 Mean age: 59.8 years Sex: 9 (52.9%) females, 8 (47.1%) males Ethnicity: not reported Setting: inpatient Country: USA |
|
| Interventions | 2 study groups:
Music selections provided: not reported Number of sessions: 3 Length of sessions: 15‐30 min Categorized as music therapy |
|
| Outcomes | Spiritual well‐being (Functional Assessment of Chronic Illness Therapy‐Spiritual Well Being Scale, FACIT‐Sp.): post‐test scores | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “...and after they signed the consent form, they were randomly assigned to a controlled condition or an experimental music therapy condition via a computer program” (p. 241). |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Music therapist and participants could not be blinded. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | This study did not address objective outcomes. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Ten participants were lost in music therapy group, seven in the control group. Attrition rate: 50% |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No conflict of interest reported |
Danhauer 2010.
| Study characteristics | ||
| Methods | RCT 2‐arm parallel‐group design |
|
| Participants | Patients with cancer undergoing bone marrow biopsy Diagnosis: hematological malignancy Total N randomized: 63 N randomized to music group: 29 N randomized to control group: 30 N analyzed in music group: 29 N analyzed in control group: 30 Mean age: 50.9 years Sex: not provided Ethnicity: 46 (78%) white, 13 (22%) black Setting: outpatient Country: USA |
|
| Interventions | 2 study groups:
Music selections provided: participants selected from 8 music CDs with various types of relaxing music (classical, harp, general instrumental, nature sounds, country, gospel and jazz) Number of sessions: 1 Length of sessions: 20‐60 min Categorized as music medicine |
|
| Outcomes | Anxiety (STAI‐S): post‐test scores Pain (VAS): post‐test scores |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated number list (personal communication with principal investigator) |
| Allocation concealment (selection bias) | Low risk | Researcher was blind to randomized blocks (personal communication with principal investigator). |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | This study did not address objective outcomes. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rate: 6.3%. Data for 4 participants were incomplete. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No report of conflict of interest |
Doro 2017.
| Study characteristics | ||
| Methods | RCT 2‐arm parallel‐group design |
|
| Participants | Adult oncology patients undergoing hematopoietic stem cell transplantation Type of cancer: not reported in article. Personal communication with author: neoplastic hematological diseases (n = 100, 100%) Total N randomized: 100 Total N analyzed: 100 N randomized to music group: 50 N randomized to control group: 50 N analyzed in music group: 50 N analyzed in control group: 50 Mean age: 33.35 years Sex: 45 (45%) females, 55 (55%) males Ethnicity: not reported Setting: inpatient Country: Brazil |
|
| Interventions | 2 study groups: 1. Music therapy group: individual music therapy sessions with trained music therapist performing popular songs that were part of the social‐musical‐cultural identity of the participant. Participant played along using rhythmic instruments. 3. Control group: standard care Music selections provided: popular songs that were part of the social‐musical‐cultural identity of the participant Number of sessions: not reported Length of sessions: 30 min Categorized as music therapy |
|
| Outcomes | Pain (VAS): post‐test scores Anxiety (VAS): post‐test scores Mood (VAS): post‐test scores |
|
| Notes | Due to large baseline differences, the findings of this study could not be included in the meta‐analysis as change score and post‐test scores cannot be combined in the computation of SMD. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "One contributor not involved with the research threw a dice and communicated the number on the face to the researcher" (p. 1015). |
| Allocation concealment (selection bias) | Low risk | "One contributor not involved with the research threw a dice and communicated the number on the face to the researcher" (p. 1015). |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding is not possible in studies that use active music interventions. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | No objective outcomes were included. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | Unclear risk | Outcome assessor was "external psychology student" (p. 1015) but it was not explicitly stated that they were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rate: 0% |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | "The authors declare that they have no competing interests" (p. 1018). |
Duocastella 1999.
| Study characteristics | ||
| Methods | RCT 2‐arm parallel‐group design |
|
| Participants | Children with neoplasms needing chemotherapy Diagnosis: acute lymphocytic leukemia (n = 9, 27%), osteosarcoma (n = 5, 15%), Burkitt's lymphoma (n = 2, 6%), acute myeloid leukemia (n = 2, 6%), synovial sarcoma (n = 2, 6%), Hodgkin's (n = 2, 6%), tumor in the trunk (n = 2, 6%), Wilm's tumor (n = 2, 6%), Ewings sarcoma (n = 1, 3%), brain tumor (n = 1, 3%), lymphoblastic lymphoma (n = 1, 3%), primitive neuroectodermal tumor (n = 1, 3%) Total N randomized: 33 Total N analyzed: 30 N randomized to music group: 17 N randomized to control group: 16 N analyzed in music group:15 N analyzed in control group:15 Mean age: 10.6 years Sex: 15 (50%) females, 15 (50%) males Ethnicity: not provided Setting: inpatient Country: Spain |
|
| Interventions | 2 study groups:
Music selections provided: cultural and ethnic characteristics were considered in selecting songs and instruments. Number of sessions: 1 Length of sessions: 45 min Categorized as music therapy |
|
| Outcomes | Mood (Patient Opinion Likert Scale, OPEL): post‐test scores Immunoglobulin A (IgA) levels: change scores |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Translation sheet: "Computer‐generated number list" |
| Allocation concealment (selection bias) | Low risk | Translation sheet: "Statistical program Aleator" |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The music therapist and the participants could not be blinded. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | Staff responsible for analysing IgA were likely unaware of the participants' group assignment. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective data. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There were 3 dropouts (9%) (1 in control group). |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No conflict of interest reported |
Ferrer 2005.
| Study characteristics | ||
| Methods | CCT 2‐arm parallel‐group design |
|
| Participants | Adults with cancer receiving chemotherapy Diagnosis: no details reported Total N randomized: unclear N randomized to music group: unclear N randomized to control group: unclear N analyzed in music group: 25 N analyzed in control group: 25 Mean age: 55 years Sex: 26 (52%) females, 24 (48%) males Ethnicity: not provided Setting: outpatient Country: USA |
|
| Interventions | 2 study groups:
Music selections provided: patient‐preferred music with guitar accompaniment Number of sessions: 1 Length of sessions: 20 min Categorized as music therapy |
|
| Outcomes | Anxiety (VAS): post‐test scores Fatigue (VAS): post‐test scores Systolic blood pressure (SBP): post‐test scores Diastolic blood pressure (DBP): post‐test scores Heart rate: post‐test scores Fear (VAS), worry (VAS), level of comfort (VAS), level of relaxation (VAS): not used in this review |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The music therapist and the participants were not blinded. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | It was unclear whether the number of participants analyzed equalled the number of participants randomised. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No funding was received |
Firmeza 2017.
| Study characteristics | ||
| Methods | RCT 2‐arm parallel‐group design |
|
| Participants | Adults in the post‐surgical period, undergoing chemotherapy or radiotherapy Type of cancer: head and neck (n = 40, 100%) Total N randomized: 40 Total N analyzed: 40 N randomized to music group: 20 N randomized to control group: 20 N analyzed in music group: 20 N analyzed in control group: 20 Mean age: not reported Sex: 32 (80 %) females, 8 (20%) males Ethnicity: not reported Setting: outpatient Country: Brazil |
|
| Interventions | 2 study groups: 1. Music group: listening to classical music 2. Control group: standard care Music selections provided: "Spring" from the Four Seasons composition by Vivaldi with 60 to 80 beats per minute. Its first musical movement, (Allegro) has an E Major tonality and quaternary rhythm (4/4). In the second movement (Largo), the tonality changes to C minor, and the rhythm becomes ternary (3/4). In its last movement (Allegro Pastorale), the tonality returns to E Major, and the rhythm becomes quaternary again (12/8). Number of sessions: 1 Length of sessions: 30 min Categorized as music medicine |
|
| Outcomes | Anxiety (STAI‐S): change scores HR: change scores RR: change scores SBP: change scores DBP: change scores |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "For those who met the inclusion criteria, the randomization process was performed using the random number table generated in the Epi‐Info program version 7.1.4." (p. 2). |
| Allocation concealment (selection bias) | Low risk | "We emphasize that in order to guarantee concealment of the participant’s allocation, their designation was only known to the study administrator after opening a properly sealed envelope which contained the condition selected for that participant" (p. 2). |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Control participants were not given headsets, therefore, personnel were not blinded. Participants were not blinded. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Unclear risk | Objective outcomes were collected, however, authors did not give details regarding who collected the data. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition: n = 4 (9%) |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Unclear risk | No information was provided on funding source or conflicts of Interest. |
Fredenburg 2014a.
| Study characteristics | ||
| Methods | RCT 2‐arm parallel‐group design |
|
| Participants | Adult cancer patients recovering from a blood and marrow transplant Type of cancer: acute myelogenous leukemia (n = 3, 8.0%), acute lymphoblastic leukemia (n = 2, 5.9%), chronic lymphocytic leukemia (n = 3, 8.0%), non‐Hodgkin's lymphoma (n = 5, 14.7%), myelodysplastic syndromes (n = 2, 5.9%), multiple myeloma (n = 7, 20.6%), leukemia (not specified) (n = 6, 17.6%), lymphoma (not specified) (n = 1, 2.9%), other (n = 3, 8.0%) Total N randomized: 34 Total N analyzed: 32 N randomized to music group: 14 N randomized to control group: 20 N analyzed in music group: 12 N analyzed in control group: 20 Mean age: 53.5 Sex: 17 (55.9%) female, 15 (44.1%) male Ethnicity: Asian (n = 1, 2.9%), Latino (n = 3, 8%), white (n = 23, 67.6%), other (n = 5, 14.7%) Setting: inpatient Country: USA |
|
| Interventions | 2 study groups:
Music selections provided: participant's preferred music Number of sessions: 1 Length of sessions: 30 min Categorized as music therapy |
|
| Outcomes | Positive and negative affect (PANAS), pain (NRS): post‐test scores | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Participants were randomly assigned via a computer program to either the experimental group (n = 12) or wait‐list control group (n = 20)" (p. 176). |
| Allocation concealment (selection bias) | High risk | No allocation concealment used (personal communication with chief investigator) |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Music therapist and participants could not be blinded. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | This study did not address objective outcomes. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "2 participants did not complete measures" (p. 177). Attrition rate: 6% |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No conflict of interest reported |
Fredenburg 2014b.
| Study characteristics | ||
| Methods | RCT 2‐arm parallel‐group design |
|
| Participants | Adults in bone marrow transplant unit Type of cancer: acute myelogenous leukemia (n = 2, 18.2%), acute lymphoblastic leukemia (n= 2, 18.2%), chronic lymphocytic leukemia (n = 2, 18.2%), Hodgkin's disease (n = 1, 9.1%), multiple myeloma (n = 1, 9.1%), non‐Hodgkin's lymphoma (n = 2, 18.2%), and lymphoma (n = 1, 9.1%) Total N randomized: 13 Total N analyzed: 11 N randomized to music group: 8 N randomized to control group: 5 N analyzed in music group: 7 N analyzed in control group: 4 Mean age: 49.69 Sex: n = 3 (27.3%) female, n = 8 (72.7%) male Ethnicity: white: n = 10 (90.9%), other: n = 1 (9.1%) Setting: inpatient Country: USA |
|
| Interventions | 2 study groups:
Music selections provided: patient‐preferred live music Number of sessions: 3‐5 Length of sessions: 30‐45 min Categorized as music therapy |
|
| Outcomes | Fatigue (Multidimensional Fatigue Inventory, MFI): change scores | |
| Notes | Means and standard errors were reported in the journal article. Standard deviations were obtained from the primary author. Because of large baseline differences between the groups, JB computed change scores and associated SDs. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The participants were randomly assigned via a computer program to either the experimental (n = 7) or wait‐list control (n = 4) groups " (p. 436). |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Music therapist and participants could not be blinded. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | This study did not address objective outcomes. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Flowchart reported that 13 participants consented and randomized; 11 analyzed (p. 435). Attrition rate: 16% |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No conflict of interest reported |
Gimeno 2008.
| Study characteristics | ||
| Methods | CCT Cross‐over trial |
|
| Participants | Adult patients with cancer undergoing chemotherapy Diagnosis: breast cancer (n = 10, 50%), non‐small cell lung cancer (n = 5, 25%), lymphoma (n = 2, 10%), sarcoma (n = 1, 5%), colon cancer (n = 1, 5%), tongue cancer (n = 1, 5%) Total N randomized: 20 Total N analyzed: 10 Mean age: 55.6 years Sex: 16 (80%) females, 4 (20%) males Ethnicity: 9 (45%) white, 1 (5%) black, 1 (5%) Latino, 9 (45%) Asian Setting: outpatient Country: USA |
|
| Interventions | 2 study groups:
Music selections provided: new age music Number of sessions: 3 BMGIM sessions and 3 imagery‐only sessions Length of sessions: 60‐90 min Categorized as music therapy |
|
| Outcomes | HR: post‐test scores Nausea and emesis (no standard deviations (SD) reported): not included in this review |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Low risk | Cross‐over trial; all participants received both sessions. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding of participants and music therapist was not possible given the interactive nature of the music therapy sessions. |
| Blinding of outcome assessment (detection bias) Objective outcomes | High risk | Outcome assessors were not blinded. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition rate: 50%. 1 participant was excluded from the analysis because she only completed 4 sessions. Principal investigator mentioned other reasons for withdrawal but did not provide specific numbers. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No conflict of interest reported |
Hanser 2006.
| Study characteristics | ||
| Methods | RCT 2‐arm parallel‐group design |
|
| Participants | Women with metastatic breast cancer Diagnosis: metastatic breast cancer (stage IV) Total N randomized: 70 N randomized to music group: 35 N randomized to control group: 35 N analyzed in music group: 20 N analyzed in control group: 22 Mean age: 51.5 years Sex: 70 (100%) females, 0 males Ethnicity: 58 (83%) white, 7 (10%) black, 1 (2%) Latino Setting: outpatient Country: USA |
|
| Interventions | 2 study groups:
Music provided: live music based on participant's preferences and needs Number of sessions: 3 Length of sessions: 45 min Categorized as music therapy |
|
| Outcomes | Depression (HADS): post‐test scores Anxiety (HADS): post‐test scores Physical well‐being (the Functional Assessment of Cancer Therapy‐General, FACT‐G Physical Wellbeing Subscale): post‐test scores QoL (FACT‐G): post‐test scores Spirituality (Functional Assessment of Chronic Illness Therapy‐Spiritual Well‐being Scale, FACIT‐Sp): change scores |
|
| Notes | The 3 music sessions were spread over 15 weeks. Music therapy treatment was usually offered on a weekly or biweekly basis with this population. The author reported that it was not feasible to have participants come to the clinic each week and that because of this spread, the intervention was highly diluted. Therefore, the data of this study were not included in the meta‐analysis of this review. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Computer‐generated random numbers determined the assignment of numbered folders to control or experimental conditions" (p. 117). |
| Allocation concealment (selection bias) | Low risk | Quote: "the participants opened the sealed envelope to reveal group assignment to either the experimental/music therapy intervention or control/usual care condition" (p. 117). |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The music therapist and the participants could not be blinded. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | This study did not address objective outcomes. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition rate: n = 28 or 40%. Music therapy group participants cancelled before initiation of the study: (too busy, n = 5); from baseline to first follow‐up (too busy, n = 2; no interest, n = 2; moved, n = 1; health limits, n = 1; lost, n = 1); and from first to second follow‐up (health limits, n = 1; died, n = 1; lost, n = 1). Control group participants cancelled before the initiation of the study: (too busy, n = 2; died, n = 2); from baseline to first follow‐up (not interested, n = 1; moved, n = 1; died, n = 2); and from first to second follow‐up (died, n = 2; lost, n = 3) |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | High risk | The 3 music sessions were spread over 15 weeks. Music therapy treatment was usually offered on a weekly or biweekly basis with this population. The author reported that it was not feasible to have participants come to the clinic each week. No report of conflict of interest |
Harper 2001.
| Study characteristics | ||
| Methods | RCT 4‐arm parallel‐group design |
|
| Participants | Adults with cancer undergoing chemotherapy Diagnosis: breast (n = 13, 32.5%), colon (n = 12, 30%), ovarian (n = 7, 17.5%), lung (n = 7, 17.5%), prostate (n = 1, 2.5%) Total N randomized: 40 N randomized to music‐only group: 10 N randomized to problem‐focused visualization group: 10 (not included in this review) N randomized to emotion‐focused visualization group: 10 (not included in this review) N randomized to control group: 10 N analyzed in music group: 10 N analyzed in control group: 10 N analyzed in problem‐focused visualization: 10 (not included in this review) N analyzed in emotion‐focused visualization: 10 (not included in this review) Mean age: 52 years Sex: 33 (83%) females, 7 (17%) males Ethnicity: 32 (80%) white, 4 (10%) black, 4 (10%) Latino Setting: outpatient Country: USA |
|
| Interventions | 2 study groups:
Music selections provided: new age music, namely Health Journeys: Cancer Image Path Number of sessions: 1 Length of sessions: 30 min Categorized as music medicine |
|
| Outcomes | Anxiety (STAI‐S): change scores Anxiety (Beck Anxiety Inventory, BAI): not used in this review Coping (Coping Orientations to Problems Experienced, COPE): not used in this review HR, SBP, DBP: change scores White blood cell count (WBC), red blood cell count (RBC), absolute neutrophil count (ANC): not used in this review; only measured at intake and at 6 weeks follow‐up while only 1 music session was used |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A table of random numbers was used to assign each participant number to a condition" (personal communication with principal investigator). |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Personnel and participants were not blinded. |
| Blinding of outcome assessment (detection bias) Objective outcomes | High risk | Outcome assessors for WBC, RBC, and ANC were blinded. Outcome assessor for HR, SBP, and DBP was not blinded (personal communication with principal investigator). |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No subject loss in music group or control group |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | — |
Hilliard 2003.
| Study characteristics | ||
| Methods | RCT 2‐arm parallel‐group design |
|
| Participants | Adults with terminal cancer Diagnosis: cancer of lung (n = 27, 33.75%), colon (n = 7, 8.75%), kidney (n = 3, 3.75%), nasopharynx (n = 1, 1.25%), prostate (n = 1, 1.25%), liver (n = 2, 2.5%), esophogeal (n = 3, 3.75%), breast (n = 5, 6.25%), pancreas (n = 5, 6.25%), brain (n = 5, 3.75%), oral cavity (n = 1, 1.25%), ovary (n = 2, 2.5%), stomach (n = 2, 2.5%), endometrium (n = 1, 1.25%), sinus (n = 1, 1.25%), larynx (n = 1, 1.25%), leukemia (n = 2, 2.5%), melanoma (n = 2, 2.5%), multiple myeloma (n = 3, 3.75%), lymphoma (n = 1, 1.25%), head, neck and face (n = 1, 1.25%) and unspecified cancer (n = 3, 3.75%) Total N randomized: unclear N randomized to music group: unclear N randomized to control group: unclear N analyzed in music group: 40 N analyzed in control group: 40 Mean age: 65.5 years Sex: 40 (50%) females, 40 (50%) males Ethnicity: 60 (75%) white, 20 (25%) black Setting: home hospice care Country: USA |
|
| Interventions | 2 study groups:
Music provided: music therapy interventions were selected based on the participant's in‐the‐moment needs Number of sessions: 2 to 13. Sessions were offered weekly or bi‐weekly until the participant died. Length of sessions: unknown Categorized as music therapy |
|
| Outcomes | QoL (Hospice QoL Index‐Revised): change scores were computed by JB to allow for computation of pooled effect size (SMD) with other studies that reported change scores. Physical status (Palliative Performance Scale): post‐test scores Length of life (in days) |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: " A computer generated number list was used for randomisation" (personal communication with principal investigator). |
| Allocation concealment (selection bias) | Low risk | Quote: "Researcher and assistant did not know what treatment patient was assigned to until after consent was completed" (personal communication with principal investigator). |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The music therapists and participants could not be blinded. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | Outcome assessors were not blinded, but it was unlikely that the report of length of life (in days) would have been biased. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Quote: "When participants were lost due to death before they had completed 2 sessions, additional participants were recruited until a complete data set of 80 participants was obtained" (personal communication with principal investigator). |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No report of conflict of interest |
Horne‐Thompson 2008.
| Study characteristics | ||
| Methods | RCT Two‐arm parallel‐group design |
|
| Participants | Terminally ill patients (8% with non‐cancer diagnosis) Diagnosis: Amyloidosis (n = 1, 4%), bowel cancer (n = 1, 4%), breast cancer (n = 4, 16%), glioblastoma (n = 2, 8%), lung cancer (n = 2, 8%), lymphoma (n = 2, 8%), mesothelioma (n = 1, 4%), metastatic melanoma (n = 1, 4%), non‐Hodgkin’s lymphoma (n = 1, 4%), non small cell lung carcinoma (n = 3, 12%), oesophageal cancer (n = 1, 4%), ovarian cancer (n = 1, 4%), rectal cancer (n = 3, 12%),thyroid cancer (n = 1, 4%) Total N randomized: 25 N randomized to music group: 13 N randomized to control group: 12 N analyzed in music group: 13 N analyzed in control group: 12 Mean age: 73.9 years Sex: 11 (44%) females, 14 (66%) males Ethnicity: not reported Setting: inpatient Country: Australia |
|
| Interventions | 2 study groups: 1. Music therapy group: music therapy methods chosen by the registered music therapist in consultation with the participant as being most appropriate for the participant on the day. These techniques included playing live familiar music, singing, music and relaxation, music and imagery, improvisation, music‐assisted counseling, reminiscence, and listening to recorded music. 2. Control condition: volunteer sitting with the participant, undertaking activities that a volunteer would normally do, such as reading to the participant, engaging in conversation, and/or providing emotional support |
|
| Outcomes | Symptoms (ESAS): range of improvement | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants were randomly assigned to treatment arm. Specific randomization method not reported |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding of participants and music therapist was not possible given the interactive nature of the music therapy sessions. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | No objective outcomes included in this study |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rate: 0% |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Unclear risk | No conflict of interest statement included in the publication |
Huang 2006.
| Study characteristics | ||
| Methods | RCT 2‐arm parallel‐group design |
|
| Participants | Adult cancer patients with pain Diagnosis of sample included in final analysis (n = 126): cancer of head or neck (n = 51, 41%), gastrointestinal (n = 25, 20%), hematological (n = 16, 13%), genitourinary (n = 15, 12%), lung (n = 7, 6%), bone (n = 1, 1%), other (n = 11, 9%) Total N randomized: 129 N randomized to music group: 65 N randomized to control group: 64 N analyzed in music group: 62 N analyzed in control group: 64 Mean age: 54 years Sex: 38 (30%) females, 88 (70%) males Ethnicity: 129 (100%) Taiwanese Setting: inpatient Country: Taiwan |
|
| Interventions | 2 study groups:
Music provided: music was sedative (60‐80 beats) without lyrics, with a sustained melody quality, and controlled volume and pitch. Participants were asked to select from 4 audiotapes: 2 with Taiwanese music (Taiwanese folk songs and Buddhist music) and 2 with American music (harp music and piano music). Number of sessions:1 Length of sessions: 30 min Categorized as music medicine |
|
| Outcomes | Pain (VAS): post‐test scores | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A computerized minimization program was used to randomise and conceal the allocation until after assignment and to stratify the groups on hospital unit" (p. 2). |
| Allocation concealment (selection bias) | Low risk | Quote: "A computerized minimization program was used to randomise and conceal the allocation until after assignment and to stratify the groups on hospital unit" (p. 2). |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | This study did not address objective outcomes. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rate: 2.4%. Inability to focus on the music (n = 1), did not complete music protocol because of interruptions (n = 2) |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No report of conflict of interest |
Hunter 2020.
| Study characteristics | ||
| Methods | RCT 3‐arm parallel‐group |
|
| Participants | Adults receiving chemotherapy or radiation therapy Type of cancer: Breast cancer 401 (85%), gastrointestinal cancer 30 (6%), other 43 (9%) Total N randomized: 474 N randomized to music group: 159 N randomized to mindful relaxation: 160 (not analyzed in this review) N randomized to control group: 155 N analyzed in music group: midpoint: 107, endpoint: 118 N analyzed in mindfulness relaxation (MR): midpoint: 96, endpoint 107 (not analyzed in this review) N analyzed in control group: midpoint: 100, endpoint: 112 Mean age: Information not reported Sex: 435 (91.8%) females, 39 (8.2%) males Ethnicity: White, non‐Hispanic 318 (67.1%) Black, non‐Hispanic 54 (11.4%) Hispanic 96 (20.3%) Asian, non‐Hispanic or unknown 5 (1.1%) Setting: outpatient Country: United States including Puerto Rico |
|
| Interventions | 3 study groups: 1. Music group: The Relaxing Music group received a recording to be utilized in a manner identical to the MR, but which did not contain any specific instructions on relaxation or meditation; rather it consisted of relaxing music with nature sounds or a vocal track. The participants also received general information on the management of symptoms related to chemotherapy in a session of equivalent time to the MR training session. 2. Control group: In the SC group, participants received general information on the management of symptoms related to chemotherapy as would be typical of that CCOP site. The same duration of individual contact with the nurse occurred in all conditions. 3. Mindfulness relaxation group: MR consisted of a single exercise, composed of guided mindfulness, imagery, and relaxation practices of approximately 20 minutes’ duration which was repeated throughout the course of chemotherapy. Oncology nurses from the CCOP network volunteered to be trained in the intervention by the study team. Following training, each nurse prepared a master recording of the MR exercise to use with his or her participants. (not analyzed in this review). Music selections provided: Relaxing music with nature sounds or a vocal track Number of sessions: 4‐6 depending on chemotherapy protocol Length of sessions: approximately 20 minutes Categorized as music medicine |
|
| Outcomes | Anticipatory nausea (Morrow Assessment of Nausea and Emesis): odds ratio | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Patients with newly diagnosed cancer, who were scheduled to undergo chemotherapy, were adaptively randomized 26 in a ratio of 1:1:1 to MR, RM, or SC" (p. 1735). |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment methods were not described. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | The mindfulness group received personal instruction from a nurse. The music group followed the same protocol. It was not clear how instructions were given, but it was assumed that the nurse knew the group assignment as the protocol was the same as for the mindfulness participants. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | No objective outcomes included |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition rate: n = 122 (25.7%) |
| Selective reporting (reporting bias) | High risk | Although participants completed a number of psychosocial and quality of life measures, the primary outcome was nausea and vomiting. The current paper only presented the data for the primary outcomes. |
| Other bias | Unclear risk | Dr. Fisch is employed by Aim Specialty Health, a subsidiary of Anthem, Inc. All other authors declared no conflicts of interest (p. 1733). It was unclear if Dr. Fish's employment presented a conflict of interest. |
Jasemi 2016.
| Study characteristics | ||
| Methods | RCT 2‐arm parallel‐group design |
|
| Participants | Adults Type of cancer: soft tissue (n = 31, 52%), bone (n = 14, 23%), leukemia (n = 15, 25%) Total N randomized: 60 Total N analyzed: 60 N randomized to music group: 30 N randomized to control group: 30 N analyzed in music group: 30 N analyzed in control group: 30 Mean age: not reported Sex: 33 (55%) females, 27 (45%) males Ethnicity: not reported Setting: not reported Country: Iran |
|
| Interventions | 2 study groups: 1. Music group: music listening 2. Control group: standard care Music selections provided: relaxing light music like the sea, rain, and water sounds Number of sessions: 3 Length of sessions: 20 min Categorized as music medicine |
|
| Outcomes | Depression and anxiety (HADS): post‐test of total scale scores (see note below) | |
| Notes | Authors only reported a total HADS score. HADS does not allow for the use of a total score. Instead, subscores for anxiety and for depression should be reported. Therefore, the data from this study were not included in the meta‐analyses. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Participants were randomly allocated to two groups of controls and experiments using simple random sampling method" (p. 456). |
| Allocation concealment (selection bias) | Unclear risk | Information about allocation concealment was not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No Walkman/headset was given to control group participants, therefore, personnel were not blinded; participants were not blinded. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | No objective outcomes were included. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information about attrition and no participant flow chart were included. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | "This research was financially supported by Urmia University of Medical Sciences. Conflicts of interest: There are no conflicts of interest" (p. 458). |
Jin 2011.
| Study characteristics | ||
| Methods | RCT 2‐arm parallel‐group design |
|
| Participants | Adults with primary liver cancer Type of cancer: liver (n = 102, 100%) Total N randomized: 102 N randomized to music group: 50 N randomized to control group: 52 N analyzed in music group: 50 N analyzed in control group: 52 Mean age: 56.7 Sex: not reported Ethnicity: 100% Chinese Setting: inpatient Country: China |
|
| Interventions | 2 study groups:
Music selections provided: This study used the Gaotian‐Music relaxation series, which is recorded by the Center of Music Therapy and published by the people's Liberation Army Health Audio Video Publishing House. The participants could choose any music they liked from the following 4 CDs: The Sea Reverie, Mountain Language, The Stream Chant, Grassland Meditation Number of sessions: 1 Length of sessions: for duration of surgery Categorized as music medicine |
|
| Outcomes | HR, RR, SBP, DBP: post‐test scores Anxiety (STAI): post‐test scores |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Translation sheet: table of random numbers |
| Allocation concealment (selection bias) | Unclear risk | Translation sheet: not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) Objective outcomes | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective data. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No subject loss |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No conflict of interest reported |
Karadag 2019.
| Study characteristics | ||
| Methods | RCT 2‐arm parallel‐group design |
|
| Participants | Women in early‐stage breast cancer undergoing radiation therapy Type of cancer: breast (n = 60, 100%) Total N randomized: 60 Total N analyzed: 60 N randomized to music group: 30 N randomized to control group: 30 N analyzed in music group: 30 N analyzed in control group: 30 Mean age: 59.4 years, SD ± 13.28 Sex: 60 (100%) females, (0%) males Ethnicity: not reported Setting: outpatient Country: Turkey |
|
| Interventions | 2 study groups: 1. Music group: listening to music 2. Control group: standard care Music selections provided: Bach's 19 trio sonatas in which James Galway plays the flute Number of sessions: 25 Length of sessions: 20‐40 min Categorized as music medicine |
|
| Outcomes | Depression (HADS‐D): post‐test scores, change score computed by JB Anxiety (HADS‐A): post‐test scores Comfort: Radiation Therapy Comfort Questionnaire (RTCQ): post‐test scores |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Use of alternate assignment: "Among the patients who agreed to participate in the study, the first patient who came to the radiation oncology outpatient clinic was assigned to the intervention group and the second patient was assigned to control group so that they were randomly assigned to the study groups" (p. 40‐41). |
| Allocation concealment (selection bias) | High risk | Use of alternate assignment prevented allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants in the music treatment arm listened to music via MP3 and headsets player during radiation. Control participants were not provided with MP3 player and headset. Therefore, personnel were not blinded. Participants were not blinded. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | No objective outcomes were included. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rate: 0% |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | "The financial support for this study was provided by the investigators themselves. The authors declared no potential conflicts of interest with respect to the authorship and/or publication of this article" (p. 43). |
Keenan 2017.
| Study characteristics | ||
| Methods | RCT 2‐arm parallel‐group design |
|
| Participants | Adults following hematopoietic stem cell transplant Type of cancer: acute myelogenous leukemia (AML) (n = 4, 20%), chronic myelogenous leukemia (CML) (n = 2, 10%), non‐Hodgkins lymphoma (n = 8, 40%), multiple myeloma (n = 8, 40%) Total N randomized: 20 Total N analyzed: 20 N randomized to music group: 10 N randomized to control group: 10 N analyzed in music group: 10 N analyzed in control group: 10 Mean age: 54 years, SD (11) Sex: 12 (60%) females, 8 (40%) males Ethnicity: 6 (30%) African American, 1 (5%) Latino, 13 (65%) Caucasian Setting: not reported Country: USA |
|
| Interventions | 2 study groups: 1. Music group: listening to Pandora Radio 2. Control group: standard care Music selections provided: A variety of musical selections via Pandora Number of sessions: 1 Length of sessions: 30 min Categorized as music medicine |
|
| Outcomes | Pain and mood (see note) | |
| Notes | This study met the inclusion criteria, however, none of the data were included in meta‐analyses. The statistical reporting was very poor with P values that were impossible (e.g. P = 1.23 for pain). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "A random number table was used to create a randomization sequence" (p. 41). |
| Allocation concealment (selection bias) | Unclear risk | No information about allocation concealment was reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Control participants were not given a headset and blank CD to achieve blinding of personnel. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | No objective outcomes included |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | There was no flow chart or information about attrition. |
| Selective reporting (reporting bias) | Low risk | No suggestions of selective outcome reporting |
| Other bias | Low risk | No funding received |
Kwekkeboom 2003.
| Study characteristics | ||
| Methods | RCT 3‐arm parallel‐group design |
|
| Participants | Adults with cancer having noxious medical procedures such as tissue biopsy or port placement or removal Diagnosis of sample that was included in final analysis (n = 58): breast cancer (n = 17, 29%), lymphoma (n = 17, 29%), leukemia (n = 9, 16%), colorectal cancer (n = 3, 5%), other (n = 12, 21%). Total N randomized: 60 N randomized to music group: 24 N randomized to audiobook group: 15 N randomized to control group: 21 N analyzed in music group: 24 N analyzed in audiobook group: 14 (not included in this review) N analyzed in control group: 20 Mean age: 53.28 years Sex: 40 (69%) females, 18 (31%) males Ethnicity: 60 (100%) white Setting: inpatient Country: USA |
|
| Interventions | 2 study groups:
Music selections provided: participants selected preferred music from a variety of music styles offered by the researcher and listened to music through headphones. Number of sessions: 1 Length of sessions: duration of procedure Categorized as music medicine |
|
| Outcomes | Anxiety (STAI‐S): post‐test scores Pain (NRS): post‐test scores Sense of control: not included in this review |
|
| Notes | Author's comment: "Patients may not want to be distracted or inattentive during the medical procedure as they may have felt the need to monitor what was happening. Some patients specifically commented that the music or book tape made it impossible for them to hear or focus on the surgeon". | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated number list (personal communication with principal investigator) |
| Allocation concealment (selection bias) | Low risk | Opaque sealed envelopes (personal communication with principal investigator) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Personnel and participants were not blinded. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | This study did not address objective outcomes. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rate: n = 2 (3%). 1 participant was excluded because he was randomized to the audiobook group but requested music; 1 from the control group was excluded because the surgeon requested that music be played. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | This work was funded by a 2001 grant from the Univeristy of Iowa, Central Investment Fund for Research Enhancement. |
Letwin 2017.
| Study characteristics | ||
| Methods | RCT 2‐arm parallel‐group design |
|
| Participants | Adults on a medical oncology/hematology unit Type of cancer: leukemia (n = 8, 53%), lung (n = 2, 13%), lymphoma (n = 2, 13%), pancreatic (n = 2, 13%), verrucous carcinoma (n = 1, 7%) Total N randomized: 15 Total N analyzed: 15 N randomized to music group: 8 N randomized to control group: 7 N analyzed in music group: 8 N analyzed in control group: 7 Mean age: 53.8 years Sex: 6 (40%) females, 9 (60%) males Ethnicity: not reported Setting: inpatient Country: USA |
|
| Interventions | 2 study groups: 1. Music therapy group: The protocol consisted of a two‐day session format providing opportunities for rapport‐building during day one and the discussion of resilience themes and strategies during day two. During day one, the PI discussed what types of music the participants were interested in and then transitioned to resilience‐themed patient‐preferred live music (PPLM) providing participants an opportunity to choose songs from the song menu. During day two, the session focused on resilience‐themed PPLM and resilience‐focused dialogue based upon the responses from the participants. The day two protocol was divided into three brief dialogues and four opportunities for song choice, with the PI alternating between resilience‐themed PPLM and resilience‐focused dialogue. The PI facilitated discussion using the following dialogue types: opening dialogue, dialogue concerning song choice within a category of resilience (social support, spiritual, hope, inner strength), future oriented dialogue, and closing dialogue. Between each dialogue, the PI directed the participant back to the music and played a song chosen by the participant from a 23‐item resilience‐themed song menu including folk, popular, country, and sacred music. All songs were sung live using a Yamaha steel string acoustic guitar for accompaniment. Following the song, the PI observed the participant’s response to the music and then transitioned to the next resilience‐focused dialogue. 2. Control group: wait‐list control standard care Music selections provided: a 23‐item resilience‐themed song menu including folk, popular, country, and sacred music. Number of sessions: 2 Length of sessions: 30‐45 min Categorized as music therapy |
|
| Outcomes | Resilience (Response to Stressful Events Scale (RSES)): post‐test scores Pain (NRS): post‐test scores |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Participants were randomly assigned to the experimental or control condition via a computer program" (p. 120). |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Personnel and participants could not be blinded in active music interventions. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | No objective outcomes included |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition rate: n = 8 (20%) |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Unclear risk | No conflict of interest or funding statement was included. |
Li 2004.
| Study characteristics | ||
| Methods | CCT 2‐arm parallel‐group design |
|
| Participants | Adults with gastric cancer awaiting surgery Diagnosis: stage II and III gastric cancer Total N randomized: unclear N randomized to music group: unclear N randomized to control group: unclear N analyzed in music group: 30 N analyzed in control group: 30 Mean age: 68.5 years Sex: 23 (38%) females, 37 (62%) males Ethnicity: 60 (100%) Chinese Setting: inpatient Country: China |
|
| Interventions | 2 study groups:
Music selections provided: Chinese classical music (6 different compositions) (no further detail provided) Number of sessions: 2 sessions/day for 4 days preoperatively, totaling 8 sessions Length of sessions: 20‐30 min Categorized as music medicine |
|
| Outcomes | Anxiety (Zung State Anxiety Scale, SAS): post‐test scores | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not provided in translation of study report |
| Allocation concealment (selection bias) | Unclear risk | Not provided in translation of study report |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not provided in translation of study report |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | This study did not address objective outcomes. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | It was unclear whether the number of participants analyzed equalled the number of participants recruited. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No conflict of interest reported |
Li 2012.
| Study characteristics | ||
| Methods | RCT 2‐arm parallel‐group design |
|
| Participants | Adult patients with breast cancer after radical mastectomy Type of cancer: breast (n = 120, 100%) Total N randomized: 120 N randomized to music group: 60 N randomized to control group: 60 N analyzed in music group: 60 at 1st post‐test; 54 at 3rd post‐test N analyzed in control group: 60 at 1st post‐test; 51 at 3rd post‐test Mean age: 42 years Sex: 120 (100%) female Ethnicity: not reported Setting: inpatient Country: China |
|
| Interventions | 2 study groups:
Music selections provided: participants selected their preferred music and controlled the music volume. Number of sessions: twice daily Length of sessions: 30 min Categorized as music medicine trial |
|
| Outcomes | Anxiety (STAI): post‐test score Pain (Short‐Form of McGill Pain Questionnaire ‐ Chinese version): post‐test score Depression (Zung Self rating Depression Scale): change score (computed by JB) Length of hospital stay (days) |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The randomisation procedure was performed with 120 random numbers produced by a computer program and all patients were randomly allocated to two groups: an experimental group (n = 60) and a control group (n = 60)" (p. 1178). |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel were not blinded. "Because of the specificity of the study, no blinding was used" (p. 1147). |
| Blinding of outcome assessment (detection bias) Objective outcomes | High risk | "Because of the specificity of the study, no blinding was used" (p. 1147). |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "None of the participants in the experimental and control groups was lost at the first post‐test. Fifty‐four participants remained in the experimental group (six participants lost) and 51 participants remained in the control group (nine participants lost) at the second and third post‐tests, respectively. A total of 15 patients (12.5%) were lost to follow‐up" (p. 1150). |
| Selective reporting (reporting bias) | Low risk | The reporting of outcomes was divided over three publications but there was no indication that some outcomes may have not been reported. |
| Other bias | Low risk | No conflict of interest reported |
Liao 2013.
| Study characteristics | ||
| Methods | RCT 3‐arm parallel‐group design |
|
| Participants | Advanced tumor node metastasis cancer patients Type of cancer: tumor node metastasis Total N randomized: 160 N randomized to Chinese Medicine (CM) 5‐element music group: 66 N randomized to Western music group: 63 (not included in this review) N randomized to control group: 31 N analyzed in Chinese Medicine (CM) 5‐element music group: 57 N analyzed in Western music group: 58 (not included in this review) N analyzed in control group: 31 Mean age: 63.1 years Sex: 83 (51.9%) female, 77 (48.1%) male Ethnicity: not reported although likely that the majority of the participants were Chinese Setting: inpatient Country: China |
|
| Interventions | 3 study groups:
Music selections provided: participants in the CM 5‐element music group were offered CM 5‐element music composed by Prof Shi Feng. Number of sessions: 1 session/day for 5 days/week for a total duration of 3 weeks Length of sessions: 30 min Categorized as music medicine |
|
| Outcomes | Quality of life (Hospice Quality of Life Index‐Revised (HQLI‐R)) Physical functioning (KPS): change scores |
|
| Notes | Change scores were computed by JB because of significant baseline differences between the groups. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "SAS 9.2 statistical software was used to generate random sequence numbers based on the 2:2:1 ratio" (p. 737). |
| Allocation concealment (selection bias) | Low risk | "The random allocation scheme was put into a brown envelope. When a patient accorded with the inclusion criteria, implementers opened the envelope to obtain the subject's random allocation" (p. 737). "The randomized scheme was sealed in an opaque envelope" (p. 737‐8). |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | "A single‐blind design was adopted in the trial, that is, the subject remained blinded, while the researcher knew the intervention program" (p. 738). However, participants knew whether they were listening to music or not, thus participants in the control group were not blinded. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | No objective measures were included. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | "A single‐blind design was adopted in the trial, that is, the subject remained blinded, while the researcher knew the intervention program" (p. 738). However, participants knew whether they were listening to music or not, thus participants in the control group were not blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "Fourteen patients dropped out of the study. 7 patients dropped out because of aggravation to the disease condition. 7 patients withdrew voluntarily during the study" (p. 738). Attrition rate: 8.75% |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | Study was supported by the project of the Chinese Geriatric Oncology society of the "eleventh‐5 year: plan of ministry of civil affairs" (no 2008‐47‐2‐45). |
Lin 2011.
| Study characteristics | ||
| Methods | RCT 3‐arm parallel‐group design |
|
| Participants | Adult cancer patients receiving chemotherapy Type of cancer: lung (n = 14, 14.3%), breast (n = 40, 40.8%), other (n = 44, 44.9%) Total N randomized: 123 N randomized to music group: not reported N randomized to the verbal relaxation group: not reported N randomized to control group: not reported N analyzed in music group: 34 N analyzed in the verbal relaxation group: 30 (not used in this review) N analyzed in control group: 34 Mean age: 53 years Sex: 65 (66.3%) female, 33 (33.7%) male Ethnicity: not reported Setting: outpatient Country: Taiwan |
|
| Interventions | 3 study groups:
Music selections provided: during the preparation period, participants listened to Songs of the Pacific ('Ambient Moods‐Whale Song') including the sound of sea waves, seabirds and whales. During the deep relaxation period, a meditation‐relaxation with taped recorded verbal instructions guided the participant. In the deep relaxation period, light music, Forest Piano with sounds of nature, such as wind, birds and piano were played. In the music listening period, Violin Rain and Aroma Lavender were played. Number of sessions: 1 Length of sessions: 60 min Categorized as music medicine. Although the authors wrote that the intervention used GIM, a music therapy intervention, the explanations provided indicated that participants listened through a pre‐recorded tape with verbal instructions rather than the intervention being implemented by a trained music therapist. |
|
| Outcomes | Anxiety (C‐STAI): post‐test scores Skin temperature and behavioural state: no means and SDs reported, therefore, not included in this review |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "To maintain good balance, a permuted block randomisation was used to randomise patients who met the inclusion criteria into experimental, comparison or control group. A random number sequence is generated. Each possible permuted block is assigned a number. Using each number in the random number sequence in turn selected the next block, determining the next participant allocations. The six block design contained equal proportions in each group with randomisation to remove sequence bias" (p. 991). |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | "Head phones were then applied for the intervention and comparison groups" (p. 992). Appeared that personnel may have been blinded but this was not clearly reported. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | "Equipment malfunction occurring in 12 subjects resulted in incomplete data. Thirteen subjects withdrew during the study owing to complaints of music preference or personal needs (e.g. toileting). Ninety‐eight subjects provided data for analysis" (pp. 992‐993). Attrition rate: 20.3% |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No conflict of interest reported |
Moradian 2015.
| Study characteristics | ||
| Methods | RCT 3‐arm parallel‐group design |
|
| Participants | Adults diagnosed with breast cancer Type of cancer: breast cancer Total N randomized: 99 N randomized to Nevasic audio group: 34 N randomized to music group: 32 N randomized to control group: 33 N analyzed in Nevasic audio group: 34 (not used in this review) N analyzed in music group: 32 N analyzed in control group: 33 Mean age: 49.6 years Sex: n = 99 (100%) females Ethnicity: not reported Setting: inpatient Country: Iran |
|
| Interventions | 3 study groups:
Music selections provided: pre‐selected music via CD player with headphones Number of sessions: Participant daily self‐administered music listening Length of sessions: not reported Categorized as music medicine |
|
| Outcomes | Mood (EORTC), QoL (EORTC ‐ Global Health Status), fatigue (EORTC), nausea (EORTC), pain (EORTC), physical functioning (EORTC): post‐test scores | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The participants were randomly assigned to one of the three treatment groups using a list (generated by nQuery Advisor program), done by a statistician who was independent of this study” (p. 283). |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel were not blinded. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | No objective measures were included. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Intention‐to‐treat analysis was used. However, by day 5, there was loss to follow‐up for 30 participants representing an attrition rate of 30%. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Unclear risk | "The authors declare no conflicts of interest." "This work was supported in part by funding from the Cancer Experiences Collaborative (CECo), a Research Collaborative funded by the National Cancer Research Institute in the UK; and Mashhad University of Medical Sciences in Iran. We are grateful to DAVAL Ltd, UK for providing us with Nevasic CDs and CD players free of charge for the purposes of this study" (p. 290). |
Mou 2020.
| Study characteristics | ||
| Methods | RCT 2‐arm parallel‐group design |
|
| Participants | Adult lung cancer patients undergoing peripherally inserted central catheter (PICC) placement procedure Type of cancer: squamous cell carcinoma (n = 114, 38%), lung adenocarcinoma (n = 104, 34.67%), small cell lung cancer (n = 38, 12.67%), other (n = 44, 14.66%) Total N randomized: 300 Total N analyzed: 300 N randomized to music group: 150 N randomized to control group: 150 N analyzed in music group: 150 N analyzed in control group: 150 Mean age: 57.31 years Sex: 59 (20%) females, 241 (80%) males Ethnicity: not reported Setting: inpatient Country: China |
|
| Interventions | 2 study groups: 1. Music group: music listening through headphones during the catheterization process 2. Control group: standard care Music selections provided: a slow rhythm, low tone, soothing melody with 60–80 beats/min or less was chosen. The participants selected their preferred music from three music libraries of 10 pieces of music each, including classical music, light music, and folk music. Number of sessions: 1 Length of sessions: duration of PICC placement, approximately 30 min Categorized as music medicine |
|
| Outcomes | Anxiety (NRS): post‐test scores HR, RR, SBP, DBP: post‐test scores |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The patients were randomly allocated to two groups using 304 random numbers produced by computer software, with 152 in each group" (p. 2). |
| Allocation concealment (selection bias) | High risk | "There was no blinding; both the researcher and the participant knew the allocation" (p. 2). |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | "There was no blinding" (p. 2). |
| Blinding of outcome assessment (detection bias) Objective outcomes | High risk | Since the participants in the music group wore headphones but those in the control group did not, outcome assessors were not blinded. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Flow chart did not include n analyzed; outcome table (Table 3) did not include information on n analysed. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | "The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. The author(s) received no financial support for the research, authorship, and/or publication of this article" (p. 8). |
Nguyen 2010.
| Study characteristics | ||
| Methods | RCT 2‐arm parallel‐group design |
|
| Participants | Children with cancer undergoing lumbar puncture (LP) Diagnosis: leukemia Total N randomized: 40 N randomized to music group: 20 N randomized to control group:20 N analyzed in music group: 20 N analyzed in control group: 20 Mean age: 9.1 years Sex: 15 (38%) females, 25 (62%) males Ethnicity: 40 (100%) Vietnamese Setting: inpatient Country: Vietnam |
|
| Interventions | 2 study groups:
Music selections provided: traditional Vietnamese songs and children's songs Number of sessions: 1 Length of sessions: music started 10 min before LP and continued for the length of the procedure. Duration of the procedure was on average 23 min. Categorized as music medicine |
|
| Outcomes | Anxiety (STAI‐Short form): post‐test scores Pain (NRS): post‐test scores Heart rate, respiratory rate, oxygen saturation level, SBP and DBP: post‐test scores |
|
| Notes | Measurements for these outcomes were also obtained during the procedure and were reported in the study report. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization was carried out using opaque envelopes, half of which contained a paper that said 'music' and half a paper that said 'no music'" (p. 147). |
| Allocation concealment (selection bias) | Low risk | Quote: "Randomization was carried out using opaque envelopes, half of which contained a paper that said 'music' and half a paper that said 'no music'" (p. 147). |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Personnel were blinded. Quote: "The researcher and the physician did not know to which group the patient belonged" (p. 148). Participants were not blinded since they knew whether they were listening to music or not. However, it was unlikely that this influenced their physiological responses. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | Blinding was used for objective outcomes. Quote: "The researcher and the physician did not know to which group the patient belonged. Heart rate (HR), blood pressure (BP), and oxygen saturation (SpO2) were recorded, and the respiratory rate (RR) was measured manually by the researcher" (p. 148). |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The flowchart indicated no subject loss. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | The authors declared no conflicts of interest with respect to the authorship or publication of this article. The authors received no financial support for the research or authorship of this article. |
O'Callaghan 2012.
| Study characteristics | ||
| Methods | RCT 2‐arm parallel‐group design |
|
| Participants | Adult cancer patients during initial radiotherapy treatment Type of cancer: prostate (n = 42, 42%), cervix (n = 10, 10%), endometrium (n = 9, 9%), breast (n = 7, 7%), lung (n = 5, 5%), other (n = 27, 27%) Total N randomized: 100 N randomized to music group: 50 N randomized to control group: 50 N analyzed in music group: 48 N analyzed in control group: 49 Mean age: 52.5 years Sex: 41 (41%) female, 59 (59%) male Ethnicity: not reported Setting: outpatient Country: Australia |
|
| Interventions | 2 study groups:
Music selections provided: participants were asked to bring their own preferred music to the first radiotherapy session Number of sessions: 1 Length of sessions: duration of the radiotherapy treatment Categorized as music medicine |
|
| Outcomes | Anxiety (STAI): post‐test scores | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "After obtaining informed consent from participants at radiotherapy planning stage, 100 participants were randomized into control (standard radiotherapy; no music) or intervention (standard radiotherapy plus self selected music) arms balanced by gender using a computer‐generated minimisation technique" (p. 474). |
| Allocation concealment (selection bias) | Low risk | Use of computer‐generated minimization technique |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | "The triangulation mixed method convergence model design comprised a single centre, non‐blinded parallel group, randomized controlled trial" (p. 474). |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | This study did not address objective outcomes. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "One control group and two music group participants withdrew prior to initial radiotherapy" (p. 474). Attrition rate = 3% |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | "Conflict of interest: The authors have no financial disclosures" (p. 473). |
Palmer 2015.
| Study characteristics | ||
| Methods | RCT 3‐arm parallel‐group design |
|
| Participants | Female cancer patients Type of cancer: breast cancer Total N randomized: 207 N randomized to live music group: 69 N randomized to recorded music group: 70 N randomized to control group: 68 N analyzed in live music group: 68 N analyzed in recorded music group: 68 N analyzed in control group: 65 Mean age: 59.4 years Sex: 207 (100%) females Ethnicity: 150 (74.6%) white, 46 (22.9%) black, 3 (1.5%) Asian, 2 (1%) Latino Setting: inpatient Country: USA |
|
| Interventions | 3 study groups:
Music selections provided: patient‐preferred music Number of sessions: 1 Length of sessions: 5 min Categorized as: music therapy |
|
| Outcomes | Anesthesia requirements: the amount of propofol needed to reach sedation of Bispectral Index (BIS) score of 70 Anxiety (Global Anxiety‐VAS): change scores Recovery time: recorded as the interval between surgery end time and the time when the participant had met discharge criteria according to hospital policy and procedure, determined by the recovery nurse Participant satisfaction (Likert scale) |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Participants were randomly assigned at a 1:1:1 ratio to a control or one of two experimental groups with use of an online randomisation module, which ensured adequate concealment" (p. 3163). |
| Allocation concealment (selection bias) | Low risk | "Participants were randomly assigned at a 1:1:1 ratio to a control or one of two experimental groups with use of an online randomisation module, which ensured adequate concealment" (p. 3163). "A permuted block randomisation scheme was used with random block sizes to prevent personnel from guessing the next assignment" (p. 3163). |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Music therapist and participants could not be blinded. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Intention‐to‐treat analysis was used for all analyses. 137 participants were randomized to the live music or the SC group; 133 completed all measurements. This represented a dropout rate of 3%. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | "Supported by Grant No. J0251, from The Kulas Foundation. Assistance with REDCap was provided through Clinical and Translational Science Collaborative Grant No. UL1TR 000439 at Case Western Reserve University. The Kulas Foundation had no role in the design or conduct of the study; the collection, management, analysis, or interpretation of the data; the preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication." |
Pedersen 2020.
| Study characteristics | ||
| Methods | RCT 2‐arm parallel‐group design |
|
| Participants | Adults undergoing endorectal ultrasonography (ERUS) examination Type of cancer: rectal (n = 126, 100%) Total N randomized: 126 Total N analyzed: 126 N randomized to music group: 66 N randomized to control group: 60 N analyzed in music group: 66 N analyzed in control group: 60 Mean age: 67.1 years Sex: 46 (36.5%) female, 80 (63.5%) male Ethnicity: not reported Setting: outpatient Country: Denmark |
|
| Interventions | 2 study groups: 1. Music group: listening to music 2. Control group: standard care Music selections provided: relaxing instrumental tunes were playing already when the participants in the music group entered the examination room, i.e. non‐lyrical music with 60‐80 beats per minute. Number of sessions: 1 Length of sessions: duration of procedure Categorized as music medicine |
|
| Outcomes | Pain during ERUS (VAS): only means were reported, no standard deviations. Pain during colonoscopy (VAS): only means were reported, no standard deviations. |
|
| Notes | A different number of male/female participants were reported in the abstract and results section compared to Table 3. This review used the data reported in Table 3. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Alternate assignment was used: "Randomization was carried out with a random number generator. An odd and even number would allocate patients to the non‐music and music groups, respectively" (p. 2). |
| Allocation concealment (selection bias) | High risk | Alternate assignment prevented allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Music was played using overhead sound system. Therefore, personnel were not blinded. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | No objective outcomes were included. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | Low risk | Participants were blinded to the study hypothesis: "The patients were informed that the questionnaire aimed to explore discomfort during the ERUS examination. They were not told that the investigation also focused on the possible beneficial effect of music during ERUS" (p. 2). |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rate: 0% |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | "The authors declare no conflict of interest" (p. 5). |
Pinto 2012.
| Study characteristics | ||
| Methods | CCT 2‐arm parallel‐group design |
|
| Participants | Adult breast cancer patients after surgery Type of cancer: breast Total N randomized: 29 N randomized to music group: 15 N randomized to control group: 14 N analyzed in music group: 15 N analyzed in control group: 14 Mean age: 58 years Sex: 29 (100%) female Ethnicity: Brazilians (n = 29, 100%) Setting: inpatient Country: Brazil |
|
| Interventions | 2 study groups:
Music selections provided: recording of The Four Seasons by Vivaldi Number of sessions: 2 Length of sessions: 20‐40 min Categorized as music medicine trial |
|
| Outcomes | Anxiety (STAI), temperature, blood pressure, heart rate, respiratory rate: only means were reported. Since no SDs were reported, we were not able to include this study in the meta‐analysis. | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | [translation] Patients whose hospital records end[ed] with even numbers were grouped in the experimental group. |
| Allocation concealment (selection bias) | High risk | Allocation concealment was not possible because of systematic method of group allocation. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel were not blinded. |
| Blinding of outcome assessment (detection bias) Objective outcomes | High risk | No blinding was used. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | Low risk | This study did not include subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There were no withdrawals. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No conflict of interest reported |
Porter 2018.
| Study characteristics | ||
| Methods | RCT 2‐arm parallel‐group design |
|
| Participants | Adults in inpatient hospice Type of cancer: No information provided in the article. Personal communication with author: all but 4 participants (7%) had cancer diagnosis. Therefore, study was included. Total N randomized: 51 Total N analyzed: 28 N randomized to music group: 25 N randomized to control group: 26 N analyzed in music group: 15 N analyzed in control group: 13 Mean age: 66.9 years SD (11.2) Sex: 36 (71%) females, 15 (29%) males Ethnicity: 51 (100%) white Setting: inpatient Country: Ireland |
|
| Interventions | 2 study groups: 1. Music therapy group: music therapy in an individual setting, delivered by a trained and registered music therapist 2. Control group: standard care Music selections provided: No information provided Number of sessions: 2 Length of sessions: 45 min Categorized as music therapy |
|
| Outcomes | QoL (McGill Quality of Life Questionnaire): change scores | |
| Notes | The protocol was initially planned for up to 6 sessions over 3 weeks. Due to very high attrition rate, the 3‐week protocol was deemed not feasible and only outcome data after 1 week were included in the study report. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Consenting patients were randomly allocated to the intervention or control group using a 1:1 allocation ratio. An independent statistician conducted blocked randomization with randomly permuted block sizes, which was used to fill opaque randomization envelopes" (p. 2). |
| Allocation concealment (selection bias) | Low risk | "An independent statistician conducted blocked randomization with randomly permuted block sizes, which was used to fill opaque randomization envelopes. These were stored in the clinical investigator’s locked filing cabinet at the hospice and used in sequence, thereby ensuring allocation concealment up to the point of randomization" (p. 2). |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The music therapist and participants could not be blinded in trials that use active music therapy interventions. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | No objective outcomes included |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | "Seventy one percent of participants were lost to follow up by week 3, the proposed primary endpoint. The primary endpoint was moved from week 3, when 71% were lost to follow up to week 1, when 33% were lost" (p. 4). |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | "The authors declare that they have no competing interests. This research was funded by a Northern Ireland Health and Social Care Research and Development Division Enabling Award. The funding body had no role in the design of the study, collection, analysis, interpretation of data or in writing the manuscript" (p. 8). |
Ramirez 2018.
| Study characteristics | ||
| Methods | RCT 2‐arm parallel‐group design |
|
| Participants | Adults in palliative care Type of cancer: not reported Total N randomized: 40 Total N analyzed: 40 N randomized to music group: 20 N randomized to control group: 20 N analyzed in music group: 20 N analyzed in control group: 20 Mean age: 69 years, SD (15) Sex: 13 (32.5%) females, 27 (67.5%) males Ethnicity: not reported Setting: inpatient Country: Spain |
|
| Interventions | 2 study groups: 1. Music therapy group: music therapy using a receptive song, an active song, and a relaxation/imaginative receptive intervention 2. Control group: participants were accompanied by the same music therapists for approximately 30 min in which they conversed freely about music and their music preferences Music selections provided: instrumental and vocal pieces in a variety of music genres (both classical and popular music) e.g. Canon de Pachelbel, La Bella Lola, Rien de rien, Hey Jude, Color Esperanza Number of sessions: 1 Length of sessions: 30 min Categorized as music therapy |
|
| Outcomes | Symptoms (Edmonton Symptom Assessment System): only P values reported Arousal and valence (EEG) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Patients were randomly assigned to the MT group or to the company group by using the method of randomly permuted blocks" (p. 2). |
| Allocation concealment (selection bias) | Unclear risk | No information about allocation concealment reported |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding was not possible in trials that use active music interventions. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Unclear risk | The authors did not state who administered or collected EEG data and whether they were blinded to treatment allocation. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rate: 0% |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | "This work was partly sponsored by Fundación Memora, the Spanish TIN project TIMUL (TIN2013‐48152‐C2‐2‐R), and the European Union Horizon 2020 research and innovation program under grant agreement No. 688269 (TELMI project)" (p. 6). |
Ratcliff 2014.
| Study characteristics | ||
| Methods | CCT 3‐arm parallel‐group design |
|
| Participants | Adult cancer patients who had undergone hematopoietic stem cell transplant Type of cancer: leukemia (n = 57, 63.3%), lymphoma (n = 13, 14.4%), other (n = 20, 22.2%) Total N randomized: 90 N randomized to music therapy group: 29 N randomized to unstructured music group: 30 (not used in this review) N randomized to control group: 31 N analyzed in music therapy group: 29 N analyzed in unstructured music group: 30 (not used in this review) N analyzed in control group: 31 Mean age: 44.3 years Sex: 47 (52%) female, 43 (48%) male Ethnicity: 59 (65.5%) white, 7 (7.8%) African‐American, 11 (12.2%) Latino, 4 (4.4%) Asian, 9 (10%) other Setting: outpatient or inpatient in transition to outpatient setting Country: USA |
|
| Interventions | 3 study groups:
Music selections provided: patient‐preferred music selected from a researcher provided database Number of sessions: 4 Length of sessions: 50 min Categorized as music therapy |
|
| Outcomes | Mood (POMS‐Short Form): change score (computed by JB) Quality of Life (FACIT‐G and FACIT‐BMT): change scores Cancer‐related symptoms (MD Anderson Symptom Inventory): not included in meta‐analysis |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Patients were randomly assigned to one of three groups: (1) ISO‐principle music therapy (MT) group, (2) unstructured music (UM) group, and (3) usual care (UC) control group" (p. 2). |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding of music therapist and participants was not possible. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | This study did not include objective outcomes. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | At the 1‐week follow‐up, there was 8.4% attrition. At the 4‐ week follow‐up, there was 27% attrition (additional data received from Dr. Lorenzo). |
| Selective reporting (reporting bias) | High risk | "...blood samples were drawn but results will be reported in future manuscript." (p. 3). |
| Other bias | Low risk | "This research was funded in part by a grant from The Maurice Amado Foundation, by Cancer Center Support Grant CA016672 from the National Institutes of Health, and by a cancer prevention fellowship for Chelsea Ratcliff supported by the National Cancer Institute Grant R25T CA057730, Shine Chang, Ph.D., Principal Investigator" (p. 8). |
Reimnitz 2018.
| Study characteristics | ||
| Methods | RCT 2‐arm parallel‐group design |
|
| Participants | Adults hospitalized on an oncology blood and marrow transplant unit Type of cancer: acute lymphoblastic leukemia (n = 1, 3%), acute myeloid leukemia, (n = 7, 20%), aplastic anaemia (n = 2, 5%), bone and marrow transplant (n = 2, 5%), cancer (sic)(n = 3, 8.5%), chronic myelomonocytic leukemia (CMML) (n = 2, 5%), CMML‐2 (n = 1, 3%), diffuse large B‐cell lymphoma (n = 1, 3%), graft‐versus‐host disease (GVHD) (n = 1, 3%), hemophagocytic lymphohistiocytosis (n = 1, 3%), leukemia (n = 4, 11%), lymphoma (n = 2, 5%), multiple myeloma (n = 4, 11%), myelodysplastic syndrome (n = 3, 8.5%), non‐Hodgkin’s lymphoma (n = 1, 3%), stem cell transplant (n = 1, 3%) Total N randomized: 38 Total N analyzed: 35 N randomized to music group: 20 N randomized to control group: 18 N analyzed in music group: 18 N analyzed in control group: 17 Mean age: 58.03 years Sex: 20 (57%) females, 14 (43%) males Ethnicity: 1 (3%) Middle American (sic), 30 (86%) Caucasian, 4 (11%) not specified Setting: inpatient Country: USA |
|
| Interventions | 2 study groups: 1. Music therapy group: listening to patient‐preferred live music 2. Control group: standard care wait‐list control Music selections provided: not reported Number of sessions: 1 Length of sessions: 30 min Categorized as music therapy |
|
| Outcomes | Energy (Lee Visual Analogue Scale for Fatigue): post‐test scores Fatigue (Lee Visual Analogue Scale for Fatigue): post‐test scores Pain (NRS): post‐test scores |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Participants were randomly assigned via a computer program to either the experimental group (n = 18) or wait‐list control group (n = 17)" (p. 4). |
| Allocation concealment (selection bias) | Unclear risk | Information about allocation concealment was not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding was not possible in studies with active music intervention. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | No objective outcomes included |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition: n = 3 (7.8%) |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | "No potential conflict of interest was reported by the authors" (p. 12). |
Robb 2008.
| Study characteristics | ||
| Methods | CCT 3‐arm parallel‐group design |
|
| Participants | Children with cancer Diagnosis: no further details provided Total N randomized: 83 N randomized to active music engagement group: 27 N randomized to music listening group: 28 (not included in this review) N randomized to control group: 28 N analyzed in active music engagement group: 27 N analyzed in music listening group: 28 (not included in this review) N analyzed in audiobook control group: 28 Mean age: not reported Sex: not reported Ethnicity: not reported Setting: inpatient Country: USA |
|
| Interventions | 2 study groups:
Music selections provided: children's songs Number of sessions: 1 Length of sessions: 30 min Categorized as music therapy |
|
| Outcomes | Positive affect (behavioral form): post‐test scores Active engagement (behavioral form): post‐test scores Initiation (behavioral form): post‐test scores |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "[P]articipants were not allocated to the research conditions at random, but were sequentially assigned to one of three study conditions" (Erratum published online). |
| Allocation concealment (selection bias) | High risk | Quote: "Participants were sequentially assigned one of three study conditions. Assignment was done in the same manner at each hospital to maintain an equal number of participants in each condition across all sites." |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The music therapist could not be blinded given the interactive nature of the music therapy session. It was unclear whether the children were blinded to the purpose of the study. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | This study did not address objective outcomes. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Outcome assessors were not blinded. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | No data records were kept on number of subjects approached, consented and withdrawn (personal communication with principal investigator). |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | "This research study was sponsored through a National Academy of Recording Arts and Sciences (NARAS) grant awarded to the American Music Therapy Association (AMTA). This study received additional support through an institutional post‐doctoral fellowship, CA 117865‐O1A1. |
Robb 2014.
| Study characteristics | ||
| Methods | RCT 2‐arm parallel‐group design |
|
| Participants | Adolescents and young adults undergoing hematopoietic stem cell transplant Type of cancer: leukemia ( n = 53, 46.4%), lymphoma ( n = 28, 25.0 %), solid tumor ( n = 32, 28.6%) Total N randomized: 113 N randomized to music group: 59 N randomized to control group: 54 N analyzed in music group: 40 N analyzed in control group: 40 Mean age: 17.3 years Sex: 42.5% female, 57.5% male Ethnicity: 12 (10.6%) African‐American, 66 (58.4%); white, 23 (20.4%); mixed ethnicity, 7 (6.2%); other, 5 (4.4%); Setting: inpatient Country: USA |
|
| Interventions | 2 study groups:
Music selections provided: participants created their own songs with the music therapist. Number of sessions: 6 Length of sessions: not reported Categorized as music therapy |
|
| Outcomes | Illness‐related distress (McCorkle Symptom Distress Scale), coping (Jalowiec Coping Scale‐Revised), spiritual perspective (Reed Spiritual Perspective Scale); social integration (Perceived Social Support), family environment (Family Adaptability/Cohesion Scale), hope‐derived meaning (Herth Hope Index), self transcendence (Reed Self Transcendence Scale), and resilience (Haase Resilience in Illness Scale): effect sizes | |
| Notes | Effect sizes were reported in the publication. No means or SDs were reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Participants were randomised to the TMV or low‐dose, control group using 24 strata (8 sites individually stratified by 3 age groups: 11‐14, 15‐18, and 19‐24 years)" (p. 911). |
| Allocation concealment (selection bias) | Low risk | "We used central randomisation by a third party. So after a participant completed the baseline measures, the computer triggered randomisation. The project manager is then notified electronically (e‐mail generation) about the participant's group assignment" (personal communication with investigator). |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Music therapist and participants could not be blinded. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | This study did not address objective outcomes. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | "An intent‐to‐treat analysis was performed in which all available questionnaire data at T2 and T3 were used, and participants were analysed according to their assigned group regardless of their degree of adherence to the protocols for the intervention and low‐dose control groups" (p. 913‐4). Dropout rate was 28% at T2 and 41% at T3. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | "This work as funded by the National Institute of Nursing Research (R01NR008583) and the National Cancer Institute (U10CA098543 and U10CA095861)" (p. 916). |
Robb 2017.
| Study characteristics | ||
| Methods | RCT 2‐arm parallel‐group design |
|
| Participants | Parents and young children with cancer Type of cancer: leukemia (n = 9, 56%), tumor (n = 7, 44%) Total N dyads randomized: 16 Total N dyads analyzed: 16 N dyads randomized to music group: 9 N dyads randomized to control group: 7 N dyads analyzed in music group: 9 N dyads analyzed in control group: 7 Mean age child: 5.5 years Mean age parent: 33.85 years Sex child: 8 (50%) females, 8 (50%) males Sex parent: not reported Ethnicity child: 2 (13%) Hispanic or Latino, 13 (81%) not Hispanic or Latino, 1 (6%) unknown Race child: 13 (81%) white, 1 (6%) African‐American, 2 (13%) other Parent Ethnicity: 1 (6%) Hispanic or Latino, 7 (44%) not Hispanic or Latino, 8 (50%) unknown Parent Race: 7 (44%) white, 0 (0%) African‐American, 1 (6%) other, 8 (50%) unknown or not reported Setting: inpatient Country: USA |
|
| Interventions | 2 study groups: 1. Music therapy group: parent‐delivered Active Music Engagement intervention 2. Control group: audio‐storybooks Music selections provided: not reported Number of sessions: 3 Length of session: 45 min Categorized as music therapy |
|
| Outcomes | Emotional distress (POMS‐SF): post‐test scores Emotional distress (IES‐Revised): post‐test scores Child engagement (Behave coding form): post‐test scores Child distress (Facial affect‐behave coding form): post‐test scores |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Randomization assignments in blocks of 2 or 4 were created by the biostatistician using a computer" (p. 209). |
| Allocation concealment (selection bias) | Low risk | "Assignments were made by the project manager at enrollment using sealed numbered opaque envelopes" (p. 210). |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding was not possible in studies that used active music interventions. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | No objective outcomes included |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rate: 0% |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | "This work was funded by the first author’s institutional CTSI career award NIH/PHS (NCCR) KL2RR025760‐02 and IUPUI RESPECT center pilot study grant. Conflicts of interest: None declared" (p. 218). |
Romito 2013.
| Study characteristics | ||
| Methods | CCT 2‐arm parallel‐group design |
|
| Participants | Adult breast cancer patients receiving chemotherapy Type of cancer: localised tumor (n = 50, 80.6%), metastatic tumor (n = 12, 19.4%) Total N randomized: 62 Total N analyzed: 62 N randomized to music group: 31 N randomized to control group: 31 N analyzed in music group: 31 N analyzed in control group: 31 Mean age: 54.2 years Sex: 62 (100%) female Ethnicity: not reported Setting: outpatient Country: Italy |
|
| Interventions | 2 study groups:
Music selections provided: active singing using vocal holding techniques Number of sessions: 1 Length of sessions: 150 min Categorized as music therapy |
|
| Outcomes | Depression, anxiety, anger, stress, need for help: only means were reported (no standard deviations). Therefore, the results could not be included in the meta‐analysis. | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "The patients gave informed consent to participate and were quasi‐randomly assigned to the experimental and control arms of the study" (p. 439). "On Mondays and Wednesdays of each week, the first consecutive eligible patients of the day who gave their informed consent to participate in the study were placed in the same room for chemotherapy infusion and took part in the experimental group. On Tuesdays and Thursdays the same procedure was followed and these patients were assigned to the control groups. 31 patients were allocated to the experimental group and 31 to the control group" (p. 439). |
| Allocation concealment (selection bias) | High risk | Alternate assignment prohibited allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding of music therapist and participants was not possible. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | This study did not address objective outcomes. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not reported |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | "The authors declare that there is no conflict of interest" (p. 443). |
Rosenow 2014.
| Study characteristics | ||
| Methods | RCT 2‐arm parallel‐group design |
|
| Participants | Adult patients recovering from a bone marrow transplant Type of cancer: leukemia (n = 12, 66.7%), multiple melanoma (n = 5, 27.8%), unknown (n = 1, 5.6%) Total N randomized: 18 N randomized to music group: 8 N randomized to control group: 10 N analyzed in music group: 8 N analyzed in control group:10 Mean age: 53.6 years Sex: 100% female Ethnicity: 2 (11.1%) African‐American, 1 (5.6%) Asian‐American, 14 (77.8%) white, 1 (5.6%) Latino Setting: inpatient Country: USA |
|
| Interventions | 2 study groups:
Music selections provided: music therapist played patient‐preferred live music with guitar and voice. Number of sessions: 1 Length of sessions: 45 min Categorized as music therapy |
|
| Outcomes | Fatigue (Brief Fatigue Inventory): change scores | |
| Notes | This manuscript included 2 studies. Only the second study was used in this review as the first study was not an RCT or CCT. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "After obtaining consent to participate in the study, the researchers consulted a randomized list to ascertain each participant’s condition in the study" (p. 68). |
| Allocation concealment (selection bias) | High risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding of music therapist and participants was not possible. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | This study did not address objective outcomes. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not reported |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No conflict of interests reported |
Rossetti 2017.
| Study characteristics | ||
| Methods | RCT 2‐arm parallel‐group design |
|
| Participants | Cancer patients undergoing simulation for radiation therapy Type of cancer: breast (n = 38, 48.7%), head and neck (n = 40, 51.3%) Total N randomized: 78 Total N analyzed: 78 N randomized to music group: 39 N randomized to control group: 39 N analyzed in music group: 39 N analyzed in control group: 39 Mean age: Median age reported 58.5 years; range 26‐77 (51) Sex: 51 (65.4%) females, 27 (34.6%) males Ethnicity: not reported Setting: outpatient Country: USA |
|
| Interventions | 2 study groups: 1. Music therapy group: listening to music during simulation after consultation with music therapist 2. Control group: standard care Music selections provided: Participant‐identified music was retrieved from an mp3 music file database kept on an Apple MacBook Pro organized in iTunes, version 12.1, containing > 20,000 individual pieces spanning a broadly diverse collection of culture‐centered music genres. Approximately 40 min of music was chosen based on each participant’s preferences. Number of sessions: 1 Length of sessions: 20 min before start of RT and then during RT Categorized as music therapy |
|
| Outcomes | Anxiety (STAI‐S): post‐test scores and change score Distress (Symptom Distress Thermometer): post‐test scores and change score |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Subjects were randomized following a randomization schedule generated by a biostatistician, in the order in which they were accrued into the study" (p. 104). |
| Allocation concealment (selection bias) | Unclear risk | No information about allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding was not possible in studies with active music interventions. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | No objective outcomes included |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rate: 0% |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | "Conflict of interest: none" (p. 103) |
Shaban 2006.
| Study characteristics | ||
| Methods | CCT 2‐arm parallel‐group design |
|
| Participants | Adults with cancer with pain Diagnosis: no further details available in translation of study report Total N randomized: 100 N randomized to music group: 50 N randomized to control group: 50 N analyzed in music group: 50 N analyzed in control group: 50 Mean age: not reported Sex: not reported Ethnicity: 100 (100%) white Setting: unclear if inpatient or outpatient (treatment provided in hospital) Country: Iran |
|
| Interventions | 2 study groups:
Music selections provided: 3 types of music (no further detail provided in translation of study report) Number of sessions: 3 Length of sessions: 30 min Categorized as music medicine |
|
| Outcomes | Pain (VAS): post‐test scores | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Alternate assignment. Quote: "The first patient included in one group and second person to another group" (personal communication with principal investigator). |
| Allocation concealment (selection bias) | High risk | Alternation method |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Personnel and participants were not blinded. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | This study did not address objective outcomes. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No dropouts reported. However, it was unlikely that no attrition occurred in a study with this sample size. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Unclear risk | Funding information and conflict of interest statement were not provided in the translation of the study report. |
Smith 2001.
| Study characteristics | ||
| Methods | RCT 2‐arm parallel‐group design |
|
| Participants | Adults with cancer receiving radiation therapy Diagnosis: prostate (n = 24, 55%), lung (n = 6, 14%), head or neck (n = 4, 9%), colorectal (n = 4, 9%), squamous cell skin (n = 2, 5%), stomach (n = 1, 2%), melanoma (n = 1, 2%) Total N randomized: 44 N randomized to music group: 20 N randomized to control group: 24 N analyzed in music group: 19 N analyzed in control group: 23 Mean age: 62.8 years Sex: 42 (100%) males Ethnicity: 31 (74%) white, 5 (12%) black, 5 (12%) Latino, and 1 (2%) other Setting: outpatient Country: USA |
|
| Interventions | 2 study groups:
Music selections provided: participants were asked to select from rock and roll, big band, country and western, classical, easy listening, Spanish, or religious music. Number of sessions: daily for duration of treatment Length of sessions: 30 min Categorized as music medicine |
|
| Outcomes | Anxiety (STAI‐S): post‐test scores after 1 week of music interventions | |
| Notes | Post‐test scores for week 3 and week 5 were also reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A biostatistician prepared a randomisation list using a computer. Only one member of the research team had access to this list of case numbers and randomisation assignments, which was maintained in a locked filing cabinet" (p. 856). |
| Allocation concealment (selection bias) | Low risk | Central randomisztion. Quote: "At the time the patient agreed to participate in the study and the consent form was signed, the research associate called the registrar to obtain the patient's assigned case number and randomisation group". |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Participants were not blinded. It was unclear whether the personnel were blinded. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | This study did not address objective outcomes. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rate: 5% Quote:"Two patients, one from each group, were excluded from final analysis because of incomplete data". |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | This study was supported, in part, by a grant from Sigma Theta Tau, Delta Beta Chapter, of the College of Nursing at the University of South Florida. |
Stordahl 2009.
| Study characteristics | ||
| Methods | CCT 2‐arm parallel‐group design |
|
| Participants | Women at the completion of treatment for breast cancer Type of cancer: breast (n = 20, 100%) Total N randomized: 20 Total N analyzed: 20 N randomized to music group: 10 N randomized to control group: 10 N analyzed in music group: 10 N analyzed in control group: 10 Mean age: 48.35 years Sex: n = 20 (100%) females Ethnicity: n = 9 (45%) Latino, n = 6 (30%) white, n = 5 (25%) African‐American/Caribbean black Setting: outpatient Country: USA |
|
| Interventions | 2 treatment conditions:
Music selections provided: contemporary sedative music was paired with standard spoken relaxation directives Number of sessions: 4 Length of sessions: 20‐30 min Categorized as music therapy trial |
|
| Outcomes | Depression [Center for Epidimiologic Diseases ‐ Depression Scale (CES‐D)]: post‐test scores Mood (POMS ‐ Short Form): post‐test scores |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants and personnel could not be blinded. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | This study did not include objective measures. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not reported |
| Selective reporting (reporting bias) | Low risk | No indication of selective reporting |
| Other bias | Low risk | No indication of conflict of interest |
Straw 1991.
| Study characteristics | ||
| Methods | RCT 2‐arm parallel‐group design |
|
| Participants | Adults with cancer receiving chemotherapy Diagnosis: no further details provided Total N randomized: unclear N randomized to music group: unclear N randomized to control group: unclear N analyzed in music group: 9 N analyzed in control group: 10 Mean age: 49 years Sex: 13 (27%) females, 26 (73%) males Ethnicity: not provided Setting: unclear if inpatient or outpatient Country: USA |
|
| Interventions | 2 study groups:
Music selections provided: a music tape was created by the researcher. If the participants disliked the music, they could listen to a tape of their own. Number of sessions: participants listened to tape during chemotherapy treatments and at home. Participants were encouraged to listen to the tape each day. Length of sessions: 30‐40 min Categorized as music medicine |
|
| Outcomes | Anxiety (STAI‐S): post‐test scores QoL (Functional Living Index): post‐test scores Level of control: not included in this review |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Random assignment of subjects to condition involved choosing pieces of paper from a box. Half of the pieces had 'one' written on them, and half a 'two'. In this way, subjects had an equal chance being assigned to either group". |
| Allocation concealment (selection bias) | Low risk | Not reported but we assumed that lots were drawn in the presence of the subjects. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Personnel and participants were not blinded. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | This study did not address objective outcomes. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | It was unclear whether the number of participants analyszd equalled the number of participants recruited. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | — |
Tuinmann 2017.
| Study characteristics | ||
| Methods | RCT 2‐arm parallel‐group design |
|
| Participants | Patients with high‐dose chemotherapy and stem cell support Type of cancer: Hodgkin (n = 1, 5%), non‐Hodgkin (n = 7, 10.6%), myeloma (n = 36, 54.5%), testicular (n = 16, 24.2%), leukemia (n = 2, 3%), other (n = 4, 6.1%) Total N randomized: 66 Total N analyzed: 29 N randomized to music group: 33 N randomized to control group: 33 N analyzed in music group: 15 N analyzed in control group: 14 Mean age: 50.6 years Sex: 24 (36.4%) females, 42 (63.3%) males Ethnicity: not reported Setting: inpatient Country: Germany |
|
| Interventions | 2 study groups: 1. Music therapy group: music therapy delivered by a trained music therapist 2. Control group: standard care Music selections provided: not reported Number of sessions: average of 8 Length of sessions: 20‐50 min Categorized as music therapy |
|
| Outcomes | Depression (HADS): effect size Anxiety (HADS): effect size Emotional functioning (EORT subscale): effect size QoL (EORTC QLQ‐C30): effect size Pain (EORT subscale): effect size IgA, T4, T8, NK, Ig‐G: effect size Physical functioning (Karnofsky Performance Score): effect size |
|
| Notes | Since only effect sizes were reported, no data were included in the meta‐analyses. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information about randomization method |
| Allocation concealment (selection bias) | Unclear risk | No information about allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding was not possible in studies with active music interventions. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Unclear risk | No information about blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition: n = 13 (19.6%) |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | "This study was sponsored by the ‘Else‐Kröner‐Fresenius‐Stiftung’ from 01.11.2008‐31.10.2010 (P33/08//A19/08) and 01.11.2010‐ 31.10.2012 (P23/10//A34/10). The authors have declared that there is no conflict of interest" (p. 383). |
Vachiramon 2013.
| Study characteristics | ||
| Methods | RCT 2‐arm parallel‐group design |
|
| Participants | Adults with skin cancer Type of cancer: skin (100%) Total N randomized: 100 Total N analyzed: 100 N randomized to music group: 50 N randomized to control group: 50 N analyzed in music group: 50 N analyzed in control group: 50 Mean age: 64.3 years Sex: 33 (33%) female, 67 (67%) male Ethnicity: not reported Setting: inpatient Country: USA |
|
| Interventions | 2 study groups:
Music selections provided: participants chose a musical genre, artist, or track, which was entered into internet radio (Pandora Media, Inc., Oakland, CA), which creates a mix of music according to the listener's preferences Number of sessions: 1 Length of sessions: 15‐60 min Categorized as music medicine trial |
|
| Outcomes | Anxiety (STAI): post‐test scores | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Using a randomisation table (a table of random numbers), eligible subjects were randomly assigned into one of two groups: a control group with no music or a treatment group that listened to the music of their choice during surgery" (p. 299). |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants was not possible. Personnel were not blinded. "This study was designed as an open‐labelled randomized controlled trial" (p. 299). |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | This study did not address objective outcomes. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No attrition |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No conflict of interest reported |
Verstegen 2016.
| Study characteristics | ||
| Methods | RCT 2‐arm parallel‐group design |
|
| Participants | Adults on blood and marrow transplant unit Type of cancer: adrenoleukodystrophy (n = 1, 10%), acute myeloid leukemia (n = 2, 20%), chronic lymphocytic leukemia (CLL) (n = 1, 10%), non‐Hodgkin (n = 4, 40%), uterine (n = 1, 10%), not specified (n = 1, 10%) Total N randomized: 12 Total N analyzed: 10 N randomized to music group: 6 N randomized to control group: 6 N analyzed in music group: 5 N analyzed in control group: 5 Mean age: 62.3 years Sex: 7 (70%) females, 3 (30%) males Ethnicity: 9 (90%) Caucasian, 1 (10%) other Setting: inpatient Country: USA |
|
| Interventions | 2 study groups: 1. Music therapy group: individualized music therapy (patient‐preferred live music) 2. Control group: standard care wait‐list control Music selections provided: hope‐based song menu Number of sessions: 2 Length of sessions: 30‐60 min Categorized as music therapy |
|
| Outcomes | Hope (Herth Hope Index): post‐test scores Pain (11‐point Likert‐type pain scale): post‐test scores |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Participant conditions were randomized via computer‐based randomization generator" (p. 12). |
| Allocation concealment (selection bias) | Unclear risk | No information about allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding was not possible in studies with active music interventions. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | No objective outcomes included |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition: n = 2 (16.6%) |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | Thesis acknowledgment section free from wording indicating other sources of bias |
Verstegen 2018.
| Study characteristics | ||
| Methods | RCT 2‐arm parallel‐group design |
|
| Participants | Adults hospitalized for bone marrow transplantation Type of cancer: aplastic anemia (n =1, 7.7%), acute myeloid leukemia (n = 3, 23.1%), acute promyelocytic leukemia (n = 1, 7.7%), chronic myeloid leukemia (n = 2, 15.4%), myelodysplastic syndromes (n = 1, 7.7%), Hodgkin’s lymphoma (n = 1, 7.7%), multiple myeloma (n = 1, 7.7%), leukemia (not specified) (n = 3, 23.1%) Total N randomized: 13 Total N analyzed: 13 N randomized to music group: 6 N randomized to control group: 7 N analyzed in music group: 6 N analyzed in control group: 7 Mean age: 52.66 years Sex: 7 (54%) females, 6 (46%) males Ethnicity: 13 (100%) Caucasian Setting: inpatient Country: USA |
|
| Interventions | 2 study groups: 1. Music therapy group: music therapy (patient‐preferred live music) 2. Control group: standard care Music selections provided: not reported Number of sessions: 1 Length of sessions: 20‐30 min Categorized as music therapy |
|
| Outcomes | Wide awake/drowsy (The Quick Mood Scale (QMS) derived from POMS): post‐test scores Relaxed/anxious (QMS): post‐test scores Cheerful/depressed (QMS): post‐test scores, change score computed by JB Friendly/aggressive (QMS): post‐test scores Clear headed/confused (QMS): post‐test scores Well‐coordinated/clumsy (QMS): post‐test scores Pain (NRS): post‐test scores |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Patients were randomly assigned via a computer program to experimental or control conditions in this pilot effectiveness study" (p. 422). |
| Allocation concealment (selection bias) | Unclear risk | No information about allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding was not possible in studies with active music interventions. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | No objective outcomes included |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information about attrition |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Unclear risk | No financial or conflict of interest statements provided in the article |
Wan 2009.
| Study characteristics | ||
| Methods | RCT 2‐arm parallel‐group design |
|
| Participants | Adult cancer patients with pain Diagnosis: cancer of the lung, liver, gastrointestinal, lymphoma Total N randomized: 136 Total N analyzed: 136 N randomized to music group: unclear N randomized to control group: unclear N analyzed in music group: 65 N analyzed in control group: 71 Mean age: 52.5 years Sex: 76 (56%) females, 60 (44%) males Ethnicity: 136 (100%) Chinese (Han) Setting: inpatient Country: China |
|
| Interventions | 2 study groups:
Music selections provided: no details on the music reported Number of sessions: 1 Length of sessions: 30 min Categorized as music medicine |
|
| Outcomes | Depression (CES‐D): post‐test scores Anxiety (STAI‐S): post‐test scores Pain (NRS): post‐test scores |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Translation quote: "Simple randomizations" |
| Allocation concealment (selection bias) | High risk | Not used |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Personnel and participants were not blinded. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | This study did not address objective outcomes. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | It was unclear whether the number of participants analyzed equalled the number of participants recruited. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Unclear risk | Funding information and conflict of interest statement were not provided in the translation of the study report. |
Wang 2015.
| Study characteristics | ||
| Methods | RCT 2‐arm parallel‐group design |
|
| Participants | Adults after surgery for lung cancer Type of cancer: lung (n = 60, 100%) Total N randomized: 60 Total N analyzed: 60 N randomized to music group: 30 N randomized to control group: 30 N analyzed in music group: 30 N analyzed in control group: 30 Mean age: 53.65 Sex: 25 (41%) females, 35 (58%) males Ethnicity: not reported Setting: inpatient Country: China |
|
| Interventions | 2 study groups:
Music selections provided: Western classical music and Chinese music Number of sessions: 5 pre‐surgery music‐assisted relaxation and 4 postsurgery in ICU Length of sessions: pre‐surgery 15 min, postsurgery 1 h Categorized as music therapy |
|
| Outcomes | Pain Self Rating Anxiety Scale (SAS) and visual analogue scale (VAS): pre‐test, post‐SBP, DBP, heart rate (HR), pulse oxygen saturation (SpO2), respiratory rate, SAS score, VAS score, drug dose, and total consumption of sufentanil at 4, 8, 12, 16, 20, and 24 h were recorded postoperatively. | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Consecutive patients were recruited and randomly assigned to the MT group and control (C) group by using a random‐numbers table and sealed sequential envelopes prepared by an independent statistician" (p. 668). |
| Allocation concealment (selection bias) | Low risk | "Consecutive patients were recruited and randomly assigned to the MT group and control (C) group by using a random‐numbers table and sealed sequential envelopes prepared by an independent statistician" (p. 668). |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel were not blinded. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | For objective outcomes, the following was reported: "All postoperative measurements were evaluated and confirmed by two independent observers. Observations were compared between them, and differences were solved by discussion" (p. 669). Therefore, rating of low risk for objective outcomes |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There were no withdrawals. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | "The study was funded by grant no. 2012FJ2004 from the Department of Science and Technology of Hunan Province, China". "No competing financial interests exist" (p. 672). |
Warth 2015.
| Study characteristics | ||
| Methods | RCT 2‐arm parallel design |
|
| Participants | Adults in palliative care Type of cancer: breast (n = 17, 20%), pancreatic (n = 11, 13%), ovarian (n = 7, 8%), prostate (n = 6, 7%), other (n = 43, 51%). With two exceptions (2.5%), all patients were suffering from malignant tumor diseases. Total N randomized: 84 Total N analyzed: 84 N randomized to music group: 42 N randomized to control group: 42 N analyzed in music group: 42 N analyzed in control group: 42 Mean age: 63 years, SD (13.4) Sex: 60 (71%) females, 24 (29%) males Ethnicity: not reported Setting: palliative care Country: Germany |
|
| Interventions | 2 study groups: 1. Music therapy group: live music‐based relaxation exercises 2. Control group: listened to a verbal relaxation exercise, 20‐min excerpt from the MIndfulness‐Based Stress Reduction (MBSR), played through headphones. Music selections provided: Taking account of the participant’s breathing pattern, the volume, dynamics, and intensity of the monochord playing were increased and vocal improvisation was begun in Ionian or Mixolydian mode. Number of sessions: 2 Length of sessions: 30 min Categorized as music therapy |
|
| Outcomes | Relaxation (VAS): post‐test scores Well‐being (VAS): post‐test scores QoL Overall (EORTC QLQ‐C15 PAL): post‐test scores QoL Fatigue: post‐test scores, change score Pain (VAS): post‐test scores Heart rate variability: post‐test scores Blood volume pulse amplitude: post‐test scores |
|
| Notes | Because the control treatment arm used verbal relaxation exercise, the results of this study were not included in the music intervention versus standard care alone comparison. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The allocation sequence was compiled before the beginning of the study, using computerized block randomization (block size: 6)" (p. 789). |
| Allocation concealment (selection bias) | Low risk | "Participants were allocated to one of the two study groups using sealed, sequentially numbered envelopes provided by the study assistant" (p. 789). |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding was not possible in studies with active music interventions. |
| Blinding of outcome assessment (detection bias) Objective outcomes | High risk | "No further blinding methods (of therapists or assessors) could be implemented" (p. 789). |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rate for primary outcome: n = 6 (7.1%) |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | "The authors declare that no conflict of interest exists" (p. 792). |
Wren 2019.
| Study characteristics | ||
| Methods | RCT 3‐arm parallel‐group design |
|
| Participants | Adults undergoing biopsy and breast cancer surgery Type of cancer: breast (n = 56, 100%) Total N randomized: 56 (138 consented to participate prior to biopsy. Among consented participants, 56 received an abnormal biopsy result and subsequently underwent surgery) Total N analyzed: 47 (19 not included in this review) N randomized to music group: 46 N randomized to meditation 45 (not included in this review) N randomized to control group: 44 N analyzed in music group: 12 N analyzed in meditation group: 19 (not included in this review) N analyzed in control group: 16 Mean age: 56 years Sex: 56 (100%) females, (0%) males Ethnicity: 39 (73.6%) white, 12 (22.6%) African‐American, 2 (3.8%) Asian‐American Setting: outpatient Country: USA |
|
| Interventions | 2 study groups: 1. Music group: participants listened to music using headphones/earbuds. 2. Meditation group (not included in this review) 3. Control group: standard care Music selections provided: not reported Number of sessions: not reported (encouraged daily home practice) Length of sessions: not reported (encouraged listening to 20 min of music daily) Categorized as music medicine |
|
| Outcomes | Anxiety (STAI‐S): post‐test scores, change scores computed by JB Self‐compassion (Self‐compassion scale‐short form, SCS‐SF): post‐test scores Fatigue (FACIT Fatigue scale): post‐test scores, change scores computed by JB Breast pain (2‐items adapted from BPI): post‐test scores (included in the pain outcome meta‐analysis) Body pain (4‐item Brief Pain Inventory): post‐test scores (not included in the pain outcome meta‐analysis) HR, SBP, DBP: post‐test scores |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Participants were then randomized to one of the three study conditions with equal allocation (stratified by ultrasound vs. stereotactic‐guided biopsy) using the program Block Stratified Randomization Version 5.0" (p. 3584). |
| Allocation concealment (selection bias) | Unclear risk | No information about allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Both the meditation and music group participants wore headphones but standard care participants did not during the biopsy. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Unclear risk | Unclear whether outcome assessment personnel were blinded |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition: n = 5 (8.9%) |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | "The authors declare that there are no conflicts of interest" (p. 3591). |
Xie 2001.
| Study characteristics | ||
| Methods | CCT (randomization method unclear) 2‐arm parallel‐group design |
|
| Participants | Adults with cancer receiving chemotherapy Diagnosis: no further details available in the translation of the study report Total N randomized: 260 Total N analyzed: 260 N randomized to music group: 124 N randomized to control group: 136 N analyzed in music group: 124 N analyzed in control group: 136 Mean age: not reported Sex: not reported Ethnicity: 260 (100%) Chinese Setting: not reported Country: China |
|
| Interventions | 2 study groups:
Music selections provided: no details provided Number of sessions: 2 times per day for 20 days Length of sessions: 60 min Categorized as music medicine |
|
| Outcomes | Physical functioning (Karnofsky Performance Scale): post‐test scores QoL (QoL Questionnaire for Chinese cancer patients): change scores were computed by JB to allow for computation of pooled effect size (SMD) with other studies that reported change scores. |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Personnel and participants were not blinded. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | This study did not address objective outcomes. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | It was unclear whether the number of participants analyzed equalled the number of participants recruited. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Unclear risk | Funding information and conflict of interest statement were not provided in the translation of the study report. |
Yates 2015.
| Study characteristics | ||
| Methods | RCT 2‐arm parallel‐group design |
|
| Participants | Adult Type of cancer: appendix (n = 1, 3%), bladder (n = 1, 3%), breast (n = 2, 7%), colon/rectal (n = 5, 19%), liposarcoma (n = 1, 3%), melanoma (n = 1, 3%), ovarian (n = 2, 7%), pancreatic (n = 1, 3%), papillary (n = 1, 3%), tumor (reported as such in article, no further detail is provided) (n = 2, 7%), uterine (n = 3, 11%), other (n = 6, 23%) Total N randomized: 26 Total N analyzed: 22 N randomized to music group: 13 N randomized to control group: 13 N analyzed in music group: 11 N analyzed in control group: 11 Mean age: 57.59 Sex: 22 ( 84 % ) females, 4 ( 15 %) males Ethnicity: 2 (7%) Latino, 21 (80%) white, 3 (11%) other Setting: inpatient Country: USA |
|
| Interventions | 2 study groups:
Music selections provided: patient‐preferred live music Number of sessions: 1 Length of sessions: 20‐30 min Categorized as music therapy |
|
| Outcomes | 6 mood states measured by the Quick Mood Scale (QMS), namely wide awake/drowsy, relaxed/anxious, cheerful/depressed, friendly/aggressive, clearheaded/confused, well‐coordinated/clumsy. Only the relaxed/anxious and cheerful/depressed states were included in this review: post‐test scores | |
| Notes | Means and standard errors were reported in the journal article. Standard deviations were obtained from the primary author. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “We used a computer program on randomizer.org to create a series of 0 and 1. A 0 meant a participant was in the control group” (personal communication with chief investigator). |
| Allocation concealment (selection bias) | High risk | No allocation concealment used (personal communication with chief investigator) |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Music therapist and participants could not be blinded. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | This study did not include objective outcomes. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Out of 26 participants, 4 were lost: “Four participants were not included in data analyses as two participants fell asleep, one participant had a visit from the doctor, and one participant did not complete the form correctly" (p. 59). Attrition rate: 8.5% |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No conflict of interest reported |
Zhao 2008.
| Study characteristics | ||
| Methods | RCT 2‐arm parallel‐group design |
|
| Participants | Adults with cancer undergoing radiation therapy Diagnosis: cancer of the lung, esophagus, gastric, liver, breast, ovary, uterine, renal, bladder, ureter Total N randomized: 95 Total N analyzed: 95 N randomized to music group: 49 N randomized to control group: 46 N analyzed in music group: 49 N analyzed in control group: 46 Mean age: 53.87 years Sex: 43 (45%) females, 52 (55%) males Ethnicity: 95 (100%) Chinese (Han) Setting: outpatient Country: China |
|
| Interventions | 2 study groups:
Music selections provided: sacred music (Buddhism and Christianity), Chinese classical music, Western classical music, or yoga music Number of sessions: 1 Length of sessions: 30 min Categorized as music medicine |
|
| Outcomes | Anxiety (Zung State Anxiety Scale): post‐test scores Anxiety (Hamilton Anxiety Scale, HAMA): not included in this review HR, RR, SBP, DBP: post‐test scores |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Drawing of lots |
| Allocation concealment (selection bias) | High risk | Not used |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Personnel and participants were not blinded. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | This study did not address objective outcomes. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | It was unclear whether the number of participants analyzed equalled the number of participants recruited. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Unclear risk | Funding information and conflict of interest statement were not provided in the translation of the study report. |
Zhou 2015.
| Study characteristics | ||
| Methods | RCT 2‐arm parallel‐group design |
|
| Participants | Adults with breast cancer (n = 170, 100%) Total N randomized: 170 Total N analyzed: 170 N randomized to music group: 85 N randomized to control group: 85 N analyzed in music group: 85 N analyzed in control group: 85 Mean age: 47.01 years Sex: n = 170 (100%) females Ethnicity: not reported Setting: inpatient Country: People's Republic of China |
|
| Interventions | 2 study groups:
Music selections provided: Chinese relaxation music, classical folk music, religious music Number of sessions: not reported Length of sessions: 30 min Categorized as music medicine |
|
| Outcomes | Depression (Zung Self rating Depression Scale, ZSDS) Anxiety (State Anxiety Inventory, SAI) |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The patients were randomly allocated to two groups using 170 random numbers produced by computer software" (p. 55). |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel were not blinded. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | This study did not include objective outcomes. |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There were no withdrawals. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | "We thank the Dreyfus Health Foundation, New York for funding this study" (p. 59). |
ANC: absolute neutrophil count ASCT: autologous stem cell transplant BAI: Beck Anxiety Inventory BDI: Beck Depression Inventory BIS: Bispectral Index BMQ: Berlin Mood Questionnaire BMGIM: Bonny Method of Guided Imagery and Music BPI: Brief Pain Inventory bpm: beat per minute CCOP: Community Clinical Oncology Program CCT: controlled clinical trial CD(3/4/8): cluster of differentiation 3/4/8 CES‐D: Center for Epidemiologic Studies Depression Scale CM: Chinese medicine CMML: chronic myelomonocytic leukemia COPE: Coping Orientation to Problems Experienced Inventory DBP: diastolic blood pressure EEG: electroencephalogram EORTC(QLQ‐C30/CIS PAL): European Organization for Research and Treatment on Cancer ERUS: endorectal ultrasonography ESAS: Edmonton Symptom Assessment System FACIT‐BMT/F/G/Sp: Functional Assessment of Chronic Illness Therapy‐Bone Marrow Transplant/General/Spiritual FACT‐G: Functional Assessment of Cancer Therapy ‐ General GIM: guided imagery and music GVHD: Graft‐Versus‐Host Disease HADS: Hospital Anxiety and Depression Scale HAMA: Hamilton Anxiety Scale HQLI‐R: Hospice Quality of Life Index ‐ Revised HR: heart rate ICU: intensive care unit IES: Impact of Events Scale IgA: Immunoglobulin A Ig‐G: Immunoglobulin G KPS: Karnofsky Performance Scale LP: lumbar puncture MAP: mean arterial pressure MBSR: Mindfulness‐based stress reduction MFI: Multidimensional Fatigue Inventory MM: music medicine MR: Mindfulness relaxation MT: music therapy NK: Natural killer cells NRS: numeric rating scale OPEL: Patient Opinion Likert Scale PANAS: Positive and Negative Affect Schedule PI: principal investigator PICC: Peripherally inserted central catheter POMS‐SF: Profile of Mood States ‐ Short Form PPLM: Patient‐Preferred Live Music PSQI: Pittsburgh Sleep Quality Index QMS: Quick Mood Scale QoL: quality of life RBC: red blood cell RCT: randomized controlled trial RR: respiration rate RSES: Rosenberg Self‐Esteem Scale RT: radiation therapy RTCQ: Radiation Therapy Comfort Questionnaire SAI: State Anxiety Inventory SAS: State Anxiety Scale SBP: systolic blood pressure SC: standard care SCS‐SF: Self‐Compassion Scale ‐ Short Form SCT: stem‐cell transplantation SD: standard deviation SEM: standard error of the mean SMD: Standardized mean difference Sp02: oxygen saturation STAI‐S: Spielberger State‐Trait Anxiety Inventory ‐ State Anxiety form TMV: therapeutic music video VAS: visual analogue scale WBC: white blood cell ZSDS: Zung Self‐Rating Depression Scale
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Akombo 2006 | Not RCT or CCT |
| Allen 2010 | Study with cancer survivors ‐ not population of interest |
| Ardila 2010 | Not RCT or CCT |
| Augé 2015a | Not population of interest |
| Augé 2015b | Not RCT or CCT |
| Bailey 1983 | Not RCT or CCT |
| Barrera 2002 | Not RCT or CCT |
| Barry 2010 | Standard care control group was allowed to listen to music (authors stated that otherwise they would not have been able to obtain ethics approval), and 4 out of 6 pediatric participants did. If all participants had opted to listen to music, we could have included this study in the music therapy versus music medicine comparison. |
| Bergmark 2016 | No music only intervention |
| Bilgic 2017 | Not RCT or CCT |
| Boldt 1996 | Not RCT or CCT |
| Bozcuk 2006 | Not RCT or CCT |
| Bunt 1995 | Not RCT or CCT |
| Burke 1997 | Sample included participants with malignant as well as benign tumours |
| Burns 2001b | Not RCT or CCT |
| Canga 2012 | Not RCT or CCT |
| Capitulo 2015 | Not RCT or CCT; summary article of the Nguyen 2010 study |
| Cermak 2005 | Severe confounding issues with study design: the music group received 2 sessions whereas the control group only received 1. In addition, only post‐test data were obtained in this small scaled study; therefore, we could not ascertain baseline equivalence between groups. |
| Chi 2009 | No music intervention |
| Cuenot 1994 | Not RCT or CCT |
| Dadkhah 2019 | No music only intervention |
| Domingo 2015 | Used non‐standardized measurement tools. The authors used a standardized scale (HADS) to measure anxiety and depression but reported a total score for the scale whereas this scale's scoring guidelines explicitly stated that only subscale total scores (one for anxiety and one for depression) should be used. |
| Dvorak 2015 | Study included cancer patients and their caregivers. Statistics were reported per treatment arm for participants and caregivers combined. Separate statistics were reported for cancer participants in the experimental group but not for those in the control group. |
| Ezzone 1998 | Insufficient data reporting; attempts to contact authors unsuccessful |
| Fancourt 2015 | Not RCT or CCT |
| Fernando 2019 | Not RCT or CCT |
| Flaugher 2002 | Not RCT or CCT |
| Frank 1985 | Not RCT or CCT |
| Furioso 2002 | Not RCT or CCT |
| Gencer 2019 | Not RCT or CCT |
| Giordano 2020 | Not RCT or CCT. Assignment to treatment arm was based on whether or not the music therapist was present on the unit. |
| Gutsell 2013 | Not all participants were cancer patients (13%). |
| Hasenbring 1999 | Insufficient data reporting; attempts to contact authors unsuccessful |
| Hogenmiller 1986 | Unacceptable methodological quality: there were important pain‐related differences between the 2 groups at pre‐test. For example, there was unequal distribution of different procedures with the music group, which had significantly more biopsy procedures than the control group. Because biopsy procedures are more painful than other procedures included in the study, the author flagged this as a serious confounding variable. In addition, the amount of time that the participant listened to music was not controlled. The author stated that some participants only listened for 30 seconds prior to procedure. |
| Huang 2000 | Not RCT or CCT |
| Jeppesen 2018 | Not population of interest |
| Jourt‐Pineau 2012 | Not RCT or CCT |
| Jourt‐Pineau 2013 | Not RCT or CCT |
| Karagozoglu 2013 | Not RCT or CCT |
| Kemper 2008 | Not RCT or CCT |
| Kongsawatvorakul 2016 | Not population of interest |
| Krishaswamy 2016 | Not RCT or CCT |
| Lawson 2016 | 15% participants were not cancer patients. |
| Lee 2000 | Not RCT or CCT |
| Lee 2012 | Insufficient data reporting; study report included graphic representation of results but did not include means and standard deviations. |
| Lesiuk 2015 | Not RCT or CCT |
| Liao 2018 | No music only intervention |
| Liu 2014 | This is poster abstract. Multiple attempts to contact author to get additional data unsuccessful |
| Liu 2019 | Not music only intervention |
| Lopez 2019 | Not RCT or CCT |
| Na Cholburi 2004 | Article could not be located. We requested the article through our interlibrary loan departments and through our Cochrane Review Group. These attempts were unsuccessful. We then googled the investigator and e‐mailed her to request the research report. We sent 3 email requests over a period of 8 months but received no response. |
| Nakayama 2009 | Not RCT or CCT |
| Perkins 2018 | Not RCT or CCT |
| Pfaff 1989 | Not RCT/CCT |
| Pienta 1998 | Not RCT or CCT |
| Robinson 2009 | Not RCT or CCT |
| Rose 2008 | Not RCT or CCT |
| Sadat 2009 | Not RCT or CCT |
| Sahler 2003 | Not RCT or CCT |
| Sanchez‐Juaregui 2019 | Not population of interest |
| Schur 1987 | Not RCT or CCT |
| Sedei 1980 | Thesis could not be located; attempts to contact author unsuccessful |
| Shao 2019 | Not intervention of interest |
| Soo 2016 | Not population of interest |
| Sriasih 2019 | Not RCT or CCT |
| Standley 1992 | Not RCT or CCT |
| Stark 2012 | Not population of interest |
| Tan 2008 | Unacceptable methodological quality; control group exposed to background music |
| Tellez 2016 | Not population of interest |
| Thompson 2011 | Not RCT or CCT |
| Tilch 1999 | Not RCT or CCT |
| Toccafondi 2018 | Not RCT or CCT |
| Uggla 2018 | Not population of interest. Majority of participants had non‐malignant diagnosis. |
| Vohra 2011 | Not RCT or CCT |
| Walden 2001 | Not RCT or CCT |
| Warth 2018 | Not RCT or CCT |
| Washington 1990 | Not RCT or CCT |
| Weber 1997 | Not RCT or CCT |
| Whitney 2013 | Not RCT or CCT |
| Wurr 2000 | Not RCT or CCT (personal communication with principal investigator) |
| Yang 2019 | Not intervention of interest |
| Yildirim 2007 | Not RCT or CCT |
| Zimmernam 1989 | Not RCT or CCT |
CCT: controlled clinical trial HADS: Hospital Anxiety and Depression Scale RCT: randomized controlled trial
Characteristics of studies awaiting classification [ordered by study ID]
Banyai 2017.
| Methods | RCT |
| Participants | Breast cancer patients |
| Interventions | Hypnosis versus music listening versus control group (described as "receiving special personal attention") |
| Outcomes | QoL, monocyte count, absolute neutrophil count, NK cell activity, post‐traumatic growth |
| Notes | We requested the findings or full‐text article from the authors but did not receive a response. |
Bates 2019.
| Methods | RCT |
| Participants | Adult cancer patients during hematopoietic stem cell transplant |
| Interventions | Music therapy versus standard care |
| Outcomes | Distress, QoL, pain, anxiety, and mood |
| Notes | Dissertation only included preliminary data. Full study has been completed but data have not yet been published (personal communication with PI). |
Colwell 2020.
| Methods | Feasibility study, RCT |
| Participants | Adults with cancer diagnosis |
| Interventions | Music therapy (patient‐selected singing with accompaniment (traditional) versus patient‐created chant using the Orff process) versus standard care |
| Outcomes | Pain, fatigue, state anxiety, and mood |
| Notes | This study was identified when this review update was about to be completed. Therefore, it will be included in next update. |
Dehkhoda 2016.
| Methods | RCT |
| Participants | 120 adult blood cancer patients receiving chemotherapy |
| Interventions | Two intervention groups of active and receptive music therapy and a control group |
| Outcomes | Sleep quality |
| Notes | We requested the findings or full‐text article from the authors but did not receive a response. |
Dileo 2015.
| Methods | RCT Cross‐over study design |
| Participants | Adult cancer patients with chronic pain |
| Interventions | Two study conditions: 1. Music therapy condition: Music entrainment provided by a trained music therapist. The therapist provided an improvisation that started with sounds of the pain and moved into healing music. The pain sounds and healing music were collaboratively designed with the participant according to the participants descriptions of the pain and their preferences for music that sounded healing. 2. Control condition: Listening to preferred recorded music that the participant identified as soothing. |
| Outcomes | Pain (VAS), vital signs, pain medication usage, number of bowel movements |
| Notes | Study has been completed but findings are not yet available. |
Duong 2013.
| Methods | RCT |
| Participants | Adult patients with multiple myeloma or lymphoma (Hodgkin's or non‐Hodgkin's) who are undergoing ASCT |
| Interventions | Music therapy versus standard care |
| Outcomes | Primary outcomes: nausea and pain Secondary outcomes: mood disturbance, quality of life, use of morphine‐equivalent dose of narcotic medications |
| Notes | Study has been completed but findings are not available. |
Hseih 2019.
| Methods | RCT |
| Participants | The title suggest that this study was conducted with breast cancer survivors yet the abstract stated that participants were patients with breast cancer. |
| Interventions | Home‐based music intervention versus active control of listening to ambient music |
| Outcomes | Symptom severity, pain, and fatigue |
| Notes | We requested the findings or full‐text article from the authors but did not receive a response. |
Massimiliani 2017.
| Methods | RCT |
| Participants | Cancer patients during chemotherapy (N = 100) |
| Interventions | Music intervention versus standard care |
| Outcomes | Anxiety, heart rate, respiratory rate, blood pressure |
| Notes | We requested the findings or full‐text article from the authors but did not receive a response. |
Mondanaro 2020.
| Methods | RCT |
| Participants | Adults diagnosed with breast cancer, lung cancer, or gastrointestinal cancer |
| Interventions | Instrumental improvisational music therapy compared with vocal improvisational music therapy compared with standard care |
| Outcomes | Mental health (resilience, anxiety, stress, and depression), pain |
| Notes | This study was published in November 2020 when this review update was close to completion. Therefore, it will be assessed for inclusion in the next update. |
O'Brien 2010.
| Methods | RCT mixed methods |
| Participants | Adult patients with cancer |
| Interventions | Guided Original Lyrics and Music (GOLM) songwriting |
| Outcomes | Mood, distress levels, QoL, and satisfaction with hospital stay |
| Notes | Study was completed but has not yet been published. We attempted multiple times to obtain the full‐text dissertation from the investigator during the 2016 update but did not receive this. We continued to be unsuccessful in obtaining the full dissertation. |
Secord 2016.
| Methods | RCT |
| Participants | Women undergoing surgical treatment for breast cancer (N = 70) |
| Interventions | Listening to music versus placebo (headphones with no music) |
| Outcomes | Pain, opioid consumption and length of stay |
| Notes | We requested the findings or full‐text article from the authors but did not receive a response. |
Toole 2017.
| Methods | RCT |
| Participants | Women with early stage breast cancer receiving chemotherapy |
| Interventions | Music therapy versus standard care |
| Outcomes | Anxiety, sleep quality, depression, QoL |
| Notes | We requested the findings or full‐text article from the authors but did not receive a response. |
Xiao 2018.
| Methods | RCT |
| Participants | Breast cancer patients (N = 100) |
| Interventions | Participants were randomly assigned to a control group (standard care), aroma therapy group, music intervention group, and a joint‐therapy group |
| Outcomes | Anxiety and pain |
| Notes | We requested the findings or full‐text article from the authors but did not receive a response. |
Zhai 2017.
| Methods | RCT |
| Participants | Adults with gastrointestinal cancer (N = 106) |
| Interventions | Music intervention versus standard care |
| Outcomes | Depression, physical functioning |
| Notes | We requested the findings or full‐text article from the authors but did not receive a response. |
Zhang 2017.
| Methods | RCT |
| Participants | Adult cancer patients receiving chemotherapy |
| Interventions | Music intervention versus standard care |
| Outcomes | Vomiting, nausea, and QoL |
| Notes | We requested the findings or full‐text article from the authors but did not receive a response. |
ASCT: autologous stem cell transplant GOLM: Guided Original Lyrics and Music NK: natural killer PI: principal investigator QoL: quality of life RCT: randomized controlled trial VAS: visual analogue scale
Characteristics of ongoing studies [ordered by study ID]
ChiCTR1800014398.
| Study name | The effects of multidimensional psychological interventions on the chemotherapy response in patients with epithelial ovarian cancer: a prospective multi‐center trial |
| Methods | RCT |
| Participants | Adults with epithelial ovarian cancer |
| Interventions | Cognitive health education versus behavioural interventions versus music (it was unclear which one was the control condition) |
| Outcomes | Depression, anxiety, QoL, noradrenaline level in serum, cortisol level in serum, IL‐6 level in serum, noradrenaline level in tumour tissues |
| Starting date | 2016 |
| Contact information | Huang Yunke 326754918@qq.com |
| Notes |
ChiCTR1800020016.
| Study name | Effect of music therapy for anxiety and depression in elderly patients undergoing lung cancer surgery |
| Methods | RCT |
| Participants | Adults undergoing thoracic surgery for lung cancer |
| Interventions | Music versus standard care |
| Outcomes | Anxiety and depression |
| Starting date | 2018 |
| Contact information | Li Yang 18297604268@163.com |
| Notes |
ChiCTR1900022098.
| Study name | Perioperative effect of music therapy on patients with thoracoscopic lung cancer: a randomized controlled trial |
| Methods | RCT |
| Participants | Adults scheduled for thoracoscopic radical resection of lung cancer |
| Interventions | Listening to music versus standard care |
| Outcomes | Heart rate, systolic blood pressure, diastolic blood pressure, mean arterial pressure, pain, postoperative agitation, analgesic dosage |
| Starting date | 2017 |
| Contact information | Wang Changming wangchangmingmzk@163.com |
| Notes |
ChiCTR‐IOR‐16010190.
| Study name | Directed imagery and five‐element music on advanced non‐small cell lung cancer patients with psychological distress in chemotherapy period: a randomized controlled trial |
| Methods | RCT |
| Participants | Non‐small cell lung cancer patients |
| Interventions | Five‐element music versus directed imagery |
| Outcomes | Distress |
| Starting date | 2017 |
| Contact information | Dr. Jing 729012934@qq.com |
| Notes | Research is complete and the paper in progress for publication (personal communication with PI). |
CTRI/2017/09/009919.
| Study name | Effectiveness of music on pain, heart rate, blood pressure, temperature, anxiety and quality of life among patients with cancer during chemotherapy |
| Methods | RCT |
| Participants | Adults with stage II or stage III cancer |
| Interventions | Listening to instrumental music versus standard care |
| Outcomes | Anxiety, QoL, heart rate, blood pressure, salivary cortisol and salivary amylase levels |
| Starting date | 2016 |
| Contact information | Dr Syed Imran syed_vinu@yahoo.co.in |
| Notes |
CTRI/2018/09/015801.
| Study name | A randomized controlled trial on the effect of Indian classical music for chemotherapy and radiotherapy‐induced anxiety, pain and mood disturbance in head and neck cancer ‐ a pilot study |
| Methods | RCT |
| Participants | Adults with head and neck cancer |
| Interventions | Listening to Indian classical music versus standard care |
| Outcomes | Anxiety, pain, and mood |
| Starting date | 2018 |
| Contact information | Prakash Saxena pu.saxena@manipal.edu |
| Notes | Results completed 26/8/2019. We contacted the author to receive the results but we did not receive a response. |
IRCT20120905010744N2.
| Study name | The effectiveness of hypnotherapy, relaxation and music therapy on control of pain in children with cancer |
| Methods | RCT |
| Participants | Children with cancer |
| Interventions | Hypnotherapy versus relaxation training versus music versus standard care |
| Outcomes | Pain |
| Starting date | 2017 |
| Contact information | Fayegh Yousefi fykmsu@gmail.com |
| Notes |
IRCT20130731014229N8.
| Study name | Effect of music on blood cell levels in patients with acute leukemia under chemotherapy |
| Methods | RCT |
| Participants | Adults with acute leukemia undergoing chemotherapy |
| Interventions | Music intervention versus standard care |
| Outcomes | Blood cell count (red blood cells, hemoglobin, white blood cells, neutrophils, basophils, monocytes and lymphocytes) |
| Starting date | 2016 |
| Contact information | Hadi Jafarimanesh nurse_science@yahoo.com |
| Notes |
NCT0258312.
| Study name | Guided imagery and music for the reduction of side effects of chemotherapy in teenagers |
| Methods | RCT |
| Participants | Teenagers receiving chemotherapy for cancer treatment |
| Interventions | Guided imagery and music, chemotherapy, and standard care compared with chemotherapy and standard care |
| Outcomes | Acute nausea, distress regarding nausea, amount of nausea‐reducing medicine consumed, chemotherapy side effects, acute vomiting, pain, days to absolute neutrophil count recovery, duration of fatigue, distress regarding fatigue, food intake, weight, sense of coherence, and satisfaction with music intervention |
| Starting date | 2014 |
| Contact information | ilan@sanfi.dk |
| Notes | Data collection is scheduled to be completed September 2021 (personal communication with PI). |
NCT02583139.
| Study name | The effect and meaning of designed music narratives on anticipatory, acute, and delayed side effect of chemotherapy in children (7‐12 years) with cancer: a randomized controlled multisite study |
| Methods | RCT |
| Participants | Children (7‐12 years old) with cancer who are receiving chemotherapy |
| Interventions | 4 music narratives for children each comprising an introductory relaxation exercise, a resource‐oriented narrative including guided imagery suggestions and relaxing nature scenarios plus specially composed music |
| Outcomes | Duration (min) and intensity of acute nausea, frequency of vomiting, fatigue, pain, food intake, weight |
| Starting date | 2014 |
| Contact information | ilan@sanfi.dk |
| Notes | Data collection is scheduled to be completed September 2021 (personal communication with PI). |
NCT03378089.
| Study name | Music therapy and hematopoietic stem cell transplant |
| Methods | RCT |
| Participants | Adults undergoing inpatient allogeneic stem cell transplant |
| Interventions | Music therapy versus standard care |
| Outcomes | Distress, pain, anxiety, mood, QoL, narcotic medication intake |
| Starting date | 2018 |
| Contact information | Navneet Majhail, MD, Cleveland Clinic, Taussig Cancer Institute |
| Notes | Study was completed on 6/21/2020. Results have not been published yet (personal communication with research team). |
NCT03432247.
| Study name | Pain management support study for patients with advanced cancer |
| Methods | RCT |
| Participants | Adults with advanced cancer |
| Interventions | Interactive music therapy versus active control (verbal support sessions) |
| Outcomes | Pain intensity, pain interference, participant perception of change, anxiety, mood, perceived support, self‐efficacy, salivary cortisol, lachrymal dopamine, serum oxytocin, serum B‐endorphin |
| Starting date | 2017 |
| Contact information | Joke Bradt jbradt@drexel.edu |
| Notes | Anticipated completion date: June 2021 |
NCT03511079.
| Study name | Music as a perioperative therapy in breast cancer patients |
| Methods | RCT |
| Participants | Breast cancer patients |
| Interventions | Music listening versus standard care |
| Outcomes | Pain, sleep quality, depression, salivary cortisol, salivary melatonin, salivary C‐reactive protein |
| Starting date | 2018 |
| Contact information | Kristine Widders kwidders@pennstatehealth.psu.edu |
| Notes |
NCT03538223.
| Study name | Music listening to reduce anxiety and stress in patients undergoing radiotherapy |
| Methods | RCT |
| Participants | Adults with cancer undergoing radiotherapy |
| Interventions | Listening to music (Melomics‐Health listening) versus individualized listening versus standard care |
| Outcomes | Anxiety and stress |
| Starting date | 2018 |
| Contact information | Afredo Raglio alfredo.raglio@icsmaugeri.it |
| Notes |
NCT03683420.
| Study name | Music in reducing distress in participants with cancer during chemotherapy treatment |
| Methods | RCT |
| Participants | Adults with cancer undergoing chemotherapy |
| Interventions | Music listening versus standard care |
| Outcomes | Pain, mood, distress |
| Starting date | 2018 |
| Contact information | Felicity Harper, Barbara Ann Karmanos Cancer Institute |
| Notes | Anticipated ending date: 12/31/2020 |
NCT03740984.
| Study name | Effects of music or hypnotherapy on cancer patients during chemotherapy (F‐Chem) |
| Methods | RCT |
| Participants | Adults with breast cancer or ovarian cancer undergoing chemotherapy |
| Interventions | Hypnotherapy versus music listening versus standard care |
| Outcomes | Depression, QoL, emetic episodes, fatigue, heart rate |
| Starting date | 2018 |
| Contact information | Joscha Reinhard Joscha.reinhard@helios-gesundheit.de |
| Notes | Anticipated completion date 2023 |
NCT03955003.
| Study name | Fatigue, Anxiety, Music, and Entertainment (FAME) Study |
| Methods | RCT |
| Participants | Adults receiving chemotherapy or radiotherapy |
| Interventions | Group drumming versus standard care |
| Outcomes | Fatigue, anxiety, cognitive function, positive affect |
| Starting date | 2019 |
| Contact information | Shelley White shelley.white@hci.utah.edu |
| Notes |
NCT04052074.
| Study name | Complementary therapy in home palliative care patients and their caregivers (COMTHECARE) |
| Methods | RCT |
| Participants | Adult oncology patients receiving palliative care |
| Interventions | Music versus psycho‐education |
| Outcomes | Pain, anxiety, depression, mood, insomnia, and QoL |
| Starting date | 2019 |
| Contact information | inmaculada.valero.sspa@juntadeandalucia.es |
| Notes |
NTR7546.
| Study name | Intraoperative Music to PROMote PaTient oUtcome (IMPROMPTU): a double‐blind, placebo‐controlled, randomized multicenter trial |
| Methods | RCT |
| Participants | Patients undergoing elective surgical esophageal or stomach cancer resection |
| Interventions | Intraoperative music versus standard care |
| Outcomes | Postoperative pain |
| Starting date | 2018 |
| Contact information | Fuv.fu@erasmusmc.nl |
| Notes | We contacted the author and were informed that recruiting was halted due to the COVID‐19 pandemic |
PI: principal investigator QoL: quality of life RCT: randomized controlled trial
Differences between protocol and review
Disease‐free survival was listed in the protocol as a secondary outcome but was excluded in the review as per recommendation of the peer review.
We slightly altered the MEDLINE search strategy, removing the words 'compose' and 'composing' as text words because they resulted in hundreds of irrelevant returns.
We added the RILM Abstracts of Music Literature database to the search strategy as per recommendation of the peer review.
In the current update of the review, we decided to include studies that included a few participants (< 10% of total sample) with non‐cancer diagnoses (e.g. aplastic anemia). We reviewed all studies that were excluded in previous versions of this review to verify whether those studies should remain excluded due to the study population not meeting the eligibility criteria for this review. To ensure that the addition of these studies did not impact the magnitude of the effect size, a sensitivity analysis was added.
In the current review, we decided to keep the analyses separate for the adult participant studies and the pediatric participant studies.
In the current review, we edited the list of primary and secondary outcomes to give examples of possible outcome measures to those assessed.
Contributions of authors
Background, objectives, criteria for considering studies: Bradt, Dileo Search strategies, methods: Bradt (reviewed and approved by Dileo) Database searches and handsearches: Bradt, Biondo, Dileo, Myers‐Coffman Screening search results: Bradt, Biondo, Myers‐Coffman Organising retrieval of papers: Bradt Screening retrieved papers against inclusion criteria: Bradt, Biondo, Myers‐Coffman Appraising quality of papers: Bradt, Dileo, Biondo, Myers‐Coffman Abstracting data from papers: Bradt, Biondo, Myers‐Coffman, Bradt Writing to authors of papers for additional information: Bradt, Biondo, Myers‐Coffman Providing additional data about papers: Bradt Obtaining and screening data on unpublished studies: Bradt Data management for the review: Bradt Entering data into Review Manager (Review Manager 5 2020): Bradt, Biondo, Myers‐Coffman RevMan statistical data: Bradt Other statistical analysis not using RevMan: Bradt Interpretation of data: Bradt, Dileo Statistical inferences: Bradt Writing the review: Bradt (reviewed and approved by Dileo, Biondo, Myers‐Coffman) Securing funding for the review: Dileo (for original review) Guarantor for the review (one author): Bradt Person responsible for reading and checking review before submission: Bradt
Sources of support
Internal sources
-
Drexel University, USA
Drexel University provided financial support for a research assistant to assist with the update of this review
External sources
State of Pennsylvania Formula Fund, USA
Declarations of interest
Joke Bradt ‐ None known Cheryl Dileo ‐ None known Katherine Myers‐Coffman ‐ None known Jacelyn Biondo ‐ None known
Edited (no change to conclusions)
References
References to studies included in this review
Alam 2016 {published data only}
- Alam M, Roongpisuthipong W, Kim NA, Goyal A, Swary JH, Brindise RT, et al. Utility of recorded guided imagery and relaxing music in reducing patient pain and anxiety, and surgeon anxiety, during cutaneous surgical procedures: a single-blinded randomized controlled trial. Journal of the American Academy of Dermatology 2016;75(3):585-9. [DOI: ] [DOI] [PubMed] [Google Scholar]
Alcantara‐Silva 2018 {published data only}
- Alcantara-Silva TR, De Freitas-Junior R, Freitas NMA, De Paula Junior W, Da Silva DJ, Machado GDP, et al. Music therapy reduces radiotherapy-induced fatigue in patients with breast or gynecological cancer: a randomized trial. Integrative Cancer Therapies 2018;17(3):628-35. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Arruda 2016 {published data only}
- Arruda MA, Garcia MA, Garcia JB. Evaluation of the effects of music and poetry in oncologic pain relief: a randomized clinical trial. Journal of Palliative Medicine 2016;19(9):943-8. [DOI: ] [DOI] [PubMed] [Google Scholar]
Bates 2017 {published data only}
- Bates D, Bolwell B, Majhail NS, Rybicki L, Yurch M, Abounader D, et al. Music therapy for symptom management after autologous stem cell transplantation: results from a randomized study. Biology of Blood and Marrow Transplantation 2017;23(9):1567-72. [DOI: 10.1016/j.bbmt.2017.05.015.] [DOI] [PubMed] [Google Scholar]
Beck 1989 {published and unpublished data}
- Beck SLC. The Effect of Therapeutic Use of Music on Cancer Related Pain [PhD thesis]. Salt Lake City, UT: University of Utah, 1989. [Google Scholar]
- Beck SLC. The therapeutic use of music for cancer-related pain. Oncology Nursing Forum 1991;18(8):1327-37. [PubMed] [Google Scholar]
Bieligmeyer 2018 {published data only}
- Bieligmeyer S, Helmert E, Hautzinger M, Vagedes J. Feeling the sound - short-term effect of a vibroacoustic music intervention on well-being and subjectively assessed warmth distribution in cancer patients: a randomized controlled trial. Complementary Therapies in Medicine 2018;40:171-8. [DOI: 10.1016/j.ctim.2018.03.002] [DOI] [PubMed] [Google Scholar]
Binns‐Turner 2008 {unpublished data only}
- Binns-Turner PG. Perioperative Music and its Effects on Anxiety, Hemodynamics, and Pain in Women Undergoing Mastectomy [PhD thesis]. Tuscaloosa, Alabama: University of Alabama, 2008. [PubMed] [Google Scholar]
Bradt 2015 {published data only}
- Bradt J, Potvin N, Kesslick A, Shim M, Radl D, Schriver E, et al. The impact of music therapy versus music medicine psychological outcomes and pain in cancer patients: a mixed methods study. Support Care Cancer 2015;23:1261-71. [DOI] [PubMed] [Google Scholar]
Bro 2019 {published and unpublished data}
- Bro ML, Johansen C, Vuust P, Enggaard L, Himmelstrup B, Mourits-Andersen T, et al. Effects of live music during chemotherapy in lymphoma patients: a randomized, controlled, multi-center trial. Supportive Care in Cancer 2019;17(10):3887-96. [DOI: 10.1007/s00520-019-04666-8] [DOI] [PubMed] [Google Scholar]
- Bro ML. Resonance: Music as Adjuvant for Cancer Treatment [PhD Thesis]. University of Southern Denmark, 2019. [Google Scholar]
Bufalini 2009 {published data only}
- Bufalini A. Role of interactive music in oncological paediatric patients undergoing painful procedures. Minerva Pediatrica 2009;61(4):379-89. [PubMed] [Google Scholar]
Bulfone 2009 {published and unpublished data}
- Bulfone T, Quattrin R, Zanotti R, Regattin L, Brusaferro S. Effectiveness of music therapy for anxiety reduction in women with breast cancer in chemotherapy treatment. Holistic Nursing Practice 2009;23(4):238-42. [DOI] [PubMed] [Google Scholar]
Burns 2001a {published data only}
- Burns DS. The effect of the Bonny Method of Guided Imagery and Music on the mood and life quality of cancer patients. Journal of Music Therapy 2001;38(1):51-65. [DOI] [PubMed] [Google Scholar]
Burns 2008 {published data only}
- Burns DS, Azzouz F, Sledge R, Rutledge C, Hincher K, Monahan PO, et al. Music imagery for adults with acute leukemia in protective environments: a feasibility study. Support Care Cancer 2008;16(5):507-13. [DOI] [PubMed] [Google Scholar]
Burns 2009 {published and unpublished data}
- Burns DS, Robb SL, Haase JE. Exploring the feasibility of a therapeutic music video intervention in adolescents and young adults during stem-cell transplantation. Cancer Nursing 2009;32(5):E8-16. [DOI] [PubMed] [Google Scholar]
- NCT00305851. Music therapy or book discussion in improving quality of life in young patients undergoing stem cell transplant. clinicaltrials.gov/ct2/show/NCT00305851 (date first received 21 March 2006. [CDR0000463879] [COG-ANUR0631] [NCT00305851]
Burns 2018 {published data only}
- Burns DS, Meadows AN, Althouse S, Perkins SM, Cripe LD. Differences between supportive music and imagery and music listening during outpatient chemotherapy and potential moderators of treatment effects. Journal of Music Therapy 2018;55(1):83-108. [DOI: 10.1093/jmt/thy001] [DOI] [PubMed] [Google Scholar]
Burrai 2014 {published data only}
- Burrai V, Micheluzzi V, Bugani V. Effects of live sax music on various physiological parameters, pain level, and mood level in cancer patients. Holistic Nursing Practice 2014;28:301-11. [DOI] [PubMed] [Google Scholar]
Cai 2001 {published data only}
- Cai GR, Li PW, Jiao LP. Clinical observation of music therapy combined with anti-tumor drugs in treating 116 cases of tumor patients. Zhongguo Zhongxiyi Jiehe Zqzhi [Chinese Journal of Integrated Traditional & Western Medicine] 2001;21(12):891-4. [PubMed] [Google Scholar]
- Cai GR, Yi Q, Peiwen L, Liping J, Liang L. Music therapy in treatment of cancer patients. Zhongguo Xinli Weisheng Zazhi [Chinese Mental Health Journal] 2001;15(3):179-81. [Google Scholar]
Cassileth 2003 {published data only}
- Cassileth BR, Vickers AJ, Magill LA. Music therapy for mood disturbance during hospitalisation for autologous stem cell transplantation: a randomised controlled trial. Cancer 2003;98(12):2723-9. [DOI] [PubMed] [Google Scholar]
Chen 2004 {published data only}
- Chen LZ, Xie Z, Feng ZH, Huang G, Yin ZM, Yu ZH. Effect of cognitive behavioral intervention therapy on immunological function of patients with breast cancer. Chinese Journal of Clinical Rehabilitation 2004;8(29):6310-11. [Google Scholar]
Chen 2013 {published data only}
- Chen LC, Wang TF, Shih YN, Wu LJ. Fifteen-minute music intervention reduces pre-radiotherapy anxiety in oncology patients. European Journal of Oncology Nursing 2013;17(4):436-41. [DOI] [PubMed] [Google Scholar]
Chen 2018 {published data only}
- Chen SC, Chou CC, Chang HJ, Lin MF. Comparison of group vs self-directed music interventions to reduce chemotherapy-related distress and cognitive appraisal: an exploratory study. Supportive Care in Cancer 2018;26(2):461-9. [DOI: 10.1007/s00520-017-3850-1] [DOI] [PubMed] [Google Scholar]
Chen 2020 {published data only}
- Chen SC, Yeh ML, Chang HJ, Lin MF. Music, heart rate variability, and symptom clusters: a comparative study. Supportive Care Cancer 2020;28(1):351-60. [DOI: 10.1007/s00520-019-04817-x] [DOI] [PubMed] [Google Scholar]
Clark 2006 {published data only}
- Clark M, Isaacks-Downton G, Wells N, Redlin-Frazier S, Eck C, Hepworth JT, et al. Use of preferred music to reduce emotional distress and symptom activity during radiation therapy. Journal of Music Therapy 2006;43(3):247-65. [DOI] [PubMed] [Google Scholar]
Cook 2013 {published data only}
- Cook EL, Silverman MJ. Effects of music therapy on spirituality with patients on a medical oncology/hematology unit: a mixed-methods approach. Arts in Psychotherapy 2013;40(2):239-44. [Google Scholar]
Danhauer 2010 {unpublished data only}
- Danhauer SC, Vishnevsky T, Campbell CR, McCoy TP, Tooze JA, Kanipe KN, et al. Music for patients with hematological malignancies undergoing bone marrow biopsy: a randomised controlled study of anxiety, perceived pain, and patient satisfaction. Journal of the Society for Integrative Oncology 2010;8(4):140-7. [PMC free article] [PubMed] [Google Scholar]
Doro 2017 {published data only}
- Doro CA, Neta JZ, Cunha R, Doro MP. Music therapy improves the mood of patients undergoing hematopoietic stem cells transplantation (controlled randomized study). Supportive Care in Cancer 2017;25(3):1013-8. [DOI: 10.1007/s00520-016-3529-z] [DOI] [PubMed] [Google Scholar]
Duocastella 1999 {published data only}
- Duocastella AC. Effect of music on children with cancer. Revista de Enfermeria 1999;22(4):293-8. [PubMed] [Google Scholar]
Ferrer 2005 {published and unpublished data}
- Ferrer A. The Effect of Live music on Decreasing Anxiety in Patients Undergoing Chemotherapy Treatment [MSc/MA thesis]. Tallahassee, FL: Florida State University, 2005. [DOI] [PubMed] [Google Scholar]
- Ferrer AJ. The effect of live music on decreasing anxiety in patients undergoing chemotherapy treatment. Journal of Music Therapy 2007;44(3):242-55. [DOI] [PubMed] [Google Scholar]
Firmeza 2017 {published data only}
- Firmeza MA, Rodrigues AB, Melo GAA, Aguiar MIF, Cunha GH, Oliveira PP, et al. Control of anxiety through music in a head and neck outpatient clinic: a randomized clinical trial. Revista da Escola de Enfermagem da USP 2017;51:e03201. [DOI: ] [DOI] [PubMed] [Google Scholar]
Fredenburg 2014a {published data only}
- Fredenburg HA, Silverman MJ. Effects of music therapy on positive and negative affect and pain with hospitalised patients recovering from a blood and marrow transplant: a randomised effectiveness study. Arts in Psychotherapy 2014;41(2):174-80. [Google Scholar]
Fredenburg 2014b {published data only}
- Fredenburg HA. Effects of cognitive-behavioral music therapy on fatigue in patients in a blood and marrow transplantation unit: a mixed-method pilot study. Arts in Psychotherapy 2014;41:433–44. [Google Scholar]
- Fredenburg HA. Effects of Cognitive-behavioral Music Therapy on Fatigue with Patients on a Blood and Marrow Transplantation Unit: a Convergent Parallel Mixed Methods Effectiveness Study [MA Thesis]. Minneapolis-St Paul, MN: University of Minnesota, 2013. [Google Scholar]
Gimeno 2008 {unpublished data only}
- Gimeno M. The Effect of Music and Imagery to Induce Relaxation and Reduce Nausea and Emesis in Cancer Patients Undergoing Chemotherapy Treatment [PhD thesis]. Stockton, CA: University of the Pacific, 2008. [Google Scholar]
Hanser 2006 {published data only}
- Hanser SB, Bauer-Wu S, Kubicek L, Healey M, Manola J, Hernandez M, et al. Effects of a music therapy intervention on quality of life and distress in women with metastatic breast cancer. Journal of the Society for Integrative Oncology 2006;4(3):116-24. [DOI] [PubMed] [Google Scholar]
Harper 2001 {unpublished data only}
- Harper EI. Reducing Treatment-related Anxiety in Cancer Patients: Comparison of Psychological Interventions [PhD thesis]. Dallas, TX: Southern Methodist University, 2001. [Google Scholar]
Hilliard 2003 {published data only}
- Hilliard RE. The Effects of Music Therapy on Quality of Life and Length of Life of Hospice Patients Diagnosed with Terminal Cancer [PhD thesis]. Tallahassee, FL: Florida State University, 2002. [Google Scholar]
- Hilliard RE. The effects of music therapy on the quality and length of life of people diagnosed with terminal cancer. Journal of Music Therapy 2003;40(2):113-37. [DOI] [PubMed] [Google Scholar]
Horne‐Thompson 2008 {published data only}
- Horne-Thompson A, Grocke D. The effect of music therapyon anxiety in patients who are terminally ill. Journal of Palliative Medicine 2008;11:582-90. [DOI: 10.1089/jpm.2007.0193] [DOI] [PubMed] [Google Scholar]
Huang 2006 {published and unpublished data}
- Huang S, Good M, Zauszniewski JA. The effectiveness of music in relieving pain in cancer patients: a randomised controlled trial. International Journal of Nursing Studies 2010;47(11):1354-62. [DOI: 10.1016/j.ijnurstu.2010.03.008] [DOI] [PubMed] [Google Scholar]
- Huang S. The Effects of Music on Cancer Pain [PhD thesis]. Cleveland, OH: Case Western Reserve University, 2006. [Google Scholar]
Hunter 2020 {published data only}
- Hunter JJ, Maunder RG, Sui DW, Esplen MJ, Chaoul A, Fisch MJ, et al. A randomized trial of nurse-administered behavioral interventions to manage anticipatory nausea and vomiting in chemotherapy. Cancer Medicine 2020;9(5):1733-40. [DOI: ] [NCT00086762] [DOI] [PMC free article] [PubMed] [Google Scholar]
Jasemi 2016 {published data only}
- Jasemi M, Aazami S, Zabihi RE. The effects of music therapy on anxiety and depression of cancer patients. Indian Journal of Palliative Care 2016;22(4):455-8. [DOI: 10.4103/0973-1075.191823] [DOI] [PMC free article] [PubMed] [Google Scholar]
Jin 2011 {published data only}
- Jin F, Zhao Y. Influence of music relaxation therapy on vital signs and anxiety of liver cancer patients accepting transcatheter hepatic arterial chemoembolization. Huli Yanjiu [Chinese Nursing Research] 2011;16:1429-31. [Google Scholar]
Karadag 2019 {published data only}
- Karadag E. The effect of music listening intervention applied during radiation therapy on the anxiety and comfort level in women with early-stage breast cancer: a randomized controlled trial. European Journal of Integrative Medicine 2019;27:39-44. [DOI: ] [Google Scholar]
Keenan 2017 {published data only}
- Keenan A. Effect of a Music Intervention on Pain Following Hematopoietic Stem Cell Transplant [PhD thesis]. Rush University, 2017. [Google Scholar]
Kwekkeboom 2003 {published data only}
- Kwekkeboom KL. Music versus distraction for procedural pain and anxiety in patients with cancer. Oncology Nursing Forum 2003;30(3):433-40. [DOI] [PubMed] [Google Scholar]
Letwin 2017 {published data only}
- Letwin L, Silverman MJ. No between-group difference but tendencies for patient support: a pilot study of a resilience-focused music therapy protocol for adults on a medical oncology/hematology unit. Arts in Psychotherapy 2017;55:116-25. [DOI: ] [Google Scholar]
Li 2004 {published data only}
- Li S. Applying Chinese classical music to treat preoperative anxiety of patients with gastric cancer. Huli Yanjiu [Chinese Nursing Research] 2004;18(3B):471-2. [Google Scholar]
Li 2012 {published data only}
- Li XM, Yan H, Zhou KN, Dang SN, Wang DL, Zhang YP. Effects of music therapy on pain among female breast cancer patients after radical mastectomy: results from a randomised controlled trial. Breast Cancer Research and Treatment 2011;128(2):411-9. [DOI] [PubMed] [Google Scholar]
- Li XM, Zhou KN, Yan H, Wang DL, Zhang YP. Effects of music therapy on anxiety of patients with breast cancer after radical mastectomy: a randomised clinical trial. Journal of Advanced Nursing 2012;68(5):1145-55. [DOI] [PubMed] [Google Scholar]
- Zhou K, Li XM, Yan H, Dang SN, Wang DL. Effects of music therapy on depression and duration of hospital stay of breast cancer patients after radical mastectomy. Zhonghua Yixue Zazhi [Chinese Medical Journal] 2011;124(15):2321-7. [PubMed] [Google Scholar]
Liao 2013 {published data only}
- Liao J, Yang YF, Cohen I, Zhao YC, Xu Y. Effects of Chinese medicine five-element music on the quality of life for advanced cancer patients: a randomized controlled trial. Chinese Journal of Integrated Medicine 2013;19(10):736-40. [DOI] [PubMed] [Google Scholar]
Lin 2011 {published data only}
- Lin MF, Hsieh YJ, Hsu YY, FetzerS, Hsu MC. A randomised controlled trial of the effect of music therapy and verbal relaxation on chemotherapy‐induced anxiety. Journal of Clinical Nursing 2011;20(7-8):988-99. [DOI] [PubMed] [Google Scholar]
Moradian 2015 {published data only}
- Moradian S, Walshe C, Shahidsales S, Nasiri M, Pilling M, Molassiotis A. Nevasic audio program for the prevention of chemotherapy induced nausea and vomiting: a feasibility study using a randomised controlled trial design. European Journal of Oncology Nursing 2015;19:282-91. [DOI] [PubMed] [Google Scholar]
Mou 2020 {published data only}
- Mou Q, Wang X, Xu H, Liu X, Li J. Effects of passive music therapy on anxiety and vital signs in lung cancer patients undergoing peripherally inserted central catheter placement procedure. Journal of Vascular Access 2020;21(6):875-82. [DOI: ] [DOI] [PubMed] [Google Scholar]
Nguyen 2010 {published data only}
- Nguyen TN, Nilsson S, Hellstrom A, Bengtson A. Music therapy to reduce pain and anxiety in children with cancer undergoing lumbar puncture: a randomised clinical trial. Journal of Pediatric Oncology Nursing 2010;27(3):146-55. [DOI] [PubMed] [Google Scholar]
O'Callaghan 2012 {published data only}
- O'Callaghan C, Sproston M, Wilkinson K, Willis D, Milner A, Grocke D, et al. Effect of self-selected music on adults' anxiety and subjective experiences during initial radiotherapy treatment: a randomised controlled trial and qualitative research. Journal of Medical Imaging and Radiation Oncology 2012;56(4):473-7. [DOI] [PubMed] [Google Scholar]
Palmer 2015 {published data only}
- Palmer J, Lane D, Mayo D, Schluchter M, Leeming R. Effects of music therapy on anaesthesia requirements and anxiety in women undergoing ambulatory breast surgery for cancer diagnosis and treatment: a randomised controlled trial. Journal of Clincal Oncology 2015;33(28):3162-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pedersen 2020 {published data only}
- Pedersen MRV, Dam C, Rafaelsen SR. Music and pain during endorectal ultrasonography examination: a prospective questionnaire study and literature review. Radiography 2020;26(3):E164-9. [DOI: ] [DOI] [PubMed] [Google Scholar]
Pinto 2012 {published data only}
- Pinto Junior FEL, Ferraz DLM, Cunha EQ, Santos IRM, Batista MDC. Influence of music on pain and anxiety due to surgery in patients with breast cancer [Influência da música na dor e na ansiedade decorrentes de cirurgia em pacientes com câncer de mama]. Revista Brasileira de Cancerologia 2012;58(2):135-41. [Google Scholar]
Porter 2018 {published data only}
- Porter S, McConnell T, Graham-Wisener L, Regan J, McKeown M, Kirkwood J, et al. A randomised controlled pilot and feasibility study of music therapy for improving the quality of life of hospice inpatients. BMC Palliative Care 2018;17:125. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ramirez 2018 {published data only}
- Ramirez R, Planas J, Escude N, Mercade J, Farriols C. EEG-based analysis of the emotional effect of music therapy on palliative care cancer patients. Frontiers in Psychology 2018;9:254. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ratcliff 2014 {published data only}
- Ratcliff CG, Prinsloo S, Richardson M, Baynham-Fletcher L, Lee R, Chaoul A, et al. Music therapy for patients who have undergone hematopoietic stem cell transplant. Evidence-based Complementary and Alternative Medicine 2014;2014:1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Reimnitz 2018 {published data only}
- Reimnitz L, Silverman MJ. A randomized pilot study of music therapy in the form of patient-preferred live music on fatigue, energy and pain in hospitalized adult oncology patients on a blood and marrow transplant unit. Arts & Health 2020;12(2):154-68. [DOI: ] [DOI] [PubMed] [Google Scholar]
Robb 2008 {published data only}
- Robb SL, Clair AA, Watanabe M, Monahan PO, Azzous F, Stouffer JW, et al. A non-randomised controlled trial of the active music engagement (AME) intervention on children with cancer. Psycho-Oncology 2008;17(7):699-708. [DOI] [PubMed] [Google Scholar]
Robb 2014 {published data only}
- Robb SL, Burns DS, Stegenga KA, Haut PR, Monahan PO, Meza J, et al. Randomized clinical trial of therapeutic music video intervention for resilience outcomes in adolescents/young adults undergoing hematopoietic stem cell transplant. Cancer 2014;120(6):909-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
Robb 2017 {published data only}
- Robb SL, Haase JE, Perkins SM, Haut PR, Henley AK, Knafl KA, et al. Pilot randomized trial of active music engagement intervention parent delivery for young children with cancer. Journal of Pediatric Psychology 2017;42(2):208-19. [DOI: 10.1093/jpepsy/jsw050] [DOI] [PMC free article] [PubMed] [Google Scholar]
Romito 2013 {published data only}
- Romito F, Lagattolla F, Costanzo C, Giotta F, Mattioli V. Music therapy and emotional expression during chemotherapy. How do breast cancer patients feel? European Journal of Integrative Medicine 2013;5(5):438-42. [Google Scholar]
Rosenow 2014 {published data only}
- Rosenow SC, Silverman MJ. Effects of single session music therapy on hospitalized patients recovering from a bone marrow transplant: two studies. Arts in Psychotherapy 2014;41(1):65-70. [Google Scholar]
Rossetti 2017 {published data only}
- Rossetti A, Chadha M, Torres BN, Lee JK, Hylton D, Loewy JV, et al. The impact of music therapy on anxiety in cancer patients undergoing simulation for radiation therapy. International Journal of Radiation Oncology Biology Physics 2017;99(1):103-10. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Shaban 2006 {published data only}
- Shaban M, Rasoolzadeh N, Mehran A, Moradalizadeh F. Study of two non-pharmacological methods, progressive muscle relaxation and music on pain relief of cancerous patients. Journal of Tehran Faculty of Nursing & Midwifery 2006;12(3):87. [Google Scholar]
Smith 2001 {published data only}
- Smith M, Casey L, Johnson D, Gwede C, Riggin OZ. Music as a therapeutic intervention for anxiety in patients receiving radiation therapy. Oncology Nursing Forum 2001;28(5):855-62. [PubMed] [Google Scholar]
Stordahl 2009 {unpublished data only}
- Stordahl JJ. The Influence of Music on Depression, Affect, and Benefit Finding Among Women at the Completion of Treatment for Breast Cancer [PhD thesis]. Miami, FL: University of Miami, 2009. [Google Scholar]
Straw 1991 {published data only}
- Straw GW. The Use of Guided Imagery and Relaxation for the Quality of Life of Cancer Patients Undergoing Chemotherapy [Master's thesis]. Ontario: Lakehead University, 1991. [Google Scholar]
Tuinmann 2017 {published data only}
- Tuinmann G, Preissler P, Bohmer H, Suling A, Bokemeyer C. The effects of music therapy in patients with high-dose chemotherapy and stem cell support: a randomized pilot study. Psycho-oncology 2017;26(3):377-84. [DOI: 10.1002/pon.4142] [DOI] [PubMed] [Google Scholar]
Vachiramon 2013 {published data only}
- Vachiramon V, Sobanko JF, Rattanaumpawan P, Miller CJ. Music reduces patient anxiety during Mohs surgery: an open‐label randomized controlled trial. Dermatologic Surgery 2013;39(2):298-305. [DOI] [PubMed] [Google Scholar]
Verstegen 2016 {unpublished data only}
- Verstegen AL, Silverman MJ. Effects of Hope-Based Music Therapy on Hope and Pain in Hospitalized Patients on Blood and Marrow Transplant Unit: a Convergent Parallel Mixed-Methods Pilot Study [MA Thesis]. Ann Arbor: University of Minnesota, 2016. [Google Scholar]
Verstegen 2018 {published data only}
- Verstegen AL, Silverman MJ. Effects of music therapy on mood and pain with patients hospitalized for bone marrow transplantation: a randomized effectiveness pilot study. Journal of Creativity in Mental Health 2018;13(4):418-28. [DOI: ] [Google Scholar]
Wan 2009 {published data only}
- Wan Y, Mao Z, Qiu Y. Influence of music therapy on anxiety, depression and pain of cancer patients. Huli Yanjiu [Chinese Nursing Research] 2009;23(5A):1172-5. [Google Scholar]
Wang 2015 {published and unpublished data}
- Wang Y, Tang H, Guo Q, Liu J, Liu X, Luo J, et al. Effects of intravenous patient-controlled sufentanil analgesia and music therapy on pain and haemodynamics after surgery for lung cancer: a randomised parallel study. Journal of Alternative and Complementary Medicine 2015;21(11):667-72. [DOI] [PubMed] [Google Scholar]
Warth 2015 {published data only}
- Warth M, Keßler J, Hillecke TK, Bardenheuer, HJ. Trajectories of terminally ill patients' cardiovascular response to receptive music therapy in palliative care. Journal of Pain and Symptom Management 2016;52(2):196-204. [DOI: 10.1016/j.jpainsymman.2016.01.008] [DOI] [PubMed] [Google Scholar]
- Warth M, Keßler J, Hillecke TK, Bardenheuer HJ. Music therapy in palliative care. Deutsches Arzteblatt International 2015;112(46):788-94. [DOI: 10.3238/arztebl.2015.0788] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wren 2019 {published data only}
- Wren AA, Shelby RA, Soo MS, Huysmans Z, Jarosz JA, Keefe FJ. Preliminary efficacy of a loving kindness meditation intervention for patients undergoing biopsy and breast cancer surgery: a randomized controlled pilot study. Supportive Care in Cancer 2019;27(9):3583-92. [DOI: ] [DOI] [PubMed] [Google Scholar]
Xie 2001 {published data only}
- Xie Z, Wang G, Yin Z, Liao S, Lin J, Yu Z, et al. Effect of music therapy and inner image relaxation on quality of life in cancer patients receiving chemotherapy. Zhongguo Xinli Weisheng Zazhi [Chinese Mental Health Journal] 2001;15(3):176-8. [Google Scholar]
Yates 2015 {published data only}
- Yates G, Silverman M. Immediate effects of single-session music therapy on affective state inpatients on a post-surgical oncology unit: a randomised effectiveness study. Arts in Psychotherapy 2015;44:57-61. [Google Scholar]
Zhao 2008 {published data only}
- Zhao PT, Liang J, Shao QJ, Liang F, Yuan HQ, You FS. Interventional effects of musical therapy to physiological and psychological conditions in process of radiotherapy for patients with cancer. Zhonghua Zhongliu Fangzhi Zazhi [Chinese Journal of Cancer Prevention and Treatment] 2008;15(14):1097-9. [Google Scholar]
Zhou 2015 {published data only}
- Zhou K, Li X, Li J, Liu M, Dang S, Wang D, et al. A clinical randomised controlled trial of music therapy and progressive muscle relaxation training in female breast cancer patients after radical mastectomy: results on depression, anxiety and length of hospital stay. European Journal of Oncology Nursing 2015;19:54-9. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Akombo 2006 {unpublished data only}
- Akombo D. Effects of Listening to Music as an Intervention for Pain and Anxiety in Bone Marrow Transplant Patients [PhD thesis]. Gainesville, FL: University of Florida, 2006. [Google Scholar]
Allen 2010 {unpublished data only}
- Allen J. The Effectiveness of Group Music and Imagery on Improving the Self-concept of Breast Cancer Survivors [PhD thesis]. Philadelphia, PA: Temple University, 2010. [Google Scholar]
Ardila 2010 {published data only}
- Ardila E. Complementary medicine and cancer [Las medicinas complementarias y el cáncer]. Revista Colombiana de Cancerología 2010;12(3):127-8. [Google Scholar]
Augé 2015a {published data only}
- Augé PM, Mercadal-Brotons M, Resano CS. The effect of music therapy on mood and quality of life in female breast cancer survivors [Efecto de la musicoterapia en el estado anímico y calidad de vida de un grupo de mujeres supervivientes de cáncer de mama]. Psicooncología 2015;12(1):105-28. [Google Scholar]
Augé 2015b {published and unpublished data}
- Augé P, Mercadal-Brotons M, Resano C. The effect of music therapy on mood and quality of life in colorectal cancer patients [Efecto de la musicoterapia en el estado de ánimo y calidad de vida de pacientes con cáncer colorectal]. Psicooncología 2015;12(2-3):259-82. [Google Scholar]
Bailey 1983 {published data only}
- Bailey LM. The effects of live music versus tape-recorded music on hospitalised cancer patients. Music Therapy 1983;3(1):17-28. [Google Scholar]
Barrera 2002 {published data only}
- Barrera ME, Rykov MH, Doyle SL. The effects of interactive music therapy on hospitalised children with cancer: a pilot study. Psycho-Oncology 2002;11:379-88. [DOI] [PubMed] [Google Scholar]
Barry 2010 {published data only}
- Barry P, O'Callaghan C, Wheeler G, Grocke D. Music therapy CD creation for initial paediatric radiation therapy: a mixed methods analysis. Journal of Music Therapy 2010;47(3):233-63. [DOI] [PubMed] [Google Scholar]
Bergmark 2016 {published data only}
- Bergmark K. Clipped wings: body image and sexuality in women treated for gynaecological cancer. World Congress of Psycho-Oncology 2016;25:148. [Google Scholar]
Bilgic 2017 {published data only}
- Bilgic S, Acaroglu R. Effects of listening to music on the comfort of chemotherapy patients. Western Journal of Nursing Research 2017;39:307-11. [DOI: ] [DOI] [PubMed] [Google Scholar]
Boldt 1996 {published data only}
- Boldt S. The effects of music therapy on motivation, psychological well-being, physical comfort, and exercise endurance of bone marrow transplant patients. Journal of Music Therapy 1996;33(3):164-88. [Google Scholar]
Bozcuk 2006 {published data only}
- Bozcuk H, Artac M, Kara A, Ozdogan M, Sualp Y, Topcu Z, et al. Does music exposure during chemotherapy improve quality of life in early breast cancer patients? A pilot study. Medical Science Monitor 2006;12(5):200-5. [PubMed] [Google Scholar]
Bunt 1995 {published data only}
- Bunt L, Marston-Wyld J. Where words fail music takes over: a collaborative study by a music therapist and a counsellor in the context of cancer care. Music Therapy Perspectives 1995;13(1):46-50. [Google Scholar]
Burke 1997 {published data only}
- Burke M. Effects of physioacoustic intervention on pain management of postoperative gynaecological patients. In: Music Vibration and Health. Cherry Hill, NJ: Jeffrey Books, 1997. [Google Scholar]
Burns 2001b {published data only}
- Burns SJI, Harbuz MS, Hucklebrideg F, Bunt L. A pilot study into the therapeutic effects of music therapy at a self-help cancer center. Alternative Therapies in Health Medicine 2001;7(1):48-56. [PubMed] [Google Scholar]
Canga 2012 {published data only}
- Canga B, Hahm CL, Lucido D, Grossbard ML, Loewy JV. Environmental music therapy apilot study on the effects of music therapy in a chemotherapy infusion suite. Music and Medicine 2012;4(4):221-30. [Google Scholar]
Capitulo 2015 {published data only}
- Capitulo KL. Music therapy to reduce pain and anxiety in children with cancer undergoing lumbar puncture: a randomised clinical trial. American Journal of Maternal/Child Nursing 2015;40(4):268. [Google Scholar]
Cermak 2005 {unpublished data only}
- Cermak AM. The Effect of Music Therapy and Songwriting on Anxiety, Depression, and Quality of Life in Cancer Patients and their Family as Measured by Self-report [Master's thesis]. Tallahassee, FL: Florida State University, 2005. [Google Scholar]
Chi 2009 {unpublished data only}
- Chi G. Music Relaxation Video and Pain Control: a Randomised Controlled Trial for Women Receiving Intracavitary Brachytherapy for Gynecological Cancer [PhD thesis]. Denton, TX: Texas Women's University, 2009. [Google Scholar]
Cuenot 1994 {unpublished data only}
- Cuenot LR. Effects of Brief Adjunctive Music Therapy on Chronic Cancer Pain Intensity [PhD thesis]. Gainesville, FL: University of Florida, College of Nursing, 1994. [Google Scholar]
Dadkhah 2019 {published data only}
- Dadkhah B, Anisi E, Mozaffari N, Amani F, Pourghasemian M. Effect of music therapy with periorbital massage on chemotherapy-induced nausea and vomiting in gastrointestinal cancer: a randomized controlled trial. Journal of Caring Sciences 2019;8(3):165-71. [DOI: 10.1517/jcs.2019.024] [DOI] [PMC free article] [PubMed] [Google Scholar]
Domingo 2015 {published data only}
- Domingo JP, Escudé Matamoros NE, Danés CF, Abelló HV, Carranza JM, Ripoll AR, et al. Effectiveness of music therapy in advanced cancer patients admitted to a palliative care unit: a non-randomised controlled, clinical trial. Music & Medicine 2015;7(1):23-31. [Google Scholar]
Dvorak 2015 {published and unpublished data}
- Dvorak A. Music therapy support groups for cancer patients and caregivers: a mixed methods approach. Canadian Journal of Music Therapy 2015;21(1):69-105. [Google Scholar]
Ezzone 1998 {published data only}
- Ezzone S, Baker C, Rosselet R, Terepka E. Music as an adjunct to antiemetic therapy. Oncology Nursing Forum 1998;25(9):1551-6. [PubMed] [Google Scholar]
Fancourt 2015 {unpublished data only}
- Fancourt D. The Psychoneuroimmunology of Music: Modulation of Psychological State, Stress Levels and Immune Response through Participator Interventions [PhD thesis]. London, England: University College London, 2015. [Google Scholar]
Fernando 2019 {published data only}
- Fernando GVMC, Wanigabadu LU, Vidanagama B, Samaranayaka TSP, Jeewandara JMKC. Adjunctive effects of a short session of music on pain, low-mood and anxiety modulation among cancer patients: a randomized crossover clinical trial. Indian Journal of Palliative Care 2019;25(3):367-73. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Flaugher 2002 {unpublished data only}
- Flaugher M. The Intervention of Music on Perceptions of Chronic Pain, Depression, and Anxiety in Ambulatory Individuals with Cancer [PhD thesis]. Birmingham, AL: University of Alabama at Birmingham, 2002. [Google Scholar]
Frank 1985 {published data only}
- Frank JM. The effects of music therapy and guided visual imagery on chemotherapy induced nausea and vomiting. Oncology Nursing Forum 1985;12(5):47-52. [PubMed] [Google Scholar]
Furioso 2002 {unpublished data only}
- Furioso MM. The Effect of Group Music Therapy on Coping, Psychosocial Adjustment, and Quality of Life for Women with Breast Cancer [PhD thesis]. East Lansing, MI: Michigan State University, 2002. [Google Scholar]
Gencer 2019 {published data only}
- Gencer D, Diel A, Klotzbach K, Christians K, Rauch M, Meissner R, et al. Cancer patients and music: (prospective) results from a survey to evaluate potential complementary treatment approaches. Journal of Cancer Research and Clinical Oncology 2019;145:2141-8. [DOI: 10.1007/s00432-019-02959-3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Giordano 2020 {published data only}
- Giordano F, Zanchi B, De Leonardis F, Rutigliano C, Esposito F, Brienza N, et al. The infulence of music therapy on preoperative anxiety in pediatric oncology patients undergoing invasive procedures. Arts in Psychotherapy 2020;68:101649. [DOI: 10.1016/j.aip.2020.101649] [DOI] [Google Scholar]
Gutsell 2013 {published data only}
- Gutgsell KJ, Schluchter M, Margevicius S, DeGolia PA, McLaughlin B, Harris M, et al. Music therapy reduces pain in palliative care patients: a randomized controlled trial. Journal of Pain and Symptom Management 2013;45:822–31. [DOI: ] [DOI] [PubMed] [Google Scholar]
Hasenbring 1999 {published data only}
- Hasenbring M, Schulz-Kindermann F, Hennings U, Florian M, Linhart D, Ramm G, et al. The efficacy of relaxation/imagery, music therapy and psychological support for pain relief and quality of life: first results from a randomised controlled clinical trial. Bone Marrow Transplantation 1999;23:166. [Google Scholar]
Hogenmiller 1986 {published and unpublished data}
- Hogenmiller JR. The effect of selected classical music on acute pain related to bone marrow aspiration and biopsy in the cancer patient. Oncology Nursing Forum 1986;13(2):86. [Google Scholar]
Huang 2000 {unpublished data only}
- Huang SH. Effects of Music Therapy on Relieving Pain and Symptom Distress among Hospice Cancer Patients [Master's thesis]. Taipei: Taipei Medical College, 2000. [Google Scholar]
Jeppesen 2018 {published data only}
- Jeppesen E, Pedersen C, Larsen K, Walsted E, Rehl A, Ehrenriech J, et al. Music prior to bronchoscopy reduces anxiety in patients with suspected lung cancer. European Respiratory Journal 2018;52:PA2826. [DOI: 10.1183/13993003.congress-2018.PA2826] [DOI] [Google Scholar]
- Jeppesen E, Pedersen CM, Larsen KR, Rehl A, Bartholdy K, Backer V. Positive effect of MusiCure on patients undergoing bronchochoscopy - a randomized controlled trial. European Respiratory Journal 2016;48(Suppl 60):PA3074. [DOI: 10.1183/13993003.congres-2016.PA3074] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeppesen E, Pedersen CM, Larsen KR, Walsted ES, Rehl A, Ehrenreich J, et al. Listening to music prior to bronchoscopy reduces anxiety - a randomized controlled trial. European Clinical Respiratory Journal 2019;6:1583517. [DOI: 10.1080/20018525.2019.1583517] [DOI] [PMC free article] [PubMed] [Google Scholar]
Jourt‐Pineau 2012 {published data only}
- Jourt-Pineau C. Music therapy in oncology: an evaluation of the effects of music therapy on pain and anxiety in hospitalized oncology patients [La musicotherapie en oncologie: evalutaion des effets de la musicotherapie sur la douleur et l'anxiete chez les patients hospitalises et/ou suivis en service d'oncologie]. La Revue Francaise de Musicotherapie 2012;32(1):4-108. [Google Scholar]
Jourt‐Pineau 2013 {published data only}
- Jourt-Pineau C, Guetin S, Vedrine L, Le Moulec S, Poirier JM, Ceccaldi B. Effects of music therapy on pain and anxiety in treating cancer patients: a feasibility study. Douleurs 2013;14(4):200-7. [Google Scholar]
Karagozoglu 2013 {published data only}
- Karagozoglu S, Tekyasar F, Yilmaz FA. Effects of music therapy and guided visual imagery on chemotherapy-induced anxiety and nausea-vomiting. Journal of Clinical Nursing 2013;22(1-2):39-50. [DOI] [PubMed] [Google Scholar]
Kemper 2008 {published data only}
- Kemper KJ, Hamilton CA, McLean TW, Lovato J. Impact of music on paediatric oncology outpatients. Pediatric Research 2008;64(1):105-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kongsawatvorakul 2016 {published data only}
- Kongsawatvorakul C, Charakorn C, Paiwattananupant K, Lekskul N, Rattanasiri S, Lertkhachonsuk AA. Limited impact of music therapy on patient anxiety with the large loop excision of transformation zone procedure: a randomized controlled trial. Asian Pacific Journal of Cancer Prevention 2016;17:2853-6. [PMID: ] [PubMed] [Google Scholar]
Krishaswamy 2016 {published data only}
- Krishnaswamy P, Nair S. Effect of music therapy on pain and anxiety levels of cancer patients: a pilot study. Indian Journal of Palliative Care 2016;22:307-11. [DOI: 10.4103/0973-1075.185042] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lawson 2016 {published data only}
- Lawson ML, Glennon C, Fuscus V, Harrell VS, Krause KA, Moore AB, et al. Effects of making art and listening to music on symptoms related to blood and marrow transplantation. Oncology Nursing Forum 2016;43(2):E56-E63. [DOI: 10.1188/16.ONF.E56-E63] [DOI] [PubMed] [Google Scholar]
Lee 2000 {unpublished data only}
- Lee YJ. Effects of Music Therapy on Pain Level, Physiological Response and Psychological Perception of Cancer Patients [Master's thesis]. Taipei: Chang-Gung University, 2000. [Google Scholar]
Lee 2012 {published data only}
- Lee EJ, Bhattacharya J, Sohn C, Verres R. Monochord sounds and progressive muscle relaxation reduce anxiety and improve relaxation during chemotherapy: a pilot EEG study. Complementary Therapies in Medicine 2012;20(6):409-16. [DOI] [PubMed] [Google Scholar]
Lesiuk 2015 {published data only}
- Lesiuk T. The effect of mindfulness-based music therapy on attention and mood in women receiving adjuvant chemotherapy for breast cancer: a pilot study. Oncology Nursing Forum 2015;42(3):276-82. [DOI: ] [DOI] [PubMed] [Google Scholar]
Liao 2018 {published data only}
- Liao J, Wu Y, Zhao Y, Zhao YC, Zhang X, Zhao N, et al. Progressive muscle relaxation combined with Chinese medicine five-element music on depression for cancer patients: a randomized controlled trial. Chinese Journal of Integrative Medicine 2018;24(5):343-7. [DOI: 10.1007/s11655-017-2956-0] [DOI] [PubMed] [Google Scholar]
Liu 2014 {published data only}
- Liu X, Yang H, Zou R, Tang F, Tang H, Lou Y. The effect of music therapy and countermeasures design during cancer therapy in China. Psycho-oncology 2014;23(S3):193. [Google Scholar]
Liu 2019 {published data only}
- Liu H, Gao X, Hou Y. Effects of mindfulness-based stress reduction combined with music therapy on pain, anxiety, and sleep quality in patients with osteosarcoma. Brazilian Journal of Psychiatry 2019;4(16):540-5. [DOI: 10.1590/1516-4446-2018-0346] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lopez 2019 {published data only}
- Lopez G, Christie AJ, Powers-James C, Bae MS, Dibaj SS, Gomez R, et al. The effects of inpatient music therapy on self-reported symptoms at an academic cancer center: a preliminary report. Supportive Care in Cancer 2019;27:4207-12. [DOI: 10.1007/s00520-019-04713-4] [DOI] [PubMed] [Google Scholar]
Na Cholburi 2004 {published data only}
- Na Cholburi JS, Hanucharurnkul S, Waikakul W. Effects of music therapy on anxiety and pain in cancer patients. Thai Journal of Nursing Research 2004;8(3):173-81. [Google Scholar]
Nakayama 2009 {published data only}
- Nakayama H, Kikuta F, Takeda H. A pilot study on effectiveness of music therapy in hospice in Japan. Journal of Music Therapy 2009;46(2):160-72. [DOI] [PubMed] [Google Scholar]
Perkins 2018 {published data only}
- Perkins RS, Boyce M, Byrtek MC, Ellis RC, Hill C, Fitzpatrick PS, et al. Roadmap to wellness: exploring live customized music at the bedside for hospitalized children. Frontiers in Oncology 2018;8(21):1-6. [DOI: 10.3389/fonc.2018.00021] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pfaff 1989 {published data only}
- Pfaff VK, Smith KE, Gowan D. The effects of music-assisted relaxation on the distress of paediatric cancer patients undergoing bone marrow aspirations. Children's Health Care 1989;18(4):232-6. [Google Scholar]
Pienta 1998 {published data only}
- Pienta D. The effects of guided imagery & music on the self esteem and well-being of cancer survivors. Unpublished paper. Data on file.
Robinson 2009 {unpublished data only}
- Robinson A. Music During Chemotherapy. Effects on Patients with Gynecologic Malignancies with Emphasis on Physical Symptoms and Coping: Results of a Prospective Study. [Musik während der Chemotherapie. Effekte auf Patientinnen mit Gynäkologischen Malignomen unter Besonderer Berücksichtigung von Körperlichen Beschwerden und Krankheitsverarbeitung: Ergebnisse einer Prospektiven Studie] [PhD thesis]. Berlin: Universitätsmedizin, Berlin, 2009. [Google Scholar]
Rose 2008 {published data only}
- Rose JP, Weis J. Sound meditation in oncological rehabilitation: a pilot study of a receptive music therapy group using the monochord. Forschende Komplementarmedizin 2008;15(6):335-43. [DOI] [PubMed] [Google Scholar]
Sadat 2009 {published data only}
- Sadat Hoseini AAS. Effect of music therapy on chemotherapy nausea and vomiting in children with malignancy. Journal of Hayat 2009;15(2):5-14. [Google Scholar]
Sahler 2003 {published data only}
- NCT00032409. The effects of music therapy-based stress reduction on bone marrow transplant recipients. clinicaltrials.gov/ct2/show/NCT00032409 (date first received 20 March 2002).
- Sahler OJZ, Hunter BC, Liesveld JL. The effect of using music therapy with relaxation imagery in the management of patients undergoing bone marrow transplantation: a pilot feasibility study. Alternative Therapies in Health and Medicine 2003;9(6):70-4. [PubMed] [Google Scholar]
Sanchez‐Juaregui 2019 {published data only}
- Sanchez-Jauregui T, Tellez A, Juarez-Garcia D, Garchi CH, Garcia FE. Clinical hypnosis and music in breast biopsy: a randomized clinical trial. American Journal of Clinical Hypnosis 2018;61(3):244-57. [DOI: 10.1080/00029157.2018.1489776] [DOI] [PubMed] [Google Scholar]
Schur 1987 {published data only}
- Schur JM. Alleviating behavioral distress with music or Lamaze pant-blow breathing in children undergoing bone marrow aspirations and lumbar punctures. Dissertation Abstracts International, 48(3-B)889 1987.
Sedei 1980 {unpublished data only}
- Sedei C. The Effectiveness of Music Therapy on Specific Statements Verbalized by Cancer Patients [Master's thesis]. Fort Collins, CO: Colorado State University, 1980. [Google Scholar]
Shao 2019 {published data only}
- Shao J, Xiao T, Shi M, Zhou X, Wang Z, Lin T, et al. Effect of multimedia-based nursing visit on perioperative anxiety in esophageal squamous cell carcinoma patients undergoing video-assisted thoracoscopic surgery. Psychology, Health & Medicine 2019;24(10):1198-206. [DOI: 10.1080/13548506.2019.1595678] [DOI] [PubMed] [Google Scholar]
Soo 2016 {published data only}
- Soo MS, Jarosz JA, Wren AA, Soo AE, Mowery YM, Johnson KS, et al. Imaging-guided core-needle breast biopsy: impact of meditation and music interventions on patient anxiety, pain, and fatigue. Journal of the Ammerican Colloge of Radiology 2016;13:526-34. [DOI: 10.1016/j.jacr.2015.12.004] [DOI] [PubMed] [Google Scholar]
Sriasih 2019 {published data only}
- Sriasih NK, Allenidekania A, Wanda D. The effects of the COMMASH-E intervention on the fatigue, sleep quality and functional status of children with cancer in Indonesia. Comprehensive Child and Adolescent Nursing 2019;42(S1):197-207. [DOI: 10.1080/24694193.2019.1594451] [DOI] [PubMed] [Google Scholar]
Standley 1992 {published data only}
- Standley JM. Clinical applications of music and chemotherapy: the effects on nausea and emesis. Music Therapy Perspectives 1992;10(1):27-35. [Google Scholar]
Stark 2012 {unpublished data only}
- Stark JC. Perceived Benefits of Group Music Therapy for Breast Cancer Survivors: Mood, Psychosocial Wellbeing, and Quality of Life [PhD thesis]. Michigan, USA: Michigan State University, 2012. [Google Scholar]
Tan 2008 {published data only}
- Tan BL, Sin ACF, Ho SM, Lee KH, Poh J, Chua GP, et al. Effect of music in reducing anxiety levels among patients who receive their first dose of chemotherapy treatment. Singapore General Hospital Proceedings 2008;17(1):46-56. [Google Scholar]
Tellez 2016 {published data only}
- Tellez A, Sanchez-Jauregui T, Juarez-Garcia DM. Breast biopsy: the effects of hypnosis and music. International Journal of Clinical and Experimental Hypnosis 2016;64(4):456-69. [DOI: 10.1080/00207144.2016.1209034] [DOI] [PubMed] [Google Scholar]
Thompson 2011 {unpublished data only}
- Thompson S. The Effect of Group Music Therapy on Anxiety, Depression, Quality of Life and Coping with Women with Stage I and Stage II Breast Bancer: a Mixed Methods study [PhD thesis]. Melbourne: The University of Melbourne, 2011. [Google Scholar]
Tilch 1999 {published data only}
- Tilch S, Haffa-Schmidt U, Wandt H, Kappauf H, Schafer K, Birkmann J, et al. Supportive music therapy improves mood state in patients undergoing myeloablative chemotherapy. Bone Marrow Transplantation 1999;23:170. [Google Scholar]
Toccafondi 2018 {published data only}
- Toccafondi A, Bonacchi A, Mambrini A, Miccinesi G, Prosseda R, Cantore M. Live music intervention for cancer inpatients: the Music Givers format. Palliative and Supportive Care 2018;16:777-84. [DOI: 10.1017/S1478951517000165] [DOI] [PubMed] [Google Scholar]
Uggla 2018 {published data only}
- Uggla L, Bonde LO, Hammar U, Wrangsjo B, Gustafsson B. Music therapy supported the health-realted quality of life for children undergoing haematopoietic stem cell transplants. Acta Paediatrica 2018;107:1986-94. [DOI: 10.1111/apa.14515] [DOI] [PMC free article] [PubMed] [Google Scholar]
Vohra 2011 {published data only}
- Vohra S, Nilsson S. Does music therapy reduce pain and anxiety in children with cancer undergoing lumbar puncture? Focus on Alternative and Complementary Therapies 2011;16(1):66-7. [Google Scholar]
Walden 2001 {published data only}
- Walden EG. The effects of group music therapy on mood states and cohesiveness in adult oncology patients. Journal of Music Therapy 2001;38(3):212-38. [DOI] [PubMed] [Google Scholar]
Warth 2018 {published data only}
- Warth M, Kessler J, Van Kampen J, Ditzen B, Bardenheuer H. ‘Song of Life’: music therapy in terminally ill patients with cancer. BMJ Supportive & Palliative Care 2018;8:167-70. [DOI: 10.1136/bmjspcare-2017-001475] [DOI] [PubMed] [Google Scholar]
Washington 1990 {unpublished data only}
- Washington DR. The Effect of Music Therapy on Anxiety Levels of Terminally Ill Cancer Patients: a Pilot Study [Master's thesis]. Philadelphia, PA: Hahnemann University, USA, 1990. [Google Scholar]
Weber 1997 {published data only}
- Weber S, Nuessler V, Wilmanns W. A pilot study on the influence of receptive music listening on cancer patients during chemotherapy. International Journal of Arts Medicine 1997;5(2):27-35. [Google Scholar]
Whitney 2013 {unpublished data only}
- Whitney Q. The Effect of Music Therapy on Five-year Disease-free Survival Rates in Pediatric Neuroblastoma [Master's thesis]. Ithaca, NY: Weill Medical College of Cornell University, 2013. [Google Scholar]
Wurr 2000 {unpublished data only}
- Wurr CJ. Evaluation of music therapy in pediatric oncology - a pilot study. Academic Unit of Child & Adolescent Mental Health, University of Leeds, UK 2000.
Yang 2019 {published data only}
- Yang J, Weng L, Chen Z, Cai H, Lin X, Hu Z, et al. Development and testing of a mobile app for pain management among cancer patients discharged from hospital treatment: randomized controlled trial. Journal of Medical Internet Research mHealth and uHealth 2019;7(5):e12542. [DOI: 10.2196/12542] [DOI] [PMC free article] [PubMed] [Google Scholar]
Yildirim 2007 {published data only}
- Yildirim S, Gurkan A. The influence of music on anxiety and the side effects of chemotherapy [Muzigin, kemoterapi yan etkilerine ve kaygi duzeyine etkisi]. Anadolu Psikiyatri Dergisi 2007;8(1):37-45. [Google Scholar]
Zimmernam 1989 {published data only}
- Zimmerman L, Pozehl B, Duncan K, Schmitz R. Effects of music in patients who had chronic cancer pain. Western Journal of Nursing Research 1989;11(3):293-309. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Banyai 2017 {published data only}
- Banyai E, Jozsa E, Jakubovits E, Vargay A, Zsigmond O, Horvath Z. Evidence based research on the role of hypnosis as a psychological intervention in the care of breast cancer patients: a randomised prosepctive controlled study. Psycho-Oncology 2017;26(Suppl 3):61. [Google Scholar]
Bates 2019 {published data only}
- Bates DS, Dileo C. The Effects of Pre-Transplant Music Therapy on Distress, Quality of Life, Pain, Anxiety, Mood, and Pain Medication for Patients Undergoing Hematopoietic Stem Cell Transplant [PhD Thesis]. Philadelphia: Temple University, 2019. [Google Scholar]
Colwell 2020 {published data only}
- Colwell CM, Fiore J. Feasibility of patient-created Orffchant as a music-based intervention in supportive cancer care. Journal of Music Therapy 2020;54:e1-e31. [DOI] [PubMed] [Google Scholar]
Dehkhoda 2016 {published data only}
- Dehkhoda F, Vinayak S, Vinayak R. Clinical trial of effect of music-therapy on sleep quality in blood cancer patients. Nordic Journal of Music Therapy 2016;25(Suppl 1):124-5. [DOI: 10.1080/08098131.2016.1180154] [DOI] [Google Scholar]
Dileo 2015 {unpublished data only}
- Dileo C. Music entrainment with cancer patients with chronic pain. www.temple.edu/boyer/community/aqlresearch.asp (accessed 23 January 2016).
Duong 2013 {unpublished data only}
- Duong HK, Bates D, Rybicki LA, Kalaycio M, Steven A, Sobecks R, et al. A randomised study of music therapy in patients undergoing autologous stem cell transplant: decrease in narcotic medication use for pain control. In: 55th Annual Meeting of the American Society of Hematology; 2013 Dec 7-10; New Orleans, LA. New Orleans, LA: American Society of Hematology, 2013.
Hseih 2019 {published data only}
- Hsieh FC, Miao NF, Tseng IJ, Chiu HL, Kao CC, Liu D, et al. Effect of home-based music intervention versus ambient music on breast cancer survivors in the community: a feasibility study in Taiwan. European Journal of Cancer Care 2019;28(4):e13064. [DOI: 10.1111/ecc.13064] [DOI] [PubMed] [Google Scholar]
Massimiliani 2017 {published data only}
- Massimiliani B, Pellegrino R, Donnarumma L, Perrone L, Riondino S, Roselli M. Music intervention during chemotherapy infusion reduces anxiety in oncological patients. Annals of Oncology 2017;28(Suppl 6):VI82. [DOI: ] [Google Scholar]
Mondanaro 2020 {unpublished data only}
- Mondanaro JF, Sara G, Thachil R, Pranjić M, Rossetti A, Sim GE, et al. The effects of clinical music therapy on resiliency in adults undergoing infusion: a randomized, controlled trial. Journal of Pain and Symptom Management 2021;61(26):1099-1108. [DOI: 10.1016/j.jpainsymman.2020.10.032] [DOI] [PubMed] [Google Scholar]
- NCT02261558. Effects of clinical music improvisation on resiliency of adults undergoing infusion therapy. http://clinicaltrials.gov.
O'Brien 2010 {unpublished data only}
- O'Brien E. The Effect of the Guided Original Lyrics and Music (GOLM) Songwriting Protocol on Cancer Patients' Mood, Distress Levels, Quality of Life, and Satisfaction with Hospital Stay [PhD thesis]. Melbourne: University of Melbourne, in progress. [Google Scholar]
Secord 2016 {published data only}
- Secord S, Whitmore S, Derman S, Gill J, Goktepe O. A randomized control trial evaluating perioperative music therapy on postoperative pain for women undergoing surgical treatment for breast cancer. In: PAINweek Abstract Book Postgraduate Medicine. Vol. 128, Suppl 2. 2016. [DOI: 10.1080/00325481.2016.1224633] [DOI]
Toole 2017 {published data only}
- Toole M, Bendinger GM, Ensor JE, Alvarez Tapias C, Smith E, McGuire E, et al. A randomized study of personalized music therapy for patients with early stage breast cancer receiving chemotherapy. Cancer Research 2017;77:4. [DOI: 10.1158/1538-7445.SABCS16-OT3-08-01] [DOI] [Google Scholar]
Xiao 2018 {published data only}
- Xiao Y, Li L, Xie Y, Xu J, Liu Y. Effects on aroma therapy and music intervention on paitn and anxious for breast cancer patients in the perioperative period. Zhong Nan Da Xue Xue Bao Yi Xue Ban [Journal of Central South University] 2018;43(6):656-61. [DOI: <span class="citation-doi">10.11817/j.issn.1672-7347.2018.06.013</span>] [DOI] [PubMed] [Google Scholar]
Zhai 2017 {published data only}
- Zhai W, Liu N. Effect of TCM music therapy for hospice care of patients with gastrointestinal cancer. World Chinese Journal of Digestology 2017;25(4):388-91. [Google Scholar]
Zhang 2017 {published data only}
- Zhang L. Effect of patients tailored music intervention in relieving chemotherapy induced nausea and vomiting. Cancer Nursing (International Conference on Cancer Nursing) 2017;40(Suppl 1):E5. [Google Scholar]
References to ongoing studies
ChiCTR1800014398 {published data only}
- ChiCTR1800014398. The effects of multidimensional psychological interventions on the chemotherapy response in patients with epithelial ovarian cancer\ [The effects of multidimensional psychological interventions on the chemotherapy response in patients with epithelial ovarian cancer: a prospective multi-center trial]. chictr.org.cn/showproj.aspx?proj=24284 (first received 11 January 2018). [ChiCTR1800014398]
ChiCTR1800020016 {published data only}
- ChiCTR1800020016. Effect of music therapy for anxiety and depression in elderly patients undergoing lung cancer surgery. chictr.org.cn/showproj.aspx?proj=33732 (first received 12 November 2018). [ChiCTR1800020016]
ChiCTR1900022098 {published data only}
- ChiCTR1900022098. Effect of music on perioperative period of thoracoscopy patients with lung cancer [Perioperative effect of music therapy on patients wth thoracoscopic lung cancer: a randomized controlled trial]. chictr.org.cn/showproj.aspx?proj=37238 (first received 25 March 2019). [ChiCTR1900022098]
ChiCTR‐IOR‐16010190 {published data only}
- ChiCTR-IOR-16010190. Directed imagery and five-element music on advanced non-small cell lung cancer patients with psycholgical distress in chemotherapy period: a randomized controlled trial. chictr.org.cn/showproj.aspx?proj=17090 (first received 19 December 2016).
CTRI/2017/09/009919 {published data only}
- CTRI/2017/09/009919. Effectiveness of music on pain, heart rate, blood pressure, temperature, anxiety and quality of life among patients with cancer during chemotherapy [Effect of music therapy on bio-physiological and psychological outcomes during chemotherapy among patients with cancer]. ctri.nic.in/Clinicaltrials/pmaindet2.php?trialid=15411&EncHid=&userName=Imran (first received 26 September 2017). [CTRI/2017/09/009919]
CTRI/2018/09/015801 {published data only}
- CTRI/2018/09/015801. Trial on the effect of Indian classical music on head and neck cancer patients [A randomized controlled trial on the effect of Indian classical music for chemotherapy and radiotherapy induced anxiety, pain and mood disturbance in head and neck cancer - a pilot study]. ctri.nic.in/Clinicaltrials/pmaindet2.php?trialid=25937 (first received 24 September 2018). [CTRI/2018/09/015801]
IRCT20120905010744N2 {published data only}
- IRCT20120905010744N2. The effectiveness of hypnotherapy, relaxation and music therapy on control of pain in children with cancer. en.irct.ir/trial/28389 (first received 14 July 2019). [IRCT20120905010744N2]
IRCT20130731014229N8 {published data only}
- IRCT20130731014229N8. Effect of music on blood cell levels in patients with acute leukemia [Effect of music on blood cell levels in patients with acute leukemia under chemotherapy]. en.irct.ir/trial/38080 (first received 16 March 2019). [IRCT20130731014229N8]
NCT0258312 {unpublished data only}
- NCT02583126. Guided imagery and music for the reduction of side effects of chemotherapy in teenagers [The effect and meaning of a designed guided imagery and music intervention on anticipatory, acute, and delayed side effects of chemotherapy in teenagers with cancer: a randomized controlled multisite study]. clinicaltrials.gov/ct2/show/NCT02583126 (first received 22 October 2015).
NCT02583139 {unpublished data only}
- NCT02583139. Designed music narratives for the reduction of side effects of chemotherapy in children (7-12 years) with cancer [The effect and meaning of designed music narratives on anticipatory, acute, and delayed side effects of chemotherapy in children (7-12 years) with cancer: a randomized controlled multisite study]. clinicaltrials.gov/ct2/show/NCT02583139 (first received 22 October 2015).
NCT03378089 {published data only}
- NCT03378089. Music therapy and hematopoietic stem cell transplant [The effects of pre-transplant music thearpy for patients undergoing hematopoietic stem cell transplant]. clinicaltrials.gov/ct2/show/NCT03378089 (first received 19 December 2017). [NCT03378089]
NCT03432247 {published data only}
- NCT03432247. Pain management support study for patients with advanced cancer [Mechanisms of music therapy to palliate pain in patients with advanced cancer]. clinicaltrials.gov/ct2/show/NCT03432247 (first received 14 February 2018). [NCT03432247]
NCT03511079 {published data only}
- NCT03511079. Music as a perioperative therapy in breast cancer patients [Impact of perioperative music on quality of life measures and biomarker levels in breast cancer patients]. clinicaltrials.gov/ct2/show/NCT03511079 (first recieved 27 April 2018). [NCT03511079]
NCT03538223 {published data only}
- NCT03538223. Music listening in radiotherapy treatment (MuLi_RT) [Music listening to reduce anxiety and stress in patients undergoing radiotherapy]. clinicaltrials.gov/ct2/show/NCT03538223 (first received 29 May 2018. [NCT03538223]
NCT03683420 {published data only}
- NCT03683420. Music in reducing distress in participants with cancer during chemotherapy treatment [Using music as a tool for distress reduction during cancer treatment]. clinicaltrials.gov/ct2/show/NCT03683420 (first received 25 September 2018. [NCT03683420]
NCT03740984 {published data only}
- NCT03740984. Effects of music or hypnotherapy on cancer patients during chemotherapy (F-Chem) [Effects of music or hypnotherapy on cancer patients during chemotherapy - A prospective off-centre randomized placebo-controlled trial]. clinicaltrials.gov/ct2/show/NCT03740984 (first received 14 November 2018. [NCT03740984]
NCT03955003 {published data only}
- NCT03955003. Fatigue, anxiety, music, and entertainment (FAME) study (FAME) [Addressing fatigue, anxiety, and cognitive impairment through thythmic effects: A pilot feasibility study using a group drumming intervention with cancer patients]. clinicaltrials.gov/ct2/show/NCT03955003 (first received 17 May 2019). [NCT03955003]
NCT04052074 {published data only}
- NCT04052074. Complementary therapy in home palliative care patients and their caregivers (COMTHECARE) [Complementary therapy in home palliative care patients and their caregivers. A clinical trial]. clinicaltrials.gov/ct2/show/NCT04052074 (first received 14 July 2020). [NCT04052074]
NTR7546 {published data only}
- NTR7546. Intraoperative Music to PROMote PaTient oUtcome (IMPROMPTU): a double-blind, placebo-controlled, randomized multicenter trial. trialregister.nl/trial/7330 (first received 1 October 2018). [NTR7546]
Additional references
Bradt 2010
- Bradt J, Dileo C. Music therapy for end-of-life care. Cochrane Database of Systematic Reviews 2010, Issue 1. Art. No: CD007169. [DOI: 10.1002/14651858.CD007169.pub2] [DOI] [PubMed] [Google Scholar]
Bradt 2013a
- Bradt J, Dileo C, Potvin N. Music for stress and anxiety reduction in coronary heart disease patients. Cochrane Database of Systematic Reviews 2013, Issue 12. Art. No: CD006577. [DOI: 10.1002/14651858.CD006577] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bradt 2013b
- Bradt J, Dileo C, Shim M. Music interventions for preoperative anxiety. Cochrane Database of Systematic Reviews 2013, Issue 6. Art. No: CD006908. [DOI: 10.1002/14651858.CD006908.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bradt 2014
- Bradt J, Dileo C, Grocke D. Music interventions for mechanically ventilated patients. Cochrane Database of Systematic Reviews 2014, Issue 12. Art. No: CD006902. [DOI: 10.1002/14651858.CD006902.pub3] [DOI] [PubMed] [Google Scholar]
Burns 1999
- Burns DS. The effect of the Bonny methods of guided imagery and music on the quality of life and cortisol levels of cancer patients. Journal of Music Therapy 2001;38(1):51-65. [DOI: 10.1093/jmt/38.1.51] [DAI-A 61/01] [DOI] [PubMed] [Google Scholar]
Cohen 1988
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd edition. Hillsdale, NJ: Lawrence Earlbaum Associates, 1988. [Google Scholar]
Cucherat 2007
- Cucherat M. Quantitative relationship between resting heart rate reduction and magnitude of clinical benefits in post-myocardial infarction: a meta-regression of randomized clinical trials. European Heart Journal 2007;28(24):3012-9. [DOI] [PubMed] [Google Scholar]
Deeks 2001
- Deeks JJ, Altman DG, Bradburn MJ. Statistical methods for examining heterogeneity and combining results from several studies in meta-analysis. In: Egger M, Davey Smith G, Altman DG, editors(s). Systematic Reviews in Health Care: Meta-Analysis in Context. 2nd edition. London: BMJ Publication Group, 2001:285-312. [Google Scholar]
Dileo 1999
- Dileo C. A classification model for music and medicine. In: Applications of Music in Medicine. National Association of Music Therapy, 1999:1-6. [Google Scholar]
Dileo 2005
- Dileo C, Bradt J. Medical Music Therapy: A Meta-analysis & Agenda for Future Research. Cherry Hill: Jeffrey Books, 2005. [Google Scholar]
Dileo 2006
- Dileo C. Effects of music and music therapy on medical patients: a meta-analysis of the research and implications for the future. Journal of the Society of Integrative Oncology 2006;4(2):67-70. [DOI] [PubMed] [Google Scholar]
Dileo 2007
- Dileo C, Bradt J. Music therapy: applications to stress management. In: Lehrer & Woolfolk, editors(s). Principles and Practice of Stress Management. 3rd edition. New York: Guilford Press, 2007. [Google Scholar]
Elbourne 2002
- Elbourne DR, Altman DG, Higgins JPT, Curtin F, Worthington HV, Vaillancourt JM. Meta-analyses involving cross-over trials: methodological issues. International Journal of Epidemiology 2002;31:140–9. [DOI] [PubMed] [Google Scholar]
GRADEpro 2020 [Computer program]
- McMaster University (developed by Evidence Prime, Inc.) GRADEpro Guideline Development Tool. McMaster University (developed by Evidence Prime, Inc.), 2020.
Haun 2001
- Haun M, Mainous R, Looney S. Effect of music on anxiety of women awaiting breast biopsy. Behavioral Medicine 2001;27(3):127-32. [DOI] [PubMed] [Google Scholar]
Higgins 2002
- Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Statistics in Medicine 2002;21:1539-58. [DOI] [PubMed] [Google Scholar]
Higgins 2021
- Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.2 (updated February 2021). Cochrane, 2021. Available from www.training.cochrane.org/handbook. 2021.
Howlader 2019
- Howlader N, Noone AM, Krapcho M, Miller D, Brest A, Yu M, et al. SEER Cancer Statistics Review, 1975-2016. seer.cancer.gov/csr/1975_2016/ (accessed prior to 25 August 2021).
Johnson 2011
- Johnson DC, Polusny MA, Erbes CR, King D, King L, Litz BT, et al. Development and initial validation for the Response to Stressful Experiences Scale. Military Medicine 2011;176(2):161-9. [DOI] [PubMed] [Google Scholar]
King 2003
- King CR, Hinds BS. Quality of life from Nursing and Patient Perspectives: Theory, Research and Practice. Sudbury: Jones and Bartlett Publishers, 2003. [Google Scholar]
Kohler 2020
- Köhler F, Martin ZS, Hertrampf RS, Gäbel C, Kessler J, Ditzen B, et al. Music therapy in the psychosocial treatment of adult cancer patients: a systematic review and meta-analysis. Frontiers in Psychology 2020;11:651. [DOI: 10.3389/fpsyg.2020.00651] [DOI] [PMC free article] [PubMed] [Google Scholar]
Langendam 2013
- Langendam MW, Akl EA, Dahm P, Glasziou P, Guyatt G, Schunemann HJ. Assessing and presenting summaries of evidence in Cochrane Reviews. Systematic Reviews 2013;23(2):81. [DOI] [PMC free article] [PubMed] [Google Scholar]
Magill 2009
- Magill L. Meaning of the music: the role of music in palliative care music therapy as perceived by bereaved caregivers of advanced cancer patients. American Journal of Hospice and Palliative Medicine 2009;26(1):33-9. [DOI] [PubMed] [Google Scholar]
Magill 2011
- Magill L, O’Callaghan C. Music therapy in supportive cancer care. Music and Medicine 2011;3:7-8. [Google Scholar]
Magill 2015
- Magill L. Music therapy in oncology. In: Breitbart WS, Butow PN, Jacobsen PB, Lam WWT, Lazenby M, Loscalzo MJ, editors(s). Psycho-Oncology. 3rd edition. New York: Oxford University Press, 2015:499-502. [Google Scholar]
Massie 2004
- Massie MJ. Prevalence of depression in patients with cancer. Journal of the National Cancer Institute. Monographs 2004;32:57-71. [DOI] [PubMed] [Google Scholar]
McAuley 2000
- McAuley L, Pham B, Tugwell P, Moher D. Does the inclusion of grey literature influence estimates of intervention effectiveness reported in meta-analyses? Lancet 2000;356(9237):1228-31. [DOI] [PubMed] [Google Scholar]
McClean 2012
- McClean S, Bunt L, Daykin N. The healing and spiritual properties of music therapy at a cancer care centre. Journal of Alternative and Complementary Medicine 2011;18(4):402-7. [DOI] [PubMed] [Google Scholar]
McCracken 2009
- McCracken LM, Keogh E. Acceptance, mindfulness, and values-based action may counteract fear and avoidance of emotions in chronic pain: an analysis of anxiety sensitivity. Journal of Pain 2009;10(4):408-15. [DOI] [PubMed] [Google Scholar]
McKinney 2002
- McKinney CH. Quantitaive research in guided imagery and music (GIM): a review. In: Bruscia KE, Grocke DE, editors(s). Guided Imagery and Music: the Bonny Method and Beyond. Gilsum, New Hampshire, US: Barcelona, 2002:449-466. [Google Scholar]
McNair 1971
- McNair DM, Lorr M, Droppleman LF. Manual for the Profile of Mood States. San Diego, CA: Educational and Industrial Testing Services, 1971. [Google Scholar]
Meader 2014
- Meader N, King K, Llewellyn A, Norman G, Brown J, Rodgers M, et al. A checklist designed to aid consistency and reproducibility of GRADE assessments: development and pilot validation. Systematic Reviews 2014;3:82. [DOI] [PMC free article] [PubMed] [Google Scholar]
Montgomery 2000
- Montgomery GH, Bovbjerg DH. Pre-infusion expectations predict post-treatment nausea during repeated adjuvant chemotherapy infusion for breast cancer. British Journal of Health Psychology 2000;5(2):105-19. [Google Scholar]
Nightingale 2013
- Nightingale CJ, Rodriguez C, Carnaby G. The impact of music interventions on anxiety for adult cancer patients: a meta-analysis and systematic review. Integrative Cancer Therapies 2013;12(5):393-403. [DOI] [PubMed] [Google Scholar]
Norton 2004
- Norton TR, Manne SL, Rubin S, Carlson J, Hernandez E, Edelson MI, et al. Prevalence and predictors of psychological distress among women with ovarian cancer. Journal of Clinical Oncology 2004;22(5):919-26. [DOI] [PubMed] [Google Scholar]
O'Callaghan 2015
- O’Callaghan C, Magill L. Music therapy with adults diagnosed with cancer and their families. In: Edwards J, editors(s). Oxford Handbook of Music Therapy. Oxford University Press, 2015:112-34. [Google Scholar]
Parle 1996
- Parle M, Jones B, Maguire P. Maladaptive coping and affective disorders among cancer patients. Psychological Medicine 1996;26(4):735-44. [DOI] [PubMed] [Google Scholar]
Raison 2003
- Raison CL, Miller AH. Depression in cancer: new developments regarding diagnosis and treatment. Biological Psychiatry 2003;54(3):283-94. [DOI] [PubMed] [Google Scholar]
Review Manager 5 2020 [Computer program]
- Nordic Cochrane Centre, the Cochrane Collaboration Review Manager 5 (RevMan 5). Version 5.4.1. Copenhagen: Nordic Cochrane Centre, the Cochrane Collaboration, 2020.
Robb 2010
- Robb SL, Carpenter JS, Burns DS. Reporting guidelines for music-based interventions. Journal of Health Psychology 2010;16(2):342-52. [DOI: 10.1177/1359105310374781] [DOI] [PMC free article] [PubMed] [Google Scholar]
Rossettini 2018
- Rossettini G, Carlino E, Testa M. Clinical relevance of contextual factors as triggers of placebo and nocebo effects in musculoskeletal pain. BMC Muscoskeletal Disorders 2018;19(27):e-pub. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Schünemann 2011
- Schünemann HJ, Oxman AD, Higgins JPT, Vist GE, Glasziou P, Guyatt GH. Chapter 11: Presenting results and ‘Summary of findings' tables. In: Higgins JPT, Green S (editors), Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from training.cochrane.org/handbook/archive/v5.1.
Sellick 1999
- Sellick SM, Crooks DL. Depression and cancer: an appraisal of the literature for prevalence, detection, and practice guideline development for psychological interventions. Psycho-Oncology 1999;8(4):315-33. [DOI] [PubMed] [Google Scholar]
Spielberger 1983
- Spielberger CD, Gorsuch RL, Lushene PR, Vagg PR, Jacobs AG. Manual for the State-Trait Anxiety Inventory. Palo Alto: Consulting Psychologists Press, Inc, 1983. [Google Scholar]
Thune‐Boyle 2006
- Thune-Boyle IC, Myers LB, Newman SP. The role of illness beliefs, treatment beliefs, and perceived severity of symptoms in explaining distress in cancer patients during chemotherapy treatment. Behavioral Medicine 2006;32(1):19-29. [DOI] [PubMed] [Google Scholar]
Van't Spijker 1997
- Van't Spijker A, Trijsburg RW, Duivenvoorden HJ. Psychological sequelae of cancer diagnosis: a meta-analytical review of 58 studies after 1980. Psychosomatic Medicine 1997;59(3):280-93. [DOI] [PubMed] [Google Scholar]
Zhang 2012
- Zhang JM, Wang P, Yao J, Zhao L, Davis MP, Walsh D, et al. Music interventions for psychological and physical outcomes in cancer: a systematic review and meta-analysis. Supportive Care in Cancer 2012;20(12):3043-53. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Bradt 2011
- Bradt J, Dileo C, Grocke D, Magill L. Music interventions for improving psychological and physical outcomes in cancer patients. Cochrane Database of Systematic Reviews 2011, Issue 8. Art. No: CD006911. [DOI: 10.1002/14651858.CD006911.pub2] [DOI] [PubMed] [Google Scholar]
Bradt 2016
- Bradt J, Dileo C, Magill L, Teague A. Music interventions for improving psychological and physical outcomes in cancer patients. Cochrane Database of Systematic Reviews 2016, Issue 8. Art. No: CD006911. [DOI: 10.1002/14651858.CD006911.pub3] [DOI] [PubMed] [Google Scholar]


