Abstract
Introduction:
Internet-delivered behavioral weight control is promising for expanding the reach and availability of weight management, but online programs produce lower weight losses than typically achieved in person. Financial incentives have been shown to increase weight losses. The current study examined whether adding financial incentives for self-monitoring and achieving target weight losses increases weight losses attained in a fully online, group-based behavioral weight management program compared with the same program alone.
Study design:
RCT.
Setting/participants:
Adults with overweight and obesity (N=418; 91% female; 28% minority) were recruited from two clinical centers.
Intervention:
The intervention was a 24-session online group-based behavioral weight control program with weekly synchronous chat sessions (Internet-only) or the same program with weekly financial incentives for self-monitoring body weight and dietary intake daily and for achieving target weight losses at 2 and 6 months (Internet + incentives).
Main outcome measures:
This study measured weight loss at 6 months and treatment engagement (attendance, self-monitoring of body weight, dietary intake, physical activity). Data were collected between February 2016 and August 2018, and analyses were completed in 2019.
Results:
Participants randomized to Internet + incentives lost more weight (–6.4 [SD=5.5] kg) than those in the Internet-only group (–4.7 [SD=6.6] kg; p<0.01). Further, a higher proportion of the Internet + incentives group achieved ≥5% weight loss (55%) compared with those in the Internet-only group (40%; p<0.05). Treatment engagement was higher in the Internet + incentives condition, with greater self-monitoring of behaviors targeted by incentives, as well as higher rates of behaviors not targeted and higher self-reported physical activity. Study retention was higher among those in the Internet + incentives condition (91%) than those in the Internet-only condition (81%; p=0.003).
Conclusions:
Adding financial incentives to a program delivered fully online increases weight losses compared with the program alone and can achieve weight losses comparable to in-person programs, offering potential for substantial geographic reach.
INTRODUCTION
Behaviorally based interventions delivered in person successfully produce clinically significant weight losses of 5%–10%,1,2 and can ameliorate many comorbidities associated with obesity.3 However, reach and availability of in-person programs are limited. The Internet is a promising medium for expanding reach and availability of evidence-based programs; moreover, Internet-based programs have demonstrated clinically significant weight loss in half of individuals offered the intervention.4,5 However, average weight losses achieved online are smaller than those achieved with the same intervention conducted in person.4,6 Therefore, it is important to identify strategies to enhance weight loss outcomes in online interventions.
Although extensive research demonstrates that providing financial incentives can increase weight loss outcomes,7–9 few studies have examined financial incentives within the context of a structured online weight loss program. One study examined the addition of incentives to a hybrid Internet program (one in-person session plus an online program with automated feedback) and found that incentives produced significantly greater weight loss than did the low-intensity Internet program alone.10 However, the authors are aware of no studies examining the addition of financial incentives to a group-based, interactive behavioral weight control program delivered fully online. Furthermore, most previous work incentivized weight loss outcomes rather than behaviors associated with successful weight loss, even though some have speculated that incentivizing weight loss–promoting behaviors might be more effective.11–14 In addition, most incentivization schemes studied to date provided the financial reward at some end point, rather than in real time. Reinforcement is a more potent behavior change driver when it is proximal to the behaviors being rewarded,15 so more proximal incentive payouts may exert a powerful influence on self-regulation behaviors and ultimately produce better weight loss.
Therefore, the current study sought to determine whether 6-month weight loss outcomes achieved and treatment engagement (e.g., self-monitoring, attendance) in an online, group-based behavioral weight management program could be enhanced with the addition of financial incentives compared with the same program without financial incentives. Costs associated with providing incentives were also examined.
METHODS
This parallel RCT was conducted at two clinical sites and randomly allocated participants in a 1:1 ratio to either: (1) online behavioral lifestyle program with weekly synchronous group-based chat sessions (Internet-only) or (2) the same program with financial incentives contingent upon achieving weekly behavioral goals and weight loss targets (Internet + incentives). The study was approved by the Committee on Human Research in the Behavioral Sciences at the University of Vermont and the IRB at the University of South Carolina. This trial is registered at www.clinicaltrials.gov (NCT02688621). Participants consented to participation in an 18-month intervention, and the current paper focuses on the protocol-specified primary outcome of 6-month weight loss.
Study Population
Volunteers were recruited over a 24-month period through community-based efforts (e.g., flyers, health fairs), targeted e-mails using available distribution lists (e.g., worksites, professional organizations, sororities), and word of mouth. Interested individuals applied via a study recruitment website that provided a study overview and obtained initial screening data, followed by a phone interview and in-person orientation. Eligible individuals had to be aged ≥18 years; have a BMI between 25 and 50 kg/m2; and have access to a computer (at home or work), the Internet, and a smartphone. Individuals were ineligible if they took medications that might affect weight loss, reported substantial recent weight loss, had a history of bariatric surgery or major medical/psychiatric conditions, or were enrolled in another weight reduction program. Participants were required to complete a behavioral run-in by logging into the group chat webpage, as well as complete 3 consecutive days of self-monitoring in myfitnesspal.com and “friend” the program (for counselor review of self-monitoring records). Finally, they had to agree to be randomized. Participants indicated availability for pre-determined group times; these intact groups were balanced by baseline BMI distribution and cluster randomized using a biased coin approach by the UVM Biostatistical Coordinating Center.
Intervention
The manualized online intervention was adapted from in-person, group-based behavioral lifestyle programs16,17 and has been previously demonstrated effective in producing clinically meaningful weight losses.4,5 The intervention focused on reducing calorie intake and increasing physical activity using self-management skills, such as self-monitoring, goal setting, problem solving, and relapse prevention. Weekly 1-hour text-based online synchronous chat sessions offered over 6 months were facilitated by experienced behavioral weight control counselors who followed a structured curriculum. Interactive chats focused on reinforcing behavioral skills and providing social support. Groups combined participants from both clinical sites but maintained separation between conditions. Participants were provided with access to a secure, password-protected, interactive study website containing behavioral lessons with weekly homework that corresponded to each chat, a bulletin board for group communications, educational resources, and dynamic updates with weight loss tips, healthy recipes, and announcements of local physical activity events.
Participants were prescribed a calorie goal ranging from 1,200 to 1,800 kcal/day based on initial weight and a dietary fat goal corresponding to ≤25% of calories from fat.16,17 They were also provided graded moderate-to-vigorous physical activity goals that progressed to 200 minutes/week18 and graded step goals that progressed to 10,000 steps/day. All participants were instructed to weigh themselves daily and record their weight on the study website; if they did not have a scale, one was provided. Participants were instructed to record dietary intake, minutes of physical activity, and number of steps in MyFitnessPal daily. Group counselors sent participants weekly e-mails with tailored feedback based on participants’ self-monitoring, acknowledging successful enactment of behavioral strategies and offering constructive suggestions for areas to change in the future.
Individuals randomized to Internet + incentives received the same behavioral intervention as the Internet-only condition, including the same dietary and physical activity goals, behavioral strategies to reach these goals, and online delivery format. The only difference in conditions was that participants in Internet + incentives also received financial incentives contingent on self-monitoring of targeted behaviors and achieving milestone weight loss targets at 2 and 6 months. Dietary self-monitoring and self-weighing were incentivized weekly for the first 8 weeks, as the initial weeks of a weight loss program represent a period when behavioral patterns are established.19 These behaviors were selected because both are associated with effective long-term weight management.20–23 Participants could receive up to $15/week if they reported recording their dietary intake and weighing themselves on all 7 days of the week (i.e., 14 behaviors) or $10/week if they indicated some combination of these behaviors at least ten times. Incentives were delivered weekly using an electronic gift card (Amazon), allowing proximal reinforcement of behaviors. E-mails announcing the incentive amount were sent weekly to those who earned an incentive and a “loss-framed” message24–26 was sent to those who did not earn anything or received less than the full incentive amount; these loss-framed e-mails reminded participants that they had “left money on the table.” Weeks were independent, allowing individuals who may have lapsed in their self-management behaviors in 1 week to resume the behaviors and receive a full incentive the following week. In addition to weekly payouts, participants in the Internet + incentives group could receive incentives for achieving weight loss targets at the 2-month and 6-month clinic visits. Weight losses as early as 2 months are strong indicators of long-term success27,28 and were therefore selected for reinforcement in addition to incentivizing 6-month weight losses, which was the primary outcome. At 2 months, those who lost ≥5% received $35 and those who lost ≥3% received $25; at 6 months, those who lost ≥10% earned $75 and those who lost ≥5% received $50. The maximum incentive available during the 6-month period was $230.
Measures
All measures were obtained at baseline, 2 months, and 6 months in the clinic unless otherwise indicated. Data were collected between February 2016 and August 2018 by assessors blinded to treatment assignment.
Weight change was the primary dependent measure. Weight was measured in the clinic on a calibrated digital scale. Height was measured using a wall-mounted stadiometer at baseline only. BMI was calculated as weight (kg)/height (m)2 and obesity was defined as BMI ≥30 kg/m2. The proportion who achieved clinically significant weight losses of ≥5% and ≥10% from baseline was also examined.
Self-reported sociodemographic characteristics were collected at baseline by online questionnaire.
Counselors recorded participant attendance at online group chat sessions. Participants were asked to submit a daily update on the study website indicating whether they met their calorie goal, how many minutes of moderate-to-vigorous physical activity they completed, number of steps taken, and whether they weighed themselves (and, if so, to report their weight). These self-reported updates were used to characterize treatment engagement in both study arms and to guide weekly payouts for participants in the Internet + incentives arm.
Research staff recorded payouts for weekly incentives and achieving target weights at 2 and 6 months.
Statistical Analysis
The study was designed to detect a 2.2-kg group weight loss difference between groups with a standard deviation of 5.8 kg,4,5 a 5% Type I error rate, and 80% power. To adjust for possible clustering effects in this nested design, the adjusted variance estimate was increased to 7.67, calculated using a conservative intraclass correlation coefficient of 0.05. The required sample size was 177, which was increased to 208 participants per condition to allow 15% attrition and ensure 16 participants within each online chat group. Weight losses at 2 months and 6 months were examined, with 6-month weight loss identified a priori as the primary outcome. For intent-to-treat analyses, multiple imputation was used to create 100 complete data sets, which were analyzed separately and then the results were combined. Data were imputed by the fully conditional specification method (FCS option in SAS PROC MI), with two steps within the FCS procedure. Month 2 values were imputed with baseline weight, chat group, age, baseline BMI, sex, and race as covariates.29 Month 6 values were imputed with the same covariates as well as Month 2 weights (both observed and imputed). Imputation was done separately for each arm.30 Weight change analyses were conducted in 2019 with imputed data using a mixed linear model with repeated measures nested within participants and participants nested within randomized clusters (i.e., online chat groups). Completer analyses were conducted in similar fashion using only those with weight data available. Similar analyses were run to evaluate adherence measures (e.g., number of days reporting weight, minutes of moderate-to-vigorous physical activity). Missing data were either treated as indicative of non-adherence (dichotomous outcomes) or ignored when the outcome was continuous. All analyses were conducted using SAS, version 9.4. Statistical significance was defined as p<0.05 (two-tailed).
RESULTS
A total of 418 participants were randomized (Figure 1). Participants were predominantly female, obese, and well-educated, with 28% self-identifying as African American or another racial minority group. There were no significant baseline differences between conditions with respect to sociodemographic characteristics or body weight (Table 1). Twenty-six separate groups were randomized (13 into each condition).
Figure 1.
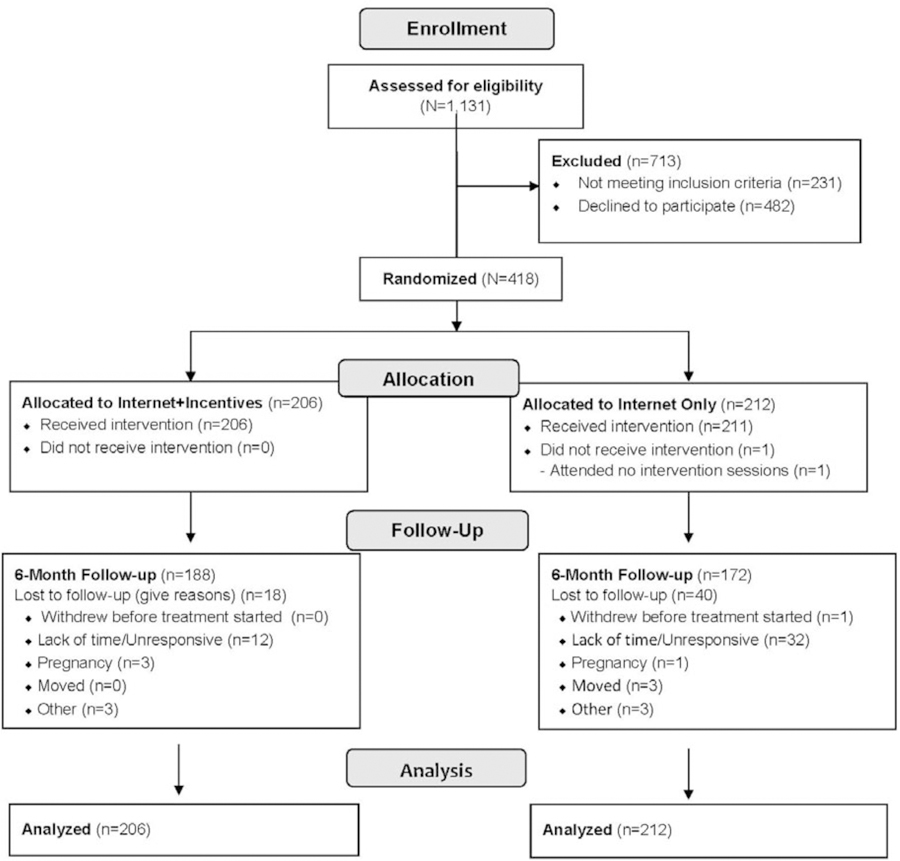
CONSORT flow diagram.
Table 1.
Baseline Sample Characteristics
| Characteristics | Internet-only (n=212) |
Internet + incentives (n=206) |
|---|---|---|
| Age, years, M±SD | 48±11 | 50±11 |
| Female, n (%) | 194 (92) | 187 (91) |
| Race, n (%) | ||
| White | 158 (77) | 145 (68) |
| African American | 63 (30) | 44 (21) |
| Other minority | 4 (2) | 4 (2) |
| Clinical site, n (%) | ||
| South Carolina | 106 (50) | 103 (50) |
| Vermont | 106 (50) | 103 (50) |
| Weight, kg, M±SD | 97.8 ± 19.5 | 95.6 ± 15.9 |
| BMI, M±SD | 35.8 ± 5.9 | 35.5 ± 5.5 |
| Obese, ≥30 BMI, n (%) | 174 (82) | 169 (82) |
| Education, n (%) | ||
| College degree or higher | 169 (80) | 161 (78) |
| Employed full time, n (%) | 177 (83) | 169 (82) |
Follow-up data were provided by 94% of randomized participants at 2 months, with no difference between conditions. Although retention was high for 6-month data collection (>85%), there were significant differences between conditions, with greater retention among those in Internet + incentives group than the Internet-only group (91% vs 81%, χ2(1)=8.97, p=0.003). Those missing data at 6 months were significantly younger (43.1 [SD=11.0] vs 49.8 [SD=10.8] years, p<0.001) and more likely to be female (89% vs 90%, p=0.04) than those who provided follow-up data.
Participants in the Internet + incentives group lost significantly more weight at 2 months than those in the Internet-only group. This pattern was evident in both the intent-to-treat and completers analyses (Table 2). A significantly higher proportion of those in the internet + incentives group experienced clinically meaningful weight losses of ≥5% at 2 months, and they were more likely to achieve the other incentivized benchmark weight loss of 3% than were those in the Internet-only group. At 6 months, greater weight loss among those in Internet + incentives relative to Internet-only was sustained, with those in the incentivized condition losing 2% more than the control group. In addition, in the intent-to-treat analyses, clinically meaningful weight losses were significantly more likely among participants in the Internet + incentives group than those in the Internet-only group.
Table 2.
Weight Losses
| Variable | All randomized participantsa | Completers | ||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Internet-only | Internet + incentives | Group difference (95% CI) | t (24) | Internet-only | Internet + incentives | Group difference (95% CI) | t (24) | |
| 2-month data collection | ||||||||
| n (%) | 212 (100) | 206 (100) | 194 (92) | 195 (95) | ||||
| Weight loss, kg, M±SD | 3.1 ± 3.4 | 4.3 ± 3.0 | 1.2 (0.5, 1.9) | 3.55 *** | 3.2 ± 3.4 | 4.3 ± 3.0 | 1.2 (0.6, 1.9) | 3.78 *** |
| Weight loss, %, M±SD | 3.2 ± 3.1 | 4.5 ± 3.1 | 1.2 (0.6, 2.0) | 3.61 *** | 3.3 ± 3.1 | 4.5 ± 3.0 | 1.3 (0.6, 1.6) | 3.95 *** |
| ≥3% weight loss, n (%) | 105 (50) | 132 (64) | 15 (5, 23) | 2.99 ** | 105 (54) | 132 (68) | 14 (4, 22) | 2.73 * |
| ≥5% weight loss, n (%) | 46 (22) | 86 (42) | 20 (8, 33) | 3.58 ** | 46 (24) | 86 (44) | 21 (8, 34) | 3.57 *** |
| 6-month data collection | ||||||||
| n (%) | 212 (100) | 206 (100) | 172 (81) | 188 (91) | ||||
| Weight loss, kg, M±SD | 4.7 ± 6.6 | 6.4 ± 5.5 | 2.1 (0.4, 3.8) | 2.66 ** | 5.2 ± 6.5 | 6.7 ± 5.4 | 1.7 (0.4, 3.0) | 2.63 * |
| Weight loss, %, M±SD | 4.9 ± 6.4 | 6.8 ± 5.7 | 2.0 (0, 4) | 2.51 * | 5.4 ± 6.1 | 7.1 ± 5.5 | 1.8 (0.4, 3.2) | 2.55 * |
| ≥5% weight loss, n (%) | 85 (40) | 114 (55) | 15 (4, 26) | 2.72 * | 85 (49) | 114 (61) | 11 (0, 21) | 2.00 |
| ≥10% weight loss, n (%) | 34 (16) | 58 (28) | 12 (2, 26) | 2.41 * | 34 (20) | 58 (31) | 11 (0, 25) | 2.04 |
Note: Boldface indicates statistical significance
p<0.05
p<0.01
p<0.001
Multiple imputation used to generate missing data for intent-to-treat analyses.
Greater treatment engagement was observed in the Internet + incentives group compared with the Internet-only group (Table 3). During the first 2 months, participants in Internet + incentives engaged in greater self-monitoring of the incentivized behaviors (i.e., body weight and dietary self-monitoring) and also monitored non-incentivized behaviors (i.e., physical activity) more frequently. Further, volume of physical activity (i.e., daily steps and minutes of moderate-to-vigorous physical activity) reported by participants in the Internet + incentives condition was significantly greater than the Internet-only condition during the first 2 months.
Table 3.
Treatment Engagement
| Variable | Internet-only | Internet + incentives | p-value |
|---|---|---|---|
| Weeks 1‒8 (Months 1‒2) | |||
| Attendance | |||
| Number weekly group chat sessions attended (out of 8), M±SD | 6.7± 1.9 | 7.4 ± 1.2 | 0.0007 |
| Proportion attending ≥75% of weekly group chat sessions | 85% | 93% | 0.007 |
| Self-monitoring | |||
| Number of days with body weight self-reported (out of 56), M±SDa | 32 ± 17 | 49 ± 10 | <0.0001 |
| Proportion recording body weight ≥50% of days (i.e., ≥28 days) | 61% | 95% | <0.0001 |
| Dietary intake, days reported recording (out of 56), M±SDa | 36 ± 17 | 50 ± 10 | <0.0001 |
| Proportion reporting recorded dietary intake ≥50% days (i.e., ≥28 days) | 72% | 96% | <0.0001 |
| Physical activity, days reported (out of 56), M±SD | 37 ± 17 | 50 ± 10 | <0.0001 |
| Proportion reporting physical activity ≥50% days (i.e., ≥28 days) | 75% | 96% | <0.0001 |
| Self-reported goal attainmentc | |||
| Number of weeks met goal of ≥200 minutes/week of MVPA (max 8; M±SD) | 1.8 ± 2.3 | 3.3 ± 2.9 | <0.0001 |
| Number days met goal of ≥10,000 steps/day (max 56; M±SD) | 9.2 ± 11.8 | 15.1 ± 14.7 | <0.0001 |
| Number of days met calorie goal (max 56; M±SD) | 24 ± 15 | 36 ± 13 | <0.0001 |
| Self-reported physical activityd | |||
| Minutes/week on days when minutes reported, M±SD | 132 ± 98 | 200 ± 127 | <0.0001 |
| Number steps/day on days when steps reported, M±SD | 7,071 ± 2,813 | 7,806 ± 2,659 | 0.01 |
| Weeks 9‒24 (Months 3‒6) | |||
| Attendance | |||
| Number weekly group chat sessions attended (out of 16), M±SD | 9.1 ± 5.2 | 11.2 ± 4.4 | 0.0005 |
| Proportion attending ≥75% of weekly group chat sessions | 46% | 62% | 0.0151 |
| Self-monitoring | |||
| Number of days with body weight self-reported (out of 112), M±SDb | 40 ± 36 | 66 ± 37 | <0.0001 |
| Proportion recording body weight ≥50% of days (i.e., ≥56 days) | 35% | 63% | <0.0001 |
| Dietary intake, days reported recording (out of 112), M±SDb | 44 ± 30 | 66 ± 38 | <0.0001 |
| Proportion reporting recorded dietary intake ≥50% days (i.e., ≥56 days) | 39% | 49% | 0.0006 |
| Physical activity, days reported (out of 112), M±SD | 47 ± 39 | 68 ± 38 | <0.0001 |
| Proportion reporting physical activity ≥50% days (i.e., ≥56 days) | 42% | 63% | 0.0008 |
| Self-reported goal attainmentc | |||
| Number of weeks met goal of ≥200 minutes/week of MVPA (max 16; MSD) | 3.0 ±4.6 | 5.5 ± 5.8 | <0.0001 |
| Number days met goal of ≥10,000 steps/day (max 112; M±SD) | 18.3 ± 26.2 | 27.0 ± 29.3 | 0.0004 |
| Number of days met calorie goal (max 112; M±SD)d | 33 ± 32 | 48 ± 33 | <0.0001 |
| Self-reported physical activityd | |||
| Minutes/week on days when minutes reported, M±SD | 133 ± 99 | 191 ± 148 | 0.003 |
| Number steps/day on days when steps reported, M±SD | 8,174 ± 3,134 | 8,386 ± 2,769 | 0.44 |
| Month 1‒Month 6 | |||
| Attendance | |||
| Number weekly group chat sessions attended (out of 24), M±SD | 16 ± 6.6 | 18 ± 5.1 | <0.0001 |
| Proportion attending ≥75% of weekly group chat sessions | 51% | 70% | 0.002 |
| Self-monitoring | |||
| Number of days with body weight self-reported (out of 168), M±SDa | 72 ± 51 | 115 ± 43 | <0.0001 |
| Proportion recording body weight ≥50% of days (i.e., ≥84 days) | 42% | 74% | <0.0001 |
| Dietary intake, days reported recording (out of 168), M±SDa | 85 ± 54 | 119 ± 44 | <0.0001 |
| Proportion reporting recorded dietary intake ≥50% days (i.e., ≥84 days) | 49% | 76% | <0.0001 |
| Physical activity, days reported (out of 168), M±SD | 85 ± 54 | 118 ± 44 | <0.0001 |
| Proportion self-monitoring physical activity ≥50% days (i.e., ≥84 days) | 49% | 75% | <0.0001 |
| Self-reported goal attainmentc | |||
| Number of weeks met goal of ≥200 minutes/week of MVPA (max 24; M±SD) | 5 ± 6 | 9 ± 8 | <0.0001 |
| Number days met goal of ≥10,000 steps/day (max 168; M±SD) | 27 ± 36 | 42 ± 41 | 0.0003 |
| Number of days met calorie goal (max 168; M±SD)d | 56 ± 44 | 83 ± 42 | <0.0001 |
| Self-reported physical activityd | |||
| Minutes/week on days when minutes reported, M±SD | 127 ± 91 | 193 ± 131 | <0.0001 |
| Number steps/day on days when steps reported, M±SD | 7,447 ± 2,888 | 8,057± 2,672 | 0.04 |
Notes: Boldface indicates statistical significance (p<0.05).
Incentivized during Weeks 1‒8 in the Internet + incentives condition.
No longer incentivized during Weeks 9‒24.
If no self-report of adherence to calorie, step or minutes physical activity goal was provided on a given day, it was assumed that the goal was not met on that day.
Includes reported data only (no imputed data).
MVPA, moderate-to-vigorous physical activity.
After weekly behavioral incentives ended (in Week 9), higher engagement continued among those in the Internet + incentives condition; those who had previously received incentives self-reported self-weighing, dietary intake, and exercise on more days in the next 4 months than did those in the Internet-only group. Further, those in the Internet + incentives group met exercise treatment goals (i.e., steps and minutes of moderate-to-vigorous physical activity) during this period more often than the Internet-only group. Engagement tended to be higher during the initial 2 months of treatment for both conditions than it was later in treatment (Table 3), with the exception of the proportion of days on which 10,000 steps/day were achieved, which was higher in the final treatment period for those in Internet + incentives relative to the first 8 weeks. Attendance at chats was higher in the Internet + incentives condition, with an average of 18 weekly group chats (75% of available sessions) attended across the 6-month intervention period compared with 16 (67%) chats in the Internet-only condition (χ2(1)=4.84, p<0.0001).
Participants in the Internet + incentives condition received a payout in 7.2 (SD=1.7) of 8 weeks, with per capita payouts averaging $99 (SD=$27) for weekly incentives. Only 3% (n=6) of participants failed to meet criteria to receive at least one weekly incentive. Incentivized weight loss targets were reached by 64% of participants at 2 months, 42% received the maximum incentive for achieving ≥5% weight loss ($35), and an additional 22% received the lower payout ($25) for losing ≥3%. At 6 months, incentivized weight loss targets were achieved by 55% (28% received the maximum incentive for achieving ≥10% weight loss [$75] and an additional 27% received the smaller payout [$50] for losing ≥5%). Incentive costs during the 6-month period, including weekly payouts plus weight loss bonuses, averaged $153 per participant (of a possible $230) at an incremental cost/kg of $85 relative to those receiving the online program alone.
DISCUSSION
The addition of financial incentives to an online behavioral weight loss program with synchronous group chats significantly increased weight losses, with those receiving financial incentives achieving a 2% incremental weight loss advantage over what was seen among individuals provided the same online program without incentives. Average weight losses among completers of the Internet + incentives program was 7.1%. These weight losses are comparable to the 6.9% achieved at 6 months among completers in the in-person Diabetes Prevention Program, a gold standard intensive lifestyle obesity treatment.22 Furthermore, 55% of participants in the Internet + incentives group achieved clinically meaningful weight losses of ≥5%, and 28% lost ≥10% at 6 months. Participants receiving the Internet + incentives program were significantly more likely to achieve clinically meaningful weight losses than were participants who received Internet-only treatment, and weight loss outcomes in the Internet + incentives group compare favorably with the 49% of participants in the Diabetes Prevention Program who achieved the ≥7% weight loss goal.22 Noteworthy in the current study is that these clinically meaningful weight losses were produced without a single in-person intervention session. Thus, by combining online treatment with financial incentives, it is possible to provide a weight loss program to individuals located across significant geographic distances and produce outcomes approximating those achieved in premier in-person programs, all without a single in-person contact.
The superior and substantial weight loss outcomes observed with the addition of financial incentives were accompanied by significantly better treatment engagement than was evident among individuals receiving the Internet-only program. Among those receiving financial incentives, there was higher attendance at group chat sessions and more days of self-monitoring of all target behaviors (diet, physical activity, and weight) than was observed among those receiving Internet-only. The incentive group also self-reported higher levels of physical activity. Interestingly, improved treatment engagement was not limited to the behaviors targeted by incentives. Participants in the Internet + incentives condition not only had significantly higher frequency of behaviors incentivized weekly (i.e., self-monitoring weight and diet) but also behaviors that were not incentivized (i.e., self-monitoring physical activity, self-reporting meeting steps, physical activity and calorie goals, and attending chat sessions). This ripple effect is particularly noteworthy because these particular “spillover” behaviors are each strongly associated with successful weight loss.31 This finding is consistent with Leahey et al.,10 who also found a ripple effect in which participants were significantly more likely to log in to the website and view lessons even though those aspects of program participation were not targeted with incentives.
Additionally, the pattern of greater treatment engagement observed during the first 8 weeks when weekly incentives were in place was sustained even after weekly incentives for self-regulatory behaviors were discontinued. This apparent continued impact of initial weekly incentives was noted for behaviors which had been targeted with incentives, as well as aspects of treatment engagement that had not been incentivized. Emphasizing key self-monitoring behaviors early in programs by the use of incentives may have assisted in initial habit formation,32 and these habits may have been maintained after incentives for the specific behaviors were withdrawn. Alternatively, increased satisfaction with weight losses achieved during the initial 2 months may have enhanced motivation for continued engagement in effective weight control behaviors.33 Importantly, incentivized behaviors did not “extinguish” or discontinue when financial incentives were withdrawn, as observed in other studies.11 However, incentives offered for meeting weight loss goals at 6 months may have contributed to continued behavioral engagement after weekly process incentives were discontinued.
The current study is one of the few to offer both process incentives (for behaviors associated with weight loss outcomes) and outcome incentives (for achieving target weight losses). Most studies examining financial incentives for weight loss have offered outcome incentives only.34–41 However, there is burgeoning interest in process incentives to reinforce use of behavioral strategies which increase the likelihood of sustained successful weight loss.11,13,14,42 Leahey and colleagues10 demonstrated that a combination of process and outcome incentives enhanced weight losses when added to their low-intensity, automated online program. Within the context of an in-person behavioral weight control program, Jeffery et al.43 found that providing financial incentives for calorie restriction produced weight losses comparable to incentivizing weight loss goals, both of which were superior to incentivizing attendance at group sessions. However, the optimal combination and magnitude of weight loss-based incentives versus behavior-based incentives remains unclear.44
Similarly, the optimal timing of incentives remains unclear. Weekly behavioral incentives early in the program and outcome incentives at the 2-month clinic visit reflected evidence that “starting strong” is critical to long-term weight loss success.27,45 “Front loading” incentives for weight loss during the first 3 months of a 6-month intervention produced more total weight loss than steady payments throughout the intervention or “back loading” rewards in the latter half of the program.35 Theoretically, offering reinforcement such as financial incentives during the acquisition of behavioral skills will increase performance of those skills, and reviews indicate incentives may be most effective in the initial phase of treatment delivery.11 However, few studies offer clear guidance on the best incentive scheme. Further, pragmatic concerns often guide incentive implementation. For example, the decision in the current study to curtail self-monitoring incentives after 8 weeks reflected limited resources as well as the reasoning that it might be advantageous to discontinue self-monitoring incentives while weekly chat sessions were still ongoing to allow continued counselor support for sustained behavior rather than eliminate weekly contact and behavioral incentives simultaneously. It is possible that weight losses may have been greater if process incentives were offered for a longer period or higher amounts were provided. The incentive scheme utilized appears to have been successful in increasing weight loss relative to the program without incentives, but it is one of many combinations that could be implemented to target both process and outcome measures. Future research should identify which incentive strategy is optimal and cost effective.
Weekly payouts were made for incentives that were accrued weekly, distinguishing this payout scheme from other studies that “reward” frequently but don’t pay out frequently. It is not clear what role this proximal payout may have played in promoting behavior changes. Distal payment may diminish motivation and dilute the impact of incentives42; this may be particularly relevant when considering process incentives. However, the optimal payout approach is not known.
The financial incentives offered in the current study augmented weight losses over and above the online program alone and produced average weight losses on par with premier in-person programs, with incentive costs averaging $153 per participant over the 6-month intervention, or $85 per additional kg lost relative to the non-incentivized intervention. These cost data provide insight into level of engagement with the incentive protocol, as well as an estimate of the additional costs associated with providing incentives. However, these estimates do not consider the full costs of delivering treatment, nor are participant costs assessed, so direct comparisons with cost analyses of other incentivized and online obesity interventions are not appropriate, and the cost effectiveness of the approach is unknown. Nonetheless, emerging evidence indicates incentive-based programs delivered at least partially online may be cost effective relative to similar programs without incentives.10
Limitations
This study includes a predominantly female population who all had access to a computer and smartphone and a relatively high education level, which may limit the generalizability of the findings. Further, although retention rates were high overall (86% of participants providing 6-month data), the authors experienced greater attrition in the Internet-only condition (19%) than in the Internet + incentives condition (9%). Other studies have found incentives positively associated with retention,41 leading some investigators to suggest that comparison groups in incentive-based studies should also be compensated to decrease attrition and avoid inflating the value of incentive schemes.46 In addition, the authors are unable to disentangle the effects of weight loss milestone incentives and weekly behavioral incentives on treatment engagement and weight loss. Although a growing literature supports the efficacy of rewarding the achievement of weight loss, participants have greater control over their behaviors than they do over their absolute weight loss. Thus, it is attractive to consider both targets for incentives. Future research to determine which combination of process and outcome incentives maximizes long-term weight control will be necessary. Additional limitations include the use of self-reported physical activity, as well as the lack of data on participant costs, which precludes detailed comparisons with other online and incentives treatment program. Finally, these data examine the 6-month weight trajectory and do not address long-term weight maintenance patterns following financial incentives. This is common among studies of financial incentives for obesity treatment; reviews indicate most studies are 6 months in duration or less,7,11 leaving questions about sustained impact of incentives largely unanswered. However, short-term weight losses strongly predict longer-term weight losses,27,45 and thus improved 6-month weight losses observed here might suggest better long-term weight losses. Strengths of the study include the randomized design, the racially diverse sample, and the daily digital assessment of treatment engagement, including self-monitoring.
CONCLUSIONS
The major findings of this study are that the addition of process and outcome financial incentives enhanced weight loss outcomes in an online group-based behavioral weight control program compared with the program alone and that the incentive-augmented program produced 6-month weight losses similar to those achieved in premier in-person programs. Incentives also enhanced self-monitoring behaviors, session attendance, and self-reported physical activity. Given the potential for disseminating weight loss interventions online, further research is needed to understand which behaviors and outcomes should be incentivized, the timing and amount of incentives needed to produce the largest and most sustained weight losses, and the cost effectiveness of adding process and outcome incentives to online weight control. However, health insurance plans and worksites that already incentivize participation in weight loss programs might want to consider the combination of process and outcome incentives.
ACKNOWLEDGMENTS
This manuscript was supported in part by funding from the National Institute of Diabetes and Digestive and Kidney Diseases (DK 056746) awarded to Drs. West and Harvey.
The study sponsor had no role in study design, data collection or interpretation, or in manuscript preparation. No financial disclosures were reported by the authors of this paper.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Trial registration: This study is registered at www.clinicaltrials.gov NCT02688621.
The authors have no conflicts of interest or financial relationships to report.
REFERENCES
- 1.Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393–403. 10.1056/nejmoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Look AHEAD Research Group. Reduction in weight and cardiovascular disease risk factors in individuals with type 2 diabetes: one-year results of the Look AHEAD trial. Diabetes Care. 2007;30(6):1374–1383. 10.2337/dc07-0048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gregg EW, Flores MR. The impact of intentional weight loss on major morbidity and mortality. In: Wadden TA, Bray GA, eds. Handbook of Obesity Treatment, Second Edition. New York, NY: Guilford Publications; 2018:185–207. [Google Scholar]
- 4.Harvey-Berino J, West D, Krukowski R, et al. Internet delivered behavioral obesity treatment. Prev Med. 2010;51(2):123–128. 10.1016/j.ypmed.2010.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.West DS, Harvey JR, Krukowski RA, Prewitt TE, Priest J, Ashikaga T. Do individual, online motivational interviewing chat sessions enhance weight loss in a group-based, online weight control program? Obesity (Silver Spring). 2016;24(11):2334–2340. 10.1002/oby.21645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Finkelstein EA, Verghese NR. Incremental cost-effectiveness of evidence-based non-surgical weight loss strategies. Clin Obes. 2019;9(2):e12294. 10.1111/cob.12294. [DOI] [PubMed] [Google Scholar]
- 7.Jeffery RW. Financial incentives and weight control. Prev Med. 2012;55(suppl):S61–S67. 10.1016/j.ypmed.2011.12.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Paul-Ebhohimhen V, Avenell A. Systematic review of the use of financial incentives in treatments for obesity and overweight. Obes Rev. 2008;9(4):355–367. 10.1111/j.1467-789x.2007.00409.x. [DOI] [PubMed] [Google Scholar]
- 9.Gong Y, Trentadue TP, Shrestha S, Losina E, Collins JE. Financial incentives for objectively-measured physical activity or weight loss in adults with chronic health conditions: a meta-analysis. PLoS One. 2018;13(9):e0203939. 10.1371/journal.pone.0203939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Leahey TM, Subak LL, Fava J, et al. Benefits of adding small financial incentives or optional group meetings to a web-based statewide obesity initiative. Obesity (Silver Spring). 2015;23(1):70–76. 10.1002/oby.20937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Burns RJ, Donovan AS, Ackermann RT, Finch EA, Rothman AJ, Jeffery RW. A theoretically grounded systematic review of material incentives for weight loss: implications for interventions. Ann Behav Med. 2012;44(3):375–388. 10.1007/s12160-012-9403-4. [DOI] [PubMed] [Google Scholar]
- 12.Volpp KG, Pauly MV, Loewenstein G, Bangsberg D. P4P4P: an agenda for research on pay-for-performance for patients. Health Aff (Millwood). 2009;28(1):206–214. 10.1377/hlthaff.28.1.206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jay M, Orstad SL, Wali S, et al. Goal-directed versus outcome-based financial incentives for weight loss among low-income patients with obesity: rationale and design of the Financial Incentives foR Weight Reduction (FIReWoRk) randomised controlled trial. BMJ Open. 2019;9(4):e025278. 10.1136/bmjopen-2018-025278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hashemi A, You WJ, Boyle KJ, Parmeter CF, Kanninen BJ, Estabrooks PA. Identifying financial incentive designs to enhance participation in weight loss programs. J Obes Weight Loss Ther. 2015;5:247. 10.4172/2165-7904.1000247. [DOI] [Google Scholar]
- 15.Bandura A Social foundations of thought and action: a social cognitive theory. Englewood Cliffs, NJ: Prentice-Hall, Inc; 1986. [Google Scholar]
- 16.The Look AHEAD Research Group. The Look AHEAD Study: a description of the lifestyle intervention and the evidence supporting it. Obesity (Silver Spring). 2006;14(5):737–752. 10.1038/oby.2006.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.The Diabetes Prevention Program (DPP) Research Group. The Diabetes Prevention Program (DPP): description of lifestyle intervention. Diabetes Care. 2002;25(12):2165–2171. 10.2337/diacare.25.12.2165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jakicic JM, Tate DF, Lang W, et al. Objective physical activity and weight loss in adults: the step-up randomized clinical trial. Obesity (Silver Spring). 2014;22(11):2284–2292. 10.1002/oby.20830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Krukowski RA, Harvey-Berino J, Bursac Z, Ashikaga T, West DS. Patterns of success: online self-monitoring in a web-based behavioral weight control program. Health Psychol. 2013;32(2):164–170. 10.1037/a0028135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zheng YG, Klem ML, Sereika SM, Danford CA, Ewing LJ, Burke LE. Self-weighing in weight management: a systematic literature review. Obesity (Silver Spring). 2015;23(2):256–265. 10.1002/oby.20946. [DOI] [PubMed] [Google Scholar]
- 21.Burke LE, Wang J, Sevick MA. Self-monitoring in weight loss: a systematic review of the literature. J Am Diet Assoc. 2011;111(1):92–102. 10.1016/j.jada.2010.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wing RR, Hamman RF, Bray GA, et al. Achieving weight and activity goals among diabetes prevention program lifestyle participants. Obes Res. 2004;12(9):1426–1434. 10.1038/oby.2004.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.West DS, Dutton G, Delahanty LM, et al. Weight loss experiences of African American, Hispanic, and non-Hispanic white men and women with type 2 diabetes: the Look AHEAD trial. Obesity (Silver Spring). 2019;27(8):1275–1284. 10.1002/oby.22522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rothman AJ, Bartels RD, Wlaschin J, Salovey P. The strategic use of gain- and loss-framed messages to promote healthy behavior: how theory can inform practice. J Comm. 2006;56(suppl 1):S202–S220. 10.1111/j.1460-2466.2006.00290.x. [DOI] [Google Scholar]
- 25.Jensen JD, Ratcliff CL, Yale RN, Krakow M, Scherr CL, Yeo SK. Persuasive impact of loss and gain frames on intentions to exercise: a test of six moderators. Commun Monogr. 2018;85(2):245–262. 10.1080/03637751.2017.1353699. [DOI] [Google Scholar]
- 26.Lim JS, Noh G-Y. Effects of gain-versus loss-framed performance feedback on the use of fitness apps: mediating role of exercise self-efficacy and outcome expectations of exercise. Comput Human Behav. 2017;77:249–257. 10.1016/j.chb.2017.09.006. [DOI] [Google Scholar]
- 27.Unick JL, Neiberg RH, Hogan PE, et al. Weight change in the first 2 months of a lifestyle intervention predicts weight changes 8 years later. Obesity (Silver Spring). 2015;23(7):1353–1356. 10.1002/oby.21112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Unick JL, Leahey T, Kent K, Wing RR. Examination of whether early weight loss predicts 1-year weight loss among those enrolled in an Internet-based weight loss program. Int J Obes (Lond). 2015;39(10):1558–1560. 10.1038/ijo.2015.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Groenwold RH, Donders AR, Roes KC, Harrell FE Jr., Moons KG. Dealing with missing outcome data in randomized trials and observational studies. Am J Epidemiol. 2012;175(3):210–217. 10.1093/aje/kwr302. [DOI] [PubMed] [Google Scholar]
- 30.Sullivan TR, White IR, Salter AB, Ryan P, Lee KJ. Should multiple imputation be the method of choice for handling missing data in randomized trials? Stat Methods Med Res. 2018;27(9):2610–2626. 10.1177/0962280216683570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dolan P, Galizzi MM. Like ripples on a pond: Behavioral spillovers and their implications for research and policy. J Econ Psychol. 2015;47:1–16. 10.1016/j.joep.2014.12.003. [DOI] [Google Scholar]
- 32.Charness G, Gneezy U. Incentives to exercise. Econometrica. 2009;77(3):909–931. 10.3982/ecta7416. [DOI] [Google Scholar]
- 33.Finch EA, Linde JA, Jeffery RW, Rothman AJ, King CM, Levy RL. The effects of outcome expectations and satisfaction on weight loss and maintenance: correlational and experimental analyses - a randomized trial. Health Psychol. 2005;24(6):608–616. 10.1037/0278-6133.24.6.608. [DOI] [PubMed] [Google Scholar]
- 34.Volpp KG, John LK, Troxel AB, Norton L, Fassbender J, Loewenstein G. Financial incentive–based approaches for weight loss: a randomized trial. JAMA. 2008;300(22):2631–2637. 10.1001/jama.2008.804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Finkelstein EA, Linnan LA, Tate DF, Birken BE. A pilot study testing the effect of different levels of financial incentives on weight loss among overweight employees. J Occup Environ Med. 2007;49(9):981–989. 10.1097/jom.0b013e31813c6dcb. [DOI] [PubMed] [Google Scholar]
- 36.John LK, Loewenstein G, Troxel AB, Norton L, Fassbender JE, Volpp KG. Financial incentives for extended weight loss: a randomized, controlled trial. J Gen Intern Med. 2011;26(6):621–626. 10.1007/s11606-010-1628-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kullgren JT, Troxel AB, Loewenstein G, et al. Individual-versus group-based financial incentives for weight loss: a randomized, controlled trial. Ann Intern Med. 2013;158(7):505–514. 10.7326/0003-4819-158-7-201304020-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kullgren JT, Troxel AB, Loewenstein G, et al. A randomized controlled trial of employer matching of employees’ monetary contributions to deposit contracts to promote weight loss. Am J Health Promot. 2016;30(6):441–452. 10.1177/0890117116658210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Patel MS, Asch DA, Troxel AB, et al. Premium-based financial incentives did not promote workplace weight loss in a 2013‒15 study. Health Aff (Millwood). 2016;35(1):71–79. 10.1377/hlthaff.2015.0945. [DOI] [PubMed] [Google Scholar]
- 40.Paloyo AR, Reichert AR, Reuss-Borst M, Tauchmann H. Who responds to financial incentives for weight loss? Evidence from a randomized controlled trial. Soc Sci Med. 2015;145:44–52. 10.1016/j.socscimed.2015.09.034. [DOI] [PubMed] [Google Scholar]
- 41.Driver SL, Hensrud D. Financial incentives for weight loss: a one-year randomized controlled clinical trial. J Am Coll Cardiol. 2013;61(10 suppl):E1459. 10.1016/s0735-1097(13)61459-x. [DOI] [Google Scholar]
- 42.VanEpps EM, Troxel AB, Villamil E, et al. Effect of process- and outcome-based financial incentives on weight loss among prediabetic New York Medicaid patients: a randomized clinical trial. Am J Health Promot. 2019;33(3):372–380. 10.1177/0890117118783594. [DOI] [PubMed] [Google Scholar]
- 43.Jeffery RW, Thompson PD, Wing RR. Effects on weight reduction of strong monetary contracts for calorie restriction or weight loss. Behav Res Ther. 1978;16(5):363–369. 10.1016/0005-7967(78)90005-0. [DOI] [PubMed] [Google Scholar]
- 44.Finkelstein EA, Bilger M, Baid D. Effectiveness and cost-effectiveness of incentives as a tool for prevention of non-communicable diseases: a systematic review. Soc Sci Med. 2019;232:340–350. 10.1016/j.socscimed.2019.05.018. [DOI] [PubMed] [Google Scholar]
- 45.Nackers LM, Ross KM, Perri MG. The association between rate of initial weight loss and long-term success in obesity treatment: does slow and steady win the race? Int J Behav Med. 2010;17(3):161–167. 10.1007/s12529-010-9092-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Thirumurthy H, Asch DA, Volpp KG. The uncertain effect of financial incentives to improve health behaviors. JAMA. 2019;321(15):1451–1452. 10.1001/jama.2019.2560. [DOI] [PubMed] [Google Scholar]


