Abstract
Aim
This study aims to explore the change process among chronic kidney disease patients in shared decision‐making.
Design
Qualitative research is the design applied.
Method
Original transcripts from an earlier study involving a purposive sample of 31 patients with chronic kidney disease provided a source of information. The data collection was conducted from August 2017–January 2018. Data analysis applied the thematic analysis method.
Results
Three themes were identified: from avoidance to being forced to accept, decision‐making process of action and facilitating factors. After making the psychological adjustments necessary for undergoing dialysis treatment, participants experience the process of decision‐making action. The improvement of knowledge and ability increases the patient's self‐determination consciousness and strengthens confidence in decision‐making. The nurse and the patient's family are both important facilitating factors, and they assist through the entire SDM process.
Keywords: chronic kidney disease, renal replacement therapy, shared decision‐making
1. INTRODUCTION
End‐stage renal disease (ESRD) is a serious public health problem, and its incidence and prevalence are increasing globally (Wetmore & Collins, 2016). According to a report by the United States Renal Data System, the incidence and prevalence of ESRD in Taiwan have ranked first worldwide for many years (U. S. Renal Data System., 2018). In addition to kidney transplantation and conservative management, haemodialysis and peritoneal dialysis are currently the primary therapies for ESRD. These different treatment options will have different effects on a patient's family, work and social activities (Hamilton et al., 2017; Khan et al., 2019). Through shared decision‐making (SDM), patients can obtain information regarding different renal replacement therapies (RRT) and their impacts on future daily life, and thereby make appropriate choices. The purpose of this study, therefore, is to describe the psychological change process of participants with chronic kidney disease (CKD) during the SDM process. It is hoped that improved understanding of this process in participants engaging in SDM may lead to interventions that can increase the effectiveness of SDM and is aimed at assisting patients in choosing the appropriate RRT.
2. BACKGROUND
Shared decision‐making is an approach used in the clinical situation that desires the intentional and cooperative involvement of both patients and healthcare professionals (HCPs) in the process of deliberation about treatment options (Gionfriddo et al., 2014). SDM is viewed as fundamental to safe and effective health care, and when there are reasonable options available to patients, it encapsulates a more patient‐centric healthcare target (Joseph‐Williams et al., 2014), which includes three stages: an information exchange, a deliberation regarding the available treatment options and reaching agreement on a final decision (Charles et al., 1999). In the SDM process, HCPs contribute by providing information regarding the risks and benefits of the different treatment options, whereas patients put forward their own values and preferences. Both parties share information and then agree on the final treatment to be implemented (Charles et al., 1997).
The application of SDM for renal RRT is to assist CKD patients in making the appropriate choice of RRT and in making the necessary preparations. Presently, most research in this area has focused on various SDM interventions. The results of such studies have shown the effectiveness levels of the different interventions, including increased levels of knowledge and decision self‐efficacy, as well as the ability to decrease decisional conflict (Bailey et al., 2016; Causarano et al., 2015). However, although SDM interventions for patients have been well researched, the psychological change process in patients while engaging in SDM is not yet known. Many discussions have been made on the factors affecting RRT decision‐making in the past. Two systematic reviews in kidney care found that patients' decision‐making was influenced by the following factors: the acquisition of relevant knowledge; the relationship with others (family or HCPs); disruption to current life; the desired degree of control; and risks and benefits of treatment (Harwood & Clark, 2013; Morton et al., 2010). In addition, the role of culture and language, patient‐professional communication (trust and power‐distance), decisional awareness and decision ability were also influencing factors (Muscat et al., 2018). These factors provide valuable information, however, identifying the influencing factors of the choice of dialysis treatment did not convey the patient's personal experience in SDM. SDM differs from the general decision‐making process, for it emphasizes the transfer of power and the improvement of ability. Therefore, it is important to understand how the patient's motivation for participation was driven, in addition to the process of improving ability and decision‐making awareness. These psychological changes of decision‐making were very important.
Nurses, as the largest group of healthcare providers, are key in assisting participants in choosing the appropriate RRT. As participants engage in SDM, nurses must understand the patients’ psychological changes as they proceed through the SDM process. Therefore, more studies are needed to expand the understanding of the psychological changes of patients during the SDM process. We applied the qualitative approach to capture the unique experiences of CKD patients during the SDM process and make helpful suggestions in order to assist patients in making informed decisions.
3. METHODS
3.1. Design
A qualitative study was conducted from August 2017–January 2018. Qualitative data obtained from an earlier study are reported in this paper. Quantitative and qualitative data were collected simultaneously for this study (Ho et al., 2019). We conducted three interviews for each participant according to the three stages of SDM. All of the qualitative data collected were drawn from the contents of these interviews during the SDM process.
3.2. Participants
Original transcripts from an earlier study involving a purposive sample of 31 participants with CKD provided a source of information. Patients in the original mixed‐methods study (Ho et al., 2019) required the following criteria: diagnosis of CKD with a glomerular filtration rate <30 ml/min per1.73 m2, minimum age of 20 years old and the ability to communicate in Mandarin. We excluded those potential participants with absolute contraindications for haemodialysis or peritoneal dialysis. The primary researcher of this study is a nephrology nurse at the recruiting hospital. The participants were approached and recruited in face‐to‐face conversations by the primary researcher during appointments at the hospital. In total, 36 participants were approached. Of those, three refused to continue at some point, one dropped out due to hospitalization, and one did not return to the clinic. Therefore, a total of 31 participants were ultimately included in the study.
3.3. Data collection
The primary researcher who had regular care responsibilities for the participants and had relationships of trust with them conducted the interviews. Each participant of this study took part in three face‐to‐face interviews lasting about 30–50 min each time, with one‐month intervals between each interview. Each interview had its agenda based on the three stages of SDM. The primary researcher of this study and participants shared their views and opinions based on the agenda. The agenda for the first interview (C1) was to understand the participant's perception about their disease and to understand their views on dialysis treatment. The second agenda (C2) obtained their preferences for different treatment options. Their final decision and reasons for making the decision were shared in the third agenda (C3). Participants of this study were encouraged to freely share their feelings about the disease, their thoughts on dialysis treatment, and their experiences with the decision‐making process. Audio recordings were made during all of the interviews and were transcribed verbatim within 24 hr, and additionally, field notes were taken by the primary researcher.
3.4. Data analysis
This study applied the thematic analysis method because it is particularly useful for processing open‐ended question responses obtained in interview data (Kao, 2001). First, the given transcript was read several times as a whole to determine any hidden significance. Second, the key points, events or feelings in the verbatim transcripts were reviewed and were given a preliminary open coding. Preliminary categorization of the open coding was conducted in order to discover the conceptual attributes, and those conceptual attributes were then named with appropriate terms according to the initial categorization. Third, the related names were compared and summarized into sub‐themes. The common sub‐themes between the transcripts were then summarized to form themes. Excel was used to manage the data. The primary researcher coded the data and verified it with one other researcher to refine the different concept categories and identify relationships among these categories. Reporting adheres to the consolidated criteria for reporting qualitative research checklist.
3.5. Rigour
We applied the concepts of credibility, dependability, transferability and confirmability to evaluate the rigour of the research (Streubert & Carpenter, 2010). The primary researcher has received qualitative interview training, had regular care responsibilities for the participants and had developed relationships of mutual trust with them. In addition to this, we also conducted peer debriefing. After ending each stage of consultation interviews, we randomly selected one interview record for a peer debriefing, and the two researchers then compared and discussed their interpretations of the data until a consensus was reached on the interpretation that was most consistent with the original meaning of the data, an approach that contributed to the credibility and dependability of data. The transferability of the findings was also secured by generating detailed descriptions of the study methodology, sample selection criteria, data collection process and context. Finally, the confirmability of the findings was also secured by checking the associated notes and text of the original data to ensure that the interpretations of the findings were not influenced by personal opinions and biases.
3.6. Ethical
The study protocol for the earlier study and this secondary analysis was approved by the research ethics committee (CRREC‐106‐058). Informed consent for participation and recording was obtained before the first consultation interview began with a given participant. To maintain anonymity, all of the participants were only assigned numbers, and all identifying data have been excluded.
4. RESULTS
Thirty‐one participants ranging in age from 27 to 86 years were included in the original study (Ho et al., 2019). The mean age of the participants was 63.5 years (SD = 13.8). Among them, the majority of participants were male (51.6%). Most of the participants were unemployed (80.6%), and 13 (41.9%) had an elementary school level of education or less (Table 1). According to study results, we identified the SDM process for RRT (Figure 1). The data extract process is shown in Table 2.
TABLE 1.
Participant characteristics
| NO | Ages | Gender | Employment status | Education level |
|---|---|---|---|---|
| NO.2 | 74 | Male | Retirement (Professor) | Graduate school |
| NO.3 | 76 | Male | Retirement | Elementary school |
| NO.4 | 61 | Female | Unemployed | High school |
| NO.5 | 70 | Female | Unemployed | Elementary school |
| NO.6 | 70 | Female | Unemployed | Elementary school |
| NO.10 | 57 | Male | Truck driver | High school |
| NO.11 | 40 | Female | Housewife | High school |
| NO.12 | 63 | Female | Unemployed | Junior high school |
| NO.13 | 48 | Male | Repairman | Elementary school |
| NO.14 | 78 | Female | Unemployed | Illiterate |
| NO.15 | 44 | Female | Housewife | High school |
| NO.16 | 62 | Female | Unemployed | Elementary school |
| NO.17 | 27 | Male | Waiter | University |
| NO.18 | 52 | Male | Unemployed | Junior high school |
| NO.19 | 56 | Male | Unemployed | College school |
| NO.20 | 74 | Female | Unemployed | Elementary school |
| NO.22 | 68 | Female | Unemployed | Junior high school |
| NO.23 | 86 | Male | Unemployed | Illiterate |
| NO.24 | 72 | Male | Unemployed | Elementary school |
| NO.25 | 82 | Female | Unemployed | Elementary school |
| NO.26 | 79 | Male | Retirement | Elementary school |
| NO.27 | 79 | Female | Unemployed | Illiterate |
| NO.28 | 70 | Male | Retirement | High school |
| NO.29 | 62 | Male | Unemployed | High school |
| NO.30 | 74 | Male | Unemployed | Junior high school |
| NO.31 | 60 | Female | Unemployed | Elementary school |
| NO.32 | 59 | Female | Waitress | High school |
| NO.33 | 74 | Male | Unemployed | Elementary school |
| NO.34 | 50 | Male | Part‐time job | High school |
| NO.35 | 55 | Female | Housewife | University |
| NO.36 | 46 | Male | Painter | Junior high school |
FIGURE 1.
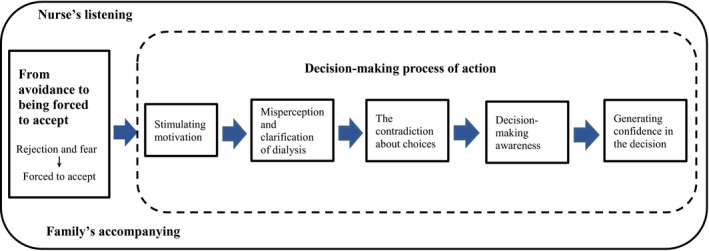
Shared decision‐making for renal replacement therapy
TABLE 2.
Data extract process
| Theme | Subtheme | Preliminary categorization | Open coding |
|---|---|---|---|
| From avoidance to being forced to accept | Rejection and fear | At a loss for the future | What problems will I face after dialysis? The end of the meaning of life Loss of autonomy |
| I do not want dialysis, refusing to understand | I do not want dialysis yet Go to the hospital three times a week Refusing to understand | ||
| Forced to accept | Awareness of disease | Symptoms appear Decreased kidney function | |
| I had to accept it | Unavoidable fact Even if you feel scared, you still have to face it | ||
| Decision‐making process of action | Stimulating motivation | Needs after acceptance of dialysis | Began interested in dialysis Pose questions |
| Motivation | The doctor told me the condition Feel uncomfortable | ||
| Misperception and clarification of dialysis | External clues provided by non‐professionals | Information from the Internet or books Information provided via news media Information from friends or neighbours | |
| Inherent views | Hearsay Misperceptions Negative experiences of others | ||
| The contradiction about choices | The impacts of one's future life | Time and place can be flexible Autonomy Maintain the current lifestyle Affect my work | |
| To weigh the pros and cons | Take away my freedom Impact on the family Kidney donation will affect a family member's health | ||
| Decision‐making awareness | I can have another choice | I had the right to choose Seeking answers to questions | |
| Behavioural activation | Actively asking questions Proactively discuss with the doctor | ||
| Generating confidence in the decision | Knowledge increased confidence | I can perform peritoneal dialysis by myself Past successful experiences | |
| What suits me best | I know what suits me The better option for me | ||
| Facilitating Factors | Families accompanying | Psychological comfort | Family is my supportive power Share my worries |
| Support my decision | My choice is supported by my family family discuss together | ||
| Nurse's listening | Listening to me | Can relax to inquire Analyse the pros and cons with me | |
| Trusted confidant | Pour out my worries Trust each other |
4.1. From avoidance to being forced to accept
An antecedent event consisting of a psychological change process had to occur before the action process could begin. The avoidance was usually the participant's first response, and some even refused to engage in conversations about dialysis. But after recognizing the severity of the decline in renal function, they were forced to accept dialysis.
4.1.1. Rejection and fear
When told they had to receive dialysis treatment, most of the participants refused to accept it. Some of the participants felt that they had lost a meaningful life, they feared a life of suffering, and they perceived such a life to be worse than death. For example, one of the participants said,
I think if really I have to do it, I think every day is the last day (NO.11_ C1).
Some participants feared dependence on family members or the loss of autonomy in managing daily life. One of the participants said,
My husband and I can’t drive, I have to let my son pick me up to the hospital for dialysis three times a week. This means that everything depends on the child (NO.14_ C1).
Participants refused to face the dialysis treatment, so they had no motivation to understand the different forms of RRT, and became even more resistant to and afraid of RRT. As one patient put it:
I didn’t want to listen to any information about dialysis before because I couldn’t accept the need for dialysis at that time. When I really accepted my need for dialysis, maybe I was also afraid, very afraid … Of course, I was afraid because I had never had dialysis, so I didn’t know what would happen (NO.15_ C2).
4.1.2. Forced to accept
For many participants who had not yet suffered severe symptoms of CKD at the time of their decision‐making, the experience of gradually worsening symptoms led them to eventually favour dialysis. As one participant described it, reports from his physician regarding his disease condition, coupled with the downward trends in his kidney function indicated by his blood draw reports, caused him to begin to realize that he needed dialysis.
My body seems to have the symptoms I was told I would have, and the doctor told me about the possibility of starting dialysis. At that time, I started to feel uncomfortable, and I couldn’t take part in daily life, so, in fact, I was forced to accept reality … I was helpless, but I had to accept it (NO.2_ C1).
The participants explained how their daily life was influenced by increasingly severe symptoms, forcing them to face the fact that dialysis was necessary.
The kidneys won't get better even if you take medicine. I still can't work. I can only be…accept it. What can I do if I don't accept it? (NO.20_ C1).
Among many participants, dialysis decisions were perceived as a choice between a life‐saving measure and facing death. Some participants realized that dialysis was necessary for survival and chose to accept dialysis as there was no alternative. Many other participants accepted dialysis when physical symptoms became more apparent and began affecting their daily life.
4.2. Decision‐making process of action
When participants experience a psychological adjustment process and can face their dialysis needs, there will be greater motivation to understand dialysis. This is the start of the SDM action process for participants.
4.2.1. Stimulating motivation
Once participants come to a decision to accept dialysis and recognize the need for it, their motivation will be stimulated. This leads to a participant endorsing or identifying with the value or importance of a behaviour, and motivation to understand dialysis treatment. Two participants described their interest in dialysis treatment as follows:
Last year, I didn’t have the symptoms. However, I feel uncomfortable this year, the doctor is telling me that my kidney function is poor….I had to face dialysis, I think I had to try to understand dialysis better (NO.29_C2).
I don't know what dialysis treatment is … I was not curious before, but now I am… I want to know more about it (NO.11_ C2).
4.2.2. Misperception and clarification of dialysis
Participants used the knowledge of various modalities to assess how particular dialysis modalities would impact their future life, but lack of familiarity with dialysis and reliance on information from external clues led to misperceptions regarding the treatment. A participant's ideas often come from external clues provided by non‐professionals, including the news media, the Internet or books. As one participant said,
I read in a book that it can have the problem of the reverse intake of dialysates, which I thought would make my edema worse….but this turned out not to be the case, peritoneal dialysis will not make my symptoms worse (NO.2_C2).
Many of the participants had preconceptions of dialysis based on life experiences and also word‐of‐mouth communication, which led to a negative perception of dialysis treatment. A participant put it this way:
I heard others say that peritoneal dialysis requires intubation, and I thought that the tube would be very long, and not easy to carry. I did not expect… the peritoneal dialysis catheter is so short (NO.13_C2).
For some participants, these perceptions were influenced by witnessing friends undergo dialysis and the negative impacts that it had on their lives. One participant said,
When I saw my friend's discomfort after dialysis, I thought hemodialysis seemed to have many problems, but now it sounds like there are not so many problems as long as the water intake is controlled (NO.28_C2).
4.2.3. The contradiction about choices
Participant's clarified any misunderstandings regarding dialysis treatment; however, they often faced contradictions when choosing the appropriate treatment. Participants did not want to change their current lifestyles more than necessary and considered their personal values and preferences. All of the study participants described their choice as a process involving various contradictions. Facing and making decisions about dialysis were stressful for participants. They had to consider their current life, values and anticipated future life. They talked about considering various potential choices, as well as about which of their preferences were most important. As one of them said,
I wonder if I could replace the dialysate by myself, which would be more flexible for me … Yes, I have financial considerations. I still have to work, so it would be best if the choice of dialysis does not affect my ability to work (NO.17_ C2).
Some participants believed that the time‐consuming nature of dialysis would restrict their daily life and take away their freedom. As one participant said,
Although I think that dialysis treatment performed by medical staff is safer, I have to think about it… because if I go for dialysis… no doubt I will have to go to the hospital three times a week (NO.3_C2).
Although participants know that kidney transplantation is the best option, few participants chose this treatment during the interviews. This differs from viewpoints in Western culture. In Chinese culture, parents usually consider the health of their children to be more important than their own health.
It sounds like a kidney transplant would be good, but if my son donates a kidney to me, what would he do if his other kidney gets damaged (NO.5_C2)?
Throughout the interviews, the participants asked the researcher many questions regarding dialysis. Many of these questions were related to the different types of dialysis treatment and dialysis access. The questions represent contradiction and uncertainty. Consultations provided information about dialysis treatment that they could relate to the context of their own life in order to make modality choices. The researcher and participant relationship helped to clarify the participant's personal values and preferences enabling the participant to select their own suitable dialysis method.
I am concerned about dialysis tubes….I really feel concerned about infection…but after the consultations with you, I think that peritoneal dialysis is more suitable for me because I need to work (NO.36_ C3).
4.2.4. Decision‐making awareness
When participants gain knowledge in the decision process, they become more engaged in decision‐making. One participant began to realize that they had the right to choose their preferred treatment during the consultation and to actively seek discussions with doctors. A 44‐year‐old woman described active choices characterized by many deliberations with the doctor,
In the past, the doctor never told me that peritoneal dialysis was an option. He said, ‘I don’t think you’re suitable for that; rather, your best options are hemodialysis … but now that I know about peritoneal dialysis … I can make a choice (C2). I know the doctor has my best interests in mind, but I think that peritoneal dialysis is the better option for me. It isn’t the doctor who must ultimately decide. I discuss it with the doctor, I think that peritoneal dialysis is the better option for me (C3).
4.2.5. Generating confidence in the decision
For most of the participants, improvements in their knowledge gave them increased confidence in choosing a dialysis treatment method. After realizing that they had the right to choose and comparing the relevant advantages and disadvantages, a participant expressed that they will choose a treatment method that is more in line with their expectations. As a 74‐year‐old male participant stated,
At that time, the doctor asked me to undergo a fistula surgery, I just listened to the doctor (C1) … I think I will decide to choose one of these two treatments (hemodialysis or peritoneal dialysis) (C2) … Now, I think peritoneal dialysis is more suitable … I think I will discuss it with the doctor (C3).
Case 17 was a participant with type 1 diabetes. After understanding the different RRT, he thought that he could perform peritoneal dialysis without problems, and his successful experiences in performing insulin injections in the past also strengthened his confidence in performing peritoneal dialysis. He said,
I think it’s a habit problem, just like insulin injections, and now I’m used to that … I think I can replace the dialysate myself. I think peritoneal dialysis is more suitable for me because I think hemodialysis would be more inconvenient, I need to work (NO.17_ C3).
4.3. Facilitating factors
4.3.1. Nurse's listening
Most participants felt comfortable during the interview. Throughout the SDM process, the primary researcher of this study, and also the nurse, provided emotional support for the participant and helped to reduce the participant's psychological pressure. One participant said,
I felt like this process was almost unbearable. The doctor was somewhat intimidating to me, and while the doctor didn’t ask me to meet with you, I do find that I want to discuss things with you and that after doing so, I feel better (NO.2_C2).
The primary researcher of this study also provided informational support for participants during the interview, so that participants could clarify their concerns and choose the treatment method most suitable for them.
I used to reject the need for dialysis. When the doctor told me about it, I didn’t want to hear it, but I felt that what you said seemed quite reasonable. That is, not always asking me about dialysis, but helping me analyze how I will receive treatment in the future (NO.11_ C3).
4.3.2. Family accompanying
In Chinese culture, the support and understanding of family members are important, and family members will usually discuss the options together. For every participant, decision‐making was shared with members of their family. As one participant said,
In discussing it with my family, we considered many problems … My family still thinks that hemodialysis should be more suitable for me, so I think I will choose hemodialysis (NO.10_ C3).
These narratives reflected negotiation between participants and their families and showed the powerful influence that families had over participants' decisions. In the decision‐making process, the family is the main source of emotional support. In contrast to the more informational support provided by health professionals, the family provides substantial emotional support to participants. As one participant responded,
I will tell my parents what the doctor said, and my mother always tells me to be cheerful … as long as I have any condition, I always will tell them about it, and then I will feel better (NO.17_ C1).
5. DISCUSSION
The results of this study presented the change process with improvement in the participant's ability and power transfer during the process of participating in SDM. Avoidance and fear were usually the initial reactions of the participants, but after realizing the serious impact of the disease on their life, they were forced to accept the dialysis. Initially, participants felt stressed when encouraged to share in making health‐related decisions. This was not the traditional way. Through encouragement and knowledge about their health condition, they overcame their original fears and were able to work together with the physician to make informed decisions related to their health care. Increasing the participant's motivation was a factor in a participant's willingness to learn about their disease and to follow the process towards final decision‐making. This involved clarifying misunderstandings about dialysis treatment, gaining confidence with more knowledge, discussing their values and opinions, learning about the various treatment methods, and finally enhancing their ability to choose the treatment they would prefer.
5.1. Accept the need for dialysis to trigger the motivation
Autonomy is one of the main concepts underlying SDM (Obeidat et al., 2013). A prerequisite for autonomy is that the patient has awareness of and cognitive motivation regarding the disease, including feeling the impact and threat of the disease to their existing life or social role (Ellis‐Stoll & Popkess‐Vawter, 1998). In particular, CKD is a “silent disease.” Most patients with CKD lack awareness of the disease. In our study, we found that, when faced with the impact of dialysis treatment, a participant's first response is typically to deny the need for dialysis. At that point, the participant has no motivation to understand the nature of RRT. It is only when the participant accepts the need for dialysis that they begin to be motivated to understand the disease. Charles et al., 2004 pointed out that the patients’ preparation regarding the disease is one of the contributing factors for their participation in SDM. When the patient is not ready to face the disease, they will not be willing to participate in SDM (Charles et al., 2004). In the social cognition theory of Bandura, it is mentioned that the three factors of people, behaviour, and environment will interact to affect an individual's behaviour. Personal beliefs and motives, etcetera, often strongly and powerfully control and guide people's behaviours, and those behaviours and their results will in turn affect the content and emotional response of personal thinking (Bandura, 1977). When a patient's intrinsic motivation is activated and awakens the consciousness needed to make one's own decisions, the patient will want to further understand the different RRTs and will show active decision‐making participation through their behaviours. Therefore, it is important to stimulate a patient's awareness of the disease before engaging in SDM; the patient must realize that they have to face dialysis in the future, and then, the motivation to understand the options will be triggered.
5.2. SDM involves the knowledge and power transfer
In our study, we found that participants are often passive recipients in medical decision‐making at the beginning. In Taiwan's medical culture, patients generally believe that they lack relevant knowledge. When patient's participation in decision‐making is not valued by HCPs, and when patients feel limited by a HCPs professional authority, patients can easily become “invisible” and feel they dare not express their opinions. Charles et al., 1997. pointed out that SDM is seen as a mechanism to decrease the knowledge and power asymmetry between doctors and patients by increasing patients' information and sense of autonomy; it should be regarded as a process of empowering the patient (Charles et al., 1997). More specifically, HCPs should seek to provide complete information to achieve the purpose of enhancing the patient's knowledge and ability in decision‐making. The sharing of knowledge between HCPs and patients can increase their sense of autonomy and control, bringing greater balance to the power imbalance between patients and HCPs. This knowledge will also assist in enhancing the patient's confidence in making decisions. In addition, ability improvement will increase active participation, building patient confidence, and achieving the purpose of power transfer. Therefore, “ability improved” will strengthen “power transfer” and vice versa.
5.3. Decision‐making factors
Our study has found that the selection of the dialysis method by a participant was a process of contradictory decision‐making and strongly influenced by the participant's values, personal background and desire for minimal disturbance in life. The results were similar to those of Morton et al., (2010) and Harwood and Clark (2013). A systematic literature review by Morton et al., (2010) concluded that the core factors affecting treatment choices were confronting mortality, lack of choice, obtaining knowledge of available choices and weighing how to maintain their lifestyle. Harwood and Clark (2013) pointed out that the elements in decision‐making were the consideration of life and death, the minimal interference of dialysis on personal life and the necessary knowledge. The participants expressed many questions about dialysis and life with dialysis throughout the interviews. Therefore, increasing knowledge about dialysis is important for decision‐making and reducing uncertainty, for the decision‐making process involves weighing the perceived risks and benefits of different RRTs. Personal factors influenced dialysis modality decisions, especially the impact on a patient's lifestyle. There were many discussions between HCPs and patients focusing on patient values and the impact of different RRTs, enabling patients to make informed choices.
5.4. SDM source of support
Our study has found that the psychological support given to a participant by a nurse can soothe the participant's unease in the face of unknown dialysis treatment encouraging them to speak more freely about their concerns. The trust relationship between patients and HCPs helped override patients’ fears and concerns regarding dialysis (Griva et al., 2019) and encouraged patients’ to obtain medical information (Harwood & Clark, 2013), for patients felt safer in engaging in discussions with HCPs. The study pointed out that trusting relationships were seen as crucial to active participation with clinical decisions, and patients felt more at ease and able to confide and share personal information with HCPs (Cervantes et al., 2016; Walker et al., 2017). In our study, mutual trust makes participants more willing to share their life experiences, values, preferences, strengthening the effective transmission of knowledge and to be at ease asking questions when discussing treatment options. Therefore, the trust relationship is indispensable during the decision process, especially in SDM. In this process, a sense of being respected, understood and cared for is essential to forming the experiences of connection and trust. Establishing such trust should start even before the beginning of the SDM process.
Although trust may enhance SDM, it may also foster a more passive patient role (Muscat et al., 2018; Peek et al., 2013). Patients who lack expertise often look for the opinion of professionals. This suggests that excessive trust in the HCPs can create passivity and hinder the patient from making decisions autonomously. In Taiwan's medical culture, information provided by HCPs is viewed by patients as superior to their own. In SDM, information was shared, and this highlights a need for HCPs to support patients, helping them to become aware of the unique contributions that they bring to decision‐making such as their personal values and preferences. Peek et al., 2013 pointed out that trust was also enhanced when patients felt HCPs encouraged them to share information, which creates a good cycle thereby balancing trust in professionals.
Social support is an important factor affecting decision‐making, especially from their family members (Harwood & Clark, 2013). According to our study, family members have always been a powerful source of participant support. This was similar to the results of Harwood and Clark (2014) finding that family members provide assistance with decision‐making and emotional support. An earlier study similarly found that patients rely on family members for support throughout their dialysis decisions, and regardless of race, this kind of influence on the decision was consistent (Muscat et al., 2018). The influence of family support was more significant, especially for the elderly. Harwood and Clark (2014) found that age was not a barrier to home dialysis. If there is not enough family support, older adults with CKD have limited options. In our study, most of the participants expressed the need to discuss the decision with their families, and they would not make decisions alone. In traditional Chinese culture, medical decision‐making usually requires family members to participate, and the patient hopes that his family can not only participate, but also support his decision‐making; family relations cannot be ignored in medical decision‐making in traditional Chinese cultures. The patients rely on the support of their family members, but their choice of dialysis also affects their family members (Harwood & Clark, 2013). Even if young patients have the ability to make decisions, they must consider the impacts and burdens of their decisions on other family members when making those decisions. Therefore, the family plays a very important role in the SDM process in Asian cultures. Despite family members having to shoulder the responsibilities of care, however, they demonstrate a willingness to support patients in undergoing dialysis, showing the degree to which Asians traditionally value family. Ability improvement was important not only for the patient but also for the family because decision‐making was collaborative. In order for family members to provide support during the SDM process, they too were required to gain knowledge about dialysis (Harwood & Clark, 2014). Information was shared between the patients, family and HCPs, so every attempt should be made to include families in the SDM process. Together, our findings lend support for families to be included in the SDM, which reinforces the need for family members to participate in decision‐making.
5.5. Limitations
There were some limitations to our study. All the participants were from the same hospital, and there was minimal diversity in the areas that the participants came from. This limitation may influence the transferability of the findings to similar groups of CKD patients. We hope to address this limitation through future studies conducted in other geographic locations. Furthermore, some patients refused to be interviewed, because they did not want to talk about dialysis treatment. This could have distorted the views of this study report, insofar as it reflects the perspectives of patients who were more open to talking about their decision‐making experiences.
6. CONCLUSION
This paper has implications for HCPs, both as change agents in the SDM process in their roles of fostering the active involvement of CKD patients. Our study provides important new information about the SDM process for RRT. Understanding this process may help patients make informed and autonomous treatment decisions. After making the psychological adjustments necessary for undergoing dialysis treatment, patients experience the decision‐making process. After receiving the knowledge of options, the participants will begin to think about the impacts of different treatments on their future life and may swing back and forth between different choices because of contradictions. The improvement of knowledge and ability makes the patient's self‐determination consciousness rise and strengthens the confidence of decision‐making. This result revealed the outcome of the empowerment process. The nurse and the patient's family are both important facilitating factors in the SDM mode, and they run through the entire SDM process.
CONFLICT OF INTEREST
No conflict of interest has been declared by the authors.
AUTHOR CONTRIBUTIONS
YFH, YCC and ICL: Research idea and study design, data analysis/interpretation. ICL: Supervision or mentorship. YFH: Data acquisition. Each author contributed important intellectual content during manuscript drafting or revision, accepts personal accountability for the author's own contributions, and agrees to ensure that questions pertaining to the accuracy or integrity of any portion of the work are appropriately investigated and resolved.
ACKNOWLEDGMENTS
The authors would like to thank all the patients, nephrology nurses and physicians for their assistance in the study process.
Ho Y‐F, Chen Y‐C, Li I‐C. A qualitative study on shared decision‐making of patients with chronic kidney disease. Nursing Open. 2021;8:3430–3440. 10.1002/nop2.891
Funding information
This work was supported by the China Medical University, Taiwan (grant number: CMU109‐N‐23). The funders did not have a role in study design, data collection, analysis, reporting or the decision to submit for publication.
DATA AVAILABILITY STATEMENT
The data presented in this study are available on request from the corresponding author.
REFERENCES
- Bailey, R. A. , Pfeifer, M. , Shillington, A. C. , Harshaw, Q. , Funnell, M. M. , VanWingen, J. , & Col, N. (2016). Effect of a participant decision aid (PDA) for type 2 diabetes on knowledge, decisional self‐efficacy, and decisional conflict. BMC Health Services Research, 16, 10. 10.1186/s12913-016-1262-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandura, A. (1977). Self‐efficacy: Toward a unifying theory of behavioral change. Psychological Review, 84, 191–215. 10.1037//0033-295X.84.2.191 [DOI] [PubMed] [Google Scholar]
- Causarano, N. , Platt, J. , Baxter, N. N. , Bagher, S. , Jones, J. M. , Metcalfe, K. A. , Hofer, S. O. P. , O’Neill, A. C. , Cheng, T. , Starenkyj, E. , & Zhong, T. (2015). Pre‐consultation educational group intervention to improve shared decision‐making for post mastectomy breast reconstruction: A pilot randomized controlled trial. Supportive Care in Cancer, 23, 1365–1375. 10.1007/s00520-014-2479-6 [DOI] [PubMed] [Google Scholar]
- Cervantes, L. , Zoucha, J. , Jones, J. , & Fischer, S. (2016). Experiences and values of latinos with end stage renal disease: A systematic review of qualitative studies. Nephrology Nursing Journal, 43(6), 479–494. [PubMed] [Google Scholar]
- Charles, C. , Gafni, A. , & Whelan, T. (1997). Shared decision‐making in the medical encounter: What does it mean? (or it takes at least two totango). Social Science & Medicine, 44(5), 681–692. 10.1016/S0277-9536(96)00221-3 [DOI] [PubMed] [Google Scholar]
- Charles, C. , Gafni, A. , & Whelan, T. (1999). Decision‐making in the physician‐participant encounter: Revisiting the shared treatment decision‐making model. Social Science & Medicine, 49(5), 651–661. 10.1016/S0277-9536(99)00145-8 [DOI] [PubMed] [Google Scholar]
- Charles, C. , Gafni, A. , & Whelan, T. (2004). Self‐reported use of shared decision‐making among breast cancer specialists and perceived barriers and facilitators to implementing this approach. Health Expectations, 7, 338–348. 10.1111/j.1369-7625.2004.00299.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis‐Stoll, C. C. , & Popkess‐Vawter, S. (1998). A concept analysis on the process of empowerment. Advances in Nursing Science, 21, 62–68. 10.1097/00012272-199812000-00007 [DOI] [PubMed] [Google Scholar]
- Gionfriddo, M. R. , Leppin, A. L. , Brito, J. P. , LeBlanc, A. , Boehmer, K. R. , Morris, M. A. , Erwin, P. J. , Prokop, L. J. , Zeballos‐Palacios, C. L. , Malaga, G. , Miranda, J. J. , McLeod, H. M. , Rodríguez‐Gutiérrez, R. , Huang, R. , Morey‐Vargas, O. L. , Murad, M. H. , & Montori, V. M. (2014). A systematic review of shared decision making interventions in chronic conditions: A review protocol. Systematic Reviews, 3, 38. 10.1186/2046-4053-3-38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griva, K. , Seow, P. S. , Seow, T. Y. , Goh, Z. S. , Choo, J. , Foo, M. , & Newman, S. (2019). Participant‐related barriers to timely dialysis access preparation: A qualitative study of the perspectives of participants, family members, and health care providers. Kidney Medicine, 2, 29–41. 10.1016/j.xkme.2019.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton, A. J. , Clissold, R. L. , Inward, C. D. , Caskey, F. J. , & Ben‐Shlomo, Y. (2017). Sociodemographic, psychologic health, and lifestyle outcomes in young adults on renal replacement therapy. Clinical Journal of the American Society of Nephrology, 12, 1951–1961. 10.2215/CJN.04760517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harwood, L. , & Clark, A. M. (2013). Understanding pre‐dialysis modality decision‐making: A meta‐synthesis of qualitative studies. International Journal of Nursing Studies, 50, 109–120. 10.1016/j.ijnurstu.2012.04.003 [DOI] [PubMed] [Google Scholar]
- Harwood, L. , & Clark, A. M. (2014). Dialysis modality decision‐making for older adults with chronic kidney disease. Journal of Clinical Nursing, 23, 3378–3390. 10.1111/jocn.12582 [DOI] [PubMed] [Google Scholar]
- Ho, Y. F. , Chen, Y. C. , Huang, C. C. , Hu, W. Y. , Lin, K. C. , & Li, I. C. (2019). The effects of shared decision making in different renal replacement therapies decision in participants with chronic kidney disease (CKD). Journal of Nursing Research, 28, e109. 10.1097/jnr.0000000000000386 [DOI] [PubMed] [Google Scholar]
- Joseph‐Williams, N. , Elwyn, G. , & Edwards, A. (2014). Knowledge is not power for participants: A systematic review and thematic synthesis is of participant‐reported barriers and facilitators to shared decision making. Participant Education and Counseling, 94, 291–309. 10.1016/j.pec.2013.10.031 [DOI] [PubMed] [Google Scholar]
- Kao, S. C. (2001). The lifeworld of chinese women living with their husbands studying abroad: Interpretation and reflection. Indigenous Psychological Research in Chinese Societies, 16, 225–285. 10.6254/2001.16.225 [DOI] [Google Scholar]
- Khan, A. , Khan, A. H. , Adnan, A. S. , Sulaiman, S. , & Mushtaq, S. (2019). Prevalence and predictors of depression among hemodialysis participants: A prospective follow‐up study. BMC Public Health, 19, 531. 10.1186/s12889-019-6796-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morton, R. L. , Tong, A. , Howard, K. , Snelling, P. , & Webster, A. C. (2010). The views of participants and carers in treatment decision making for chronic kidney disease: Systematic review and thematic synthesis of qualitative studies. BMJ (Clinical Research ed.), 19, 340:c112. 10.1136/bmj.c112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muscat, D. M. , Kanagaratnam, R. , Shepherd, H. L. , Sud, K. , McCaffery, K. , & Webster, A. (2018). Beyond dialysis decisions: A qualitative exploration of decision‐making among culturally and linguistically diverse adults with chronic kidney disease on haemodialysis. BMC Nephrology, 19, 339. 10.1186/s12882-018-1131-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Obeidat, R. F. , Homish, G. G. , & Lally, R. M. (2013). Shared decision making among individuals with cancer in non‐Western cultures: A literature review. Oncology Nursing Forum, 40, 454–463. 10.1188/13.ONF.454-463 [DOI] [PubMed] [Google Scholar]
- Peek, M. E. , Gorawara‐Bhat, R. , Quinn, M. T. , Odoms‐Young, A. , Wilson, S. C. , & Chin, M. H. (2013). Participant trust in physicians and shared decision‐making among African‐Americans with diabetes. Health Communication, 28, 616–623. 10.1080/10410236.2012.710873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Streubert, H. J. , & Carpenter, D. R. (2010). Qualitative research in nursing: Advancing the humanistic imperative, 5th ed. Lippincott Williams & Wilkins Publications. [Google Scholar]
- U. S. Renal Data System., 2018 2018 ADR Chapters: End‐stage renal disease (ESRD) in the United States‐International comparisons. https://www.usrds.org/2018/view/Default.aspx [Google Scholar]
- Walker, R. C. , Walker, S. , Morton, R. L. , Tong, A. , Howard, K. , & Palmer, S. C. (2017). Māori participants' experiences and perspectives of chronic kidney disease: A New Zealand qualitative interview study. British Medical Journal Open, 7, e013829. 10.1136/bmjopen-2016-013829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wetmore, J. B. , & Collins, A. J. (2016). Global challenges posed by the growth of end‐stage renal disease. Renal Replacement. Therapy, 2, 15. 10.1186/s41100-016-0021-7 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.


