Abstract
Purpose
Children with chronic diseases exhibit a higher incidence of emotional–behavioural problems. Though sandplay therapy is a universally recognized psychological treatment method, experimental evidence for this form of therapy is lacking. Our aims were to examine the effectiveness of sandplay therapy in reducing emotional and behavioural problems in school‐age children with chronic diseases as well as anxiety and depression in their caregivers.
Design and methods
A total of 60 children and their caregivers were enrolled in the present study between January and October 2019. A randomized controlled trial was conducted at the Children's Hospital of Chongqing Medical University, China. Participants were divided into an intervention and a control group. Both groups received regular treatment, and the intervention group received additional sandplay therapy. Four behavioural rating scales were used to evaluate the differences between the two groups. The children's scores on the Child Behavior Checklist (CBCL), Eysenck Personality Questionnaire (EPQ), Self‐Rating Anxiety Scale (SAS) and Self‐Rating Depression Scale (SDS) before and after the intervention were compared using the Mann–Whitney test. The Wilcoxon signed rank test was also employed to compare the median results before and after treatment.
Results
The total scores for CBCL, anxiety and depression, withdrawal, and social behavioural problems for children in the intervention group were all lower than the corresponding scores for those in the control group (p < .05). The EPQ scores for emotional stability and psychosis in the intervention group were both lower than those in the control group (p < .05). The SAS and SDS scores for the caregivers of children in the intervention group were also lower than the corresponding scores for those in the control group (p < .05).
Conclusion
Sandplay therapy can reduce anxiety, withdrawal, and social behavioural problems in school‐age children with chronic diseases, as well as relieve anxiety and depression symptoms in their caregivers. Our study provided evidence for the clinical application of sandplay therapy and highlights the importance of offering and integrating psychological treatment in clinical nursing care.
Keywords: behavioural interventions, child and adolescent, chronic disease, mental health promotion, nursing role, sandplay therapy
1. INTRODUCTION
Children with chronic diseases have complex health conditions. Consequently, they exhibit a higher incidence of emotional–behavioural problems, which is four times greater than that among their physically healthy peers (Hysing et al., 2007). Children are still undergoing cognitive and psychological development and their immature coping strategies in response to adverse external stimuli (chronic pain, poor physical conditions, etc.) make them more prone to chronic diseases (Zeltzer et al., 2008). Though children do not necessarily develop psychological illnesses, they constantly grapple with emotional–behavioural problems (Douma et al., 2018). Delfos and Gempel divided emotional–behavioural problems into two categories: externalizing and internalizing problems. The former includes oppositional defiant disorder, conduct disorder and situational attention deficit disorder, while the latter refers to mood disorder, anxiety disorder and attention deficit disorder (Gimpel & Hollard, 2003; Martine, 2004).
Chronic diseases influence the emotional and behavioural expressions of children in many ways. Changes in normal bodily functions (physical limitations, long‐term pain, etc.), the need to adapt to special diet restrictions and enduring the side effects of treatment or medication bring about negative emotions including worry, distress and anxiety (LeBovidge et al., 2003). Restrictions to participation in different activities, reduced social identity and a lack of normal peer interactions in daily life also result in a negative self‐concept and greater self‐consciousness in children. Such situations can make children feel ashamed about their physical defects, cause psychological behavioural problems (social withdrawal, aggression) (Blackman & Gurka, 2007), detrimentally affect treatment coordination and increase the risk of negative long‐term health outcomes (Kongkaew et al., 2014). Chronic disease is also a stressor to family members, especially caregivers. Families of patients with chronic diseases face a heavier financial burden and more daily organizational problems (Sawin et al., 2003). For instance, isolation, immobilization, frequent hospitalization and restrictions of normal activities, which sometimes persist after the end of treatment, result in emotional disturbance in parents (Lemos et al., 2020; Schepers et al., 2018). In addition to their children's medical regimen, parents also worry about their children's adherence to treatment, long‐term prognosis and current and future levels of independence (Mullins et al., 2007). Therefore, the psychological stresses experienced by parents can be roughly divided into two types: personal and parental. Personal stress refers to psychological stress including depression, anxiety and posttraumatic stress symptoms, while parental stress refers to an indirect emotional strain (frustration or guilt) stemming from the demands of parenthood (Deater‐Deckard et al., 2015; Norberg & Boman, 2008). These stresses can last as long as 5–10 years after the completion of treatment and put parents, children and other caregivers at risk for adverse outcomes (Vrijmoet‐Wiersma et al., 2010).
China has nearly two hundred million children with chronic diseases (Zheng & Zheng, 2015). Leukaemia and chronic kidney disease are two of the most common chronic diseases in China and share characteristics such as recurrent pain and restrictions in daily life activities. Sandplay is a useful adjunct for the mainly cognitive and behavioural techniques commonly used by school guidance counsellors. Several studies have examined the effects of sandplay on children with cerebral palsy (Wang et al., 2015) and on children with separation anxiety (Hamideh & Zohreh, 2015), but there is still insufficient research on the effectiveness of sandplay at reducing emotional–behavioural problems in children with chronic diseases in China. Due to the shortage of paediatric psychologists, filling the gap with nursing practitioners has been proposed (Schwartz et al., 2017). Therefore, integrating emotional and behavioural treatments into traditional nursing care is a priority.
In this study, we used the sandplay theory as a theoretical framework. Sandplay therapy is a psychological therapy method created by Dora Kalff, a Swiss analytical psychologist, in the 1950s. Kalff used Jung's analytical psychology as the foundation for sandplay therapy, borrowed Margaret Lowenfeld's "The world technique," and integrated them with Eastern thoughts and philosophies. In contrast to the prevailing interpretation of psychoanalysis at the time, Lowenfeld pioneered the idea that sandplay was a natural interest for children and correlated play with psychological development in children. Inspired by the concept, Kalff integrated the theory with Jung's analytical psychology. She retained the original methodological system, upgraded the miniature toys provided for the play session and named the new therapy “sandplay” (Chiesa, 2012). Half a century later, a standard sandplay therapy session requires an independent, quiet room with basic equipment including (1) a sandbox: a sandbox with a size of 57 × 72 × 7 centimetres with the bottom painted blue to reflect water or the sea; (2) sand: water should also be provided so that the children have a choice of both wet and dry sand (Chiesa, 2012); (3) miniature objects: the objects should be organized in categories including animals and plants, every‐day and cartoon figures, buildings, military machineries, transportation and miscellaneous (Plotts et al., 2008).
As a form of play therapy, sandplay is an effective intervention for children. The main advantage of sandplay is the unconditional admissive environment created. During sandplay therapy, children can express their emotions freely using sand, water and miniature objects, which promotes nurse–child interactions. Richards et al. (2012) stated that school children can externalize their trauma due to the safe environment created in sandplay therapy, effectively reducing their social withdrawal level. Sandplay therapy requires little language skill and allows children to express themselves or respond nonverbally through sandplay creations. Lu et al. (2010) applied sandplay to school children with autism spectrum disorder. The results suggested that sandplay successfully increased the children's language expression levels, their participation in social activities and their symbolic, voluntary and creative play performance. Furthermore, sandplay therapy can help children construct an idealized world to express their demands and expectations for the future or reconstruct distressing experiences in the past to relieve their emotions. Mariefrance (2007) applied sandplay therapy to immigrant and refugee preschoolers and found that sandplay offered the children a chance to express sentiments derived from a combination of past and present experiences and helped them develop suitable coping strategies.
Sandplay is widely utilized by mental health workers and is especially suitable for paediatric nurses. Regardless of the therapists’ orientation, sandplay therapy provides a special and progressively organized approach that helps children better engage in the therapeutic process (Hamideh & Zohreh, 2015).
With a growing number of children becoming more vulnerable to long‐lasting physical health problems and emotional trauma across their lifetime, it has become more difficult for paediatric nurses to respond (Wise, 2007). Sandplay therapy is an effective technique that enables children to express their emotions, reveal traumas, and develop safe relationships and self‐actualization. However, the efficacy of sandplay therapy in children with chronic diseases remains undetermined. Therefore, in the present study, we set up sandplay treatment rooms in the Nephrology and Hematology wards (each room was equipped with a set of standard sandplay equipment purchased from professional companies) to examine the clinical effectiveness of sandplay therapy in school‐age children with chronic diseases who have emotional and behavioural problems.
2. METHOD
2.1. Design
A two‐armed parallel randomized controlled trial was used to examine the effectiveness of sandplay therapy for children with chronic diseases. The caregivers of the children completed the Child Behavior Checklist (CBCL), the Zung Self‐Rating Depression Scale (SDS), and the Zung Self‐Rating Anxiety Scale (SAS) while the children completed the Eysenck Personality Questionnaire (EPQ) before and after the sandplay therapy (see Diagram 1).
DIAGRAM 1.
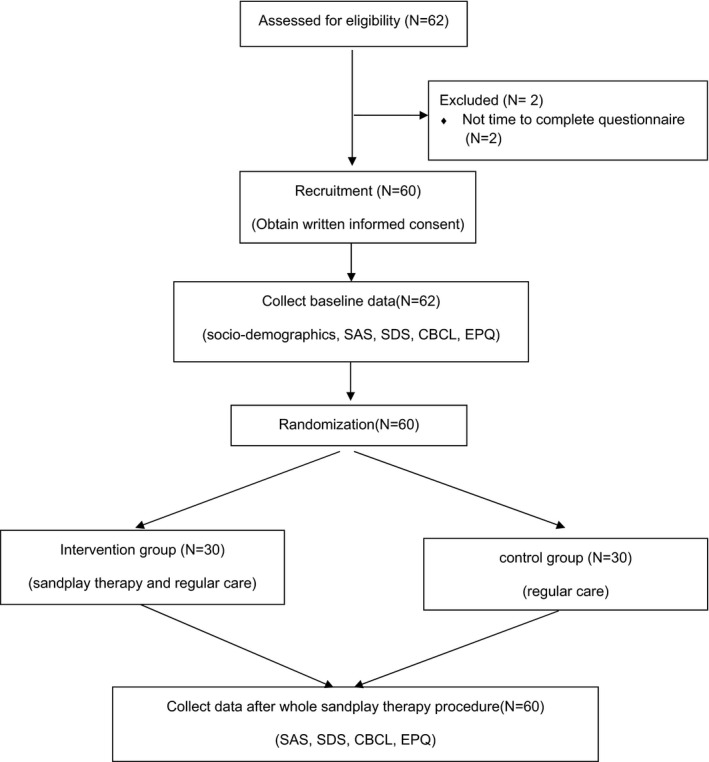
Flow diagram
A two‐armed parallel randomized controlled trial was used to assess the effectiveness of sandplay therapy for children with chronic diseases between January and October 2019. The entire therapeutic procedure consisted of six sessions of sandplay therapy, performed 1–2 times a week for 60–90 min each, and the total treatment lasted about 2 months. Eligible children and their caregivers in both groups were instructed to complete the CBCL, EPQ, SAS, and SDS in a private room after providing consent. All questionnaires were completed before and after the sandplay therapy procedure. The follow‐up diagram is presented in Diagram 2.
DIAGRAM 2.
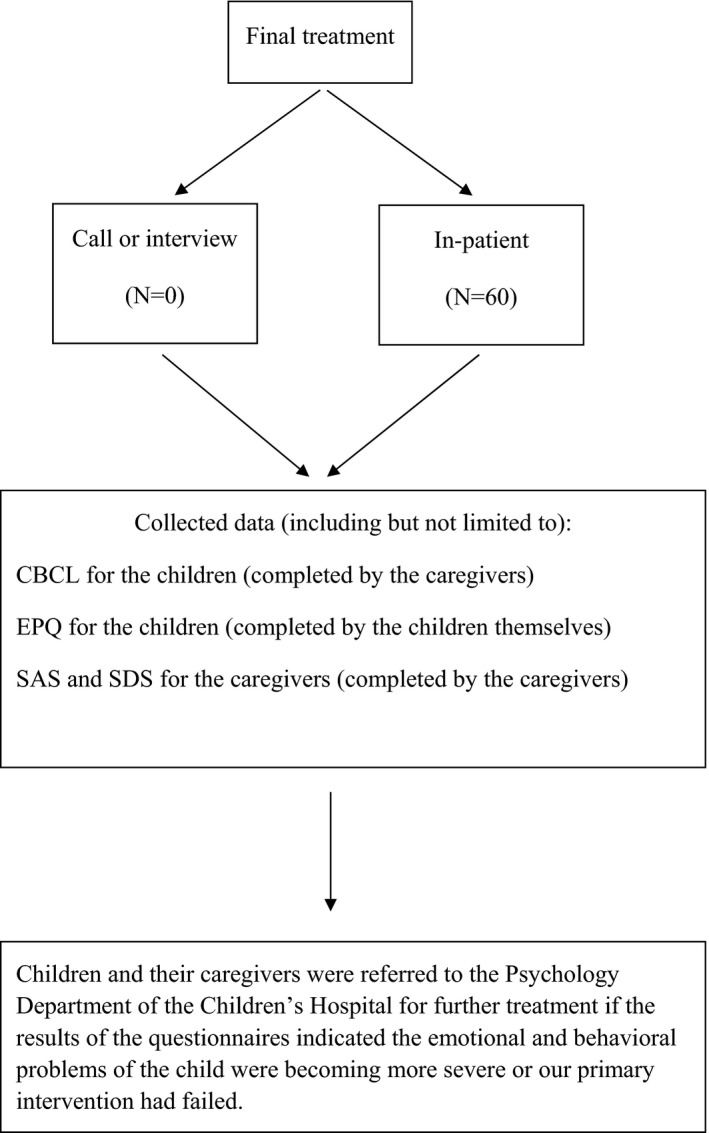
Follow‐up diagram
2.2. Setting
Our research was conducted at the Children's Hospital of Chongqing Medical University, China. The sandplay treatment rooms were set up in the Nephrology and Hematology wards, and we ensured the rooms were relatively independent, quiet, and sufficiently bright. Each room was equipped with a set of standard sandplay equipment purchased from professional companies. The size of the sand table was 57 × 72 × 7 cm. The interior and bottom of the table were both painted blue to simulate the colour of the sky and sea and to encourage the children to relax. Soft sand was added to the table. The miniatures used consisted of animals, flowers, every‐day figures, religious figures, buildings, military machinery, vehicles, etc., totalling more than 2,000 pieces. Potted plants, tables, chairs and sofas were set up in the sandplay treatment rooms to create a safe, relaxing and warm treatment environment.
Sandplay therapists were required to have a Chinese National Grade III Psychological Consultant Certification and to undergo professional sandplay therapy training. After passing the subsequent assessment, the sandplay therapists conducted therapy procedures under the guidance of an experienced psychotherapist with regular supervision.
2.3. Participants
The participants were children receiving long‐term treatment at the Children's Hospital of the Medical University and one of their main caregivers. According to the order of hospital admittance for children with chronic diseases, participants were recruited based on the following inclusion criteria: (1) children aged 6 to 12 with a diagnosis that met the criteria for leukaemia or chronic kidney disease; (2) a total score on the CBCL questionnaire that exceeded the Chinese norm; and (3) children and their caregivers were all Chinese speaking and able to complete the questionnaires. The exclusion criteria were as follows: (1) children and primary caregivers were unable to communicate well with the researchers; (2) the disease condition of the children was in a critical stage; and (3) refusal to participate in the study.
According to previous research (Maoqun et al., 2016), the sample size required to detect a Cohen's d effect size of 0.6 from sandplay therapy in the intervention and control groups was calculated. Twenty‐five cases each were deemed sufficient to observe an effect of at least 80% power at a 5% level of significance, in consideration of an attrition rate of up to 15%. Thirty participants each were therefore enrolled in the intervention and control groups. The enrolled children and their caregivers were informed about the study and its purpose. Those who agreed to participate signed an informed consent form.
2.4. Randomization
After signing the informed consent form, the children eligible to undergo sandplay therapy were numbered by the order of enrolment in the study. The children randomly selected an opaque envelope containing a group identifier (intervention or control) prepared in advance by an independent statistician. The ratio of assignment to the intervention and control groups was 1:1.
2.5. Control group: Regular nursing care
Children in the control group received regular nursing care without sandplay therapy. Regular nursing care consisted of routine disease care and daily expressions of consolation and encouragement by the medical staff.
2.6. Intervention group: Sandplay therapy
The main theme and topic of each sandplay therapy session were set according to the sandplay model suggested by Margaret Lowenfeld (see Table 1), which follows a standard procedure and can be adjusted according to the therapy situation (Hamideh & Zohreh, 2015). To ensure the session was effective, only one child was admitted to the sandplay room at a time. Before the session began, the therapist led the child through a strict hand hygiene procedure and introduced the settings of the sandplay treatment room with a soft and gentle voice. After the child became familiar with the environment, the therapist guided the child to touch the sand and take five deep breaths to relax. The therapist particularly emphasized that the sandplay creation could be anything and that the child would not be judged. While the child engaged in sandplay, the therapist recorded the child's behaviour and the miniatures used. The therapist adopted a "silent witness" approach, accepted, appreciated and accompanied the child, and created a safe, tolerant and supportive atmosphere so that the child could devote themselves wholeheartedly to the process of making sandplay creations. After the treatment session, according to the psychological state of the child, the therapist asked the child to introduce their sandplay creations, communicated with the child, and guided them to appreciate and explore their inner world. After the sandplay therapy session, the therapist took pictures with the child's permission and saved the images as files, then guided the child to repeat the hand hygiene procedure.
TABLE 1.
Margaret Lowenfeld's sandplay therapy model
| Goals: Establishing emotional and friendly relationship with children and building trust in children | First |
| Goals: Simulating the environment of school and home, expressing interest in the two main environment | Second |
| Goals: Trying to reduce children's emotional and behaviour problems | Third |
| Goals: Proposing now pedagogical strategies and trying to playing a role in this process | Forth |
| Goals: Gradual recovery, enthusiasm or calm children's negative emotion or behaviour | Fifth |
| Goals: Disappearance of all symptoms of children's emotional and behaviour problems | Sixth |
2.7. Primary outcome measures
2.7.1. The emotional–behavioural problems
The CBCL for ages 6–18 (CBCL/6–18) is widely used to assess emotional–behavioural problems in children and contains 113 items. The responses are rated with a three‐point scale and parents or caregivers select the most appropriate rating (0 = never, 1 = sometimes, 2 = very often or always) based on their children's behaviours in the preceding 6 months. Higher scores indicate more emotional–behavioural problems. The questionnaire is broadly divided into two categories: introversion factors (depression, social withdrawal and poor communication) and extraversion factors (hyperactivity, aggression and disciplinary behaviour). These categories are more specifically divided into eight aspects: Anxiety/Depression, Somatic complaints, Attention problems, Rule‐breaking behaviour, Aggressive behaviour, Withdrawal, Social problems and Thought problems. The upper limits for the Chinese norm are 40–42 for boys and 37–41 for girls. A CBCL score reductive ratio (rate of difference in scores before and after intervention) ≥25% is regarded as effective. The retesting reliability of the scale was reported to be 0.950, and the Cronbach's report for internal consistency was 0.93 (Zuoji, 2005).
The parental scale was used in this study.
2.7.2. The personality of the children
The EPQ, compiled by Eysenck H.J, a professor of psychology, is one of the most widely used personality questionnaires. In this study, the EPQ (Chinese version) revised by Yaoxian Gong was used. This version of the EPQ contains a total of 88 questions and the possible responses for all questions are "yes" or "no." The EPQ uses the factor analysis method to evaluate four main dimensions of personality: Neuroticism (N), Extraversion (E), Psychoticism (P) and Lie (L). The Chinese version has been confirmed to have adequate internal consistency for the four subscales (0.70–0.88) (Yaoxian, 1986).
2.7.3. Secondary outcome measures
The SDS and SAS are self‐evaluation questionnaires used to assess anxiety and depression. Each contains 20 items and uses a four‐point rating system (1 = none or seldom, 2 = sometimes, 3 = usually, 4 = always or most of the time). The total scores range from 20 to 80 and lower scores indicate a lower severity of anxiety/depression. The standard scores can be stratified into three levels: mild (53–62), moderate (63–72) and extreme (72 or higher). The Cronbach's α values for the Chinese versions of the SAS and SDS are 0.862 and 0.931, respectively, showing good reliability (Liu et al., 1995).
2.7.4. Sociodemographic characteristics
The social and demographic characteristics of the participants, including the sex and current age of the children, educational level of the caregivers and other important descriptors, were collected using a questionnaire created in‐house in accordance with the research target.
2.7.5. Data collection and analysis
Essential disease‐related data (initial diagnosis, disease duration, treatment procedure, etc.) were collected from the medical records of the children. Data were analysed by means of the Statistical Package for the Social Sciences software (version 25.0). Mean ± standard deviation was used to describe the average ages of the children, frequencies were used to present the sociodemographic characteristics, and median (p25, p75) was used for the statistical description of the assessment scores (CBCL, EPQ, SAS and SDS). The average ages of the children in the intervention and control groups were compared using the t test. The CBCL, EPQ, SAS and SDS scores before and after the intervention were compared with the Mann–Whitney test. The Wilcoxon signed rank test was also used to compare the median scores before and after the treatment. The children's gender, diagnosis, and illness duration were compared with the chi‐squared test. A two‐sided test significance level of p < .05 was used in all statistical analyses.
3. RESULTS
3.1. Sociodemographic and clinical characteristics of participants
A total of 62 children and their caregivers were enrolled in the present study between January and October 2019. Two children failed to complete the entire sandplay therapy procedure because they transferred to other hospitals and the rest completed the full procedure. Therefore, the data for a total of 60 children and their caregivers were analysed, with 30 participants in each group. There were 15 boys and 15 girls in the intervention group and 16 boys and 14 girls in the control group. The ages of the children in each group ranged from 6 to 12 years, with mean ages of 9.30 (SD 1.58) and 8.97 (SD 1.33), respectively, and no statistical difference (t = 0.886, p = .380). The sex, type of disease and duration of the illness for the children were not statistically significant either (χ2 = 0.067, p = .796; χ2 = 0.069, p = .793; χ2 = 2.584, p = .108). Other data were comparable and are presented in Tables 2 and 3.
TABLE 2.
The comparison of sociodemographic and clinical characteristics
| Group | Gender | Age | Diagnosis | Duration of diagnosis | CBCL (p25‐p75) | |||
|---|---|---|---|---|---|---|---|---|
| Male | Female | (x ± S) | Chronic kidney disease | Leukaemia | Within one year | One year or over | ||
| Intervention | 15 | 15 | 9.30 ± 1.58 | 12 | 18 | 22 | 8 | 65 (57.25–70) |
| Control | 16 | 14 | 8.97 ± 1.33 | 13 | 17 | 16 | 14 | 59.5 (52.75–65.25) |
| Test statistics | χ2 = 0.067 | t = 0.886 | χ2 = 0.069 | χ2 = 2.584 | Z = 1.415 | |||
| p values | .796 | .380 | .793 | .108 | .140 | |||
Analysis using t test, Mann–Whitney test and chi‐square test.
Abbreviation: CBCL, child behavior checklist.
TABLE 3.
Sociodemographic and clinical characteristics of the control (n = 30) and intervention (n = 30) groups
| Characteristics | Control (n = 30) | Intervention (n = 30) | χ2 | p |
|---|---|---|---|---|
| Sex of the child | ||||
| Female | 14 (46.7%) | 12 (40.0%) | 1.071 | .301 |
| Male | 16 (53.3%) | 18 (60.0%) | — | — |
| Accompanied by | ||||
| Mother only | 29 (96.7%) | 27 (90.0%) | / | .237 |
| Father only | 0 (0.0%) | 3 (10.0%) | — | — |
| Both parents | 0 (0.0%) | 0 (0.0%) | — | — |
| Other relatives | 1 (3.3%) | 0 (0.0%) | — | — |
| Highest education attainment of the accompanied family | ||||
| Primary or below | 20 (66.7%) | 19 (63.3%) | 0.517 | .772 |
| Secondary | 6 (20.0%) | 5 (16.7%) | — | — |
| College or above | 4 (13.3%) | 6 (20.0%) | — | — |
| Disease of the child | ||||
| Leukaemia | 18 (60.0%) | 13 (43.3%) | 1.669 | .196 |
| Chronic kidney disease | 12 (40.0%) | 17 (56.7%) | — | — |
| First diagnose | ||||
| Yes | 14 (46.7%) | 11 (36.7%) | 0.617 | .432 |
| No | 16 (53.3%) | 19 (63.3%) | — | — |
| Duration of illness | ||||
| Within one year | 16 (53.3%) | 22 (73.3%) | 2.584 | .108 |
| One year or over | 14 (46.7%) | 8 (26.7%) | — | — |
3.2. Changes in CBCL scores
The effective rate was 53% according to the CBCL score reductive ratio. No significant differences in the total and subscales scores were noted between the control and intervention groups before the intervention. In contrast, significant differences between the scores before and after the sandplay therapy in the control and intervention groups were found in the total scores (z = 6.320, p = .00), anxiety (z = 6.016, p = .00), attention problems (z = 3.571, p = .00), aggressive behavior (z = 6.138, p = .00), withdrawal (z = 4.680, p = .00) and social problems (z = 4.594, p = .00). The control group showed no significant difference in the total and subscales scores after treatment. However, there were statistically significant difference in the total scores (z = 4.784, p = .00), anxiety (z = 4.633, p = .00), attention problems (z = 3.830, p = .00), aggressive behaviour (z = 4.797, p = .00), withdrawal (z = 4.638, p = .00) and social problems (z = 4.555, p = .00) in the intervention group (see Table 4).
TABLE 4.
CBCL scores of control and intervention group
| Group | Time | Total score, Median (IQR) | Anxious, Median (IQR) | Somatic complains, Median (IQR) | Attention problems, Median (IQR) | Rule‐breaking behaviour, Median (IQR) | Aggressive behaviour, Median (IQR) | Withdrawn, Median (IQR) | Social problems, Median (IQR) | Thought problems, Median (IQR) |
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Before | 65 (57.25–70) | 10.5 (7–14) | 6 (2.75–8) | 8 (5.75–8) | 2 (1–6.25) | 14.5 (8.75–17.25) | 6 (4–10) | 5 (4–8) | 4 (1–13) |
| After | 47 (39.75–57.5) | 5 (3–7) | 5 (3–6.25) | 6 (4–8.25) | 2 (1–6) | 6 (4–9) | 3 (1–4) | 3.5 (1–5) | 3.5 (1–11) | |
| Changes before and after | −17 (−23, −10) | −6 (−8, −4) | 0 (−2, 0) | −1 (−2, 0) | 0 (−1, 0) | −8 (−9, −5) | −3 (−5, −2) | −3 (−4, −1) | 0 (0, 0) | |
| Z | −4.784 | −4.633 | −3.048 | −3.830 | −2.629 | −4.797 | −4.638 | −4.555 | −1.890 | |
| p | <.001 | <.001 | .002 | <.001 | .009 | <.001 | <.001 | <.001 | ||
| Control | Before | 59.5 (52.75–65.25) | 9 (6.75–13) | 3.5 (1–8) | 8 (5–9) | 5 (1–8) | 10 (4.75–15.25) | 7.5 (6–10) | 6 (3–7) | 8 (3.75–12) |
| After | 58.50 (54.5–63.5) | 9 (7–13) | 3.5 (1.62.5) | 7.5 (5–9) | 5 (1–7) | 9 (5–14.25) | 7 (5–10) | 6 (2.75–7.25) | 7.5 (3–11.25) | |
| Changes before and after | −1 (−3, 2) | 0 (0, 1) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (−1, 0) | 0 (−1, 2) | 0 (−2, 1) | 0 (0, 0) | |
| Z | −0.847 | −0.476 | −1.983 | −2.07 | −1.912 | −2.564 | 0 | −0.99 | −1.732 | |
| p | .397 | .634 | .047 | .038 | .056 | .010 | 1.000 | .322 | .083 | |
| Z (two groups before intervention) | 1.761 | 1.002 | 1.713 | 0.469 | 1.268 | 1.895 | 1.121 | 0.469 | 0.840 | |
| p | .078 | .317 | .087 | .639 | .205 | .058 | .262 | .639 | .401 | |
| Z (two groups after intervention) | 3.670 | 4.639 | 1.293 | 0.953 | 1.597 | 1.935 | 4.863 | 2.958 | 0.884 | |
| p | .000** | .000** | .196 | .341 | .110 | .053 | .000** | .003** | .377 | |
| Z (two groups changes before and after) | −6.320 | −6.016 | −1.714 | −3.571 | −1.122 | −6.138 | −4.680 | −4.594 | −0.438 | |
| p | <.001 | <.001 | .087 | <.001 | .262 | <.001 | <.001 | <.001 | .661 | |
Analysis using Mann–Whitney test and Wilcoxon signed rank test.
Abbreviations: CBCL, child behavior checklist; IQR, interquartile range (25th centile–75th centile).
**:P < 0.05
[Correction added on 5 October 2021 after first online publication: all z value in the preceding paragraph have been updated in this version]
3.3. Changes in EPQ scores
The distribution of changes in personality showed in the N scales and P scales (see Table 5). There were significant differences in the N (z = 3.952, p = .000) and P (z = 3.829, p = .000) scales in the intervention group as well as between the control and intervention groups before and after the sandplay therapy (z = 3.790, p = .000; z = 2.275, p = .000). In the E scale, there was a statistical difference between the two groups before and after sandplay therapy (z = 2.391, p = .017; z = 2.189, p = .029) (see Table 6). The total distribution of changes in personality.
TABLE 5.
The distribution of changes in personality
| Before (N = 60) | After (N = 60) | |||
|---|---|---|---|---|
| 0–43.3 | 43.4– | Total | ||
| N | 0–43.3 | 8 (13.33%) | 11 (18.33%) | 19 (31.67%) |
| 43.4– | 27 (45.00%) | 14 (23.33%) | 41 (68.33%) | |
| Total | 35 (58.33%) | 25 (41.66%) | 60 (100.00%) | |
| p | .009 | |||
| P (psychoticism) | 0–43.3 | 43.4– | Total | |
| 0–43.3 | 6 (10.00%) | 1 (1.67%) | 7 (11.67%) | |
| 43.4– | 7 (11.67%) | 46 (76.67) | 53 (88.33%) | |
| Total | 13 (21.67%) | 47 (78.34%) | 60 (100.00%) | |
| p | .039 |
Analysis using McNemar test.
TABLE 6.
EPQ scores of control and intervention group [Correction added on 5 October 2021 after first online publication: Group name ‘Control’ and ‘Intervention’ were interchanged and have been corrected in this version]
| Group | Time | EPQ‐E, Median (IQR) | EPQ‐N, Median (IQR) | EPQ‐P, Median (IQR) | EPQ‐L, Median (IQR) |
|---|---|---|---|---|---|
| Intervention | Before | 40 (35–45) | 50 (40–55) | 55 (55–60) | 55 (50–60) |
| After | 40 (35–45) | 35 (35–40) | 45 (40–50) | 55 (45–55) | |
| Changes before and after | 0 (−5, 5) | −15 (−20, −5) | −5 (−15, −5) | −5 (−10, 5) | |
| Z | 0 | −3.952 | −3.829 | −0.989 | |
| p | 1.000 | <.001 | <.001 | .322 | |
| Control | Before | 50 (50–60) | 50 (40–61.25) | 55 (45–60) | 55 (43.75–60) |
| After | 45 (40–60) | 50 (40–61.25) | 55 (45–60) | 55 (50–60) | |
| Changes before and after | −5 (−10, 10) | 0 (−15, 15) | 0 (0, 0) | 0 (−5, 5) | |
| Z | −0.425 | −0.145 | −1.732 | −1.016 | |
| p | .671 | .885 | .083 | .310 | |
| Z (two groups before intervention) | 2.391 | 0.405 | 0.749 | 0.479 | |
| p | .017* | .686 | .454 | .632 | |
| Z (two groups after intervention) | 2.189 | 3.790 | 3.620 | 1.504 | |
| p | .029* | .000** | .000** | .133 | |
| Z (two groups changes before and after) | −0.439 | −2.275 | −4.491 | −1.507 | |
| p | .661 | .023 | <.001 | .132 | |
Analysis using Mann–Whitney test and Wilcoxon signed rank test.
Abbreviations: E, extraversion; EPQ, Eysenck personality questionnaire; IQR, interquartile range (25th centile–75th centile); L, lie; N, neuroticism; P, psychoticism.
**:P < 0.05
[Correction added on 5 October 2021 after first online publication: all z value in the preceding paragraph have been updated in this version]
3.4. SAS and SDS scores of the caregivers of children with chronic disease
The SAS and SDS scores of the caregivers of children in the intervention group showed statistically significant differences before and after the sandplay therapy (z = 4.270, p = .001; z = 4.680, p = .000). The comparison of the two groups after the intervention was also statistically significant (z = 2.847, p = .004; z = 3.580, p = .000) (see Table 7).
TABLE 7.
The SAS and SDS scores of the caregivers before and after the sandplay therapy
| Group | Time | SAS, Median (IQR) | SDS, Median (IQR) |
|---|---|---|---|
| Intervention | Before | 55.00 (49.00–65.13) | 64.25 (58.38–71.25) |
| After | 50.63 (43.69–54.25) | 51.00 (48.00–61.81) | |
| Changes before and after | −6.5 (−9.75, −2.75) | −9.13 (−11.75, −6) | |
| Z | −4.207 | −4.680 | |
| p | <.001 | <.001 | |
| Control | Before | 57.88 (48.75–67.25) | 63.38 (54.75–68.63) |
| After | 56.88 (49.81–64.94) | 61.25 (55.75–64.63) | |
| Changes before and after | −2.13 (−3.25, 2) | −1.63 (−4.5, 2.75) | |
| Z | −1.801 | −1.111 | |
| p | .072 | .267 | |
| Z (two groups before intervention) | 0.910 | 0.710 | |
| p | .363 | .478 | |
| Z (two groups after intervention) | 2.847 | 3.580 | |
| p | .004** | .000** | |
| Z (two groups changes before and after) | −3.543 | −5.109 | |
| p | <.001 | <.001 | |
Analysis using Mann–Whitney test and Wilcoxon signed rank test.
Abbreviations: IQR, interquartile range (25th centile–75th centile); SAS, self‐rating anxiety scale; SD, standard deviation; SDS, self‐rating depression scale.
**:P < 0.05
[Correction added on 5 October 2021 after first online publication: value for z and p in the preceding paragraph have been updated to correspond with Table 7]
4. DISCUSSION
A previous study examined the effects of sandplay therapy on children with emotional–behavioural problems (Richards et al., 2012). Our study aimed to expand the scope of application for this form of therapy. Overall, children with chronic diseases who received sandplay therapy exhibited significantly fewer emotional–behavioural problems than those who did not.
Limited mobility, chronic pain and special restrictions (food, clothing, housing and transportation) all affect children with chronic diseases to varying degrees. Previous studies have shown that these children had 1.5 times more behavioural problems than normal children, including antisocial behavioural, hyperactivity and social withdrawal/peer conflict (Blackwell et al., 2019; Wise, 2007). Li et al. (2008) investigated emotional problems in 203 children aged 8 to 16 with chronic diseases and found that 43.8% had anxiety, 30.0% had depression, and 26.1% had both anxiety and depression. However, methods to reduce emotional–behavioural problems in children with chronic diseases in China have received insufficient attention.
4.1. Effects of sandplay therapy on emotional–behaviour problems
The positive results in the present study support the effectiveness of sandplay therapy as the scores for anxiety, withdrawal and social problems in the intervention group were lower after sandplay therapy. Analysis of children's actions during sandplay revealed that the sandplay process can be roughly divided into two stages: the first stage consisted of trauma presentation and conflict intensification, while the second stage consisted of transformation and healing. As the intervention progressed, the traumatic elements gradually decreased and the themes of healing and hope became more apparent.
At the beginning of sandplay, the children often exhibited obvious resistance, impulsiveness and restlessness because they had a limited understanding of the procedure. The safe and empathic environment created by the therapist helped reduce the children's resistance to the medical staff, loosen their self‐restraint and encourage them to gradually express their inner world. Through guidance, the children began to express their traumatic experiences and negative emotions by selecting miniatures, creating a sand world and symbolic narrations. As the sandplay progressed, the children manifested internal conflict and questioning of their abilities by destroying and rebuilding the scene, destroying old creations and recreating them. A possible explanation for this behaviour is that through the three‐dimensional environment for expression provided by sand in the visual and kinesthetic channels (including movement and touch), the children could gradually release themselves from a state of avoidance and resistance, transforming from the role of a victim in previous experiences to the creator of new experiences and gaining more initiative. During this stage, the therapist employed positive transference therapy to reduce inappropriate emotional regulation methods (aggression or self‐injury) as well as promote and consolidate positive behaviours to help the children enter the next transformation stage.
In the second stage, as the duration of the disease increased, low social desire and negative emotions caused by limited activities and pain from the disease gradually emerged (Harding et al., 2002). Anxiety and depression cause withdrawal and avoidance during medical treatment. Traumatic themes in the sandplay creations decreased and a hesitation in self‐cognition became apparent as well as the desire for school activities, family and a normal social life. Treatment at this stage was focussed on active communication and interactions between the therapist and child. The therapist adopted an inclusive attitude and provided affirmations to help the child increase their emotional stability, strengthen their self‐identity, balance the nurse–child interpersonal relationship and establish an appropriate level of self‐awareness.
4.2. Effects of sandplay therapy on children's personality
School age is an important period for personality formation and psychological development in children. This period is also an important stage for children to develop their self‐identity and a healthy personality (Lizhu, 2015). Though personality is comprised of a combination of psychological characteristics with certain tendencies and is relatively stable, it is influenced by heredity, age and environment (Berg et al., 2016). As a serious negative stimulus, chronic diseases strongly influence the formation and improvement of children's personalities.
Consistent with previous studies (Hovens et al., 2016; Jinxiang et al., 2018), the children's scores for emotional stability (N scale) and psychosis (P scale) in the Eysenck personality assessment significantly decreased after the intervention. A likely explanation is that by providing a safe, relaxed and unlimited protective environment, sandplay therapy can alleviate children's negative emotions, enabling them to adjust their emotions and reduce the frequency of strong reactions when faced with a serious stimulation (pain, activity limitation). In addition, the unconditional attention and positive feedback the children receive from the therapist and parents during sandplay therapy can increase prosocial behaviours, reduce their resistance to the external environment and benefit the process of socialization. Consequently, the children's mental quality scores decreased.
4.3. Effects of sandplay therapy on caregiver's emotional problems
The results of the present study showed that the anxiety and depression scores of the caregivers decreased after sandplay therapy. When parents are faced with long‐term negative stimuli due to chronic diseases, they experience multiple stressors such as medical procedures, instability of family roles and lack of social support, often resulting in emotional overreactions, such as irritability, anxiety and depression (Cousino & Hazen, 2013; Haverman et al., 2013). These negative emotions not only affect the mental health of the parents, but also affect their social interactions, marital relationships, careers and other aspects of their lives. These situations usually trigger polarized responses such as overprotection or over‐neglect due to difficulties balancing the two extremes. Overprotective parents may lead to low levels of dependence and self‐efficacy in the children, while over‐neglect may lead to low self‐esteem and self‐denial.
In the present study, two sessions of family sandplay therapy were conducted after individual therapy, which promoted the connection between the medical staff and the family and alleviated negative emotions in the caregivers. According to our clinical observations, family sandplay strengthened the communication between the caregivers and their children, which is conducive to improving family interactions and helping caregivers discover their children's potential abilities. It also helps the children feel more positive about the support and care they receive from their family, find an outlet to vent emotions, balance their inner world, and foster trust between the family and medical staff.
5. LIMITATIONS
One of the limitations of the current study was that children and their caregivers were recruited from one hospital; hence, the generalizability of the results may be limited. Additionally, the lack of blinding may be a primary source of bias. However, due to the nature of sandplay therapy, it is difficult to blind the children, caregivers and therapists. Despite knowing they are undergoing an intervention, children are unlikely to change their behaviours (Silva et al., 2017). To minimize the potential bias, we chose a series of objective questionnaires to evaluate the effectiveness of the sandplay therapy on children with emotional–behavioural problems, and the assessors who collected the data (the scores for questionnaires, children's clinical data and sociodemographic) were blinded. Finally, other undetected factors may be responsible for the results such as the functioning of the family, the rearing style of the parents or the coping strategy of the children. Further studies should take these factors into account and include the family's condition.
6. CONCLUSION
Paediatric nurses, as evaluators of children's problems, implementers of nursing measures, collaborators with other professionals and educators of children and their families, are indispensable in influencing the mental health of children with chronic diseases. In 2010, the International Council of Nurses (ICN) proposed the theme "nurses dominate chronic disease management" to highlight the leading role of nurses in chronic disease management. The impact of chronic diseases in children usually manifests in their behaviours and emotions; thus, it is important to help children reduce these negative influences.
Sandplay therapy is a universal psychological method that is suitable for adoption in medical settings, as supported by our findings. China has the largest population of children with chronic diseases. Though many studies have highlighted the importance of offering and integrating psychological help into standard clinical nursing care, the topic has not received enough attention. Our findings provide positive empirical evidence that sandplay therapy can effectively reduce anxiety, withdrawal and social problems in children with chronic diseases as well as anxiety and depression in their caregivers. Furthermore, our findings will contribute to the development of a comprehensive and quality paediatric care system, improving patient satisfaction, increasing the trust of children and their families in the medical staff and society, improving nurse–child interactions and expanding the scope of the nursing profession in China.
CONFLICTS OF INTERESTS
None declared.
ETHICAL STATEMENTS
This study was approved by the Institutional Review Board of Children's Hospital of Chongqing medical University, China. File No.: 2018‐116.
PATIENT CONSENT
Parental/guardian consent obtained.
ACKNOWLEDGEMENTS
None.
Tan, J. , Yin, H. , Meng, T. , & Guo, X. (2021). Effects of sandplay therapy in reducing emotional and behavioural problems in school‐age children with chronic diseases: A randomized controlled trial. Nursing Open, 8, 3099–3110. 10.1002/nop2.1022
Funding information
The authors disclosed receipt of the following financial support for the research, authorship and publication of this article: this work was supported by the Demonstration of Technology Innovation and Application of Chongqing Science and Technology Commission (general project of social livelihood), China. Project No.: cstc2018jscx‐msybx0065
[Correction added on 8 September 2021 after first online publication: some values inside the text and group names in table 6 have been updated in this version]
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author, Huaying Yin. The data are not publicly available due to their containing information that could compromise the privacy of research participants.
REFERENCES
- Berg, V. , Lummaa, V. , Rickard, I. J. , Silventoinen, K. , Kaprio, J. , & Jokela, M. (2016). Genetic associations between personality traits and lifetime reproductive success in humans. Behavior Genetics, 46(6), 742–753. 10.1007/s10519-016-9803-5 [DOI] [PubMed] [Google Scholar]
- Blackman, J. A. , & Gurka, M. J. (2007). Developmental and behavioral comorbidities of asthma in children. Journal of Developmental and Behavioral Pediatrics, 28(2), 92–99. 10.1097/01.DBP.0000267557.80834.e5 [DOI] [PubMed] [Google Scholar]
- Blackwell, C. K. , Elliott, A. J. , Ganiban, J. , Herbstman, J. , Hunt, K. , Forrest, C. B. , Camargo, C. A. Jr , & Program Collaborators for Environmental influences on Child Health Outcomes . (2019). General health and life satisfaction in children with chronic illness. Pediatrics, 143(6), e20182988. 10.1542/peds.2018-2988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiesa, C. (2012). Scripts in the sand: Sandplay in transactional analysis psychotherapy with children. Transactional Analysis Journal, 42(4), 285–293. 10.1177/036215371204200407 [DOI] [Google Scholar]
- Cousino, M. K. , & Hazen, R. A. (2013). Parenting stress among caregivers of children with chronic illness: A systematic review. Journal of Pediatric Psychology, 38(8), 809–828. 10.1093/jpepsy/jst049 [DOI] [PubMed] [Google Scholar]
- Deater‐Deckard, K. , Chen, N. , & El Mallah, S. (2015). Parenting stress. Oxford Bibliographies Online, booklist. [Google Scholar]
- Douma, M. , Scholten, L. , Maurice‐Stam, H. , & Grootenhuis, M. A. (2018). Online cognitive‐behavioral based group interventions for adolescents with chronic illness and parents: Study protocol of two multicenter randomized controlled trials. BMC Pediatrics, 18(1), 235. 10.1186/s12887-018-1216-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gimpel, G. A. , & Hollard, M. L. (2003). Emotional and behavioural problems of young children. Guilford Press. [Google Scholar]
- Hamideh, M. N. , & Zohreh, M. A. (2015). The Effectiveness of sandplay therapy in reducing symptoms of separation anxiety in children 5 to 7 years old. Journal of Educational Sciences and Psychology, 1(5), 47–53. [Google Scholar]
- Harding, T. A. , Compas, B. E. , Colletti, R. B. , Catherine, S. , Boyer, M. C. , & Konik, B. S. (2002). Parent reports of coping and stress responses in children with recurrent abdominal pain. Journal of Pediatric Psychology, 27(3), 215–226. 10.1093/jpepsy/27.3.215 [DOI] [PubMed] [Google Scholar]
- Haverman, L. , van Oers, H. A. , Limperg, P. F. , Houtzager, B. A. , Huisman, J. , Darlington, A.‐S. , Maurice‐Stam, H. , & Grootenhuis, M. A. (2013). Development and validation of the distress thermometer for parents of a chronically ill child. Journal of Pediatrics, 163(4), 1140–1146.e2. 10.1016/j.jpeds.2013.06.011 [DOI] [PubMed] [Google Scholar]
- Hovens, J. G. , Giltay, E. J. , van Hemert, A. M. , & Penninx, B. W. (2016). Childhood maltreatment and the course of depressive and anxiety disorders: The contribution of personality characteristics. Depress and Anxiety, 33(1), 27–34. 10.1002/da.22429 [DOI] [PubMed] [Google Scholar]
- Hysing, M. , Elgen, I. , Gillberg, C. , Lie, S. A. , & Lundervold, A. J. (2007). Chronic physical illness and mental health in children. Results from a large‐scale population study. Journal of Child Psychology and Psychiatry, 48(8), 785–792. 10.1111/j.1469-7610.2007.01755.x [DOI] [PubMed] [Google Scholar]
- Jinxiang, T. , Xiao, H. , & Yadong, P. (2018). Correlation study on personality characteristics and mental health of children and adolescents. Sichuan Mental Health, 31(3), 263–267. [Google Scholar]
- Kongkaew, C. , Jampachaisri, K. , Chaturongkul, C. A. , & Scholfield, C. N. (2014). Depression and adherence to treatment in diabetic children and adolescents: A systematic review and meta‐analysis of observational studies. European Journal of Pediatrics, 173(2), 203–212. 10.1007/s00431-013-2128-y [DOI] [PubMed] [Google Scholar]
- Lacroix, L. , Rousseau, C. , Gauthier, M.‐F. , Singh, A. , Giguère, N. , & Lemzoudi, Y. (2007). Immigrant and refugee preschoolers’ sandplay representations of the tsunami. The Arts in Psychotherapy, 34(2), 99–113. 10.1016/j.aip.2006.09.006 [DOI] [Google Scholar]
- LeBovidge, J. S. , Lavigne, J. V. , Donenberg, G. R. , & Miller, M. L. (2003). Psychological adjustment of children and adolescents with chronic arthritis: A meta‐analytic review. Journal of Pediatric Psychology, 28(1), 29–39. 10.1093/jpepsy/28.1.29 [DOI] [PubMed] [Google Scholar]
- Lemos, M. S. , Lima, L. , Silva, C. , & Fontoura, S. (2020). Disease‐related parenting stress in the post‐treatment phase of pediatric cancer. Comprehensive Child and Adolescent Nursing, 43(1), 65–79. 10.1080/24694193.2019.1570393 [DOI] [PubMed] [Google Scholar]
- Li, Y. , Wei, M. , & Page, G. , et al. (2008). Stressors, coping strategies and psychosocial state of children with chronic illness. Chin J Contemp Pediatr, 10(3), 337–342. https://doi.org/CNKI:SUN:DDKZ.0.2008‐03‐022 [PubMed] [Google Scholar]
- Liu, X. , Tang, M. , & Chen, K. (1995). The comparison between SDS and CES‐D in evaluating depressive symptoms in university students. Chinese Mental Health Journal, 1(9), 19–20. [Google Scholar]
- Lizhu, Y. (2015). Thirty years of research on personality development and cultivation of Chinese children and adolescents. Psychological Development and Education, 1, 9–14. [Google Scholar]
- Lu, L. , Petersen, F. , Lacroix, L. , & Rousseau, C. (2010). Stimulating creative play in children with autism through sandplay. The Arts in Psychotherapy, 37(1), 56–64. 10.1016/j.aip.2009.09.003 [DOI] [Google Scholar]
- Maoqun, R. , Wenyu, Y. , & Nong, X. (2016). The effectiveness of stage‐based one‐to‐one sandplay therapy in children with tourette′s syndrome. Journal of Nursing Science, 31(19), 11–20. 10.3870/j.issn.1001-4152.2016.19.011 [DOI] [Google Scholar]
- Martine, F. D. (2004). Children and behavioural problems. Jessica Kingsley. [Google Scholar]
- Mullins, L. L. , Wolfe‐Christensen, C. , Pai, A. L. , Carpentier, M. Y. , Gillaspy, S. , Cheek, J. , & Page, M. (2007). The relationship of parental overprotection, perceived child vulnerability, and parenting stress to uncertainty in youth with chronic illness. Journal of Pediatric Psychology, 32(8), 973–982. 10.1093/jpepsy/jsm044 [DOI] [PubMed] [Google Scholar]
- Norberg, A. L. , & Boman, K. K. (2008). Parent distress in childhood cancer: A comparative evaluation of posttraumatic stress symptoms, depression and anxiety. Acta Oncologica, 47(2), 267–274. 10.1080/02841860701558773 [DOI] [PubMed] [Google Scholar]
- Plotts, C. , Lasser, J. , & Prater, S. (2008). Exploring sandplay therapy: Application to individuals with traumatic brain injury. International Journal of Play Therapy, 17(2), 138–153. 10.1037/1555-6824.17.2.138 [DOI] [Google Scholar]
- Richards, S. D. , Pillay, J. , & Fritz, E. (2012). The use of sand tray techniques by school counsellors to assist children with emotional and behavioural problems. The Arts in Psychotherapy, 39(5), 367–373. 10.1016/j.aip.2012.06.006 [DOI] [Google Scholar]
- Sawin, K. J. , Bellin, M. H. , Roux, G. , Buran, C. , Brei, T. J. , & Fastenau, P. S. (2003). The experience of parenting an adolescent with spina bifida. Rehabilitation Nursing, 28(6), 173–185. 10.1002/j.2048-7940.2003.tb02057.x [DOI] [PubMed] [Google Scholar]
- Schepers, S. A. , Sint Nicolaas, S. M. , Maurice‐Stam, H. , Haverman, L. , Verhaak, C. M. , & Grootenhuis, M. A. (2018). Parental distress 6 months after a pediatric cancer diagnosis in relation to family psychosocial risk at diagnosis. Cancer, 124(2), 381–390. 10.1002/cncr.31023 [DOI] [PubMed] [Google Scholar]
- Schwartz, R. H. , O'Laughlen, M. C. , & Kim, J. (2017). Survey to child/adolescent psychiatry and developmental/behavioral pediatric training directors to expand psychiatric‐mental health training to nurse practitioners. Journal of the American Association of Nurse Practitioners, 29(6), 348–355. 10.1002/2327-6924.12450 [DOI] [PubMed] [Google Scholar]
- Silva, R. D. , Austregesilo, S. C. , Ithamar, L. , & Lima, L. S. (2017). Therapeutic play to prepare children for invasive procedures: A systematic review. Jornal De Pediatria, 93(1), 6–16. 10.1016/j.jped.2016.06.005 [DOI] [PubMed] [Google Scholar]
- Vrijmoet‐Wiersma, C. M. , Egeler, R. M. , Koopman, H. M. , Bresters, D. , Norberg, A. L. , & Grootenhuis, M. A. (2010). Parental stress and perceived vulnerability at 5 and 10 years after pediatric SCT. Bone Marrow Transplantation, 45(6), 1102–1108. 10.1038/bmt.2009.309 [DOI] [PubMed] [Google Scholar]
- Wang, M. , Petrini, M. A. , & Guan, Q. (2015). Evaluation of family‐centred services from parents of Chinese children with cerebral palsy with the Measure of Processes of Care. Child: care, health and development, 41(3), 408–415. 10.1111/cch.12183 [DOI] [PubMed] [Google Scholar]
- Wise, P. H. (2007). The future pediatrician: The challenge of chronic illness. Journal of Pediatrics, 151(5 Suppl), S6–S10. 10.1016/j.jpeds.2007.08.013 [DOI] [PubMed] [Google Scholar]
- Yaoxian, G. (1986). Revised Eysenck personality questionnaire manual. Hunan Medical College Press. [Google Scholar]
- Zeltzer, L. K. , Lu, Q. , Leisenring, W. , Tsao, J. C. I. , Recklitis, C. , Armstrong, G. , Mertens, A. C. , Robison, L. L. , & Ness, K. K. (2008). Psychosocial outcomes and health‐related quality of life in adult childhood cancer survivors: A report from the childhood cancer survivor study. Cancer Epidemiology, Biomarkers & Prevention, 17(2), 435–446. 10.1158/1055-9965.Epi-07-2541 [DOI] [PubMed] [Google Scholar]
- Zheng, Y. , & Zheng, X. (2015). Current state and recent developments of child psychiatry in China. Child and Adolescent Psychiatry and Mental Health, 9, 10. 10.1186/s13034-015-0040-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuoji, Z. (2005). Manual of behavioral medicine scale. China Medical Electronic Audiovisual Press. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author, Huaying Yin. The data are not publicly available due to their containing information that could compromise the privacy of research participants.


