Abstract
Aim
To explore whether self‐efficacy has any positive or negative mediating effects between family functioning and quality of life among elders with chronic diseases.
Design
A cross‐sectional study.
Methods
Questionnaires were collected from 516 community‐dwelling elderly individuals with chronic diseases using a convenience sampling method. The questionnaires included the Self‐efficacy for Managing Chronic Disease Six‐Item Scale, the Family Adaptation Partnership Growth Affection Resolve Index and the MOS 36‐Item Short Form Health Survey.
Results
Family functioning and self‐efficacy impacted the quality of life of community‐dwelling elderly individuals with chronic diseases. Family functioning was mediated by self‐efficacy and had an indirect impact on quality of life. The mediating effect accounted for 62.50% of the total effect.
Keywords: chronic diseases, elders, family functioning, quality of life, self‐efficacy
1. INTRODUCTION
With the ageing of the global population, the number of community‐dwelling elderly individuals with chronic diseases is increasing (Sun et al., 2019; Zhou et al., 2016). It was reported that the four most common non‐communicable chronic diseases (NCDs) among elderly individuals were cancer, diabetes, cardiovascular disorders and lung disease. The four major NCDs and a handful of other chronic conditions were responsible for two‐thirds of mortality globally in 2016 (Nugent, 2019). In China, the Study of Global AGEing and Adult Health (SAGE)‐China Wave 1 cross‐sectional study reported that half of the elderly individuals in China had at least one chronic illness (Zhao et al., 2018). In 2015, the China Family Development Report (2015) released by the National Health and Family Planning Commission showed that half of all elderly people were living without children (Croll et al., 2019), and the proportion was higher in rural areas than in urban areas; additionally, their family functioning was poor. Because of the characteristics of chronic diseases in the elderly population, such as long disease duration, difficult self‐healing, complex aetiology, many complications, and high cost of treatment, coupled with retirement syndrome and other family and social factors, physical and psychological diseases are common in the elderly population and seriously affect patients's quality of life (Botes et al., 2018; Maresova et al., 2019). Additionally, chronic diseases place a heavy burden on the family and society, attracting the focus of medical services (Nurchayati et al., 2019; Wu et al., 2019).
Bandura defined self‐efficacy as the conviction that one can successfully execute the behaviour required to produce an outcome (Bandura, 1977). In other words, self‐efficacy is the perceived confidence that a person has the ability to accomplish something. Self‐efficacy is thought to be an important factor in initiating and maintaining physical activity and is therefore believed to improve quality of life through its effects on both positive affect and negative affect (Hager et al., 2019; Lee et al., 2016; Yeung & Lu, 2014). Previous studies have verified that self‐efficacy has certain influences on the quality of life of patients with chronic diseases (Du et al., 2018; Selzler et al., 2020; Zhang, Gilmour, et al., 2020; Zhang, Xue, et al., 2020). Lee's study demonstrated that self‐efficacy, anxiety and depression play major roles in determining the perception of quality of life in cancer patients (Lee et al., 2016). Omran's research showed that health‐related quality of life in patients with type 2 diabetes is related to self‐efficacy, self‐care activities and health literacy (Omran & McMillan, 2018).
Family is the core of society and provides not only material support but also spiritual and emotional support. Family functioning, in which the family is regarded as a system, refers to interactions with family members that involve physical, emotional, and psychological activities and affects many aspects of family life (Wang et al., 2015; Wei et al., 2020). Family functioning plays a crucial role in the growth of individuals, and if the family does not operate in such a way that it performs its basic functions, family members will have a variety of problems (Zhang, Gilmour, et al., 2020; Zhang, Xue, et al., 2020). In recent years, nursing professionals have expanded the focus of their attention from the patient alone to the patient and the family (Fjortoft et al., 2020). Good family support has a major impact on the patients' recovery from disease and on the improvement of self‐efficacy and quality of life (Konradsen et al., 2018). Previous studies have shown that family functioning can improve self‐efficacy (Puspasari et al., 2018; Wu & Sheng, 2019). Additionally, previous studies have demonstrated that family functioning has certain influences on the quality of life of patients with chronic diseases (Andrade et al., 2020). For example, Azmoude's paper showed that good family functioning associated with better quality of life in diabetics (Azmoude et al., 2016).
In Summary, previous studies have shown that family functioning has been separately associated with self‐efficacy and quality of life. Additionally, self‐efficacy has been found to be a major variable that affects the quality of life of patients with chronic diseases. Self‐efficacy may be involved in the psychological mechanism underlying the relationship between family functioning and quality of life in people with chronic diseases. However, to the best of our knowledge, no study has been conducted with a focus on the mediating effects of self‐efficacy between family functioning and quality of life in community‐dwelling elderly individuals with chronic diseases. Thus, the research questions of this study were as follows: (a) What are the levels of family functioning, self‐efficacy and quality of life among elderly individuals with chronic diseases? (b) What are the relationships among family functioning, self‐efficacy and quality of life? (c) To what extent, if at all, does self‐efficacy mediate the association between family functioning and quality of life in community‐dwelling elderly individuals with chronic diseases?
2. METHODS
2.1. Participants and sampling
Elderly individuals from different communities in Jiangsu Province (eastern China), Yunnan Province (southwestern China), Hunan Province (central China) and Shanxi Province (northern China) were selected by convenience sampling. The inclusion criteria were as follows (Kuhirunyaratn et al., 2019): (a) community‐dwelling people aged 60 years and older; (b) the presence of one or more chronic diseases such as hypertension or diabetes or others; and (c) ability to communicate normally and cooperate with investigation and evaluation. The exclusion criteria were as follows: (a) participants with obvious mental disorders or obvious cognitive impairment; and (b) participants with acute respiratory, circulatory or digestive diseases or injuries. Verbal informed consents were obtained from all participants, and they could withdraw from the study at any time.
2.2. Measurements
2.2.1. Questionnaire on sociodemographic characteristics
The questionnaire was designed by the researchers themselves and included sociodemographic characteristics and general features of their diseases (type of disease, duration of disease, etc.).
2.2.2. Self‐efficacy for managing chronic disease 6‐item scale (SECD6)
The SECD6 was created by Lorig (Lorig et al., 2001) and includes 6 items in total. Each item has 10 response categories ranging from ‘No confidence at all’ (1 point) to ‘With absolute confidence’ (10 points); thus, the average item score ranges from 1–10, where higher average scores indicate better self‐efficacy. The Chinese version of SECD6 has good internal consistency with a Cronbach's alpha of 0.91 (Jiang et al., 2020).
2.2.3. Family adaptation, partnership, growth, affection and resolve (APGAR) index
The APGAR index was designed by Good according to the characteristics of family functioning. The APGAR includes five items: adaptation, partnership, growth, affection and resolve. All of the items are positive items, and each one includes three options: often = 2, sometimes = 1, and almost never = 0. Total scores on this scale can range from 0–10; a score of 0–3 indicates severe family dysfunction, 4–7 indicates moderate family dysfunction, and 8–10 indicates good family functioning. The Chinese version of the APGAR has been used widely in China, and it has been found to have good validity and reliability (Sun et al., 2011).
2.2.4. MOS 36‐Item short form health survey (SF‐36)
The SF‐36, translated by the School of Medicine, Zhejiang University, includes 36 items (Dong et al., 2017). The score conversion formula is as follows: conversion score = (actual score − the lowest possible score in this aspect)/(the difference between the highest possible score and the lowest possible score in this aspect) × 100. The higher the score, the better the quality of life. The scale consists of nine dimensions: general health, physiological function, role physiological, body pain, role emotional, mental health, vitality, social function and health transition. The scale can be divided into two subscales: the physical component summary and the mental component summary. The Cronbach's alpha values for the internal consistency reliability were 0.72 and 0.88, respectively. The 2‐week test–retest reliability coefficients were 0.66 and 0.94, respectively (Hsu et al., 2018). The mental component summary includes vitality, social function, role emotional and mental health. The physical component summary includes physiological function, role physiological, body pain and general health. The total score on the SF‐36 is the sum of all items except health transition.
2.3. Data collection
Data were collected from 01 January–31 December 2019. After training and passing an examination, five nursing students began to conduct the investigation. Investigators went to community meeting sites or participants' homes, explained the purposes and methods of the study to the elderly individuals and then sent out questionnaires with their consent. While meeting face to face with the elderly participants, the researchers explained the meaning of each item clearly, and the participants could ask the researchers questions at any time if they could not understand the questionnaire. A total of 519 questionnaires were sent out. However, there questionnaires had unanswered questions and therefore invalid. Thus, a total of 516 valid questionnaires were collected, for an effective rate of 99.42%.
2.4. Data analysis
Data were analysed using SPSS 20.0 and AMOS 20.0. Frequencies and descriptive statistics were used to describe the data. Pearson correlation analysis was used to verify the correlations among the participants' self‐efficacy, family functioning and quality of life. A structural equation model was applied to determine the intermediary effects of self‐efficacy between family functioning and quality of life, and statistical significance was defined as p < .05.
2.5. Ethical consideration
The study was reviewed and approved by the Ethics Committee of School of Nursing, Yangzhou University (YZUHL2019001). The study was carried out in compliance with the tenets of the Declaration of Helsinki. Verbal informed consents were obtained from all participants. All personal information was encrypted.
3. RESULTS
3.1. Sociodemographic characteristics, self‐efficacy, family functioning and quality of life of the participants
A total of 516 community‐dwelling elderly people took part in this study; the sociodemographic characteristics of the respondents are presented in Table 1. The distribution of participants' chronic disease types is presented in Figure 1.
TABLE 1.
Distribution of respondents' sociodemographic characteristics (N = 516)
| Characteristics | Observation (N) | Percentage (%) |
|---|---|---|
| Gender | ||
| Female | 255 | 49.42 |
| Male | 261 | 50.58 |
| Age group (years) | ||
| 60–69 | 207 | 40.12 |
| 70–79 | 210 | 40.70 |
| 80 and above | 99 | 19.19 |
| Education level | ||
| Illiterate or barely literate | 192 | 37.21 |
| Primary school | 156 | 30.23 |
| Junior high school | 87 | 16.86 |
| Senior high school or technical secondary school | 42 | 8.14 |
| Junior college diploma or higher | 39 | 7.56 |
| Residence | ||
| Urban residents | 165 | 31.98 |
| Rural residents | 264 | 51.16 |
| Urban–rural fringe area | 87 | 16.86 |
| Current living conditions | ||
| Living alone | 54 | 10.47 |
| With spouse | 279 | 54.07 |
| With children and grandchildren | 180 | 34.88 |
| With others | 3 | 0.58 |
FIGURE 1.
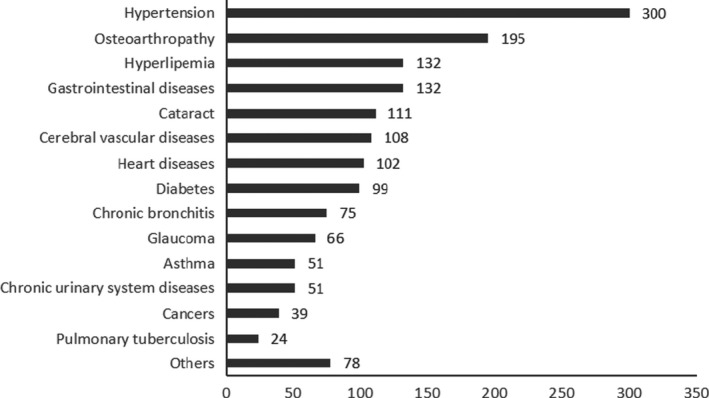
Distribution of participants' chronic disease types
The average scores for self‐efficacy and family functioning were 6.219 ± 2.059 and 8.035 ± 2.248, respectively. The average scores for general health, physiological function, role physiological, body pain, role emotional, mental health, vitality and social function were 55.878 ± 17.937, 68.576 ± 26.470, 61.773 ± 44.293, 74.581 ± 20.036, 72.674 ± 40.500, 68.256 ± 17.384, 66.337 ± 16.720 and 47.929 ± 11.879, respectively. The average scores for the physical component summary and the mental component summary were 260.808 ± 88.584 and 255.196 ± 72.876, respectively. The average total score for the 8 dimensions was 516.004 ± 151.884, and the average health transition score was 48.256 ± 21.517.
3.2. Correlation analysis of the participants' self‐efficacy, family functioning and quality of life
The results of the correlation analysis of self‐efficacy, family functioning and the quality of life of the community‐dwelling elders with chronic diseases are shown in Table 2. All variables were positively correlated and had statistical significance (all p < .01).
TABLE 2.
Correlation analysis of self‐efficacy, family functioning and the quality of life of the community‐dwelling elders with chronic diseases
| SECD6 | APGAR | General health | Physiological function | Role physiological | Body pain | Role emotional | Mental health | Vitality | Social function | Physical component summary | Mental component summary | SF‐36 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SECD6 | 1 | ||||||||||||
| APGAR | 0.462** | 1 | |||||||||||
| General health | 0.625** | 0.320** | 1 | ||||||||||
| Physiological function | 0.605** | 0.355** | 0.518** | 1 | |||||||||
| Role physiological | 0.507** | 0.247** | 0.526** | 0.584** | 1 | ||||||||
| Body pain | 0.416** | 0.347** | 0.477** | 0.523** | 0.487** | 1 | |||||||
| Role emotional | 0.431** | 0.382** | 0.425** | 0.581** | 0.694** | 0.392** | 1 | ||||||
| Mental health | 0.515** | 0.394** | 0.446** | 0.509** | 0.436** | 0.370** | 0.562** | 1 | |||||
| Vitality | 0.543** | 0.330** | 0.531** | 0.524** | 0.484** | 0.431** | 0.516** | 0.762** | 1 | ||||
| Social function | 0.474** | 0.342** | 0.499** | 0.644** | 0.531** | 0.587** | 0.551** | 0.591** | 0.610** | 1 | |||
| Physical component summary | 0.655** | 0.373** | 0.728** | 0.814** | 0.891** | 0.723** | 0.695** | 0.544** | 0.604** | 0.692** | 1 | ||
| Mental component summary | 0.564** | 0.438** | 0.546** | 0.670** | 0.687** | 0.501** | 0.898** | 0.822** | 0.797** | 0.750** | 0.768** | 1 | |
| SF‐36 | 0.653** | 0.428** | 0.687** | 0.796** | 0.850** | 0.662** | 0.836** | 0.712** | 0.735** | 0.763** | 0.952** | 0.928** | 1 |
Abbreviations: APGAR, Family Adaptation, Partnership, Growth, Affection and Resolve; SECD6, Self‐efficacy for Managing Chronic Disease 6‐item Scale.
p < .01.
3.3. Analysis of the mediating effects of self‐efficacy
In order to test whether self‐efficacy mediated the relationship between family functioning and quality of life, regression analysis was employed. The first step evaluated whether family functioning (as an independent variable) predicted quality of life (as a dependent variable). The second step tested the relationships between family functioning (as an independent variable) and self‐efficacy (a mediator). In step 3, when self‐efficacy was induced in the model, family functioning was found to have a significant impact on quality of life. The results are all displayed in Table 3. The mediation model is displayed in Figure 2, and the model was demonstrated to fit well by the following indicators: goodness‐of‐fit index (GFI) = 0.978, adjusted goodness‐of‐fit index (AGFI) = 0.964, standardized root mean square residual (SRMR) = 0.026, root mean square error of approximation (RMSEA) = 0.038, normal fit index (NFI) = 0.985, and incremental fit index (IFI) = 0.993. Similarly, the results regarding whether self‐efficacy is a mediator of the relationship between family functioning and the physical component summary or mental component summary are shown in Tables 4 and 5. The mediation models are displayed in Figure 3 and both models were demonstrated to fit well: GFI = 0.968 and 0.977, AGFI = 0.954 and 0.944, SRMR = 0.036 and 0.040, RMSEA = 0.037 and 0.039, NFI = 0.965 and 0.971, and IFI = 0.983 and 0.984, for the physical component summary and mental component summary, respectively. The results showed that self‐efficacy played a partial intermediary role between family functioning and quality of life, and the ratio of intermediary effects to total effects was calculated as 0.462 × 0.579/0.428 × 100% = 62.500%. Additionally, self‐efficacy played a partial intermediary role between family functioning and both the physical component summary and the mental component summary, the ratios of intermediary effects to total effects were calculated as 0.462 × 0.614/0.373 × 100% = 76.050% and 0.462 × 0.461/0.438 × 100% = 48.626%, respectively.
TABLE 3.
The mediating effects of self‐efficacy on family functioning and quality of life
| Step | Independent variable | Dependent variable | Adjusted R 2 | F | β | t | p |
|---|---|---|---|---|---|---|---|
| Step1 | Family functioning | Quality of life | .181 | 115.014 | 0.428 | 10.724 | <.01 |
| Step2 | Family functioning | Self‐efficacy | .212 | 139.425 | 0.462 | 11.808 | <.01 |
| Step3 | Family functioning | Quality of life | .444 | 206.918 | 0.160 | 4.325 | <.01 |
| Self‐efficacy | 0.579 | 15.632 | <.01 |
FIGURE 2.
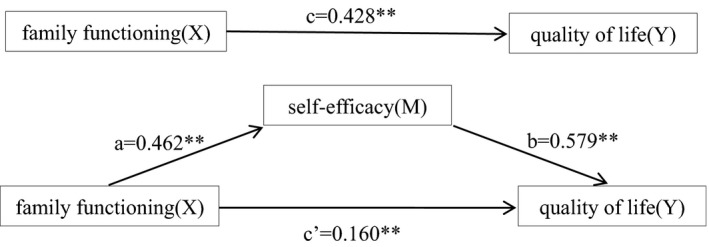
Mediation model of the effects of self‐efficacy on the relationship between family functioning and quality of life. **p < .01
TABLE 4.
The mediating effects of self‐efficacy on family functioning and physical component summary
| Step | Independent variable | Dependent variable | Adjusted R 2 | F | β | t | p |
|---|---|---|---|---|---|---|---|
| Step1 | Family functioning | Physical component summary | .138 | 83.193 | 0.373 | 9.121 | <.01 |
| Step2 | Family functioning | Self‐efficacy | .212 | 139.425 | 0.462 | 11.808 | <.01 |
| Step3 | Family functioning | Physical component summary | .433 | 197.886 | 0.090 | 2.401 | .017 |
| Self‐efficacy | 0.614 | 16.406 | <.01 |
TABLE 5.
The mediating effects of self‐efficacy on family functioning and mental component summary
| Step | Independent variable | Dependent variable | Adjusted R 2 | F | β | t | p |
|---|---|---|---|---|---|---|---|
| Step1 | Family functioning | Mental component summary | .190 | 121.675 | 0.438 | 11.031 | <.01 |
| Step2 | Family functioning | Self‐efficacy | .212 | 139.425 | 0.462 | 11.808 | <.01 |
| Step3 | Family functioning | Mental component summary | .356 | 143.265 | 0.225 | 5.635 | <.01 |
| Self‐efficacy | 0.461 | 11.554 | <.01 |
FIGURE 3.
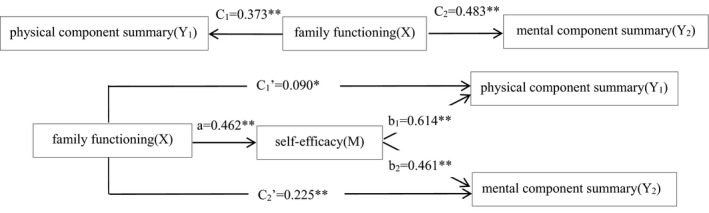
Mediation model of the effects of self‐efficacy on the relationship of family functioning with physical component summary or mental component summary. *p < .05, **p < .01
4. DISCUSSION
In this study, a total of 333 elderly individuals were ‘living alone’ or ‘living with their spouses’; that is, the proportion of participants living without children was 64.53% (higher than shown by national data), which may be related to the growing proportion of elderly individuals living without children and the large rural population in this study. In this study, the top four chronic disease types were hypertension (300, 58.14%), osteoarthropathy (195, 37.79%), hyperlipidemia (132, 25.58%) and chronic gastrointestinal diseases (132, 25.58%). Although the study was carried out in communities and inpatients were not included, the incidence of each type of chronic disease was still high. Hypertension and other chronic diseases have a high incidence in the elderly population in China. If the situation cannot be resolved properly and in time, it will lead to serious social and economic problems (Cao et al., 2017; Zhao et al., 2018).
In this study, the participants' average SECD6 score was 6.219 ± 2.059, which is at a moderate value and indicates that the self‐efficacy of the participants needs to be improved. This result was similar to that of a previous study (Fan & Lv, 2016). The average APGAR score was 8.035 ± 2.248, indicating that family functioning was relatively good. The average total score on the eight main dimensions of the SF‐36 was 516.004 ± 151.884, which was consistent with a study in China showing that the quality of life of elderly individuals based on the community nursing model was higher than the quality of life of elderly individuals based on the family and institutional nursing model. This may be because there was no strict separation between community nursing and family nursing in this study and because the basic characteristics of the participants were slightly different.
Self‐efficacy refers to people's subjective judgment and inner experience of whether they can successfully complete a certain behaviour. Quality of life is determined by an individual's physiological function, psychological status and other factors (Tuluce & Kutluturkan, 2018). In this study, self‐efficacy and quality of life were positively correlated and had a significant relationship. Research by Chirico et al. (2017) showed a positive relationship between self‐efficacy for coping with cancer and quality of life. Additionally, research findings from Son and Won (2017) demonstrated that the self‐efficacy of elderly patients with hypertension could affect their quality of life directly and could act as an intermediary variable influencing the effects of other variables on quality of life. The results of these prior studies were in accordance with the results of the present study.
In a study of the relationship between family functioning and quality of life, researchers found that people with better family functioning had higher quality of life, and correlation analysis showed that quality of life and family functioning had a strong positive correlation (Lu et al., 2017). This means that the low family functioning of elderly patients with chronic diseases was an important factor affecting their quality of life. In the present study, family functioning had a significant positive correlation with each dimension of quality of life, which was in agreement with the previous research results. Caregiving by family members has an extremely important impact on the quality of life of elderly individuals.
In this study, there was a statistically significant between self‐efficacy and family functioning. It is suggested that caregivers should help patients establish a systematic social and family support network and pay additional attention to family members, especially spouses and children, to help them participate in patients' disease management. Doctors and nurses can teach family members how to care for patients properly and can give supervision and full support in terms of emotion and action, which plays an extremely important role in improving patients' self‐efficacy, prolonging the stable period of disease and promoting patients' recovery.
To test the intermediary effects of self‐efficacy between family functioning and quality of life, we can use the intermediary effects test procedure summarized by Wen (Wen & Fan, 2015). If self‐efficacy has intermediary influences on family functioning and quality of life, the following three conditions should be met: (a) family functioning (as an independent variable) significantly predicts quality of life (as a dependent variable); (b) family functioning (as an independent variable) significantly predicts self‐efficacy (as an intermediary variable); and (c) family functioning and self‐efficacy jointly predict quality of life. When self‐efficacy (the intermediary variable) is added, if the influences of family functioning on quality of life are not significant, the intermediary variable shows a full intermediary effect, and if the influences of family functioning on quality of life are significant, the intermediary variable shows a partial intermediary effect. We found that self‐efficacy played a partial mediating role between family functioning and quality of life according to the above conditions, and the ratio of mediating effects to total effects was 62.500% in this study. Similarly, self‐efficacy also played a partial mediating role between family functioning and both the physical component summary and mental component summary, and the ratios of mediating effects to total effects were 76.050% and 48.626%, respectively. The proportions of the mediating effects of self‐efficacy were relatively large, especially between family functioning and the physical component summary. The findings suggested that higher family functioning was associated with more positive self‐efficacy, which, in turn, was associated with better quality of life. This finding demonstrated that effective family functioning can improve the ability of community‐dwelling elderly patients with chronic diseases to cope with their disease and control their emotions; additionally, it is conducive to cultivating the self‐efficacy of the patients. A strong sense of self‐efficacy can strengthen elderly people's capacity for self‐attribution and self‐adjustment, enabling them to take note of the combination of internal and external factors, which plays an important role in the health management of chronic diseases. Self‐efficacy can mobilize the subjective initiative of the patients so that they fully participate in self‐management of the disease, which is of great significance in improving their quality of life. Consequently, self‐efficacy, as a mediator, plays a key role in the process of behaviour change and is an important factor in maintaining and improving quality of life.
4.1. Strengths
To the best of our knowledge, this is the first representative analysis of the mediating effect of self‐efficacy in the association between family functioning and quality of life in community‐dwelling elderly individuals with chronic diseases. In addition, a variety of statistical methods (descriptive analysis, Pearson's correlation analysis and structural equation modelling) were employed to investigate the relationship among family functioning, self‐efficacy and quality of life.
4.2. Limitations
This study has a few limitations. First, we used a cross‐sectional design, with data being collected at only one point in time. Therefore, the study could not identify the changes and trends over time and, as such, might provide weak evidence of correlations among self‐efficacy, family functioning and quality of life. Second, the convenience sample may not be representative of the targeted population, and the results may be biased. In the future, we need to expand the sample size and use stratification and random sampling to enrich the research results and make them more representative.
5. CONCLUSION
This study demonstrated that family functioning, self‐efficacy and quality of life are closely related in community‐dwelling elderly individuals with chronic diseases. Family functioning, with self‐efficacy as the intermediary, has certain impacts on quality of life. This suggests that medical and health personnel should increase their focus on the indirect impacts of family functioning in the care process of community‐dwelling elderly patients with chronic diseases to enhance the patients' self‐efficacy and improve their quality of life.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
AUTHOR CONTRIBUTIONS
Yuan Yuan and Hui‐wen Xu contributed equally to this work. Wei‐juan Gong and Jing‐yan Liang contributed equally to this work. Yuan Yuan, Hui‐wen Xu, Wei‐juan Gong and Jing‐yan Liang : Study design, study conduction, collection and analysis of data and manuscript draft preparation. Akio Kitayama and En Takashi: Data collection, statistical analysis and manuscript draft preparation. Song Zhang, Ying Wang: Data collection. All authors read and approved the final manuscript.
ACKNOWLEDGEMENT
The authors would like to thank the participants for their supports in making this study possible.
Yuan Y, Xu H‐W, Zhang S, et al. The mediating effect of self‐efficacy on the relationship between family functioning and quality of life among elders with chronic diseases. Nurs Open. 2021;8:3566–3574. 10.1002/nop2.906
Funding information
This work was supported by the National Natural Science Foundation of China (81570392); the National Key R&D Program of China (2016YFE0126000); the National 2018 local universities science, education, culture and health introduction project – high‐end foreign experts project (GDW20183200386); the Key R&D projects of Yangzhou (YZ2020097) and the Open project of Key Laboratory of zoonosis in Jiangsu Province (HX20014).
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
REFERENCES
- Andrade, J. M. , Andrade, F. C. D. , Duarte, Y. A. D. , & de Andrade, F. B. (2020). Association between frailty and family functionality on health‐related quality of life in older adults. Quality of Life Research, 29(6), 1665–1674. 10.1007/s11136-020-02433-5 [DOI] [PubMed] [Google Scholar]
- Azmoude, E. , Tafazoli, M. , & Parnan, A. (2016). Assessment of family functioning and its relationship to quality of life in diabetic and non‐diabetic women. Journal of Caring Sciences, 5(3), 231–239. 10.15171/jcs.2016.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandura, A. (1977). Self‐efficacy: Toward a unifying theory of behavioral change. Psychological Review, 84(2), 191–215. 10.1037//0033-295x.84.2.191 [DOI] [PubMed] [Google Scholar]
- Botes, R. , Vermeulen, K. M. , Correia, J. , Buskens, E. , & Janssen, F. (2018). Relative contribution of various chronic diseases and multi‐morbidity to potential disability among Dutch elderly. BMC Health Services Research, 18(1), 24. 10.1186/s12913-017-2820-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao, G. , Chen, C. , Lin, Q. , Chen, Y. , Zhen, Z. , Zou, Y. , Liu, J. , Wu, M. , Wang, R. , Liu, M. , Zhao, C. , Lu, S. , Ng, M.‐Y. , Tse, H.‐F. , & Yiu, K.‐H. (2017). Prevalence, clinical characteristics and echocardiography parameters of non‐resistant, resistant and refractory hypertension in Chinese. Postgraduate Medicine, 129(2), 187–192. 10.1080/00325481.2017.1272398 [DOI] [PubMed] [Google Scholar]
- Chirico, A. , Lucidi, F. , Merluzzi, T. , Alivernini, F. , De Laurentiis, M. , Botti, G. , & Giordano, A. (2017). A meta‐analytic review of the relationship of cancer coping self‐efficacy with distress and quality of life. Oncotarget, 8(22), 36800–36811. 10.18632/oncotarget.15758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Croll, P. H. , Voortman, T. , Vernooij, M. W. , Baatenburg de Jong, R. J. , Lin, F. R. , Rivadeneira, F. , Ikram, M. A. , & Goedegebure, A. (2019). The association between obesity, diet quality and hearing loss in older adults. Aging, 11(1), 48–62. 10.18632/aging.101717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong, A. , Chen, S. , Zhu, L. , Shi, L. , Cai, Y. , Zeng, J. , & Guo, W. (2017). The reliability and validity of chinese version of sf36 v2 in aging patients with chronic heart failure. Aging Clinical and Experimental Research, 29(4), 685–693. 10.1007/s40520-016-0614-6 [DOI] [PubMed] [Google Scholar]
- Du, S. Z. , Hu, L. L. , Bai, Y. M. , Dong, J. S. , Jin, S. J. , Zhang, H. , & Zhu, Y. (2018). The influence of self‐efficacy, fear‐avoidance belief, and coping styles on quality of life for Chinese patients with chronic nonspecific low back pain: A multisite cross‐sectional study. Pain Practice, 18(6), 736–747. 10.1111/papr.12660 [DOI] [PubMed] [Google Scholar]
- Fan, X. Z. , & Lv, F. (2016). Psychosocial factors associated with self‐efficacy for managing chronic disease in patients with chronic heart failure. European Journal of Cardiovascular Nursing, 15(4), 255–261. 10.1177/1474515114566157 [DOI] [PubMed] [Google Scholar]
- Fjortoft, A. K. , Oksholm, T. , Forland, O. , Delmar, C. , & Alvsvag, H. (2020). Balancing contradictory requirements in homecare nursing‐A discourse analysis. Nursing Open, 7(4), 1011–1019. 10.1002/nop2.473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hager, A. G. M. , Mathieu, N. , Lenoble‐Hoskovec, C. , Swanenburg, J. , de Bie, R. , & Hilfiker, R. (2019). Effects of three home‐based exercise programmes regarding falls, quality of life and exercise‐adherence in older adults at risk of falling: Protocol for a randomized controlled trial. BMC Geriatrics, 19, 13. 10.1186/s12877-018-1021-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsu, T. W. , Chang, H. C. , Huang, C. H. , Chou, M. C. , Yu, Y. T. , & Lin, L. Y. (2018). Identifying cut‐off scores for interpretation of the Heart Failure Impact Questionnaire. Nursing Open, 5(4), 575–582. 10.1002/nop2.168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang, W. , Zhang, Y. , Yan, F. , Liu, H. , & Gao, R. (2020). Effectiveness of a nurse‐led multidisciplinary self‐management program for patients with coronary heart disease in communities: A randomized controlled trial. Patient Education and Counseling, 103(4), 854–863. 10.1016/j.pec.2019.11.001 [DOI] [PubMed] [Google Scholar]
- Konradsen, H. , Dieperink, K. B. , Lauridsen, J. , Sorknaes, A. D. , & Ostergaard, B. (2018). Validity and reliability of the danish version of the ice expressive family functioning and ice family perceived support questionnaires. Scandinavian Journal of Caring Sciences, 32(4), 1447–1457. 10.1111/scs.12591 [DOI] [PubMed] [Google Scholar]
- Kuhirunyaratn, P. , Prasomrak, P. , & Jindawong, B. (2019). Effects of a health education program on fall risk prevention among the urban elderly: A quasi‐experimental study. Iranian Journal of Public Health, 48(1), 103–111. 10.18502/ijph.v48i1.788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee, E. H. , Lee, Y. W. , & Moon, S. H. (2016). A structural equation model linking health literacy to self‐efficacy, self‐care activities, and health‐related quality of life in patients with type 2 diabetes. Asian Nursing Research, 10(1), 82–87. 10.1016/j.anr.2016.01.005 [DOI] [PubMed] [Google Scholar]
- Lorig, K. R. , Sobel, D. S. , Ritter, P. L. , Laurent, D. , & Hobbs, M. (2001). Effect of a self‐management program on patients with chronic disease. Effective Clinical Practice, 4(6), 256–262. [PubMed] [Google Scholar]
- Lu, C. J. , Yuan, L. X. , Lin, W. Q. , Zhou, Y. , & Pan, S. M. (2017). Depression and resilience mediates the effect of family function on quality of life of the elderly. Archives of Gerontology and Geriatrics, 71, 34–42. 10.1016/j.archger.2017.02.011 [DOI] [PubMed] [Google Scholar]
- Maresova, P. , Javanmardi, E. , Barakovic, S. , Barakovic Husic, J. , Tomsone, S. , Krejcar, O. , & Kuca, K. (2019). Consequences of chronic diseases and other limitations associated with old age ‐ A scoping review. BMC Public Health, 19(1), 1431. 10.1186/s12889-019-7762-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nugent, R. (2019). Preventing and managing chronic diseases. BMJ, 364, l459. 10.1136/bmj.l459 [DOI] [PubMed] [Google Scholar]
- Nurchayati, S. , Utomo, W. , & Karim, D. (2019). Correlation between family support and quality of life among hypertensive patients. Enfermeria Clinica, 29, 60–62. 10.1016/j.enfcli.2018.11.020 [DOI] [Google Scholar]
- Omran, S. , & McMillan, S. (2018). Symptom severity, anxiety, depression, self‐ efficacy and quality of life in patients with cancer. Asian Pacific Journal of Cancer Prevention, 19(2), 365–374. 10.22034/APJCP.2018.19.2.365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puspasari, J. , Rachmawati, I. N. , & Budiati, T. (2018). Family support and maternal self‐efficacy of adolescent mothers. Enfermeria Clinica, 28, 227–231. 10.1016/S1130-8621(18)30073-1 [DOI] [Google Scholar]
- Selzler, A. M. , Habash, R. , Robson, L. , Lenton, E. , Goldstein, R. , & Brooks, D. (2020). Self‐efficacy and health‐related quality of life in chronic obstructive pulmonary disease: A meta‐analysis. Patient Education and Counseling, 103(4), 682–692. 10.1016/j.pec.2019.12.003 [DOI] [PubMed] [Google Scholar]
- Son, Y. J. , & Won, M. H. (2017). Depression and medication adherence among older Korean patients with hypertension: Mediating role of self‐efficacy. International Journal of Nursing Practice, 23(3), e12525. 10.1111/ijn.12525 [DOI] [PubMed] [Google Scholar]
- Sun, L. , Clarke, R. , Bennett, D. , Guo, Y. U. , Walters, R. G. , Hill, M. , Parish, S. , Millwood, I. Y. , Bian, Z. , Chen, Y. , Yu, C. , Lv, J. , Collins, R. , Chen, J. , Peto, R. , Li, L. , & Chen, Z. (2019). Causal associations of blood lipids with risk of ischemic stroke and intracerebral hemorrhage in Chinese adults. Nature Medicine, 25(4), 569–574. 10.1038/s41591-019-0366-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun, L. , Sun, L. N. , Sun, Y. H. , Yang, L. S. , Wu, H. Y. , Zhang, D. D. , Cao, H. Y. , & Sun, Y. (2011). Correlations between psychological symptoms and social relationships among medical undergraduates in Anhui Province of China. International Journal of Psychiatry in Medicine, 42(1), 29–47. 10.2190/PM.42.1.c [DOI] [PubMed] [Google Scholar]
- Tuluce, D. , & Kutluturkan, S. (2018). The effect of health coaching on treatment adherence, self‐efficacy, and quality of life in patients with chronic obstructive pulmonary disease. International Journal of Nursing Practice, 24(4), e12661. 10.1111/ijn.12661 [DOI] [PubMed] [Google Scholar]
- Wang, B. Y. , He, P. , & Dong, B. R. (2015). Association between family functioning and cognitive impairment among Chinese nonagenarians/centenarians. Geriatrics & Gerontology International, 15(9), 1135–1142. 10.1111/ggi.12410 [DOI] [PubMed] [Google Scholar]
- Wei, Y. X. , Liu, B. P. , Ma, Z. Y. , Zhou, L. , & Jia, C. X. (2020). Family functioning and suicide among the elderly in rural China a case‐control psychological autopsy study. Journal of Nervous and Mental Disease, 208(2), 131–137. 10.1097/Nmd.0000000000001116 [DOI] [PubMed] [Google Scholar]
- Wen, Z. L. , & Fan, X. T. (2015). Monotonicity of effect sizes: Questioning kappa‐squared as mediation effect size measure (vol 20, pg 193, 2015). Psychological Methods, 20(2), 193–203. 10.1037/met0000040 [DOI] [PubMed] [Google Scholar]
- Wu, F. , & Sheng, Y. (2019). Social support network, social support, self‐efficacy, health‐promoting behavior and healthy aging among older adults: A pathway analysis. Archives of Gerontology and Geriatrics, 85, 103934. 10.1016/j.archger.2019.103934 [DOI] [PubMed] [Google Scholar]
- Wu, F. L. , Tai, H. C. , & Sun, J. C. (2019). Self‐management experience of middle‐aged and older adults with type 2 diabetes: A qualitative study. Asian Nursing Research, 13(3), 209–215. 10.1016/j.anr.2019.06.002 [DOI] [PubMed] [Google Scholar]
- Yeung, N. C. , & Lu, Q. (2014). Affect as a mediator between self‐efficacy and quality of life among Chinese cancer survivors in China. European Journal of Cancer Care, 23(1), 149–155. 10.1111/ecc.12123 [DOI] [PubMed] [Google Scholar]
- Zhang, J. H. , Gilmour, S. , Liu, Y. C. , & Ota, E. (2020). Effect of health literacy on quality of life among patients with chronic heart failure in china. Quality of Life Research, 29(2), 453–461. 10.1007/s11136-019-02332-4 [DOI] [PubMed] [Google Scholar]
- Zhang, Y. , Xue, G. , Chen, Y. , An, K. , & Chen, L. (2020). Factors related to spiritual health in Chinese haemodialysis patients: A multicentre cross‐sectional study. Nursing Open, 7(5), 1536–1543. 10.1002/nop2.535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao, C. J. , Wong, L. P. , Zhu, Q. , & Yang, H. (2018). Prevalence and correlates of chronic diseases in an elderly population: A community‐based survey in Haikou. PLoS One, 13(6), e0199006. 10.1371/journal.pone.0199006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou, M. , Wang, H. , Zhu, J. , Chen, W. , Wang, L. , Liu, S. , Li, Y. , Wang, L. , Liu, Y. , Yin, P. , Liu, J. , Yu, S. , Tan, F. , Barber, R. M. , Coates, M. M. , Dicker, D. , Fraser, M. , González‐Medina, D. , Hamavid, H. , … Liang, X. (2016). Cause‐specific mortality for 240 causes in China during 1990–2013: A systematic subnational analysis for the global burden of disease study 2013. The Lancet, 387(10015), 251–272. 10.1016/S0140-6736(15)00551-6 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, upon reasonable request.


