Abstract
Aim
The aim of the study was to determine the psychometric properties, construct validity and internal consistency of the Chinese language version of the Nurse Professional Competence scale short form.
Design
A methodological design was used.
Methods
Questionnaire data from 260 nursing students nearing graduation from 2 universities in China were analysed using confirmatory factor analysis, known‐group validity and internal consistency.
Results
The confirmatory factor analysis revealed that the model was acceptable, and the analyses for known‐group validity revealed statistically significant differences in all factors and the total scale of the Nurse Professional Competence scale short form. Internal consistency revealed that Cronbach's alpha values exceeded 0.70 for all factors and the total scale. The Chinese language version of the Nurse Professional Competence scale short form has acceptable construct validity and good internal consistency.
Keywords: nurse professional competence, nursing students, psychometric testing, reliability, short form, validity
1. INTRODUCTION
Professional competence is the ability to use a set of knowledge, skills and behaviours to successfully perform jobs, roles or responsibilities (World Health Organization, 2015). In the rapid development of healthcare systems, nurses constitute a vital professional group who must be competent in providing safe, high‐quality and cost‐effective healthcare (International Council of Nurses, 2019). In 2018, the National Health Commission and Ministry of Education of the People's Republic of China constructed guidelines on nursing education and training policies to promote the reform and development of nursing services (Ministry of Health, 2018). The guideline emphasized that nurse competency is the key issue for nursing educators and administrators, and assessing and improving competency is a vital aspect in meeting requirements for an improved health system. This highlights the need for a valid instrument measuring nurse professional competence that is grounded in nurses’ core competencies.
2. BACKGROUND
Assessing and improving nurse competency is considered important aspect in nursing practice and education. In China, several attempts have been made and a wide range of instruments have been developed to assess nursing competence. There are some weaknesses with the instruments currently in use. There are many generic and specific instruments used as assessment indicators of nurse competence that were constructed based on literature reviews or expert opinions. However, most of these instruments were developed without rigorous testing for psychometric properties, such as the Competency Evaluation Index System for nursing students (Xu & Sun, 2013), the Competency Evaluation Index for nursing interns (Huang et al., 2019), the Competency Evaluation Indicator System for new nurses (Xiao et al., 2020) and the Competency Evaluation System for specialized nurses (Bi et al., 2018; Huang et al., 2020; Li et al., 2018; Lu, 2020). These evaluation indexes could provide a reference for training and performance assessment in nursing education and clinical nursing, but their use in research is less valuable as long as validity not rigorously tested.
Some instruments were developed by modifying existing scales (Chen & Sun, 2014; Hu et al., 2011; Zhao et al., 2008) or translating international scales (Li et al., 2011). During the development of some modified instruments, exploratory factor analyses (EFAs) tested their construct validities. However, confirmatory factor analysis (CFA; which provides information on latent constructs by explaining the association between the observed variables) was not applied to instruments such as the Nursing Graduate Competency Self‐Assessment Questionnaire (Chen & Sun, 2014) and the Competency Inventory for Registered Nurses (Liu et al., 2007). In addition, these instruments lacked items regarding safety and evidence‐based practice, which are some of the core competencies of nursing (Institute of Medicine (U.S.) et al., 2003) and should be rigorously assessed by nursing competency instruments. It is therefore necessary to use an instrument with rigorous and comprehensive assessment of nurse professional competence in a Chinese context.
There are numerous reliable and valid instruments in the international literature for assessing nursing competence. Most of the developing instruments are based on literature reviews (Cowan et al., 2008), conceptual analyses (Takase & Teraoka, 2011) or Benner's description of knowledge in clinical practice (Meretoja et al., 2004). Only the Nurse Professional Competence scale (NPC), which was developed in 2014 and revised in 2018 by Swedish experts (Nilsson et al., 2014, 2018), was based on formal competence requirements from The Swedish Board of Health and Welfare (2005), The Swedish Society of Nursing (2017), and World Health Organization (2001), and is consistent with the six core competencies identified by the Institute of Medicine (2003). Ethical considerations and a holistic approach to nursing were also emphasized in the competency requirements (The Swedish Board of Health & Welfare, 2005).
The NPC scale comprised 88 items within 8 factors, and has been evaluated (Nilsson et al., 2014) and determined to be a psychometrically sound scale in several studies (Gardulf et al., 2019; Nilsson et al., 2014, 2019). An English translation of the Swedish NPC scale is now available (Nilsson et al., 2016). This NPC scale was translated and used in Austria, Germany, Norway, Portugal and Switzerland as part of the European Network Nursing Academies project (Nilsson et al., 2016, 2019), and has also been used in Australia (van der Mortel et al., 2020) and the Kingdom of Saudi Arabia (Halabi et al., 2020; Nilsson et al., 2019) on samples of clinical nurses (Halabi et al., 2020) and nursing students nearing graduation (Gardulf et al., 2016).
The 88 items of the original NPC scale combined with additional instruments made the questionnaire time‐consuming for respondents. The short form (SF) of the NPC scale with 35 items was developed in an attempt to improve the response rate (Nilsson et al., 2018). The following six competence areas were included in the SF questionnaire: (a) nursing care, (b) value‐based nursing care, (c) medical and technical care, (d) care pedagogics, (e) documentation and administration of nursing care, and (f) development, leadership and organization of nursing care. The NPC‐scale SF was reported be a reliable scale, with Cronbach's alpha values from 0.71–0.86. The construct validity of the scale was supported by principal components analysis, CFA and the known‐group validity in the previous studies (Halabi et al., 2020; Nilsson et al., 2018).
The aim of the study was to determine the psychometric properties, construct validity and internal consistency of the NPC‐scale SF Chinese language version (NPC‐SF‐C).
3. METHOD
This was a multi‐step study where the NPC‐scale SF firstly was translated to Chinese, tested in think‐aloud interviews with 8 nursing students and thereafter tested for its psychometric properties in a questionnaire study with 260 nursing students.
3.1. Instrument translation
Three physicians familiar with both the Swedish and Chinese healthcare systems translated the Swedish language version of the NPC‐scale SF to Chinese, and vice versa. The first step involved each person providing a forward translation of one‐third of the items from Swedish to Chinese. The second step was a backward translation (Chinese to Swedish), in which each person translated a different third of the items. The back‐translated and original versions were then compared and discussed in the research group (second and last authors) along with the translators, resulting in smaller adjustments being made to the Chinese version. The translation process was performed based on recommendations by Nilsson et al. (2016). After the translation, the scale was tested in think‐aloud interviews with four Chinese nursing students in their second semester of the third year. In the first round of interviews, the students could not fully understand the meaning of items 10, 24, 29, 32, 34 and 35. The author who conducted the think‐aloud interviews contacted the authors who developed the original version of the NPC‐scale SF, and then made small adjustments to some phrases (e.g. changing work‐related risk to nursing occupational risk) to better match phrases used in nursing in China. The author who conducted the interviews also discussed the phrasing with two nursing teachers in informal discussion format. The scale was then tested in a new round of think‐aloud interviews with four new nursing students. In the second round, the students understood the meaning of the items but had questions and suggestions regarding items 2, 3 and 26. For example, a suggestion for item 2 “meet patient's basic physical needs” was to provide examples, and “eating, nutritional intake, and relaxation” was added. The first, second and last authors repeatedly discussed all of the changes in order to reach a consensus.
3.2. Evaluation of validity and reliability of the NPC‐SF‐C
3.2.1. Design
To test the construct validity and internal consistency of the NPC‐SF‐C, we used questionnaire data and a cross‐sectional correlation design.
3.2.2. Participants
The study participants included 260 nursing students from 2 universities in China. The students had completed their clinical education/internship and were in their last semester before graduation. The nursing programmes at the universities were 4‐year bachelor's degrees with students performing their clinical education in the last year.
3.2.3. Data collection
Data were collected using online questionnaires in June 2018 (146 of 198 eligible participants from 2 universities, with a response rate of 73.7%) and a paper version on March 30, 2019 (114 of 151 eligible participants from 1 university, with a response rate of 75.5%), with a total response rate of 74.5% (260 of 349 eligible students). Additional data were collected for one of the universities in 2019 in order to reach the 200‐participant minimum for a CFA (Myers et al., 2011). Two email and phone call reminders were sent to nonresponders.
3.2.4. Instrument
The NPC‐scale SF (Nilsson et al., 2018) measures nurse professional competence and consists of 35 items divided into 6 factors: nursing care (5 items), value‐based nursing care (5 items), medical and technical care (6 items), care pedagogics (5 items), documentation and administration of nursing care (8 items), and development, leadership and organization of nursing care (6 items). The response alternatives, for each item, are presented on a 7‐point scale from 1 (to a very low degree)–7 (to a very high degree). Raw scores of the items in a factor are summarized, divided by the highest possible score in that factor and multiplied with 100. The scale has been translated into several languages (NPC Research Group, 2019) and used in numerous countries (Halabi et al., 2020; van der Mortel et al., 2020; Nilsson et al., 2019).
The 88‐item NPC scale was originally developed in Sweden (Nilsson et al., 2014), and the NPC‐scale SF was later developed to satisfy the need for shorter a scale (Nilsson et al., 2018). The construct validity of the NPC‐scale SF has been reported as satisfactory (using EFA and CFA) and Cronbach's alpha values ranged from 0.71–0.86 for the factors, demonstrating its internal consistency (Nilsson et al., 2018).
3.2.5. Data analyses
To examine construct validity, a CFA was performed using SPSS Amos software (IBM) and to examine internal consistency, Cronbach's alpha values were calculated. Absolute parameters such as the chi‐square (χ2) test, root–mean–square error of the approximation (RMSEA) and standardized root–mean–square residual (SRMR), and relative parameters such as comparative fit index (CFI) were used as goodness‐of‐fit indexes (Kline, 2013b). The value of χ2 is preferably nonsignificant, but where this does not occur, RMSEA is also recommended, with an acceptable value being <0.08 (Kline, 2013a). If the 90% confidence interval (CI) exceeds 0.10, there may be problems with the model (Kline, 2013b). SRMR was also used, with an acceptable value being <0.10 (Kline, 2013b). An acceptable value for CFI is >0.95, but >0.90 is also accepted (Kääriäinen et al., 2011). Construct validity was also tested with known‐group validity using the question: “Did you have enough opportunities to perform different kinds of nursing skills during your internship?” It is assumed that the scores for the NPC‐scale SF factors will be significantly higher among those answering “yes” (N = 106) than those answering “no” (N = 154).
Data are presented using mean, standard deviation, median, quartile, skewness and kurtosis values. Student's t test was used to compare the “yes” and “no” groups. SPSS Statistics (version 24, IBM) was used to analyse data, except for CFAs.
3.3. Ethical consideration
The regional ethical review board of the University where the authors affiliated approved this study (No. 20180089). The purpose and methods were described to the participants in writing, and they were also given assurances about their privacy, confidentiality and right to withdraw from the study with no explanation.
4. RESULTS
4.1. Characteristics of participants
In the psychometric test of the instrument, 260 nursing students participated, the mean age of the students was 22.2 years (range 20–29), 93% were female, and 63% applied for undergraduate studies with nursing as their first choice (Table 1).
TABLE 1.
Demographic characteristics of the samples (N = 260)
| Characteristic | Categories | N (%) | Mean(SD) | Range |
|---|---|---|---|---|
| Age, years | 22.2 (0.9) | 20–29 | ||
| Gender | Male | 18 (6.9) | ||
| Female | 242 (93.1) | |||
| Living area | Rural area | 156 (60.0) | ||
| Urban area | 104 (40.0) | |||
| First choice selecting nursing major | Yes | 165 (63.5) | ||
| No | 95 (36.5) | |||
| Having enough opportunities to perform nursing skills | Yes | 106 (40.8) | ||
| No | 154 (59.2) | |||
Abbreviation: Standard deviation (SD).
4.2. Construct validity, CFA and known‐group validity
A CFA with maximum likelihood estimation was used to test the six‐factor solution, allowing correlations between the factors. Correlations between some error terms were also allowed based on results of the modification indexes (see Figure 1). Goodness‐of‐fit index values for the final model were χ2 1,351.065 p < .001, CMIN/Df 2.554, RMSEA 0.077 (90% confidence intervals 0.072–0.083), CFI 0.901 and SRMR 0.0488. Items, factors, descriptive data and factor loadings are presented in Table 2 and Figure 1.
FIGURE 1.
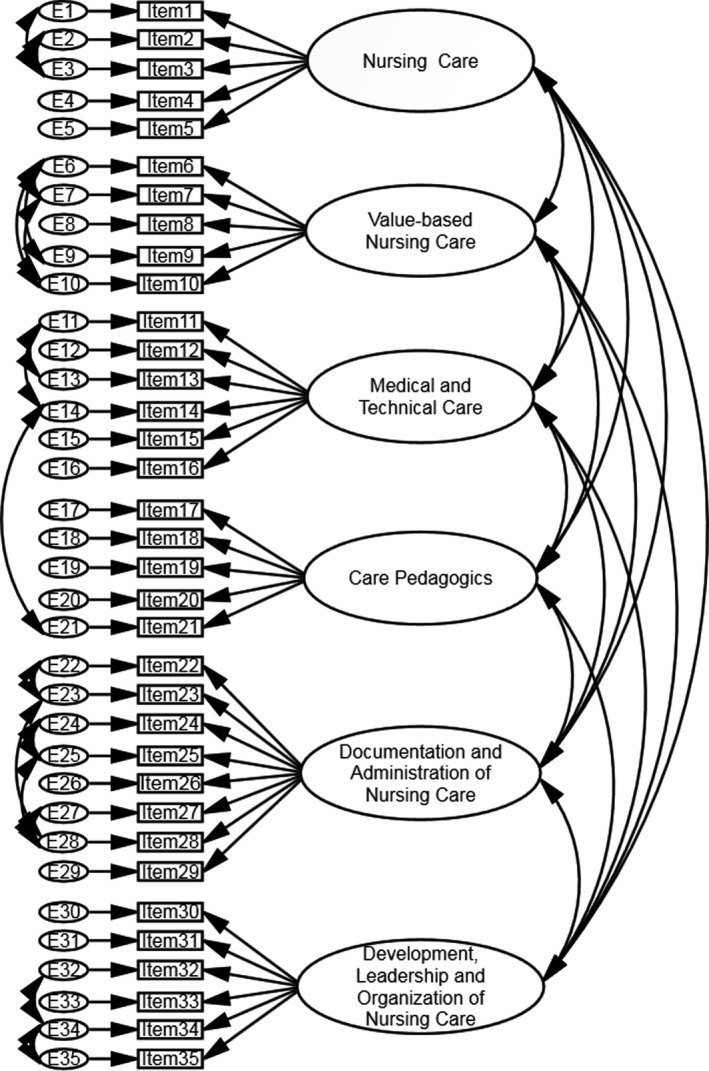
Flow chart presenting the underlying construct of the NPC‐SF Chinese language version ([error term] E)
TABLE 2.
Factor loadings in the confirmatory factor analyses and scores for the items and factors (N = 260)
|
Factors/items (Cronbach's Alpha) Ability to….. |
Factor loadings ML | Factor loadings ML/standardized | Mean (SD) | Median (Q1;Q3) | Skewness/Kurtosis |
|---|---|---|---|---|---|
| Nursing care, 5 items (0.86) | 80.4 (12.8) | 82.9 (74.3;85.7) | −1.11/1.66 | ||
| 1. Independently apply the nursing process | 0.970 | 0.698 | 5.5 (1.2) | 6 (5;6) | −1.08/0.90 |
| 2. Meet patient's basic physical needs | 1.054 | 0.764 | 5.7 (1.2) | 6 (5;6) | −1.38/2.32 |
| 3. Meet patient's specific physical needs | 0.787 | 0.564 | 5.3 (1.2) | 6 (4.25;6) | −0.92/0.80 |
| 4. Document patient's physical status | 0.988 | 0.782 | 5.9 (1.1) | 6 (6;7) | −1.75/4.68 |
| 5. Document patient's psychological status | 1 | 0.797 | 5.7 (1.0) | 6 (5;6) | −1.08/1.59 |
| Value‐based nursing care, 5 items (0.91) | 87.1 (11.8) | 85.7 (82.9;97.1) | −1.20/1.37 | ||
| 6. Respectfully communicate with patients, relatives and staff | 1.005 | 0.800 | 6.2 (1.0) | 6 (6;7) | −1.63/3.46 |
| 7. Show respect for patient autonomy, integrity and dignity | 0.987 | 0.853 | 6.2 (0.9) | 6 (6;7) | −1.43/1.82 |
| 8. Enhance patients’ and relatives’ knowledge and experiences | 0.968 | 0.793 | 5.9 (1.0) | 6 (5;7) | −0.87/0.41 |
| 9. Show respect for different values and beliefs | 0.940 | 0.802 | 6.2 (0.9) | 6 (6;7) | −1.61/3.22 |
| 10. Contribute to a holistic view of the patient | 1 | 0.850 | 6.0 (1.0) | 6 (6;7) | −1.29/2.22 |
| Medical and technical care, 6 items (0.78) | 83.0 (11.5) | 85.7 (76.2;92.3) | −0.88/0.97 | ||
| 11. Manage drugs and clinical application of knowledge in pharmacology | 1.090 | 0.711 | 5.6 (1.1) | 6 (5;6) | −0.92/0.87 |
| 12. Independently administer prescriptions | 0.698 | 0.282 | 4.7 (1.8) | 5 (4;6) | −0.66/−0.63 |
| 13. Pose questions about unclear instructions | 1.022 | 0.660 | 6.1 (1.1) | 6 (6;7) | −1.81/4.07 |
| 14. Support patients during examinations and treatments | 1.077 | 0.789 | 6.1 (1.0) | 6 (6;7) | −1.64/3.83 |
| 15. Follow up on patient's conditions after examinations and treatments | 1.050 | 0.865 | 6.1 (0.9) | 6 (6;7) | −1.11/1.21 |
| 16. Handle medical/technical equipment according to legislation and safety routines | 1 | 0.831 | 6.2 (0.9) | 6 (6;7) | −1.16/1.17 |
| Care pedagogics, 5 items (0.91) | 86.1 (11.7) | 85.7(82.9;94.3) | −1.22/2.28 | ||
| 17. Provide patients and relatives with support to enhance participation in patient care | 0.942 | 0.689 | 5.8 (1.1) | 6 (5;7) | −1.32/2.71 |
| 18. Inform and educate individual patients and relatives | 1.036 | 0.897 | 6.1 (0.9) | 6 (6;7) | −1.17/1.76 |
| 19. Inform and educate groups of patients and relatives | 1.059 | 0.868 | 6.0 (1.0) | 6 (6;7) | −1.28/2.13 |
| 20. Make sure that information given to the patient is understood | 1.002 | 0.899 | 6.1 (0.9) | 6 (6;7) | −1.17/2.10 |
| 21. Motivate the patient to adhere to treatments | 1 | 0.796 | 6.2 (1.0) | 6 (6;7) | −1.74/4.73 |
| Documentation and administration of nursing care, 8 items (0.95) | 85.4 (11.7) | 85.7(80.4;94.2) | −1.32/2.79 | ||
| 22. Make use of relevant data in patient records | 1.029 | 0.823 | 6.0 (1.0) | 6 (6;7) | −1.08/1.09 |
| 23. Use information technology as a support in nursing care | 1.039 | 0.832 | 6.0 (1.0) | 6 (6;7) | −1.40/2.74 |
| 24. Document according to current legislation | 1.013 | 0.846 | 6.1 (0.9) | 6 (6;7) | −1.38/2.79 |
| 25. Comply with current legislation and routines | 0.990 | 0.859 | 6.2 (0.9) | 6 (6;7) | −1.24/1.80 |
| 26. Handle sensitive personal data in a safe way | 1.102 | 0.872 | 6.1 (1.0) | 6 (6;7) | −1.66/4.20 |
| 27. Observe work‐related risks and prevent them | 1.052 | 0.775 | 5.8 (1.1) | 6 (5;6) | −1.14/2.11 |
| 28. Continuously engage in professional development | 0.982 | 0.781 | 5.8 (1.0) | 6 (5;6) | −0.78/0.50 |
| 29. Lead and develop health staff teams | 1 | 0.828 | 6.0 (0.9) | 6 (6;7) | −1.08/1.34 |
| Development, leadership and organization of nursing care, 6 items (0.91) | 85.2 (11.1) | 85.7(81.0;92.9) | −0.92/0.94 | ||
| 30. Act adequately in the event of unprofessional conduct among employees | 1.029 | 0.741 | 5.8 (1.0) | 6 (5;6) | −0.92/1.36 |
| 31. Apply principles of disaster medicine | 1.022 | 0.863 | 6.1 (0.9) | 6 (6;7) | −1.13/1.40 |
| 32. Search and review relevant literature for evidence‐based nursing | 0.977 | 0.751 | 5.9 (0.9) | 6(5.25;6) | −1.11/2.34 |
| 33. Interact with other professionals in care pathways | 1.038 | 0.828 | 6.1 (0.9) | 6 (6;7) | −1.21/1.40 |
| 34. Teach, supervise and assess students | 0.999 | 0.745 | 5.9 (1.0) | 6 (6;7) | −0.91/0.38 |
| 35. Supervise and educate staff | 1 | 0.794 | 6.0 (0.9) | 6 (6;7) | −0.92/0.53 |
Abbreviation: Maximum likelihood (ML), Standard deviation (SD), quartile (Q), for total scale (all items), the Cronbach's Alpha level was 0.97.
The results regarding known‐group validity revealed that the scores in all factors and in the total score of the NPC‐SF‐C were significantly higher for the “yes” group than the “no” group (all p values <.001; Table 3).
TABLE 3.
Known‐group validity comparing the yes‐ and no‐group in response to the item “Did you have enough opportunities to perform different kinds of nursing skills during your internship?” (N = 260)
| Factor |
“Yes‐group” N = 106 Mean (SD) |
“No‐group” N = 154 Mean (SD) |
p‐value |
|---|---|---|---|
| Nursing care | 85.7 (9.2) | 76.7 (13.6) | <.001 |
| Value‐based nursing care | 91.3 (8.8) | 84.1 (12.8) | <.001 |
| Medical and technical care | 88.2 (8.5) | 79.3 (11.9) | <.001 |
| Care pedagogics | 90.5 (9.1) | 83.2 (12.4) | <.001 |
| Documentation and administration of nursing care | 89.8 (8.4) | 82.4 (12.7) | <.001 |
| Development, leadership and organization of nursing care | 88.8 (9.3) | 82.7 (11.6) | <.001 |
| Total scale | 89.1 (7.6) | 81.5 (11.0) | <.001 |
p‐value for Student's t test.
Abbreviation: SD, Standard deviation.
4.3. Descriptive data and internal consistency
Internal consistency, quantified using Cronbach's alpha, had values of 0.784–0.945 for the factors and 0.972 for the total scale. The mean factor scores for the NPC‐SF‐C ranged from 80.4 (nursing care)–87.1 (value‐based nursing care), and the mean item scores ranged from 4.7 (item 12)–6.2 (items 6, 7, 9, 16, 21 and 25).
5. DISCUSSION
5.1. Validity and reliability of NPC‐SF‐C
In this study, we translated the NPC‐scale SF from Swedish into Chinese. The results indicated that the NPC‐SF‐C had acceptable construct validity and good internal consistency for the self‐assessment of professional competence among Chinese nursing students.
CFA and known‐group validity were used to test the construct validity for the NPC‐SF‐C. CFA through structural equation modelling is prioritized over EFA when empirical or theoretical evidence is available to interpret the relationships among observed variables for the latent factors (Kline, 2013b). CFA findings indicated that the item factor loading was satisfactory, with values of 0.56–0.90. Item 12 (can independently administer prescriptions) is an exception, with a loading to factor 3 (medical and technical care) of 0.28, which does not meet the item retention criteria. The factor loading values for item 12 may have been poor due to most of the participants (72.3%) having no work experience, not being registered nurses, and not being able to administer prescriptions without the supervision of a registered nurse. Chinese nursing students receive clinical education/internships in their fourth year. Swedish nursing students start to practice administering prescriptions with their preceptor earlier during their clinical education, approximately during their third semester.
Since “can independently administer prescriptions” (item 12) belongs to the core competency of safety (Institute of Medicine (U.S.) et al., 2003), this item was retained in the NPC‐SF‐C. The CFA results indicated that the NPC‐SF‐C (with item 12) shared the six‐factor structural model of the original scale, and the goodness‐of‐fit indexes indicated that the model provided an acceptable fit to the data. Although the χ2 test had a significant result, when χ2 divided by the number of degrees of freedom (CMIN/df) was 2.55, below the recommended value of 3 (Kline, 2013b). The CFI value was >0.90 (Kääriäinen et al., 2011), RMSEA was 0.077, and SRMR 0.0488, suggesting an acceptable model fit to the data (Kline, 2013b). These results theoretically support the construct validity of the original NPC‐SF.
The construct validity was also measured as the known‐group validity. It was assumed that students who responded “yes” on the item “Did you have enough opportunities to perform different kinds of nursing skills during your internship?” should also score higher on NPC‐scale SF than those who responded “no.” Statistically significant differences were found between the two groups (those who answered “no” and those who answered “yes” to the previous item) for all factors and the total score of the NPC‐SF‐C, indicating that the nursing students with more practical experience have greater professional competence. This result is consistent with a previous report of registered nurses with more work experience having a higher level of professional competence (Halabi et al., 2020). Work experience has been reported as an important factor influencing professional competence among registered nurses (Aqtash et al., 2017). These findings suggest that the NPC‐SF‐C has good discrimination performance and is a useful instrument for identifying the differences between the professional competence of nursing students with different practical experiences.
The Cronbach's alpha values for the six factors were 0.78–0.95, indicating that the NPC‐SF‐C was reliable. In the Swedish NPC‐SF, the factors had internal consistency values of 0.71–0.86 (Nilsson et al., 2018). The number of response alternatives was changed from four in the original version of the NPC‐SF to seven in order to increase the scale's reliability (Streiner et al., 2003), as recommended by Nilsson et al. (2018). These findings were also similar to the English version of the NPC‐SF, which was tested among registered nurses working in Saudi Arabia, with Cronbach's alpha values for the factors of 0.86–0.93 (Halabi et al., 2020).
5.2. Status of nursing competence among Chinese nursing students
High mean scores were present for the Chinese nursing students nearing graduation, ranging from 80.4 (nursing care)–87.1 (value‐based nursing care) on the six factors of professional competence. Nursing students nearing graduation from the 3‐year nursing education programme in Sweden had mean scores ranging from 76.4 (documentation and administration of nursing)–87.2 (value‐based nursing care; Carlsson, 2020). Chinese nursing students showed the lowest score for the factor of nursing care when compared with the results in the studies among nursing students in Europe and Sweden (Forsman et al., 2020; Nilsson et al., 2019). The present study had discouraging results, with students having low scores in item 1 (“ability to independently apply the nursing process”) and item 3 (“ability to meet patients specific physical needs”). Therefore, nursing educators and administrators must pay more attention to the application of the nursing process to improve the professional competence of nursing students.
5.3. Limitations
This study found that the psychometric properties of the NPC‐SF‐C are acceptable, but some limitations should also be considered. The cross‐cultural adaption of the NPC‐SF‐C was a pretest to two rounds of think‐aloud interviews among only eight female nursing students in their third year of study who have similar professional knowledge to the sample. According to recommendations from the World Health Organization on the cross‐cultural and conceptual equivalence for the adaption of instruments, a pretest should be conducted through a cognitive review involving at least 10 respondents (both male and female) in each round who are not eligible for the main study (World Health Organization, 2020). The nursing students were recruited from two universities in China using convenience sampling, which often results in sampling bias that can impair the generalizability of the results. The test–retest reliability and predictive validity of the instrument were also not tested.
6. CONCLUSION
Our findings indicate that the NPC‐SF‐C has acceptable construct validity and good internal consistency. In addition, Chinese nursing students had the highest score for the factor of value‐based nursing care and the lowest score for the factor of nursing care, most notably for item 1 (“ability to independently apply the nursing process”) and item 3 (“ability to meet patients specific physical needs”). The scale can be used to measure the self‐rated professional competence of nursing students. Future studies should test the validity of the NPC‐SF‐C in Chinese registered nurses.
6.1. Relevance to practice and research
These results have implications for both nursing education and clinical nursing. The current study has obtained promising results regarding psychometric properties of the NPC‐SF‐C when used amongst nursing students nearing graduation. The NPC‐SF‐C should be used in additional studies including new nursing graduates and registered nurses with professional experience. In previous research, the NPC scale was used to evaluate professional competence among registered nurses (Halabi et al., 2020) and assess the effects of nursing education programmes (Gardulf et al., 2019), which may be efficacious for the NPC‐SF‐C. Therefore, this scale could be used in nursing practice as a guide in altering the competence development strategies for clinical nurses to match the requirements of the improved health system. The NPC‐SF‐C may be useful in nursing education as an evaluation tool for exploring education reform programmes, such as self‐directed study programmes among nursing students.
Our findings have implications for future studies. The NPC‐SF‐C was evaluated using nursing students, and future studies should include registered nurses in order to assess professional competence within actual healthcare settings in China. In previous studies, the NPC scale was used to evaluate the effects of inter‐professional education (Castrèn et al., 2017), and the effects of a new education curriculum (Theander et al., 2016). Future interventional studies should be conducted using the NPC‐SF‐C to assess the effects of education reform programmes among nursing students. It has been previously reported that professional competence is related to background factors (Carlsson, 2020; Gardulf et al., 2016), self‐efficacy (Falk‐Brynhildsen et al., 2019) and other factors, and so future moderating or mediating studies could use the NPC‐SF to further analyse the relation mechanism using structural equation modelling. Charette et al. (2020) suggested that further research should generate more evidence regarding the measurement properties of existing scales using different populations or contexts.
AUTHOR CONTRIBUTIONS
LX: Conceptualization, Methodology (design), Formal analysis, Investigation (data collection), Data Curation, Writing – original draft, Writing – review and editing, Project administration and Funding acquisition. JN: Conceptualization, Methodology (design) and Writing – review and editing. JZ: Methodology (design), Investigation (data collection) and Writing – review and editing. ME: Conceptualization, Methodology (design), Formal analysis, Writing – original draft, Writing – review and editing and Project administration.
CONFLICT OF INTREST
No conflict of interest was declared by the authors.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available in the supplementary material of this article.
Supporting information
Table S1
Table S2
Table S3
Data S1
ACKNOWLEDGEMENTS
The authors would like to thank all the Chinese nursing students for their participants and thank Professor Zanhua Zhou for data collection and fund providing.
Xu, L. , Nilsson, J. , Zhang, J. , & Engström, M. (2021). Psychometric evaluation of Nurse Professional Competence Scale—Short‐form Chinese language version among nursing graduate students. Nursing Open, 8, 3232–3241. 10.1002/nop2.1036
Funding information
This study was supported by grants from Department of Education Research Fund in Zhejiang Province, Grant/Award Number: jg20180360; Department of Education Research Fund in Zhejiang Province, Grant/Award Number:jg20190418
REFERENCES
- Aqtash, S. , Robb, W. F. , Hunter, L. H. , Almuhtasib, M. , Hamad, A. , & Brownie, S. M. (2017). Self‐assessed competence of experienced expatriate nurses in a rural and remote setting. SAGE Open Nursing, 3, 1–7. 10.1177/2377960817702382 [DOI] [Google Scholar]
- Bi, N. , Chen, J. , & Yang, X. (2018). Construction of competent characteristic system and level standard model for orthopedic specialized nurses. Chinese Journal of Modern Nursing, 24(1), 22–27. [Google Scholar]
- Carlsson, M. (2020). Self‐reported competence in female and male nursing students in the light of theories of hegemonic masculinity and femininity. Journal of Advanced Nursing, 76(1), 191–198. 10.1111/jan.14220 [DOI] [PubMed] [Google Scholar]
- Castrèn, M. , Mäkinen, M. , Nilsson, J. , & Lindström, V. (2017). The effects of interprofessional education ‐ Self‐reported professional competence among prehospital emergency care nursing students on the point of graduation ‐ A cross‐sectional study. International Emergency Nursing, 32, 50–55. 10.1016/j.ienj.2017.02.004 [DOI] [PubMed] [Google Scholar]
- Charette, M. , McKenna, L. G. , Maheu‐Cadotte, M. , Deschênes, M. , Ha, L. , & Merisier, S. (2020). Measurement properties of scales assessing new graduate nurses’ clinical competence: A systematic review of psychometric properties. International Journal of Nursing Studies, 110, 103734. 10.1016/j.ijnurstu.2020.103734 [DOI] [PubMed] [Google Scholar]
- Chen, L. , & Sun, H. (2014). Research on preparation and evaluation about nursing graduate competency self‐assessment questionnaire. Chinese Nursing Research, 28(21), 2591–2593. [Google Scholar]
- Cowan, D. T. , Wilson‐Barnett, D. J. , Norman, I. J. , & Murrells, T. (2008). Measuring nursing competence: Development of a self‐assessment tool for general nurses across Europe. International Journal of Nursing Studies, 45(6), 902–913. 10.1016/j.ijnurstu.2007.03.004 [DOI] [PubMed] [Google Scholar]
- Falk‐Brynhildsen, K. , Jaensson, M. , Gillespie, B. M. , & Nilsson, U. (2019). Swedish operating room nurses and nurse anesthetists’ perceptions of competence and self‐efficacy. Journal of PeriAnesthesia Nursing, 34(4), 842–850. 10.1016/j.jopan.2018.09.015 [DOI] [PubMed] [Google Scholar]
- Forsman, H. , Jansson, I. , Leksell, J. , Lepp, M. , Sundin Andersson, C. , Engström, M. , & Nilsson, J. (2020). Clusters of competence: Relationship between self‐reported professional competence and achievement on a national examination among graduating nursing students. Journal of Advanced Nursing, 76(1), 199–208. 10.1111/jan.14222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardulf, A. , Florin, J. , Carlsson, M. , Leksell, J. , Lepp, M. , Lindholm, C. , Nordström, G. , Theander, K. , Wilde‐Larsson, B. , & Nilsson, J. (2019). The Nurse Professional Competence (NPC) Scale: A tool that can be used in national and international assessments of nursing education programmes. Nordic Journal of Nursing Research, 39(3), 137–142. 10.1177/2057158518824530 [DOI] [Google Scholar]
- Gardulf, A. , Nilsson, J. , Florin, J. , Leksell, J. , Lepp, M. , Lindholm, C. , Nordström, G. , Theander, K. , Wilde‐Larsson, B. , Carlsson, M. , & Johansson, E. (2016). The Nurse Professional Competence (NPC) Scale: Self‐reported competence among nursing students on the point of graduation. Nurse Education Today, 36, 165–171. 10.1016/j.nedt.2015.09.013 [DOI] [PubMed] [Google Scholar]
- Halabi, J. O. , Lepp, M. , & Nilsson, J. (2020). Assessing self‐reported competence among registered nurses working as a culturally diverse work force in public hospitals in the Kingdom of Saudi Arabia. Journal of Transcultural Nursing, 32(1), 69–76. 10.1177/1043659620921222 [DOI] [PubMed] [Google Scholar]
- Hu, B. , Yang, S. , Gang, T. , Shao, W. , & Li, D. (2011). Research on evaluation indexes of core competence of nurses. Chinese Nursing Management, 11(10), 67–69. [Google Scholar]
- Huang, T. , Yang, Y. , Zhong, Y. , Liu, Y. , Li, N. , Tan, Y. , Deng, L. , Chen, S. , Huang, Y. , Ye, S. , & Chen, L. (2019). Construction of competency evaluation indexes for full‐time undergraduate nursing students. Modern Clinical Nursing, 18(12), 59–64. [Google Scholar]
- Huang, Y. , Feng, Z. , Huang, C. , & Xu, Y. (2020). Development of a competency evaluation system for nursing care of AIDS patients. Chinese Journal of Nursing, 55(4), 563–568. [Google Scholar]
- Institute of Medicine (U.S.) , Greiner, A. & Knebel, E. (2003). Health Professions Education: A bridge to quality. National Academies Press. [PubMed] [Google Scholar]
- International Council of Nurses (2019). ICN International Workforce Forum calls for urgent action from governments to address global nursing shortage. Retrieved from https://www.icn.ch/news/icn‐international‐workforce‐forum‐calls‐urgent‐action‐governments‐address‐global‐nursing [Google Scholar]
- Kääriäinen, M. , Kanste, O. , Elo, S. , Pölkki, T. , Miettunen, J. , & Kyngäs, H. (2011). Testing and verifying nursing theory by confirmatory factor analysis. Journal of Advanced Nursing, 67(5), 1163–1172. 10.1111/j.1365-2648.2010.05561.x [DOI] [PubMed] [Google Scholar]
- Kline, R. B. (2013a). Assessing statistical aspects of test fairness with structural equation modelling. Educational Research and Evaluation, 19(2–3), 204–222. 10.1080/13803611.2013.767624 [DOI] [Google Scholar]
- Kline, R. B. (2013b). Chapter 6: Exploratory and confirmatory factor analysis. In Petscher Y., Schatschneider C., & Compton D. L. (Eds.), Applied Quantitative Analysis in Education and the Social Sciences (pp. 173–207). Routledge. [Google Scholar]
- Li, C. , Kong, X. , Carrie, B. L. , Zhang, Y. , Li, X. , & Liu, X. (2011). The reliability and validity of the Chinese version of the Competency Performance Examination [in Chinese]. Chinese Journal of Nursing Education, 8(9), 393–395. 10.3761/j.issn.1672-9234.2011.09.003 [DOI] [Google Scholar]
- Li, Q. , Fu, L. , Fang, L. , Deng, H. , & Lai, D. (2018). Construction of evaluation index system for competency of community nurses. Chinese Nursing Research, 32(24), 3866–3869. [Google Scholar]
- Liu, M. , Kunaiktikul, W. , Senaratana, W. , Tonmukayakul, O. , & Eriksen, L. (2007). Development of competency inventory for registered nurses in the People’s Republic of China: Scale development. International Journal of Nursing Studies, 44(5), 805–813. 10.1016/j.ijnurstu.2006.01.010 [DOI] [PubMed] [Google Scholar]
- Lu, J. (2020). Construction of evaluation index system for nursing posts in neonatal intensive care unit. Journal of Nursing Administration, 20(2), 99–102. [Google Scholar]
- Meretoja, R. , Isoaho, H. , & Leino‐Kilpi, H. (2004). Nurse competence scale: Development and psychometric testing. Journal of Advanced Nursing, 47(2), 124–133. 10.1111/j.1365-2648.2004.03071.x [DOI] [PubMed] [Google Scholar]
- Ministry of Health (2018). Guideline about Nursing Education and Training to promote the reform and development of nursing service, Ministry of Health of the People’s Republic of China. Retrieved from http://www.nhc.gov.cn/yzygj/s7659/201807/257b5617f77f4aaf93ea331a6b876fec.shtm [Google Scholar]
- Myers, N. D. , Ahn, S. , & Jin, Y. (2011). Sample size and power estimates for a confirmatory factor analytic model in exercise and sport: A Monte Carlo approach. Research Quarterly for Exercise and Sport, 82(3), 412–423. 10.1080/02701367.2011.10599773 [DOI] [PubMed] [Google Scholar]
- Nilsson, J. , Engström, M. , Florin, J. , Gardulf, A. , & Carlsson, M. (2018). A short version of the nurse professional competence scale for measuring nurses’ self‐reported competence. Nurse Education Today, 71, 233–239. 10.1016/j.nedt.2018.09.028 [DOI] [PubMed] [Google Scholar]
- Nilsson, J. , Gardulf, A. , & Lepp, M. (2016). Process of translation and adaptation of the Nurse Professional Competence (NPC) Scale. Journal of Nursing Education and Practice, 6(1), 100–103. 10.5430/jnep.v6n1p100 [DOI] [Google Scholar]
- Nilsson, J. , Johansson, E. , Egmar, A. , Florin, J. , Leksell, J. , Lepp, M. , Lindholm, C. , Nordström, G. , Theander, K. , Wilde‐Larsson, B. , Carlsson, M. , & Gardulf, A. (2014). Development and validation of a new tool measuring nurses self‐reported professional competence—the Nurse Professional Competence (NPC) Scale. Nurse Education Today, 34(4), 574–580. 10.1016/j.nedt.2013.07.016 [DOI] [PubMed] [Google Scholar]
- Nilsson, J. , Mischo‐Kelling, M. , Thiekoetter, A. , Deufert, D. , Mendes, A. C. , Fernandes, A. , Kirchhoff, J. W. , & Lepp, M. (2019). Nurse professional competence (NPC) assessed among newly graduated nurses in higher educational institutions in Europe. Nordic Journal of Nursing Research, 39(3), 159–167. 10.1177/2057158519845321 [DOI] [Google Scholar]
- NPC Research Group (2019). NPC Research Project. Retrieved from https://npcresearchgroup.com [Google Scholar]
- Streiner, D. , Norman, G. , & Cairney, J. (2003). Chapter 4: Scaling responses. In: Streiner D., Norman G., & Cairney J. (Eds) Health Measurement Scales: A Practical Guide to Their Development and Use (pp 29–60, 3rd edn). Oxford University Press . [Google Scholar]
- Takase, M. , & Teraoka, S. (2011). Development of the holistic nursing competence scale. Nursing & Health Sciences, 13(4), 396–403. 10.1111/j.1442-2018.2011.00631.x [DOI] [PubMed] [Google Scholar]
- The Swedish Board of Health and Welfare (2005). Competence Requirements for Registered Nurses. The Swedish National Board of Health and Welfare. Retrieved from https://www.alvsbyn.se/wp‐content/uploads/2014/06/2005‐105‐1_20051052.pdf [Google Scholar]
- The Swedish Society of Nursing (2017). Competence Requirements for Registered Nurses. The Swedish Society of Nursing. Retrieved from https://www.swenurse.se/globalassets/01‐svensk‐sjukskoterskeforening/publikationer‐svensk‐sjukskoterskeforening/kompetensbeskrivningarpublikationer/kompetensbeskrivning‐legitimerad‐sjukskoterska‐2017‐for‐webb.pdf [Google Scholar]
- Theander, K. , Wilde‐Larsson, B. , Carlsson, M. , Florin, J. , Gardulf, A. , Johansson, E. , Lindholm, C. , Nordström, G. , & Nilsson, J. (2016). Adjusting to future demands in healthcare: Curriculum changes and nursing students’ self‐reported professional competence. Nurse Education Today, 37, 178–183. 10.1016/j.nedt.2015.11.012 [DOI] [PubMed] [Google Scholar]
- van der Mortel, T. , Nilsson, J. , & Lepp, M. (2020). Validating the Nurse Professional Competence Scale in Australia among Bachelor Nursing Students. Collegian: The Australian Journal of Nursing Practice, Scholarship and Research, 28(2), 244–251. 10.1016/j.colegn.2020.06.010 [DOI] [Google Scholar]
- World Health Organization (2001). Nurses and Midwives for Health: WHO European Strategy for Nursing and Midwifery Education. World Health Organization, Europe. https://www.euro.who.int/__data/assets/pdf_file/0009/125748/E72922.pdf?ua [Google Scholar]
- World Health Organization (2015). Roles and Responsibilities of Government Chief Nursing and Midwifery Offices: a Capacity‐Building Manual. World Health Organization, Global. Retrieved from https://www.who.int/hrh/nursing_midwifery/15178_gcnmo.pdf?ua=1 [Google Scholar]
- World Health Organization (2020). Process of Translation and Adaptation of Instruments. World Health Organization, Global. Retrieved from https://www.who.int/substance_abuse/research_tools/translation/en/ [Google Scholar]
- Xiao, F. , Xiong, L. , He, J. , Chang, X. , Xiang, Y. , Li, X. , & Xu, C. (2020). Development of evaluation indicator system of independent working for new nurses based on Delphi method. Chinese Nursing Research, 34(1), 28–33. [Google Scholar]
- Xu, L. , & Sun, H. (2013). Study on competency comprehensive evaluation index system for nursing graduates. Chinese Nursing Research, 27(12), 1065–1067. 10.3969/j.issn.1009-6493.2013.12.004 [DOI] [Google Scholar]
- Zhao, R. , Wu, Y. , Jin, N. , Shao, C. , Yang, F. , Liu, J. , Li, R. , Guo, M. , Shi, S. , & Li, S. (2008). Development and evaluation of the instrument to identify nurse’s core competence. Chinese Journal of Nursing, 6, 485–489. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1
Table S2
Table S3
Data S1
Data Availability Statement
The data that support the findings of this study are available in the supplementary material of this article.


