Abstract
Aim
To select and obtain relevant evidence of airway management in adult critically ill patients at home and abroad, formulate clinical quality review indicators based on evidence and analyse obstacle factors and promoting factors in evidence‐based nursing practice. To promote standardized ICU airway management evidence‐based nursing practice to provide the basis.
Design
Obstacle factor analysis.
Methods
Take the Joanna Briggs Institute (JBI) evidence‐based healthcare model as theoretical guidance, establish evidence‐based problems, form a team, systematically search for literature, evaluate quality and summarize evidence, establish quality review indicators and review methods, analyse obstacles and facilitating factors based on the review results and formulate corresponding action strategies.
Results
According to the 29 best evidences, 21 review indicators were developed. Through the results of clinical quality review, the main barriers to evidence‐based practice were analysed: the lack of nurse training and relevant evidence‐based knowledge at the practitioner level, the lack of standardized procedures for airway management and the lack of materials at the system level.
Conclusion
There is a big gap between airway management evidence and clinical practice in critically ill adult patients. Therefore, improvement measures should be formulated for obstacle factors to promote effective transformation of evidence into clinical practice.
Keywords: artificial airway, critically ill patients, evidence‐based practice, management, obstacle analysis, review of nursing quality
What is already known about this topic
Most of the clinical practices and decisions of airway management in adult patients with critical illness are not based on the best evidence, but on clinical experience, and there is still a big gap between theory and practice.
What this paper adds
Based on the guidance of evidence‐based theory model, this paper analysed the barriers and promoting factors of evidence‐based airway management practice for adult critically ill patients, promoted the development of evidence‐based best practices and continuously improved clinical quality.
1. INTRODUCTION
Artificial airway refers to the insertion of a catheter into the trachea through the mouth/nasal or tracheotomy site to establish a smooth gas exchange channel, improve the ventilation function and thereby correct the body's hypoxic state (Juan, 2017). In clinical practice, poor quality of airway management in critically ill patients can lead to related complications, aggravate the patient's original condition, prolong the patient's hospital stay and increase treatment costs (Branson et al., 2014, Umobong et al., 2018 and Feng D et al., 2019). Prospective studies have been carried out on the main complications of airway management in intensive care units abroad, and relevant data show that the quality of airway management is not optimistic (Cook et al., 2011). According to domestic literature, among patients with artificial airway in the intensive care unit, the incidence of lung infection is 40.6% (Yi et al., 2018), and the cuff pressure compliance rate is an average of 35.29% (Lirong et al., 2018). Only 9.2% of ICU nurses met the requirements of the guidelines for sputum suction operations (Zheng et al., 2015) and cannot follow the clinical practice guidelines well (Guihua et al., 2015), and there is still a big gap between theory and clinical practice.
Evidence‐based health care is the core guiding ideology of medical and healthcare decision‐making in the 21st century, and it plays an important role in promoting the scientificity, effectiveness and standardization of global medical and healthcare decision‐making. However, most of the current clinical practice and decision‐making are not based on the best evidence, but based on clinical experience, which makes the clinical practice have greater variability, resulting in poor results, inefficiency and unfair use of resources. Evidence‐based nursing is beneficial to improve the clinical outcome of patients and improve the quality of clinical nursing. The evidence‐based practice of scholars such as Chan et al. (2017) and Yan et al. (2019) has been successfully applied in different areas of nursing, enabling decision‐makers and practitioners to make evidence‐based decisions at the point of care.
The JBI evidence‐based healthcare model was first proposed by Professor Alan Pearson of the Joanna Briggs Evidence‐based Health Care Centre in Australia in 2005 (Pearson et al., 2005) and updated in 2016 (Jordan et al., 2016). In 2009, it was introduced into China by Professor Hu Yan of JBI Evidence‐based Nursing Cooperation Center of Fudan University, providing theoretical guidance and methods for domestic nursing staff to carry out evidence‐based nursing practice (Yan & Yufang, 2018). The JBI model of evidence‐based health care aims to promote global health through evidence‐based practices and is its core value. The key steps of evidence‐based practice in this mode mainly include Evidence Generation, Evidence Synthesis, Evidence Transfer and Evidence Implementation. This paper aims to analyse the obstacle factors and promoting factors before the application of evidence and formulate action strategies to facilitate the subsequent clinical practice of evidence.
2. METHODS
2.1. Identify evidence‐based nursing problems
The clinical problems of airway management were structured to establish evidence‐based problems based on the PIPOST model of JBI Evidence‐Based Healthcare Centers (Dang et al., 2017; Jordan et al., 2016; Pearson et al., 2005; Yan & Yufang, 2018). P (Population) is the evidence application population: critically ill patients with tracheal intubation or tracheotomy; I (Intervention) refers to intervention measures: intervention measures for airway management; P (Professional) is a professional who applies evidence, including medical staff and clinical managers; O (Outcome) is the outcome: the incidence of lung infection in adult critically ill patients with tracheal intubation or tracheotomy, sputum characteristics, NICU length of stay, nurses' compliance with evidence‐based airway management in critically ill adults, nurse‐related knowledge awareness rate; S (Setting) is the place of evidence implementation: neurosurgical intensive care unit (NICU) in a level III first‐class hospital in Hubei Province, China; T (Type of evidence) is the type of evidence: highest clinical decision‐making, guidelines, systematic reviews, expert consensus and summary of evidence.
2.2. Build a team
Set up an evidence‐based nursing team consisting of 12 members. Among them, there is a director of the nursing department and a project tutor, who is responsible for the development of the evidence‐based practice programme. One deputy head nurse who participated in the workshop training of evidence transformation project of Fudan University Evidence‐based Nursing Center was responsible for overall planning, coordination and guidance. The deputy chief physician of the department and the head nurse were responsible for guiding and supervising the implementation of the programme. Three graduate students who have participated in the training of Fudan University Evidence‐based Nursing Center are responsible for evidence retrieval, quality evaluation and evidence collection. There are 4 specialist nurses in the department, who are responsible for collating and analysing expert opinions, clinical data collection and baseline investigation together with graduate students.
2.3. To search for evidence of airway management in adults with critical illness
This study is based on JBI evidence‐based healthcare model, structured clinical problems according to the PIPOST model and formulated retrieval strategies. Search from top to bottom according to the "6S Evidence Resource Pyramid Model" (Dicenso et al., 2009), use computer to search up to date, Joanna Briggs Institute (JBI) evidence‐based healthcare centre database, British Medical Journal (BMJ), National Guideline Clearinghouse (NGC), American Society of Critical Care Medicine (SCCM), British National UK National Institute for Health and Care Excellence (NICE), Cochrane library, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Medline, PubMed, CBMdisc, CNKI and Wanfang database on all evidence of airway management of adult critically ill patients, including advanced clinical decision support, guidelines, systematic reviews, evidence summary and expert consensus. The search time limit is from the establishment of the database to 15 August 2019. After preliminary screening and re‐screening of the retrieved literature, a total of 25 literatures were included, including 1 of advanced clinical decision support, 7 of guidelines, 8 of systematic evaluation, 5 of evidence summary and 4 of expert consensus. The flow chart of literature search is shown in Figure 1.
FIGURE 1.
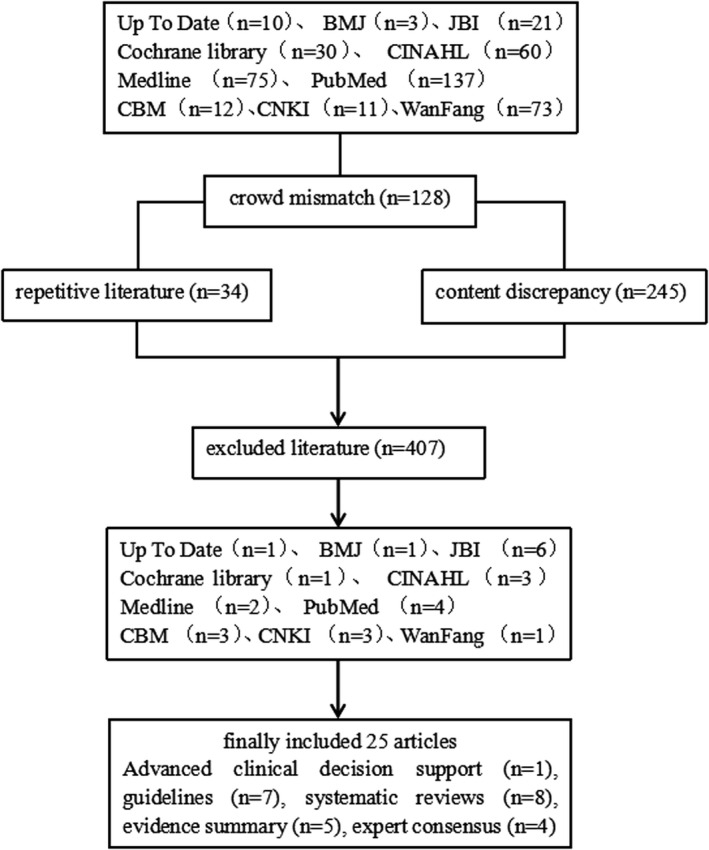
Literature search flow chart
2.4. Evaluation and summary of the best evidence for airway management in critically ill adults
(1) Literature quality evaluation: The quality evaluation of the guideline uses the AGREEⅡ (Brouwers et al., 2010) evaluation scale to be independently completed by 2 researchers, and the quality evaluation of the systematic review and expert consensus is conducted by 2 researchers using the quality evaluation tool of the Australian JBI Evidence‐based Health Care Center (Yan & Yufang, 2018) independently completed, the quality evaluation of advanced clinical decision‐making and evidence summary traces the original literature on which the evidence is based and selects corresponding evaluation tools for quality evaluation according to the type of literature. After systematic quality evaluation, a total of 25 articles were included. (2) Evaluation of evidence items: the evidence included in the literature was extracted, the evidence grading and evidence recommendation grading system of the Australian JBI Evidence‐based Health Care Center (2014 edition) (Yan & Yufang, 2018) were adopted, and the evidence from clinical decisions, guidelines, evidence summaries and expert consensus was traced back to the original literature for the grading of the evidence. The clinical expert group evaluated the feasibility, suitability, clinical significance and validity of the evidence according to the FAME evaluation form of the JBI evidence (Yan & Yufang, 2018) to determine whether the evidence was included.
2.5. Establish evidence‐based nursing review indicators and baseline review
The review indicators should involve structure, process and result levels (Zhou Yingfeng,et al., 2016). (1) Structural indicators: refer to the various resources needed in the process of practice; (2) Process indicators: refer to the action strategies adopted in the process of practice; (3) Result indicators: refer to the effects produced in the process of practice; at the same time, it should be credible, effective and measurable characteristics to comprehensively evaluate the status of clinical practice and best practice implementation (Cao et al., 2019; Donabedian A, 1988; Zhou Yingfeng,et al., 2016). Based on the best evidence and after two rounds of discussion, the members of this research group and the expert group determined the localized quality review indicators and developed the review methods to conduct a baseline review of the clinical practice of airway management for adult critically ill patients in the Department of Neurosurgery, a level III first‐class hospital in Jingzhou City, Hubei Province, China.
3. RESULTS
3.1. Included evidence
This study was summarized from seven aspects: airway assessment, airway attraction timing, cuff pressure management, airway humidification, airway attraction, tracheotomy care, oral care and so on, and a total of 44 best evidences were included (Yujiao et al., 2021). A total of 15 stakeholders in the hospital were invited to conduct evidence FAME evaluation (Yan & Yufang, 2018), including feasibility, appropriateness, clinical significance and effectiveness. The evidences were selected and 29 evidences were obtained, as shown in Table 1.
TABLE 1.
Best evidence for airway management in critically ill adults after FAME evaluation
| Evidence dimension | Content of evidence | Recommendation grade |
|---|---|---|
| Airway assessment | 1. The skin condition of the patient's tracheostomy should be assessed daily and cleaned according to the patient's needs. If there is redness, tenderness, swelling, inflammation, smell, high skin temperature, yellow‐green discharge around the stoma or fever in the patient, the clinician should be notified. If there are obvious signs of infection, it is recommended to provide culture/sensitive specimens (Picot et al., 2019) | A |
| Airway suction timing | 2. When blood oxygen saturation or partial pressure of oxygen decreases (American Association for Respiratory Care, 2010) | A |
| 3. When frequent coughing or respiratory distress syndrome occurs (American Association for Respiratory Care, 2010) | A | |
| Cuff pressure management | 4. Daily tracheal tube care includes monitoring and maintaining balloon pressure, ideally 20cm H2O~30 cmH2O to avoid under‐inflation or over‐inflation (Hyzy, 2018) | A |
| 5. Cuff pressures should be monitored and recorded at least once every nursing shift and after manipulation of the tracheostomy tubes (Fong, 2017) | A | |
| 6. The cuff pressure cannot be inflated by the finger touch method based on experience (Respiratory Therapeutics Group of Respiratory Medicine Branch of Chinese Medical Association, 2014a, 2014b) | A | |
| 7. When there is no automatic inflator device, manually re‐measure the cuff pressure every 6–8 hr. The inflation pressure should be higher than the ideal value of 2 cmH2O during each measurement and clean the water in the pressure measuring tube in time (Respiratory Therapeutics Group of Respiratory Medicine Branch of Chinese Medical Association, 2014a, 2014b) | A | |
| 8. When the patient's airway pressure is low or the spontaneous breathing is weak and sputum suction, the cuff pressure should be increased appropriately; when the patient's position changes, the cuff pressure should be remeasured (Respiratory Therapeutics Group of Respiratory Medicine Branch of Chinese Medical Association, 2014a, 2014b) | B | |
| Airway humidification | 9. Regularly evaluating and adjusting airway humidification and sputum drainage measures can effectively prevent airway sputum scab formation. Ipratropium bromide 0.5mg, budesonide 1mg, 2−3times/day aerosol inhalation is recommended, and ambroxol hydrochloride 30 mg, 2–3 times/day can be intravenously injected to facilitate expectorant (Chinese Medical Association Neurosurgery Branch et al., 2016) | B |
|
A | |
| 11. Heat‐and‐moisture exchangers are most commonly used, in which gas flow is directed through a heated water bath prior to inspiration. (Fong, 2017) | A | |
| 12. There was no difference between HMES and HHS in terms of artificial airway obstruction, pneumonia, and mortality. the choice of humidifiers should be made according to the clinical context, trying to avoid possible complications and reaching the appropriate performance at lower costs (Vargas et al., 2017) | A | |
| 13. The use of either active heated humidifier or passive heat moisture exchange (HME), saline nebulizers, sprays humidification in all patients with a tracheostomy tube is recommended (Fong, 2017) | B | |
| 14. The airway humidification effect of continuous oxygen atomization inhalation is better than that of micro pump or infusion pump continuous dripping of humidifying liquid (Xinyang et al., 2015) | A | |
| 15. Continuous airway humidification can reduce the incidence of pneumonia in patients with tracheotomy(Jing & Hongying, 2016) | B | |
| 16. The effect of 0.45% sodium chloride solution on airway humidification is similar to that of water for sterilization injection, but the incidence of adverse events is low, and 0.45% sodium chloride solution is more suitable for airway humidification (Ruijuan, Wenjie, et al., 2015; Ruijuan, Zhe, et al., 2015) | A | |
| Airway Attraction | 17. It is recommended that endotracheal suctioning should be performed only when secretions are present, and not routinely(American Association for Respiratory Care, 2010) | A |
| 18. It is suggested that the duration of the suctioning event be limited to less than 15 s (American Association for Respiratory Care, 2010) | B | |
| 19. A tracheal catheter with subglottic suction is recommended to reduce the incidence of VAP and shorten the time of mechanical ventilation (Respiratory Therapeutics Group of Respiratory Medicine Branch of Chinese Medical Association, 2014a, 2014b) | A | |
| 20. Continuous oral suction and oral suction before turning over can reduce the incidence of VAP and prolong the time of VAP (Respiratory Therapeutics Group of Respiratory Medicine Branch of Chinese Medical Association, 2014a, 2014b) | B | |
| 21. The suction catheter should be inserted to the carina and then retracted 1–2 cm before suctioning is performed, or the length of the suction catheter is estimated by measuring an identical endotracheal tube (Hu et al., 2019) | A | |
| 22. Deep suctioning is necessary in patients with large amounts of secretions in the lower airways (Hu et al., 2019) | B | |
| 23. Perform suctioning at least every 8‐hr to reduce the risk of partial occlusion of the endotracheal tube and the accumulation of secretions (Hu et al., 2019) | B | |
| 24. Preoxygenation by the delivery of 100% oxygen for at least 30 s before and after the suctioning procedure is recommended to prevent a decrease in oxygen saturation, especially when the patient has a clinically important reduction in oxygen saturation with suctioning (Hu et al., 2019) | B | |
| Tracheostomy care | 25. The tracheotomy wound has to be kept clean and dry to prevent postincisional wound infection (Leyn et al.,2007) | B |
| 26. The inner cannula should be changed daily or more frequently if necessary (Fong, 2017) | B | |
| 27. Gauze dressings which are pre‐cut should be used, rather than cutting gauze squares, as frayed edges can be a potential source of infection (Le, 2017) | B | |
| 28. Patients with copious secretions often require frequent dressing changes to keep the skin dry and prevent maceration of tissue and skin break‐down (Le, 2017) | A | |
| Oral Care | 29. Oral hygiene care incorporating chlorhexidine mouthrinse or gel is effective in reducing the development of ventilator‐associated pneumonia in adults in intensive care. Regular oral hygiene care with chlorhexidine gluconate is recommended to all patients with mechanical ventilation (Hua et al., 2016) | A |
3.2. Determine review indicators and review methods
Based on the 29 best evidences finally determined, the evidence‐based nursing team developed 21 quality review indicators, including 3 structural indicators, 15 process indicators and 3 outcome indicators, and determined the object of review and data collection methods for each review indicator, as shown in Table 2.
TABLE 2.
Evidence‐based nursing review indicators and review methods for airway management in adult critically ill patients
| Review indicators | Review object | Review method |
|---|---|---|
| Indicator 1. The patient's tracheostomy wound appears red, tender, swollen, inflammation, smell, high skin temperature and yellow‐green secretions can be seen around the stoma, or the patient has fever, the nurse immediately informs the doctor. | Patient | View on‐site |
| Indicator 2. The patient has signs of infection at the tracheostomy site, follow the doctor's advice for bacterial culture. | Patient | View on‐site |
| Indicator 3. When the patient has decreased blood oxygen saturation, decreased blood oxygen partial pressure and frequent coughing and respiratory distress, the nurse should perform airway suction for the patient. | Patient | View on‐site |
| Indicator 4. When the patient needs to suck sputum, the airway pressure is low and the spontaneous breathing is weak, increase the cuff pressure appropriately. | Patient | View on‐site |
| Indicator 5. After the patient turns over, wipes the bath, and transfers, the nurse should re‐measure the cuff pressure. | Patient | View on‐site |
| Indicator 6. Patients who have established artificial airways undergo continuous oxygen humidification and follow the doctor's instructions to inhale 2–3 times per day. | Patient | View on‐site |
| Indicator 7. The artificial airway humidification fluid uses 0.45% sodium chloride solution for continuous airway humidification. | Patient | View on‐site |
| Indicator 8. When the patient has sputum in the airway, it should be sucked in time, and the sputum suction time is ≤15 s. Patients with no sputum or little sputum should perform a suction at least 8 hr. | Patient、nursing record sheet | View on‐site, Check nursing records |
| Indicator 9. Oral suction before turning over and after oral care. | Patient | View on‐site |
| Indicator 10. Establishment of artificial airway patients use subglottic suction tracheal tube. | Patient | View on‐site |
| Indicator 11. Use special tracheostomy gauze when changing dressings for tracheostomy wounds, and keep the skin at the tracheostomy site dry. | Patient | View on‐site |
| Indicator 12. Patients with mechanical ventilation use chlorhexidine mouthwash for oral care once for 6 hrr−8 hr. | Patient | View on‐site |
| Indicator 13. The nurse evaluates the skin condition of the patient's tracheotomy every day and keeps the wound clean and dry and replaces it at any time when it is contaminated. | Nurse | View on‐site |
| Indicator 14. Use a manual measurement cuff pressure gauge to monitor the airbag pressure every 6 ~ 8 hr and maintain it at 20 ~ 30 cm H2O. The inflation pressure should be higher than the ideal value 2 cm H2O during each measurement. | Nurse、nursing record sheet | View on‐site, Check nursing records |
| Indicator 15. When monitoring the cuff pressure, clean the water in the pressure measuring tube in time. | Nurse | View on‐site |
| Indicator 16. The nursing class monitors and records the cuff pressure once after the tracheotomy wound dressing is changed. | Nurse、nursing record sheet | View on‐site, Check nursing records |
| Indicator 17. Cuff pressure monitoring cannot use finger touch to determine the degree of inflation. | Nurse | View on‐site |
| Indicator 18. Nurses regularly evaluate airway humidification and adjust dynamically. | Nurse | View on‐site |
| Indicator 19. The patient has a large amount of secretions in the airway and the nurse needs to perform deep suction. | Nurse | View on‐site |
|
Indicator 20. The nurse needs to measure the length of the suction tube inserted into the patient's airway before suctioning (1) Insert into the carina and retract the suction tube 1–2 cm (2) Measure the same tracheal tube to estimate the length of the suction tube |
Nurse | View on‐site |
| Indicator 21. The nurse pre‐oxygenated the patient with pure oxygen for at least 30 s before and after suction | Nurse | View on‐site |
3.3. Review of baseline results
The baseline was to understand the current situation of airway management in the department. A total of 36 adult patients with artificial airway were included in the review, who were admitted to the neurosurgical intensive care unit of a level III first‐class hospital in Jingzhou, Hubei Province, China, from 30 June to 31 July 2020. At the same time, 25 NICU nurses were included as the subjects of baseline review. Questionnaire survey was conducted to evaluate the degree of mastery and implementation of airway management knowledge in critically ill patients. The baseline results show that, except for the compliance of review indicator 10 which is 71.43%, the compliance of most of the review indicators is low. The compliance of specific clinical review indicators is shown in Table 3; the qualified rate of airway management knowledge test was 44%, and the scores of knowledge, behaviour and attitude questionnaires are shown in Table 4.
TABLE 3.
Summary table of compliance with clinical review Indicators
| Review Indicators | Number of cases | Review result | Clinical compliance rate (%) | ||
|---|---|---|---|---|---|
| Y | N | NA | |||
| Indicator 1 | 36 | 1 | 14 | 21 | 6.67 |
| Indicator 2 | 36 | 0 | 10 | 20 | 0 |
| Indicator 3 | 36 | 6 | 20 | 4 | 23.07 |
| Indicator 4 | 36 | 2 | 28 | 0 | 6.67 |
| Indicator 5 | 36 | 0 | 30 | 0 | 0 |
| Indicator 6 | 36 | 11 | 19 | 0 | 36.67 |
| Indicator 7 | 36 | 0 | 30 | 0 | 0 |
| Indicator 8 | 36 | 14 | 16 | 0 | 46.67 |
| Indicator 9 | 36 | 0 | 30 | 0 | 0 |
| Indicator 10 | 36 | 8 | 21 | 1 | 27.59 |
| Indicator 11 | 36 | 0 | 23 | 7 | 0 |
| Indicator 12 | 36 | 0 | 28 | 2 | 0 |
| Indicator 13 | 50 | 8 | 42 | 0 | 16.00 |
| Indicator 14 | 50 | 22 | 28 | 0 | 44.00 |
| Indicator 15 | 50 | 0 | 0 | 0 | 0 |
| Indicator 16 | 50 | 8 | 42 | 0 | 16.00 |
| Indicator 17 | 50 | 35 | 14 | 1 | 71.43 |
| Indicator 18 | 50 | 2 | 48 | 0 | 4.00 |
| Indicator 19 | 50 | 6 | 44 | 0 | 12.00 |
| Indicator 20 | 50 | 0 | 0 | 0 | 0 |
| Indicator 21 | 50 | 0 | 43 | 7 | 0 |
Annotation Y: Compliance with review indicators.
N: Non‐compliance with review indicators.
NA: Not applicable.
Clinical compliance rate = Y cases (number of cases)/[total number of cases (number of cases)‐NA cases (number of cases)].
The number of samples for review indicators 13–21 is 25 × 2 = 50 (nursing responsibility working group +nursing auxiliary working group).
TABLE 4.
The scores of airway management knowledge, behaviour and attitude questionnaire in critically ill patients
| Project | Min | Max | Average ± standard deviation | Pass rate (%) |
|---|---|---|---|---|
| Knowledge | 6 | 80 | 54.64 ± 15.11 | 44 |
| Behaviour | 14 | 32 | 23.40 ± 5.715 | 20 |
| Attitude | 16 | 30 | 24.20 ± 4.865 | 84 |
3.4. Obstacles and facilitators
Based on the results of the baseline review, the evidence‐based team members performed obstacle factor analysis for the review indicators with low compliance and conducted obstacle analysis seminars, listed the review indicators with compliance <60%, analysed obstacle factors through the method of brainstorming and formulated corresponding action strategies, as shown in Table 5.
TABLE 5.
Obstacle factors, facilitating factors and action strategies in the care of adult critically ill patients
| Review Indicators | Obstacle factor | Facilitating factors | Action strategies |
|---|---|---|---|
| Indicator 1, 2, 12 | 1 Nurses lack awareness and knowledge of assessment | 1. There are many young nurses in the department with strong desire to learn | 1. Carry out artificial airway assessment training for nurses |
| 2. Doctors did not pay enough attention to airway management and did not cooperate well | 2. New business learning in the department, a better atmosphere for medical and nursing cooperation | 2. Strengthen the learning of airway knowledge in the department, establish an airway management team and take responsibility to people | |
| Indicator 3, 4, 7, 8, 9, 14, 18, 19 | 1. Nurses lack knowledge of airway management in critically ill patients | 1. After the COVID‐19 outbreak, the hospital has adopted various online and offline learning methods | 1. Carry out training on evidence‐based knowledge related to artificial airway for nurses |
| 2. Airway management knowledge is outdated and not updated in time | 2. Hospitals and universities have jointly purchased Chinese and English databases | 2. Encourage department nurses to actively consult literature, learn the latest knowledge, and train literature retrieval methods | |
| 3. Lack of systematic training for airway management | 3. Establish airway management plan and related procedures for adult critically ill patients | ||
| 4. Lack of a unified airway management process | |||
| Indicator 5, 13, 15, 16, 20 | 1. Nurses are busy | 1. The department has more nurses with standardized training | 1. Increase nursing human resources |
| 2. Standardized implementation and recording have increased the workload of nurses, and nurses are resistant | 2. The department is currently equipped with a bedside mobile nurse station | 2. Plans to put the mobile nurse station into use | |
| 3. Insufficient awareness of artificial airway nursing | 3. The department is carrying out multiple airway quality improvement projects | 3. Strengthen the supervision and guidance of managers | |
| Indicator 6, 10, 17 | 1. The department does not pay enough attention to airway humidification management | 1. Due to the relocation of the new hospital area, the hospital has a plan to strengthen the nursing quality management of the critical care department | 1. Strengthen the learning of airway humidification knowledge and establish airway humidification management procedures |
| 2. The department has not introduced subglottic catheter products | 2. The department of the new hospital district has plans to introduce related equipment, subglottic catheters and other products | 2. Introducing subglottic catheter products | |
| 3. Lack of leadership | 3. Leaders attach importance to airway management of critically ill patients | 3. Get support from leaders | |
| Indicator 11 | 1. The department lacks special gas switching medicine package products | 1. The departments of the new hospital area have the enthusiasm and action ability for standardized management and high‐quality nursing | 1. Introduce special gas switching medicine package products |
| 2. No special mouthwash is used in the department | 2. Explain the benefits of chlorhexidine mouthwash to the patient's family, and inform the patient's family to purchase a chlorhexidine mouthwash correctly |
4. DISCUSSION
4.1. The best evidence combined with clinical professional judgement is beneficial to the construction of quality review indicator
According to the FAME principle of evidence (Yan & Yufang, 2018) in the early stage of the study, 29 pieces of evidence were finally included from 7 aspects of airway management in adult critically ill patients. The content to be considered in the FAME principle mainly includes the following four aspects: (1) feasibility of evidence (F) : evidence that clinical intervention is physically, economically and culturally practical, what is the cost‐effectiveness of carrying out the practice and whether the required resources are available. (2) Appropriateness of evidence (A): whether the practice method is culturally acceptable in the environment, whether it is suitable for the situation and whether it can be used in most people. (3) The clinical significance of the evidence (M): whether the practice method is related to the positive experience of the patient and whether it will not cause the patient to have a bad experience. (4) Effectiveness of evidence (E): whether the practice can achieve the expected clinical effects and health outcomes, whether the practice is safe and whether it can be benefited. According to the collected evidence content and the actual situation of the NICU departments, the expert group screened out the evidence suitable for the NICU in Jingzhou level III first‐class Hospital, Hubei Province, China. In this study, the evaluators of the evidence were trained in the relevant evidence‐based training to ensure the reliability of the evidence.
4.2. Development of airway management review indicator and review method for adult critically ill patients according to evidence
In standardized evidence‐based practice, the formulation of review indicators should be based on the best available evidence in various fields, and the review indicators should be effective, relevant, feasible and flexible and closely fit with various stakeholders (Pearson & Jordan, 2007; Yingfeng et al., 2016). Scientific, normative and implementable review indicators will provide clear goals for researchers and practitioners and provide the basis for further development of action reform strategies (Boult et al., 2007). The review indicators should correspond to the summary of evidence, and the review indicators should be decomposed or combined according to the corresponding evidence, so as to make the quality review operable (Pearson & Jordan, 2007; Yan & Yufang, 2018). For example, evidence 1: the skin condition of the patient's tracheostomy should be assessed daily and cleaned according to the patient's needs. If there is redness, tenderness, swelling, inflammation, smell, high skin temperature, yellow‐green discharge around the stoma or fever in the patient, the clinician should be notified. If there are obvious signs of infection, it is recommended to provide culture/sensitive specimens (see Table 1). It can be broken down into 3 review indicators: 1. the patient's tracheostomy wound appears red, tender, swollen, inflammation, smell, high skin temperature and yellow‐green secretions can be seen around the stoma, or the patient has fever. 2. The patient showed signs of infection at the tracheotomy, and the nurse followed the doctor’s order to do a bacterial culture. 3. When the patient has decreased blood oxygen saturation, decreased blood oxygen partial pressure and frequent coughing and respiratory distress, the nurse should perform airway suction for the patient (see Table 2). For example, evidence 2: when blood oxygen saturation or partial pressure of oxygen decreases and evidence 3: when frequent coughing or respiratory distress syndrome occurs (see Table 1), these two pieces of evidence can be combined into one review indicator, that is review indicator 3: when the patient has decreased blood oxygen saturation, decreased blood oxygen partial pressure, and frequent coughing and respiratory distress, the nurse should perform airway suction for the patient. And so on, the team developed 21 review indicators based on 29 best evidences. The review method for the measurement indicators is also to choose an appropriate method according to the characteristics of the review indicator. In the study, for the behaviours of nursing operations, we chose to observe on‐site, and for evaluation and recording, we chose to view and consult the nursing record sheet. This is consistent with the establishment of report review indicators for other evidence‐based practice researches and the selection principles of corresponding review methods (Cao et al., 2019).
4.3. Analysis of clinical review indicator results of airway management in adult critically ill patients
It can be seen from the review results that, except for the review indicator 17, which is 71.43%, the compliance of the other 20 review results is poor (0%~44.00%, all <60%), and the knowledge test pass rate is only 44%. At the level of practitioners, clinical compliance is generally low, nursing staff have insufficient awareness of airway management in critically ill patients and lack of clinical operations. Most of the nursing staff lack evidence‐based knowledge of airway management in adult critically ill patients, which is related to the lack of training of airway management knowledge in departments and absence of evidence‐based knowledge. In practice, clinical nursing staff failed to actively consult relevant literature and learn the latest guidelines for airway management, resulting in obsolete relevant knowledge. This indicates that there is a large gap between the best evidence and clinical practice of airway management in critically ill adults.
4.4. Obstacle factors and countermeasures analysis of airway management review indicators in adult critically ill patients
Practice is the only way to implement evidence‐based reform, as a process of systematic reform, the application of evidence is bound to encounter obstacles at different levels. Therefore, it is necessary to evaluate the obstacles in the application of evidence and then formulate targeted action strategies. It can be seen from the system level that the department lacks the airway management process specification and medical equipment, and the airway management measures are single. At present, the department is carrying out a number of airway quality improvement projects, and the department of the new hospital has plans to introduce relevant instruments and equipment and other products, all of which are promoting factors at the system level. At the practitioner level, nursing staff's weak awareness of airway management and lack of knowledge in adult critically ill patients are the main obstacles, while leaders attach great importance to airway management, young nurses in departments and strong desire for learning, hospitals and universities have purchased Chinese and English databases, these are all promoting factors at the practitioner level. Therefore, using the many factors that currently exist in the department to formulate action strategies, it is required to actively carry out the training of evidence‐based knowledge about artificial airway for nursing staff, encourage department nurses to actively consult literature, learn the latest knowledge, and the department establishes airway management for adult critically ill patients standardize processes and introduce corresponding medical equipment, promote the development of evidence‐based best practices, and continuously improve clinical quality.
5. CONCLUSION
Airway management has always been the focus and difficulty of the intensive care unit, and it is also a hot spot for scholars at home and abroad. Effective airway management is an important guarantee to improve the treatment effect of critically ill patients, which can reduce the incidence of complications and shorten the length of hospital stay. The use of evidence‐based nursing methods to achieve airway management of adult critically ill patients is an inevitable choice for the development of clinical nursing in the future. This study completed the review of the status quo before the introduction of evidence into the clinic, ascertained the obstacles to the clinical application of the best evidence for airway management in adult critically ill patients and formulated corresponding solutions, which will be implemented in the next step in practice, complete the clinical application of the best evidence and ultimately achieve the goal of improving the clinical outcome of critically ill patients and improving the quality of clinical care.
6. ETHICAL CONSIDERATION
Ethical approval or individual consent was not applicable.
7. DATA AVAILABILITY STATEMENTS
The [DATA TYPE] data used to support the findings of this study are available from the corresponding author upon request.
CONFLICT OF INTEREST
No conflict of interest.
AUTHOR CONTRIBUTIONS
Yan Yujiao and Ding Juan made significant contributions to concept and design, literature retrieval, data acquisition, data analysis and drafting of manuscripts; Zeng Xurui contributed to data preparation, drafting of manuscripts and strict revision of important knowledge content; Wang Hong contributed to the revision and proofreading of the paper. In addition, all authors read and approved the final manuscript.
ACKNOWLEDGEMENT
The authors thank the evidence‐based nursing team, critical care management experts, hospital and NICU medical staff who participated in this study.
Yujiao Y, Juan D, Xurui Z, Hong W. Establishment of evidence‐based nursing review indicators for airway management of adult critical patients and analysis of obstacle factors. Nurs Open. 2021;8:3677–3687. 10.1002/nop2.898
Funding information
Funding Project: One of Jingzhou Central Hospital.
Yan Yujiao and Ding Juan are joint first authors.
REFERENCES
- American Association for Respiratory Care (2010). AARC clinical practice guidelines endotracheal suctioning of mechanically ventilated patients with artificial airways 2010. Respiratory Care, 55(6), 758–764. 10.1007/s12028-010-9333-6 [DOI] [PubMed] [Google Scholar]
- Boult, M. , & Maddern, G. J. (2007). Clinical audits: Why and for whom. ANZ Journal of Surgery, 77(7), 572–578. 10.1111/j.1445-2197.2007.04140.x [DOI] [PubMed] [Google Scholar]
- Branson, R. D. , Gomaa, D. , & Rodriquez, D. Jr (2014). Management of the artificial airway. Respiratory Care, 59(6), 974–990. 10.4187/respcare.03246 [DOI] [PubMed] [Google Scholar]
- Brouwers, M. C. , Kho, M. E. , Browman, G. P. , Burgers, J. S. , Cluzeau, F. , Feder, G. , Fervers, B. , Graham, I. D. , Grimshaw, J. , Hanna, S. E. , Littlejohns, P. , Makarski, J. , & Zitzelsberger, L. (2010). AGEREEⅡ:advancing guideline development, reporting and evaluation in health care. CMAJ, 182(18), E839–E842. 10.1503/cmaj.090449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao, R. , Fen, H. , Xiaoping, Z. , Jin, Y. , Wang, L. , Cheng, X. , Deng, L. , Cao, Z. , Ma, J. , Xiao, M. (2019). Establishment of review index for evidence‐based nursing of ICU patients with physical restraint and analysis of obstacle factors. Chinese Journal of Nursing, 54(04), 485–489. 10.3761/j.issn.0254-1769.2019.04.001 [DOI] [Google Scholar]
- Chan, R. J. , Bowers, A. , & Barton‐Burke, M. (2017). Organizational strategies for building capacity in evidence‐based oncology nursing practice: A case report of an australian tertiary cancer center. The Nursing Clinics of North America, 52(1), 149–158. 10.1016/j.cnur.2016.10.001 [DOI] [PubMed] [Google Scholar]
- Chinese Medical Association Neurosurgery Branch, China Neurosurgery Critical Care Management Cooperative Group . (2016). Expert consensus on airway management of critically ill patients in Chinese neurosurgery. Chin Med, 96(21), 1639–1642. 10.3760/cma.j.issn.0376-2491.2016.021.004 [DOI] [Google Scholar]
- Cook, T. M. , Woodall, N. , Harper, J. , & Benger, J. (2011). Major complications of airway management in the UK: Results of the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society. Part 2: Intensive care and emergency departments. British Journal of Anaesthesia, 106(5), 632–642. 10.1093/bja/aer059 [DOI] [PubMed] [Google Scholar]
- Dang, D. , & Dearholt, S. L. (2017). Johns Hopkins nursing evidence‐based practice: Model and guidelines. Indianapolis, Indiana: Sigma Theta Tau. [Google Scholar]
- De Leyn, P. , Bedert, L. , Delcroix, M. , Depuydt, P. , Lauwers, G. , Sokolov, Y. , Van Meerhaeghe, A. , & Van Schil, P. (2007). Tracheotomy: Clinical Review and Guidelines. European Journal of Cardio‐Thoracic Surgery, 32(3), 412–421. 10.1016/j.ejcts.2007.05.018 [DOI] [PubMed] [Google Scholar]
- DiCenso, A. , Bayley, L. , & Haynes, R. B. (2009). Accessing pre‐appraised evidence: Fine‐tuning the 5S model into a 6S model. Evidence‐Based Nursing, 12(4), 99–101. 10.1136/ebn.12.4.99-b [DOI] [PubMed] [Google Scholar]
- Donabedian, A. (1988). The quality of care. How can it be assessed? JAMA: The Journal of the American Medical Association, 260(12), 1743–1748. 10.1001/jama.260.12.1743. [DOI] [PubMed] [Google Scholar]
- Feng, D.‐Y. , Zhou, Y.‐Q. , Zhou, M. I. , Zou, X.‐L. , Wang, Y.‐H. , & Zhang, T.‐T. (2019). Risk factors for mortality due to ventilator‐associated pneumonia in a Chinese Hospital: A retrospective study. Medical Science Monitor, 25, 7660–7665. 10.12659/MSM.916356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fong, E. (2017). Tracheostomy: Management of patients.. http://ovidsp.dc2.ovid.com/sp‐4.02.0b/ovidweb.cgi?&S=PEJMFPBGBKEBPIJNIPCKCHEHCLCLAA00&Link+Set=S.sh.52%7c1%7csl_190 [Google Scholar]
- Guihua, H. , Hong, R. , Zhiying, Y. , Jiale, H. , & Leilei, Y. (2015). A literature survey on the current situation of domestic and foreign nurses implementing artificial airway suction ability. PLA Nursing Journal, 15:17‐19. 10.3969/j.issn.1008-9993.2015.15.005 [DOI] [Google Scholar]
- Hu, J. , Yu, L. , Jiang, L. , Yuan, W. , Bian, W. , Yang, Y. , & Ruan, H. (2019). Developing a guideline for endotracheal suctioning of adults with artificial airways in the perianesthesia setting in China. Journal of PeriAnesthesia Nursing, 34(1), 160–168.e164. 10.1016/j.jopan.2018.03.005 [DOI] [PubMed] [Google Scholar]
- Hua, F. , Xie, H. , Worthington, H. V. , Furness, S. , Zhang, Q. I. , & Li, C. (2016). Oral hygiene care for critically Ill patients to prevent ventilator‐associated pneumonia. Cochrane Database Systematic Review, 10(10), CD008367. 10.1002/14651858.CD008367.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyzy, R. C. (2018). Complications of the Endotracheal Tube Following Initial Placement: Prevention and Management in Adult Intensive Care Unit Patients. https://www.uptodate.com/contents/complications‐of‐the‐endotracheal‐tube‐following‐initialplacement‐prevention‐and‐managemet‐in‐adultintensive‐care‐unit‐patients
- Jing, W. , & Hongying, P. (2016). A Meta analysis of the effects of two different airway humidification methods on patients with tracheotomy. China Critical Care Medicine, 2016(1), 63–69. 10.3760/cma.j.issn.2095-4352.2016.01.012 [DOI] [Google Scholar]
- Jordan, Z. , Lockwood, C. , Aromataris, E. , & Munn, Z. (2016). The updated JBI model for evidence‐based healthcare. The Joanna Briggs Institute[EB/OL]. http://www.joannabriggs.org/jbi‐approach.html [DOI] [PubMed] [Google Scholar]
- Juan, L. (2017). Analysis of sputum suction complications in ICU patients with artificial airway and comparative study on the effect of different suction depths. Fourth Military Medical University. [Google Scholar]
- Le, L. K. (2017. ). Tracheostomy: Dressing. http://ovidsp.dc2.ovid.com/sp‐4.02.0b/ovidweb.cgi?&S=PEJMFPBGBKEBPIJNIPCKCHEHCLCLAA00&Link+Set=S.sh.46%7c1%7csl_190
- Lirong, Y. , & Shuhua, L. I. (2018). A study on improving the rate of compliance with suitable airbag pressure for patients with artificial airway. Chinese Nursing Management, 18(z1), 53–54. 10.3969/j.issn.1672-1756.2018z1.202 [DOI] [Google Scholar]
- Pearson, A. , Jordan, Z. (2007).Evidence‐based clinical practice in nursing and health care: assimilating research, experience and expertise. : Wiley‐Blackwell, 137–153. [Google Scholar]
- Pearson, A. , Wiechula, R. , Court, A. , & Lockwood, C. (2005). The JBI model of evidence‐based healthcare. International Journal of Evidence‐Based Healthcare, 3(8), 207–215. 10.1111/j.1479-6988.2005.00026.x [DOI] [PubMed] [Google Scholar]
- Picot, E. (2019). Tracheostomy: Stoma Care. http://ovidsp.dc2.ovid.com/sp‐4.02.0b/ovidweb.cgi?&S=HNEBFPAJHFEBPIFBIPCKCGEHNLGKAA00&Link+Set=S.sh.21%7c1%7csl_190
- Respiratory Therapeutics Group of Respiratory Medicine Branch of Chinese Medical Association . (2014). Expert consensus on attraction of adult airway secretions (draft). Chinese Journal of Tuberculosis and Respiratory, 37(11), 809–811. 10.3760/cma.j.issn.1001-0939.2014.11.004 [DOI] [Google Scholar]
- Respiratory Therapeutics Group of Respiratory Medicine Branch of Chinese Medical Association . (2014). Expert consensus on the management of artificial airway balloon (draft). Chin J Tuberc Respir Dis, 37(11), 816–819. 10.3760/cma.j.issn.1001-0939.2014.11.006 [DOI] [Google Scholar]
- Ruijuan, J. , Wenjie, L. , Zhengzheng, X. , & Yachao, Z. (2015). Meta analysis of the artificial airway humidification effect of 0.45% sodium chloride solution and sterile water for injection. CHIN MOD MED, 22(13), 4–7.CNKI:SUN:ZGUD.0.2015‐13‐003 [Google Scholar]
- Ruijuan, J. , Zhe, S. , & Yanzhi, Z. (2015). Meta analysis of the artificial airway humidification effect of different concentrations of sodium chloride solution. China Clinical Nursing, 7(4), 284–288. 10.3969/j.issn.1674-3768.2015.04.003 [DOI] [Google Scholar]
- Umobong, E. U. , & Mayo, P. H. (2018). Critical care airway management. Critical Care Clinics, 34(3), 313–324. 10.1016/j.ccc.2018.03.006 [DOI] [PubMed] [Google Scholar]
- Vargas, M. , Chiumello, D. , Sutherasan, Y. , Ball, L. , Esquinas, A. M. , Pelosi, P. , & Servillo, G. (2017). Heat and Moisture Exchangers (HMEs) and Heated Humidifiers (HHs) in adult critically Ill patients: a systematic review, meta‐analysis and meta‐regression of randomized controlled trials. Critical Care, 21(1), 123. 10.1186/s13054-017-1710-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xinyang, S. , Hongmei, X. , Meilin, W. , & Zhenzhu, L. (2015). Meta analysis of artificial airway humidification effect of continuous oxygen atomization inhalation and continuous drip infusion of humidification liquid. Nurs J Chin PLA, 32(20), 7–12. 10.3969/j.issn.1008-9993.2015.20.002 [DOI] [Google Scholar]
- Yan, H. U. , & Yufang, H. (2018). Evidence‐based nursing, 2nd ed. People's Medical Publishing House. [Google Scholar]
- Yan, X. U. , Weilin, S. , Liwei, L. , Peihong, S. , Xiaoli, Y. , & Yanpei, C. (2019). Evidence‐based nursing practice to reduce physical restraint of ICU patients. Chinese Journal of Nursing, 54(01), 19–24.CNKI:SUN:ZHHL.0.2019‐01‐005 [Google Scholar]
- Yi, P. U. , Zhi, Z. , Yan, W. , Chenyin, Q. , & Qiuyan, W. (2018). Analysis of pathogenic bacteria and influencing factors of lower respiratory tract infection in patients with artificial airway in intensive care unit. Chinese Journal of Nosocomial. Infection, 28(7), 991–993. 10.11816/cn.ni.2017-172742 [DOI] [Google Scholar]
- Yingfeng, Z. , Yan, H. , Ying, G. , Weijie, X. , & Zheng, Z. (2016). Promote evidence‐based best practices to continuously improve clinical quality. Nursing Research, 30(35), 4432–4434. 10.3969/j.issn.1009-6493.2016.35.025 [DOI] [Google Scholar]
- Yujiao, Y. , Juan, D. , Chaohan, L. , Mo, F. , & Hong, W. (2021). A review of the best evidence for airway management in critically ill adults. Journal of Nursing(China), 28(03), 39–45. 10.16460/j.issn1008-9969.2021.03.039 [DOI] [Google Scholar]
- Zheng, W. , Jiaming, W. , Wencheng, Y. , Yifeng, G. , & Aimin, G. (2015). Investigation on the status quo and evidence‐based practice attitude of ICU nurses in airway management. Chinese Nursing Management, 15(5), 563–566. 10.3969/j.issn.1672-1756.2015.05.015 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The [DATA TYPE] data used to support the findings of this study are available from the corresponding author upon request.


