Abstract
Background
Antiretroviral therapy (ART) has been shown to significantly reduce the likelihood of transmission to other people as well as promoting the health of people living with Human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS) (PLH). The purpose of this study was to assess the HIV care continuum of PLH in Korea using the national health insurance system (NHIS) database.
Materials and Methods
From 2006 to 2015, ART prescription/laboratory test claim data and enlisted accompanying comorbidities were extracted from the NHIS database. Utilizing these data, proportion of PLH on ART among those who registered to Korea Disease Control and Prevention Agency (KDCA), HIV viral load testing, prescription trends of ART, medication possession ratio (MPR) of ART, and accompanying comorbidities were reviewed. Factors related with MPR <90% was also investigated among demographic factors, ART prescription, and accompanying comorbidities.
Results
During the observation period, the number of people receiving ART prescription increased from 2,076 in 2006 to 9,201 in 2015. Considering the number of PLHs reported by the KDCA, the proportion of PLHs who received ART prescription increased from 55.4% to 87.6% during the study period. The median value of ART MPR increased from 76.4% to 94.2% and the proportion of patients with MPR >90% increased from 54.3% to 78.2%. The most commonly accompanying comorbidities were dyslipidemia (55.7%), osteoporosis (16.3%), hypertension (15.7%) and diabetes (13.7%), respectively. The proportion of PLH with two or more comorbid conditions increased from 22.0% to 31.6%. Regarding the factors associated with suboptimal compliance, age less than 50 years old, under support of National Medical Aid, alcoholic liver disease, mental and behavioral disorders due to use of alcohol, and ART regimen of protease inhibitor and non-single table regimen integrase strand transfer inhibitor were related with MPR <90%.
Conclusion
The proportion of PLHs who received ART prescription and median MPR of ART increased during the study period. However, proportion of patients with MPR >90% was 78.2% in 2015 and there are still much room for improvement in the aspect of compliance.
Keywords: HIV/AIDS, Care continuum, Antiretroviral therapy, Medication possession ratio, Comorbidity
Introduction
Recent scientific advances have shown that antiretroviral therapy (ART) not only preserves the health, quality of life, and life expectancy of people living with human immunodeficiency virus (PLH), but also enables PLH who take HIV-medicine as prescribed and keep an undetectable viral load to have effectively no risk of transmitting HIV to their HIV-negative sexual partners [1]. This can be accomplished through ensuring that everyone with HIV is aware of their infection, receives the treatment they need, and achieves sustained viral suppression targeting 90-90-90 of The Joint United Nations Programme on HIV/AIDS (UNAIDS) [2]. However, it was assessed that only 64.7% and 43% among PLH are virally suppressed in Unites States and Europe/Central Asia in 2018, respectively [3,4].
The estimated prevalence of HIV is relatively low in Korea as about 0.04% in 2020 [5]. However, annually more than 1,000 new cases are reported especially among young male individuals [6]. In a prior study, 70.4% had adequate adherence to ART defined as medication possession ratio (MPR) ≥95% among Korean PLH [7]. However, there are few data in the aspect of the HIV care continuum accomplishment in Korea. In this study, we aimed to evaluate the care continuum in Korea utilizing National Health Insurance Service (NHIS) from 2006 to 2015. Additionally, class of antiretroviral regimen and major comorbidities were also retrieved and their effect on suboptimal compliance were also investigated.
Materials and Methods
1. Setting
In Korea, it is mandatory for every healthcare provider and civilians to be registered to NHIS, social insurance scheme. Regular medical service for HIV management is also covered by NHIS. Although there are out-of-pocket payments for services covered by NHIS, medical expenditure for HIV care is actually for free since the out-of-pocket payment (10% of total cost) is reimbursed by the local government. 2.8% of general population with the lowest income is supported by National Medical Aid (NMA) and they do not pay the premiums for NHIS as well as exempted for out-of-pocket payments. Essentially, there is no difference between regular NHIS and NMA in the aspect that medical expenditure, and HIV care is fully covered without additional payment. Therefore, the barrier to access medical service for HIV is relatively low in Korea and NHIS claim database practically contains the information of all PLHs who are using medical services for HIV management. NHIS database contains not only clinical diagnoses, and prescriptions for medication or laboratory tests, but also basic sociodemographic characteristics such as age, sex, and insurance status of whether NHIS or NMA.
Every doctor should refer confirmatory test to governmental reference laboratories in case of reactive result of HIV screening test and also should report to the Korea Disease control and Prevention Agency (KDCA, former Korea Centers for Disease control and Prevention) if confirmed as HIV infection. While he or she can opt whether to provide the personal identification information to KDCA or not, reimbursement of 10% (out-of-pocket payments) for HIV care is available when registered to KDCA by one’s own name. Even though it is impossible to identify the exact proportion of people who had refused to provide personal information to KDCA, the proportion of non-reporting to KDCA among PLH would be very low considering that they should pay 10% of medical expense for HIV lifelong, about 1,000 USD per year. Furthermore, it is also mandatory to report the death of HIV infected individual. Therefore, the number of reported PLH in annual surveillance report of KDCA may very close to the real PLH population in Korea.
While the provision of specific antiretroviral drug to the market has been determined by the policy of pharmaceutical companies and approval of the Korea Ministry of Food and Drug Safety (MFDS, former Korea Food and Drug Administration), there has been no restriction in the decision of doctors in when to start and what to select among the registered antiretroviral drugs. The first guideline published by the Korean Society for AIDS in 2011 recommended initiation of ART if CD4+ T cell count is below 350 cells/mm3 and selectively if it is between 350 and 500 cells/mm3 such as HIV viral load is higher than 100,000 copies/mL [8]. In 2013, universal treatment policy regardless of CD4+ T cell count was adopted in the revised guideline [9].
2. The continuum of care
To investigate the care continuum of HIV in Korea, NHIS claim database between 2006 and 2015 was utilized. Among the three UNAIDS care continuum parameters of ‘awareness of infection’, ‘receipt of ART’, and ‘achievement of sustained viral suppression’, ‘awareness of infection’ is out of scope of this study. ‘Receipt of ART’ was selected as main target population of this study composed of the individuals whose medical expenditure for ART were claimed to NHIS with the diagnosis of B20 - 24, the Korean standard classification of disease and cause of death (KCD) -5 ~ 7 code which comprehensively represents HIV infection. Because the result of laboratory test is not available in NHIS database, the proportion of ‘viral suppression’ was unmeasurable. However, it has been known that ‘viral suppression’ is equivalent with that of ‘retention in care’ which is represented as repetitive viral load test with adequate interval [10,11,12,13] and individuals who got HIV RNA viral load test more than two times per year at least 60 days apart was regards as ‘retention in care’ in this study. The valid ‘retention in care’ data were available after 2010 because HIV viral load assay had been performed by KDCA irrespective of NHIS claim until July 2009. To investigate the proportion of ‘receipt of ART’ and ‘retention in care’ among diagnosed PLHs, annual number of PLHs of KDCA annual national HIV surveillance reports was used as denominators [14].
3. Accompanying comorbidities
To investigate the accompanying comorbidities of PLHs, the KCD-5 ~ 7 codes of major comorbidities were searched among the claim data of the ART receipt population. Included disease entities are Diabetes mellitus (E10~E14), Hypertensive diseases (I10 ~ I15), Disorders of lipoprotein metabolism and other lipidaemias (E78), Osteoporosis (M80 ~ M82), Chronic kidney disease (N18 ~ N19), Viral hepatitis (B15 ~ B19), Diseases of liver (K70 ~ K77), and Mental and behavioural disorders due to use of alcohol (F10). If the disease codes were identified at least once each year, PLHs was considered to have the diseases.
4. ART prescription pattern
To investigate prescription trends of ART during the study period, all Korea MFDS registered ART drugs were analyzed. Considering that standard ART regimen is composed of two nucleoside/nucleotide reverse transcriptase inhibitors (NRTIs) and one anchor drug such as non-NRTI (NNRTI), protease inhibitor (PI), and integrase strand transfer inhibitor (INSTI), number of individuals who got prescription for specific anchor drug class was assessed. Ritonavir was not regarded as anchor drug of PI because it had been used only for boosting other PIs. The first single table regimen (STR) of Korea, elvitagravir/cobicistat/emtricitabine/tenofovir diproxil fumarte was introduce in 2014 followed by dolutegravir/lamivudine/abacavir in 2015 and these two STRs were grouped as INSTI STR separate from non-STR INSTI, raltegravir for the analysis about STR.
5. Adherence measurements and factors associated with suboptimal adherence
To evaluate the adherence of study population, ART prescription details of every individual was analyzed by yearly cohort. MPR by percent was used for adherence assessment, which is the sum of the supply days of ART in an index year divided by 365. Considering that ART is prescribed usually every three or four months, in case the last refill of prior year had not run out on the first day of the index year, remaining medication duration after the first day of the year was included to the supply days. In case the supply duration of the last prescription of index year exceeds the last day of the year, supply days before the end of year was included in the supply days.
Suboptimal adherence was defined as MPR of less than 90 percent and annual trends were investigated. To identify the factors associated with suboptimal adherence in the recent period, 2015 ART adherence data were analyzed regarding sex, age, status of medical insurance, ART anchor class, and comorbidities influencing compliance such as alcoholic liver disease (K70), chronic kidney disease (N18), fibrosis and cirrhosis of liver (K74), and mental and behavioural disorders due to use of alcohol (F10). ART anchor class was divided as PI, NNRTI, non-STR INSTI, and STR INSTI.
6. Statistical analysis
Chi-squared test was applied to compare categorical variables between two groups (under 90% MPR vs. over 90% MPR) while t-test was performed for continuous variables. A multivariate logistic regression analysis was conducted to assess the association between risk factors and suboptimal medication adherence (under 90% MPR). Statistical significance was determined at 95% confidence level (P-value <0.05). All Statistical analyses were performed by SAS 9.4 (SAS Institute, NC, USA).
Results
1. The continuum of care
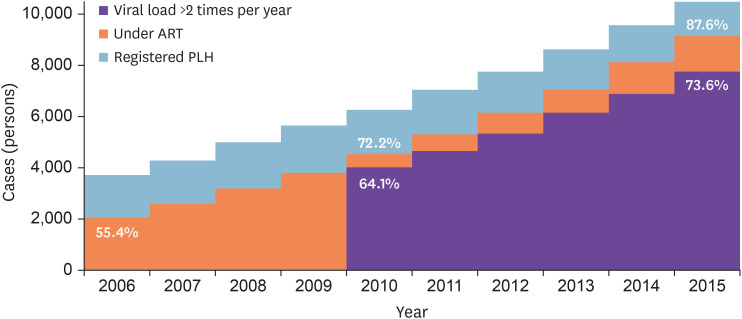
During the study period, study population who got prescription for ART with the diagnosis of HIV infection increased from 2,076 in 2006 to 9,201 in 2015 (Fig. 1) and the ‘receipt of ART’ proportion also increased from 55.4% in 2006 to 87.6% in 2015 considering the number of PLHs who had been registered to KDCA. The proportion of ‘retention in care’ calculated by HIV RNA viral load test more than two times per year at least 60 days apart increased from 64.1% in 2010 to 73.6% in 2015. Among the ‘receipt of ART’ group, male comprised 91.0% and this ratio was relatively constant during the study period. Overall mean age increased from 42.9 in 2006 to 44.6 in 2015. (Supplementary Fig. 1) While that of male was greater by 0.1 year in 2006, females were older by 4.2 years in 2015. Proportion of age over 50 was 47.7% in female in 2015 and it was 34.5% in male (data not shown). While the proportion of ‘receipt of ART’ was higher in female, the gap between female and male decreased from 13.9% in 2006 to 7.8% in 2015. The proportion of people who supported by NMA among the ‘receipt of ART’ population decreased from 30.1% to 19.0% during the study period (data not shown).
Figure 1. Proportion of under ART and regular HIV viral load testing.
ART, antiretroviral therapy; HIV, human immunodeficiency virus; PLH, people living with human immunodeficiency virus.
2. Accompanying comorbidities
Throughout the study period, most commonly accompanying comorbidities were dyslipidemia (55.7% of total people with ART prescription in 2015) followed by liver disease (21.7%) and hypertension (15.7%, Table 1). While dyslipidemia and hypertension are relatively homogenous disease entity, liver disease is very heterogenous from fatty liver (K70.6) to Hepatic failure, not elsewhere classified (K70.2), and further detail disease entities was investigated (Supplementary Table 1). Throughout the observation period, fatty liver was most common liver disease and its prevalence among PLH increased from 9.0% (187 cases out of 2,076 PLH in 2006) to 17.1% (1,571 cases out of 9,201 PLH in 2015). Besides fatty liver, the prevalence of all liver disease entities decreased. The increase in comorbidity prevalence was also most prominent in dyslipidemia (9.2%) followed by osteoporosis (8.6%). While osteoporosis in male was less than 1% before 2010, it reached 9.2% in 2015 and that of female increased form 3.9% in 2006 to 16.3% in 2015. The proportion of individuals with two or more comorbid conditions increased from 22.0% to 31.6% during the study period.
Table 1. Prevalence of accompanying comorbidities among PLH under ART (%).
| 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | Differencea | Increase Ratioa | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Diabetes mellitus | 11.8 | 11.9 | 10.9 | 15.0 | 15.8 | 14.6 | 14.5 | 14.0 | 13.6 | 13.8 | 2.0 | 1.17 | |
| Hypertension | 10.0 | 11.0 | 11.8 | 12.9 | 13.9 | 12.9 | 14.5 | 15.7 | 15.8 | 15.7 | 5.7 | 1.57 | |
| Dyslipidemia | 46.5 | 46.7 | 45.0 | 44.2 | 44.7 | 40.5 | 46.2 | 51.5 | 55.2 | 55.7 | 9.2 | 1.20 | |
| Osteoporosis | |||||||||||||
| Male | 0.8 | 1.1 | 0.9 | 0.8 | 1.0 | 2.5 | 5.4 | 6.4 | 7.2 | 9.2 | 8.4 | 11.50 | |
| Female | 3.9 | 3.0 | 5.1 | 8.4 | 8.1 | 9.3 | 10.9 | 13.7 | 12.6 | 16.3 | 12.4 | 4.18 | |
| Overall | 1.1 | 1.3 | 1.2 | 1.5 | 1.7 | 3.1 | 5.9 | 7.0 | 7.6 | 9.7 | 8.6 | 8.82 | |
| Chronic kidney disease | 0.9 | 0.7 | 0.5 | 0.7 | 0.7 | 0.7 | 0.8 | 0.9 | 1.0 | 1.1 | 0.2 | 1.22 | |
| Liver disease | 17.4 | 17.6 | 16.3 | 15.4 | 16.0 | 15.5 | 16.0 | 20.9 | 23.1 | 21.7 | 4.3 | 1.25 | |
| Viral hepatitis | 10.4 | 11.9 | 8.4 | 8.2 | 8.3 | 8.5 | 9.3 | 7.2 | 6.9 | 6.8 | −3.6 | 0.65 | |
| Alcohol dependency | 0.5 | 0.6 | 0.5 | 0.6 | 0.6 | 0.7 | 0.8 | 0.8 | 0.8 | 0.7 | 0.2 | 1.40 | |
| Comorbidities ≥2 | 22.0 | 24.5 | 20.9 | 23.1 | 25.2 | 22.8 | 25.4 | 28.7 | 30.8 | 31.6 | 9.6 | 1.44 | |
aValues were measure between 2006 and 2015.
PLH, people living with HIV/AIDS; ART, antiretroviral therapy.
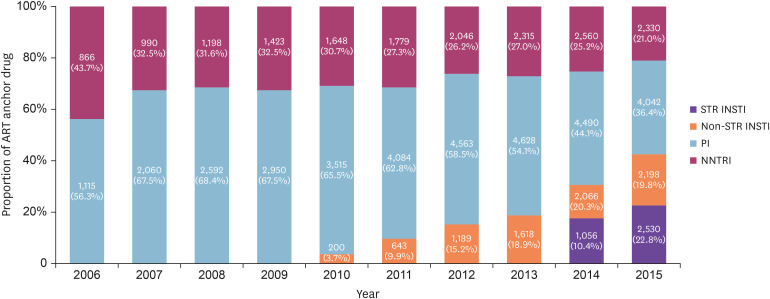
3. ART prescription pattern
Before the introduction of first INSTI, Raltegravir in 2010, PI and NNRTI were unique ART anchor drug classes. PI was more frequently prescribed than NNRTI throughout the study period and it reached to peak as 68.4% in 2008 (Fig. 2). However, after the introduction of INSTI, its proportion increased stiffly. Additionally, first STR in Korea elvitegravir/cobicistat/emtricitabine/tenofovir disoproxil fumarate was introduced in 2014 and it also belonged to INSTI. As a result, INSTI became most commonly prescribe anchor drugs (42.6%) in 2015 while PI and NNRTI comprised 36.4% and 21.0% in 2015, respectively. INSTI based single tablet regimens composed of 53.5% among INSTIs and 22.8% of all anchor drugs in 2015.
Figure 2. Proportion ART anchor drugs during the study period.
ART, antiretroviral therapy; STR INSTI, single tablet regimen integrase strand transfer inhibitor; PI, protease inhibitor; NNRTI, non-nucleoside reverse-transcriptase inhibitors.
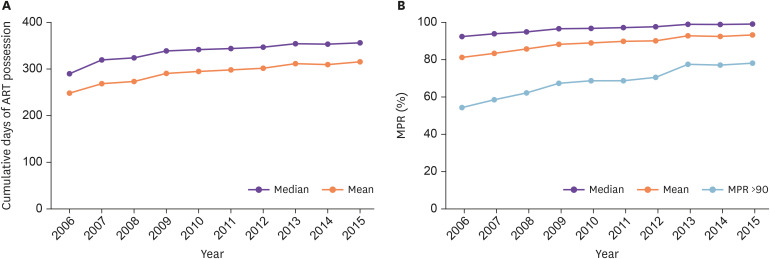
4. Adherence measurements factors associated with suboptimal adherence
Median value of cumulative days of ART possession by year increased from 291 (interquartile range [IQR] 145, 355) in 2006 to 357 (IQR 302, 370) in 2015 (Fig. 3) and it was not different by gender (P-value = 0.6190). Median MPR also increased from 92.3% (IQR 71.5, 100.0) to 99.2 (IQR 92.3, 102.5). However, proportion of PLH with MPR of more than 90% was 54.3% in 2006 and it increased just to 78.2% in 2015. Regarding the factors associated with MPR of less than 90%, age over 50 years old (crude odds ratio [cOR] 0.784), under support of NMA (cOR 1.317), Alcoholic liver disease (aOR 2.339), mental and behavioral disorders due to use of alcohol (cOR 2.683), and ART regimen of PI (cOR 1.664) and non STR INSTI (cOR 1.243) compared to INSTI STR revealed significant relationship with suboptimal adherence in univariate analysis (Table 2). Multivariate analysis revealed same trends and age group 30 - 39 was more prone to suboptimal adherence of MPR less than 90% (adjusted OR 1.216) compared with 40 - 49 group (Basic characteristics of the 2015 year cohort in 2015 was presented in Supplementary Table 2).
Figure 3. Cumulative days of ART possession (A) and MPR (B) increased during the study period. However, proportion of people living with human immunodeficiency virus with MPR of more than 90% was 54.3% in 2006 and it increased just to 78.2% in 2015 (B).
ART, antiretroviral therapy; MPR, medication possession ratio.
Table 2. Factors related with MPR <90% obtained from 2015 data.
| Crude odds ratio (95% CI) | Adjusted odds ratio (95% CI) | ||
|---|---|---|---|
| Gender | |||
| Male | 0.955 (0.797, 1.144) | 0.942 (0.773, 1.148) | |
| Female (ref) | |||
| Age | |||
| <30 | 0.959 (0.820, 1.122) | 1.184 (0.997, 1.407) | |
| 30 - 39 | 1.079 (0.940, 1.238) | 1.216 (1.047, 1.411)a | |
| 40 - 49 (ref) | |||
| ≥50 | 0.784 (0.691, 0.889)a | 0.763 (0.665, 0.875)a | |
| National Medical Aid | |||
| Covered by NHI (ref) | |||
| National Medical Aid | 1.317 (1.167, 1.486)a | 1.318 (1.151, 1.509)a | |
| Comorbidities | |||
| No comorbidity (ref) | |||
| Alcoholic liver disease | 2.339 (1.567, 3.492)a | 1.825 (1.158, 2.879)a | |
| Chronic kidney disease | 0.741 (0.439, 1.252) | 0.806 (0.449, 1.448) | |
| Fibrosis and cirrhosis of liver | 1.568 (0.885, 2.778) | 1.524 (0.811, 2.864) | |
| Mental and behavioural disorders due to use of alcohol | 2.683 (1.602, 4.343)a | 2.156 (1.227, 3.790)a | |
| Antiretroviral therapy regimen | |||
| STR INSTI (ref) | |||
| NNRTI | 1.098 (0.930, 1.295) | 1.179 (0.996, 1.396) | |
| PI | 1.664 (1.447, 1.912)a | 1.322 (1.113, 1.571)a | |
| Non STR INSTI | 1.243 (1.051, 1.470)a | 1.792 (1.549, 2.073)a | |
aSignificant at the 5% level (P-value <0.05).
Crude odds ratio was estimated by univariate logistic regression for each variable.
Adjusted odds ratio was estimated by multivariate logistic regression with gender, age, national medical aid, comorbidities, and antiretroviral therapy.
MPR, medication possession ratio; CI, confidence interval; ref, reference; NHI, national health insurance service; STR INSTI, single tablet regimen integrase strand transfer inhibitor; NNRTI, non-nucleoside reverse-transcriptase inhibitors; PI, protease inhibitor.
Discussion
In this study, we estimated the ‘receipt of ART’ and ‘retention in care’ among PLH in Korea. The ‘receipt of ART’ proportion increased from 55.4% in 2006 to 87.6% in 2015 and the ‘retention in care’ also increased from 64.1% in 2010 to 73.6% in 2015 among the PLHs who had been reported to KDCA. In 2015, the ‘receipt of ART’ and ‘retention in care’ among diagnosed PLHs in Unites States were 73.4% and 57.2%, respectively [10]. Among European Union countries, those of 2016 were 86.9% and 77.3% [15]. Considering that those of Korea in 2015 were 87.6% and 73.6%, the accessibility to HIV care and ART of Korea was fair among developed countries in 2015.
Recently, the number of PLHs and people who got HIV diagnosis in Korea in 2015 were estimated as 14,880 and 8,666 respectively by mathematical modelling and the proportion of diagnosis was estimated as 58.23% [5]. Considering those of Unites States and European Union were 86% and 84%, Korea is far from the first UNAIDS 90-90-90 target. The reason for low diagnostic rate was suggested as lack of voluntary testing [5] and the diagnostic rate of 2020 was estimated as 62.53%. Applying this data, 90-90-90 of Korea in 2015 was 58-51-43. Considering the those of Unites States and European Union were 86-63-51 and 84-73-65, Korea should focus of the increase of diagnostic rate.
Regarding the comorbidities, the prevalence data may not exactly represent study population because our results are based on the diagnosis codes included in claim data for reimbursement form NHIS. In some instances, diagnosis code enlisting is condition for reimbursement of diagnostic tests and physicians put presumptive diagnosis in the medical records and claim documents. For example, the prevalence of dyslipidemia of PLH in 2015 was 55.7% in our study. However, that from the Korea HIV/AIDS Cohort reported in 2019 was 18.8% [16] and that of Korean Nationwide data of male age over 30 from Korea National Health and Nutrition Examination Survey (KNHANES) of 2015 was 24.6% for hypercholesterolemia and 16.5% for hypertriglyceridemia [17]. The prevalence of diabetes was 13.8% and it is similar with general population [17,18]. However, while hypertension prevalence (15.7%) was similar with that of diabetes (13.8%) in our study, those of general population were 32.7% and 11.0%, respectively in 2015 [17]. Those of Korea HIV/AIDS Cohort were 12.0% and 7% [16] and it is unclear why the prevalence of hypertension is relatively low in our study. Regarding osteoporosis, the prevalence of male and female were 9.2% and 16.3% in 2015, respectively. While that of female increased gradually as 3.9% (2006), 9.3% (2011), and 16.3% in 2015, it increased stiffly from 1.0% in 2010 to 9.2% in 2015. This may be related with the introduction of Truvada containing tenofovir disoproxil fumarate in 2011 which may lower bone mineral density as adverse effect what may have led to more frequent prescription for measuring bone mineral density to relatively young male PLHs who had not been considered as high risk for osteoporosis. However, the prevalence of osteoporosis was reported as 12.9% in 2013, even among the Korean PLHs who had never been exposed to tenofovir [19]. Additionally, considering that prevalence of osteoporosis of general population male and female age of 50 were 7.5% and 37.3% in 2011 [20], it is likely that osteoporosis had been still underdiagnosed in female PLHs. Liver disease was the second most common comorbidity. Liver disease consists of 8 categories (Supplementary Table 1) and fatty liver is the most common one. The prevalence of fatty liver increased stiffly from 9% in 2006 to 17.1% in 2015 and those of all other categories of liver disease decreased such as other inflammatory liver diseases (liver abscess), fibrosis and cirrhosis of liver except for liver disorders in diseases classified elsewhere. Therefore, increase in the prevalence of overall ‘liver disease’ is solely owed to the increase in fatty liver. Additionally, another comorbidity entity ‘viral hepatitis’ also decreases from 10.4% to 6.8% during the study period [21].
It has been known that MPR is strongly associated with virologic outcomes [22] and the World Health Organization has recommended that adherence be routinely monitored at the clinic level, with a target of at least 90% adherence to minimize the risk of HIV drug resistance [23]. As mentioned before, all medical expenditure including tests and treatment associated with HIV care is fully reimbursed in Korea. While median MPR for ART is 99.2% in 2015, there are clear gaps to be filled considering that proportion of PLH with MPR of more than 90% was just 78.2% in 2015. In our study, age of 30 - 39 (compared than 40 - 49), under support of NMA, Alcoholic liver disease, Mental and behavioural disorders due to use of alcohol, and ART with PI or Non STR INSTI (compared than STR INSTI) were associated with MPR less than 90%. In a prior study, MPR over 95% was identified as 70.4% among the 8,501 newly diagnosed HIV-infected individuals during 2009 - 2016 in Korea [7] and requiring prophylactic antibiotics, female gender, age of 0 - 19 and same or over 50s compared to 30 - 39, and having a history of malignancy, lower socioeconomic status, not visiting tertiary hospital, and being diagnosed in the earlier years were risk factors for lower adherence. While risk factors as lower socioeconomic status, diagnosed in the earlier years are consistent with our study, female gender was not significant and age over 50 (compared than 40 - 49), was associated with MPR over 90% in our study. Regarding age and adherence, there have been discrepancies between studies and this may be associated with different target populations and categorization of age groups [24]. However, there were previous studies that reported reasons for poor adherence among young people as denial and fear of HIV infection, low self-esteem, and unstructured and chaotic lifestyles [25,26].
STR is preferred by patients for convenience and a few studies have shown that STR either maintains or increases treatment adherence [27,28,29]. Regarding the association of low adherence and PI based regimen but not NNRTI, it may be related with the attribute of PI class, the high genetic barrier for resistance and a low rate of treatment-emergent resistance. To the contrary, NNRTI, especially efavirenz and rilpivirine, have low barriers to resistance and it has been known that resistances may be acquired at the time of virologic failure compromising other NNRTIs such as etravirine or doravirine [30]. It is likely that PLHs with low adherence have already acquired resistances and physicians may have chosen PI and avoided NNRTI in these individuals.
It has been well known that current heavy drinking is more common among PLH than the general population [31], and at-risk alcohol use is associated with antiretroviral treatment non-adherence [32]. Alcohol dependency should be included in the HIV care policy making considering its harmful effect and that the prevalence is not decreasing in our data (Table 1).
The main limitations of our study are that we utilized registered PLHs to KDCA as number of by one's own name as ‘awareness of infection’. Let alone the individuals who are aware of HIV through only anonymous test and never visit hospital, PLHs who refuse to register to KDCA and pay 10% of medical expenditure are not included in KDCA register. To include this population, PLH who got medical service with the diagnosis of B20 - 24 regardless of ART prescription should be included in the population of HIV diagnosis as well as who did not get ART by their own decision or not fulfilling the contemporary standard for ART. However, this population data was not utilized because the number of this population was unrealistically bigger than that of total PLH registered to KDCA and this phenomenon was unexplainable despite extensive scrutinization. Additionally, we used diagnosis codes included in claim data for reimbursement and the comorbidity prevalence data may not exactly represent the study population for various reasons. Regarding the correlation between comorbidities and adherence, reverse causality cannot be excluded, especially for chronic kidney disease and osteoporosis.
In conclusion, the proportion of PLHs who received ART increased from 55.4% in 2006 to 87.6% in 2015 and median MPR also increased from 92.3% to 99.2% during the study period. However, proportion of PLH with MPR of more than 90% was just 78.2% in 2015 and age less than 50 years old, under support of NMA, alcoholic liver disease, mental and behavioral disorders due to use of alcohol, and ART regimen of PI and non STR INSTI were related with MPR of less than 90%.
Footnotes
Funding: This study was supported by Research fund of the Korean Society of Infectious Diseases.
Conflict of Interest: No conflicts of interest.
- Conceptualization: BSC.
- Data curation: BSC.
- Formal analysis: YMC.
- Methodology: BSC, YMC.
- Software: YMC.
- Supervision: BSC.
- Writing - original draft: BSC.
- Writing - review & editing: BSC, YMC.
SUPPLEMENTARY MATERIALS
Accompanying comorbidities among PLH under ART
Basic characteristics of 2015 year cohort utilized for suboptimal adherence analysis
Sex and age, proportion under ART.
References
- 1.Rodger AJ, Cambiano V, Bruun T, Vernazza P, Collins S, Degen O, Corbelli GM, Estrada V, Geretti AM, Beloukas A, Raben D, Coll P, Antinori A, Nwokolo N, Rieger A, Prins JM, Blaxhult A, Weber R, Van Eeden A, Brockmeyer NH, Clarke A, Del Romero Guerrero J, Raffi F, Bogner JR, Wandeler G, Gerstoft J, Gutiérrez F, Brinkman K, Kitchen M, Ostergaard L, Leon A, Ristola M, Jessen H, Stellbrink HJ, Phillips AN, Lundgren J PARTNER Study Group. Risk of HIV transmission through condomless sex in serodifferent gay couples with the HIV-positive partner taking suppressive antiretroviral therapy (PARTNER): final results of a multicentre, prospective, observational study. Lancet. 2019;393:2428–2438. doi: 10.1016/S0140-6736(19)30418-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.UNAIDS. 90-90-90: an ambitious treatment target to help end the AIDS epidemic. [Accessed 17 February 2021]. Available at: https://www.unaids.org/en/resources/909090.
- 3.Centers for Disease Control and Prevention (CDC) HIV Surveillance report. Supplemental report Volume 25, Number 2: Monitoring selected HIV prevention and care objectives using surveillance data, United States and 6 dependent areas, 2018. [Accessed 17 February 2021]. Available at: https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-supplemental-report-vol-25-2.pdf.
- 4.Brown AE, Hayes R, Noori T, Azad Y, Amato-Gauci AJ, Pharris A, Delpech VC The Ecdc Dublin Declaration Monitoring Network. HIV in Europe and Central Asia: progress in 2018 towards meeting the UNAIDS 90-90-90 targets. Euro Surveill. 2018;23:1800622. doi: 10.2807/1560-7917.ES.2018.23.48.1800622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee E, Kim J, Lee JY, Bang JH. Estimation of the Number of HIV Infections and Time to Diagnosis in the Korea. J Korean Med Sci. 2020;35:e41. doi: 10.3346/jkms.2020.35.e41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yoo M, Seong J, Yoon JG, Cha JO, Chung YS, Kim K, Kee MK. Characteristics of adolescents and young adults with HIV in the Republic of Korea from 2010 through 2015. Sci Rep. 2020;10:9384. doi: 10.1038/s41598-020-66314-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim J, Lee E, Park BJ, Bang JH, Lee JY. Adherence to antiretroviral therapy and factors affecting low medication adherence among incident HIV-infected individuals during 2009-2016: A nationwide study. Sci Rep. 2018;8:3133. doi: 10.1038/s41598-018-21081-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.The Korean Society for AIDS. Clinical guidelines for the diagnosis and treatment of HIV/AIDS in HIV-infected Koreans. Infect Chemother. 2011;43:89–128. [Google Scholar]
- 9.Korean Society for AIDS. The 2013 clinical guidelines for the diagnosis and treatment of HIV/AIDS in HIV-infected Koreans. Infect Chemother. 2013;45:455–461. doi: 10.3947/ic.2013.45.4.455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention (CDC) Selected national HIV prevention and care outcomes. [Accessed 17 February 2021]. Available at: https://www.cdc.gov/hiv/pdf/library/slidesets/cdc-hiv-prevention-and-care-outcomes.pdf.
- 11.Rebeiro PF, Althoff KN, Lau B, Gill J, Abraham AG, Horberg MA, Kitahata MM, Yehia BR, Samji H, Brooks JT, Buchacz K, Napravnik S, Silverberg MJ, Rachlis A, Gebo KA, Sterling TR, Moore RD, Gange SJ North American AIDS cohort collaboration on research and design. Laboratory measures as proxies for primary care encounters: implications for quantifying clinical retention among HIV-infected adults in North America. Am J Epidemiol. 2015;182:952–960. doi: 10.1093/aje/kwv181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mugavero MJ, Westfall AO, Zinski A, Davila J, Drainoni ML, Gardner LI, Keruly JC, Malitz F, Marks G, Metsch L, Wilson TE, Giordano TP Retention in Care (RIC) Study Group. Measuring retention in HIV care: the elusive gold standard. J Acquir Immune Defic Syndr. 2012;61:574–580. doi: 10.1097/QAI.0b013e318273762f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Poteat T, Hanna DB, Rebeiro PF, Klein M, Silverberg MJ, Eron JJ, Horberg MA, Kitahata MM, Mathews WC, Mattocks K, Mayor A, Rich AJ, Reisner S, Thorne J, Moore RD, Jing Y, Althoff KN. Characterizing the human immunodeficiency virus care continuum among transgender women and cisgender women and men in clinical care: a retrospective time-series analysis. Clin Infect Dis. 2020;70:1131–1138. doi: 10.1093/cid/ciz322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Korea Disease Control and Prevention Agency (KDCA) The yearbook of surveillance for HIV/AIDS in the South Korea. [Accessed 17 February 2021]. Available at: http://www.kdca.go.kr/npt/biz/npp/portal/nppPblctDtaMain.do.
- 15.European Centre for Disease Prevention and Control (ECDC) Thematic report: continuum of HIV care. 2017. [Accessed 17 February 2021]. Available at: https://www.ecdc.europa.eu/en/publications-data/thematic-report-continuum-hiv-care.
- 16.Choi Y, Choi BY, Kim SM, Kim SI, Kim J, Choi JY, Kim SW, Song JY, Kim YJ, Park DW, Kim HY, Choi HJ, Kee MK, Shin YH, Yoo M. Epidemiological characteristics of HIV infected Korean: Korea HIV/AIDS Cohort Study. Epidemiol Health. 2019;41:e2019037. doi: 10.4178/epih.e2019037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kweon S, Kim Y, Jang MJ, Kim Y, Kim K, Choi S, Chun C, Khang YH, Oh K. Data resource profile: the Korea national health and nutrition examination Survey (KNHANES) Int J Epidemiol. 2014;43:69–77. doi: 10.1093/ije/dyt228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Korean Diabetes Association (KDA) Diabetes fact sheet in Korea. 2018. [Accessed 17 February 2021]. Available at: https://www.diabetes.or.kr/pro/news/admin.php?code=admin&category=A&number=1546&mode=view.
- 19.Kim HS, Chin BS, Shin HS. Prevalence and risk factors of low bone mineral density in Korean HIV-infected patients: impact of abacavir and zidovudine. J Korean Med Sci. 2013;28:827–832. doi: 10.3346/jkms.2013.28.6.827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Korean Society for Bone and Mineral Research. Osteoporosis and osteoporotic fracture fact sheet. 2017. [Accessed 17 February 2021]. Available at: https://www.ksbmr.org/bbs/index.html?code=fact&category=&gubun=&page=1&number=700&mode=view&keyfield=&key=
- 21.Kim YC, Ahn JY, Kim JM, Kim YJ, Park DW, Yoon YK, Song JY, Kim SW, Lee JS, Choi BY, Choi YS, Choi JY, Han MG, Kang C, Choi JY. Human immunodeficiency virus (HIV) and hepatitis virus coinfection among HIV-infected Korean patients: The Korea HIV/AIDS cohort study. Infect Chemother. 2017;49:268–274. doi: 10.3947/ic.2017.49.4.268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Goldman JD, Cantrell RA, Mulenga LB, Tambatamba BC, Reid SE, Levy JW, Limbada M, Taylor A, Saag MS, Vermund SH, Stringer JS, Chi BH. Simple adherence assessments to predict virologic failure among HIV-infected adults with discordant immunologic and clinical responses to antiretroviral therapy. AIDS Res Hum Retroviruses. 2008;24:1031–1035. doi: 10.1089/aid.2008.0035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.World Health Organization (WHO) Meeting report on assessment of World Health Organization HIV drug resistance early warning indicators: report of the Early Advisory Indicator Panel meeting, 11-12 August 2011, Geneva, Switzerland. [Accessed 17 February 2021]. Available at: https://apps.who.int/iris/handle/10665/75186.
- 24.Desta AA, Kidane KM, Woldegebriel AG, Ajemu KF, Berhe AA, Zgita DN, Teweldemedhn LW, Woldegebriel LL, Bezabih NM, Woldearegay TW. Level of adherence and associated factors among HIV-infected patients on antiretroviral therapy in Northern Ethiopia: retrospective analysis. Patient Prefer Adherence. 2020;14:1585–1594. doi: 10.2147/PPA.S268395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.MacDonell K, Naar-King S, Huszti H, Belzer M. Barriers to medication adherence in behaviorally and perinatally infected youth living with HIV. AIDS Behav. 2013;17:86–93. doi: 10.1007/s10461-012-0364-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rudy BJ, Murphy DA, Harris DR, Muenz L, Ellen J Adolescent Trials Network for HIV/AIDS Interventions. Prevalence and interactions of patient-related risks for nonadherence to antiretroviral therapy among perinatally infected youth in the United States. AIDS Patient Care STDS. 2010;24:97–104. doi: 10.1089/apc.2009.0198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dejesus E, Young B, Morales-Ramirez JO, Sloan L, Ward DJ, Flaherty JF, Ebrahimi R, Maa JF, Reilly K, Ecker J, McColl D, Seekins D, Farajallah A AI266073 Study Group. Simplification of antiretroviral therapy to a single-tablet regimen consisting of efavirenz, emtricitabine, and tenofovir disoproxil fumarate versus unmodified antiretroviral therapy in virologically suppressed HIV-1-infected patients. J Acquir Immune Defic Syndr. 2009;51:163–174. doi: 10.1097/QAI.0b013e3181a572cf. [DOI] [PubMed] [Google Scholar]
- 28.Hodder SL, Mounzer K, Dejesus E, Ebrahimi R, Grimm K, Esker S, Ecker J, Farajallah A, Flaherty JF AI266073 Study Group. Patient-reported outcomes in virologically suppressed, HIV-1-Infected subjects after switching to a simplified, single-tablet regimen of efavirenz, emtricitabine, and tenofovir DF. AIDS Patient Care STDS. 2010;24:87–96. doi: 10.1089/apc.2009.0259. [DOI] [PubMed] [Google Scholar]
- 29.Kim MJ, Lee SA, Chang HH, Kim MJ, Woo JH, Kim SI, Kang C, Kee MK, Choi JY, Choi Y, Choi BY, Kim JM, Choi JY, Kim HY, Song JY, Kim SW Korea HIV/AIDS Cohort Study. Causes of HIV drug non-adherence in Korea: Korea HIV/AIDS cohort study, 2006-2015. Infect Chemother. 2017;49:213–218. doi: 10.3947/ic.2017.49.3.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hamers RL, Sigaloff KC, Wensing AM, Wallis CL, Kityo C, Siwale M, Mandaliya K, Ive P, Botes ME, Wellington M, Osibogun A, Stevens WS, Rinke de Wit TF, Schuurman R PharmAccess African studies to evaluate resistance (PASER) Patterns of HIV-1 drug resistance after first-line antiretroviral therapy (ART) failure in 6 sub-Saharan African countries: implications for second-line ART strategies. Clin Infect Dis. 2012;54:1660–1669. doi: 10.1093/cid/cis254. [DOI] [PubMed] [Google Scholar]
- 31.Galvan FH, Bing EG, Fleishman JA, London AS, Caetano R, Burnam MA, Longshore D, Morton SC, Orlando M, Shapiro M. The prevalence of alcohol consumption and heavy drinking among people with HIV in the United States: results from the HIV cost and services utilization study. J Stud Alcohol. 2002;63:179–186. doi: 10.15288/jsa.2002.63.179. [DOI] [PubMed] [Google Scholar]
- 32.Paolillo EW, Gongvatana A, Umlauf A, Letendre SL, Moore DJ. At-Risk Alcohol Use is Associated with Antiretroviral Treatment Nonadherence Among Adults Living with HIV/AIDS. Alcohol Clin Exp Res. 2017;41:1518–1525. doi: 10.1111/acer.13433. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Accompanying comorbidities among PLH under ART
Basic characteristics of 2015 year cohort utilized for suboptimal adherence analysis
Sex and age, proportion under ART.