Abstract
Background
Coronavirus disease-2019 (COVID-19) is a novel infectious disease, which presents with various clinical manifestations. There is growing evidence of an association between COVID-19 infection and autoimmune diseases. The aim of this case report was to demonstrate the association of COVID-19 infection and the development of systemic lupus erythematosus (SLE).
Case presentation
A 38 year old Iranian woman presented with progressive icterus, pleuritic chest pain, palpitation, dyspnea, photosensitivity and arthralgia 18-days after COVID-19 symptoms proved by a positive polymerized chain reaction (PCR). The chest and abdomen computerized tomography (CT) scan showed pericardial and pleural effusion and enlarged liver and abdominal lymph nodes. Antinuclear antibody (ANA), anti-double stranded deoxyribonucleic acid (anti-ds DNA) antibody and perinuclear anti-neutrophil cytoplasmic antibody (P-ANCA) were positive. She was diagnosed as SLE and was successfully treated with prednisolone 30 mg daily, hydroxychloroquine 200 mg daily and azathioprine 150 mg daily and she remarkably improved. Repeated anti-ds DNA antibody was positive. Due to nausea and abdominal discomfort, azathioprine was discontinued and replaced with mycophenolate mofetil 1500 mg daily. In the article, similar cases were presented; the mean interval between COVID symptoms and SLE presentations was 24.86 days. Pulmonary and renal involvements were the most common presentations of SLE triggered by COVID-19. The most frequently reported autoantibody was ANA
Conclusion
It is necessary to be aware of the development of lupus disease in COVID-19 infected patients, because prompt diagnosis and treatment is very important to improve their outcome.
Keywords: Autoimmunity, COVID-19, Systemic lupus erythematosus, SARS-CoV-2, Case report
1. Introduction:
Systemic lupus erythematosus (SLE) is a multi-systemic chronic inflammatory disease which involves many organs, including skin, joints, kidneys, liver, lungs and the nervous system, and is characterized by periods of remission and exacerbation [1]. It has a wide variety of clinical and immunological manifestations [2]. The immune system is impaired leading to the production of autoantibodies against host cells and making organ damages [1]. Interstitial lung disease (ILD) occurs as early as in the first 2 years in the course of SLE patients [3]. Infection is an important cause of hospital and intensive care unit (ICU) admission in SLE patients. Early disease, disease activity and damage, cyclophosphamide, erythrocyte sedimentation rate (ESR) and consumed complement (C3) were associated with infection in SLE [4]. There is an agreement to the key emerging frontline role of rheumatologists in treating COVID-19 [5].
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) can disturb immune tolerance, trigger immune response and produce pro-inflammatory cytokines [6]. Several previous articles have reported detection of autoantibodies in COVID-19 patients or development of autoimmune diseases associated with COVID-19 infection [7], [8], [9]. In a recent study, SLE was the rheumatic disease with highest priority to be vaccinated against COVID-19 [10].
The objective of this case report was to demonstrate the relation of COVID-19 infection to a case of SLE and to review the literature of similar cases.
2. Case presentation:
A 38 year old female presented to the internal medicine clinic with history of icterus, pleuritic chest pain, palpitation, photosensitivity and arthralgia for one week in December 2020. She denied abdominal pain, vomiting, pruritus or urine and fecal color changing. There was no history of alcohol, tobacco or illicit drug use. Her past medical history was unremarkable except for a diagnosis of generalized anxiety disorder (GAD) on sertraline 50 mg daily and a recent COVID-19 infection which was proved by a positive polymerized chain reaction (PCR) test about four weeks prior to this meeting. At that time, her symptoms were malaise, headache, anosmia, loss of appetite, dry cough and mild dyspnea, and she was treated with naproxen 500 mg twice daily and diphenhydramine syrup four times a day orally on outpatient basis. Her symptoms improved within two weeks. Three or four days later she developed icterus of sclera and skin, pleuritic chest pain, recurrence of dyspnea, photosensitivity and arthralgias of the small joints. The case was managed in accordance to the local ethical approval and informed written consent was obtained from the patient to publish her clinical data
On general examination, the vital signs were stable and she was not febrile. Jaundice was present on the skin and sclera. Skin lesions, oral ulcers and obvious arthritis was absent. Small non-significant and non-tender cervical lymphadenopathy was detected. Jugular venous pressure was normal. Examination of the respiratory system revealed decreased breath sounds at the bases of the lungs. Cardiovascular examination was unremarkable except for decreased heart sounds. The remaining systemic examination including abdominal was within normal limits.
Laboratory tests results were as follows: hemoglobin of 10.3 mg/dl, white blood cell count (WBC) 11.35 x103/mm3 (differential count: neutrophils 72.1%, lymphocytes 24.1%), platelet count 512 x103/mm3, creatinine 0.61 mg/dl, International normalized ratio (INR) 1.04, prothrombin time (PTT) 14 s, lactate dehydrogenase (LDH) 325 IU/ml (normal:207–414 IU/ml), aspartate transaminase (AST) 348 IU/L (normal:0–31 IU/L), alanine transaminase (ALT) 437 IU/L (normal:0–34 IU/L), alkaline phosphatase (ALP) 2069 U/L (normal:64–306 U/L), Total bilirubin 6.83 mg/dL (normal:0.3–1.2 mg/dL), Direct bilirubin 5.09 mg/dL (normal:0.1–0.4 mg/dL), erythrocyte sedimentation rate (ESR) 53 mm/hr and C-reactive protein (CRP) was positive. Urine analysis was normal. 24-hour urine protein was 22 mg/24 h. Serum protein electrophoresis was normal. Viral tests for human immunodeficiency virus (HIV), hepatitis A, B, and C were negative. At this time PCR testing for COVID-19 was negative. IgG immunoglobulin for coronavirus was positive but IgM immunoglobulin was negative.
A computerized tomography (CT) scan of chest and abdomen with and without oral and intravenous contrast was performed and showed moderate pericardial effusion, mild bilateral pleural effusion, mild enlargement of liver, multiple enlarged lymph nodes in liver hilum and para-aortic lymph node chains (Fig. 1, Fig. 2, Fig. 3 ).
Fig. 1.
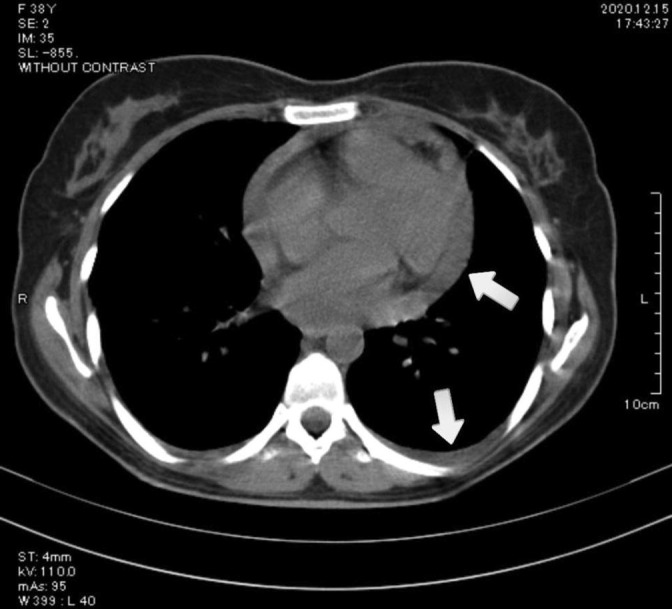
Chest computerized tomography (CT) scan without contrast showing pericardial effusion (upper arrow) and pleural effusion (lower arrow) in a 38 years old female with systemic lupus erythematosus and coronavirus disease-2019 (COVID-19).
Fig. 2.
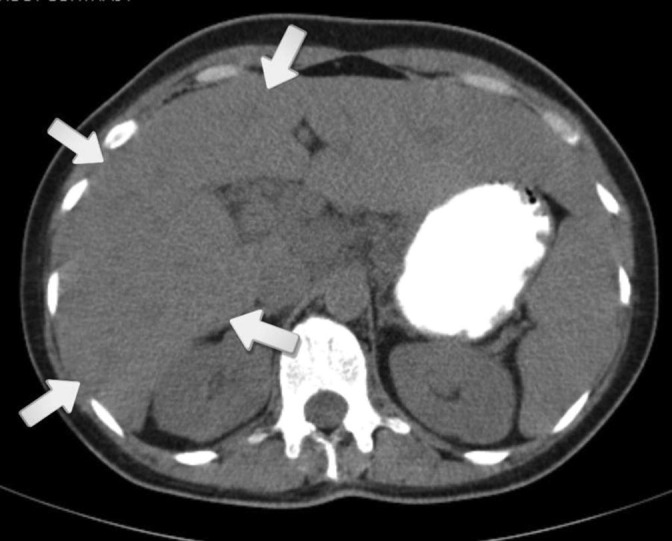
Abdominal computerized tomography (CT) scan without contrast showing mild liver enlargement (arrows showing its borders) in a 38 years old female with systemic lupus erythematosus and coronavirus disease-2019 (COVID-19).
Fig. 3.
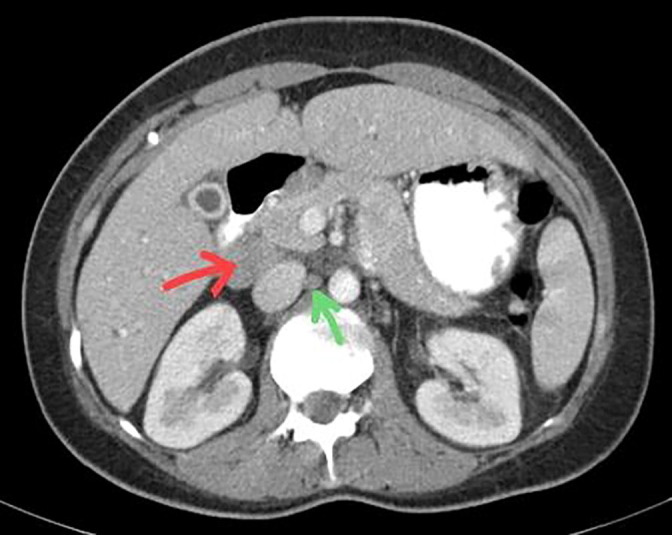
Arterial phase of abdominal computerized tomography (CT) scan with contrast showing para-aortic lymphadenopathy (green arrow), enlarged lymph nodes of liver hilum (red arrow) in a 38 years old female with systemic lupus erythematosus and coronavirus disease-2019 (COVID-19).
Considering multi-organ involvement and high levels of inflammatory markers, an immune-mediated disorder was suspected. Other differential diagnoses comprised: sarcoidosis, autoimmune and viral hepatitis, HIV, alcohol and drug hepatotoxicity, congestive hepatopathy due to right sided cardiac failure, amyloidosis, malignancies such as lymphoma. Lack of history of alcohol and drug usage and absence of right sided heart failure evidences on clinical examination and echocardiography, normal serum protein electrophoresis and negative tumor and viral markers and absence of mass in favor of malignancy in imaging, ruled out the possibility of these differential diagnoses. Immunological tests were conducted to investigate other possible diagnoses and revealed positive results for antinuclear antibody (ANA) > 10 Ratio (normal: <1), anti-double stranded deoxyribonucleic acid (anti-ds DNA) antibody 95 U/mL (normal: <25 U/mL), perinuclear anti-neutrophil cytoplasmic antibody (P-ANCA) 39.5 U/mL (normal: <5 U/mL). Anti Ro, Anti La, angiotensin converting enzyme (ACE), C3, C4, CH50 and anti-cyclic citrullinated peptide (anti-CCP) were normal. Anti-smooth muscle, anti-mitochondrial and anti-liver-kidney microsomal antibodies were negative.
She met the 2019 European League Against Rheumatism/American College of Rheumatology (EULAR/ACR) Classification Criteria for SLE [11] and treatment with prednisolone 0.5 mg/kg (30 mg) daily with gradual tapering to 5 mg daily, hydroxychloroquine 200 mg daily and azathioprine 150 mg daily was started. She was followed up in rheumatology clinic 6-weeks later. Her symptoms improved remarkably. Examination of respiratory and cardiovascular system were within normal limits. Liver function tests and bilirubin decreased to normal ranges. ESR was 53 mm/hr. Repeated positive immunological tests were as follows: anti-ds DNA antibody 468.5 U/mL (normal: <16 U/mL), P-ANCA 1/10 Titer (normal: <1/10). Other tests showed negative results. She is still under follow up in rheumatology clinic without recurrence of symptoms. Due to nausea and abdominal discomfort, azathioprine was discontinued and replaced with mycophenolate mofetil 1500 mg daily.
3. Discussion
Systemic lupus erythematosus (SLE) is an autoimmune disease with unknown etiology yet an infectious process may contribute to its pathogenesis. Viruses have been found to be more frequently associated with SLE. Epstein-Barr virus, parvovirus B19, cytomegalovirus and HIV type 1 are well recognized examples [1]. These agents may play a role in the lupus pathogenesis by triggering autoimmunity through different mechanisms including structural or functional molecular mimicry, modulate antigen processing, activation, or apoptosis of B and T cells, macrophages or dendritic cells, or encoding proteins that induce cross-reactive immune responses to self-antigens [12], [13]. There is raising concerns about the association between COVID-19 infection and autoimmune diseases (AID) [7], [8], [9]. The COVID-19 pathophysiology has revealed that in genetically predisposed patients, it could lead to the presentation or exacerbations of AIDs [14].
The adaptive immune system in lupus patients is impaired. Increased auto-reactivity of helper T cells, cytotoxic T cells, autoantibody production and B cell differentiation, in SLE has been revealed [15]. This leads to impairment in the production of interferon γ, interleukins (IL-1, IL-2), and tumor necrosis factor alpha (TNF-α), compromising a Th1 type of response, which is, generally, more effective than a Th2 response against viral infections [15], [16]. The adaptive immune system could be possibly disrupted in SARS-CoV-2 infection. Changes in cytokine production with shift from Th1 to Th2 cells has been found in HIV infection, and this could be a potential explanation for the occurrence of autoimmune phenomenon and potentially diseases after COVID-19 infection [17]. SARS-CoV-2 infection leads to autoimmunity by these possible mechanisms: molecular mimicry (cross-reacting epitope between the virus and the host), by stander killing (virus-specific CD8 + T cells migrating to the target tissues and exerting cytotoxicity), epitope spreading, viral persistence (polyclonal activation due to the constant presence of viral antigens driving immune-mediated injury) and formation of neutrophil extracellular traps [18]. A prevalence of ANA of 35.6% and lupus anticoagulant of 11.1% has been reported in patients hospitalized due to COVID-19 pneumonia [8]. Other autoantibodies such as anti-Ro/SSA have also been reported [9]. These findings indicate the role of SARS-CoV-2 in stimulating the immune system and development of lupus disease.
Our patient presented with icterus and high levels of AST, ALT, ALP and direct bilirubin. Liver injury is a manifestation of COVID-19. Abnormality of liver function tests is often transient and resolves without morbidity and mortality. There is close relationship of impaired liver function tests with severity of COVID-19. Possible mechanisms of liver injury are hypoxia, sepsis, medications of COVID-19, hyper-activated immune responses and cytokine storm [19]. The present patient developed icterus and elevated liver enzymes more than two weeks after diagnosis of COVID-19 infection when COVID-19 symptoms were resolved. The 18-days delay between COVID-19 symptoms and abnormal liver tests, positive autoantibodies and accompanying symptoms like photosensitivity and arthralgia suggested an autoimmune mechanism for liver injury in this case. A liver biopsy was not performed because icterus and liver laboratory abnormalities, began to resolve rapidly after starting the lupus treatment. COVID-19 related autoimmune hepatitis has been reported in a 57-year-old man with positive anti-smooth muscle antibody, anti-mitochondrial antibody, and anti-ds DNA antibodies. The patient was diagnosed with autoimmune hepatitis-primary biliary cholangitis overlap syndrome triggered by COVID-19 [20]. Liver involvement in the current patient appears to be due to hyper-inflammatory state in the context of lupus induced by COVID-19 infection.
Table 1 includes information about lupus or lupus-like diseases developed after or triggered by COVID-19 infection compared to the current case. For literature review, only articles that reported first presentation of SLE after COVID-19 infection were included. Articles which reported flares of known cases of SLE during or after COVID-19 infection were excluded. Five patients were females and three males (F:M 1.7:1) which was not consistent with the known sex ratio for SLE (F:M: 9–10/1) [21].The mean age was 41.87 years (18–85 years) The mean interval between COVID symptoms and SLE presentations was 24.86 days (13–60 days). COVID-19 infection was proved by PCR testing in seven cases ([17], [22], [23], [24], [25], [27] and the current one. Four cases had chest CT scan findings consistent with COVID-19 pneumonitis [22], [23], [24], [27] and three [23], [26] including the present case, had positive IgG immunoglobulin for coronavirus showing recent infection. Pulmonary involvement and acute renal injury were the most common SLE presentations among these cases. Most of them had respiratory symptoms from the initiation of COVID symptoms that progressed to respiratory distress [22], respiratory failure [17], [24], and ARDS [12]. Pleural effusion was found in four cases [17], [25], [26] including the present. Four patients presented with acute kidney injury and elevated creatinine [17], [22], [25], [26]. Icterus and elevation of liver enzymes was the main feature of the present patient. Abnormal liver function test was found in three other cases [22], [25], [27] but they did not report icterus. Positive ANA test was detected in all cases and positive anti-ds DNA was found in six ([17], [23], [24], [25], [27] similar to the present case. Low complement levels were found in all cases except ours, positive anti-Ro and La were found in two patients [23], [25] and antiphospholipid antibodies in two [17], [24]. Positive P-ANCA was found in this case and in only one of the previous articles [26]. The most common laboratory findings were proteinuria which was detected in all cases except this case, lymphopenia [17], [22], [24], [26], [27] and thrombocytopenia [17], [23], [24], [25], [26]. Eventually six patients improved and were discharged and two of them succumbed to illness.
Table 1.
Systemic lupus erythematosus (SLE) cases triggered by or developed after coronavirus disease 2019 (COVID-19).
| Articles/Year | Country | Age/sex | COVID-19 |
Interval (days) | SLE presentation | Laboratory findings | Immunological work-up | Treatment | Outcome | |
|---|---|---|---|---|---|---|---|---|---|---|
| symptoms | Dx | |||||||||
| Mantovani-Cardoso et el. [17] 2020 | USA | 18/F | malaise, fever, cough, dyspnea | PCR | 30 | Cardiac arrest, ARDS, Renal failure, pericardial/ pleural effusion, DVT |
↑Cr, lymphopenia, anemia, proteinuria, hematuria, ↓platelets, ↑CRP/ESR, ↑LDH, ↑ferritin, ↑D-dimer,↑β-2M | +ve ANA (1:2560), +ve dsDNA, ↓C3/ C4, +ve ACL, +ve LAC |
Steroids HCQ, TCZ PlasmaPh. ECMO |
death |
| El Aoud et al. [22] 2020 | France | 62/M | fever, cough, myalgia | PCR GGO |
17 | AKI, confusion, respiratory distress |
↑Cr, lymphopenia, ↑CRP, ↑LFT, proteinuria, ↓albumin, ↑α 2 globulin,↑D-dimer | +ve ANA (1/160), -ve dsDNA, Normal C |
Steroids TCZ |
improved |
| Zamani et al. [23] 2021 | Iran | 39/M | fever, cough, dyspnea, wheezing, ↓wt, anorexia |
PCR, GGO IgG | 60 | Rash, scaling, LL edema, ankle swelling, nephritis, hyperkeratosis, parasthesia |
leukopenia, ↓platelets, ↑ CRP/ESR, proteinuria |
+ve anti Ro/La, +ve dsDNA, ↓CH50, +ve anti-CCP, +ve ANA (1/160) |
Steroids HCQ CYC |
improved |
| Slimani et al.[24] 2021 | Morocco | 23/F | fever, cough, dyspnea, fatigue |
PCR, Pulm. Infilt. | 13 | Rash, respiratory failure |
lymphopenia, ↓platelets, ↑D-dimer, proteinuria, +ve direct Coombs, ↑PT/PTT |
+ve ANA,+ve dsDNA, +ve ACL, +ve LAC, +ve anti‐β2‐GP, ↓C |
Steroids | death |
| Gracia-Ramos et al. [25] 2021 | Mexico | 45/M | malaise, fever, cough, myalgia, arthralgia | PCR | 21 | Respiratory symptoms, pleural effusion, ascites, splenomegaly, renal failure, LL swelling |
↑Cr, ↓platelets, proteinuria, hematuria, anemia, ↓albumin, ↑PTT, ↑D-dimer, ↑fibrinogen, ↑ferritin, +ve CRP, ↑LFT | +ve ANA (1:1280), +ve dsDNA, +ve anti Ro/La, ↓C3 |
Steroids CQ, IVIg RTX splenectomy |
improved |
| Bonometti et al. [26] 2020 | Italy | 85/F | IgG | unconscious, AKI, vasculitis, pleural effusion, edema, peripheral cyanosis | ↑Cr, lymphopenia, ↓platelets, ↑N, ↑CRP, ↑Na, ↓K, ↑ferritin, ↑LDH, hematuria, proteinuria | +ve ANA, ↓C, atypical ANCA |
Steroids HCQ |
improved | ||
| Hali et al. [27] 2021 | Morocco | 25/F | fever, myalgia, asthenia | PCR, Pulm. Infilt. | 15 | Rash, oral ulcers, periorbital edema, pericardial effusion, vasculitis | anemia, neutropenia, lymphopenia, proteinuria, ↑ferritin, ↑LDH, ↓fibrin, ↑LFT, ↑triglycerides | +ve ANA, +ve dsDNA, ↓C |
Steroids | improved |
| This case Assar et al. 2021 |
Iran | 38/F | malaise, anosmia, cough, dyspnea, headache, anorexia |
PCR, IgG | 18 | Icterus, pleurisy, dyspnea, photosensitivity, arthralgia, pericardial/pleural effusion, ↑liver, ↑LNs | anemia, leukocytosis, ↑LFT, ↑ALP, ↑direct bilirubin, +ve CRP, ↑ESR |
+ve ANA, +ve dsDNA, +ve P-ANCA |
Steroids HCQ AZA |
improved |
COVID-19: coronavirus disease 2019, Dx; diagnosis, SLE: systemic lupus erythematosus, PCR: polymerized chain reaction, GGO: ground glass opacity, Pulm. Infilt.: pulmonary infilterates, Ig: immunoglobulin, ARDS: acute respiratory distress syndrome, DVT: deep vein thrombosis, AKI: acute kidney injury, LL: lower limbs, LNs: lumph nodes, Cr: creatinine, CRP: C-reactive protein, ESR: erythrocyte sedimentation rate, LDH: lactate dehydrogenase, β2M: beta-2 microglobulin, LFT: liver function tests, PT: prothrombin time, PTT: partial thromboplastin time, N: neutrophils, Na: sodium, K: potassium, ALP: alkaline phosphatase, ANA: anti-nuclear antibody, anti-dsDNA: anti-double stranded deoxyribonucleic acid, C: complement, ACL: anticardiolipin, LAC: lupus anticoagulant, anti-CCP: anti-cyclic citrullinated peptide, anti-β2 GP: anti-beta-2 glycoprotein, P-ANCA: perinuclear anti-neutrophil cytoplasmic antibody, HCQ: hydroxychloroquine, TCZ: tocilizumab, PlasmaPh: plasmapheresis, ECMO: extracorporeal membrane oxygenation, CYC: cyclophosphamide, CQ: chloroquine, IVIg: intravenous immunoglobulin, RTX: rituximab, AZA: azathioprine.
In conclusion, we presented a patient diagnosed as SLE following COVID-19 infection. The patient developed pleural and pericardial effusions, liver injury and positive ANA and Anti-ds DNA antibodies 18 days after initiation of COVID symptoms. She was successfully treated with prednisolone and azathioprine. COVID-19 infection has been found to stimulate immune system, leading to the production of autoantibodies and development of AIDs. It is necessary to be aware of the development of lupus disease in COVID-19 infected patients, because prompt diagnosis and treatment is very important to improve their outcome.
Credit Author Statement
SA conceived the idea to report the case. SA and DM were responsible for data collection and drafting the manuscript. MP and PS commented on the manuscript. All authors read and approved the final manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
CRediT authorship contribution statement
Shirin Assar: Project administration, Supervision, Review & editing. Mehran Pournazari: Data curation. Parviz Soufivand: Data curation. Dena Mohamadzadeh: Formal analysis, Methodology, Writing - original draft.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Peer review under responsibility of Egyptian Society of Rheumatic Diseases.
References
- 1.Illescas‐Montes R., Corona‐Castro C.C., Melguizo‐Rodríguez L., Ruiz C., Costela‐Ruiz V.J. Infectious processes and systemic lupus erythematosus. Immunology. 2019;158(3):153–160. doi: 10.1111/imm.13103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gheita T.A., Noor R.A., Abualfadl E., Abousehly O.S., El-Gazzar I.I., El Shereef R.R., et al. Adult systemic lupus erythematosus in Egypt: The nation-wide spectrum of 3661 patients and world-wide standpoint. Lupus. 2021;30(9):1526–1535. doi: 10.1177/09612033211014253. [DOI] [PubMed] [Google Scholar]
- 3.Habib H.M., Arafat W.R., Marie M.A., Eissa A.A. Pulmonary involvement in early systemic lupus erythematosus. Egyptian Rheumatologist. 2013;35(4):225–231. [Google Scholar]
- 4.Dorgham D.A., Anwar S., Khaled A.S. Infection in systemic lupus erythematosus patients. Egyptian Rheumatologist. 2021;43(2):115–118. [Google Scholar]
- 5.Gheita T.A., Salem M.N., Eesa N.N., Khalil N.M., Gamal N.M., Noor R.A., et al. ECR COVID19-Study Group. Rheumatologists' practice during the Coronavirus disease 2019 (COVID-19) pandemic: a survey in Egypt. Rheumatol Int. 2020;40(10):1599–1611. doi: 10.1007/s00296-020-04655-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Melenotte C., Silvin A., Goubet A.-G., Lahmar I., Dubuisson A., Zumla A., et al. Immune responses during COVID-19 infection. Oncoimmunology. 2020;9(1) doi: 10.1080/2162402X.2020.1807836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ciaffi J., Meliconi R., Ruscitti P., Berardicurti O., Giacomelli R., Ursini F. Rheumatic manifestations of COVID-19: a systematic review and meta-analysis. BMC Rheumatol. 2020;4:65. doi: 10.1186/s41927-020-00165-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gazzaruso C., Carlo Stella N., Mariani G., Nai C., Coppola A., Naldani D., et al. High prevalence of antinuclear antibodies and lupus anticoagulant in patients hospitalized for SARS-CoV2 pneumonia. Clin Rheumatol. 2020;39(7):2095–2097. doi: 10.1007/s10067-020-05180-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fujii H., Tsuji T., Yuba T., Tanaka S., Suga Y., Matsuyama A., et al. High levels of anti-SSA/Ro antibodies in COVID-19 patients with severe respiratory failure: a case-based review : High levels of anti-SSA/Ro antibodies in COVID-19. Clin Rheumatol. 2020;39(11):3171–3175. doi: 10.1007/s10067-020-05359-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hammam N., Tharwat S., Shereef R.R.E., Elsaman A.M., Khalil N.M., Fathi H.M., et al. Egyptian College of Rheumatology (ECR) COVID-19 Study Group. Rheumatology university faculty opinion on coronavirus disease-19 (COVID-19) vaccines: the vaXurvey study from Egypt. Rheumatol Int. 2021;41(9):1607–1616. doi: 10.1007/s00296-021-04941-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Aringer M., Costenbader K., Daikh D., Brinks R., Mosca M., Ramsey‐Goldman R., et al. 2019 European League Against Rheumatism/American College of Rheumatology Classification Criteria for Systemic Lupus Erythematosus. Arthritis Rheumatol. 2019;71(9):1400–1412. doi: 10.1002/art.40930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rigante D., Mazzoni M.B., Esposito S. The cryptic interplay between systemic lupus erythematosus and infections. Autoimmun Rev. 2014;13(2):96–102. doi: 10.1016/j.autrev.2013.09.004. [DOI] [PubMed] [Google Scholar]
- 13.Jara L.J., Medina G., Saavedra M.A. Autoimmune manifestations of infections. Curr Opin Rheumatol. 2018;30(4):373–379. doi: 10.1097/BOR.0000000000000505. [DOI] [PubMed] [Google Scholar]
- 14.Caso F., Costa L., Ruscitti P., Navarini L., Del Puente A., Giacomelli R., et al. Could Sars-coronavirus-2 trigger autoimmune and/or autoinflammatory mechanisms in genetically predisposed subjects? Autoimmun Rev. 2020;19(5):102524. doi: 10.1016/j.autrev.2020.102524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dabbagh M.F., Aurora L., D’Souza P., Weinmann A.J., Bhargava P., Basir M.B. Cardiac Tamponade Secondary to COVID-19. JACC Case Rep. 2020;2(9):1326–1330. doi: 10.1016/j.jaccas.2020.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ramshaw I.A., Ramsay A.J., Karupiah G., Rolph M.S., Mahalingam S., Ruby J.C. Cytokines and immunity to viral infections. Immunol Rev. 1997;159(1):119–135. doi: 10.1111/j.1600-065x.1997.tb01011.x. [DOI] [PubMed] [Google Scholar]
- 17.Mantovani Cardoso E., Hundal J., Feterman D., Magaldi J. Concomitant new diagnosis of systemic lupus erythematosus and COVID-19 with possible antiphospholipid syndrome. Just a coincidence? A case report and review of intertwining pathophysiology. Clin Rheumatol. 2020;39(9):2811–2815. doi: 10.1007/s10067-020-05310-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shah S., Danda D., Kavadichanda C., Das S., Adarsh M.B., Negi V.S. Autoimmune and rheumatic musculoskeletal diseases as a consequence of SARS-CoV-2 infection and its treatment. Rheumatol Int. 2020;40(10):1539–1554. doi: 10.1007/s00296-020-04639-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li J., Fan J.G. Characteristics and mechanism of liver injury in 2019 coronavirus disease. J Clin Transl Hepatol. 2020;8(1):13–17. doi: 10.14218/JCTH.2020.00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Singh B., Kaur P., Maroules M. Autoimmune Hepatitis-Primary Biliary Cholangitis Overlap Syndrome Triggered by COVID-19. Eur J Case Rep Intern Med. 2021;8(3) doi: 10.12890/2021_002264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Alonso M.D., Martínez-Vázquez F., Riancho-Zarrabeitia L., Díaz de Terán T., Miranda-Filloy J.A., Blanco R., et al. Sex differences in patients with systemic lupus erythematosus from Northwest Spain. Rheumatol Int. 2014;34(1):11–24. doi: 10.1007/s00296-013-2798-9. [DOI] [PubMed] [Google Scholar]
- 22.El Aoud S., Morin C., Lorriaux P., Obert J., Sorial D., Chaabouni T., et al. COVID-19 presenting as lupus erythematosus-like syndrome. Disaster Med Public Health Prep. 2020;1–4 doi: 10.1017/dmp.2020.358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zamani B., Moeini Taba S.M., Shayestehpour M. Systemic lupus erythematosus manifestation following COVID-19: a case report. J Med Case Rep. 2021;15(1):29. doi: 10.1186/s13256-020-02582-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Slimani Y., Abbassi R., El Fatoiki F.-Z., Barrou L., Chiheb S. Systemic lupus erythematosus and varicella-like rash following COVID-19 in a previously healthy patient. J Med Virol. 2021;93(2):1184–1187. doi: 10.1002/jmv.26513. [DOI] [PubMed] [Google Scholar]
- 25.Gracia-Ramos A.E., Saavedra-Salinas M.Á. Can the SARS-CoV-2 infection trigger systemic lupus erythematosus? A case-based review Rheumatol Int. 2021;41(4):799–809. doi: 10.1007/s00296-021-04794-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bonometti R., Sacchi M.C., Stobbione P., Lauritano E.C., Tamiazzo S., Marchegiani A., et al. The first case of systemic lupus erythematosus (SLE) triggered by COVID-19 infection. Eur Rev Med Pharmacol Sci. 2020;24(18):9695–9697. doi: 10.26355/eurrev_202009_23060. [DOI] [PubMed] [Google Scholar]
- 27.Hali F., Jabri H., Chiheb S., Hafiani Y., Nsiri A. A concomitant diagnosis of COVID-19 infection and systemic lupus erythematosus complicated by a macrophage activation syndrome: A new case report. Int J Dermatol. 2021;60(8):1030–1031. doi: 10.1111/ijd.15592. [DOI] [PMC free article] [PubMed] [Google Scholar]


