Date: 14-18 September 2021
Location: Virtual Meeting
Sponsorship: Publication of this supplement was sponsored by MCA Events on behalf of the European Society of Paediatric Radiology (ESPR), Union of European Neonatal and Perinatal Societies (UENPS), European Foundation for the Care of Newborn Infants (EFCNI).
All content was reviewed and selected by the Scientific Committee and selected abstract reviewers, which held full responsibility for the abstract selections.
*Presenting author names have asterisks in the contributor lists.
ID 50. The effects of mean platelet volume, nucleated red blood cells and right ventricular systolic pressure on prediction of severity of transient tachypnea of the newborn
Yusuf Çelik1, Dilek Kahvecioğlu1*, İbrahim Ece1, Fatih Atik1, Aslıhan Köse Çetinkaya1, Medine Ayşin Taşar1
1University of Health Sciences, Ankara Training and Research Hospital, Ankara, Turkey
Background: Transient tachypnea of the newborn (TTN) is a common clinical problem that often occurs in the first hours after birth. Although it is considered to be a benign clinical course, some cases may have severe symptoms and require ventilation support. In this study, we aimed to determine the association between the mean platelet volume (MPV), nucleated red blood cell (nRBC), right ventricular systolic pressure (RVSP) and the severity of TTN.
Methods: Patients with TTN were divided into two groups according to Silverman score (<7:group 1[n:34] and ≥7: Group 2 [n:30]). The groups were compared in terms of demographic characteristics, hematologic parameters and RVSP within the first 24 h after admission.
Results: Mean birth weight of the patients were 3033.4±364.1 g and median gestational age were 38 weeks (min–max 34–42). The rate of C/S was found to be higher (p = 0.015) and APGAR scores at 1th and 5th minutes (p = 0.001, p = 0.003 respectively) were lower in Group 2. The comparison of respiratory findings were mentioned in Table 1. In terms of hematologic parameters; Group 2 had significantly higher thrombocyte, haemoglobin, hematocrit and nRBC levels (p < 0.05). RVSP were found to be higher in Group 2 (p: 0.001). In logistic regression analysis, nRBC was found to be the most important independent parameter affects Silverman score at admission (OR: 7.065, CI: 1258–39,670, p: 0.026).
Conclusion: This is the first study that investigates the effects of nRBC and RVSP on severity of TTN. It shows that patients with high nRBC and RVSP values may have poor prognosis, require longer ventilation support and longer duration of hospitalization.
| Group-1 (n = 34) Silverman score < 7 |
Group-2 (n = 30) Silverman score ≥ 7 |
p | |
|---|---|---|---|
| Respiratory rate at admissiona | 64 (60–78) | 68 (62–88) | 0.003 |
| Downe’s score at admissiona | 4 (2–7) | 7 (7–10) | 0.001 |
| Downe’s score at 24th houra | 1 (0–3) | 3 (1–10) | 0.001 |
| Silverman score at 24th houra | 1 (0–3) | 3 (1–9) | 0.001 |
| Oxygen free saturation at admissiona | 93 (84–98) | 90 (81–94) | 0.001 |
| Duration of hospitalizationa | 3 (1–8) | 6 (2–15) | 0.001 |
| Respiratory support (n) | |||
| Hood | 25 | 3 | 0.001 |
| nCPAP | 9 | 17 | |
| nSIMV | 0 | 7 | |
| SIMV | 0 | 3 | |
| Duration of oxygen treatmenta | 2 (1–5) | 4 (1–14) | 0.001 |
aMedian (min−max).
(ID 50) - Table 1. The comparison of respiratory findings
None declared.
ID 54. A randomised trial of prophylactic oropharyngeal surfactant for preterm infants
Madeleine Murphy1*, Jan Miletin2, Hans Jørgen Guthe3, Claus Klingenberg4, Vincent Rigo5, Richard Plavka6, Kajsa Bohlin7, Almerinda Pereira8,Tomas Juren9, Colm O’Donnell1
1National Maternity Hospital, Dublin, Ireland, 2Coombe Women and Infants University Hospital, Dublin, Ireland, 3Haukeland University Hospital, Bergen, Norway, 4University Hospital of North Norway, Tromsø, Norway, 5Centre Hospitalier Universitaire de Liège, Belgium, 6Charles University, Prague, Czech Republic, 7Karolinska Institutet, Stockholm, Sweden, 8Hospital de Braga, Braga, Portugal, 9University Hospital Brno, Brno, Czech Republic
Background: Preterm infants are at high risk of developing respiratory distress syndrome (RDS). Endotracheal surfactant is effective in preventing and treating RDS; however, intubation is invasive and associated with adverse effects. Half of infants born <29 weeks’ gestation initially managed with continuous positive airway pressure (CPAP) are ultimately intubated for surfactant. Administration of surfactant into the pharynx has been reported in preterm animals and humans and may be effective. We wished to determine whether giving oropharyngeal surfactant at birth reduces the rate of endotracheal intubation for respiratory failure in preterm infants within 120 hours.
Methods/design: Infants born before 29 weeks’ gestation who were free of major anomalies were enrolled to this unblinded study at nine centres in six European countries. They were randomly assigned to receive oropharyngeal surfactant at birth in addition to CPAP or CPAP alone. The primary outcome was intubation within 120 h of birth, either for bradycardia and/or apnoea despite respiratory support in the delivery room, or for pre-specified respiratory failure criteria in the neonatal intensive care unit. Secondary outcomes included incidence of mechanical ventilation, chronic lung disease, and death before hospital discharge.
Results: A total of 251 infants were included in the study; 126 infants were assigned to oropharyngeal surfactant and 125 infants to control. The groups were well matched at study entry; their mean (SD) gestational age was 26 (2) vs 26 (2) weeks, and their mean (SD) birth weight was 874 (261) vs 851 (253) g respectively. There was no difference between groups in the rate of intubation at 120 hours [79/126 (63) vs 81/125 (65)%, p = 0.793] (table). There were no differences between the groups in the rate or duration of mechanical ventilation; the rates of bronchopulmonary dysplasia, chronic lung disease, or postnatal steroid use; or in the rate of death before hospital discharge.
Conclusion: Administration of surfactant into the oropharynx immediately after birth in addition to CPAP compared to CPAP alone did not reduce the rate of intubation amongst infants born before 29 weeks’ gestation in the first 5 days of life.
| OP Surfactant N = 126 |
Control N = 125 |
P value | |
|---|---|---|---|
| Primary intention-to-treat analysis | |||
| Intubated within 120 h of life | 79 (63) | 81 (65) | 0.793 |
| GA < 26 weeks | 40/48 (83) | 35/44 (80) | 0.789 |
| GA 26–28+6 weeks | 39/78 (50) | 46/80 (57) | 0.429 |
| Other outcome measures | |||
| Pneumothorax, n (%) | 21 (17) | 9 (7) | 0.031 |
| Pulmonary hemorrhage, n (%) | 6 (5) | 5 (4) | 0.999 |
| Mechanical ventilation, n (%) | 77 (62) | 81 (66) | 0.511 |
| Days of mechanical ventilation, median (IQR) | 1 (0, 8) | 2 (0, 7) | 0.445 |
| Postnatal corticosteroids, n (%) | 27 (22) | 29 (24) | 0.762 |
| Days of respiratory support, median (IQR) | 53 (27, 73) | 50 (26, 72) | 0.798 |
| BPD, n (%) | 72 (70) | 73 (69) | 0.882 |
| CLD, n (%) | 26 (26) | 29 (29) | 0.637 |
| Medical treatment for PDA, n (%) | 26 (21) | 37 (30) | 0.110 |
| Surgical treatment for PDA, n (%) | 2 (8) | 2 (5) | 0.99 |
| Necrotising enterocolitis, n (%) | 10 (8) | 13 (10) | 0.259 |
| IVH grade 3 or 4, n (%) | 8 (6) | 8 (7) | 0.999 |
| Cystic PVL, n (%) | 4 (3) | 4 (3) | 0.999 |
| ROP treated with laser or intravitreal injections, n (%) | 13 (10) | 10 (8) | 0.339 |
| Death before hospital discharge, n (%) | 23 (19) | 22 (19) | 0.999 |
| Survival without BPD at hospital discharge, n (%) | 31 (25) | 32 (26) | 0.884 |
| Survival without CLD at hospital discharge, n (%) | 71 (58) | 72 (60) | 0.794 |
| Duration of hospitalisation, median (IQR), days | 73 (53, 92) | 75 (53, 88) | 0.798 |
| Home oxygen therapy, n (%) | 3 (3) | 10 (9) | 0.048 |
BPD bronchopulmonary dysplasia, CLD chronic lung disease, PDA patent ductus arteriosus, IVH intraventricular haemorrhage, PVL periventricular leukomalacia, ROP retinopathy of prematurity.
(ID 54) - Table. Outcome measures.
Chiesi Farmaceutici, manufacturers of poractant alfa (Curosurf), supplied the study drug free of charge; they had no role in study design; and no role in data collection, analysis or interpretation.
ID 83. Short-term effects of systemic hydrocortisone initiated 7 to 14 days after birth in ventilated very preterm infants
Nienke Halbmeijer1*, Wes Onland1, Filip Cools2, Andre Kroon3, Marja van der Heide-Jalving4, Peter Dijk5, Henrica van Straaten4, Arjan te Pas6, Thilo Mohns7, Els Bruneel8, Arno van Heijst9, Boris Kramer10, Anne Debeer11, Inge Zonnenberg12, Yoann Marechal13, Henry Blom14, Katleen Plaskie15, Martin Offringa16, Anton van Kaam1
1Emma Children’s Hospital, Amsterdam Reproduction & Development research institute, Amsterdam UMC, University of Amsterdam, Amsterdam, The Netherlands, 2Universitair Ziekenhuis Brussel, Brussel, Belgium, 3Erasmus Medical Center Rotterdam, Rotterdam, The Netherlands, 4Isala Medical Center, Zwolle, The Netherlands, 5University Medical Center Groningen, Beatrix Children’s Hospital, University of Groningen, Groningen, The Netherlands, 6Leiden University Medical Center, Leiden, The Netherlands, 7Maxima Medical Center, Veldhoven, The Netherlands, 8Ziekenhuis Oost-Limburg, Genk, Belgium, 9Radboud University Medical Center-Amalia Childrens Hospital, Nijmegen, The Netherlands, 10Maastricht University Medical Center, Maastricht, The Netherlands, 11Universitair ziekenhuis Leuven, Leuven, Belgium, 12Medical Center Utrecht, Utrecht, The Netherlands, 13Centre Hospitalier Universitaire de Charleroi, Charleroi, Belgium, 14Universitair Ziekenhuis Antwerpen, Antwerpen, Belgium, 15St Augustinus ziekenhuis, Antwerpen, Belgium, 16the Hospital for Sick Children Research Institute, University of Toronto, Toronto, Canada
Background: The Systemic Hydrocortisone To Prevent Bronchopulmonary Dysplasia in preterm infants (the SToP-BPD) study is the first large randomized placebo-controlled trial investigating the effect of systemic hydrocortisone treatment initiated in the second week of life in ventilator-dependent preterm infants on the primary outcome death or bronchopulmonary dysplasia at 36 weeks’ postmenstrual age. In the current study, we performed a secondary in-depth analysis of the short-term pulmonary and systemic effects of hydrocortisone treatment based on the data collected in the SToP-BPD study.
Methods: Eligible preterm infants with a gestational age <30 weeks and/or birth weight <1250 g were randomly assigned between 7–14 days of life to a 22–day course of systemic hydrocortisone (cumulative dose 72.5 mg/kg; n = 182) or placebo (n = 190). Data on extubation, ventilator mode and settings, blood glucose levels, and blood pressure were recorded daily during the 22-day treatment course. Changes over time during the first 7 days of treatment for the ventilator mode and settings, blood glucose levels, and blood pressure were compared between treatment groups with linear mixed effects models.
Results: At the end of the 22-day treatment course, a significantly lower proportion of infants in the hydrocortisone group failed extubation compared to the placebo group (23.2% [42/181] vs 34.9% [66/189], respectively; crude risk difference, −11.7% [95% CI, −20.7% to −2.4%]). Mean airway pressure, fraction of inspired oxygen and respiratory index decreased significantly over the first 7 days of treatment in infants treated with hydrocortisone compared to placebo (−0.42 cmH2O [95% CI, −0.48 to −0.35], −0.02 [95% CI, −0.02 to −0.01], and −0.37 [95%, CI −0.44 to −0.30], respectively; all p < 0.001). Blood glucose levels and mean blood pressure increased significantly over the first 7 days in hydrocortisone treated infants (0.14 mmol/L [95% CI, 0.08 to 0.21] and 0.84 mmHg [95% CI, 0.58 to 1.09], respectively; both p < 0.001).
Conclusion: Systemic hydrocortisone initiated between 7–14 days after birth in mechanically ventilated preterm infants born before 30 weeks’ gestation significantly improves the pulmonary condition, thereby facilitating weaning and extubation from invasive mechanical ventilation.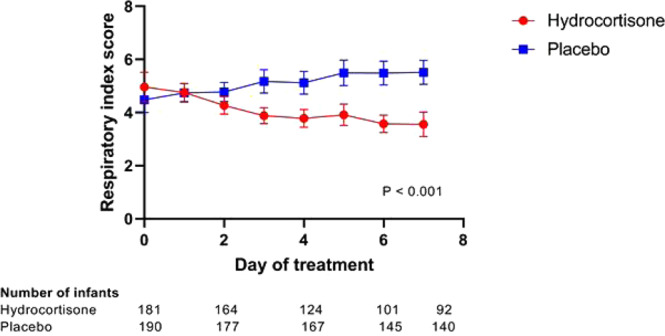
(ID 83) - Fig. 1. Changes over first 7 days of treatment in mean values for Respiratory Index (defined as MAWP × FiO2), with 95% confidence intervals analyzed with linear mixed effects models.
None declared.
ID 85. Congenital diaphragmatic hernia outcomes in a population with a high incidence of associated anomalies
Moath Alhamad1*, Dhullipala Anand1
1Sidra Medicine, Doha, Qatar
Background: Congenital diaphragmatic hernia (CDH) is a complex congenital condition with significant morbidity and mortality. The morbidity and mortality are increased when CDH is associated with other anomalies. Reported survival varies between centers but is mostly around 70%. The rates of termination of pregnancy (TOP), however, are high in many of these centers, especially for pregnancies with CDH and other anomalies. In this study, we report the outcomes of a population of CDH infants with a high incidence of associated anomalies but a low rate of TOP, and we compare these outcomes to published literature.
Methods: The data from CDH-Qatar (CDH-Q) registry (established as a part of CDH-Q program at Sidra Medicine), between April 2018 and December 2020, was compared to the published data by the CDH study group (CDHSG), the European Surveillance of congenital anomalies (EUROCAT), Florida Birth Defects Registry, and other centers.
Results: During the study period, 35 infants with CDH were treated at Sidra Medicine, with a median birth gestational age of 38 weeks (IQR 36–39) and birth weight of 2.78 kg (IQR 2.22–3.17). 27 infants (77%) were inborn, and 30 infants (86%) were diagnosed prenatally. None of the prenatally diagnosed cases resulted in TOP. A unique aspect of CDH-Q is the high rates of infants with associated congenital heart disease (23%), genetic abnormalities (26%), and major congenital anomalies (46%), as these rates are higher than what was reported in literature. Despite that, CDH-Q survival rates are similar to those reported in literature: Overall survival to home discharge is 69%, with higher survival among infants who were actively resuscitated at birth (73%), infants who underwent surgical repair (80%), and infants with isolated CDH (79%).
Conclusion: To our knowledge, CDH-Q is the first and only dedicated program for treatment of CDH in the Middle East. Considering the unique patient population with low incidence of TOP and higher incidence of genetic and congenital anomalies, the outcomes of CDH-Q are similar to published literature. Establishing a CDH registry for the Middle East would be beneficial to study and compare the characteristics and outcomes of CDH in this unique patient population.
None declared.
ID 185. Air distribution during non-invasive high-frequency ventilation in preterm infants
Vincent Gaertner1*, Andreas Waldmann2, Peter Davis3, Dirk Bassler1, Laila Springer4, David Tingay5, Christoph Rüegger1
1University Hospital Zurich and University of Zurich, Zurich, Switzerland, 2University Medical Center, Rostock, Germany, 3Newborn Research Centre and Neonatal Services, The Royal Women’s Hospital, Melbourne, Australia, 4Children’s Hospital, Tübingen, Germany, 5The Royal Children’s Hospital, Melbourne, Australia
Introduction: The use of non-invasive high-frequency oscillatory ventilation (nHFOV) in preterm infants may be beneficial in selected clinical situations. However, the underlying pathophysiological mechanisms are still unexplained.
Objectives: To compare distribution of ventilation and aeration between nHFOV and nasal continuous positive airway pressure (nCPAP).
Methods: During a recent randomized crossover trial comparing nHFOV with nCPAP, electrical impedance tomography (EIT) data were recorded from 30 preterm infants in prone position. Thirty consecutive breaths were extracted for four recordings per mode of ventilation. During nHFOV, mean airway pressure equaled nCPAP pressure and the smallest amplitude to achieve visible chest wall vibration was used. Ventilation distribution of spontaneous breaths was assessed in 32 horizontal slices. Differences in end-expiratory lung impedance (EELI) between nHFOV and nCPAP were calculated for the whole lung and for four horizontal regions of interest.
Main results: Overall, 228 recordings were analyzed. Ventilation distribution of spontaneous breaths was similar between nHFOV and nCPAP. Considering the entire EIT signal including oscillatory volumes, aeration of the lung was increased during nHFOV compared to nCPAP [Mean difference (95% CI) = 0.4 (0.2–0.6) AU/kg, p = 0.013]. This effect was mainly due to an increase in EELI in the non-gravity-dependent regions of the lung [ΔEELINGD = 6.9 (0.0–13.8) AU/kg, p = 0.028; ΔEELImidNGD = 6.8 (1.2–12.4) AU/kg, p = 0.009], see Fig. 1.
Conclusion: Distribution of spontaneous breathing is similar during nHFOV and nCPAP but overall aeration is higher during nHFOV, particularly in the non-gravity-dependent regions of the lung. This may indicate that spontaneous breathing is not affected by nHFOV but that the superimposed oscillations contribute to potential clinical benefits.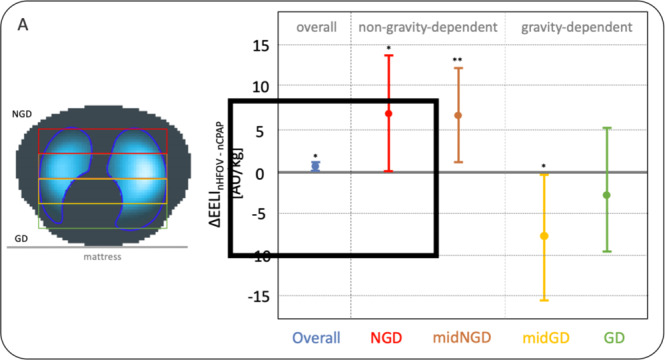
(ID 185) - Changes in aeration between nHFOV and nCPAP. Mean and 95% CI of ΔEELI over the whole lung and for four quantiles of the lung (non-gravity-dependent to gravity dependent) are shown separately.
None declared.
ID 203. Premedication before less invasive surfactant administration: a systematic review
Sophie Tribolet1*, Nadège Hennuy1, Diane Snyers1, Vincent Rigo1
1Centre hospitalier universitaire de Liège, Liège, Belgium
Background: Surfactant therapy is the cornerstone of the management of respiratory distress syndrome. Alternatives to endotracheal intubation for surfactant administration currently include “less invasive surfactant administration”. Its effectiveness was demonstrated by meta-analyses and guidelines now recommend it as the optimal method of surfactant administration in spontaneously breathing babies. While it still requires a direct laryngoscopy, the issue of sedation and analgesia during the procedure remains controversial as 52% of European neonatologists do not use any.
Methods: Medline via Ovid, Embase, Scopus and Cochrane Library of Trials were searched for studies of LISA after sedation without any filters or limits independently by two reviewers. Risk of bias (RoB) and quality assessment were evaluated using the RoB2 for RCT or the Newcastle Ottawa Scales (NOS) for cohort studies.
Results: We included eight studies: one RCT, two prospective, three retrospective and two RCT comparing INSURE and LISA after sedation (LISA arms assessed as prospective cohorts), for a total of 908 newborns.
Failure, defined as need for intubation or for a second dose of surfactant was no different between sedated and unsedated groups. Infant pain was significantly reduced, with more infants evaluated as comfortable. LISA with sedations led to higher occurrences of intraprocedural desaturation and need for positive pressure ventilation, but need for mechanical ventilation within 24 or 72 h of life was not significantly different. Clinical tolerance and complications (hypotension, mortality, air leaks, BPD…) were similar. Procedural conditions were evaluated as good or excellent in 83% after sedation.
Discussion and conclusion: This systematic review highlighted that analgesia or sedative drugs increase infant comfort and allow good procedural conditions, with a limited impact on the clinical evolution. Many questions remain about the optimal drug and dosage, given the need to maintain spontaneous breathing and to act only for the shortest duration. Despite limited data, we found no reason to avoid sedative drugs for LISA, given how deleterious awake laryngoscopy can be. Large RCT’s should be initiated in units currently not sedating infants prior to LISA.
Other
Prospero registration: CRD42020205365.
No source of founding.
None declared.
ID 223. Incidence, predictors and outcomes of pulmonary hypertension in extremely premature babies with moderate to severe broncho pulmonary dysplasia: ten years’ experience from a tertiary surgical neonatal centre in United Kingdom
Irina Branescu1*, Simona Vladareanu2, Sandeep Shetty3, Justin Richards3, Anay Kulkarni3
1'Carol Davila’ University of Medicine and Pharmacy, St. George’s University Hospital, London, United Kingdom, 2’Carol Davila’ University of Medicine and Pharmacy, Bucharest, Romania, 3St. George’s University, St. George’s University Hospital, London, United Kingdom
Background: As extreme prematurity survival rates increase, bronchopulmonary dysplasia (BPD) remains the most common morbidity. Pulmonary hypertension (PHT) is independently associated with poor outcomes in babies with BPD. The incidence of PHT in BPD patients have been reported to be between 17–24% and carry high mortality up to 50% within 2 years of diagnosis.
Methods: Single centre retrospective cohort study with prospective objective review by a single observer of all echocardiography assessments done for screening for PHT in extremely premature babies with moderate to severe BPD. All infants ≤32 weeks’ gestation, admitted to St George’s Hospital between March 2010 and July 2020 with moderate to severe BPD at 36 weeks’ corrected gestation, were included. Infants with complex congenital anomalies, genetic syndromes and surgical conditions were excluded.
Results: Out of total 563 preterm infants ≤32 weeks’ gestation, 275 babies with moderate to severe BPD were included in the study. Echocardiography screening for PHT was done for 229 babies. Thirty-four babies (12%) were observed to have PHT with 13 babies (4%) having severe/supra-systemic PHT. Need for invasive or non-invasive respiratory support at 36 weeks corrected gestation was associated with PHT (OR: 5.7, 95% CI: 2.64–12.3). None of the babies who didn’t need non-invasive/invasive respiratory support at 36 weeks corrected gestation developed severe PHT. Ten babies (30%) with PHT associated to severe BPD died before discharge from neonatal unit. PHT was associated with death before discharge from the neonatal unit (OR: 9.7, 95% CI: 3.5–27).
Conclusion: Incidence of PHT in babies with moderate to severe BPD was lower than reported literature. Extremely premature babies with severe BPD, who need invasive/non-invasive respiratory support at 36 weeks’ corrected gestation, are more likely to develop PHT. Babies with severe BPD and PHT are more likely to die before discharge from the neonatal unit than babies without PHT.
None.
ID 237. The DELUX study—Development of Lung volumes during extubation of preterm infants
Leonie Plastina1*, Vincent Gaertner1, Andreas D. Waldmann2, Janine Thomann1, Dirk Bassler1, Christoph M. Rüegger1
1University Hospital and University of Zurich, Zurich, Switzerland, 2Rostock University Medical Center, Rostock, Germany
Background: Prolonged endotracheal ventilation can lead to inflammation, tissue damage and the disruption of lung development. To reduce these risks, clinicians aim to extubate preterm infants to non-invasive respiratory support as soon as possible. Prediction of successful extubation is crucial to avoid adverse outcomes associated with re-intubation. A low lung volume after extubation has been identified as an important predictor of extubation failure, emphasizing the relevance of functional residual capacity (FRC) for subsequent clinical outcomes. This study aims to measure changes in end-expiratory lung impedance (EELI) using electrical impedance tomography (EIT) as a marker of functional residual capacity (FRC) during the entire extubation procedure of very preterm infants.
Methods: Prospective observational study in preterm infants born at 26–32 weeks gestation being extubated to non-invasive respiratory support. Changes in EELI and cardiorespiratory parameters (heart rate, oxygen saturation) were recorded at pre-specified events during the extubation procedure compared to baseline (before first handling of the infant).
Results: Overall, 2912 breaths were analysed in 12 infants. There was a global change in EELI during the extubation procedure (p = 0.029, see Fig. 1). EELI was lowest at time of extubation [median (IQR) difference to baseline: −0.30 AU/kg (−0.46; −0.14); corresponding to FRC loss of 10.2 ml/kg (4.8; 15.9), padj = 0.004]. The biggest EELI loss occurred during plaster removal of the endotracheal tube [median change (IQR): −0.18 AU/kg (−0.22; −0.07), padj = 0.004]. The biggest increase in EELI occurred between the positional change of the infant from supine to prone position (padj = 0.106). After 10 min in prone position EELI was significantly higher compared to plaster removal and extubation (padj = 0.004). EELI changes were highly correlated with changes in SpO2/FiO2 ratio (r = 0.48, p < 0.001). Forty percent of FRC were re-recruited at the tenth breath after initiation of non-invasive ventilation (p < 0.001).
Conclusions: The extubation procedure is associated with significant changes in FRC attributable mainly to two events. Plaster removal is the major factor contributing to FRC loss during extubation and turning the infant prone after extubation is helpful in re-establishing FRC. This study provides novel information for determining the optimal way of extubating a preterm infant.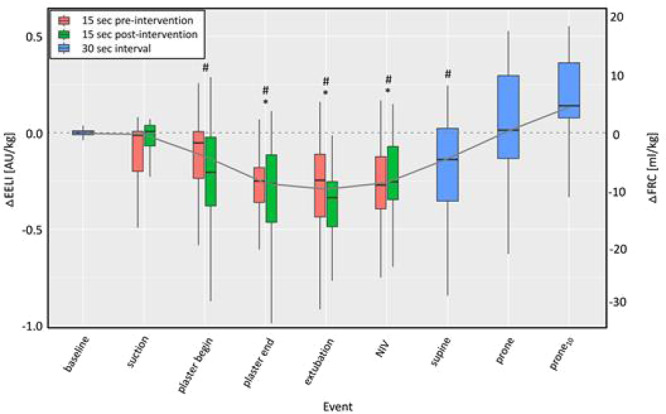
(ID 237) - Red and green boxplots show the 15 s before and after the respective intervention and blue boxplots show results for 30-s intervals without intervention. EELI changed significantly (Friedman’s test: p = 0.029)
None declared.
ID 258. The translational potential of the preterm rabbit as a BPD animal model
Matteo Storti1*, Francesca Ricci2, Costanza Casiraghi2, Chiara Catozzi2, Giorgio Aquila2, Ilaria Minato1, Maria Chiara Iannitello1, Danilo Tatoni1, Francesca Ravanetti1, Luisa Ragionieri1, Roberta Ciccimarra1, Matteo Zoboli1, Gino Villetti2, Fabrizio Salomone2, Barbara Montanini1, Simone Ottonello1
1University of Parma, Parma, Italy, 2Chiesi Farmaceutici, Parma, Italy
Background: Bronchopulmonary dysplasia (BPD) is the most common complication of premature babies born with underdeveloped lungs. Animal models are pivotal to study its pathophysiology. Given the low maintenance cost and the short gestation period, BPD mouse models are commonly used in pre-clinical practice. However, unlike babies who are born at term in the alveolar phase, mice are naturally delivered with structurally immature (although functional) lungs in the saccular phase (gestational age, GA 21th). Rabbits share some of the mice practical advantages, but they are born at term (GA 31th) in the alveolar phase of lung development, as it occurs in humans and can be delivered prematurely (GA 28th). To date, a comparative transcriptomic analysis is lacking. The aim of the study was to compare the relevant gene expression (GE) profiles of both species to evaluate the rabbit translational potential as a BPD model.
Methods: GE analysis was performed on lung samples from term (GA 31th) and preterm (GA 28th) rabbits and compared with the mouse lung GE dataset (GA 18.5th and GA 21th) generated by Beauchemin K.J. et al (GSE74243). Pathways enrichment analysis was performed based on differentially expressed genes identified in each species (GA 18.5th vs GA 21th and GA 28th vs GA 31th). Common pathways involved in lung development of preterm rabbits and term mice were evaluated.
Results: Lung development-related pathways such as cell cycle and mitosis-related processes were significantly enriched in both GA 18.5th mice and preterm-delivered (GA 28th) rabbits lungs, compared to their term counterparts. Common pathways, including angiogenesis, vasculature development, humoral immune system, and leukocyte migration, were found to be enriched in both species delivered at term, despite their different lung developmental phases. In contrast, no enriched common pathways emerged from the comparison between preterm rabbits and term mice.
Conclusion: Our analysis revealed that common enriched pathways are present in mice and rabbits born both preterm and term, despite their different lung development phases. Since preterm delivery is not feasible in mice, this study suggests a potential higher translational of the preterm rabbit model for studying the dysregulation of lung development-related pathways, leading to BPD in humans.
Ricci F., Casiraghi C., Catozzi C., Aquila G., Salomone F. & Villetti, G. are Chiesi employees. Other authors have no conflict of interest.
ID 287. The role of transforming growth factor beta isoforms in the development of bronchopulmonary dysplasia
Rebecca Calthorpe1*, Alan Smyth1, Amanda Tatler1
1University Of Nottingham, Nottingham, United Kingdom
Background: Bronchopulmonary dysplasia (BPD) is the most common complication of prematurity. Mechanical ventilation is an essential treatment strategy in the care of extremely preterm infants, however it also contributes to BPD development. An important signalling pathway that is relevant lung development, remodelling and BPD development is the transforming growth factor beta (TGFβ) signalling pathway. TGFβ exists as three isoforms; TGFβ1, TGFβ2 and TGFβ3. Increased TGFβ1 results in increased matrix deposition and fibrosis, whilst caffeine inhibited TGFβ1 activation in epithelial cells and reduced fibrosis in ex-vivo precision cut lung slices in mice. The role of TGFβ2 and TGFβ3 in fibrosis, BPD development and the impact of caffeine and other medications commonly prescribed in the prevention or treatment of BPD on these isoforms are currently less well understood.
Methods: Immortalised human bronchial epithelial cells (iHBECs) were exposed to cyclical mechanical stretch (CMS) at 15% elongation, 1 Hz vs control using the Flexcell system for up to 48 h and results analysed by western blot and Elisa. Additionally, iHBECs were exposed to caffeine 50 µM or dexamethasone 10 µM (0-48 h) and TGFβ isoform expression measured by real time qPCR.
Results: CMS increased TGFβ activation, demonstrated by increased pSmad2 at both 4 and 24 h, compared with unstretched cells. Furthermore, caffeine and dexamethasone demonstrated TGFβ isoform specific effects. Caffeine citrate showed a >10-fold increase in TGFβ2 expression from 0 to 48 h which was not seen with the other isoforms, while dexamethasone showed a trend towards increased TGFβ3 expression by 48 h (p = 0.07).
Conclusion: Based on these data, this suggests CMS used to mimic mechanical ventilation in a neonate increased TGFβ activation. This may be responsible for the increased fibrosis seen following mechanical ventilation, thus contributing to BPD development. Furthermore, caffeine and dexamethasone may have TGFβ isoform specific effects. A more detailed understanding of the role of TGFβ isoforms in fibrosis and BPD development is essential.
AS reports grants from Vertex and expenses from Teva and Vertex, outside the submitted work. RC is supported by a National Institute for Health Research (NIHR) Academic Clinical Fellowship.
ID 296. The gradient of arterial carbon dioxide to end-tidal carbon dioxide levels over the first week after birth in ventilated newborn infants
Nadja Bednarczuk1*, Emma Williams1, Theodore Dassios2, Anne Greenough1
1King’s College London, London, United Kingdom, 2King’s College Hospital NHS Foundation Trust, London, United Kingdom
Background: Monitoring of exhaled carbon dioxide levels by capnography is becoming routine in neonatal intensive care. The gradient of arterial carbon dioxide (PCO2) to end-tidal carbon dioxide (EtCO2) levels may be utilised to monitor patterns over time. In mechanically ventilated children, this relationship has been utilised during invasive ventilation demonstrating greater divergence in worsening pulmonary disease. The aim of this study was to establish whether similar changes occurred within the neonatal population and to describe the trends between PCO2-EtCO2 values during the first week after birth in infants of differing gestational ages.
Methods: A retrospective cohort study of infants who required invasive mechanical ventilation between January 2020–January 2021 was undertaken. Preterm infants required ventilatory support for pulmonary insufficiency and term infants were mechanically ventilated due to poor perinatal adaptation. There was no neonatal mortality before 28 days. Infants were ventilated with the SLE6000 ventilator and sidestream end-tidal capnography monitoring was incorporated into the circuit. Baseline demographics and ventilatory requirements were collected. The difference between simultaneously measured PCO2 and EtCO2 values were calculated and averaged per day of ventilation in the two gestational age groups.
Results: Sixty infants were included. Thirty preterm infants had a median (range) gestational age of 27.0 (22.6–30.6) weeks and birthweight of 890 (540–1785) grams and the 30 term infants had a median gestational age of 40.0 (37.3–41.9) weeks and birthweight 3330 (2455–4420) grams. The average PCO2-EtCO2 gradient during the first week after birth in preterm infants was 14.3 mmHg and in term infants 6.89 mmHg (p < 0.001). On day one after birth, the PCO2-EtCO2 gradient in preterm infants was 10.7 mmHg higher than in term infants (22.0 versus 11.3 mmHg). At day 7, this difference reduced to 4.6 mmHg (11.1 versus 6.5 mmHg). This longitudinal convergence was likely due to improving respiratory status in the preterm infants (Fig. 1).
Conclusion: In both groups, the gradient decreased over the first week after birth. An increase in the PCO2-EtCO2 gradient then could act as an early warning sign of respiratory deterioration and therefore alert clinicians to consider further investigation.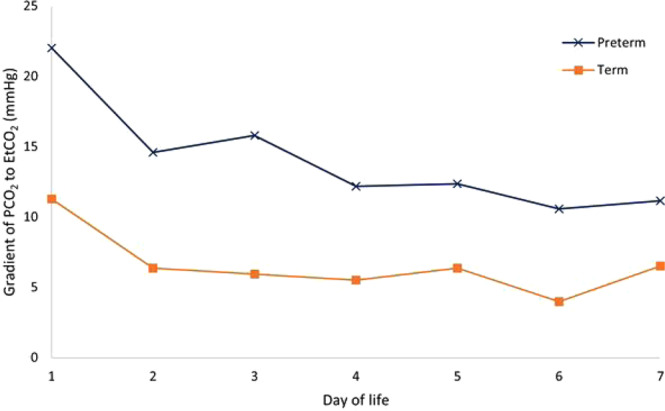
(ID 296) - Fig. 1. Trend in PCO2-EtCO2 gradient during the first week after birth.
None declared.
ID 318. Left ventricular diastolic function in very preterm infants
Camilla Rigotti1*, Daniela Doni1, Emanuela Zannin1, Abedulrhman Abdelfattah1,2, Maria Luisa Ventura1
1Fondazione Monza E Brianza Per Il Bambino E La Sua Mamma, Monza, Italy, 2Hashemite University, Zarqa, Jordan
Background: Pulmonary vascular disease contributes to the pathophysiology of bronchopulmonary dysplasia (BPD), but the specific role of postcapillary pathophysiology and left diastolic dysfunction as modulators of BPD is unclear. We aimed at (1) describing the trajectories of left heart diastolic function and (2) evaluating the association between left ventricular diastolic function and respiratory outcomes in very preterm infants.
Methods: We retrospectively analyzed data of 50 infants <32 weeks’ gestation who underwent echocardiogram evaluations at 7, 14, 28 days of postnatal age (PNA) and 36 and 40 weeks postmenstrual age (PMA). We assessed diastolic function by the E/E′ ratio. We compared E/E′ over time in infants with and without BPD using two-way ANOVA for repeated measurements. We assessed the association between E/E′ at 28 days and respiratory outcomes by linear regressions.
Results: We included 50 infants in the analysis (GA = 28.4 ± 2.3 weeks, birth weight = 1089 ± 366 g), 23 (46%) of whom developed BPD. In infants who developed BPD, E/E′ increased over time and was significantly higher at 14, 28 days PNA, 36 and 40 weeks PMA than at 7 days PNA (Fig. 1). E/E′ at 28 days PNA was significantly higher in infants with than without BPD, and it was significantly associated with the total duration of respiratory support (p = 0.003) and oxygen therapy (p = 0.003).
Conclusion: Our data suggest that left ventricular diastolic dysfunction may contribute to the pathophysiology of BPD and that serial echographic assessments of E/E′ may allow the identification of infants at risk of worse respiratory outcomes.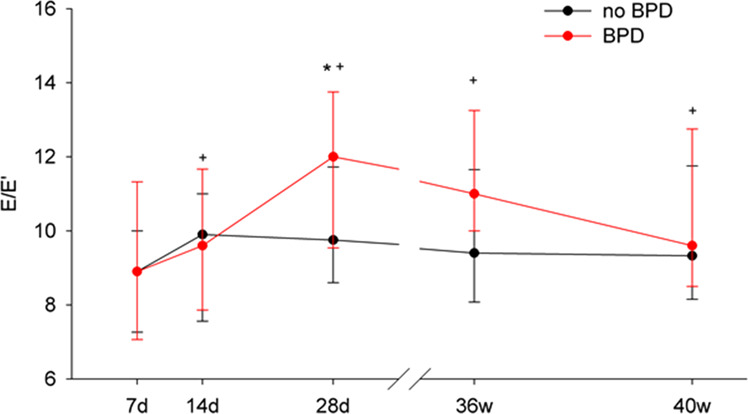
(ID 318) - E/E′ in infants with and without BPD. Data expressed as medians and IQR. *p < 0.05 vs no BPD, +p < 0.05 vs day 7 within BPD.
None declared.
ID 359. Lung ultrasound score evolution in premature newborns without bronchopulmonary dysplasia: a multicenter study
Almudena Alonso-Ojembarrena1*, Mónica de las Heras-Martín2, Alba Pérez-Pérez4, Victoria Aldecoa-Bilbao3, Paula Alonso-Quintela5, Javier Rodriguez-Fanjul7, Ana Concheiro-Guisán6, Alberto Trujillo-Fagundo8,Nerea López-Vazquez2, Rebeca Gregorio-Hernández4, Ignacio Oulego-Erroz5, Cristina Durán-Hernández6, Marcelino Pumarada-Prieto6
1Puerta Del Mar University Hospital, Cádiz, Spain, 2Basurto Universitary Hospital, Bilbao, Spain, 3Hospital Clínic Barcelona,MBCNatal - Barcelona Center for Maternal-Fetal and Neonatal Medicine., Barcelona, Spain, 4Gregorio Marañón Universitary Hospital, Madrid, Spain, 5Complejo Asistencial Universitario de León., León, Spain, 6Alvaro Cunqueiro Hospital, Vigo, Spain, 7Germans Trias i Pujol University Hospital., Badalona, Spain, 8Dr. Josep Trueta Universitary Hospital., Girona, Spain
Background: Lung ultrasound score (LUS) has proven as a valuable tool to predict bronchopulmonary dysplasia (BPD) in premature newborns, but the evolution of LUS in infants without moderate-severe BPD (msBPD) has not been studied.
Methods: We measured LUS in premature newborns born before 32 weeks, at birth, at three days of life (DOL), at one week, and then weekly until 36 weeks’ postmenstrual age (PMA). We excluded those with msBPD, and created four groups according to gestational age (GA) at birth: group 1 (23–25 weeks), group 2 (26–27 weeks), group 3 (28–29 weeks) and group 4 (30–32 weeks). To compare LUS between groups in each time evaluated, we calculated repeated measures ANOVA. In order to estimate LUS evolution in each group, we used linear multilevel mixed-effects regression to adjust for repeated measurements.
Results: 256 patients were included: 22 patients (9%) in group 1, 49 (19%) in group 2, 69 (27%) in group 3, and 116 (45%) in group 4. In group 1, LUS were different at 3 DOL, 1, 2, 3 and 4 weeks, versus 11 weeks (p < 0.02), and at the same moments, and 5 weeks (p < 0.04), compared to 12 weeks; in group 2, the differences were between birth compared to 11 (p = 0.018) and 12 weeks (p = 0.034); in group 3, we got significant differences at birth compared to 8 weeks (p = 0.006); and in group 4, at birth compared to 3 DOL, 1, 2, 3, 4, 5 and 6 weeks (p < 0.04). Model regression was estimated with a spline at 1 week, and showed statistical significance for the interaction between GA and time (p < 0.001), with an increase and a steady phase in the first weeks only in groups 1 and 2, as well as a decrease afterwards until the end of follow up. In the other groups, there was a decrease in LUS from birth until the end of the study, although more immature infants showed higher values of LUS at birth (see Fig. 1).
Conclusion: LUS in premature newborns born before 32 weeks without msBPD, decrease from birth until 36 weeks’ PMA, and the evolution is different according to GA at birth.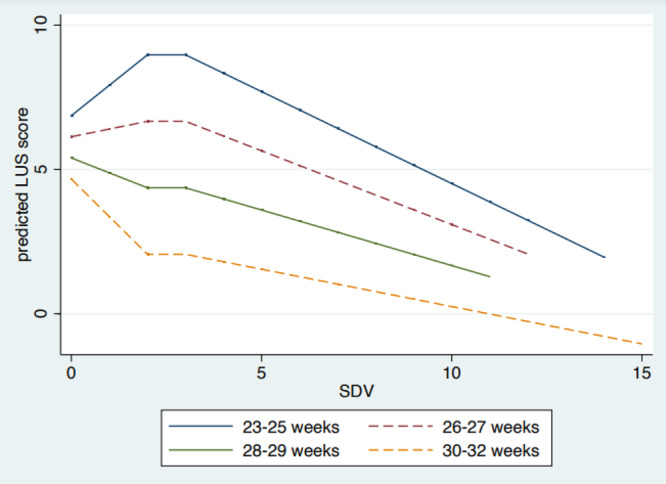
(ID 359) - Fig. 1. Predicted LUS evolution in premature infants without moderate-severe BPD according to gestational age at birth, by lineal multilevel mixed-effects regression.
None declared.
ID 366. Respiratory system reactance at 36 weeks post-menstrual age as a marker of lung disease in very preterm infants
Emanuela Zannin1*, Camilla Rigotti1, Roland Neumann2, Raffaele Dellacà3, Sven Schulzke2, Maria Luisa Ventura1
1Fondazione Monza E Brianza Per Il Bambino E La Sua Mamma, Monza, Italy, 2University Children’s Hospital Basel UKBB, Basel, Switzerland, 3Politecnico di Milano, Milano, Italy
Background: Bronchopulmonary dysplasia (BPD) is the most common morbidity of preterm birth and is associated with respiratory problems that can persist into adulthood. Functional markers of lung disease would facilitate the evaluation of clinical interventions and outcome prediction. This study aimed to evaluate whether lung mechanics assessed non-invasively by the forced oscillation technique (FOT) would be associated with the severity of lung disease in very preterm infants at 36 weeks of post-menstrual age (PMA).
Methods: We studied infants below 32 weeks’ gestation at 36 weeks PMA. We applied FOT using a mechanical ventilator (Fabian HFOi, Vyaire) that superimposed small amplitude oscillations (10 Hz) on a continuous positive airway pressure (5 cm H2O), and we computed respiratory system reactance (Xrs) from the flow and pressure signals measured at the airways opening. We compared Xrs between BPD groups (classified according to the 2001 National Institute of Health definition) using one-way ANOVA on ranks. We assessed the association between Xrs and the total duration of respiratory support by linear regression.
Results: 49 infants were measured (median (IQR) GA = 29.6 (28.2, 31.0) weeks, birth weight 1170 (993, 1530) g). 38 (78%) infants were classified as no BPD, 5 (10%) as mild BPD, and 6 (12%) as moderate-severe BPD. Xrs was significantly lower in infants with moderate-severe BPD than in infants without BPD (Fig. 1), indicating reduced respiratory system compliance. Xrs presented a statistically significant negative association with the total duration of respiratory support, which persisted after adjusting for gestational age, postnatal age, weight z-score and sex.
Conclusion: FOT is a non-invasive bedside tool for lung function testing that has the potential to provide physiological markers of lung disease. Indeed, Xrs measured at 36 weeks PMA reflects the severity of lung disease.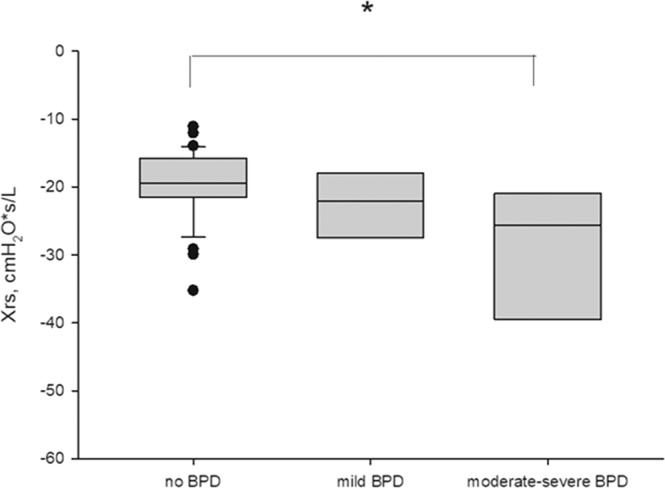
(ID 366) - Fig. 1: Respiratory system reactance (Xrs) in infants with no, mild and moderate-severe BPD. *p < 0.05 vs no BPD.
Politecnico di Milano, the institution of RD, has received research grants from Autronics and Vyaire not related to the topic of this study.
ID 386. Duration of invasive mechanical ventilation has small influence on diaphragmatic growth in preterm infants
Almudena Alonso-Ojembarrena1*, Julia Rodriguez-Medina2, Alicia Morales-Navarro2, Blanca González-Haba Martínez1
1Puerta Del Mar Universitary Hospital, Cádiz, Spain, 2University of Cádiz, Cádiz, Spain
Background: Diaphragm shortening fraction (DSF) has been used to predict extubation failure and diaphragm disfunction in adults and children. However, the influence of invasive mechanical ventilation (IMV) in this measure has been poorly studied in preterm infants.
Methods: We conducted an observational study including preterm infants born before 32 weeks (PT32w), with DU at birth, 3 days of life (DOL), and weekly until 36 weeks' postmenstrual age (PMA) or discharge. We excluded infants with major malformations or chromosomopathies. We measured diaphragm inspiratory and expiratory thickness (DIT and DET) and shortening fraction (DSF) in the apposition zone of the left side of the thorax. As the main variable that influences diaphragm growth is birth weight, patients were divided in two groups: less or higher than 1000 g; and in three groups according to the duration of IMV: 0–3 days, 3–12 days or >12days (P25, P50 and P75 in our sample). We compared DIT, DET and SF between groups using ANOVA, and we also calculated a multilevel mixed-effects regression model to predict the three measures’ evolution on time, using birth weight and IMV days as effect modifying variables.
Results: One hundred and eighteen patients were included: 53 (45%) weighted less than 1000 g at birth. Fifty-six (47%) had less than 3 IMV days, 20 (17%) 3–12 days and 42 (36%) more than 12 days. DIT differences were not significative at any time point using ANOVA (Fig. 1). However, birth weight and IMV days were related to DIT and DET change on time according to multilevel mixed-effects (p < 0.001 for both). On the other hand, DSF didn’t change throughout the duration of the study in any group.
Conclusion: Days of IMV influence the DIT and DET growth in PT32w since birth until 36 weeks’ PMA or discharge, but the main variable related to diaphragm grow is birth weight. DSF does not change since birth until 36 weeks’ PMA or discharge.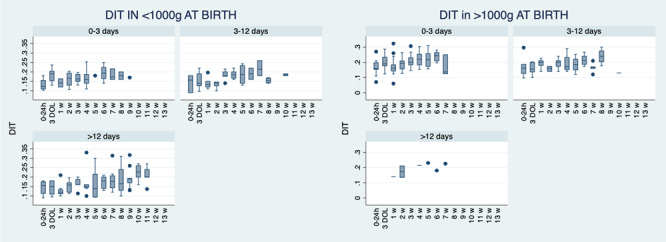
(ID 386) - Diaphragm inspiratory thickness evolution on time in preterm infants born before 32 weeks, according to birth weight and days on invasive mechanical ventilation.
None declared.
ID 394. Evaluation of early rescue high-frequency ventilation to very low birth weight infants
Arthur Oliveira1, Taina Ferrari1, Mauricio Lauriano1, Davi Aragon1, Fábia Celini1, Cristina Calixto1, Cristina Ferreira1, Adriana Carnevale1, Ana Beatriz Gonçalves1, Walusa Gonçalves-Ferri1*
1Hospital Das Clínicas De Ribeirão Preto - FMUSP/RP, Ribeirão Preto, Brazil
Background: High-frequency ventilation (HFV) uses small volumes to preserve the structure and architecture of the lung parenchyma. However, the most frequent indication is when conventional mechanical ventilation fails (severe lung conditions). In our hospital, we indicate early rescue HFV (better conditions lungs). This study evaluates the outcomes related to the early rescue to high-frequency ventilation in preterm infants.
Methods: Patients <1500 g who required HFV were evaluated through a retrospective cohort study from January 2017 to December 2020.
The neonatology team performed the indication for HFV. The patients were divided into two groups according to HFV indication: early rescue group, following the institutional protocol (mean airway pressure > 10 and/or driving pressure > 14); and the control group (late rescue), which received indication only if conventional ventilation failed; late rescue (RR > 60 bpm and/or driving pressure > 20 cm H2O).
The variables evaluated: development of pneumothorax, presence of pulmonary hemorrhage, bronchopulmonary dysplasia (BPD), the severity of BPD, and failure of extubation, days of ventilation, death related to HFV, and severe neurological outcome(delayed neuro-psychomotor development (DNPM) and/or IVH > III/IV Volpe criteria).
To estimate the relative risks, simple and multiple log-binomial regression models were adjusted. Gender, gestational age, and antenatal steroids were the covariates. The hazard ratio was estimated using the Cox proportional hazards model to compare the groups concerning mechanical ventilation days, considering the same covariables mentioned above. The software used was R 4.0.5 and SAS 9.4.
Results: 139 children used high-frequency ventilation, with 98 newborns receiving early rescue and 41 newborns receiving late rescue. The early rescue and late rescue groups had, respectively: mean gestational age 26.1 (SD: 2.2) versus 26.4 (SD: 2.4) weeks and birth weight 777.3 g (SD: 254.6) versus 797.4 g (SD: 260.3).
There was no association between early rescue and unfavorable lung or severe neurological outcomes.
Early rescue presented as protective factor to death (AdjRR: 1.64 (1.05; 2.60)) and to ventilation mechanical length (AdjHR: 0.66 (0.45; 0.97)).
Conclusion: The early rescue HFV to VLBW infants decreased mortality and is associated with less ventilation mechanical length.
(ID 394) - Table 1: Multiple log-binomial regression of pulmonary and neurological outcomes according to groups.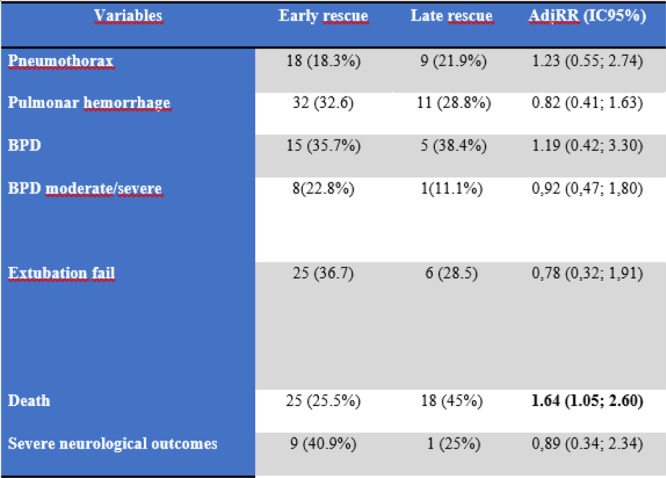
None declared.
ID 429. Fetal predictors of neonatal respiratory failure in congenital pulmonary malformations
Caroline Archambeau1,3*, Jean-Marc Biard1, Eddy Bodart2, Olivier Danhaive1
1Saint-Luc University Hospital, Brussels, Belgium, 2CHU UCL Namur - site de Godinne, Yvoir, Belgium, 3Jolimont Hospital, La Louvière, Belgium
Background: Congenital pulmonary malformations may result in severe respiratory symptoms at birth in a subset of cases. Our aim was to identify antenatal factor predicting such risk.
Methods: The study cohort included 39 cases of congenital pulmonary airway malformations (CPAM), pulmonary sequestration (PS) and other lung focal developmental anomalies diagnosed prenatally and treated from 2008 to 2019 at Saint-Luc University Hospital, a level IV national reference center; infants with congenital diaphragmatic hernia, tracheal defects and multiple congenital anomalies were excluded. When available, estimated lesion volume on fetal US were compared between the groups of infants with neonatal respiratory failure and those asymptomatic at birth.
Results: Gestational ages were 35.5 ± 4.1 weeks (mean ± SD) for the respiratory failure group vs. 38.9 ± 1.2 weeks for the asymptomatic group (Student’s T-test, p = 0.005). Birthweight z-scores were similar for both groups. The male/female ratio was 54%. 12 infants (31%) required a NICU hospitalization for respiratory failure. Two required invasive ventilation, seven non-invasive ventilation, one nasal canula O2 and two home monitoring for persisting tachypnea and occasional desaturations. One infant had a pneumothorax. Four required neonatal surgery, two of which died.
Fetal predicting factors: Lesion volume on fetal US was significantly larger in the respiratory failure group (29.5 ± 11.6 cm3) than in the asymptomatic group (19.0 ± 5.6 cm3) (Student’s T-test, p = 0.02), see figure. These lesions were predominantly CPAM in the respiratory failure group (10 CPAM/3 PS), and PS in the asymptomatic group (11 CPAM/13 PS/1 lobar emphysema/1 bronchogenic cyst) (Fisher’s test, p = 0.1). Six infants in the whole cohort required invasive fetal intervention for significant mediastinal shift and/or hydrops (thoraco-amniotic shunts and/or thoracocentesis): five of these ended up in the respiratory failure group vs. one in the asymptomatic group (Fisher’s test, p < 0.001); two were delivered prematurely (29 and 30 weeks).
Conclusion: The main predictor of neonatal respiratory failure was the size of the lesion on fetal US and the presence of significant mediastinal shift or hydrops. Our data suggest that fetuses with congenital pulmonary malformations >20 cm3 and/or requiring fetal intervention should be delivered in level III/IV centers with NICU and neonatal surgery services available.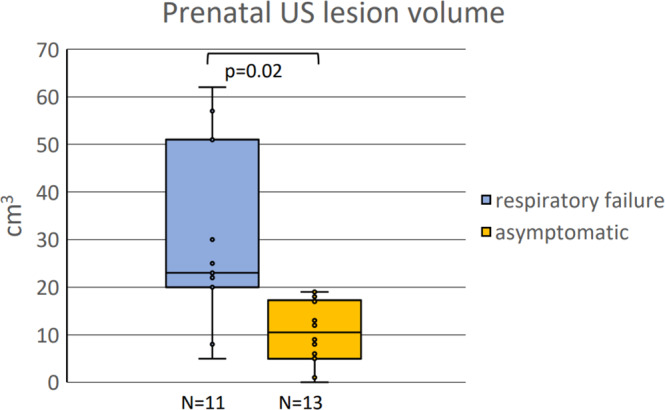
(ID 429) - Prenatal US lesion volume
None declared.
ID 452. HFV is an effective starting type of respiratory support in ELBW premature infants in the delivery room with severe RDS: a prospective, randomized, pilot study
Aleksei Mostovoi1*, Anna Karpova1, Nikolai Volodin2, Nikolai Karpov3
1State budgetary institution of health care of Kaluga region «Kaluga regional clinical hospital», Kaluga, Russian Federation, 2Russian Association of Perinatal Medicine Specialists (RASPM), Moscow, Russian Federation, 3State budgetary institution of health care of Yaroslavl region "Tutaev’s Central district hospital", Yaroslavl, Russian Federation
Background: When performing mechanical ventilation through the endotracheal tube in the delivery room, it is important to take into account the fact that the tidal volume in ELBW infants with RDS usually does not exceed 3.8 ml/kg (2.8-4.7 ml/kg). Severe surfactant deficiency determines high compliance and short time constant. It turns out that when performing mechanical ventilation in premature infants with ELBW and severe RDS, based on the physiological properties of the lungs, it is necessary to select such a ventilation mode in which a small amount of gas will enter the lungs in combination with a short inspiration time. Consequently, to ensure adequate gas exchange and maintain the necessary minute ventilation of the lungs, a frequency will be required several times higher than the average physiological one.
Objective: Comparison of two methods of initial respiratory support: high-frequency positive pressure ventilation (HFPPV) and conventional mechanical ventilation (CMV) in extremely low birth weight (ELBW) infants.
Materials and methods: prospective, randomized, pilot study, carried out in one level III perinatal center. Thirty-two ELBW babies was randomly separated in two groups: group A—HFPPV (n = 17), group B— CMV (n = 15).
Results: The recovery time for heart rate more than 100 beats per minute in group A was faster than in group B (33.9 vs. 79.2 s; p = 0.002). Maximum FiO2 for the period of staying in hospital was significantly higher in group B (0.37 vs. 0.73; p < 0.001). Mortality in CMV group was significantly higher (0% versus 27%; p = 0.038).
Conclusion: HFPPV in the delivery room in ELBW babies effectively restores heart rate, reduces the risk of lungs injury and the risk of death before discharge from the hospital.
Not declare.
ID 516. Nasal high flow to optimise stability during intubation in neonates: results of the NOSI pilot trial
Jason Foran1*, Carmel Moore1, Shirley Moore1, Jyothsna Purna1, Anna Curley1
1National Maternity Hospital, Holles Street Ireland, Dublin, Ireland
Background: Adult studies of patients with acute respiratory failure requiring intubation, have demonstrated that high-flow heated and humidified oxygen via nasal cannulae (HFNC) during intubation reduces oxygen desaturation. We hypothesised that in neonates requiring intubation the use of HFNC at 6 L/min and FiO2 of 1 would decrease the duration of hypoxia.
Methods: Setting: Tertiary neonatal unit. All babies requiring intubation in the neonatal unit included. Randomised controlled two-arm trial (RCT). Computer-generated randomization sequence used. Ethics committee approved deferred consent as intubation is an emergency procedure. Premedication with fentanyl, atropine and suxamethonium. Real time second by second data retrieved from clinical monitor. Intervention: pre-oxygenation/ventilation with Neopuff Infant Resuscitator device followed by HFNC 6L/min, FiO2=1, at time of laryngoscopy. Control: pre-oxygenation/ventilation with Neopuff then HFNC applied with zero flow. Primary outcome: cumulative duration of hypoxaemia <75% up to (ETCO2 detector confirmed) successful intubation. Study blinded to data collector/analyst. Simultaneous running of suction adjacent to baby blinded intubators to potential sound of HFNC at nares. Secondary outcome variables included oxygenation quality, time to SpO2 < 65%, 75%, 85%, lowest oxygen saturation and complications related to intubation. Mann Whitney U test used for analysis of primary outcome.
Results: 36 babies enrolled ; 24 preterm <34 weeks gestation, 12 ≥34weeks. Within the preterm cohort median cumulative time <75% oxygen was 39 vs 42 s, intervention vs control, p = 0.99. In the group> 34 weeks median was zero seconds in both groups. Mean time to reach 75% in preterm group was 62.6s vs 53.8s intervention vs control, p = 0.11. Group ≥34 weeks mean was 37.7s vs 45.5s (p=0.37). Preterm: mean time to <60% saturation was 90.3 vs 63.6 s in the control arm p=0.04. Babies showed increased instability in control group following attempts lasting >1 min (see Fig.).
Conclusion: We demonstrated that this HFNC trial was feasible. Although this pilot study did not detect a significant difference in time below 75% the trial has provided baseline data to adequately power a RCT of HFNC with a similar primary outcome. We noted that use of HFNC resulted in a statistically significant, reduced rate of desaturation (averaged over 10 s) within infants <34 weeks.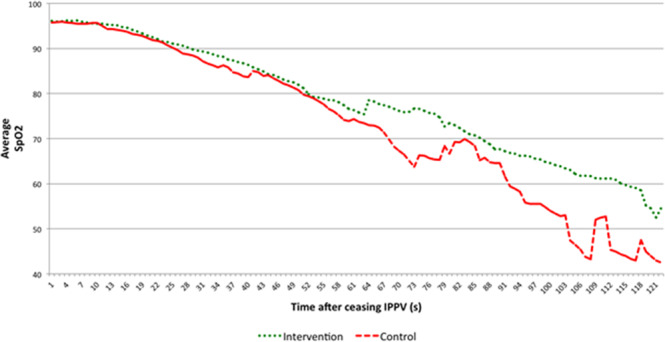
(ID 516) - Average SpO2 from cessation of IPPV for intervention and control arms of <34+0 week infants
None declared.
ID 533. Utilising population data to develop safer personalised preterm infant clinical treatments and trials
T’ng Chang Kwok1*, Don Sharkey1
1University of Nottingham, Nottingham, United Kingdom
Background: Preterm birth below 28 weeks gestation is associated with significant mortality and morbidity. Reducing these through randomised controlled trials (RCTs) often requires large numbers of infants recruited over many years. Identifying more accurately those at greatest risk of death or serious morbidity would allow better RCTs targeting those most likely to benefit and reducing potential harm in those least likely to. We aimed to estimate the number of infants excluded from the recent early low-dose hydrocortisone RCT (PREMILOC, Baud, Lancet 2016) who died or developed bronchopulmonary dysplasia (BPD); and those included with minimal likely benefit.
Methods: Routinely collected data from infants <32 weeks gestation admitted to 185 neonatal units in England and Wales from 2010 to 2017 were extracted. The combined prevalence of mortality and BPD by gestation, birthweight and gender was determined. We estimated the number of infants 28–31 weeks gestation who died or developed BPD and those <28 weeks gestation least likely to benefit. We also compared respiratory support requirement on neonatal discharge versus 36 weeks corrected gestational age (CGA).
Results: 62,864 infants were analysed. The combined prevalence of death/respiratory support at 36 weeks CGA and on discharge respectively varies with gestation, birthweight and gender (Figure). For example, risk of death/BPD for a small-for-gestational-age 28-week infant changes from 75% to 46% (male) or 61% to 35% (female) for death/respiratory support at discharge.
Of the 42,873 infants ≥28 weeks gestation, 8,368 (19.5%) died or developed BPD and may have benefited from early hydrocortisone. Between 36 weeks and discharge, 283 (1.8%) of the surviving 15,652 infants <28 weeks died, and 4877 (31.2%) came off all respiratory support.
Conclusion: This study provides novel, contemporary data on mortality and respiratory outcomes across a national population of high-risk infants including at neonatal discharge. Using prophylactic hydrocortisone as an example, we show that about a fifth of very preterm infants could potentially benefit from treatment and nearly a third of extremely preterm infants would get little or no benefit. Utilising a few individual characteristics, it is possible to risk-stratify individual patients for particular treatments or inclusion in RCTs, providing personalised medicine and research.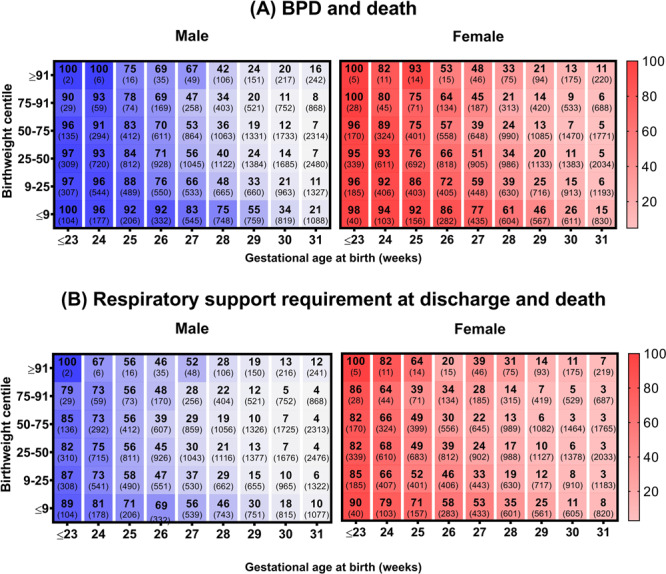
(ID 533) - Figure: Heat map depicting the combined a BPD and death (n = 62,334); b post-discharge respiratory support requirement and death (n = 62,113) prevalence (% (n)) of very preterm infants by gestation, birthweight and gender.
None declared.


