Abstract
Background
We aimed to investigate the prevalence of poor uncorrected visual acuity and the difference among students with different ages and residential areas in the Northeast of China. The relationships between screen time, nighttime sleep duration, and poor uncorrected visual acuity would be explored.
Methods
It was a cross-sectional study using multi-stage stratified random sampling method to recruit participants. 2149 students have completed questionnaires and underwent visual acuity examinations. The dose–response curve method was applied to examine the non-linear associations between sleep duration and poor uncorrected visual acuity under different screen time subgroups.
Results
The overall prevalence of poor uncorrected visual acuity and severe poor uncorrected visual acuity was 84.7% and 63.3%, respectively. The dose–response curve showed the odds ratios (ORs) of sleep duration for the poor uncorrected visual increased relatively slowly when screen time <1 hour, then increased dramatically in screen time ≥1 hours. The ORs of sleep time and poor uncorrected visual acuity showed a U-shaped change trend among students with 2 or more hours of screen time every day.
Conclusion
We found associations between nighttime sleep duration and poor uncorrected visual acuity in adolescents. However, these associations were not consistent across all screen time categories.
Keywords: adolescent, poor uncorrected visual acuity, prevalence, screen time, sleep duration
Introduction
The vision problem has become a global challenge in recent years, especially for developing countries. 1 In recent decades, the prevalence of myopia has dramatically increased in China, especially among younger population. 2 The World Health Organization released the first World Vision Report on October 8, 2019, revealing that over 2.2 billion people have a visual impairment or blindness worldwide. 3 In East Asia, the prevalence of poor uncorrected visual acuity among teenagers exceeded 80%. 4 According to surveys developed by the National Health Commission and the Ministry of Education of the People’s Republic of China and other departments, the overall rate of myopia among Chinese children and adolescents was 53.6% in 2018, which occupied 14.5% of 6-year-old children, 36.0% of primary school students, 71.6% of junior high school students, and 81.0% of senior high school students. 5 Uncorrected visual acuity has been widely used as a proxy measure for myopia in children in previous studies, and it has achieved a satisfactory sensitivity and specificity profile for myopia screening. 6 Therefore, poor uncorrected visual acuity in children provides a proxy measure of myopia.
Before the year 2000, electronic products (eg, televisions, computers, tablets, gaming consoles, and smartphones, etc.) were not common in China and the world. During that time, researchers found that main factors contributing to poor vision in adolescents were heavy schoolwork load, long-term reading and writing at close range, neglect of physical exercise, poor lighting condition in the learning environment, 7 and genetics. 8 After entering the 21st century, electronic media pervaded modern lives. In the United States, most school-aged children and adolescents spent around 7 hours per day in front of an electronic screen. 9 Approximately 60% of all Chinese adolescents have least 1 electronic product (eg, television, computer, mobile phone, video game console) in their bedrooms. 10 Ji et al reported that in China, 34.3% of all secondary school students spent 2 hours or more daily (and 13.5% spent ≥ 4 hours/day) watching televisions and 25.6% of all senior high school students spent 2 hours or more per day (and 5.5% spent ≥4 hour/day) on the internet. 11 Long screen time can affect vision, according to the American Academy of Ophthalmology (AOA); long screen time can lead to eye fatigue, redness, blurred vision, myopia, and other eye symptoms. 12 Kozeis found that staring at electronic screens regularly can lead to eye discomfort, blurred vision, fatigue, headaches, and other symptoms. 13 Taptagaporn 14 reported burning eyes and muscle pain were common symptoms resulted from long time use of electronic media. 14 Staying in front of electronic screens for an extensive period of time, regardless of the purpose, will make people more vulnerable to the risk of poor uncorrected visual acuity. 15
The consequences of excessive screen time on visual acuity have been addressed by numerous scholars. 16 The effects of screen time on sleep patterns and sleep qualities were also the focus of study for researchers around the world. 17 Recent reviews of studies that focused on school-aged children and adolescents documented a robust inverse association between screen time and sleep quality.18,19 Empirical evidences demonstrated that adolescents who spent more time using screens had shorter sleep duration, delayed bedtimes, later sleep latency, more sleep disturbance symptoms, and more severe sleep deficiency. Screen-based activities also delay bedtime or truncate total sleep time. For example, light produced from smartphones can suppress production of melatonin in human bodies, which will lead to less drowsiness, difficulty to fall into sleep, and results in non-restorative sleep. 20
Epidemiologic studies have consistently reported a U-shaped association between self-reported habitual sleep duration and adverse health outcomes such as mortality, incident heart disease, diabetes, and obesity. 21 However, the dose–response relationship between sleep duration and poor visual acuity, and the shape of this association were remained unclear and debated. Recently, some epidemiologic studies have investigated the relationship between sleep duration and poor visual acuity. The Korean National Health and Nutrition Examination Survey found a significant relationship between shorter sleep duration and poor visual acuity using population-based data from Korean adolescents aged 12–19 years old. 22 Another study on Japanese children found that poor sleep quality was significantly correlated with severe poor visual acuity.23 However, a study on Chinese children investigated the relationship between sleep duration and poor visual acuity, showing that they were not significantly associated. 24 Surprisingly, Xu et al 25 found that people with longer nighttime sleep duration would have higher risks of poor visual acuity from a community-based study of 5613 Chinese residents aged 60 years and older.
Inconsistencies in findings regarding the shape of the dose–response relationship between sleep duration and visual acuity may be partly because of screen time assessment. Summarized evidences from 67 studies in schoolchildren proposed that screen time is negatively associated with sleep duration in 90% of studies. 18 At present, the relationship between sleep duration and poor visual acuity remains controversial and has not been extensively evaluated. Furthermore, there were few studies that were interested in the associations between poor uncorrected visual acuity, sleep duration, and screen time.
Methods
Study Participants
The study took place in Jilin Province, one of the 3 provinces in the Northeast of China with a total population of 27.04 million and a total land surface of 187,400 square kilometers. 26 It has a temperate monsoon climate, with typical continental characteristics, namely, megathermal wet summers and dry cold winters. 27
This was a cross-sectional study, conducted from December 2017 to January 2018 in Jilin Province, designed to investigate the relationship between screen time, nighttime sleep duration, and poor uncorrected visual acuity among teenagers aged between 14 and 18 years old. Multi-stage stratified random sampling method was used to recruit the study sample. In Stage 1, all cities in Jilin Province were classified into 3 categories according to per capita gross national product: economically advanced cities, economically moderate cities, and economically behind cities. One city was randomly selected from each of these categories, for a total of 3 cities. In Stage 2, each city was further divided into suburban and urban areas based on their geographical locations, which made total of 6 unique areas. In Stage 3, two senior high schools were randomly selected from each urban district, and one senior high school was randomly selected from each suburban district. In Stage 4, we randomly selected 2 classes from each grade (grade 10, 11, 12) in each school. A total of 80 students were selected from each grade. Thus, the number of participants was “80 × 3 × (2 + 1) × 3 = 2160.” We calculated the sample size using a non-response rate of 10%. We added 8–10 students in each grade. Finally, we issued “2160 × (1 + 10%) = 2376” questionnaires.
As a result, we recruited 2184 students as the total participants for the study. After excluding subjects with missing sleep duration data (n = 15) and those with incomplete ID (n = 20), data from 2149 participants was admitted and analyzed.
Examination
We used a logarithm of the minimum angle of resolution (logMAR) chart by ophthalmologists. 28 LogMAR (using the Standard for Logarithmic Visual Acuity Charts, GB/T 11533-2011 of the Standardization Administration of the People’s Republic of China) is the “gold standard” used by majority of clinical trials or interventions. 29
The poor uncorrected visual acuity was defined as monocular visual acuity under 5.0, and severe poor uncorrected visual acuity was defined as monocular visual acuity under 4.5. 30
To calculate the body mass index (BMI), weight and height of participants were measured directly by trained personnel. Participants were classified according to their BMI following the established WHO classification: underweight (BMI <18.49), normal weight (BMI = 18.5–24.9), and overweight (BMI ≥25). 31
Questionnaire Survey
Sleep duration was assessed by a single item that asked respondents to report how many hours they slept each night on average in the past month. We divided all the participants into 3 groups according to the criteria created by the National Sleep Foundation’s recommendations as follows, short sleep duration: < 7 hours/d, medium sleep duration: 7–9 hours/d, and long sleep duration: ≥9 hours/d. 32
Participants reported their screen time by answering the question “How many hours per day did you spend on electronic items (eg, television, computer, mobile phone, video game console) in the past month?” The question has previously shown acceptable validity and reliability in the Chinese population. 33 Daily screen time was categorized as <2 hours/day and ≥2 hours/day. 34
We investigated factors including demographic informations: gender (male or female), residence (urban or suburban), mode of delivery (vaginal, cesarean and unknown), frequency of vigorous physical activity including running, swimming, and playing football or basketball per week (0, 1–4, 4–7 times/week), residence in school (yes or no), attending an after-school tutorial program (yes or no), smoking (yes or no).
Statistical Analysis
Descriptive statistics with frequency, median, interquartile range (Q1–Q3) were used to represent the visual acuity variables. The acuity visual variable was dichotomized and analyzed regarding their relationships with other parameters by using univariate analysis. Demographic variables like gender, residence, mode of delivery, frequency of vigorous physical activity, residence in school, BMI, attending an after-school tutorial program, and smoking were included as covariates in the adjusted models. Binary logistic regression was performed to analyze ORs for nighttime sleep duration, screen time, and poor uncorrected visual acuity.
The dose–response curve can provide the continuous ORs, 35 especially for the non-linear associations between sleep duration and poor uncorrected visual acuity. In addition, the restricted cubic splines is one of the most ideal function models used in dose–response analysis, which allows the risk to vary without sudden jump from one interval to the next one. 36 Data analyses were carried out by R software (Version 3.0.2, 2013-09-25; R Foundation for Statistical Computing, http://www.cran.r-project.org/) The restricted cubic splines in the Hmisc package were used to investigate the dose–response curve of associations between sleep duration and poor uncorrected visual acuity.
Ethics Approval and Consent to Participate
Ethical approval was granted by the Institutional Review Board of Jilin University (2017-09-06). Before the study started, participants were asked to give their written consents to the research group after being orally informed about the study protocols. They had completed knowledge about the study procedures and understood that their personal information would be strictly protected and confidentiality would be maintained by the research group.
Results
The prevalence of poor uncorrected visual acuity and severe poor uncorrected visual acuity among students was 84.7% and 63.3%, respectively. 5.7% students have been identified with only right poor uncorrected visual acuity, 3.6% students with only left poor uncorrected visual acuity, 75.4% students were identified with poor uncorrected visual acuity on both side, and 15.3% students had normal vision. (Table 1).
Table 1.
Percentage of Participants in Visual Acuity Range.
| Characteristic | Right poor uncorrected visual acuity | Left poor uncorrected visual acuity | Both poor uncorrected visual acuity | None poor uncorrected visual acuity |
|---|---|---|---|---|
| All participants | 123(5.7) | 77(3.6) | 1620(75.4) | 329(15.3) |
| Gender | ||||
| Male | 58(5.8) | 34(3.4) | 728(73.2) | 174(17.5) |
| Female | 65(5.6) | 43(3.7) | 892(77.3) | 155(13.3) |
| Residence | ||||
| Urban | 87(6.1) | 48(3.4) | 1114(78.1) | 178(12.4) |
| Suburban | 36(5.0) | 29(4.0) | 506(70.1) | 151(20.9) |
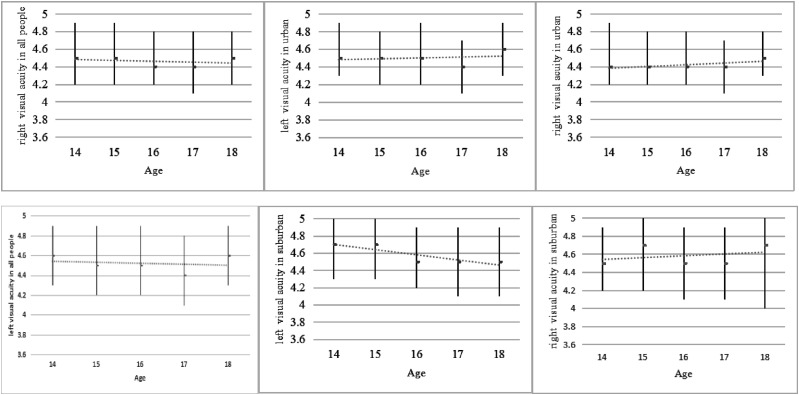
A significant negative correlation was found between visual acuity of both eyes and age among all participants aged 14–18 years old (left: r = −.079, P < .001; right: r = −.067, P = .002). And statistical difference on visual acuity level was found between the urban and suburban areas for both eyes (P < .001) (Figure 1).
Figure 1:
The visual acuity of students with age of 14–18 years in all, urban, and suburban areas in China. For each age of year, the median with interquartile range of visual acuity was presented.
The results of univariate and multivariate analyses of factors associated with poor uncorrected visual acuity status were shown in Table 2. Unexpectedly, after multivariate analyses, that study found that among those, participants who were living in urban areas (OR = 1.63, 95% CI = 1.24–2.15, P < .001), screen time more than 2 hours/day (OR = 1.62, 95% CI = 1.01–2.28, P = .004), and sleep duration more than 9 hours on average (OR = 1.51, 95% CI = 1.09–2.10, P = .024) were associated with a higher risk of poor uncorrected visual acuity.
Table 2.
Associations Between Poor Uncorrected Visual Acuity Status and Possible Risk Factors.
| Characteristic | Univariate analysis | Multivariate analysis | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P | OR | 95% CI | P | |
| Gender | ||||||
| Female | 1.00 | 1.00 | ||||
| Male | .73 | .57–.92 | .007 | .83 | .63–1.09 | .179 |
| Residence | ||||||
| Suburban | 1.00 | 1.00 | ||||
| Urban | 1.87 | 1.47–2.37 | <.001 | 1.63 | 1.24–2.15 | <.001 |
| Mode of delivery | ||||||
| Vaginal | 1.00 | 1.00 | ||||
| Cesarean | .66 | .50–.88 | .004 | .72 | .54–.96 | .025 |
| Unknown | 1.18 | .87–1.59 | .291 | 1.10 | .80–1.50 | .576 |
| Frequency of vigorous physical activity (times/week) | ||||||
| 0 | 1.00 | 1.00 | ||||
| 1–4 | .68 | .52–.86 | .002 | .56 | .44–.80 | .001 |
| 4–7 | .63 | .43–.91 | .014 | .66 | .43–1.03 | .069 |
| Screen time (hours) | ||||||
| <1 | 1.00 | 1.00 | ||||
| 1–2 | 1.44 | 1.06–1.96 | .021 | 1.56 | 1.19–2.04 | .001 |
| >=2 | 1.58 | 1.05–2.38 | .027 | 1.62 | 1.01–2.28 | .004 |
| BMI | ||||||
| Low | 1.00 | 1.00 | ||||
| Normal | 1.48 | 1.14–1.92 | .003 | 1.31 | .99–1.72 | .053 |
| High | 1.53 | 1.09–2.18 | .014 | 1.17 | .80–1.69 | .422 |
| Residence in school | ||||||
| Yes | 1.00 | 1.00 | ||||
| No | .57 | .44–.74 | <.001 | .708 | .53–.94 | .016 |
| Attending an after-school tutorial program | ||||||
| No | 1.00 | 1.00 | ||||
| Yes | 1.86 | 1.44–2.40 | <.001 | 1.39 | 1.05–1.86 | .023 |
| Sleep duration daily(hours) | ||||||
| <7 | 1.00 | 1.00 | ||||
| 7–9 | 1.29 | 1.04–1.61 | .045 | 1.13 | .88–1.45 | .352 |
| >=9 | 1.30 | 1.02–1.66 | .032 | 1.51 | 1.09–2.10 | .024 |
| Smoking | ||||||
| Yes | 1.00 | 1.00 | ||||
| No | .72 | .52–.99 | .048 | .98 | .69–1.39 | .895 |
Our study revealed a negative association between screen time and sleep duration (r = -.203, P < .001). Results from the regression analysis examining the associations between screen time and sleep duration with poor uncorrected visual acuity were shown in Table 3. Compared to participants with less than 1 hour of screen time every day, participants with 1–2 hours of screen time daily and short sleep duration were associated with higher poor uncorrected visual acuity risk (OR = 1.68, 95% CI: 1.26–2.21). However, participants with over 2 hours of screen time every day had highest risk of developing poor uncorrected visual acuity regardless of their sleep duration (short: OR = 2.07, medium: OR = 1.20, long: OR = 1.49).
Table 3.
Sleep Duration Classified Associations Between Screen Time and Poor Uncorrected Visual Acuity.
| Screen time(hours) | Short sleep | Medium sleep | Long sleep | |||
|---|---|---|---|---|---|---|
| Crude OR (95% CI) | Adjusted a OR (95% CI) | Crude OR (95% CI) | Adjusted a OR (95% CI) | Crude OR (95% CI) | Adjusted a OR (95% CI) | |
| <1 | Ref | Ref | Ref | Ref | Ref | Ref |
| 1–2 | 1.69(1.28–2.23)** | 1.68(1.26–2.21)** | 1.03(.83–1.26) | 1.03(.81–1.24) | 1.12(.71–1.78) | 1.29(.92–1.79) |
| >=2 | 2.18(1.46–3.24)** | 2.07(1.47–2.91)** | 1.32(1.13–1.55)** | 1.20(1.03–1.40)** | 1.66(1.25–2.21)** | 1.49(1.11–1.99)** |
aAdjusted for gender, residence, mode of delivery, frequency of vigorous physical activity, BMI, residence in school, attending an after-school tutorial program, smoking.
**P < .001.
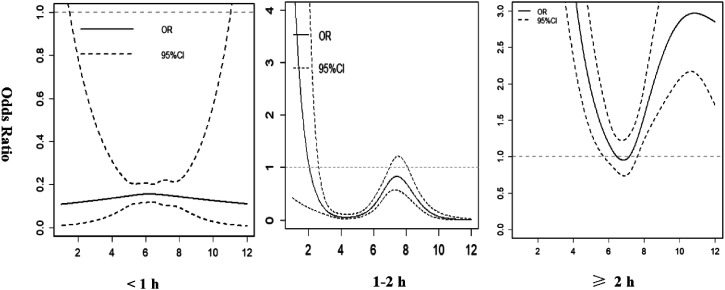
Figure 2 showed how the ORs of sleep duration developed in poor uncorrected visual acuity by screen time. The ORs of sleep duration among poor uncorrected visual acuity with screen time (<1 hour) were fairly low as sleep duration increased. The ORs of higher short sleep duration in poor uncorrected visual acuity were extremely greater than long sleep duration in poor uncorrected visual acuity among screen time (1–2 hours). The ORs of sleep time and poor uncorrected visual acuity showed a U-shaped change trend among screen time (≥2 hours).
Figure 2.
Associations between sleep duration and poor uncorrected visual acuity with 95% CI (n = 2149) in Jilin. The solid line represents OR, and the dotted line represents 95% CI.
Discussion
In this population-based study, the prevalence of poor uncorrected visual acuity and severe poor uncorrected visual acuity in high school students in the Northeast of China was 84.7% and 63.3%, respectively. Compared with the reported prevalence of poor uncorrected visual acuity from 2014 Chinese National Surveys on Students’ Constitution and Health (CNSSCH), the overall prevalence of poor uncorrected visual acuity was 66.6%. The prevalence of poor uncorrected visual acuity ranged from 50.6% to 76.2% in each province (autonomous region, municipality) in 2014 CNSSCH. 37 In mainland of China, a large diversity of visual acuity was found among different geographic regions. 38 These data suggested that poor uncorrected visual acuity was a serious public health problem in Jilin province along with other areas of China. The increase in prevalence of poor uncorrected visual acuity was largely because of genetics; another possible reasons could be the change of environment, educational achievement, degree of urbanization, geographical regions, and meteorological features. 39 Apart from those, one of the main reasons of higher prevalence of poor uncorrected visual acuity in Jilin province is that long harsh winter contributes to high prevalence of poor uncorrected visual acuity among residents living in the Northeast of China because the coldness reduces residents’ motivations to do outdoor activities, which in turn increases the likelihood for more indoor activities that will exhaust eyes.
We used binary logistic regression to perform to identify poor uncorrect visual acuity risk factors. Our study was consistent with the previous study.40-42 Urban, female, older students had a higher risk of developing poor uncorrect visual acuity. The results of our study was consistent with other researches in terms of outdoor activities, 43 near work activities, 44 and obesity. 45 Further implications can be drawn from our findings, as follows.
Screen time was believed to be one of the primary causes for the increasing of the prevalence of poor uncorrected visual acuity, which was consistent with previous study. 46 Our study revealed the negative associations of screen time with sleep duration (r = −.203, P < 0.001). Screen time could affect sleep through different mechanisms. Media use may directly affect sleep duration by replacing it due to its time consuming nature, or it may interfere with sleep duration through increased psychophysiological arousal caused by the stimulating contents of the material or through bright light exposure inherent in most electronic media devices. 17
Sleep duration is greatly affected by screen time, but the relationship between sleep duration and poor visual acuity needs further investigations. So we divided the screen time into different subgroups to explore dose–response relationships between sleep duration and poor visual acuity. The ORs for sleep duration among participants with poor uncorrected visual acuity in screen time (<1 hour) were fairly low as sleep duration increased. Therefore, screen time was identified as one of the primary causes for the increase of the prevalence of poor uncorrected visual acuity. In our study, the ORs for participants with short sleep duration in poor uncorrected visual acuity were extremely greater than long sleep duration in poor uncorrected visual acuity among screen time (1–2 hours). In other words, under the same conditions of screen time (1–2 hour/day), short sleep time has a higher negative impact on poor uncorrected visual acuity. Ayaki et al23 found an association between later bedtimes, shorter sleep duration, and poorer sleep quality with increased poor uncorrected visual acuity. Another finding of our research was that the ORs of sleep time and poor uncorrected visual acuity showed a U-shaped change trend for screen time more than 2 hours. In a Korean study, they found a U-shaped association between self-reported sleep duration and poor visual acuity. Very short (≤5 hours/night) and very long (≥ 9 hours/night) sleep duration were significantly associated with poor uncorrected visual acuity risk. 47
Our findings may have solved the question “why have a number of previous studies reported significant yet contradictory results ?” For example, results from a study that enrolled 15,136 Chinese children (age range 6–18 years) indicated an increased risk for poor visual acuity (adjusted-OR = 3.37) among those who slept less than 7 hours per night compared to those who slept more than 9 hours per night. 48 In contrast, another study of 1902 Chinese children (mean age 9.80 ± .44 years) identified a higher risk for poor visual acuity among those who slept longer every night (OR = 1.02). 24
We believed the reasons for these contradictory results about sleep duration and poor visual acuity was because they did not take screen time into consideration. According to our results, there was a different dose–response relationship between sleep duration and poor uncorrect visual acuity in different subgroups of screen time. Previous studies may have ignored the role of screen time and solely explored the relationship between sleep duration and poor visual acuity.
Our findings highlighted the impact of sleep duration on poor uncorrect visual acuity, although the underlying mechanisms remain unclear. Possible reason is a considerable overlap between the biological pathways controlling sleep and ocular developments. 49 Sleep is regulated by the circadian rhythm via melatonin, which is controlled by mutual interactions with retinal dopaminergic pathways. Ocular growth is also controlled by both dopamine and melatonin involved in ocular circadian physiology. 50
Conclusion
To summarize, our study has proposed that a high prevalence of poor uncorrected visual acuity of adolescents. We found associations between nighttime sleep duration and poor uncorrected visual acuity in adolescents. However, these associations were not consistent across all screen time categories.
Limitation
Our study was a cross-sectional design, which made it difficult to draw any causal inferences from the results. Furthermore, the sleep duration and screen time status of the participants were self-report, which might be subject to reporting bias. Finally, our team needs to further discuss and verify the relationship between screen time, sleep time, and poor visual acuity.
Acknowledgments
We would like to express our gratitude to Mengzi Sun for her assistance in this study.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported by a grant from the Jilin University (2019GJTD06).
ORCID iD
Songli Mei https://orcid.org/0000-0003-0507-6373
References
- 1.Resnikoff S. Global magnitude of visual impairment caused by uncorrected refractive errors in 2004. Bull World Health Organ. 2008;86(1):63-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li DZ. Overview of students’ physical health. Sport. 2017;16:80-84. [Google Scholar]
- 3.World Health Organization. World Vision Report ; 2019. https://www.who.int/zh/news-room/detail/08-10-2019-who-launches-first-world-report-on-vision. Accessed on 18 September 2020.
- 4.Qi SY, Li JW, Jia LD, et al. Factors associated with myopia in school children in China: the Beijing childhood eye study. PLoS One 2012;7(12):e52668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang Y. The 2018 national survey on myopia among children and adolescents. Commission NH; 2019. http://www.nhc.gov.cn/xcs/s7847/201905/11c679a40eb3494cade977f65f1c3740.shtml. Accessed on 10 September 2020. [Google Scholar]
- 6.Xiang F, He M, Zeng Y, et al. Increases in the prevalence of reduced visual acuity and myopia in Chinese children in Guangzhou over the past 20 years. Eye 2013;27(12):1353-1358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pan CW, Zheng YF, Anuar AR, et al. Prevalence of refractive errors in a multiethnic Asian population: the Singapore epidemiology of eye disease study. Investig Ophthalmol Vis Sci. 2013;54(4):2590-2598. [DOI] [PubMed] [Google Scholar]
- 8.Zhang Z, Xu G, Gao J, et al. Effects of e-learning environment use on visual function of elementary and middle school students: a two-year assessment-experience from China. Int J Environ Res Publ Health. 2020;17(5):1560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Strasburger VC, Council on Communications and Media . Children, adolescents, obesity, and the media. Pediatrics 2011;128(1):201-208. [DOI] [PubMed] [Google Scholar]
- 10.Wang H, Zhong J, Hu R, et al. Prevalence of high screen time and associated factors among students: a cross-sectional study in Zhejiang, China. BMJ Open 2018;8(6):e021493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ye JC, Jiao CT, China W. Empirical changes in the prevalence of overweight and obesity among Chinese students from 1985 to 2010 and corresponding preventive strategies. Biomed Environ Sci. 2013;26(1):1-12. [DOI] [PubMed] [Google Scholar]
- 12.Kokab S, Khan MI. Computer vision syndrome: a short review. J Evol Med Dent Sci. 2012;1(6):1223-1226. [Google Scholar]
- 13.Kozeis N. Impact of computer use on children’s vision. Hippokratia. 2009;13(4):230-231. [PMC free article] [PubMed] [Google Scholar]
- 14.Taptagaporn S. Computer use among children: health and social impacts. World Congress on Ergonomics. Beijing: Peking University; 2009. [Google Scholar]
- 15.Yang GY, Huang LH, Schmid KL, et al. Associations between screen exposure in early life and myopia amongst Chinese preschoolers. Int J Environ Res Publ Health. 2020;17(3):1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Iannotti RJ, Kogan MD, Janssen I, Boyce WF. Patterns of adolescent physical activity, screen-based media use, and positive and negative health indicators in the U.S. and Canada. J Adolesc Health. 2009;44(5):493-499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cain N, Gradisar M. Electronic media use and sleep in school-aged children and adolescents: a review. Sleep Med. 2010;11(8):735-742. [DOI] [PubMed] [Google Scholar]
- 18.Hale L, Guan S. Screen time and sleep among school-aged children and adolescents: a systematic literature review. Sleep Med Rev. 2015;21:50-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lebourgeois MK, Hale L, Chang AM, et al. Digital media and sleep in childhood and adolescence. Pediatrics 2017;140(suppl 2):S92-S96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Holzman DC. What’s in a color? The unique human health effect of blue light. Environ Health Perspect. 2010;118(1):A22-A27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Patel SR, Patel SR, Blackwell T, et al. Sleep characteristics of self-reported long sleepers. Sleep 2012;35(5):641-648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jee D, Morgan IG, Kim EC. Inverse relationship between sleep duration and myopia. Acta Ophthalmol 2016;94(3):e204-e210. [DOI] [PubMed] [Google Scholar]
- 23.Ayaki M, Torii H, Tsubota K, Negishi K. Decreased sleep quality in high myopia children. Sci Rep. 2016;6:33902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhou Z, Morgan IG, Chen Q, et al. Disordered sleep and myopia risk among Chinese children. PLoS One 2015;10(3):e0121796-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Xu C, Pan C, Zhao C, et al. Prevalence and risk factors for myopia in older adult east Chinese population. BMC Ophthalmol. 2017;17(1):191-211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li C, Yan Z, Zhang L, Li Y. Research and implementation of good agricultural practice for traditional Chinese medicinal materials in Jilin Province, China. J Ginseng Res. 2014;38(4):227-232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Liu J, Yang J, Guan G, et al. Erratum to: Molecular detection and identification of piroplasms in sika deer (Cervus nippon) from Jilin Province, China. Parasit Vectors. 2016;9(1):188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hazel CA, Elliott DB. The dependency of LogMAR visual acuity measurements on chart design and scoring rule. Optom Vis Sci. 2002;79(12):788-792. [DOI] [PubMed] [Google Scholar]
- 29.Standardization Administration of the People’s Republic of China (SAC) . China Standardization; 2011:1, 29. [Google Scholar]
- 30.Yi W, Xun J, He Y, et al. Body mass index of young men in China: results from four national surveys conducted between 1955 and 2012. Med. 2016;95(6):1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Obesity: Preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000:894:18-30. [PubMed] [Google Scholar]
- 32.Max H, Kaitlyn W, Steven MA, et al. National sleep foundation’s sleep time duration recommendations: Methodology and results summary. Sleep Health. 2015;1(1):40-43. [DOI] [PubMed] [Google Scholar]
- 33.Zhang F, Yin X, Bi C, et al. Psychological symptoms are associated with screen and exercise time: a cross-sectional study of Chinese adolescents. BMC Publ Health. 2020;20(1):1695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Education C. Children, adolescents, and television. Pediatrics. 2001;107(2):423-426. [DOI] [PubMed] [Google Scholar]
- 35.Jerry P, Luigino DM, Vincenzo B, et al. Estimating dose-response relationship between ethanol and risk of cancer using regression spline models. Int J Cancer. 2005;114(5):836-841. [DOI] [PubMed] [Google Scholar]
- 36.Desquilbet L, Mariotti F. Dose-response analyses using restricted cubic spline functions in public health research. Stat Med. 2010;29(9):1037-1057. [DOI] [PubMed] [Google Scholar]
- 37.Song Y, Lei YT, Hu PJ, et al. Situation analysis of physical fitness among Chinese Han students in 2014. Beijing Da Xue Xue Bao Yi Xue Ban 2018;50(3):436-442. [PubMed] [Google Scholar]
- 38.Yi W, Xun J, Zhang JQ, et al. Visual acuity of young men in China: results from 3 national cross-sectional surveys from 1974 to 2012. Med. 2019;98(1):e13966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Diane R. Air pollution, climate, and heart disease. Circ. 2013;128(21):411-414. [DOI] [PubMed] [Google Scholar]
- 40.Rius A, Artazcoz L, Guisasola L, Benach J. Visual impairment and blindness in spanish adults. Ophthalmology. 2014;121(1):408-416. [DOI] [PubMed] [Google Scholar]
- 41.He M, Huang W, Zheng Y, et al. Refractive error and visual impairment in school children in rural southern China. Ophthalmology 2007;114(2):374-382. [DOI] [PubMed] [Google Scholar]
- 42.Guo L, Yang J, Mai J, et al. Prevalence and associated factors of myopia among primary and middle school-aged students: a school-based study in Guangzhou. Eye. 2016;30(6):796-804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rose KA, Morgan IG, Ip J, et al. Outdoor activity reduces the prevalence of myopia in children. Ophthalmology. 2008;115(8):1279-1285. [DOI] [PubMed] [Google Scholar]
- 44.Fang Y, Tao FB, Wu XY, et al. Nearwork and myopia in children and adolescents: a systematic review and meta-analysis. Chinese Journal of School Health 2013;34(11):1302-1305. [Google Scholar]
- 45.Pileggi C, Papadopoli R, De Sarro C, et al. Obesity, blood pressure, and intraocular pressure: a cross-sectional study in italian children. Obesity facts 2021;14(2):169-177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dixit R, Jindal M, Gupta P, Dubey A. Excessive usage of illuminated screen a risk factor for Myopia in adolescent population. International Journal of Current Medical And Applied Sciences 2016;10(3):173-176. [Google Scholar]
- 47.An Y, Joo CK. The U-shaped association between self-reported sleep duration and visual impairment in Korean adults: a population-based study. Sleep Med. 2016;26(1):30-36. [DOI] [PubMed] [Google Scholar]
- 48.Xu X, Wang D, Xiao G, et al. Sleep less, myopia more. Theory Clin Pract Pediatr 2017;1(1):11-17. [Google Scholar]
- 49.Ostrin LA. Ocular and systemic melatonin and the influence of light exposure. Clin Exp Optom. 2019;102(2):99-108. [DOI] [PubMed] [Google Scholar]
- 50.Chakraborty R, Ostrin LA, Nickla DL, Iuvone PM, Pardue MT, Stone RA. Circadian rhythms, refractive development, and myopia. Ophthalmic Physiol Opt. 2018;38(3):217-245. [DOI] [PMC free article] [PubMed] [Google Scholar]