Abstract
Background:
Injury incidence for physically active populations with a high volume of physical load can exceed 79%. There is little existing research focused on timing of injury and how that timing differs based on certain risk factors.
Purpose/Hypothesis:
The purpose of this study was to report both the incidence and timing of lower extremity injuries during cadet basic training. We hypothesized that women, those with a history of injury, and those in underweight and obese body mass index (BMI) categories would sustain lower extremity musculoskeletal injury earlier in the training period than men, those without injury history, and those in the normal-weight BMI category.
Study Design:
Cohort study; Level of evidence, 2.
Methods:
Cadets from the class of 2022, arriving in 2018, served as the study population. Baseline information on sex and injury history was collected via questionnaire, and BMI was calculated from height and weight taken during week 1 at the United States Military Academy. Categories were underweight (BMI <20), middleweight (20-29.99), and obese (≥30). Injury surveillance was performed over the first 60 days of training via electronic medical record review and monitoring. Kaplan-Meier survival curves were used to estimate group differences in time to the first musculoskeletal injury. Cox proportional hazard regression was used to estimate hazard ratios (HRs).
Results:
A total of 595 cadets participated. The cohort was 76.8% male, with 29.9% reporting previous injury history and 93.3% having a BMI between 20 and 30. Overall, 16.3% of cadets (12.3% of male cadets and 29.7% of female cadets) experienced an injury during the follow-up period. Women experienced significantly greater incident injury than did men (P < .001). Separation of survival curves comparing the sexes and injury history occurred at weeks 3 and 4, respectively. Hazards for first musculoskeletal injury were significantly greater for women versus men (HR, 2.63; 95% CI, 1.76-3.94) and for those who reported a history of injury versus no injury history (HR, 1.76; 95% CI, 1.18-2.64). No differences were observed between BMI categories.
Conclusion:
Female cadets and those reporting previous musculoskeletal injury demonstrated a greater hazard of musculoskeletal injury during cadet basic training. This study did not observe an association between BMI and injury.
Keywords: injury, military, basic training, injury history
Musculoskeletal injuries are commonplace in populations focused on fitness and training. 13,17,18,22,43,45 Incident injury is particularly concerning for athletic groups with a greater volume of physical load (such as high exposure to running); it can exceed 79% and varies widely depending on the population. 22,43,45 The military basic training environment is an example of a population focused on fitness and training. For example, cadet basic training at the United States Military Academy (USMA) represents the first 7 weeks of training for entering cadets. Physically, cadets are required to quickly advance their abilities and perform at the same level as soldiers in regular units across the army, including walking 12 miles (19.2 km) with >35 lb (15.88 kg) of gear; running on multiple days of the week; and passing a physical fitness test comprising pushups, situps, and a 2-mile (3.2-km) run in just 7 weeks. 41
The rapid increase in cumulative physical load significantly affects the musculoskeletal system, particularly in the lower extremity. Though often perceived as an effective strategy for enhancing physical performance, the disadvantage is that 75% of all musculoskeletal injuries in military training are due to “cumulative microtraumatic injuries caused by repeated low intensity forces.” 13 Overuse injuries including muscular strains, tendinitis, medial tibial stress syndrome, and stress fractures represent a significant financial burden, costing the US Army nearly $200 million each year 13 and negatively affecting training, combat operations, and military readiness. 27 Given the effect of these injuries, it is important to take continued steps toward mitigation. An epidemiological study to identify the factors and mechanisms associated with injury is a key step toward sports injury mitigation. 44
Evidence suggests that body mass index (BMI) is one important risk factor to consider given its correlation with musculoskeletal injury in the athletic population. 43,46 Both higher and lower BMI have been correlated with injury in the US Army basic training population. 15,18 Previous injury is also a well-known predictor of future injury in many sports and activities in both civilian and military populations. 10,17,20,26,36,39 Finally, sex is a significant correlate to injury in the military population, where women are injured at nearly twice the rate of their male counterparts, 14,17,31 particularly less fit women. 19 Alongside these potential risk variables, it is also important to assess load toleration and the schedule of training. Researchers have asserted that it is not just the cumulative load but the time over which that load is experienced that is correlated with musculoskeletal injuries. 6,7,37 The temporal aspect of the load application offers a valuable option for injury mitigation through better understanding of time varying load application. 23,30
To best inform future training, load application, and intervention to maximize injury mitigation in military training and sports, we must delineate the timing of injury and how that timing differs based on certain risk factors. Therefore, the purpose of this study was to examine both the incidence and the timing of injuries during cadet basic training. The study examined overall and specific injury types in addition to overall and subgroup injury timing. Subgroups examined included sex, history of injury, and BMI category. Additionally, we compared survivability of injury between groups using time-to-event analyses. We hypothesized that women, those with a history of injury, and those in the underweight and obese BMI categories would be injured earlier in the training period than men, those without injury history, and those in the normal-weight BMI category.
Methods
Participants and Data Collection
Data on injury history, demographics, and injury surveillance were collected at USMA in 2018. The study represented a partnership between military and civilian institutions and was reviewed by the Regional Health Command–Atlantic Institutional Review Board and the University of North Carolina at Chapel Hill Institutional Review Board.
All individuals were recruited from the population of new cadets arriving at USMA to enter cadet basic training as part of the class of 2022. Recruitment occurred on day 2 of training, where the tests and procedures were explained. Information was delivered both orally and in written format. Because of the USMA’s age standards for entry, all participants were emancipated minors or adults between the ages of 17 and 22 years and met height and weight requirements. 40 Inclusion criteria included being eligible to begin training, and cadets who consented to the study were excluded only if they stated they felt pain or did not feel as though they could complete the physical tests that were part of normal screening, including a jump landing and Army Physical Fitness Test (see Appendix Table A1). Participants understood that they were not receiving any reimbursement for participation in either of the studies. The injury surveillance period was the first 60 days of cadet basic training.
Injury Surveillance and Outcomes
Injury surveillance data originated from internal electronic medical records at USMA. Specifically, these data were collected from 2 databases: the Cadet Injury and Illness Tracking System (which is specific to USMA) and the Armed Forces Health Longitudinal Technology Application (which is US Department of Defense–wide). Because the USMA uses a closed medical system, meaning that the medical needs of the cadets are met within the military health system, all injury data are entered into 1 of these 2 systems. In the normal course of events, if a cadet feels pain and/or sustains what is perceived to be an injury, he or she presents to sick call, where a health care provider documents the details of the pain/injury, the diagnosis, and plan of care in the electronic medical record. Details of any visit to medical providers, including medical doctors, physician assistants, or physical therapists, are placed in the record.
Using International Classification of Diseases, 10th revision (ICD-10) codes, we conducted an extensive review of injuries that occurred during the first 60 days for cadets entering the USMA in 2018 within both electronic medical record systems. The majority of injury codes used were overuse in nature. Joint and soft tissue pain codes were also included. 12,13,31 A complete list of the ICD-10 codes used in the search can be found in Appendix Table A2.
For the purpose of this study, we defined an injury as any condition of the musculoskeletal system involving the lower extremities or pelvis for which the individual sought medical care. Cadet basic training is normally 48 days in length, but we included 12 days after return from training in order to capture those injuries that were sustained during but not reported until after completion of training.
Demographic and Historical Injury Data
Data on history of injury came from questions on the baseline questionnaire answered immediately after providing consent. The questionnaire asked separate questions about injuries to lower extremity anatomic locations. If the cadet answered in the affirmative to having a lower extremity injury, he or she was categorized as having a positive injury history; if one answered in the negative to all injury questions, the cadet was considered to have a negative injury history. A missing response was assumed to represent the absence of an injury.
BMI was calculated from the height and weight measured during the day 2 physical fitness test and categorized into 3 groups: underweight (<20); middleweight (20-29.99); and obese (≥30). The American Dietetic Association 35 defines underweight as having a BMI of less than 20. Similarly, 20 has been suggested as a cutoff for underweight for geriatric patients in European countries 24 and Japan. 25 Finally, sex was a variable collected as part of general demographic information. Sex was defined as a dichotomous variable with either male or female as the potential group. This was in accordance with the demographic selection options at USMA.
Statistical Analysis
Baseline descriptive statistics, including days until injury, were calculated for each type of injury as well as for each subgroup (ie, male/female). We created survival curves using the Kaplan-Meier method. The interpretation of the survival curve is that it plots the probability of being event-free on any given day of basic training having survived injury-free up to the day. 47 The population was a fixed-size closed cohort, as all cadets start training on the same date and all consented on the same day. No individuals could enter the study at a later date, and administrative right censoring was performed at the completion of the surveillance period (60 days). The log-rank test was used to quantify the difference between the survival curves.
Additionally, the Cox proportional hazards model was used to estimate hazard ratios (HRs). Like the survival function, a hazard can be interpreted as the conditional rate of the injury occurrence on any given day of training, given that the individual has not experienced injury before that point in time. The HR is estimated from the proportional hazards model, which is written as hx (t) = h 0(t) × e βx , where h 0 is the baseline hazard over time for a referent subgroup (eg, men), hx is the hazard in the comparison group (eg, women), x represents women (1) or men (0), and β is the natural log of the HR. We used 95% confidence intervals (CIs) to determine the significance of the variables, and the proportionality of hazards was evaluated by assessing the significance of time interactions in the model (α = .05). Statisitical Analyses were performed using SAS Version 9.3 (SAS Institute).
Results
Central Tendency Measures of Time to Event
A total of 595 cadets consented to and provided data for the study (48.4% of the class). A breakdown of preinjury baseline characteristics is presented in Table 1. Similar to the overall incoming cadet population in 2018, which was 76.1% male, 42 the cohort was also largely male (n = 457; 76.81%). Overall, 178 cadets (29.92%) reported a history of injury before starting at USMA. BMI ranged from 18.2 to 40.7, with 19 cadets (3.19%) having a BMI ≥30 and 21 (3.53%) having a BMI of <20. No women had a BMI of ≥30 versus 19 men. Six women had a BMI of <20 versus 15 men.
Table 1.
Baseline Characteristics: Entering Cadets at the United States Military Academy, 2018 a
| Characteristic | n (%) |
|---|---|
| Sex | |
| Male | 457 (76.81) |
| Female | 138 (23.19) |
| BMI | |
| <20 (underweight) | 21 (3.53) |
| 20-29.99 | 555 (93.28) |
| ≥30 (obese) | 19 (3.19) |
| History of injury | |
| Yes | 178 (29.92) |
| No | 417 (70.08) |
a BMI, body mass index.
During the first 60 days at USMA, 97 of the 595 cadets (16.3%) experienced a training-related musculoskeletal injury. Of these injuries, 9 (9.3%) were stress fractures, which represented a 1.5% cumulative incidence of stress fracture in the cohort during the 60 days of cadet basic training. Among female cadets, 29.7% sustained at least 1 injury compared with 12.3% of male cadets (P < .001). For stress fractures, female cadets had an incidence of injury of 2.9% compared with 1.1% of male cadets (P = .128). Female incidence of soft tissue injury was also greater at 26.8% relative to men at 10.9% (P < .001). Mean and median times to musculoskeletal injury for each subgroup based on sex, history of previous injury, and BMI are shown in Table 2.
Table 2.
Injury Characteristics: Entering Cadets at the United States Military Academy, 2018 a
| All Injuries | Stress Fractures | Soft Tissue Injuries | |||||||
|---|---|---|---|---|---|---|---|---|---|
| n | Mean ± SD | Median (IQR) | n | Mean ± SD | Median (IQR) | n | Mean ± SD | Median (IQR) | |
| Overall | 97 | 19.14 ± 14.19 | 15.00 (5.00-25.00) | 9 | 16.56 ± 12.36 | 13.00 (9.00-17.00) | 87 | 19.63 ± 14.33 | 17.00 (7.00-27.00) |
| Sex | |||||||||
| Male | 56 | 18.00 ± 14.56 | 13.00 (2.75-23.25) | 5 | 19.80 ± 16.27 | 9.00 (0.00-36.00) | 50 | 18.18 ± 14.47 | 13.50 (3.50-23.50) |
| Female | 41 | 20.71 ± 13.68 | 18.00 (10.75-25.50) | 4 | 12.50 ± 3.87 | 13.50 (8.50-18.50) | 37 | 21.60 ± 14.09 | 19.00 (12.00-26.00) |
| History of injury | |||||||||
| Yes | 41 | 23.12 ± 15.60 | 19.00 (8.50-29.50) | 1 | 7.00 ± N/A | 7.00 (N/A b ) | 40 | 23.53 ± 15.58 | 19.00 (9.50-28.50) |
| No | 56 | 16.23 ± 12.41 | 13.00 (5.25-20.75) | 8 | 17.75 ± 12.65 | 13.50 (5.00-22.00) | 47 | 16.32 ± 12.40 | 13.00 (5.00-21.00) |
| BMI | |||||||||
| <20 (underweight) | 5 | 18.20 ± 7.98 | 21.00 (11.50-30.50) | 0 | N/A b | N/A b | 5 | 18.20 ± 7.98 | 21.00 (20.00-22.00) |
| 20-29.99 | 90 | 19.44 ± 14.51 | 15.00 (5.00-25.00) | 9 | 16.56 ± 12.36 | 13.00 (9.00-17.00) | 80 | 20.01 ± 14.69 | 16.00 (5.75-26.25) |
| ≥30 (obese) | 2 | 8.00 ± 8.49 | 8.00 (2.00-14.00) | 0 | N/A b | N/A b | 2 | 8.00 ± 8.49 | 8.00 (2.00-14.00) |
a BMI, body mass index; IQR, interquartile range; N/A, not applicable.
b N/A denotes categories with 0 or 1 injuries, where calculations could not be completed.
Survival Analysis Comparisons
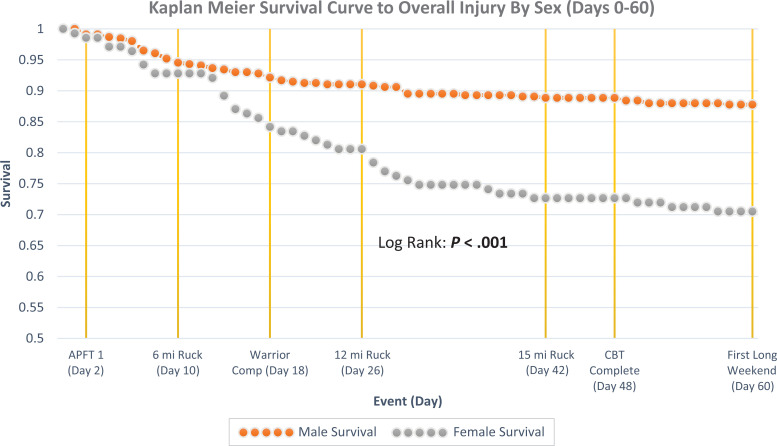
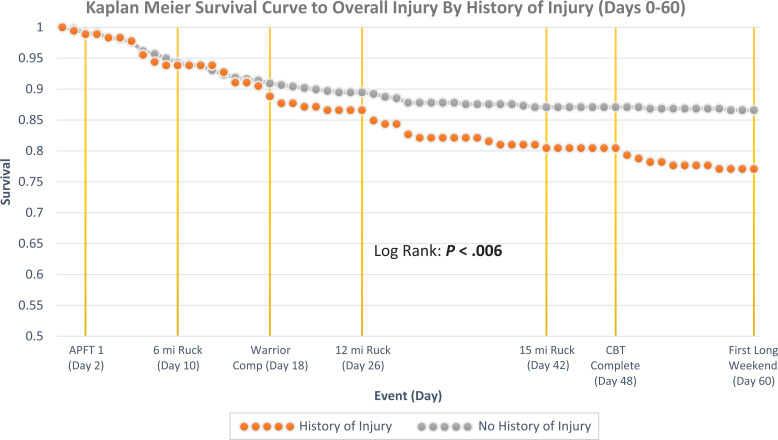
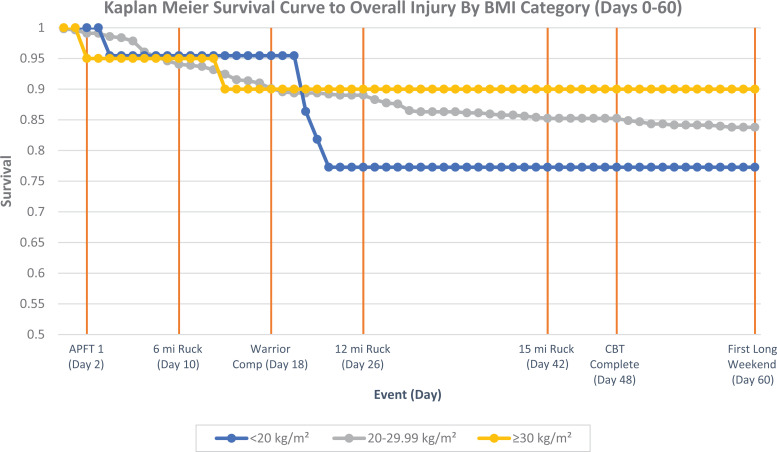
Injury-free survival time during the follow-up period was compared using Kaplan-Meier curves (Figures 1 –3) that compared subgroup survival and HRs (Table 3). The proportional hazard assumptions were met for all comparisons, as indicated by a nonsignificant time interaction; however, it must be noted that for BMI, the Kaplan-Meier survival curves did cross, indicating the possibility of violation of proportionality of hazard (P Time×BMI = 0.242).
Figure 1.
Kaplan-Meier curves by sex for incident musculoskeletal injury during basic training for entering cadets at the United States Military Academy, 2018. See Appendix Table A1 for details on events. APFT, Army Physical Fitness Test; CBT, cadet basic training; Comp, competition.
Figure 2.
Kaplan-Meier curves by history of injury for incident musculoskeletal injury during basic training for entering cadets at the United States Military Academy, 2018. See Appendix Table A1 for details on events. APFT, Army Physical Fitness Test; CBT, cadet basic training; Comp, competition.
Figure 3.
Kaplan-Meier curves by body mass index (BMI) for incident musculoskeletal injury during basic training for entering cadets at the United States Military Academy, 2018. See Appendix Table A1 for details on events. APFT, Army Physical Fitness Test; CBT, cadet basic training; Comp, competition.
Table 3.
Hazard Ratios for Musculoskeletal Injury During Cadet Basic Training at the United States Military Academy, 2018 a
| Potential Risk or Protective Factor | Univariate HR (95% CI) | Multivariate HR (95% CI) |
|---|---|---|
| Sex (female vs male) | 2.63 (1.76-3.94) | 2.52 (1.68-3.78) |
| History of injury (yes vs no) | 1.76 (1.18-2.64) | 1.63 (1.09-2.44) |
| BMI | ||
| <20 vs 20-29.99 | 1.52 (0.62-3.73) | N/A |
| ≥30 vs 20-29.99 | 0.65 (0.16-2.63) | N/A |
| 20 vs ≥30 | 2.34 (0.45-12.06) | N/A |
a BMI, body mass index; HR, hazard ratio; N/A, not applicable, not included in the multivariate model because of sparse numbers in 2 of the 3 BMI categories.
There were significant differences in survival time between men and women for lower extremity injury during the follow-up period (log-rank test, P < .001). There was notable separation between the 2 groups that emerged around week 3 of training (Figure 1). Univariate HRs (Table 3) also indicated female cadets face a greater hazard of injury during training than do male cadets (HR, 2.63; 95% CI, 1.76-3.94). Multivariate analysis including injury history as a variable produced similar results (HR, 2.52; 95% CI, 1.68-3.78) (Table 3).
Significant differences in time to injury were also observed for those reporting a history of injury relative to those reporting no history of injury (log-rank test, P < .006). Separation in survival curves between these groups appeared to expand during week 4 (Figure 2). Those with a prior history of injury had a greater hazard of incident injury than did those with no injury history in univariate analysis (HR, 1.76; 95% CI, 1.18-2.64) and in the multivariate analysis adjusting for sex (HR, 1.63; 95% CI, 1.09-2.44) (Table 3).
Comparison across the 3 categories of BMI were problematic because of distinct homogeneity of the sample. Underweight and obese categories were very underrepresented in the cadet population (Table 1). Based on visual inspection, it appeared that underweight individuals experienced a decline in survival (ie, higher rate of injury) after the Warrior Competition, though no statistically significant differences were found (Figure 3).
Discussion
Survival curve and HR comparisons indicated less survival time to musculoskeletal injury and greater hazard of injury for women and those with a history of injury. The differences were specifically noted after the first 2 weeks of training. The disparities offer an opportunity to improve injury mitigation by appropriately focusing both screening and intervention in the military and sports. The results matched our hypotheses for survival time by sex and injury history but not for BMI. However, this likely reflected the very low numbers of underweight and obese cadets in this population. Our observations may indicate a distinct difference in load tolerances among cadets and inform mitigation based on individual characteristics.
Cumulative Incidence for Injury Outcomes of Interest
The overall incidence of injury was equivocal to previous studies on USMA cadets but slightly less than the incidence of injury in army basic training overall. 13,15,20 Stress fracture incidence, specifically, was slightly lower than in previous cohorts of USMA cadets 20 and moderately lower than that found in other army basic training environments. 13,15
Differences in Survival by Sex
Our observation of a greater hazard of musculoskeletal injury for women throughout training is consistent with several studies that have highlighted a greater risk of musculoskeletal injury for women during military training. 20,32,38 There are a number of potential reasons for the noted disparities between the sexes. For example, when compared with their male counterparts, women demonstrate decreased absolute strength and power of the upper and lower extremities. 2,8 Women are also generally smaller with less muscle mass. Given that training loads are equal for both sexes, female cadets may require comparatively more effort during training. Appropriate physical training is known to build strength and increase tissue capacity. However, the greater proportional effort by female cadets could push them beyond supraphysiologic overloading 5 and toward structural failure.
Supraphysiologic overloading also appears to have a temporal component in this population. 4,6,29 Our data further suggested that the temporal component differs between the sexes and begins to diverge early, at the more exhaustive events (eg, the Warrior Competition, 12-mile ruck). We speculate that the acute effort needed to complete these events (ie, load placed upon the tissues), particularly for female cadets, was far greater than the average (ie, chronic) load placed on tissues over the previous weeks. Spikes in an acute to chronic workload ratio have been shown to increase injury risk. 4,6,9 Thus, these data support the developing case in the military literature that injury rate may also be a function of physical condition at the start of training. 1,16
Differences in Survival by History of Injury
Our observations that those with a history of injury demonstrated a greater hazard of musculoskeletal injury is consistent with injury history’s being correlated with greater risk of injury in a variety of populations. 10,17,27,36,39 Specific to the cadet population at USMA, Kucera et al 20 demonstrated a strong correlation between injury history and injury incidence in cadet basic training. We propose 2 reasons that this specific relationship could exist, both relating to the concept of tissue overload. First, the risk of injury may lie with lack of proper rehabilitation and less optimal tissue capacity. 28 Second, reduced tissue capacity for both load and recovery could lead to less survival time until injury due to the inability to remodel in sufficient time to tolerate the subsequent load without injury.
There is also evidence to suggest a disruption of sensorimotor abilities after injury, 28 which describes the second reason those with a history of injury may experience less time to injury---that lingering kinematic and/or neuromuscular deficits result in altered movement and loading profiles. Evidence for altered loading profiles is found elsewhere in the literature, particularly in those who have undergone anterior cruciate ligament reconstruction where altered kinematic changes can follow injury. 11,21 Changes in one’s kinematic or kinetic profile may alter the tissue-specific loads experienced during training. This change appears to decrease the load tolerance of the tissue for some, again leading the person to exceed the zone of supraphysiologic overload and resulting in a decreased time until injury.
Differences in Survival by BMI
Though the survival curves appear to show a drop after the Warrior Competition, our analysis showed no statistical difference between categories of BMI. It is important to note, however, that the obese and underweight categories were underrepresented in the cadet population and our BMI analyses were affected by lack of precision, as evidenced by the wide CIs for the BMI HRs. Previous research is conflicting regarding BMI and injury. Psaila and Ranson 34 reported that BMI was not associated with injury risk, while Jones et al 15 found that men with greater BMI had greater risk of musculoskeletal injury during training. Knapik et al 18 described a univariate correlation between injury risk and recruits with both high and low BMI, though only low BMI was observed to be valuable as an independent risk factor in their Cox regression model. The apparent drop in the survival curve after the Warrior Competition for the underweight category also occurs in week 3, which is common in basic training 3,33 and thus may be a function of the cumulative load at that point and not the Warrior Competition itself.
Limitations
As with any study, there were inherent weaknesses that bear highlighting. First, our sample included 48.4% of the class. Though this was a robust number, certain categories, including the underweight and obese BMI categories, were underrepresented because they are similarly underrepresented in the population because of admissions standards. 40 With regard to injury, 29.9% of the sample reported injury before attending USMA, and 16.3% of the sample experienced injury during the follow-up period. Second, the timing of major physical events does not highlight proximity to other training events that may have altered the true or perceived tissue load experienced by the individual cadet. For example, cadets from one company may have gone directly from a range or night training to a major physical event, while cadets from another company may have been more rested. Though cadets all do the same training, limitations on space and equipment require their training to be conducted at different times. Third, the day of injury used is the day the injury was reported to medical personnel, which may or may not be the day the injury was actually sustained. Fourth, we only examined injuries to the lower extremities in this study, potentially limiting our ability to understand the full effect of musculoskeletal injury during this period. Finally, we were not able to control for other potentially important variables, including race and the level of athletics in which the cadets participated (recreational vs intercollegiate).
Strengths
This study was innovative because it used survival methods to analyze time until injury, which provides information to those planning training schedules. The survival curves in Figures 1 to 3 include major training schedule events during cadet basic training, which highlight the significant physical events required of the cadets and those events’ temporal relationship to survival to musculoskeletal injury. This manner of delineating the survival time until injury has the capability of enhancing the current methodology in developing cadet basic training. Using these types of injury analyses is clinically applicable, as they can better inform load application and highlight where overloading may occur, all of which optimize load application and can help mitigate injury risk. 37
Conclusion
Survival analyses demonstrated that being male and having no history of injury were correlated with less hazard of musculoskeletal injury during cadet basic training at the USMA versus being female and having a history of injury. The disparity between these groups appears to be particularly evident after week 2. Research on fitness state before cadet basic training could be beneficial in understanding the acute to chronic workload change during the first segment of training. Finally, the use of more exact load monitoring could more precisely delineate survival until training-related injury by using total load versus days until injury.
Acknowledgment
The authors thank Story Miraldi, Alysse Woods, and Steven Davi of the John A. Feagin Jr Sports Medicine Fellowship Program and the members of the US Army–Baylor Sports Medicine Fellowship Program for their contributions to this research.
APPENDIX
Table A1.
Definitions of Cadet Basic Training Events
| • Army Physical Fitness Test: this test consists of 2 min of pushups followed by 2 min of situps followed by a 2-mile run |
| • Ruck: short for ruck marching, these are events in which a cadet wears a tactical uniform, gear, and a ruck sack, which is much like a large backpack. Normal weight for gear is at least 35 lb (15.88 kg). |
| • Warrior Competition: a multiple task event that simulates combat-related tasks (ie, carrying another cadet on a stretcher) and requires small group problem solving along with the physical tasks |
| • Cadet basic training complete: this is the day that cadets are accepted into the larger corps of cadets and begin the transition to their academic studies. |
| • First long weekend: this is typically Labor Day weekend (weekend of the first Monday in September), in which cadets have no academic requirements Saturday through Monday. |
Table A2.
ICD-10 Codes a
| Injury | ICD-10 Code | Injury | ICD-10 Code |
|---|---|---|---|
| Acute ankle and foot injuries | Acute knee and lower leg injuries | ||
| Talar dome fracture | S92.1 | Gastrocnemius strain | S86.1 |
| Calcaneal fracture | S99.0 | Fibular fracture | S82.4 |
| Cuboid subluxation/dislocation | S93.31 | Tibial fracture | S82.2 |
| Toe sprain | S93.51 | Lower leg compartment syndrome (traumatic) | T79.A |
| Great toe fracture | S92.4 | MCL sprain | S83.41 |
| Phalangeal fracture (digits 2-5) | S92.5 | LCL sprain | S83.42 |
| Phalangeal dislocation | S93.1 | ACL sprain | S83.51 |
| Sprain of interphalangeal joint | S93.51 | PCL sprain | S83.52 |
| Ankle sprain (medial or lateral) | S93.4 | Meniscal tear | S83.2 |
| High ankle sprain (syndesmotic ankle sprain) | S93.43 | Patellar fracture | S82.0 |
| Distal fibular fracture | S82.6 | Patellar subluxation/dislocation | S83.0 |
| Distal tibial fracture | S82.3 | Patellar tendon rupture | M66.85 |
| Achilles tendon rupture | S86.02 | Dislocation of knee | S83.1 |
| Peroneal tendon subluxation/dislocation | S86.39 | Sprain of other specified sites of knee and leg | S83.8 |
| Ankle dislocation | S93.0 | Sprain of unspecified site of knee and leg | S83.9 |
| Tarsal (bone) dislocation, joint unspecified | S93.31 | Pain in thigh | M79.65 |
| Midtarsal (joint) dislocation | S93.31 | Pain in lower leg | M79.67 |
| Tarsometatarsal (joint) dislocation | S93.32 | ||
| Metatarsophalangeal (joint) dislocation | S93.12 | Chronic knee and lower leg injuries | |
| Interphalangeal (joint) dislocation, foot | S93.11 | Medial tibial stress syndrome | M76.89, T79.6 |
| Sprain of foot | S93.5 | Chronic compartment syndrome | M79.A |
| Sprain of tarsometatarsal (joint) (ligament) | S93.62 | Tibial stress fracture | M84.361, M84.362 |
| Sprain of metatarsophalangeal (joint) | S93.52 | Fibular stress fracture | M84.363, M84.364 |
| Sprain of interphalangeal (joint), toe | S93.51 | Bursitis - infrapatellar, suprapatellar | M70.4 |
| Sprain of foot (unspecified) (other) | S93.60 | Chondromalacia (patella) | M22.4 |
| Pain in foot and toes | M.79.67 | Patellofemoral pain | M22.2 |
| Iliotibial band friction syndrome | M76.3 | ||
| Chronic ankle and foot injuries | Pes anserine tendinitis | M76.89 | |
| Talar dome stress fracture | S92.19 | Patellar tendinitis | M76.5 |
| Tarsal tunnel syndrome | G57.5 | Knee osteoarthritis | M17.1 |
| Plantar fasciitis | M72.2 | Pain in knee | M25.56 |
| Metatarsal stress fracture | M84.374, M84.375 | ||
| Sesamoiditis | M25.80 | Acute hip, thigh, and pelvic injuries | |
| Metatarsalgia | M77.40 | Quadriceps strain | S76.1 |
| Morton’s neuroma | G57.60 | Hamstring strain | S76.3 |
| Achilles tendinitis | M76.6, M79.61 | Femoral fracture (distal) | S72.4 |
| Anterior tibialis tendinitis | M76.81 | Femoral fracture (proximal) | S72.0 |
| Posterior tibialis tendinitis | M76.82 | Femoral head dislocation/subluxation | S73.0 |
| Peroneal tendinitis | M76.7 | Hip joint sprain | S73.1 |
| Adductor strain | S76.2 | ||
| Chronic hip, thigh, and pelvic injuries | |||
| Femoral stress fracture | M84.35 | ||
| Trochanteric bursitis | M70.6 | ||
| Osteitis pubis | M85.3 |
a ACL, anterior cruciate ligament; ICD, International Classification of Diseases; LCL, lateral collateral ligament; MCL, medial collateral ligament; PCL, posterior cruciate ligament.
Footnotes
Final revision submitted May 2, 2021; accepted May 4, 2021.
One or more of the authors has declared the following potential conflict of interest or source of funding: The parent study (JUMP-ACL study) was funded by the National Institute of Arthritis and Musculoskeletal and Skin Diseases, National Institutes of Health (R01-AR054061001). D.A.P and S.W.M. were supported by this award. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was waived by the University of North Carolina at Chapel Hill (study No. 18-3378).
References
- 1. Bell NS, Mangione TW, Hemenway D, Amoroso PJ, Jones BH. High injury rates among female Army trainees: a function of gender? Am J Prev Med. 2000;18(3)(suppl):141–146. doi:10.1016/S0749-3797(99)00173-7 [DOI] [PubMed] [Google Scholar]
- 2. Billaut F, Bishop D. Muscle fatigue in males and females during multiple-sprint exercise. Sports Med. 2009;39(4):257–278. doi:10.2165/00007256-200939040-00001 [DOI] [PubMed] [Google Scholar]
- 3. Brannen S. Injuries During Marine Corps Officer Basic Training. Vol 165. 2000. Accessed July 20, 2020. https://academic.oup.com/milmed/article-abstract/165/7/515/4832411 [PubMed] [Google Scholar]
- 4. Drew MK, Finch CF. The relationship between training load and injury, illness and soreness: a systematic and literature review. Sports Med. 2016;46(6):861–883. doi:10.1007/s40279-015-0459-8 [DOI] [PubMed] [Google Scholar]
- 5. Dye SF. The pathophysiology of patellofemoral pain a tissue homeostasis perspective. Clin Orthop Relat Res. 2005;436:100–110. doi:10.1097/01.blo.0000172303.74414.7d [DOI] [PubMed] [Google Scholar]
- 6. Eckard TG, Padua DA, Hearn DW, Pexa BS, Frank BS. The relationship between training load and injury in athletes: a systematic review. Sports Med. 2018;48:1929–1961. doi:10.1007/s40279-018-0951-z [DOI] [PubMed] [Google Scholar]
- 7. Edwards WB. Modeling overuse injuries in sport as a mechanical fatigue phenomenon. Exerc Sport Sci Rev. 2018;46(4):224–231. doi:10.1249/JES.0000000000000163 [DOI] [PubMed] [Google Scholar]
- 8. Epstein Y, Yanovich R, Moran DS, Heled Y. Physiological employment standards IV: integration of women in combat units physiological and medical considerations. Eur J Appl Physiol. 2013;113(11):2673–2690. doi:10.1007/s00421-012-2558-7 [DOI] [PubMed] [Google Scholar]
- 9. Gabbett TJ. The training-injury prevention paradox: should athletes be training smarter and harder? Br J Sports Med. 2016;50(5):273–280. doi:10.1136/bjsports-2015-095788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Grier TL, Morrison S, Knapik JJ, Canham-Chervak M, Jones BH. Risk factors for injuries in the U.S. Army Ordnance School. Mil Med. 2011;176(11):1292–1299. doi:10.7205/milmed-d-11-00215 [DOI] [PubMed] [Google Scholar]
- 11. Haughom B, Schairer W, Souza RB, Carpenter D, Ma CB, Li X. Abnormal tibiofemoral kinematics following ACL reconstruction are associated with early cartilage matrix degeneration measured by MRI T1rho. Knee. 2012;19(4):482–487. doi:10.1016/j.knee.2011.06.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hauret KG, Bedno S, Loringer K, Kao T-C, Mallon T, Jones BH. Epidemiology of exercise- and sports-related injuries in a population of young, physically active adults: a survey of military servicemembers. Am J Sports Med. 2015;43(11):2645–2653. doi:10.1177/0363546515601990 [DOI] [PubMed] [Google Scholar]
- 13. Hauschild VD, Lee T, Barnes S, Forrest L, Hauret K, Jones BH. The etiology of injuries in US Army initial entry training. US Army Med Dep J. 2018;2-18:22–29. [PubMed] [Google Scholar]
- 14. Henderson NE, Knapik JJ, Shaffer SW, McKenzie TH, Schneider GM. Injuries and injury risk factors among men and women in U.S. Army combat medic advanced individual training. Mil Med. 2000;165(9):647–652. [PubMed] [Google Scholar]
- 15. Jones BH, Bovee MW, Harris JM, III, Cowan DN. Intrinsic risk factors for exercise-related injuries among male and female army trainees. Am J Sports Med. 1993;21(5):705–710. [DOI] [PubMed] [Google Scholar]
- 16. Jones BH, Hauret KG, Dye SK, et al. Impact of physical fitness and body composition on injury risk among active young adults: a study of Army trainees. J Sci Med Sport. 2017;20:S17–S22. doi:10.1016/j.jsams.2017.09.015 [DOI] [PubMed] [Google Scholar]
- 17. Kaufman KR, Brodine S, Shaffer R. Military training-related injuries: surveillance, research, and prevention. Am J Prev Med. 2000;18(3)(suppl):54–63. doi:10.1016/S0749-3797(00)00114-8 [DOI] [PubMed] [Google Scholar]
- 18. Knapik JJ, Graham B, Cobbs J, Thompson D, Steelman R, Jones BH. A prospective investigation of injury incidence and risk factors among army recruits in combat engineer training. J Occup Med Toxicol. 2013;8(1):5. doi:10.1186/1745-6673-8-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Krauss MR, Garvin NU, Boivin MR, Cowan DN. Excess stress fractures, musculoskeletal injuries, and health care utilization among unfit and overweight female Army trainees. Am J Sports Med. 2017;45(2):311–316. doi:10.1177/0363546516675862 [DOI] [PubMed] [Google Scholar]
- 20. Kucera KL, Marshall SW, Wolf SH, Padua DA, Cameron KL, Beutler AI. Association of injury history and incident injury in cadet basic military training. Med Sci Sports Exerc. 2016;48(6):1053–1061. doi:10.1249/MSS.0000000000000872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Li G, Li JS, Torriani M, Hosseini A. Short-term contact kinematic changes and longer-term biochemical changes in the cartilage after ACL reconstruction: a pilot study. Ann Biomed Eng. 2018;46(11):1797–1805. doi:10.1007/s10439-018-2079-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lopes AD, Hespanhol LC, Yeung SS, Costa LOP. What are the main running-related musculoskeletal injuries? Sports Med. 2012;42(10):891–905. doi:10.2165/11631170-000000000-00000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Mansournia MA, Nielsen RO, Bertelsen ML, et al. Time-to-event analysis for sports injury research part 2: time-varying outcomes. Br J Sports Med. 2019;53(1):70–78. doi:10.1136/bjsports-2018-100000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Meier R, Stratton R. Basic concepts in nutrition: epidemiology of malnutrition. e-SPEN. 2008;2008:e167–e170. doi:10.1016/j.eclnm.2008.04.002 [Google Scholar]
- 25. Minagawa Y, Saito Y. The role of underweight in active life expectancy among older adults in Japan. J Gerontol B Psychol Sci Soc Sci. 2021;76(4):756–765. doi:10.1093/geronb/gbaa013 [DOI] [PubMed] [Google Scholar]
- 26. Molloy JM. Factors influencing running-related musculoskeletal injury risk among U.S. military recruits. Mil Med. 2016;181(6):512–523. doi:10.7205/MILMED-D-15-00143 [DOI] [PubMed] [Google Scholar]
- 27. Molloy JM, Pendergrass TL, Lee IE, Chervak MC, Hauret KG, Rhon DI. Musculoskeletal injuries and United States Army readiness part I: overview of injuries and their strategic impact. Mil Med. 2020;185(9-10):e1461–e1471. doi:10.1093/milmed/usaa027 [DOI] [PubMed] [Google Scholar]
- 28. Murphy DF, Connolly DAJ, Beynnon BD. Risk factors for lower extremity injury: a review of the literature. Br J Sports Med. 2003;37(1):13–29. doi:10.1136/bjsm.37.1.13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Myers NL, Mexicano G, Aguilar KV. The association between non-contact injuries and the acute: chronic workload ratio in elite level athletes: a critically appraised topic. J Sport Rehabil. 2020;29(1):127–130. doi:10.1123/jsr.2018-0207 [DOI] [PubMed] [Google Scholar]
- 30. Nielsen RO, Bertelsen ML, Ramskov D, et al. Time-to-event analysis for sports injury research part 1: time-varying exposures. Br J Sports Med. 2019;53(1):61–68. doi:10.1136/bjsports-2018-099408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Nye NS, Pawlak MT, Webber BJ, Tchandja JN, Milner MR. Description and rate of musculoskeletal injuries in Air Force basic military trainees, 2012−2014. J Athl Train. 2016;51(11):858–865. doi:10.4085/1062-6050-51.10.10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. O’Leary TJ, Wardle SL, Rawcliffe AJ, Chapman S, Mole J, Greeves JP. Understanding the musculoskeletal injury risk of women in combat: the effect of infantry training and sex on musculoskeletal injury incidence during British Army basic training. Published online February 27, 2020. BMJ Mil Heal. doi:10.1136/jramc-2019-001347 [DOI] [PubMed] [Google Scholar]
- 33. Popovich RM, Gardner JW, Potter R, Knapik JJ, Jones BH. Effect of rest from running on overuse injuries in army basic training. Am J Prev Med. 2000;18(3)(suppl):147–155. doi:10.1016/s0749-3797(99)00167-1 [DOI] [PubMed] [Google Scholar]
- 34. Psaila M, Ranson C. Risk factors for lower leg, ankle and foot injuries during basic military training in the Maltese Armed Forces. Phys Ther Sport. 2017;24:7–12. doi:10.1016/j.ptsp.2016.09.004 [DOI] [PubMed] [Google Scholar]
- 35. Reese M. Underweight: a heavy concern. Today’s Dietitian. 2008;10(1):56. Accessed November 30, 2020. https://www.todaysdietitian.com/newarchives/tdjan2008pg56.shtml [Google Scholar]
- 36. Saragiotto BT, Yamato TP, Hespanhol LC, Jr, Rainbow MJ, Davis IS, Lopes AD. What are the main risk factors for running-related injuries? Sports Med. 2014;44(8):1153–1163. doi:10.1007/s40279-014-0194-6 [DOI] [PubMed] [Google Scholar]
- 37. Soligard T, Schwellnus M, Alonso J-M, et al. How much is too much? (Part 1) International Olympic Committee consensus statement on load in sport and risk of injury. Br J Sports Med. 2016;50(17):1030–1041. doi:10.1136/bjsports-2016-096581 [DOI] [PubMed] [Google Scholar]
- 38. Sulsky SI, Bulzacchelli MT, Zhu L, et al. Risk factors for training-related injuries during U.S. Army basic combat training. Mil Med. 2018;183(suppl 1):55–65. doi:10.1093/milmed/usx147 [DOI] [PubMed] [Google Scholar]
- 39. Terry AC, Thelen MD, Crowell M, Goss DL. The Musculoskeletal Readiness Screening Tool---athlete concern for injury & prior injury associated with future injury. Int J Sports Phys Ther. 2018;13(4):595–604. doi:10.26603/ijspt20180595 [PMC free article] [PubMed] [Google Scholar]
- 40. United States Army. Army Regulation 600-9: The Army Body Composition Program. Department of the Army; 2019. [Google Scholar]
- 41. United States Military Academy, Department of Physical Education. How to physically prepare for cadet basic training. Accessed February 1, 2020. https://www.westpoint.edu/military/department-of-physical-education/cadet-candidates
- 42. United States Military Academy, Public Affairs Office. News release: class of 2022 to enter West Point. West Point; 2018. Accessed January 2, 2021. www.westpoint.edu/sites/default/files/pdfs/ABOUT/Public%20Affairs/Press%20Releases/Class%2520of%25202022%2520to%2520Enter%2520West%2520Point.pdf
- 43. Van derWorp MP, Ten Haaf DSM, Van Cingel R, De Wijer A, Nijhuis-Van der Sanden MWG, Staal JB. Injuries in runners; a systematic review on risk factors and sex differences. PLoS One. 2015;10(2):e0114937. doi:10.1371/journal.pone.0114937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Van Mechelen W, Hlobil H, Kemper HCG. Incidence, severity, aetiology and prevention of sports injuries: a review of concepts. Sports Med. 1992;14(2):82–99. doi:10.2165/00007256-199214020-00002 [DOI] [PubMed] [Google Scholar]
- 45. Videbæk S, Bueno AM, Nielsen RO, Rasmussen S. Incidence of running-related injuries per 1000 h of running in different types of runners: a systematic review and meta-analysis. Sports Med. 2015;45(7):1017–1026. doi:10.1007/s40279-015-0333-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Viester L, Verhagen EA, Hengel KMO, Koppes LL, Van Der Beek AJ, Bongers PM. The relation between body mass index and musculoskeletal symptoms in the working population. BMC Musculoskelet Disord. 2013;14:238. doi:10.1186/1471-2474-14-238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Vittinghoff E, Glidden DV, Shiboski SC, McCulloch CE. Survival analysis. In: Gail M, Krickeberg K, Samet J, Tsiatis A, Wong W, eds. Regression Methods in Biostatistics: Linear, Logistic, Survival, and Repeated Measures Models. Springer US; 2012:203–259. doi:10.1007/978-1-4614-1353-0_6 [Google Scholar]