Abstract
Background:
With recent improvements in transducer strength, image resolution, and operator training, ultrasound (US) provides an excellent alternative imaging modality for the diagnosis of rotator cuff tears.
Purpose:
To evaluate the diagnostic accuracy of US for partial- and full-thickness rotator cuff tears and biceps tendon tears, compare diagnostic values with those of magnetic resonance imaging (MRI) using arthroscopy as the reference standard, assess longitudinal improvements in accuracy, and compare diagnostic values from operators with different training backgrounds.
Study Design:
Systematic review; Level of evidence, 3.
Methods:
The PubMed and Cochrane Library databases were systematically searched for full-text journal articles published between January 1, 2010, and April 1, 2020. The inclusion criteria were studies that evaluated the diagnostic accuracy of US for rotator cuff tears or biceps tendon tears utilizing arthroscopy as the reference standard. The exclusion criteria were studies with <10 patients, studies including massive tears without reporting diagnostic data for specific tendons, and studies lacking diagnostic outcome data. Extracted outcomes included diagnostic accuracy, sensitivity, specificity, negative predictive value, and positive predictive value. The mean difference and 95% confidence interval were calculated for both US and MRI diagnostic values, and meta-analysis was conducted using the Mantel-Haenszel random-effects model.
Results:
In total, 23 eligible studies involving 2054 shoulders were included. US demonstrated a higher median diagnostic accuracy for supraspinatus tendon tears (0.83) and biceps tendon tears (0.93) as compared with subscapularis tendon tears (0.76). US was found to have a higher median accuracy (0.93) for full-thickness supraspinatus tears than partial-thickness tears (0.81). US had superior median sensitivity for partial-thickness supraspinatus tears when performed by radiologists as opposed to surgeons (0.86 vs 0.57). Meta-analysis of the 5 studies comparing US and MRI demonstrated no statistically significant difference in diagnostic sensitivity, specificity, or accuracy for any thickness supraspinatus tears (P = .31-.55), full-thickness tears (P = .63-.97), or partial-thickness tears (P = .13-.81).
Conclusion:
For experienced operators, US is a highly sensitive and specific diagnostic modality for the diagnosis of supraspinatus tears and demonstrates statistically equivalent capability to MRI in the diagnosis of both full- and partial-thickness rotator cuff tears.
Keywords: diagnostic ultrasound, rotator cuff, diagnostic imaging, systematic review, MRI
Rotator cuff tears may cause significant pain, decreased shoulder mobility, and irreparable damage to the glenohumeral joint. 37 Rotator cuff disorders are highly prevalent and represent the most common cause of shoulder disability in the United States. They are responsible for approximately 30% to 70% of shoulder pain-related conditions and 70% of shoulder-related physician visits while accounting for >4.5 million annual visits in the United States. 33,39,45 Additional population-based studies of symptomatic and asymptomatic individuals with a mean age of 58 years (range, 22-87 years) found a 21% prevalence of rotator cuff tears in the general population. 55,59 With >270,000 rotator cuff surgeries performed annually, the diagnosis and management of rotator cuff injuries accounts for >$3 billion in annual health care costs in the United States. 8,49,51 Given the high prevalence and economic burden of rotator cuff injury, accurate and cost-effective diagnostic modalities are critically important for efficient patient evaluation.
Accurate evaluation of rotator cuff pathology is necessary in the development of an algorithmic approach to guide treatment strategies. Although magnetic resonance imaging (MRI) is the preferred imaging modality for rotator cuff tears in the United States, ultrasound (US) has emerged as a convenient, viable, cost-effective alternative to MRI as a result of recent improvements in transducer strength, image resolution, and operator training. 31,48,56 Reimbursement from the Centers for Medicare & Medicaid Services for a hospital-based shoulder MRI (Current Procedural Terminology code 73221) ranges from $303.51 to $387.01, while reimbursement for a hospital-based shoulder US (Current Procedural Terminology code 76881) ranges from $144 to $189.37. Studies have suggested that this difference may be even greater within private insurance, where the average MRI reimbursement is $999.67 per patient. 60 US has also been shown to reduce patient wait times, increase efficiency, and reduce health care expenditure. 6 Therefore, US has been increasingly utilized in the diagnosis of both partial- and full-thickness rotator cuff tears. 5,43
Although US has demonstrated promising potential for evaluating rotator cuff tears, significant heterogeneity exists in the literature regarding the accuracy, sensitivity, and specificity of US in the diagnosis of full-thickness and partial-thickness tears. In a meta-analysis from 2015, Roy et al 46 found the specificity and sensitivity of US to be similar to those of MRI for the diagnosis of rotator cuff tears. Previous systematic reviews have also supported this finding, although these meta-analyses varied in their study inclusion criteria. 25,42,46 The most recent systematic review by Liang et al 26 in 2020 found the sensitivity and specificity of US to be 0.95 and 0.72, respectively, for any-sized rotator cuff tear but did not separately evaluate diagnostic values for full- and partial-thickness tears. Moreover, this review was limited by a small study size and the inclusion of both arthroscopy and MRI as the reference standards. 26 Given the rapid growth of US training and evolution of technology, an updated and comprehensive systematic review is essential to examine the diagnostic accuracy of US for both full-thickness and partial-thickness rotator cuff tears. Here, we present a systematic review of US in the diagnosis of full-thickness and partial-thickness rotator cuff tears and biceps tendon tears with arthroscopy used as the reference standard.
Methods
Literature Search
This systematic review was done in accordance with PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. 34 The PubMed and Cochrane Library databases were systematically searched for full-text journal articles in English published in the past 10 years, between January 1, 2010, and April 1, 2020. The search strings are shown in Appendix Table A1. Previous systematic reviews identified via the PubMed and Cochrane Library search were also assessed for relevant studies. These studies were also considered for inclusion in this systematic review.
Study Selection
The inclusion criteria were studies that evaluated the diagnostic accuracy of US in rotator cuff tears utilizing arthroscopy as the reference standard. The exclusion criteria included review articles, meta-analyses, systematic reviews, case reports, cadaveric studies, non-English text, studies with <10 patients, studies including massive tears without reporting diagnostic data for specific tendons, and studies lacking diagnostic outcome data.
Two authors (A.S.F. and A.L.) screened all journal articles identified via the PubMed and Cochrane Library database search as well as studies included in previous systematic reviews on the topic. Initial study inclusion was based on title and abstract review. The same 2 authors then assessed the full text of each eligible study for inclusion in the systematic review, with any disagreements resolved by discussion with a third author (R.L.P). Author names and institutional affiliations were used to determine the research group responsible for each included study. Multiple studies published by the same research group were included if patient overlap was considered unlikely based on study methodology.
A total of 804 articles were identified from the initial PubMed and Cochrane Library database search (Figure 1). An additional 367 studies were considered because of inclusion in relevant systematic reviews identified during the database search. Of the 1171 total studies reviewed, 1113 were excluded based on title and abstract, while 58 were further assessed for eligibility. Of these studies, 15 did not use arthroscopy as the reference standard, 4 were not in English, 2 included massive tears, and 4 lacked sufficient outcome data. After the removal of duplicates, 23 eligible studies involving 2054 shoulders were included in this systematic review.
Figure 1.
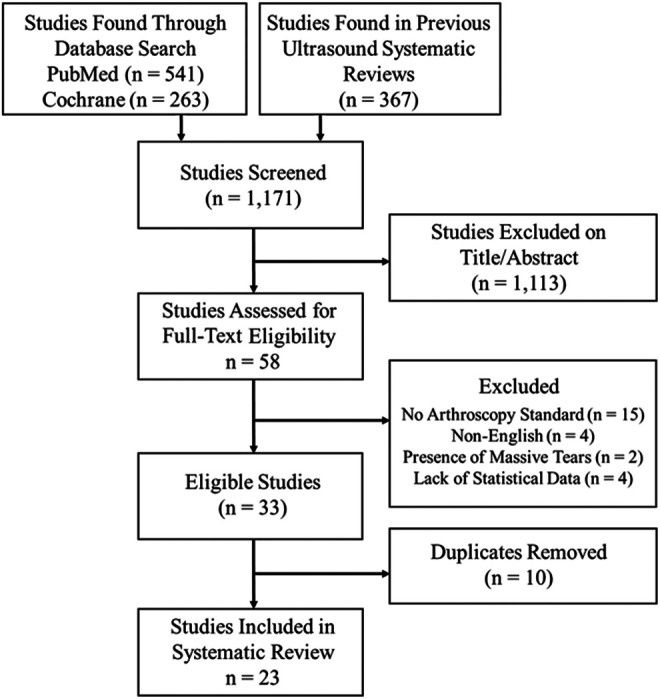
Study screening and selection process used to determine study eligibility and inclusion into the systematic review.
Data Extraction
The characteristic and diagnostic outcome data from each eligible study were extracted and inserted into predefined Excel (Version 2018; Microsoft Corp) spreadsheets by 2 authors (A.S.F. and A.L). The characteristic data included publication year, patient characteristics, study design, reference standard, injury type, time from US evaluation to arthroscopic evaluation, operator experience, and affected tendons. Diagnostic outcomes included the US diagnostic accuracy, sensitivity, specificity, negative predictive value (NPV), and positive predictive value (PPV) for any-sized, full-thickness, and partial-thickness rotator cuff tears. If additional MRI or magnetic resonance angiography (MRA) imaging was performed with arthroscopy as the standard, the same diagnostic outcomes for MRI/MRA were also extracted from the studies. If outcome data from ≥2 operators with different levels of experience were shared separately within the same study, only the diagnostic and outcome data from the most experienced operator were included. Similarly, when studies shared the outcome data from multiple cohorts of patients conducted by the same operator at various levels of experience, such as before and after a training intervention, only the outcome data from the latest cohort were included. One author (A.L.) extracted the raw diagnostic data (true positive, true negative, false positive, and false negative) when available and independently verified the reported diagnostic outcome data within the studies. Any discrepancies between raw diagnostic data and diagnostic outcomes data were resolved by deferral to the raw diagnostic data. In studies that included both MRI and arthroscopy as the reference standard, only the shoulders with arthroscopy as the reference standard were included.
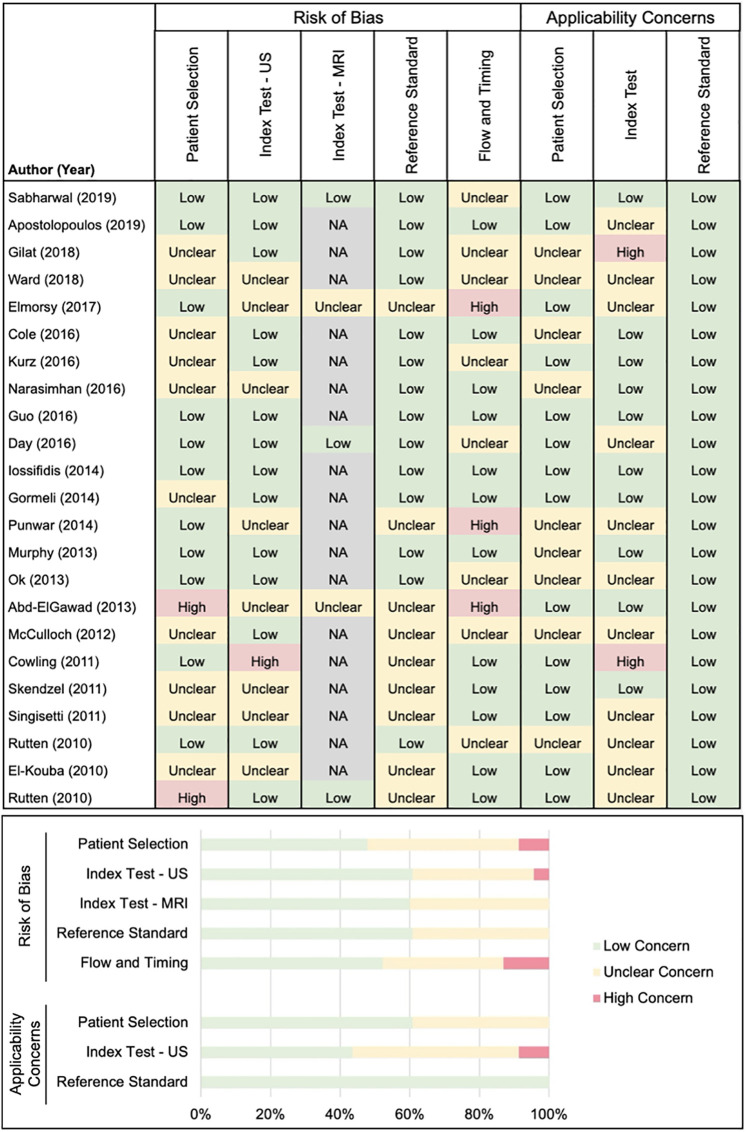
Quality and Bias Assessment
The quality and risk of bias for each included study was assessed by 2 authors (A.S.F. and A.L.) using the Quality Assessment of Diagnostic Accuracy Studies–2 (QUADAS-2) tool. 58 The QUADAS-2 tool assesses studies across 4 domains for risk of bias: patient selection, index test, reference standard, and flow and timing; and 3 domains for clinical applicability: patient selection, index test, and reference standard. For each domain, studies were assigned a score of low (low risk of bias or low concern regarding applicability), unclear, or high (high risk of bias or high concern regarding applicability). Studies that used both US and MRI as the index test were evaluated for risk of bias in each index test. Studies that did not use MRI as an index test were not assigned a score for this domain.
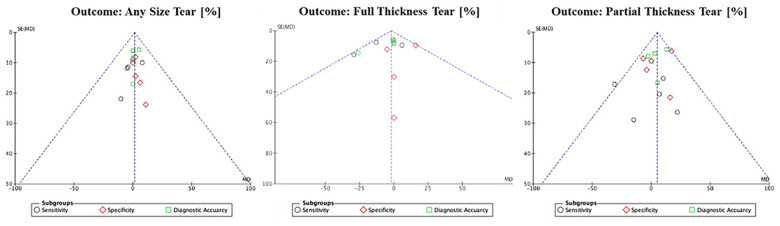
In an effort to assess for publication bias, we constructed funnel plots for each type of tear (any, full, and partial thickness) utilizing RevMan Version 5.3 (The Nordic Cochrane Centre; The Cochrane Collaboration, 2009). The plot depicts the relationship between sample size (y-axis) and the precision in estimating treatment effect (x-axis). Each individual point indicates a mean difference, and the outer dashed lines indicate a region within which 95% of studies are expected to fit into in the absence of bias. In the absence of bias, the plot resembles an inverted funnel with points symmetrically distributed about the pooled standard difference in means (dotted line centered about 0 on the x-axis).
Meta-Analysis
Diagnostic values were extracted from studies that directly compared US and MRI with arthroscopy as the gold standard. Extracted diagnostic values included sensitivity, specificity, and diagnostic accuracy for any sized–thickness, full-thickness, and partial-thickness supraspinatus tendon tears. Heterogeneity among the studies was evaluated using the I 2 statistic, where I 2 represents an estimated percentage of error attributed to interstudy variation. 21 Using the Mantel-Haenszel random-effects model, we calculated the mean differences and 95% confidence intervals (CIs) for each study and a cumulative weighted mean effect for all studies involved. The results are illustrated using forest plots. The meta-analysis was conducted with the utilization of RevMan Version 5.3. Significance was set at P <.05.
Results
Study Characteristics and Bias Assessment
Characteristic data from the 23 included studies are summarized in Table 1, and specifications of the US scanners from the studies are included in Table 2. A cohort of patients were excluded from 2 studies because MRI was used as the reference standard. 9,10 Two studies compared US capability between operators with different training backgrounds. In the study by Rutten et al, 48 the operators were a general and a musculoskeletal (MSK) radiologist, while in the work of Cole et al, 7 the operators were a MSK ultrasonographer and a general ultrasonographer. For these 2 studies, US results from only the MSK expert operator were included. Three studies compared the US diagnostic outcomes of cohorts at different points in time as surgeon ultrasonographers gained experience with the examination. 22,24,30 For these studies, the US results from only the final cohort of patients were included. Murphy et al 35 compared the performance of surgeons at different points in their training and tracked their improvement over time. For this study, we only included the diagnostic outcome data from the final cohort of patients evaluated by fellowship-trained shoulder surgeons.
Table 1.
Characteristic Data of the Included Studies (N = 23) a
| Study (Year) | Mean Patient Age, y | No. of Shoulders | Tear Type | Tendons Evaluated | Tear Thickness | US Operator |
|---|---|---|---|---|---|---|
| Sabharwal (2019) 50 | 45 | 60 | Primary | Supraspinatus | Full, partial | Radiologist (general) |
| Apostolopoulos (2019) 4 | 56 | 19 | Primary | Supraspinatus | Any | Radiologist (MSK) |
| Gilat (2018) 17 | 66 | 39 | Revision | Supraspinatus | Any, full | Surgeon |
| Ward (2018) 57 | 59 | 93 | Primary | Supraspinatus, subscapularis, biceps | Any | Radiologist (MSK), sonographer |
| Elmorsy (2017) 15 | 52 | 125 | Primary | Supraspinatus | Any, full, partial | Radiologist (MSK) |
| Cole (2016) 7 | NS | 238 | Primary | Supraspinatus | Any, full, partial | Sonographer (MSK and general) |
| Kurz (2016) 24 | 62 | 155 b | Primary | Supraspinatus | Any, full, partial | Sonographer |
| Narasimhan (2016) 36 | NS | 236 | Primary | Subscapularis | Any | Radiologist (MSK) |
| Guo (2016) 19 | 53 | 192 | Primary | Supraspinatus | Any, full, partial | NS |
| Day (2016) 10 | 55 | 19 c | Primary | Supraspinatus | Any, full, partial | Surgeon |
| Iossifidis (2014) 22 | NS | 70 b | NS | Supraspinatus | Full | Surgeon |
| Görmeli (2014) 18 | 51 | 50 | Primary | Supraspinatus | Any, full, partial | Radiologist (MSK) |
| Punwar (2014) 44 | NS | 64 | Primary | Supraspinatus | Any, full, partial | Radiologist (MSK) |
| Murphy (2013) 35 | NS | 51 b | NS | Supraspinatus | Any, full, partial | Surgeon |
| Ok (2013) 40 | NS | 51 | NS | Supraspinatus | Full, partial | Surgeon |
| Abd-ElGawad (2013) 2 | 55 | 40 | Primary | Supraspinatus | Any, full, partial | Radiologist (general) |
| McCulloch (2012) 30 | NS | 66 | Primary | Supraspinatus | Any | Surgeon |
| Cowling (2011) 9 | 45 | 122 c | NS | Supraspinatus, biceps | Any, full, partial | Sonographer |
| Skendzel (2011) 54 | 55 | 67 | NS | Biceps | Any, full, partial | Radiologist (MSK) |
| Singisetti (2011) 52 | 42 | 96 | NS | Supraspinatus, subscapularis | Any, full, partial | Radiologist (general) |
| Rutten (2010) 48 | 49 | 71 | Primary | Supraspinatus | Any, full, partial | Radiologist (MSK) |
| El-Kouba (2010) 14 | 46 | 101 | Primary | Supraspinatus | Any, full, partial | Radiologist (MSK) |
| Rutten (2010) 47 | 48 | 68 | Primary | Supraspinatus | Any, full, partial | Radiologist (MSK) |
a NS, not specified; MSK, musculoskeletal; US, ultrasound.
b Some shoulders from the study were excluded because an inexperienced operator was involved.
c Some shoulders from the study were excluded because magnetic resonance imaging was used as reference instead of arthroscopy.
Table 2.
Ultrasound Scanners Used in the Included Studies
| Study (Year) | Scanner | Portable | Scanner Release Date | Dates Used in Study | Linear Array Frequency, MHz |
|---|---|---|---|---|---|
| Sabharwal (2019) 50 | GE Voluson P8 | No | 2012 | NA | 7-12 |
| Gilat (2018) 17 | Sonosite 180 | Yes | 1998 | 1/2006 to 12/2011 | 3-11 |
| Cole (2016) 7 | GE LOGIQ E9 | No | 2009 | 1/2013 to 6/2015 | 6-15 |
| Kurz (2016) 24 | GE LOGIQ 9 GE LOGIQ E9 |
No No |
2005 2009 |
1/2007 to 5/2009 5/2009 to 6/2011 |
6-15 6-15 |
| Narasimhan (2016) 36 | Phillips iU 22 | No | 2004 | 1/2011 to 12/2012 | 5-17 |
| Guo (2016) 19 | Hitachi Preirus | No | 2009 | 5/2010 to 12/2014 | 5-13 |
| Iossifidis (2014) 22 | Mindray DP 6600 | Yes | 2007 | 5/2010 to 6/2011 | 10 |
| Görmeli (2014) 18 | GE Logiq S6 | No | 2007 | 8/2009 to 12/2010 | 7-12 |
| Murphy (2013) 35 | GE Volusion i | Yes | 2006 | 6/2009 to 12/2010 | 4.7-13 |
| Abd-ElGawad (2013) 2 | GE Logiq 5 | No | 2002 | 2/2009 to 10/2012 | 12 |
| Skendzel (2011) 54 | Phillips iU 22 GE LOGIQ 9 |
No No |
2004 2005 |
1/2007 to 2/2009 1/2007 to 2/2009 |
10-17 10-17 |
| Cowling (2011) 9 | Philips HDI 5000 | No | 1997 | 1/2005 to 7/2009 | 5-12 |
The overall risk of bias among the included studies was low, with 2 studies 2,47 exhibiting a high risk of bias in patient selection, 1 study 9 not reporting what documentation they used for US scan results, 3 studies 2,15,44 exhibiting >6 months of mean time between US and surgery, and 2 studies 9,17 using US technology from before the year 2000. The full results of the QUADAS-2 quality and bias assessment can be found in Figure 2. As there were a relatively small number of studies available for comparison, the funnel plots (Figure 3) could not truly distinguish chance from real asymmetry. However, from the available data for comparison, the plots indicated slight asymmetry and, therefore, a minimal amount of publication bias.
Figure 2.
Results of Quality Assessment of Diagnostic Accuracy Studies–2 quality and bias assessment. MRI, magnetic resonance imaging; NA, not applicable; US, ultrasound.
Figure 3.
Funnel plots of publication bias regarding ultrasound vs magnetic resonance imaging for supraspinatus tears. MD, mean difference.
The diagnostic capabilities of US in detecting any-thickness tears of the supraspinatus, subscapularis, and biceps tendons were evaluated (Table 3). US was identified as being more specific in the diagnosis of biceps tendon tears (0.99) and subscapularis tears (0.97) as compared with supraspinatus tears (0.73). However, US was the most sensitive in the diagnosis of supraspinatus tears (0.89) as compared with biceps tendon tears (0.61) and subscapularis tears (0.30). US also had a higher diagnostic accuracy for biceps tendon tears (0.93) and supraspinatus tears (0.83) as compared with subscapularis tears (0.76). US diagnosis of supraspinatus tears was further analyzed by tear thickness (Table 3). US was found to have a higher median sensitivity (0.88) and specificity (0.93) in the diagnosis of full-thickness supraspinatus tears as compared with partial-thickness tears, which demonstrated a median sensitivity and specificity of 0.65 and 0.86, respectively. US was also more accurate for full-thickness supraspinatus tears (0.93) than partial-thickness tears (0.81).
Table 3.
Ultrasound Diagnostic Values for Any-Sized Tear and for Partial- vs Full-Thickness Supraspinatus Tears a
| Any-Sized Rotator Cuff or Biceps Tear | Partial- vs Full-Thickness Supraspinatus Tears | ||||
|---|---|---|---|---|---|
| Supraspinatus | Subscapularis | Biceps | Full Thickness | Partial Thickness | |
| No. of studies (shoulders) | 17 (1448) | 3 (425) | 3 (282) | 17 (1516) | 15 (1407) |
| Diagnostic values | |||||
| Diagnostic accuracy | 0.83 (0.66-0.97) | 0.76 (0.68-0.80) | 0.93 (0.88-0.97) | 0.93 (0.67-0.97) | 0.81 (0.45-0.93) |
| Sensitivity | 0.89 (0.70-1.00) | 0.30 (0.13-0.39) | 0.61 (0.58-0.80) | 0.88 (0.50-0.96) | 0.65 (0.08-1.00) |
| Specificity | 0.73 (0.29-1.00) | 0.97 (0.93-1.00) | 0.99 (0.98-1.00) | 0.93 (0.59-1.00) | 0.86 (0.56-0.96) |
| NPV | 0.80 (0.11-1.00) | 0.76 (0.68-0.78) | 0.94 (0.86-0.99) | 0.91 (0.64-0.98) | 0.91 (0.57-1.00) |
| PPV | 0.93 (0.61-1.00) | 0.73 (0.67-1.00) | 0.92 (0.67-1.00) | 0.89 (0.67-1.00) | 0.68 (0.10-0.93) |
a Diagnostic values are reported as median (range). NPV, negative predictive value; PPV, positive predictive value.
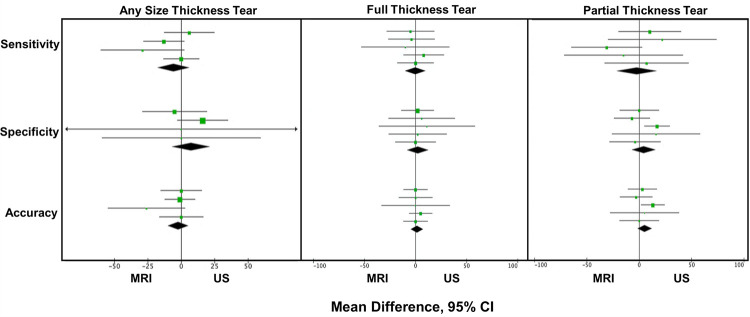
Five studies compared the diagnostic capability of US and MRI for supraspinatus tears using arthroscopy as the reference standard and were included for meta-analysis (Figure 4). 2,10,15,48,50 Median sensitivity and specificity for full-thickness tears was 0.94 and 0.94 for US and 0.94 and 0.89 for MRI, respectively. When diagnosing partial-thickness tears, median sensitivity and specificity were 0.89 and 0.89 for US and 0.85 and 0.87 for MRI, respectively. No significant heterogeneity was observed among the studies in US and MRI diagnostic outcomes when evaluating any size–thickness tears (I 2 = 0%-43%; P = .16-.59), full-thickness tears (I 2 = 0%; P = .89-.99), or partial-thickness tears (I 2 = 0%-41%; P = .15-.50). After pooling the results, no significant difference was found for the sensitivity, specificity, or accuracy of US as compared with MRI in the diagnosis of any sized–thickness tear (mean differences: sensitivity = –5.86 [95% CI, –17.69 to 5.97], P = .33; specificity = 7.39 [95% CI, –6.86 to 21.65], P = .31; diagnostic accuracy = –2.31 [95% CI, –9.97 to 5.35], P = .55), full-thickness tear (sensitivity = –0.19 [95% CI, –10.11 to 9.72], P = .97; specificity = 2.30 [95% CI, –8.08 to 12.68], P = .66; diagnostic accuracy = 1.48 [95% CI, –4.57 to 7.54], P = .63), or partial-thickness tear (sensitivity –2.36 [95% CI, –21.51 to 16.79], P = .81; specificity = 4.30 [95% CI, –7.06 to 15.66], P = .46; diagnostic accuracy = 5.25 [95% CI, –1.60 to 12.10], P = .13), respectively.
Figure 4.
Meta-analysis of ultrasound (US) and magnetic resonance imaging (MRI) diagnostic capabilities. Individual data points within each subgroup represent the mean difference and 95% CI of US and MRI diagnostic values for each included study. The results of each study were then pooled and weighted by the number of shoulders evaluated to determine overall effect.
The diagnostic capability of US by operator experience was also analyzed (Table 4). US conducted by surgeons and radiologists demonstrated similar specificity and sensitivity for full-thickness supraspinatus tears, but radiologists were identified as having a superior median sensitivity (0.86) as compared with surgeons (0.57) in detecting partial-thickness supraspinatus tendon tears. Moreover, the median PPV for partial-thickness supraspinatus tears was low for both radiologists (0.43) and surgeons (0.44).
Table 4.
Comparison of US Diagnostic Values for Supraspinatus Tear Operator Experience a
| Full-Thickness Tear | Partial-Thickness Tear | |||
|---|---|---|---|---|
| Radiologist | Surgeon | Radiologist | Surgeon | |
| No. of studies (shoulders) | 8 (579) | 5 (230) | 8 (579) | 3 (121) |
| Diagnostic values | ||||
| Diagnostic accuracy | 0.94 (0.67-0.97) | 0.92 (0.74-0.97) | 0.81 (0.63-0.93) | 0.79 (0.45-0.84) |
| Sensitivity | 0.91 (0.58-0.96) | 0.87 (0.50-0.95) | 0.86 (0.08 -1.00) | 0.57 (0.46-0.71) |
| Specificity | 0.92 (0.74 -1.00) | 0.98 (0.86 -1.00) | 0.84 (0.56-0.93) | 0.83 (0.75-0.89) |
| NPV | 0.93 (0.66-0.98) | 0.90 (0.64-0.98) | 0.94 (0.78 -1.00) | 0.83 (0.83-0.93) |
| PPV | 0.86 (0.67 -1.00) | 0.95 (0.89 -1.00) | 0.43 (0.10-0.86) | 0.44 (0.33-0.71) |
a Diagnostic values are reported as median (range). NPV, negative predictive value; PPV, positive predictive value; US, ultrasound.
In addition, we compared the diagnostic capabilities of US between articles published in the first (2010-2015) and second (2016-2020) halves of the database search period (Table 5). US demonstrated greater diagnostic accuracy for full- and partial-thickness tears among studies published between 2016 and 2020 than among studies published between 2010 and 2015. Only 12 out of 23 studies reported the US technology and linear-array frequency used (Table 2). ¶ Among this limited sample, linear-array frequency was observed to be similar among studies from both time periods, but more recent studies tended to use scanners that were more recently released.
Table 5.
Comparison of US Diagnostic Values for Supraspinatus Tears Between the First and Second Halves of the Study Period a
| Full-Thickness Tear | Partial-Thickness Tear | |||
|---|---|---|---|---|
| 2010-2015 | 2016-2020 | 2010-2015 | 2016-2020 | |
| No. of studies (shoulders) | 11 (707) | 6 (809) | 9 (515) | 6 (892) |
| Diagnostic values | ||||
| Diagnostic accuracy | 0.92 (0.67-0.97) | 0.97 (0.81-0.99) | 0.79 (0.45-0.90) | 0.91 (0.79-0.93) |
| Sensitivity | 0.88 (0.50-0.96) | 0.91 (0.77-1.00) | 0.71 (0.08-1.00) | 0.64 (0.23-0.95) |
| Specificity | 0.93 (0.74-1.00) | 0.95 (0.59-1.00) | 0.82 (0.56-0.89) | 0.92 (0.69-0.96) |
| NPV | 0.91 (0.64-0.98) | 0.89 (0.73-1.00) | 0.86 (0.78-1.00) | 0.92 (0.57-0.97) |
| PPV | 0.89 (0.67-1.00) | 0.91 (0.77-1.00) | 0.44 (0.10-0.82) | 0.70 (0.21-0.93) |
a Diagnostic values are reported as median (range). NPV, negative predictive value; PPV, positive predictive value; US, ultrasound.
Discussion
In this review, we demonstrated that US is a reliable and effective imaging modality for the diagnosis of rotator cuff tears. US was found to have a median sensitivity and specificity of 0.88 and 0.93 for full-thickness supraspinatus tears and 0.65 and 0.86 for partial-thickness supraspinatus tears, respectively. Although US was highly specific in diagnosing any-thickness subscapularis and biceps tendon tears, the respective sensitivities for subscapularis and biceps tendon tears were only 0.30 and 0.61. Moreover, improved diagnostic accuracy of US in partial-thickness tears was found in studies published within the most recent 5 years (2016-2020) as compared with studies published during the first 6 years (2010-2015) of our review. Radiologists also demonstrated a superior diagnostic sensitivity of 0.86 as compared with 0.57 for surgeons in the diagnosis of partial-thickness supraspinatus tears.
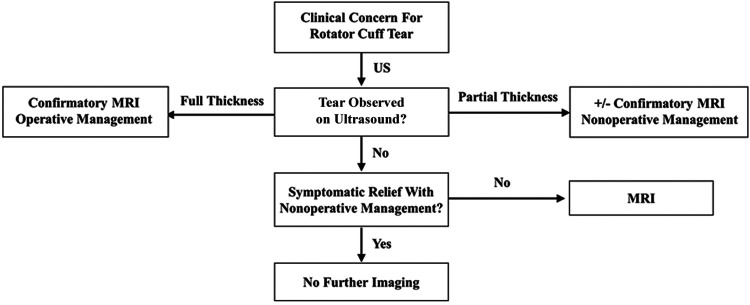
The high sensitivity and specificity of US (0.88 and 0.93, respectively) for the detection of full-thickness supraspinatus tears is consistent with prior systematic reviews and meta-analyses. 25,28,41,46 In contrast, US demonstrated a lower median sensitivity and specificity for partial-thickness tears, at 0.65 and 0.86, respectively. In support of these findings, 1 study reported that diagnostic accuracy increased with tear size for full-thickness supraspinatus tears. 9 One proposed contributing factor to the lower US sensitivity realized for partial-thickness tears may be the variable echogenicity of synovial proliferation, granulation, and scar tissue formation surrounding a partial tear, thus impeding clear tissue differentiaiton. 40 Because of the lower US sensitivity for partial-thickness tears, it has been recommended to follow a negative US examination with an MRI in patients who do not experience symptomatic relief following conservative treatment. 53 We propose a similar diagnostic US screening algorithm shown in Figure 5.
Figure 5.
Proposed ultrasound diagnostic screening algorithm for the evaluation of rotator cuff tears. MRI, magnetic resonance imaging; US, ultrasound.
While the majority of previous US studies have focused primarily on the imaging of the supraspinatus and infraspinatus tendons, concomitant tears of the subscapularis tendon are rather common, with literature reporting their identification in around 50% of all rotator cuff repairs. 12,16 Three studies in this systematic review found that US demonstrated high specificity (0.93-1.00) and low sensitivity (0.13-0.39) for diagnosing the entire spectrum of subscapularis tearing, including full or partial tears. 36,52,57 One of the likely significant contributors to the low sensitivity for subscapularis tears is the reduced access of US to the subscapularis region relative to the other rotator cuff tendons. 12 Previous studies have shown that MRI demonstrates a similarly low sensitivity for the diagnosis of subscapularis tears. 3 Three studies reported on the diagnostic outcomes of US evaluation of tears of the long head of the biceps brachii (LHB) tendon. 9,54,57 Skendzel et al 54 reported high accuracy in diagnosing LHB tendons with full-thickness tears and tendons without pathology but difficulty distinguishing between partial-thickness LHB tendon tears and other pathology, such as tendinosis and tenosynovitis. Evaluation of both the subscapularis and the LHB tendon via US is poorly represented in the literature, and further studies are needed to clearly define US diagnostic accuracy. Because of the high specificity and low sensitivity of US for subscapularis and biceps tendon tears, we suggest using US as a confirmatory diagnostic imaging modality in patients with suspected pathology but not for screening patients.
Previous reports in the literature have suggested that the diagnostic capability of US for rotator cuff pathology is heavily dependent on operator skill for both image acquisition and interpretation. 32,38 Three studies demonstrated that the accuracy, sensitivity, and specificity of US for supraspinatus tears improved with an increased number of scans among less experienced operators. 22,30,35 Rutten et al 48 showed a limit to this increasing proficiency—an experienced radiologist with MSK training and a less experienced radiologist without MSK training performed equally well in identifying full- and partial-thickness supraspinatus tears among the same 200 patients. Other studies have suggested that receiving feedback from surgical results accelerates operator training and improves operator performance. Kurz et al 24 found that an experienced MSK sonographer improved the sensitivity from 93% to 99% and specificity from 68% to 93% for detecting supraspinatus tears after attending arthroscopy procedures and reviewing the associated surgical reports. Similarly, Murphy et al 35 and Iossifidis et al 22 found that shoulder surgeons who operated on the same day as the US examination were able to achieve sensitivity and specificity values for full-thickness supraspinatus tears comparable with experienced MSK radiologists within 50 to 140 scans. This demonstrates the achievement of US proficiency far sooner than the 250 to 300 shoulder minimum put forth by the European Federation of Societies for Ultrasound in Medicine and Biology and the Royal College of Radiologists for radiologists who traditionally did not review the subsequent surgical reports. 1,23
In this systematic review, surgeons who performed US were found to identify full-thickness supraspinatus tears with the same sensitivity and specificity as radiologists (Table 4), consistent with results of a previous meta-analysis. 46 Although surgeons identified partial-thickness tears with the same specificity as did radiologists (0.83 vs 0.84), they demonstrated lower sensitivity (0.57 vs 0.86). The 3 studies 10,35,40 that reported sensitivity in detecting partial-thickness supraspinatus tears among surgeon evaluators all included surgeons with <1 year of US training. This suggests that new US operators gain proficiency in diagnosing full-thickness supraspinatus tears before partial-thickness supraspinatus tears.
In 5 of the 6 studies that reported diagnostic outcomes for surgeon-led US shoulder examinations, the surgeon who performed the US examination also performed the subsequent arthroscopic examination. 10,17,22,30,35 This lack of blinding may have influenced the results of these studies but was largely unavoidable, as operating without first visualizing the preoperative imaging adds unnecessary impediment to successful surgery. Moreover, 5 of the 6 studies followed surgeons with <1 year of shoulder US experience. 10,22,30,35,40 Our results are therefore not representative of the diagnostic sensitivity and specificity surgeons may be capable of following several years of practice. Our findings suggested that even surgeons who are relatively novice ultrasonographers are capable of properly assessing supraspinatus tendon tears via US evaluation, consistent with the results from Murphy et al, 35 who demonstrated that surgeons could gain comparable proficiency with MSK radiologists within 50 to 100 scans. The potential for surgeons to rapidly gain US proficiency in the diagnosis of rotator cuff tears has also led to an increased push to include US training in orthopaedic residency programs. 27
Five studies evaluated in this review included US and MRI diagnostic outcome data with arthroscopy as reference. 2,10,15,47,50 After meta-analysis, no significant differences were found in US and MRI diagnostic sensitivity, specificity, and accuracy for any sized–thickness, full-thickness, or partial-thickness supraspinatus tears (Figure 4). These results are consistent with those of recent systematic reviews and meta-analyses. 25,28,46 With the comparable diagnostic capabilities of US and MRI, there are several other factors that make US an appealing option. US is more affordable and efficient as compared with MRI, an appealing characteristic given the recent focus on health care expenditure and movement toward a value-based model of care. 6 Diagnostic US of the shoulder has been shown to be more cost-effective than MRI for rotator cuff tears, with lower Medicare and private insurance reimbursements. 20,60 US can also be performed in a variety of settings where it is more convenient for the patient, such as at the office or courtside at sporting events. 9 However, the incorporation of US into the diagnostic pathway requires appropriate equipment and support staff and may place an increased time burden on the surgeon. US also has essentially no contraindications. MRI, by comparison, is contraindicated for patients with implanted devices with ferromagnetic or electrically conductive materials, such as left ventricular assist devices, electrically conductive pulmonary artery monitoring catheters, and cochlear implants. 11,13,29 Finally, hemorrhage can give the false appearance of a full-thickness supraspinatus tear on MRI scans. This issue is obviated with US, as no tendon tear will be demonstrated upon dynamic visualization.
The capability of US for diagnosing rotator cuff tears is still improving. The median diagnostic accuracy of US for full-thickness supraspinatus tears increased from 0.92 to 0.97 when comparing studies published between 2010 and 2015 to studies published between 2016 and 2020 (Table 5). The median diagnostic accuracy of US for partial-thickness supraspinatus tears also increased from 0.79 to 0.91 when comparing studies published between 2010 and 2015 with studies between 2016 and 2020. We hypothesize that 2 drivers of this continuing improvement are improvements in technology and training. We found that studies from both time periods used similar linear-array frequencies but more recent studies typically employed more recently developed US scanners (Table 2). However, the significance of this finding is limited by the fact that only 12 of the 23 included studies described the US technology and frequency used. # As US training and technology continue to improve, the diagnostic accuracy of shoulder US should continue to be evaluated.
Limitations
While arthroscopy is the gold standard for assessing rotator cuff pathology, its use as the reference standard in a diagnostic study may introduce patient selection bias. Shoulders that go on to arthroscopic evaluation may have more severe pathology, while those without significant imaging findings may not be assessed arthroscopically. Additionally, 10 studies ** in our analysis did not have preoperative US for each patient who underwent arthroscopy, and 2 studies 2,47 only included the subset of arthroscopically evaluated patients with both preoperative US and preoperative MRI. This selection bias could have also potentially affected the NPV and PPV reported in this study because those values depend on the prevalence of tears within the studied cohort. As a result, the NPV and PPV reported in this study may not necessarily be representative of the general population, which may have a lower prevalence of rotator cuff tears.
Moreover, the mean time from US examination to arthroscopic evaluation was >6 months in 3 studies 2,15,44 and was not reported in another 8 studies. 10,17,24,30,40,48,50,57 Variability in time from patient presentation to surgery could influence the correlation between US results and arthroscopy because of subsequent healing or further damage.
A few subanalyses were limited by a small sample of studies, such as the comparison of diagnostic capability of US and MRI, as well as the studies reporting on subscapularis and biceps tendon pathology. Further studies evaluating the diagnostic capability of US for subscapularis and biceps tendon tears are needed to make more definitive conclusions. Although meta-analysis was used to statistically compare US and MRI diagnostic values, meta-analysis could not be done for the other subanalyses in this study, as the methodology of the other studies were incompatible for the conduction of a meta-analysis. As such, definitive statistical conclusions could not be made about the other subanalyses. However, this limitation is mitigated by the fact that only readily apparent differences and trends were reported within this study.
Conclusion
This study demonstrated that US is highly sensitive and specific in the diagnosis of supraspinatus tears and is more accurate in the diagnosis of full-thickness tears as compared to partial-thickness tears. Although US was found to be highly specific for diagnosing subscapularis and biceps tendon tears, the sensitivity was low, and the diagnostic data were limited by a small number of studies. Surgeons were found to rapidly gain proficiency for US evaluation of supraspinatus tears, but radiologists demonstrated superior sensitivity for diagnosing partial-thickness supraspinatus tears. US and MRI were also found to have statistically similar diagnostic capabilities in the diagnosis of supraspinatus tears. US is therefore a reliable imaging modality for diagnosing supraspinatus tears and can be reliably taught to orthopaedic surgeons, demonstrating the widespread potential for US in the diagnosis of rotator cuff tears. As US technology and operator training continue to improve, more systematic reviews will be needed to assess the diagnostic accuracy of US for rotator cuff pathology. Further studies evaluating the utility of US for subscapularis and biceps tendon tears are also needed to better analyze US diagnostic accuracy for rotator cuff tears.
APPENDIX
Table A1.
PubMed and Cochrane Library Literature Search Strings a
| PubMed was searched using the following
terms: (((Ultrasonograph*[text word]) OR (Ultrasound[text word]) OR (Sonography[MeSH Terms]) OR (Sonograph*[text word]) OR (US[text word])) AND ((sensitivity[text word]) OR (specificity[text word]) OR (diagnostic accuracy[text word]) OR (diagnostic value [text word]) OR (accuracy [text word]) OR (reliability [text word])) AND ((shoulder[text word]) OR (biceps tendon[text word]) OR (rotator cuff[text word]) OR (supraspinatus[text word]) OR (infraspinatus[text word]) OR (Subscapularis[text word]) OR (teres minor[text word]) OR (tendinopathy[text word]) OR (shoulder pain[text word]) OR (shoulder impingement syndrome[text word]) OR (bursitis[text word]) OR (tendinopathy[text word]) OR (bursitis[text word]))). |
| Cochrane Library was searched using the following
terms: (((Ultrasonograph*) OR (Ultrasound) OR (Sonography) OR (Sonograph*) OR (US)) AND ((sensitivity) OR (specificity) OR (diagnostic accuracy) OR (diagnostic value) OR (accuracy) OR (reliability)) AND ((shoulder) OR (biceps tendon) OR (rotator cuff) OR (supraspinatus) OR (infraspinatus) OR (Subscapularis) OR (teres minor) OR (tendinopathy) OR (shoulder pain) OR (bursitis) OR (tendinopathy) OR (bursitis))) |
a MeSH, Medical Subject Headings.
Footnotes
Final revision submitted April 4, 2021; accepted May 4, 2021.
One or more of the authors has declared the following potential conflict of interest or source of funding: X.L. has received consulting fees and royalties from FH Ortho. J.D.K. has received consulting fees from Flexion and royalties from SLACK and Springer. R.L.P. has received grant/educational support from Arthrex. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Al-Shawi A, Badge R, Bunker T. The detection of full thickness rotator cuff tears using ultrasound. J Bone Joint Surg Br. 2008;90(7):889–892. [DOI] [PubMed] [Google Scholar]
- 2. Abd-ElGawad EA, Ibraheem MA, Fouly EH. Evaluation of supraspinatus muscle tears by ultrasonography and magnetic resonance imaging in comparison with surgical findings. Egypt J Radiol Nuclear Med. 2013;44(4):829–834. [Google Scholar]
- 3. Adams CR, Schoolfield JD, Burkhart SS. Accuracy of preoperative magnetic resonance imaging in predicting a subscapularis tendon tear based on arthroscopy. Arthroscopy. 2010;26(11):1427–1433. [DOI] [PubMed] [Google Scholar]
- 4. Apostolopoulos AP, Angelis S, Yallapragada RK, et al. The sensitivity of magnetic resonance imaging and ultrasonography in detecting rotator cuff tears. Cureus. 2019;11(5):e4581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bouffard JA, Lee S-M, Dhanju J. Ultrasonography of the shoulder. Semin Ultrasound CT MR. 2000;21(3):164–191. [DOI] [PubMed] [Google Scholar]
- 6. Chiu C-H, Chen P, Chen AC-Y, et al. Shoulder ultrasonography performed by orthopedic surgeons increases efficiency in diagnosis of rotator cuff tears. J Orthop Surg Res. 2017;12(1):63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cole B, Twibill K, Lam P, Hackett L, Murrell G. Not all ultrasounds are created equal: general sonography vs. musculoskeletal sonography in the detection of rotator cuff tears. Shoulder & Elbow. 2016;8(4):250–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Colvin AC, Harrison AK, Flatow EL, Egorova N, Moskowitz A. National trends in rotator cuff repair. J Bone Joint Surg Am. 2012;94(3):227–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Cowling P, Gamble A, Rangan A. The use of shoulder ultrasound in a one-stop clinic: diagnostic accuracy for rotator cuff tear and biceps tendon pathology. Shoulder Elbow. 2011;3(1):13–16. [Google Scholar]
- 10. Day M, Phil M, McCormack RA, Nayyar S, Jazrawi L. Physician training ultrasound and accuracy of diagnosis in rotator cuff tears. Bull Hosp Jt Dis. 2016;74(3):207–211. [PubMed] [Google Scholar]
- 11. Dedini RD, Karacozoff AM, Shellock FG, et al. MRI issues for ballistic objects: information obtained at 1.5-, 3- and 7-Tesla. Spine J. 2013;13(7):815–822. [DOI] [PubMed] [Google Scholar]
- 12. Denard PJ, Burkhart SS. Arthroscopic recognition and repair of the torn subscapularis tendon. Arthrosc Tech. 2013;2(4):e373–e379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Dill T. Contraindications to magnetic resonance imaging. Heart. 2008;94(7):943–948. [DOI] [PubMed] [Google Scholar]
- 14. El-Kouba G, Andreas Huber T, Freitas JRW, et al. Comparison of complementary exams in the diagnosis of rotator cuff injuries. Rev Bras Ortop. 2010;45(5):418–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Elmorsy A, Keightley A, Flannery M. Accuracy of ultrasonography (US) and magnetic resonance imaging (MRI) in detection of rotator cuff tears in District General Hospital. Pol J Radiol. 2017;82:634–637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Garavaglia G, Ufenast H, Taverna E. The frequency of subscapularis tears in arthroscopic rotator cuff repairs: a retrospective study comparing magnetic resonance imaging and arthroscopic findings. Int J Shoulder Surg. 2011;5(4):90–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Gilat R, Atoun E, Cohen O, et al. Recurrent rotator cuff tear: is ultrasound imaging reliable? J Shoulder Elbow Surg. 2018;27(7):1263–1267. [DOI] [PubMed] [Google Scholar]
- 18. Görmeli C, Görmeli G, Yücesoy C, Ataoglu B, Kanatli U. Comparison of the results of ultrasonographic evaluation and arthroscopy in patients scheduled for surgery of the supraspinatus tendon rupture. Ann Saudi Med. 2014;34(6):522–526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Guo L-P, Wang W-M, Wang Y-H, et al. Ultrasound in assessment of supraspinatus tendon injury: correlation with arthroscopy. Chin Med J (Engl). 2016;129(3):361–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Gyftopoulos S, Guja KE, Subhas N, Virk MS, Gold HT. Cost-effectiveness of magnetic resonance imaging versus ultrasound for the detection of symptomatic full-thickness supraspinatus tendon tears. J Shoulder Elbow Surg. 2017;26(12):2067–2077. [DOI] [PubMed] [Google Scholar]
- 21. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–1558. [DOI] [PubMed] [Google Scholar]
- 22. Iossifidis A, Ibrahim EF, Petrou C. Ultrasound for the detection of full-thickness rotator cuff tears: the learning curve for an orthopaedic surgeon using a novel training method. Shoulder Elbow. 2014;7(3):158–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Klauser AS, McNally E, Chhem RK. Training musculoskeletal ultrasound specialists: European education and clinical guidelines: work in progress. In: van Deven T, Hibbert KM, Chhem RK, eds. The Practice of Radiology Education: Challenges and Trends. Springer Berlin Heidelberg; 2010:143–159. [Google Scholar]
- 24. Kurz AZ, Kelly MJ, Hackett L, Murrell GAC. Effect of surgeon-sonographer interaction on ultrasound diagnosis of rotator cuff tears: a five-year cohort study in 775 shoulders. J Shoulder Elbow Surg. 2016;25(9):1385–1394. [DOI] [PubMed] [Google Scholar]
- 25. Lenza M, Buchbinder R, Takwoingi Y, et al. Magnetic resonance imaging, magnetic resonance arthrography and ultrasonography for assessing rotator cuff tears in people with shoulder pain for whom surgery is being considered. Cochrane Database Syst Rev. 2013;2013(9):CD009020–CD009020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Liang W, Wu H, Dong F, Tian H, Xu J. Diagnostic performance of ultrasound for rotator cuff tears: a systematic review and meta-analysis. Med Ultrason. 2020;22(2):197–202. [DOI] [PubMed] [Google Scholar]
- 27. Lin A, Gasbarro G, Sakr M. Clinical applications of ultrasonography in the shoulder and elbow. J Am Acad Orthop Surg. 2018;26(9):303–312. [DOI] [PubMed] [Google Scholar]
- 28. Liu F, Dong J, Shen W-J, et al. Detecting rotator cuff tears: a network meta-analysis of 144 diagnostic studies. Orthop J Sports Med. 2020;8(2):2325967119900356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Mamas N, Andreanos K, Brouzas D, et al. Acute ocular pain during magnetic resonance imaging due to retained intraocular metallic foreign body: the role of ultrasonography and ultrasound biomicroscopy in diagnosis and management of this condition. J Ultrasound. 2018;21(2):159–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. McCulloch RA, McBride T, Choudhury Z, Armitstead C, Simons AW. Surgeon-lead shoulder ultrasound for rotator cuff tears, accuracy and learning curve. Shoulder Elbow. 2013;5(1):30–32. [Google Scholar]
- 31. Middleton WD, Edelstein G, Reinus WR, Melson GL, Murphy WA. Ultrasonography of the rotator cuff: technique and normal anatomy. J Ultrasound Med. 1984;3(12):549–551. [DOI] [PubMed] [Google Scholar]
- 32. Middleton WD, Teefey SA, Yamaguchi K. Sonography of the rotator cuff: analysis of interobserver variability. AJR Am J Roentgenol. 2004;183(5):1465–1468. [DOI] [PubMed] [Google Scholar]
- 33. Mitchell C, Adebajo A, Hay E, Carr A. Shoulder pain: diagnosis and management in primary care. BMJ. 2005;331(7525):1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Moher D, Liberati A, Tetzlaff J, Altman DG; the PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. J Clin Epidemiol. 2009;62(10):1006–1012. [DOI] [PubMed] [Google Scholar]
- 35. Murphy RJ, Daines MT, Carr AJ, Rees JL. An independent learning method for orthopaedic surgeons performing shoulder ultrasound to identify full-thickness tears of the rotator cuff. J Bone Joint Surg Am. 2013;95(3):266–272. [DOI] [PubMed] [Google Scholar]
- 36. Narasimhan R, Shamse K, Nash C, Dhingra D, Kennedy S. Prevalence of subscapularis tears and accuracy of shoulder ultrasound in pre-operative diagnosis. Int Orthop. 2016;40(5):975–979. [DOI] [PubMed] [Google Scholar]
- 37. Nathani A, Smith K, Wang T. Partial and full-thickness RCT: modern repair techniques. Curr Rev Musculoskelet Med. 2018;11(1):113–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Nazarian LN, Jacobson JA, Benson CB, et al. Imaging algorithms for evaluating suspected rotator cuff disease: Society of Radiologists in Ultrasound Consensus Conference Statement. Radiology. 2013;267(2):589–595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Oh LS, Wolf BR, Hall MP, Levy BA, Marx RG. Indications for rotator cuff repair: a systematic review. Clin Orthop Relat Res. 2007;455:52–63. [DOI] [PubMed] [Google Scholar]
- 40. Ok J-H, Kim Y-S, Kim J-M, Yoo T-W. Learning curve of office-based ultrasonography for rotator cuff tendons tears. Knee Surg Sports Traumatol Arthrosc. 2013;21(7):1593–1597. [DOI] [PubMed] [Google Scholar]
- 41. Okoroha KR, Fidai MS, Tramer JS, Davis KD, Kolowich PA. Diagnostic accuracy of ultrasound for rotator cuff tears. Ultrasonography. 2019;38(3):215–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Ottenheijm RP, Jansen MJ, Staal JB, et al. Accuracy of diagnostic ultrasound in patients with suspected subacromial disorders: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2010;91(10):1616–1625. [DOI] [PubMed] [Google Scholar]
- 43. Papatheodorou A, Ellinas P, Takis F, et al. US of the shoulder: rotator cuff and non-rotator cuff disorders. Radiographics. 2006;26(1):e23. [DOI] [PubMed] [Google Scholar]
- 44. Punwar S, Blewitt N. Pre-operative departmental ultrasound of the rotator cuff: sensitivity and specificity in a regional specialist orthopaedic centre. Shoulder Elbow. 2014;6(2):72–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Rees JL. The pathogenesis and surgical treatment of tears of the rotator cuff. J Bone Joint Surg Br. 2008;90(7):827–832. [DOI] [PubMed] [Google Scholar]
- 46. Roy J-S, Braën C, Leblond J, et al. Diagnostic accuracy of ultrasonography, MRI and MR arthrography in the characterisation of rotator cuff disorders: a systematic review and meta-analysis. Br J Sports Med. 2015;49(20):1316–1328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Rutten MJ, Spaargaren GJ, van Loon T, et al. Detection of rotator cuff tears: the value of MRI following ultrasound. Eur Radiol. 2010;20(2):450–457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Rutten MJCM, Jager GJ, Kiemeney LALM. Ultrasound detection of rotator cuff tears: observer agreement related to increasing experience. AJR Am J Roentgenol. 2010;195(6):W440–W446. [DOI] [PubMed] [Google Scholar]
- 49. Sabesan VJ, Shahriar R, Chatha K, et al. Factors affecting the cost and profitability of arthroscopic rotator cuff repair. Arthroscopy. 2019;35(1):38–42. [DOI] [PubMed] [Google Scholar]
- 50. Sabharwal T, Khanduri S, Khan S, et al. A comparative assessment between high-resolution ultrasonography and field magnetic resonance imaging in supraspinatus tear cases and its arthroscopic correlation. Cureus. 2019;11(9):e5627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Savoie FH, Field LD, Nan Jenkins R. Costs analysis of successful rotator cuff repair surgery: an outcome study. Comparison of gatekeeper system in surgical patients. Arthroscopy. 1995;11(6):672–676. [DOI] [PubMed] [Google Scholar]
- 52. Singisetti K, Hinsche A. Shoulder ultrasonography versus arthroscopy for the detection of rotator cuff tears: analysis of errors. J Orthop Surg (Hong Kong). 2011;19(1):76–79. [DOI] [PubMed] [Google Scholar]
- 53. Sipola P, Niemitukia L, Kröger H, Höfling I, Väätäinen U. Detection and quantification of rotator cuff tears with ultrasonography and magnetic resonance imaging---a prospective study in 77 consecutive patients with a surgical reference. Ultrasound Med Biol. 2010;36(12):1981–1989. [DOI] [PubMed] [Google Scholar]
- 54. Skendzel JG, Jacobson JA, Carpenter JE, Miller BS. Long head of biceps brachii tendon evaluation: accuracy of preoperative ultrasound. AJR Am J Roentgenol. 2011;197(4):942–948. [DOI] [PubMed] [Google Scholar]
- 55. Tashjian RZ. Epidemiology, natural history, and indications for treatment of rotator cuff tears. Clin Sports Med. 2012;31(4):589–604. [DOI] [PubMed] [Google Scholar]
- 56. Teefey SA, Middleton WD, Yamaguchi K. Shoulder sonography: state of the art. Radiol Clin North Am. 1999;37(4):767–785. [DOI] [PubMed] [Google Scholar]
- 57. Ward JRN, Lotfi N, Dias RG, McBride TJ. Diagnostic difficulties in the radiological assessment of subscapularis tears. J Orthop. 2018;15(1):99–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Whiting PF, Rutjes AW, Westwood ME, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155(8):529–536. [DOI] [PubMed] [Google Scholar]
- 59. Yamamoto A, Takagishi K, Osawa T, et al. Prevalence and risk factors of a rotator cuff tear in the general population. J Shoulder Elbow Surg. 2010;19(1):116–120. [DOI] [PubMed] [Google Scholar]
- 60. Yeranosian MG, Terrell RD, Wang JC, McAllister DR, Petrigliano FA. The costs associated with the evaluation of rotator cuff tears before surgical repair. J Shoulder Elbow Surg. 2013;22(12):1662–1666. [DOI] [PubMed] [Google Scholar]