Abstract
Continuity of care (COC) has been associated with lower mortality and hospitalizations and higher high blood pressure (HBP) control rates. This evidence mainly came from high income countries. We aimed to identify conditions associated with controlled HBP, particularly COC, in primary care services (PCSs) affiliated to two health insurances in Colombia, a low-median income country. A longitudinal observational study was carried out using clinical records of hypertensive adults >18 years with ≥4 clinic visits attending a contributive and a subsidized PCS in Cali (Colombia) between 2013 and 2014. Subsidized PCSs were for unemployment people and those at low socio-economic position and contributive for formal workers. COC was measured using the Bice and Boxerman index. Logistic regression models were performed to quantify the relation between COC and controlled HBP (blood pressure <140/90 mmHg). Between 2013 and 2014, among 8797 hypertensive people identified, 1358 were included: 935 (68.8%) and 423 (31.1%) from the contributive and subsidized PCSs, respectively. 856 (62.3%) were women and had a mean age of 67.7 years (SD 11.7). All people were on antihypertensive treatment. Over the study period, 522 (38.4%) people had controlled HBP, 410 (43.9%) in the contributive and 112 (26.5%) in subsidized PCSs. An increase in 1 unit of the COC index is associated with a 161% higher probability of having HBP controlled (OR, 2.61; 95% CI, 1.25–5.44). The odds of having controlled HBP increased as the number of visits rose; for example, people at the fourth visit had a 34% (OR, 1.34; 95% CI, 1.08–1.66) higher probability of reaching the target. Continuity of care was positively associated with controlled HBP. The strengthening of COC can improve the observed low HBP control rates and reduce health inequalities.
Keywords: hypertension, primary health care, continuity of patient care, Colombia
Introduction
High blood pressure (HBP) is the global leading cardiovascular risk factor. Worldwide, in 2017, HBP accounted for 10.4 million deaths mainly due to ischemic heart disease, hemorrhagic stroke, and ischemic stroke. 1 For adults ≥18 years of age, in 2015, the world standardized prevalence of HBP, blood pressure (BP) ≥140/90 mmHg, was 24.1% for men and 20.1% for women. 2 In Colombia, a low-middle income country (LMIC), the global prevalence of HBP estimated by the National Health Survey in 2007 was 22.8%, 3 and for those aged 60 years and older, the 2015 SABE survey reported a prevalence of 51.4% for men and 57.7% for women. 4
Lowering BP is directly correlated with reductions in HPB-related cardiovascular mortality and morbidity. 5 Although the percentage of people with controlled HBP (BP < 140/90 mmHg) has reached a level of 50% or more in high-income countries (HICs), the control of HBP in LMICs is still far from being acceptable, with percentages below 20%.6,7 In 2014, the High Cost Account (HCA), a national register of people with chronic conditions like HBP, revealed that among 2,827,129 people with HBP, 56.3% had controlled HBP using a target of BP<150/90 mmHg BP for those aged 60 years and older and BP <140/90 mmHg for the younger. 8 By contrast, in a sample of Colombian hypertensive people, the PURE study revealed that only 37.1% of those on antihypertensive treatment had BP <140/90 mmHg. 9
The control of HBP in people mainly relies on primary care services (PCSs) 10 ; therefore, access to and the performance of PCSs are determinant factors to improve the control of HBP.11-14 An essential attribute of PCS performance is the continuity of care (COC) defining as receiving repeated health care from the same physician. Patients form a beneficial therapeutic relationship if treated by the same doctor over time leading to better patient satisfaction, more patient-centered interventions, and also increase in positive health outcomes. 15 The COC has been associated with achieving controlled HBP and lowering both cardiovascular mortality and visits to emergency services. 16 Some evidence has shown that COC reduced between 2% and 25% the risk of hospitalization17,18 and increased the likelihood of achieving of blood pressure control targets and also the quality of life of hypertensive people.19,20 The associations have been consistent despite of differences between health systems across the world,16,17 although the impact may vary regarding PCS coverage and performance. 21
In Colombia, primary health care is mainly provided through two health insurance plans, contributive and subsidized. Unemployed people and those in the lowest socio-economic position are covered by the subsidized plan while formal workers, individuals with capacity to pay, and their dependents are covered with the contributive plan. A small percentage of the population receives healthcare from special plans. 22 The contributive is a private plan mainly financed by workers and employs contributions, and the subsidized is funded by the government means of general taxes. The special plans covered army forces, university teachers, and workers from the National Company for Oil Exploration (ECOPETROL). 23 For all health plans, a national regulation to provide healthcare for people with HBP was established in 2000, 24 and the first Colombian national clinical guidelines for the management of HBP were launched in 2013. 25 The national guideline defines HBP as having systolic blood pressure (SBP) ≥140 mmHg and/or diastolic blood pressure (DBP) ≥ 90 mmHg for adults ≥18 years of age and controlled HBP as BP below 140/90 mmHg for hypertensive people.24,25 Some reports have shown differences in health outcomes between health insurances. For example, older people from the contributive system used preventive measures more frequently than those from subsidized system in the 2015 SABE survey.26,27 Therefore, we aimed to identify conditions associated with achieving controlled HBP, particularly COC among hypertensive individuals attending two PCSs affiliated to contributive and subsidized plans in Cali, the third largest city of Colombia.
Methods
This is a retrospective longitudinal analysis of hypertensive people attending two PCSs belonged to the subsidized and contributive plans in Cali (Colombia) between 2013 and 2014. Ethical approval was obtained from ethical committees at both PCSs and the University of Valle with the number 06-014 in 2014.
The subsidized PCS was located in the East Cali and provided healthcare to people living nearby; nearly 67% belonged to low socio-economic status in 2014. 28 The contributive PCS was at southeast of Cali and provided healthcare to affiliates regardless of their residential zone. Both PCSs provide healthcare to hypertensive people based on the national regulations 24 ; and the contributive PCSs also added a family physician, as a team leader, and a program addressing renal protection.
In brief, the national guidelines established that for all hypertensive patients, the health providers should offer two annual medical visits with a general physician; the measurement of lipids, kidney function, and glycemia and electrocardiogram at the diagnosis; and access to first line antihypertensive medications without audit. Over the follow-up, the number of medical visits and the laboratory tests depended on the cardiovascular risk with at least one annual check by internal medicine specialist. The clinical checks can be carried out by professional and/or assistant nurses for those at low cardiovascular risk and controlled HBP. Hypertensive people at high cardiovascular risk and/or with comorbidities should be sent to internal medicine specialist at least three times a year.24,25
Study Population
We included individuals >18 years of age with HBP registered with one of the following codes from the International Classification of Diseases (ICD v. 10): I10X, I11.0, I11.9, I12.0, I12.9, I13.0, I13.1, I13.2, I13.9, I15.0, I15.1, I15.2, I15.8, or I15.9 29 and had more than four visits with general practitioner between January 1, 2013 and December 31, 2014 in the database provided by each PCS. A 50% of controlled HBP rate was expected according to the 2014 National Kidney Chronic Disease report. 8 We estimated the total number of people needed to identify factors associated with controlled HBP considering an odds ratio (OR) of 1.2 30 leading to a sample of 1351 people who were distributed into one-third for the subsidized and two-thirds for contributive PCSs according to the population registered with each PCS.
Data Extraction
Each PCS provided the database of people with HBP attending between January 1, 2013, and December 31, 2014. For each individual, a minimum of 4 and a maximum of 6 registers were included as the national guide established a minimum of 2 clinical visits per year for hypertensive people. 24 Data from all medical visits were included for those who had 4, 5, and 6 medical visits. For those with more than 6 medical visits, we ran an algorithm to randomly select the medical visits from which the data were extracted. Data were extracted chronologically from the PCS records following the calendar date. Information from the initial and the last medical visit identified over the study period was always extracted. A maximum of 6 visits was included for each patient, as it reflected the national guideline for the follow-up of individuals with hypertension. The administrative unit at each PCS provided the registers and the dataset of hypertensive patients to the researchers.
Variables
The primary outcome was controlled HPB defined as BP <140/90 mmHg registered at any time during the study period.8,25 The covariables were demographic characteristics, physiological variables, HBP-related conditions, non-cardiovascular comorbidities, diabetes, and other cardiovascular risk factors such as obesity as body mass index ≥30, dyslipidemia, and smoking. In both PCSs, all variables were collected from the registers which were filled by the general physician during each medical visit. The socio-economic stratum was adjudicated by the researchers based on the stratum mode of the patient’s neighborhood defined by the Administrative Office of the municipality of Cali. 31 For those with 6 or more clinical visits, the interval time between visits was calculated among the included records. Pregnant women were excluded from the analysis.
Continuity of care (COC) was defined as having been seen by the same physician throughout the included visits during the study period and was estimated based on the index developed by Bice and Boxerman. 32 The COC index was calculated according to the equation (1) where nj is the number of visits to the same physician and n is the total number of visits during the observed period. The expected values of the COC range between 0 when the physician varies at each visit to 1 when the physician did not vary
| (1) |
Statistical Analysis
A descriptive analysis was carried out by calculating percentages for categorical variables and mean and standard deviation for quantitative variables. Two multilevel logistic models were performed to estimate the association between having controlled HBP and independent variables. Thus, a cross-sectional model using the BP recorded at the last visit as the outcome and a longitudinal analysis using all BP measurements in each visit as the outcome, taking each subject as a random effect in the first level, and the PCSs for the second hierarchical level were performed. As the guideline recommended more regular medical visits for those with uncontrolled BP, we considered and analyzed the population by number of visits. The first strata were those with the minimal visits established in the guideline.24,25 Then, the population was divided into 3 groups according to the total number of clinical visits they had registered in the data set provided by each PCS such as those with 4, 5, or 6 visits and more. The control variables added to the model were age, BMI, sex, diabetes, and having any HPB-related condition, such as stroke, heart failure, coronary heart disease, or impaired kidney function. 33 For the longitudinal model, a total of 6.6% of BMI value was inputted from the last identifiable measurement to complete missing data. As aging is associated with limitations in achieving blood pressure targets due to physical changes and medical attitudes to intervene this population, we explore the interaction between age and medical visits over the period. 34 All models were adjusted for the total individual follow-up days and diabetes. Data were analyzed using STATA (version 14 2014, StataCorp LP).
Results
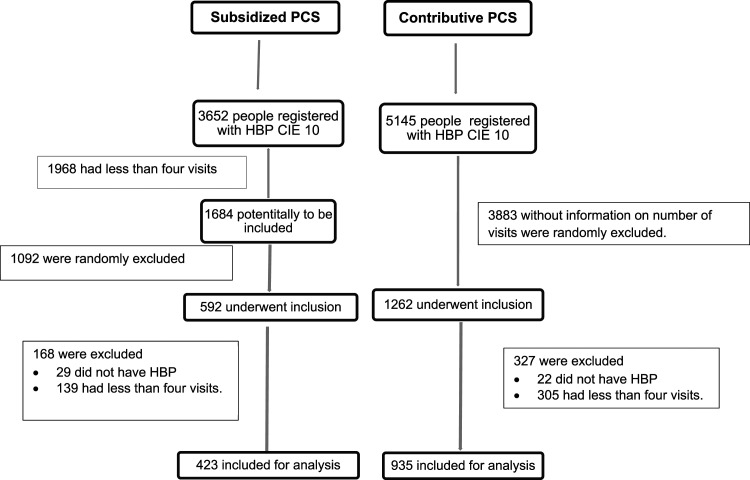
Between 2013 and 2014, we identified 3652 people with HBP among 22,456 attendances at the subsidized PCS. A total of 1968 (53.8%) with less than 4 medical visits were excluded. After, we randomly selected 592 (35.1%) people according to the sample size estimation. Then, we excluded 168 (28%) people, based on inclusion criteria, leaving 423 (72%) people for the analysis. Among 5145 registered people with diagnosis of HBP from the contributive PCS, we randomly excluded 2744 (53.3%), as the initial dataset did not contain information about the number of clinic visits per individual. From the remaining 1262 people, we excluded 327 (25.9%) based on inclusion criteria, leaving 935 (75%) for the analysis (see Figure 1).
Figure 1.
Flow diagram of the selection of included population.
The included population had a mean age of 67.7 (SD 11.7) years, and 856 (62.3%) were women. Those from the subsidized PCS were slightly older than people from the contributive PCS with a mean age of 68.5 (SD 11.9) and 67.4 (SD 11.6), respectively. All people receiving care in the subsidized PCS were at low socio-economic status compared with only 30.9% in the contributive PCS. People from the contributive PCS had more clinic visits than those in the subsidized PCS, and globally, those with BP ≥140/90 mmHg had lower length between medical visits over the period (see Table 1).
Table 1.
Characteristics of Included Population, N = 1358.
| Characteristics | Contributive PCS N = 935 | Subsidized PCS N = 423 | ||
|---|---|---|---|---|
| <60 years | ≥60 years | <60 years | ≥60 years | |
| Age (years) (SD) a | 52.6 (6.7) | 71.8 (8.8) | 52.2 (5.5) | 73.4 (8.2) |
| n (%) | 259 (27.7) | 676 (73.2) | 114 (25.9) | 309 (73.1) |
| Female, N (%) | 148 (69.2) | 386 (53.5) | 80 (80.0) | 232 (71.8) |
| Male, N (%) | 66 (30.8) | 335 (46.5) | 20 (20.0) | 91 (28.2) |
| Socio-economic strata, N (%) | ||||
| Low | 75 (35.0) | 214 (29.7) | 100 (100.0) | 322 (99.7) |
| Middle | 130 (60.7) | 470 (65.2) | 0 (.0) | 0 (.0) |
| High | 7 (3.3) | 15 (2.1) | 0 (.0) | 0 (.0) |
| Unknown | 2 (.9) | 22 (3.1) | 0 (.0) | 1 (.3) |
| Baseline clinic characteristic | ||||
| Number of people by total number of included visits N (%) | ||||
| Four visits | 38 (17.8) | 62 (8.6) | 51 (51.0) | 117 (36.2) |
| Five visits | 40 (18.7) | 104 (14.4) | 23 (23.0 | 85 (26.3) |
| Six visits | 136 (63.6) | 555 (77.0) | 26 (26.0) | 121 (37.5) |
| Mean time between visits in days (SD) a | ||||
| Four visits | 89.27 (39.69) | 103.35 (39.56) | 111.84 (29.49) | 119.76 (27.07) |
| Five visits | 89.70 (25.04) | 98.12 (27.97) | 104.44 (17.18) | 102.08 (23.31) |
| Six visits | 94.88 (19.29) | 97.89 (15.71) | 92.98 (10.84) | 93.00 (15.49) |
| Mean time between visits in days (SD) a | ||||
| Blood pressure ≥140/90 mmHg | 85.14 (28.99) | 91.18 (28.18) | 103.90 (26.21) | 103.51 (25.17) |
| Four visits | 69.56 (40.72) | 97.86 (54.36) | 108.46 (30.36) | 116.92 (28.15) |
| Five visits | 75.08 (28.97) | 72.48 (33.81) | 98.73 (19.40) | 100.59 (22.63) |
| Six visits b | 92.83 (21.81) | 93.18 (20.15) | 93.56 (10.95) | 93.80 (18.60) |
| Blood pressure <140/90 mmHg | 98.54 (20.54) | 99.97 (18.24) | 106.10 (24.64) | 104.79 (24.89) |
| Four visits | 98.54 (20.54) | 99.97 (18.24) | 106.10 (24.64) | 104.79 (24.89) |
| Five visits | 102.95 (34.81) | 103.25 (34.31) | 115.12 (30.54) | 120.11 (25.93) |
| Six visits b | 97.98 (16.55) | 98.67 (14.28) | 93.94 (9.88) | 92.00 (13.91) |
| Blood pressure <140/90 mmHg, N (%) a | 186 (71.81) | 502 (74.26) | 80 (70.18) | 193 (62.46) |
aAt baseline.
bThe interval time was measured between selected records. See text.
Among the included population, 72% (n =1036) did not have any HBP-related condition. Impaired kidney function (IKF) was the most common HBP-related condition, with 143 (10.5%) individuals, followed by chronic peripheral arterial disease (91; 6.7%), coronary heart disease (86; 6.3%), stroke (64; 4.7%), and heart failure (51; 3.7%). A higher proportion of men suffered from HBP-related diseases compared with women in both PCSs; however, a higher proportion of women in the subsidized were found with these conditions than that in the contributive PCS. Similarly, people with IKF were more frequently identified among those visiting the subsidized PCS than those from the contributive PCS. In both PCSs, people aged 60 years and older were more likely to have HBP-related conditions (see Table 2).
Table 2.
Clinical Characteristics of the Population, n = 1358.
| Clinical characteristics | Contributive PCS, n = 935 | Subsidized PCS, n = 423 | ||||||
|---|---|---|---|---|---|---|---|---|
| HBP-related chronic diseases | Male | Female | Male | Female | ||||
| <60 years | ≥60 years | <60 years | ≥60 years | <60 years | ≥60 years | <60 years | ≥60 years | |
| Coronary heart disease (N-%) | 4 (6.1) | 36 (10.8) | 2 (1.4) | 18 (4.7) | 2 (10.0) | 4 (4.4) | 1 (1.3) | 19 (8.2) |
| Stroke (N-%) | 2 (3.0) | 20 (5.9) | 3 (2.0) | 18 (4.7) | 1 (5.0) | 3 (3.3) | 3 (3.8) | 14 (6.0) |
| Heart failure (N- %) | 1 (1.5) | 13 (3.9) | 2 (1.4) | 8 (2.1) | 1 (5.0) | 6 (6.6) | 2 (2.5) | 18 (7.8) |
| Chronic peripheral artery disease (N-%) | 5 (7.7) | 48 (14.3) | 1 (.7) | 16 (4.2) | 0 (0) | 0 (0) | 2 (2.5) | 19 (8.2) |
| Impaired kidney function (N-%) | 5 (7.7) | 59 (17.6) | 4 (2.7) | 20 (5.2) | 2 (10.0) | 27 (29.7) | 2 (2.5) | 24 (10.3) |
| Cardiovascular risk factors | ||||||||
| Diabetes mellitus (N-%) | 34 (51.5) | 217 (64.8) | 48 (32.4) | 154 (39.9) | 5 (25.0) | 39 (42.9) | 35 (43.8) | 109 (46.9) |
| Dyslipidemia (N-%) | 52 (80.0) | 273 (81.5) | 110 (74.3) | 327 (84.9) | 14 (70.0) | 57 (62.6) | 50 (62.5) | 146 (62.9) |
| Obesity (N-%) a | 28 (43.1) | 111 (33.1) | 70 (47.3) | 143 (37.1) | 8 (40.0) | 4 (4.4) | 49 (61.3) | 25 (10.8) |
| Body mass index mean (SD) | 29.5 (5.16) | 27.3 (4.65) | 28.79 (5.66) | 26.97 (4.72) | ||||
| Smoking (N-%) | 5 (7.7) | 12 (3.6) | 3 (2.0) | 6 (1.6) | 0 (.0) | 6 (6.6) | 4 (5.0) | 11 (4.7) |
| Chronic diseases non-related to HBP | ||||||||
| Thyroid diseases (N-%) | 2 (3.1) | 72 (21.5) | 22 (14.9) | 109 (28.3) | 3 (15.0) | 7 (7.7) | 7 (8.8) | 39 (16.8) |
| COPD (N-%) | 0 (.0) | 19 (5.7) | 0 (.0) | 8 (2.1) | 0 (.0) | 5 (5.5) | 2 (2.5) | 14 (6.0) |
Note. COPD = chronic obstructive pulmonary Disease; HBP = high blood pressure; SD = standard deviation.
aBMI ≥ 30.
For 144 (11.4%) people, we did not identify any of the 4 cardiovascular risk factors analyzed. Dyslipidemia was the most common cardiovascular risk factor in both PCSs. A higher proportion of people with dyslipidemia, obesity, and diabetes were found in the contributive PCS compared to the subsidized PCS. In contrast, smoking was the most common cardiovascular risk factor reported in those from the subsidized PCS. In both PCSs, dyslipidemia and diabetes were more commonly found in older people, but smoking and obesity were more common in younger people. Men exhibited more cardiovascular risk factors than women, except for obesity (see Table 2).
Between 2013 and 2014, we recorded data from 6, 5, and 4 clinic visits for 838 (61.7%), 252 (18.5%), and 268 (19.7%) hypertensive people, respectively. While 691 (73.9%) people from the contributive PCS had 6 clinic visits, only 147 (34.8%) from the subsidized PCS had that number of visits. Over the study period, regardless of the total visits recorded, the proportion of people with controlled HBP was higher in the contributive (46.6%) as compared with the subsidized PCS (33.3%). Similarly, the frequency of clinic visits with the same physician was higher in the contributive PCS than it was in the subsidized PCS, COC .27 vs .10. Almost 100% of patients were on antihypertensive treatment in both PCSs. There were no differences in being on antihypertensive treatment between older (≥60 years) and younger (<60 years) patients, between sexes, or among those diagnosed with any HBP-related conditions (Table 3).
Table 3.
Performance of Services for Hypertensive People, N = 1358.
| Contributive PCS, N = 935 | Subsidized PCS, N = 453 | |||||
|---|---|---|---|---|---|---|
| People with 4 visits | People with 5 visits | People with 6 visits | People with 4 visits | People with 5 visits | People with 6 visits | |
| Number of people in each category (N-%) | 100 (10.7) | 144 (15.4) | 691 (73.9) | 168 (39.7) | 108 (25.5) | 147 (34.8) |
| People on antihypertensive treatment (N-%) | 100 (100.0) | 144 (100.0) | 691 (100.0) | 168 (100.0) | 107 (99.1) | 147 (100.0) |
| People with blood pressure <140/90 mmHg in the last visit (N-%) | 83 (83.0) | 126 (87.5) | 595 (86.1) | 119 (70.8) | 77 (72.0) | 110 (74.8) |
| People with blood pressure <140/90 mmHg over the study period (N-%) | 52 (51.49) | 76 (53.15) | 308 (44.57) | 68 (40.48) | 37 (34.26) | 36 (24.49) |
| Time between first and last visit | ||||||
| Median (days) 25%—75% quartile | 424 (273–519) | 495 (403.5–580) | 608 (550v650) | 461 (393–550) | 544 (451–590.5) | 570 (518–617) |
| Continuity of Care Index (COC) | ||||||
| Median (range) | .17 (.00–1.00) | .30 (.00–1.00) | .26 (.07–.67) | .17 (.00–.17) | .10 (.00–.30 | .07 (.00–.27) |
| Global median (10%–90% quartiles) | .27 (.07–.67) | .10 (.00–.27) | ||||
Note. N = number; % = percentage.
The odds of controlled HBP decreased 5% for every increase in one unit of BMI (odds ratio [OR], .95; 95% confidence interval [CI], .92Table 2).98) using the last BP as an outcome. Identical results were observed if all BP measures were used (OR, .96; 95% CI .94–.98). Similarly, for every year increase in age, the odds of having controlled HBP dropped by 2% (OR, .98; 95% CI .97–.99) though this association became slightly weaker in the longitudinal model (OR, 1.00; 95% CI .98–1.01). Additionally, having any HBP-related condition was associated with lower odds of having controlled HBP over the study period (OR, .77; 95% CI .61–.99), but this effect was not identified in the cross-sectional model. There was no significant association between sex and the probability of having controlled HBP. Table 4
Table 4.
Conditions Associated with Blood Pressure Below 140/90 mmHg, N = 1321 a .
| Characteristics | Having blood pressure <140/90 mmHg | |||
|---|---|---|---|---|
| Cross-sectional analysisb,c | Longitudinal analysisb,d | |||
| Odds ratio b [CI] e | P value | Odds ratio b [CI] e | P value | |
| Individual | ||||
| Age f | .98 (95% CI .97–.99) | .042 | 1.00 (95% CI .98–1.01) | .998 |
| Sex | 1.07 (95% CI .77–1.49) | .662 | .94 (95% CI .76–1.18) | .642 |
| BMI | .95 (95% CI .92–.98) | .003 | .96 (95% CI .94–.98) | .001 |
| Having any related HBP condition g | .98 (95% CI .69–1.40) | .948 | .77 (95% CI .61–.99) | .044 |
| Primary care performance | ||||
| Continuity of care | ||||
| COC | 2.61 (95% CI 1.25–5.44) | .010 | NA | |
| Being attended by the same physician at the next clinic visit | 1.52 (95% 1.28–1.80) | <.001 | ||
| Patients-visit group h | ||||
| Five visits | 1.27 (95% .79–2.03) | .318 | NA | |
| Six visits | 1.32 (95% .85–2.05) | .207 | NA | |
| People at each chronological visit recorded i | ||||
| Second visit | NA | 1.12 (95% .91–1.39) | .260 | |
| Third visit | NA | 1.17 (95% .94–1.44) | .141 | |
| Fourth visit | NA | 1.34 (95% CI 1.08–1.66) | .006 | |
| Fifth visit | NA | 1.50 (95% CI 1.18–1.89) | .001 | |
| Sixth visit | NA | 2.25 (95% CI 1.71–2.96) | <.001 | |
| Interaction effect | ||||
| Clinic visit in chronological order b age | NA | |||
| Second visit | NA | .99 (95% CI .98–1.01) | .904 | |
| Third visit | NA | .98 (95% CI .97–1.00) | .231 | |
| Fourth visit | NA | .99 (95% CI .97–1.01) | .588 | |
| Fifth visit | NA | .98 (95% CI .97–1.00) | .290 | |
| Sixth visit | NA | .97 (95% CI .95–.99) | .027 | |
| Total days between the first and the last clinic register over the study period i | 1.00 (95% CI .99-1.00) | .587 | 1.001 (95% CI 1.000–1.002) | <.001 |
| Diabetes | .95 (95% CI .76-1.20) | .684 | 1.010 (95% CI .822–1.240) | .928 |
Note. N = number
aOnly people with all variables with valid values. Body mass index (BMI)
bAdjusted for diabetes.
cOutcome recorded from the last visit
dOutcome recorded over the study period.
eCI:Confidence interval
fCentered age = 67.9 years
gHaving at least one of the following HBP-related conditions: heart failure, coronary heart disease, impaired kidney function, or stroke
hPeople were classified by the total of number visits included as: those with 4, 5, or 6 registers.
iFor everyone, the first and last register corresponded to the first and last medical visit identified chronologically during the study period
An increase in 1 unit in the COC results in almost 3-fold higher odds of having HBP controlled (OR, 2.61; 95% CI, 1.25–5.44). Similarly, the probability of controlled HBP increased by 52% (OR, 1.52; 95% CI, 1.28–1.80) at each visit with the same physician in the longitudinal model. Then, those who received healthcare by the same physician were more likely to have controlled HBP. The odds of having controlled HBP increased as the number of visits rose; for example, people at the fourth visit had a 34% (OR, 1.34; 95% CI, 1.08–1.66) higher probability of reaching the target, compared to those at the first visit. However, there was an interaction effect between each clinical visit and age. For every year increase in age, there was no variation in the probability of having HBP controlled across the clinic visits. Also, for those at the sixth clinic visit, a one-year increase in age reduced the probability of control by 3% (OR, .97; 95% CI, .95–.99) compared to those at the first clinic visit registered. For the cross-sectional analysis, there was no difference in the risk of having controlled HBP between those with 5 or 6 clinic visits compared to those with 4 clinic visits. A positive association between increases in the total of follow-up days and controlled HBP was found in the longitudinal model (see Table 4).
Discussion
In this analysis of hypertensive people being regularly treated in the Colombian contributive and subsidized PCSs, we found that hypertensive people were mainly women aged 60 years and over; individuals attending the subsidized PCS were at lower socio-economic status than those at the contributive PCS. Over the study period, 38.4% of hypertensive people had controlled HBP, 46.6% at the contributive and 33.3% at the subsidized PCSs. Better COC scores were associated with higher odds of having controlled HBP over the period. The probability of reaching the BP target also increased at each visit, but this effect was modified by age.
Despite of being under equal regulations, the percentages of hypertensive people with controlled HBP were 46.6% and 33.3% for the contributive and subsidized PCSs, respectively, over the study period. Similarly, the PURE study, which analyzed a sample of hypertensive people from twelve Colombian states, reported that people at lowest income and with lower education had poor control rates in comparison with those in opposite categories, 14% vs 22%. 9 The subsidized insurance is for those at lower socio-economic conditions. 22 The 2015 SABE survey also found that among people aged 60 years and older, the rate of controlled HBP was 44% and 54% in those in the subsidized and the contributive insurance, respectively. 4 There has been reported that people in the subsidized insurance are less likely to use preventive services and claim medicines.27,35,36 These data may reflect that access barriers to medicines and other interventions in the subsidized insurance could account for the lower blood pressure control rates in this population.
We confirmed the positive association between the COC and having controlled HBP and reduction in hypertension related-diseases mortality and morbidity.13,16 For each visit at which people were treated by the same physician, the probability of being in control increased almost 3-fold. Consistently, the COC has been associated with lower mortality rates and better HBP control across different health systems.16,37 Studies from the USA, the United Kingdom, France, and China have found that those who had been attended by the same general practitioner had up to 34% higher probability of achieving the BP target. 37 Noteworthy, a lower COC index was identified in the subsidized in relation to contributive PCS which could also explain the lower blood pressure targets in the former. Additionally, the median COC for those with 6 visits was lower compared with data reported in countries like Korea and China with .77 and .74, respectively,13,14 so the analyzed PCSs have space to improve their performance. From the patient’s perspective, familiarity, empathy, and trust in the general practitioner are mechanisms that explained the COC. And, the increasing knowledge about the patients, empathy, and stronger responsibility are GP conditions which support the pathways of COC. 15 In addition to this, in Colombia, the GPs are assigned to the called primary care programs for chronic diseases for long periods of time at PCSs which could contribute to the positive observed association.
We selected a sample of hypertensive people who met the minimal follow-up for people with HBP established in the national guidelines. Among the selected sample, people at the contributive insurance had more regular checkups than those at the subsidized insurance. Also, the lengths between visits were lower for those with BP ≥140/90 at the first visit. The integration of family physicians into the HBP program could contribute to strength the follow-up and then the achievement of HBP control targets. Family physicians providing clinical orientation and preventive strategies have been resulted in higher control rates and reduction in cardiovascular hypertension-related mortality.12,38 The program at the contributive PCS has also included a strategy focused on renal kidney prevention which includes a nephrologist consultant providing orientations to the primary group. Consistently, the integration between consultants and PCSs has been associated with higher recognition of renal function impairment and the achievement of blood pressure targets. 39 It is noticeable that people were at similar cardiovascular risk in both PCSs and markedly differences in interventions could not be expected.
Finally, the probability of having HBP controlled increased at each contact with the service mainly after the third visit. This result confirmed that the achievement of HBP control demands more than one clinical visit and a constant follow-up. 12 In Chinese people with hypertension, Zuo et al. recently reported that having 4 to 6 appointments over 1 year follow-up increased the probability of achieving BP control by 62% in comparison with having one to three. 40 Similarly, Mahmood et al. found that those adherent to the regular appointments are more likely to have controlled BP. 41 The continuous monitoring offered by community health workers, physicians, pharmacist, or other members of health team integrated into PCSs has resulted in SBP reductions up to 19 mmHg.12,42 Therefore, the European Society of Hypertension guidelines have recommended a monthly follow-up until achieving the BP target. 43 However, the data showed that older people can be less likely to have HBP controlled at the sixth visit. The lack of having received care by the same physician and poor adherence to interventions could account for that finding. Also aging has been associated with poor HBP control even in experimental conditions.44,45
Limitations and Strengths
Few studies have been carried out outside the HIC, so the current analysis added evidence on the positive impact of COC on individual health in LMIC. Leniz J and Gulliford M using data from the Chilean National Health Survey found that COC was neither associated with better HBP control nor with access to hypertensive medications. However, the measurement of COC was based on questions about awareness of general practitioner reported by people with HBP, and only 28% (258) of them were classified as having COC. 21 Our analysis used the Bice and Boxerman index which is a standard measurement to calculate COC. 32 Consistently, the higher the index, the better the health outcomes such as lower hospitalization rates, higher HBP control rates, and quality of life regardless of health system.14,16 Although the COC does not capture the quality of relationship between general practitioner and patient, our data allowed for identifying the general practitioner with a code so we can be confident that COC was accurately measured. Also, we restricted the analysis to those who adhered to the national guidelines in terms of medical visits over a limited period of 2 years. Therefore, we reduced the potential divergence between patient´s reports and data. 46
We found a lower percentage of hypertensive people reaching the BP target (42.8%) over the study period compared to that reported by the HCA, 56.3%. This register used a higher target (BP <150/90 mmHg) for older people which can account for that difference. 8 However, evidence has shown a reduction in cardiovascular mortality particularly stroke in adults over 60 years who attained systolic BP levels between 130 and 140 mm compared to those with higher levels.47,48 Additionally, we found lower HBP control rates in the subsidized than in the contributive insurance. These differences need more exploration because patient adherence and the use of non-pharmacological interventions were not assessed in the current analysis. Also, we used secondary data which are not collected for research purposes. However, our sample was formed with people who have been followed up over 2 years in both PCSs, and only 6.6% of registers had missing value in the BMI variable. Complementary, the sample only included data from those with regular medical visits such as people with more than 4 medical visits over the period because we did not measure patient-adherence. Attending medical appointments regularly has been associated with higher adherence to interventions and better BP control49,50 Finally, the rates of HBP control were consistent to that reported by the PURE and the CARMELA surveys, 37.1% and 30.6%, respectively.9,51
The probability of having BP controlled increased at each medical visit and more significantly after the third visit. The visits were not related with the date of hypertension diagnosis, but most patients were over 60 years so they could have the diagnosis for more than years. Although there are variations in medications recommended by the national guideline, we considered that the higher probability of having HBP controlled after the third visit could also be explained by the COC strengthened by the guideline. Our data showed that all patients were on antihypertensive medication over the study period, and it is known that the reduction in BP levels due to medications is similar regardless of antihypertensive class. 52 An intensification in treatment could be possible, but it is also related to COC.
In conclusion, in 2 PCSs from an LMIC, nearly 40% of hypertensive people have controlled HBP over 2 years of follow-up. The COC and regular visits to the PCSs increased the probability of achieving the HBP target. The strengthening of the follow-up for hypertensive patients regardless of insurance plan can improve the current HPB control rates. Moreover, increasing COC has the potential of reducing inequalities in health outcomes.
Acknowledgments
We thank the staff of the contributive and subsidized PCSs for the cooperation with the project. Professor Diego Iván Lucumí Cuesta for giving us comments on the manuscript.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The funding for this project came from the University of Valle with the internal number 1749 May 2014.
ORCID iDs
Lena Barrera https://orcid.org/0000-0001-9179-7796
Diego Tovar https://orcid.org/0000-0003-3490-9899
References
- 1.Stanaway JD, Afshin A, Gakidou E, et al. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet (London, England). 2018;392(10159):1923-1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhou B, Bentham J, Cesare MD, et al. Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19·1 million participants. Lancet (London, England). 2017;389(10064):37-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ministerio de Salud y Protección Social de Colombia . Encuesta Nacional de Salud. Ministerio de Salud y Protección Social de Colombia. https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/VS/ED/GCFI/ENCUESTA%20NACIONAL.pdf (2007). [Google Scholar]
- 4.Barrera L, Gómez F, Ortega D, Corhuelo J, Méndez F. Prevalence, awareness, treatment and control of high blood pressure in the elderly according to the ethnic group. Colombian survey. Colomb Méd. 2019;50(2):115-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xie X, Atkins E, Lv J, et al. Effects of intensive blood pressure lowering on cardiovascular and renal outcomes: updated systematic review and meta-analysis. Lancet. 2016;387(10017):435-443. [DOI] [PubMed] [Google Scholar]
- 6.Mills KT, Bundy JD, Kelly TN, et al. Global disparities of hypertension prevalence and control. Circulation. 2016;134(6):441-450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cifkova R, Fodor G, Wohlfahrt P. Changes in hypertension prevalence, awareness, treatment, and control in high-, middle-, and low-income countries: an update. Curr Hypertens Rep. 2016;18(8):62. [DOI] [PubMed] [Google Scholar]
- 8.Fondo Colombiano de Enfermedades de Alto Costo . Situación de la Enfermedad Renal Crónica en Colombia 2014. https://cuentadealtocosto.org/site/images/Publicaciones/Situacion%20de%20la%20ERC%20Colombia%202014.pdf. [Google Scholar]
- 9.Camacho PA, Gomez-Arbelaez D, Molina DI, et al. Social disparities explain differences in hypertension prevalence, detection and control in Colombia. J Hypertens. 2016;34(12):2344-2352. [DOI] [PubMed] [Google Scholar]
- 10.World Health Organization . Global Action Plan for the Prevention and Control of NCDs 2013-2020; 2013. [Google Scholar]
- 11.Macinko J, Leventhal DGP, Lima-Costa MF. Primary care and the hypertension care continuum in Brazil. J Ambul Care Manag. 2018;41(1):34-46. [DOI] [PubMed] [Google Scholar]
- 12.Mills KT, Obst KM, Shen W, et al. Comparative effectiveness of implementation strategies for blood pressure control in hypertensive patients. Ann Intern Med. 2018;168(2):110-120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shin DW, Cho J, Yang HK, et al. Impact of continuity of care on mortality and health care costs: a nationwide cohort study in Korea. Ann Fam Med. 2014;12(6):534-541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Leleu H, Minvielle E. Relationship between longitudinal continuity of primary care and likelihood of death: analysis of national insurance data. PLoS One. 2013;8(8):e71669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sidaway-Lee K, Pereira Gray OBE D, Harding A, Evans P. What mechanisms could link GP relational continuity to patient outcomes? Br J Gen Pract. 2021;71(707):278-281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pereira Gray DJ, Sidaway-Lee K, White E, Thorne A, Evans PH. Continuity of care with doctors-a matter of life and death? A systematic review of continuity of care and mortality. BMJ Open. 2018;8(6):e021161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kao YH, Lin WT, Chen WH, Wu SC, Tseng TS. Continuity of outpatient care and avoidable hospitalization: a systematic review. Am J Manag Care. 2019;25(4):e126-e34. [PubMed] [Google Scholar]
- 18.Nyweide DJ, Anthony DL, Bynum JPW, et al. Continuity of care and the risk of preventable hospitalization in older adults. JAMA Intern Med. 2013;173(20):1879-1885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ye T, Sun X, Tang W, Miao Y, Zhang Y, Zhang L. Effect of continuity of care on health-related quality of life in adult patients with hypertension: a cohort study in China. BMC Health Serv Res. 2016;16(1):674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Khanam MA, Kitsos A, Stankovich J, et al. Association of continuity of care with blood pressure control in patients with chronic kidney disease and hypertension. Aust J Gen Pract. 2019;48:300-306. [DOI] [PubMed] [Google Scholar]
- 21.Leniz J, Gulliford MC. Continuity of care and delivery of diabetes and hypertensive care among regular users of primary care services in Chile: a cross-sectional study. BMJ Open. 2019;9(10):e027830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.OECD . OECD Reviews of Health Systems: Colombia 2016. Paris, France: OECD Publishing; 2015. http://www.oecd.org/countries/colombia/oecd-reviews-of-health-systems-colombia-2015-9789264248908-en.htm. [Google Scholar]
- 23.World Health Organization . Primary Health Care Systems (PRIMASYS): Case Study from Colombia. Geneva, Switzerland: World Health Organization; 2017. [Google Scholar]
- 24.Ministerio de Salud y Protección Social de Colombia . Resolución 412 del 25 de febrero 2000 Por la cual se establecen las actividades, procedimientos eintervenciones de demanda inducida y obligatorio cumplimiento y se adoptan las normas técnicas y guías de atención para el desarrollo de las acciones de protección especifica y detección temprana y la atención de enfermedades de interés en salud publica. 2000. [Google Scholar]
- 25.Ministerio de Salud y Proteción Social de Colombia . Guía de práctica clínica. Hipertensión arterial primaria. Ministerio de Salud y Protección Social de Colombia 2013. https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/INEC/IETS/GPC_Completa_HTA.pdf. [Google Scholar]
- 26.Garcia-Ramirez J, Nikoloski Z, Mossialos E. Inequality in healthcare use among older people in Colombia. Int J Equity Health. 2020;19(1):168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Garcia-Subirats I, Vargas Lorenzo I, Mogollón-Pérez AS, et al. Determinantes del uso de distintos niveles asistenciales en el sistema general de seguridad social en salud y sistema único de salud en Colombia y Brasil. Gac Sanit. 2014;28(6):480-488. [DOI] [PubMed] [Google Scholar]
- 28.Secretaria de Salud Municipal . Plan Territorial de Salud de Cali. 2012-2015. Cali, Colombia: Municipal SdSP, Alcaldía de Cali. http://calisaludable.cali.gov.co/proyectos/Informes_Plan_Territorial_de_Salud_2012/pts_cali_2012_2015.pdf (2012). [Google Scholar]
- 29.World Health Organization . International Classification of Diseases for Diseases and Related Health Problems Geneva1990. http://apps.who.int/classifications/icd10/browse/2016/en#/IX. [Google Scholar]
- 30.Demidenko E. Sample size determination for logistic regression revisited. Stat Med. 2007;26(18):3385-3397. [DOI] [PubMed] [Google Scholar]
- 31.Cali Ad. Estratificación Socio-Económica Urbana Por Comunas en Cali año 2015 2015. http://datos.cali.gov.co/dataset/estratificacion-socioeconomica-urbana-por-comunas-en-cali-ano-2015. [Google Scholar]
- 32.Bice TW, Boxerman SB. A quantitative measure of continuity of care. Medical Care. 1977;15(4):347-349. [DOI] [PubMed] [Google Scholar]
- 33.Sverre E, Peersen K, Otterstad JE, et al. Optimal blood pressure control after coronary events: the challenge remains. Am J Hyperten. 2017;11(12):823-830. [DOI] [PubMed] [Google Scholar]
- 34.Benetos A, Petrovic M, Strandberg T. Hypertension management in older and frail older patients. Circ Res. 2019;124(7):1045-1060. [DOI] [PubMed] [Google Scholar]
- 35.Garcia-Subirats I, Vargas I, Mogollón-Pérez AS, et al. Barriers in access to healthcare in countries with different health systems. A cross-sectional study in municipalities of central Colombia and north-eastern Brazil. Soc Sci Med. 2014;106:204-213. [DOI] [PubMed] [Google Scholar]
- 36.Ramírez Hassan A, Cardona Jiménez J, Cadavid Montoya R. The impact of subsidized health insurance on the poor in Colombia: evaluating the case of Medellín. Econ Apl. 2013;17:543-556. [Google Scholar]
- 37.Howard DL, Carson AP, Holmes DN, Kaufman JS. Consistency of care and blood pressure control among elderly African Americans and whites with hypertension. J Am Board Fam Med. 2009;22(3):307-315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rasella D, Harhay MO, Pamponet ML, Aquino R, Barreto ML. Impact of primary health care on mortality from heart and cerebrovascular diseases in Brazil: a nationwide analysis of longitudinal data. BMJ (Clinical research ed.). 2014;349:g4014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.van Dipten C, van Berkel S, van Gelder VA, et al. Adherence to chronic kidney disease guidelines in primary care patients is associated with comorbidity. Fam Pract. 2017;34(4):459-466. [DOI] [PubMed] [Google Scholar]
- 40.Zuo H-J, Ma J-X, Wang J-W, Chen X-R, Hou L. The impact of routine follow-up with health care teams on blood pressure control among patients with hypertension. J Hum Hypertens. 2019;33(6):466-474. [DOI] [PubMed] [Google Scholar]
- 41.Mahmood S, Jalal Z, Hadi MA, Shah KU. Association between attendance at outpatient follow-up appointments and blood pressure control among patients with hypertension. BMC Cardiovasc Disord. 2020;20(1):458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.He J, Irazola V, Mills KT, et al. Effect of a community health worker-led multicomponent intervention on blood pressure control in low-income patients in Argentina. J Am Med Assoc. 2017;318(11):1016-1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Williams B, Mancia G, Spiering W, et al. [2018 ESC/ESH Guidelines for the management of arterial hypertension. The task force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH)]. Giorn Ital Cardiol. 2018;19(33):3S-73S. [DOI] [PubMed] [Google Scholar]
- 44.Asche SE, O'Connor P, Dehmer SP, et al. Patient characteristics associated with greater blood pressure control in a randomized trial of home blood pressure telemonitoring and pharmacist management. Am J Hyperten. 2016;10(11):873-880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Turner BJ, Parish-Johnson JA, Liang Y, Jeffers T, Arismendez SV, Poursani R. Implementation of the chronic care model to reduce disparities in hypertension control: benefits take time. J Gen Intern Med. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nyweide DJ. Concordance between continuity of care reported by patients and measured from administrative data. Med Care Res Rev. 2014;71(2):138-155. [DOI] [PubMed] [Google Scholar]
- 47.Moraes AAI, Baena CP, Muka T, et al. Achieved systolic blood pressure in older people: a systematic review and meta-analysis. BMC Geriatr. 2017;17(1):279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Author Anonymous. Final report of a trial of intensive versus standard blood-pressure control. N Engl J Med. 2021;384(20):1921-1930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Karter AJ, Parker MM, Moffet HH, et al. Missed appointments and poor glycemic control. Medical Care. 2004;42(2):110-115. [DOI] [PubMed] [Google Scholar]
- 50.Shahaj O, Denneny D, Schwappach A, et al. Supporting self-management for people with hypertension. J Hypertens. 2019;37(2):264-279. [DOI] [PubMed] [Google Scholar]
- 51.Hernández-Hernández R, Silva H, Velasco M, et al. Hypertension in seven Latin American cities: the cardiovascular risk factor multiple evaluation in Latin America (CARMELA) study. J Hypertens. 2010;28(1):24-34. [DOI] [PubMed] [Google Scholar]
- 52.Law MR, Wald NJ, Morris JK, Jordan RE. Value of low dose combination treatment with blood pressure lowering drugs: analysis of 354 randomised trials. BMJ. 2003;326(7404):1427. [DOI] [PMC free article] [PubMed] [Google Scholar]