Summary
Europeans are not only exposed to direct effects from climate change, but also vulnerable to indirect effects from infectious disease, many of which are climate sensitive, which is of concern because of their epidemic potential. Climatic conditions have facilitated vector-borne disease outbreaks like chikungunya, dengue, and West Nile fever and have contributed to a geographic range expansion of tick vectors that transmit Lyme disease and tick-borne encephalitis. Extreme precipitation events have caused waterborne outbreaks and longer summer seasons have contributed to increases in foodborne diseases. Under the Green Deal, The European Union aims to support climate change health policy, in order to be better prepared for the next health security threat, particularly in the aftermath of the traumatic COVID-19 experience. To bolster this policy process we discuss climate change-related hazards, exposures and vulnerabilities to infectious disease and describe observed impacts, projected risks, with policy entry points for adaptation to reduce these risks or avoid them altogether.
1. Introduction
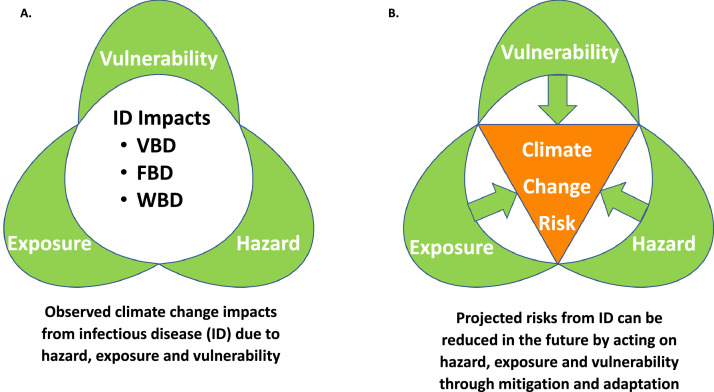
Despite the COVID-19 pandemic, according to the World Health Organization (WHO) climate change may be the defining global public health threat of the 21st century1 since it is threatening all aspects of human society including risks to human health2. Increasingly, a growing number of infectious health outcomes are associated with climate change that are inequitably distributed within and between European countries. Weather parameters contribute in a nonlinear way to infectious disease transmission3 and have been shown to be one of the key drivers of the emergence, re-emergence, and spread of infectious disease4,5. Moreover, they contribute to the survival, reproduction and distribution of disease pathogens and vectors, as well as to their transmission and geographical patterns6. While the climatic suitability for transmission may decrease in certain areas7, it may increase in others for a number of infectious diseases8. However, infectious disease impacts from climate change are not only a function of these climate hazards but also of other hazards such as pathogens or vectors (Box 1). Moreover, health impacts also depend on exposure patterns in human populations and underlying vulnerabilities (Fig. 1; Box 1). Climate change impacts result in fact from dynamic interactions between hazard, exposure and vulnerability. The complexity of the nexus of these three elements of climate change impacts was recognized in the new European Union (EU) Strategy on Adaptation9 to climate change which was adopted in February 2021 by The European Commission. The cornerstone of the strategy is to improve the knowledgebase of climate impacts and adaptation solutions by stepping up adaptation planning and climate risk assessments, by accelerating adaptation action, and by helping to strengthen climate resilience globally. Thus, the purpose of this paper is to review the observed health impacts and projected risks from infectious disease in Europe that can be attributed to climate, from the synergic perspective of hazard, exposure and vulnerability and their impacts on disease transmission (Fig. 1). Insights from this analysis offer different policy entry points for interventions on infectious disease threats from climate change.
Box 1. Definition of terms: hazard, exposure, vulnerability, impact and risk from climate change.
|
Source: Adapted from IPCC.
Alt-text: Unlabelled box
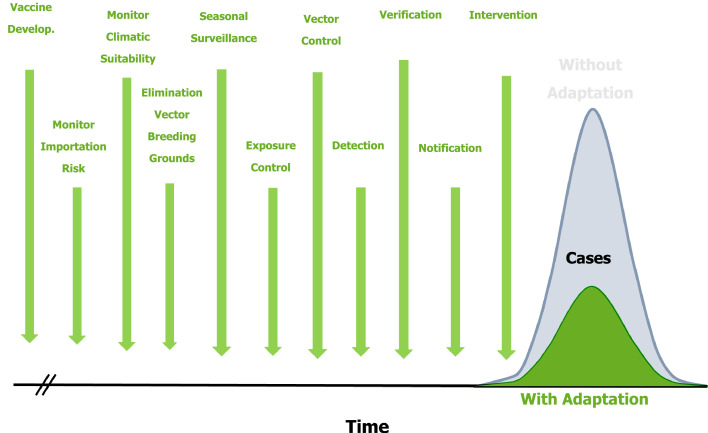
Figure 1.
Climate change impacts on infectious diseases and policy entry points for reducing climate change risks from hazards, exposure and vulnerability.
Note: ID: infectious disease; VBD: vector-borne disease; WBD: water-borne disease; FBD: food-borne disease.
2. Climate change in Europe – the current situation
Europe is experiencing a warming trend with more frequent hot spells, longer and warmer summers, and an increase in the frequency, duration and severity of heat waves (Table 1). Water availability has also changed due to a decrease in the amount of precipitation in Southern and Eastern Europe and conversely, an increase in the frequency and severity of heavy rainstorms and floods in Northern Europe10, exemplified by the July 2021 record rainfall and associated flooding in Western Europe with over 200 fatalities and highlighted population exposure and vulnerability even in highly developed countries11. In Europe, the warmest year on record was 2020, and all the warmest years were documented during the last decade. The 2019/20 winter is infamous as the warmest recorded winter ever, and 2020 the warmest recorded autumn with a significant heatwave during the summer in the western countries12.
Table 1.
Climate change and infectious diseases; hazard, exposure and vulnerability with options for climate change adaptation in Europe.
| IDs | Hazard | Exposure | Vulnerability | Adaptation option |
|---|---|---|---|---|
| VBD | Increase in ambient temperature; Changes in ecology; Extended seasons of transmission; Improved climatic and environ suitability for transmission; Invasive and indigenous vector species; (Re) emergence of pathogens; Geographic range expansion of vectors and pathogens; Extended seasons of transmission. |
Occupational and residential exposure to vectors; Global mobility; Urbanization; Land use; Geography. |
Lack of safeguards (e.g., repellant, window screens, AC); Insecticide resistance; No vaccine. |
Assure universal access to care and disease management; Improve disease surveillance for VBD; Integrate surveillance of vectors and human health; Horizontal surveillance for emerging threats; Seasonal or sentinel surveillance for selected VBD; Minimize vector exposure (e.g., window/door screens, AC, protective clothing, habitat avoidance, insecticide use) Accelerate vaccine development with new technologies; Health education and community surveillance for early outbreak detection; Monitoring of air passenger volume as epidemic precursor of disease for early warning system; Monitoring of vectorial capacity as a climatic precursor of disease for early warning system; Wetland management and elimination of vector breeding cites in the vicinity of populations; Novel vector control methods (e.g., Wolbachia-infected mosquitoes; biotechnological methods; bait; traps); Cross-border outbreak control measures; Blood bank safety through deferral strategies, screening strategies and triggers and pathogen reduction technologies. |
| WBD | Extreme weather events (storms, droughts, precipitation, floods, wildfires); Increase in ambient temperature; (Re) emergence of pathogens; Increase in sea surface temperature; Extended seasons of transmission. |
Contamination of water treatment and distribution systems; Exposure to flood water contaminated with pathogens. |
Lack of flood barriers and catchment areas; Aging water infrastructure (leaking pipes); Drought; Settlement in flood plain. | Assure universal access to care and disease management; Improve disease surveillance for WBD; Monitor recreational water, alerts and beach closures; Upgrade water catchment, storage, treatment and distribution systems to sustain extreme weather event; Protect critical infrastructure from floods, storms and sea level rise; Limit water overuse to protect aquafer; Household water purification systems; Community-based participation in water harvesting and storage; Monitor forecasts for sea surface temperature or precipitation for early warning system; Drinking water catchment management. |
| FBD | Extreme weather events (storms, droughts, precipitation, floods, wildfires); (Re) emergence of pathogens; Increase in ambient temperature; Extended seasons of transmission. |
Food preparation and storage; food contamination. |
Lack of food safety regulations; Breakdown of cold chain; Suboptimal processing, preparation, transport, storage, packaging, wrapping, exposure for sale, service, or delivery of food. | Assure universal access to care and disease management; Improve disease surveillance for FBD; Health education and promotion for food preparation and storage in a warmer climate; Infection control of livestock (e.g., salmonella vaccine for poultry; window screens on chicken coops to prevent campylobacter infection); Improve eating habits; Better food processes and storage procedures (e.g., cold chains, conservation); Monitor of climatic conditions to prevent crop damage from droughts or floods as part of early warning system. |
Note: ID: infectious disease; VBD: vector-borne disease; WBD: water-borne disease; FBD: food-borne disease.
3. Impact of the changing climate on infectious disease in Europe
Nearly two‐thirds of European human and domestic animal pathogens are climate sensitive13. Some of them cause the most significant diseases, based on morbidity and mortality, which might therefore also be affected by climate change6,14.
Here we review the most updated scientific evidence on observed health impacts and projected risks from climate change for infectious disease in Europe and examine adaptation options for infectious disease with opportunities for preparedness and response. Of particular interest were publications since 2017 that examined the specific aims of this study, and assessed the association between climate change and disease transmission in Europe.
3.1. Vector-borne diseases
Vector-borne diseases (VBDs) are mainly transmitted by arthropod vectors such as mosquitoes, which are particularly sensitive to changes in external climatic conditions because they are cold-blooded (ectothermic)15. Habitat suitability determines insect density, distribution and abundance (Table 1). Furthermore, temperature impacts the rate of pathogen maturation and replication in mosquitoes, and increases the likelihood of infection3,16. For diseases transmitted by vectors that have aquatic developmental stages, precipitation also exerts a very strong influence on VBD dynamics in various ways, depending on the differences in the ecology of mosquito vectors17.
Analysis of the underlying drivers of infectious disease threat events detected in Europe during 2008–2013 by epidemic intelligence at the European Centre of Disease Prevention and Control revealed seventeen drivers. The most important drivers of epidemic threat events caused by VBD are the natural environment, followed by climate, travel and tourism4. However, attributing VBD to climate change is complicated by nonlinear feedback loops between population susceptibility and immunity3. Yet, climate is a well-established driver of VBD epidemiology18.
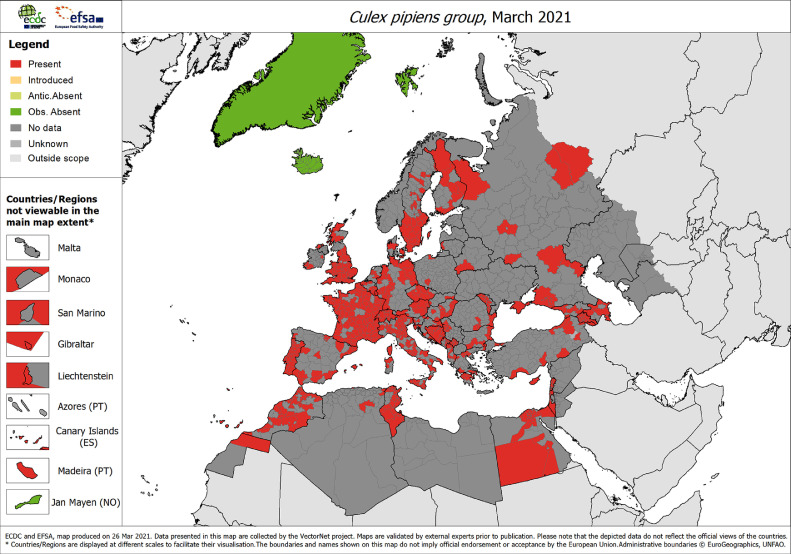
In the EU and European Economic Area (EEA) Member States and EU-neighboring countries there were 336 locally-acquired human cases of West Nile virus (WNV) infections in 2020, 463 cases in 2019, and 2083 cases in 201819. WNV is a major cause of encephalitis. Migratory birds on their flyway from sub-Saharan Africa, North Africa or the Middle East introduce WNV into Europe where the virus overwinters in mosquitoes20. The virus is then transmitted to humans, mainly by mosquito species from the genus Culex (family Culicidae) which are widely distributed in Europe, even in less vulnerable regions as Scandinavia and the United Kingdom (Fig. 2). The early and extensive WNV circulation in Southern and Central Europe in 2018 with over 2000 cases (see above) can be explained, in part, by the very high temperatures in early spring which seems to have activated the mosquito breeding season, reduced the extrinsic incubation period and thereby accelerated virus amplification in the avian and mosquito populations.21 Throughout the last decade, locally-acquired human cases of WNV infections, including deaths, occurred in a number of European countries in the South (e.g. Spain, Italy, Greece) East (e.g. Romania, Bulgaria, Hungary)22 and even North (Germany)23. For the first time, WNV infection was detected in a bird in the Netherlands, which foreshadowed the first detection of human cases in the country in the summer of 202024. The circulation of WNV has steadily expanded over the years to affect new areas in Europe.
Figure 2.
Current known distribution of the Culex pipiens group (Culex pipiens and Culex torrentium) in Europe at ‘regional’ administrative level, as of March 2021.
Source: European Centre for Disease Prevention and Control and European Food Safety Authority. Mosquito maps [internet]. Stockholm: ECDC; 2021. Available from: https://ecdc.europa.eu/en/disease-vectors/surveillance-and-disease-data/mosquito-maps.
High precipitation in late winter/early spring was found as one of the key predictors of WNV outbreaks across Europe25. Conversely, during drought conditions the lack of wetlands concentrates mosquitoes and birds around water bodies, which in turn also favors WNV transmission26. For example, a wet spring followed by drought provided the most likely explanation for the observed increase in WNV activity in Europe in 201827.
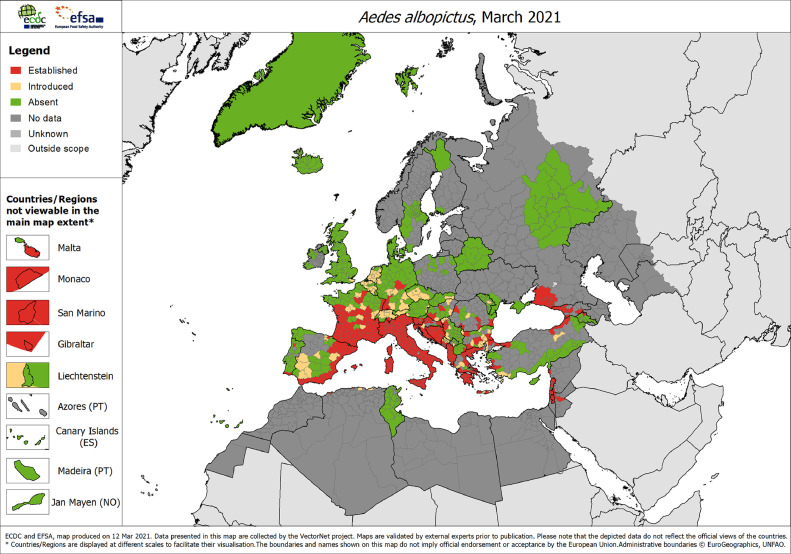
Europe has also been plagued by recurrent autochthonous outbreaks caused by different vectors that have experienced a rapid global expansion due to international mobility: Aedes aegypti and Ae. albopictus mosquitoes. Ae. aegypti is a highly competent vector for tropical diseases like dengue, chikungunya and Zika, that is restricted to warm, urban environments, whereas Ae. albopictus is a moderately competent vector for these pathogens, far more ecologically flexible, and can be found in suburban, rural, residential, and agricultural habitats28. The success of the invasion of Ae. albopictus to new regions is due to a number of ecological and human-caused factors such as its ecological plasticity, increase of trade and travel, and lack of efficient control29. Additionally, studies indicate that climate change exacerbates the risk and burden of Aedes-transmitted viruses28 and allows the introduction of events into new regions30. Based on present-day climatic conditions, there is a current potential distribution of Ae. albopictus in Europe, mainly in its southern regions30. This is comparable with the current known distribution of the vector, which has experienced a steady expansion, reaching Northern France and parts of Germany (Fig. 3)6. Indeed, a potential risk for cases of chikungunya, Zika and dengue already exists in the south-western regions29,31.
Figure 3.
Current known distribution of Aedes albopictus in Europe at ‘regional’ administrative level, as of March 2021. Source: European Centre for Disease Prevention and Control and European Food Safety Authority. Mosquito maps [internet]. Stockholm: ECDC; 2021. Available from: https://ecdc.europa.eu/en/disease-vectors/surveillance-and-disease-data/mosquito-maps
In 2007, Europe was struck for the first time by a large outbreak of 330 chikungunya cases in Italy, which raised public health concerns32. Two smaller outbreaks of autochthonous cases of chikungunya were reported in France in 2010 and 201429. Furthermore, a decade after the first outbreak in Italy, a large outbreak of 489 cases occurred during the climatically suitable season33.
During recent years, sporadic autochthonous cases of dengue were reported in southern countries, for example in Catalonia, Spain, in France in September 2019, and in France and Italy in summer 2020. Here again, cases of dengue are expected in the southern regions in the summer and autumn due to the presence of the vector and the introduction of dengue and/or chikungunya viruses by travel-associated cases returning from epidemic/endemic countries29.
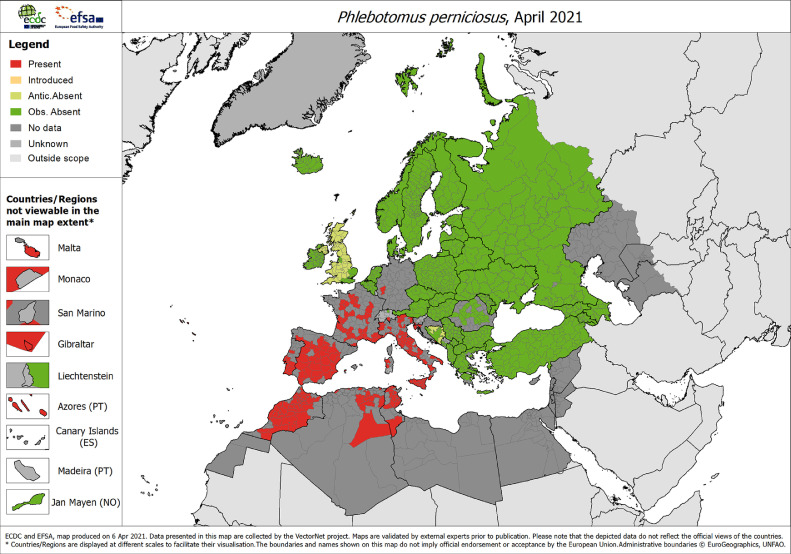
Leishmaniasis is a vector-borne disease caused by protozoa of the genus Leishmania predominantly but not exclusively confined to tropical and sub-tropical regions. It manifests itself in different forms in humans, including cutaneous leishmaniasis which causes skin lesions. In Europe, the disease burden is relatively low due to antiretroviral therapies but Leishmania spreads by the bite of infected sandflies with the primary vectors being Phlebotomus spp., present around the Mediterranean but also further North in France and Germany (Fig. 4). Leishmaniasis has been associated with exposure in poor living conditions and climate change which are, at present, rapidly exacerbating conditions that attract sand flies and leishmaniasis towards temperate regions34. Life parameters of sand flies depend mainly on temperature and, to a certain extent, on humidity. A vector population dynamic model from Greece, Cyprus and Turkey, indicated that temperature, changes in breeding habitats and in land use, do have also a strong impact on sand fly abundance35.
Figure 4.
Current known distribution of Phlebotomus perniciosus in Europe at ‘regional’ administrative level, as of April 2021. P. perniciosus one of the predominant L. infantum vectors in Europe. Source: European Centre for Disease Prevention and Control and European Food Safety Authority. Phlebotomine sandflies maps [internet]. Stockholm: ECDC; 2021. Available from: https://ecdc.europa.eu/en/disease-vectors/surveillance-and-disease-data/phlebotomine-maps
Ixodes ticks can transmit bacteria from the genus Borrelia (causing Lyme disease), which is the most prevalent tick-transmitted infection in temperate areas of Europe. They also transmit the virus that causes several thousand cases per year in the EU/EEA of tick‐borne encephalitis (TBE) which can result in severe neurological sequelae in up to 10% of patients. The geographic distribution of Ixodes ricinus, the most common arthropod vector of human disease in Europe, is related to climatic factors such as humidity, soil water, and air temperature, as well as to vegetation type, land use, and disturbance36. Studies found that I. ricinus has shifted its seasonal activity and geographical range both on latitudinal and elevation limits as a result of the increasing temperatures37. This shift and increase in activity is related to milder winters and prolonged spring and autumn seasons in the 1990s, combined with other factors such as increased vegetative cover16,38.
3.2. Food-borne diseases
The transmission pathway of food-borne pathogens from farm to fork is complex. Many of the pathogens that cause food-borne diseases (FBD) are able to persist in the environment, can sustain heat stress, and are infective at a low dose. Of those, Campylobacter is the most common bacterial cause of diarrhoeal disease in developed countries and with over 220,000 cases per year and a notification rate of 60 cases per 100,000 population. It is the most commonly reported cause of human bacterial gastroenteritis throughout the EU/EEA39. It shows a strong association with seasonality and climate variability, mainly with increased temperatures that may increase bacterial contamination at various points along the food chain40,41 (Table 1). Since Campylobacter cannot replicate outside of the host, hot ambient conditions may actually influence people's behavior, rather than replication rates which, in turn, may be translated into more risky patterns of food consumption42,43 (Table 1). A study on Campylobacter infections in England and Wales found that the increase of infections in the late spring was significantly linked to the temperature two weeks earlier. Since the relationship with temperature was not linear, it seems that the association is likely to be indirect44 and might be due to other seasonal factors such as fly transmission45 (Table 1). A study in the Nordic countries shows that the temporal and geographical distribution of Campylobacter can be associated with increases in temperature and heavy rainfall, that may increase the number of cases reported in the following week. Conversely, heat waves and winter precipitation may decrease the number of cases reported42.
With over 87,000 cases per year in the EU/EEA, salmonellosis is the second most commonly reported gastrointestinal infection in humans after campylobacteriosis, and a significant cause of food-borne outbreaks39. Salmonella is climate sensitive and grows in a narrow temperature envelope with more frequent infections in the summer months40 (Table 1). The incidence of human Salmonella infections (20.0 cases per 100,000 population) is higher in the summer period than in the winter period and thus highly seasonal. Studies show an increase in weekly temperatures is followed by an upsurge in incidence which indicates that warm weather accelerates Salmonella reproduction43,46.
3.3. Water-borne diseases
Climate change alters the continuous circulation of water on earth in unpredictable ways (Table 1). Severe weather events, flooding, storm surges, and droughts are all manifestations of the hydrological cycle gone awry47. As opposed to gradual changes in climate, abrupt and sudden changes are even more challenging for public health practice41. An extreme precipitation episode can trigger a causal chain of secondary events with unexpected consequences. Such a cascading risk pathway can have a ripple effect and damage critical infrastructure41 (Table 1). Cascading risks depend on existing vulnerabilities in society that get exacerbated by climate change48. For example, a heavy rain event can flush animal pathogens from pastures into waterways and overwhelm ageing water treatment and distributions systems, which can result in waterborne outbreaks40,49 (Table 1). An alternate urban transmission pathway of a water-borne disease (WBD) triggered by extreme weather events, characterized by warm/extremely warm and wet/extremely wet has been associated with a peak in incidence of human leptospirosis, a highly infectious, emerging water-borne zoonosis, caused by Leptospira interrogans50. As part of a systematic literature review of infectious disease following a natural disaster in Europe, eight studies described cascading risk pathways with outbreaks following flooding, four of which were caused by leptospirosis51.
The increase in global ambient temperature leads to elevated sea surface temperature which accelerates the replication of pathogenic Vibrio bacteria in marine waters. Anthropogenic climate change drives the emergence of Vibrio infections in the Baltic, which is associated with morbidity and mortality among recreational water users52.
4. Climate change scenarios and projected risk for infectious disease in Europe
Different scenarios for Europe predict that temperature will continue to rise and exacerbate the duration, frequency and intensity of heat waves53. Differential temperature increases are expected in Northwest Europe and Scandinavia in the winter and in Southeast and Southern Europe in the summer. Throughout most of Europe, less precipitation during summer along with rising temperatures will result in more frequent and intense summer droughts, exacerbating water scarcity. Conversely, heavy rainstorms and flash floods such as in July 2021 in Western Europe11, are projected to become more frequent10,54 .
Consequently, there is growing concern that higher temperatures and changes in precipitation patterns will affect the transmission of some VBD, WBD, and FBD, with increased and decreased projections depending on the affected region and degree of climatic change55. In most cases, increased transmission is predicted but contractions of the geographic distribution can also be expected. While changes in the magnitude and pattern of climate-sensitive health outcomes are likely, if thresholds are crossed, some of the changes could be significant56.
A modelling study of WNV infection spreading in Europe under climate change scenarios predicts that in 2025, progressive expansion of areas with an elevated probability for infections is expected, particularly at the edges of the current transmission. In 2050, an increase in areas with a higher probability of expansion is projected57.
Predictions suggest that Ae. albopictus will continue to be a successful invasive species spreading beyond its current geographical borders (Fig. 3). It is expected to spread broadly, with expanded distributional potential across much of western Europe and the Balkan region30. Yet, some areas are predicted to become less suitable for the species, particularly in Eastern Europe where models indicate increased aridity. Models generally project a moderate climatic suitability for chikungunya transmission, notably across France, Spain, Germany and Italy, with increased suitability in large areas by the Rhine and Rhone rivers. However, some areas by the Italian Adriatic coast are projected to experience a decline in suitability due to the increased probability of summer droughts58.
The climatic suitability for dengue transmission predicted to improve over the next decades, particularly around the Mediterranean and Adriatic coasts and in northern Italy29,59. By the end of the century increasing climatic suitability is predicted to expand into a larger part of Europe60. However, the current lack of a highly competent vector like Ae. Agypti in continental Europe renders the risk for sustained dengue outbreaks low61.
Phlebotomine sandflies, the vectors of Leishmania, have the potential to expand their range (Fig. 4), under future climatically suitable conditions, towards central and northern Europe, reaching the islands of Great Britain and Scandinavia62.
A northward shift in climate suitability for tick species from their current distribution is predicted for the coming decades63. Future scenarios indicate a potential further expansion of I. ricinus in northern and eastern Europe, resulting from milder winter conditions and extended spring and fall seasons. Such changes will enable more ticks to survive the winter, and increase the probability of tick bites16,38.
The changing climate may impact food-borne diseases as well. According to a recent study, an overall increase in campylobacteriosis of almost 200% is estimated for the Scandinavian countries by the end of the century42. This means nearly 6,000 excess campylobacter cases per year which could potentially be attributed to an extension of the transmission season and other chances to the climate. Temperature-related incidence of salmonella is also projected to increase in Europe under climate change scenarios but can be offset by public health mitigation strategies43.
5. Climate change adaptation to infectious disease in Europe
Climate change risks from infectious disease can be reduced by acting on hazards, exposure and vulnerability (Fig. 1; Table 1, Box 1). As a result of the changing climate, health systems need to be prepared for gradual and abrupt changes in health outcomes and potential new conditions, including additional threats from infectious disease transmission. The need to prevent and reduce the severity of current and future climate change impacts in Europe (Fig. 1) highlights the necessity to develop systematic policies of vector and infectious disease control programs, health action plans, adaptation strategies and resilience measures, based on the typical regional risk factors and population health needs64. A number of the adaptation options for infectious disease in Europe is part of traditional public health practice (Table 1). Regrettably, many of the infectious disease control measures have been neglected during the epidemiologic transition, but have now received renewed attention during the COVID-19 pandemic. While the core capacities in public health of the WHO International Health Regulations (IHR) have been proven to be effective to control infectious disease threat events in Europe in general48,65, but they certainly did not prove to be sufficient to contain the explosive epidemic of COVID-19 . Moreover, a number of interesting developments in the field of infectious disease control have emerged that lend themselves for the management of climate-sensitive infectious disease (Table 1). One of the most exciting new developments is the acceleration of vaccine development and the application of new technologies such as the joint BioNTech-Pfizer COVID-19 mRNA vaccine (BNT162b2) for SARS-CoV266 (Fig. 5). These new technologies have proven to be a game-changer of the COVID-19 response that can now also be applied to climate-sensitive infectious disease48.
Figure 5.
Climate change adaptation options for vector-borne diseases in Europe. Note: Time scale is relative. Source: Adapted from: Semenza JC. Cascading risks of waterborne diseases from climate change. Nature Immunol 2020;21(5):484-487.
5.1. Adaptation to VBD in Europe
The risk from VBD such as dengue or chikungunya in Europe, can be dissected into two phases: the risk for importation of the pathogens by viremic passengers arriving from endemic countries into Europe where a competent vector is present; and the risk for onwards transmission and dispersion of these pathogens to susceptible individuals by local mosquitoes, which is a function of the climatic suitability for transmission and population exposure during population movement (Fig. 5). This process was examined during the 2017 Chikungunya outbreak in France and Italy, by using flight passenger data33. These indicators highlighted the areas at risk for importation both from endemic countries but also from the outbreak zones in southeastern France and central Italy to other areas in Europe. Subsequently, the seasonal vectorial capacity of Aedes albopictus mosquitoes was computed to estimate the risk to transmit chikungunya virus. The vectorial capacity estimates can elucidate the local climatic suitability for mosquito borne outbreaks. Moreover, repeated geo-located Twitter feeds from Twitter Streaming Application Programming Interface (API) can provide information on unidirectional population mobility from the epicentre of the epidemic to other areas at risk that need to be targeted for interventions. The use of near–real-time geocoded Twitter data can help to quantify human ground movement and disentangle connectivity between outbreak hotspots33. Thus, the application of big data and analyses can be applied in real time to respond quickly to climate-sensitive infectious disease (Fig. 5; Table 1). In these areas at risk, mosquito breeding sites need to be eliminated to reduce mosquito density and seasonal surveillance should be conducted for both mosquitoes and human health to identify sentinel cases. It was demonstrated that window screens and air conditioning can substantially reduce bite intensity based on survey data from mainland France67 and by extension, exposure to infected mosquitoes (Fig. 5; Table 1). Insecticides, larvicides, and repellents can be used for vector control to minimize exposure in human populations but in case of detection, verification and notification other intervention measures should be initiated (Fig. 5; Table 1). For example, WNV outbreaks pose a threat to blood banks and the supply of safe blood products and increases the risk to the safety of blood transfusion57. Risk reduction interventions should include deferral strategies, screening strategies and triggers and also pathogen reduction technologies68 (Table 1).
5.2. Adaption to WBD in Europe
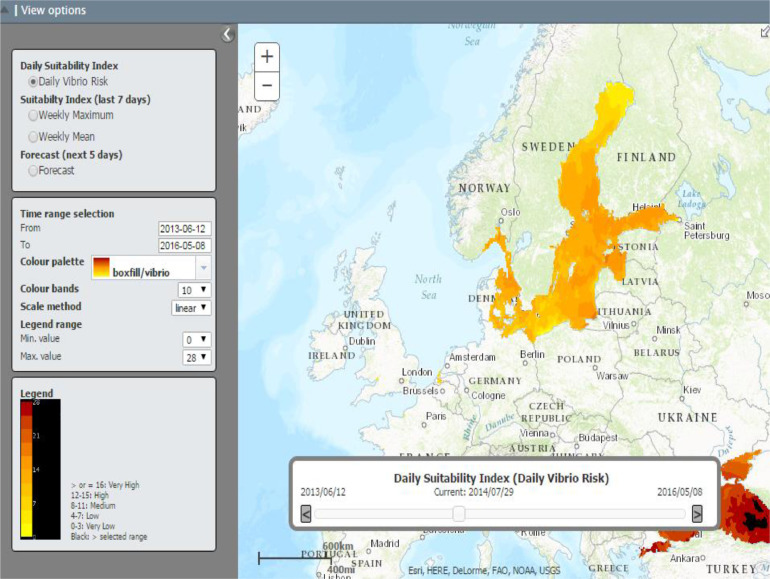
The risk from WBD is compounded by cascading climate events that trigger a sequence of secondary events that cause disruption of natural or human systems.41 For example, extended periods of excessive precipitation can saturate soils and mobilize pathogens from fields and pastures and flush them into water treatment and distribution systems which can result in waterborne outbreaks. Such a vulnerability calls for upgrading ageing water catchment, storage, treatment and distribution infrastructure and repairing leaking pipes (Table 1). Critical infrastructure needs to be protected from floods, storms and sea level rise. Adaptation interventions to contain cascading risk pathways entails also forecasting meteorological conditions predictive of climate-sensitive infectious disease emergence (Table 1). An early warning system of atmospheric forecasts can predict heavy rain events or an increase in sea surface temperature in marine waters. Monitoring sea surface temperature and salinity in real time remotely can predict the environmental suitability of pathogenic Vibrio infections in marine waters52. Such a system has been operationalized at the European Centre for Disease Prevention and Control and is in use with weekly alerts to state epidemiologists during hot summer months (Fig. 6). Beach closures, alerts to the public and notifications to health care providers can minimize the exposure of recreational water users to such marine bacteria (Table 1).
Figure 6.
ECDC Vibrio Map Viewer: environmental suitability for Vibrio spp., July 2014, Baltic Sea. Source: https://e3geoportal.ecdc.europa.eu/SitePages/Vibrio%20Map%20Viewer.aspx.
5.3. Adaption to FBD in Europe
Foodborne outbreaks have been associated with farming practices, food processing, handling, and storage that are all sensitive to climatic conditions. Outbreaks have been associated with contamination of drinking and irrigation water and along the food chain (from farm to fork) if the cold chain breaks down69. Thus, adaptation options for FWB require farm-level interventions to prevent food contamination, during production, processing, and distribution (Table 1). For example, fly screens as part of biosecurity practices in broiler chicken coops can help reduce prevalence of campylobacteriosis among humans70. However, it also entails public education campaigns for improved eating habits, safe food preparation, and storage in a warmer climate (Table 1). Moreover, the current food system accounts for up to 30% of greenhouse gas emissions which is another incentive to create climate-adapted, agroecological food production (circular agriculture).
6. Conclusions
A number of food- and waterborne diseases are climate-sensitive through direct pathways, while vector-borne diseases are mediated by vectors through indirect pathways. Attributing the contribution of climate change to disease incidence and prevalence is difficult due to other underlying drivers and determinants71. Nevertheless, the magnitude of climate-sensitive disease is considerable, also in Europe, which calls for better adaptation options (Table 1). Therefore, preparedness and response to such health security threats should be based on inter-sectorial collaboration between governmental (e.g., local, regional, national, super national) and non-governmental actors (e.g., community, commerce, faith-based organizations, civil society) and diverse scientific disciplines (e.g., biology, entomology, environment, climatology, social science)48. Epidemiological data should be merged, integrated, and analyzed with climatic, biological, environmental, ecological and demographic data in order to interpret complex disease patterns5,64,72. Predictive modelling of the expected impacts of climate change on disease transmission involving different climate and socioeconomic scenarios is critical in order to develop better early warning systems for disease outbreaks, to help decision-makers understand more precisely where or when infections will emerge or spread52,56.
Under the European Green Deal73, the EU adopted proposals to reduce net greenhouse gas emissions by at least 55% by 2030, compared to 1990 levels. As part of the European Green Deal, the EU Adaptation Strategy9 and EU4Health74, the European Climate and Health Observatory75 was created to provide access to information regarding climate change impacts on human health. Specifically, the Observatory aims to support Europe in preparing for and adapting to climate change impacts through early warning systems, information systems, indicators and tools. This review can guide the Observatory in its mandate, as proposed under the European Green Deal, and direct action towards the three cogs of the wheel: hazard, exposure or vulnerability. Fig. 1 and Table 1 exemplify policy entry points how climate change risk can be reduced by acting on the nexus of hazard, exposure and vulnerability.
Moreover, rising awareness of the potential risks from climate change among scientist from various disciplines, the health community, policymakers and the public is vital but not a given. Strengthening public awareness can be achieved by educational programs using the involvement of the media and community leaders. Health workers should provide useful insights for simplifying scientific knowledge to deliver climate-health messages72. This should include recommended prevention of negative health outcomes, such as elimination of habitats for vectors and prevention of water-borne and food-borne diseases and infections (Table 1). The punishing effect of the COVID-19 pandemic on health and socio-economic wellbeing are a stark reminder of the pitfalls of insufficient preparedness48. The take-home message from the current crisis is that preparedness and response, risk assessment, and early warning systems, along with climate change adaptation are essential in order to mitigate the impacts of the climatic changes on the (re-) emergence of infectious disease and to prevent their negative consequences for population health.
Contributors
Both authors contributed equally to this manuscript.
Data sharing
All resources for the current review appear in the reference list.
Editor disclaimer
The Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
Declaration of interests
The authors declare no competing interests.
Contributor Information
Jan C. Semenza, Email: jan.semenza@gmail.com.
Shlomit Paz, Email: shlomit@geo.haifa.ac.il.
References
- 1.WHO. Coronavirus disease (COVID-19): Climate change. 2020. https://www.who.int/news-room/q-adetail/coronavirus-disease-covid-19-climate-change (Accessed 14 Jan 2020)
- 2.WHO. COP24 Special Report Health and Climate Change. 2018. https://apps.who.int/iris/bitstream/handle/10665/276405/9789241514972-eng.pdf?ua=1 (Accessed 10 Jan 2020)
- 3.Metcalf CJE, Walter KS, Wesolowski A, Buckee CO, Shevliakova E, Tatem AJ. Identifying climate drivers of infectious disease dynamics: recent advances and challenges ahead. P Roy Soc B: Biol Sci. 2017;284(1860) doi: 10.1098/rspb.2017.0901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Semenza JC, Lindgren E, Balkanyi L, Espinosa L, Svendotter M, Penttinen P, Rocklöv J. Determinants and drivers of infectious disease threat events in Europe. Emerg Infect Dis. 2016;22(4):581–589. doi: 10.3201/eid2204.151073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hess J, Boodram LLG, Paz S, Ibarra AMS, Wasserheit JN, Lowe R. Strengthening the global response to climate change and infectious disease threats. BMJ. 2020:371. doi: 10.1136/bmj.m3081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Semenza JC, Suk JE. Vector-borne diseases and climate change: a European perspective. FEMS Microbiol Lett. 2018;365(2):fnx244. doi: 10.1093/femsle/fnx244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Murdock CC, Sternberg ED, Thomas MB. Malaria transmission potential could be reduced with current and future climate change. Sci Rep. 2016;6(1):1–7. doi: 10.1038/srep27771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Watts N, Amann M, Arnell N, Ayeb-Karlsson S, Beagley J, Belesova K. The 2020 report of The Lancet Countdown on health and climate change: responding to converging crises. Lancet. 2021;397(10269):129–170. doi: 10.1016/S0140-6736(20)32290-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.European Commission. EU Adaptation Strategy. 2021. https://ec.europa.eu/clima/sites/clima/files/adaptation/what/docs/eu_strategy_2021.pdf. (Accessed 1 July 2021)
- 10.European Commission. Climate Action - How will we be affected. https://ec.europa.eu/clima/policies/adaptation/how_en (Accessed 15 Jan 2021).
- 11.Germany floods—a global warming warning for extreme intensity of weather events. The Lancet Regional Health – Europe. 2021;7 doi: 10.1016/j.lanepe.2021.100194. Editorial. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.European Commission, Copernicus, ECMWF. 2020 warmest year on record for Europe; globally, 2020 ties with 2016 for warmest year recorded. 2021. https://climate.copernicus.eu/2020-warmest-year-record-europe-globally-2020-ties-2016-warmest-year-recorded (Accessed 1 Feb 2021)
- 13.McIntyre KM, Setzkorn C, Hepworth PJ, Morand S, Morse AP, Baylis M. Systematic assessment of the climate sensitivity of important human and domestic animals pathogens in Europe. Sci Rep. 2017;7(1):1–10. doi: 10.1038/s41598-017-06948-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brugueras S, Fernández-Martínez B, Martínez-de la Puente J, Figuerola J, Porro TM, Rius C. Environmental drivers, climate change and emergent diseases transmitted by mosquitoes and their vectors in southern Europe: A systematic review. Environ Res. 2020 doi: 10.1016/j.envres.2020.110038. [DOI] [PubMed] [Google Scholar]
- 15.Rocklöv J, Dubrow R. Climate change: an enduring challenge for vector-borne disease prevention and control. Nat Immunol. 2020;21(5):479–483. doi: 10.1038/s41590-020-0648-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Caminade C, McIntyre KM, Jones AE. Impact of recent and future climate change on vector-borne diseases. Ann NY Acad Sci. 2019;1436(1):157–173. doi: 10.1111/nyas.13950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Paz S. Effects of climate change on vector-borne diseases: An updated focus on West Nile virus in humans. Emerg Top Life Sci. 2019;3(2):143–152. doi: 10.1042/ETLS20180124. [DOI] [PubMed] [Google Scholar]
- 18.Paz S. Climate change impacts on West Nile virus transmission in a global context. Philos Trans R Soc B Biol Sci. 2015;370(1665) doi: 10.1098/rstb.2013.0561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Historical data by year - West Nile virus seasonal surveillance. https://www.ecdc.europa.eu/en/west-nile-fever/surveillance-and-disease-data/historical
- 20.Rudolf I, Betášova L, Blažejová H, Venclíková K, Straková P, Šebesta O. West Nile virus in overwintering mosquitoes, central Europe. Parasit Vectors. 2017;10(1):452. doi: 10.1186/s13071-017-2399-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Marini G, Calzolari M, Angelini P, Bellini R, Bellini S, Bolzoni L. A quantitative comparison of West Nile virus incidence from 2013 to 2018 in Emilia-Romagna, Italy. PLoS Negl Trop Dis. 2020;14(1):e0007953. doi: 10.1371/journal.pntd.0007953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.ECDC. West Nile virus in Europe in 2020 - infections among humans and outbreaks among equids and/or birds. https://www.ecdc.europa.eu/en/publications-data/west-nile-virus-europe-2020-infections-among-humans-and-outbreaks-among-equids-23 (Accessed 9 Feb 2021).
- 23.Ziegler U, Santos PD, Groschup MH, Hattendorf C, Eiden M, Höper D. West Nile virus epidemic in Germany triggered by epizootic emergence, 2019. Viruses. 2020;12(4):448. doi: 10.3390/v12040448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vlaskamp DR, Thijsen SF, Reimerink J, Hilkens P, Bouvy WH, Bantjes SE. First autochthonous human West Nile virus infections in the Netherlands, July to August 2020. Eurosurveillance. 2020;25(46):1–4. doi: 10.2807/1560-7917.ES.2020.25.46.2001904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Marcantonio M, Rizzoli A, Metz M, Rosa R, Marini G, Chadwick E. Identifying the environmental conditions favouring West Nile Virus outbreaks in Europe. PLoS One. 2015;10(3) doi: 10.1371/journal.pone.0121158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cotar AI, Falcuta E, Prioteasa LF, Dinu S, Ceianu CS, Paz S. Transmission dynamics of the West Nile virus in mosquito vector populations under the influence of weather factors in the Danube Delta. Romania. Ecohealth. 2016;13(4):796–807. doi: 10.1007/s10393-016-1176-y. [DOI] [PubMed] [Google Scholar]
- 27.Haussig JM, Young JJ, Gossner CM. Early start of the West Nile fever transmission season 2018 in Europe. Euro Surveill. 2018;23(32) doi: 10.2807/1560-7917.ES.2018.23.32.1800428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ryan SJ, Carlson CJ, Mordecai EA, Johnson LR. Global expansion and redistribution of Aedes-borne virus transmission risk with climate change. PLoS Neglect Trop D. 2019;13(3) doi: 10.1371/journal.pntd.0007213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lillepold K, Rocklöv J, Liu-Helmersson J, Sewe M, Semenza JC. More arboviral disease outbreaks in continental Europe due to the warming climate? J Travel Med. 2019;26(5):taz017. doi: 10.1093/jtm/taz017. [DOI] [PubMed] [Google Scholar]
- 30.Kamal M, Kenawy MA, Rady MH, Khaled AS, Samy AM. Mapping the global potential distributions of two arboviral vectors Aedes aegypti and Ae. albopictus under changing climate. PloS One. 2018;13(12) doi: 10.1371/journal.pone.0210122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liu Y, Lillepold K, Semenza JC, Tozan Y, Quam MB, Rocklöv J. Reviewing estimates of the basic reproduction number for dengue, Zika and chikungunya across global climate zones. Environ Res. 2020;182 doi: 10.1016/j.envres.2020.109114. [DOI] [PubMed] [Google Scholar]
- 32.Rezza G, Nicoletti L, Angelini R, Romi R, Finarelli AC, Panning M. Infection with chikungunya virus in Italy: an outbreak in a temperate region. Lancet. 2007;370(9602):1840–1846. doi: 10.1016/S0140-6736(07)61779-6. [DOI] [PubMed] [Google Scholar]
- 33.Rocklöv J, Tozan Y, Ramadona A, Sewe MO, Sudre B, Garrido J. Using big data to monitor the introduction and spread of Chikungunya, Europe, 2017. Emerg Infect Dis. 2019;25(6):1041–1049. doi: 10.3201/eid2506.180138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fischer D, Moeller P, Thomas SM, Naucke TJ, Beierkuhnlein C. Combining climatic projections and dispersal ability: a method for estimating the responses of sandfly vector species to climate change. PLoS Negl Trop Dis. 2011;5(11):e1407. doi: 10.1371/journal.pntd.0001407. Gürtler RE, editor. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Erguler K, Pontiki I, Zittis G, Proestos Y, Christodoulou V, Tsirigotakis N. A climate-driven and field data-assimilated population dynamics model of sand flies. Sci Rep. 2019;9(1):1–15. doi: 10.1038/s41598-019-38994-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Estrada-Peña A, Ortega C, Sánchez N, Desimone L, Sudre B, Suk JE, Semenza JC. Correlation of Borrelia burgdorferi sensu lato prevalence in questing Ixodes ricinus ticks with specific abiotic traits in the western palearctic. Appl Environ Microbiol. 2011;77(11):3838–3845. doi: 10.1128/AEM.00067-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Estrada-Peña A, Fernández-Ruiz N. A Retrospective Assessment of temperature trends in Northern Europe reveals a deep impact on the life cycle of Ixodes ricinus (Acari: Ixodidae) Pathogens. 2020;9(5):345. doi: 10.3390/pathogens9050345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Alkishe AA, Peterson AT, Samy AM. Climate change influences on the potential geographic distribution of the disease vector tick Ixodes ricinus. PloS One. 2017;12(12) doi: 10.1371/journal.pone.0189092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.The European Union One Health 2019 Zoonoses Report. https://www.ecdc.europa.eu/en/publications-data/european-union-one-health-2019-zoonoses-report [DOI] [PMC free article] [PubMed]
- 40.Semenza JC, Herbst S, Rechenburg A, Suk JE, Höser C, Schreiber C, Kistemann T. Climate change impact assessment of food- and waterborne diseases. Crit Rev Environ Sci Technol. 2012;42(8):857–890. doi: 10.1080/10643389.2010.534706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Semenza JC. Cascading risks of waterborne diseases from climate change. Nat Immunol. 2020;21(5):484–487. doi: 10.1038/s41590-020-0631-7. [DOI] [PubMed] [Google Scholar]
- 42.Kuhn KG, Nygård KM, Guzman-Herrador B, Sunde LS, Rimhanen-Finne R, Trönnberg L. Campylobacter infections expected to increase due to climate change in Northern. Europe. Sci Rep. 2020;10(1):13874. doi: 10.1038/s41598-020-70593-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lake IR. Food-borne disease and climate change in the United Kingdom. Environ Health. 2017;16(1):53–59. doi: 10.1186/s12940-017-0327-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Djennad A, Lo Iacono G, Sarran C, Lane C, Elson R, Höser C. Seasonality and the effects of weather on Campylobacter infections. BMC Infect Dis. 2019;19(1):255. doi: 10.1186/s12879-019-3840-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nichols GL. Fly transmission of Campylobacter. Emerg Infect Dis. 2005;11(3):361–364. doi: 10.3201/eid1103.040460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cherrie MPC, Nichols G, Iacono GL, Sarran C, Hajat S, Fleming LE. Pathogen seasonality and links with weather in England and Wales: a big data time series analysis. BMC Public Health. 2018;18(1):1067. doi: 10.1186/s12889-018-5931-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Semenza JC. In: Climate Change and Human Health. Luber G, Lemery J, Knowlton K, Sorensen C, editors. Jossey-Bass (Wiley); NJ, US: 2021. Changes in hydrology and its impacts on waterborne disease. Hobokenin press. [Google Scholar]
- 48.Semenza, JC. Lateral public health: advancing systemic resilience to climate change. The Lancet Regional Health – Europe. 10.1016/j.lanepe.2021.100193 (in press). [DOI] [PMC free article] [PubMed]
- 49.Guzman Herrador B, de Blasio BF, Carlander A, Ethelberg S, Hygen HO, Kuusi M. Association between heavy precipitation events and waterborne outbreaks in four Nordic countries, 1992-2012. J Water Health. 2016;14(6):1019–1027. doi: 10.2166/wh.2016.071. [DOI] [PubMed] [Google Scholar]
- 50.Habus J, Persic Z, Spicic S, Vince S, Stritof Z, Milas Z. New trends in human and animal leptospirosis in Croatia, 2009–2014. Acta Trop. 2017;168:1–8. doi: 10.1016/j.actatropica.2017.01.002. [DOI] [PubMed] [Google Scholar]
- 51.Suk JE, Vaughan EC, Cook RG, Semenza JC. Natural disasters and infectious disease in Europe: a literature review to identify cascading risk pathways. Eur J Public Health. 2020;30(5):928–935. doi: 10.1093/eurpub/ckz111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Semenza JC, Trinanes J, Lohr W, Sudre B, Löfdahl M, Martinez-Urtaza J. Environmental suitability of vibrio infections in a warming climate: an early warning system. Environ Health Perspect. 2017;125(10) doi: 10.1289/EHP2198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Martinez GS, Linares C, Ayuso A, Kendrovski V, Boeckmann M, Diaz J. Heat-health action plans in Europe: Challenges ahead and how to tackle them. Environ Res. 2019;176 doi: 10.1016/j.envres.2019.108548. [DOI] [PubMed] [Google Scholar]
- 54.European Environment Agency. Trends and projections in Europe. 2020. https://www.eea.europa.eu/publications/trends-and-projections-in-europe-2020 (Accessed 14 Feb 2021).
- 55.Ebi KL, Hasegawa T, Hayes K, Monaghan A, Paz S, Berry P. Health risks of warming of 1.5°C, 2°C, and higher, above pre-industrial temperatures. Environ Res Lett. 2018;13(6) [Google Scholar]
- 56.Tong S, Ebi K. Preventing and mitigating health risks of climate change. Environ Res. 2019;174:9–13. doi: 10.1016/j.envres.2019.04.012. [DOI] [PubMed] [Google Scholar]
- 57.Semenza JC, Tran A, Espinosa L, Sudre B, Domanovic D, Paz S. Climate change projections of West Nile virus infections in Europe: Implications for blood safety practices. Environ Heal. 2016;15(1):125–136. doi: 10.1186/s12940-016-0105-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Tjaden NB, Suk JE, Fischer D, Thomas SM, Beierkuhnlein C, Semenza JC. Modelling the effects of global climate change on Chikungunya transmission in the 21st century. Sci Rep. 2017;7(1) doi: 10.1038/s41598-017-03566-3. 1-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Rogers DJ, Suk JE, Semenza JC. Using global maps to predict the risk of dengue in Europe. Acta Trop. 2014;129:1–14. doi: 10.1016/j.actatropica.2013.08.008. [DOI] [PubMed] [Google Scholar]
- 60.Bouzid M, Colón-González FJ, Lung T, Lake IR, Hunter PR. Climate change and the emergence of vector-borne diseases in Europe: Case study of dengue fever. BMC Public Health. 2014;14(1):1–12. doi: 10.1186/1471-2458-14-781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Massad E, Amaku M, Coutinho FA, Struchiner CJ, Burattini MN, Khan K. Estimating the probability of dengue virus introduction and secondary autochthonous cases in. Europe. Sci Rep. 2018;8:4629. doi: 10.1038/s41598-018-22590-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Koch LK, Kochmann J, Klimpel S, Cunze S. Modeling the climatic suitability of leishmaniasis vector species in Europe. Scientific Reports. 2017;7(1):1–10. doi: 10.1038/s41598-017-13822-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Williams HW, Cross DE, Crump HL, Drost CJ, Thomas CJ. Climate suitability for European ticks: Assessing species distribution models against null models and projection under AR5 climate. Parasites Vector. 2015;8(1):440. doi: 10.1186/s13071-015-1046-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kendrovski V, Schmoll O. Priorities for protecting health from climate change in the WHO European Region: recent regional activities. Bundesgesundheitsbla. 2019;62(5):537–545. doi: 10.1007/s00103-019-02943-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Semenza JC, Sewe MO, Lindgren E, Brusin S, Aaslav KK, Mollet T, Rocklöv J. Systemic resilience to cross-border infectious disease threat events in Europe. Transbound Emerg Dis. 2019;66(5):1855–1863. doi: 10.1111/tbed.13211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Polack FP, Thomas SJ, Kitchin N, Absalon J, Gurtman A, Lockhart S. Safety and Efficacy of the BNT162b2 mRNA Covid-19 Vaccine. N Engl J Med. 2020;383:2603–2615. doi: 10.1056/NEJMoa2034577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Poinsignon A, Boulanger D, Binetruy F, Elguero E, Darriet F, Gallian P. Risk factors of exposure to Aedes albopictus bites in mainland France using an immunological biomarker. Epidemiol Infect. 2019;147:e238. doi: 10.1017/S0950268819001286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Semenza JC, Domanović D. Blood supply under threat. Nat Clim Chang. 2013;3(5):432–435. [Google Scholar]
- 69.Lake IR, Hooper L, Abdelhamid A, Bentham G, Boxall AB, Draper A. Climate change and food security: health impacts in developed countries. Environ Health Perspect. 2012;120(11):1520–1526. doi: 10.1289/ehp.1104424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Bahrndorff S, Rangstrup-Christensen L, Nordentoft S, Hald B. Foodborne disease prevention and broiler chickens with reduced Campylobacter infection. Emerg Infect Dis. 2013;19(3):425–430. doi: 10.3201/eid1903.111593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Semenza JC, Rocklöv J, Penttinen P, Lindgren E. Observed and projected drivers of emerging infectious diseases in Europe. Ann NY Acad Sci. 2016;1382(1):73–83. doi: 10.1111/nyas.13132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Fox M, Zuidema C, Bauman B, Burke T, Sheehan M. Integrating public health into climate change policy and planning: State of practice update. Int J Env Res Pub He. 2019;16(18):3232. doi: 10.3390/ijerph16183232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.European Commission. A European Green Deal. https://ec.europa.eu/info/strategy/priorities-2019-2024/european-green-deal_en (Accessed 10 July 2021)
- 74.EU4 Health 2021-2027 – a vision for a healthier European Union. https://ec.europa.eu/health/funding/eu4health_en (Accessed 12 July 2021)
- 75.The European Climate and Health Observatory. https://climate-adapt.eea.europa.eu/observatory/About/about-the-observatory/(Accessed 12 July 2021)