Abstract
The coronavirus pandemic has given everyone in society an education on the harms of spread of respiratory illness. Young healthy athletes are far less likely to suffer severe adverse consequences of viral illnesses than the elderly and frail, but they are not completely immune. Chronic fatigue (overtraining) is an uncommon outcome and myocarditis a rare one, but they both warrant due consideration. It is, therefore, a sensible individual strategy to ‘stay home when sick’ if only for these risks. Traditionally though, athletes have tended to push through (train and play when ill) because of competing concerns, such as key events/matches and ‘not wanting to let teammates down’. Data from both low COVID-19 and high COVID-19 countries show that the number of cardiovascular deaths in a society correlates with the number of respiratory deaths at the same time, further linking respiratory viruses to cardiovascular deaths. We are now more aware of public health obligations to prevent the spread of respiratory illnesses, in particular to protect the more vulnerable members the community. This hopefully will correspond with a change in the culture of sport to one where it is considered ‘the right thing to do’, to ‘stay home when sick’.
Keywords: illness, cardiology prevention, respiratory
Key messages.
What is already known
Training or competing in a group when carrying a respiratory viral illness is associated with spread to others (particularly when training indoors).
Heavy exercise when carrying respiratory viral illnesses is also associated with developing overtraining syndrome (chronic fatigue) and—uncommonly—exacerbating myocarditis.
What are the new findings
Data from the COVID-19 pandemic in both high COVID-19 countries and low COVID-19 countries have shown quite a high correlation between respiratory virus circulation (in a community) and risk of cardiovascular death (in the same community).
COVID-19 has reminded us that ‘staying home when sick’ is not only a sensible strategy for individuals, but also is a public health obligation, as respiratory viruses are associated with adverse cardiovascular outcomes.
Prevention of cardiovascular deaths is a critical public health goal. Cardiovascular deaths are the most common category of deaths in middle-aged and elderly people. Randomised controlled trials (RCTs) in recent years have demonstrated that influenza vaccines are potentially able to reduce the risk of cardiovascular events and even deaths in those with known cardiovascular disease.1 Systematic reviews of RCTs have confirmed these findings,2 with the obligatory caveats about study quality needing to temper our confidence in the strength of these findings.3 Real-world simulations resulting from the SARS-CoV-2 (COVID-19) pandemic have added weight to the association between circulating respiratory viruses and overall cardiovascular deaths, which are concentrated in the older age groups.
High correlations between respiratory deaths and cardiovascular deaths
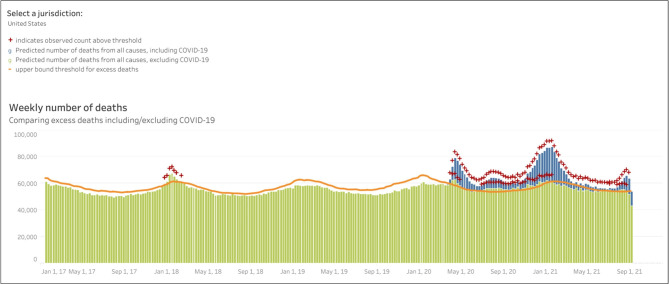
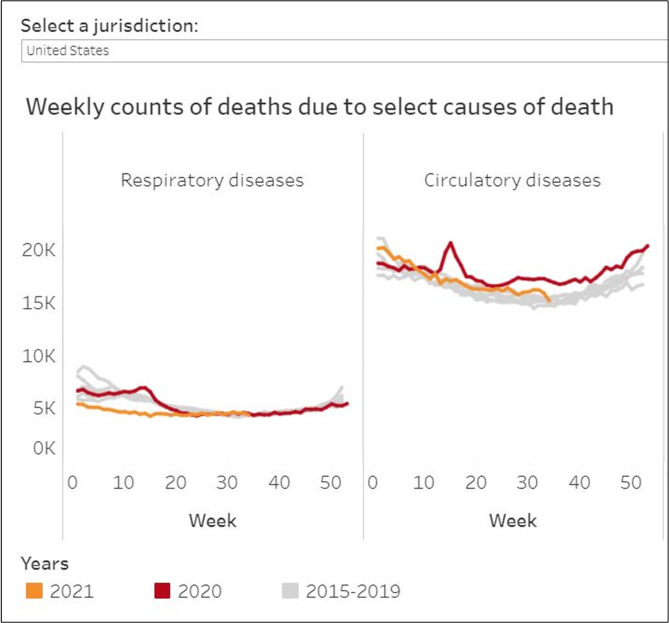
For countries badly affected by the COVID-19 pandemic, such as the USA, the number of ‘excess deaths’ above expected deaths in 2020 was slightly higher than the number of reported deaths from COVID-19 (figure 1). Unofficial rates for excess deaths in many countries are available.4 Detailed analysis of excess deaths recently reported from the USA reveals that as COVID-19 deaths rose, cardiovascular deaths rose in tandem5 (figure 2). While it is possible that there was some misdiagnosis involved, and that there were confounding factors (such as worse cardiovascular outcomes due to fear of hospital presentation), a plausible part of the explanation is that infection with COVID-19 increases the risk of cardiovascular event and death.6 7 Some of these ‘excess’ deaths would have be recorded as coronavirus deaths (if the diagnosis of COVID-19 had been made). However, potentially some of these deaths would be recorded as due to cardiovascular events if viral symptoms had been otherwise mild and the patient had not presented for COVID-19 PCR testing prior to the cardiovascular event.
Figure 1.
(A) Exce deaths in USA 2015–2021, including COVID-19, Source: CDC, available freely at: https://www.cdc.gov/nchs/nvss/vsrr/covid19/excess_deaths.htm%23dashboard, this use does not imply approval of this article by CDC.
Figure 2.
Weekly counts of death due to select causes of disease USA 2015–2021, Source: CDC, available freely at: https://www.cdc.gov/nchs/nvss/vsrr/covid19/excess_deaths.htm%23dashboard, this use does not imply approval of this article by CDC.
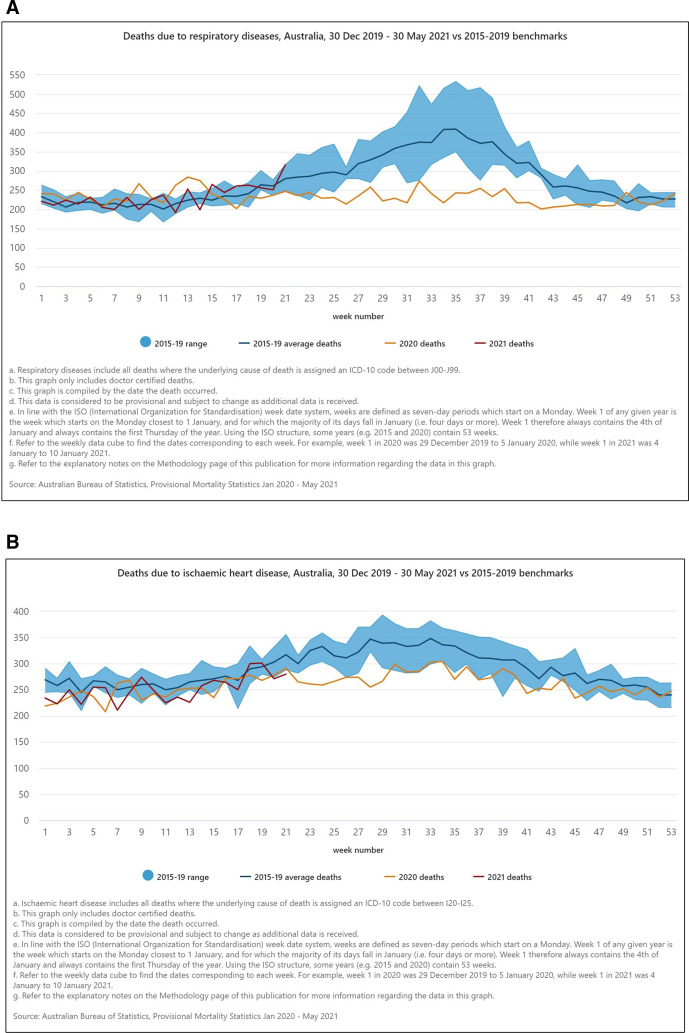
Evidence for an association strengthens when considering the mirror image scenario of a country which was not ravaged by COVID-19 in 2020. Australia had far fewer deaths than expected due to respiratory causes in the winter of 2020, with influenza and pneumonia generally being the most common causes8 (figure 3A). The likely explanation is that social distancing requirements to prevent COVID-19 spread equally reduced spread of frequent winter respiratory illnesses. It is eye-opening that cardiovascular deaths were also significantly lower than expected in the winter of 2020 in Australia (figure 3B).8
Figure 3.
(A, B) Deaths in Australia due to (A) respiratory and (B) ischaemic heart disease in 2020 and early 2021, compared with 2015–2019 benchmarks reproduced from Provisional Mortality Statistics | Australian Bureau of Statistics (abs.gov.au).
Norway’s COVID-19 experience was in between the USA and Australian extremes. Norway showed both reduced hospitalisations for influenza and cardiovascular diseases in 2020 but increased hospitalisations for COVID-19. The increase due to COVID-19 hospitalisations was less than the reduction in influenza hospitalisations.9
Further associations and limitations between environmental factors and cardiovascular deaths
These observations give additional context to epidemiological findings that overall cardiovascular deaths are more common in cold winter environments and also hot summer environments, but are less common in temperate weather conditions.10 Temperate weather conditions facilitate outdoor living, which tends to prevent spread of respiratory viruses. Weather conditions which favour indoor gatherings appear to be associated with increased cardiovascular events—and therefore it is possible that respiratory viruses are implicated.
Cardiovascular deaths in the young are infrequent
The vast majority of cardiovascular events and deaths are due to coronary artery disease in middle-age and elderly populations, so we need to be careful not to generalise these findings for these populations to the young adult populations (who play a lot of competitive sport) for whom sudden cardiac death remains rare. Recent research has shown far lower than initially expected rates of cardiac complications of COVID-19 in young athletes.11 There is a risk of overtraining when exercising hard with an infection, spread to teammates and a very small risk of exacerbating myocarditis.12 The following theories are suggested and are not contradictory, even though they seem paradoxical:
There may be a high correlation between respiratory viruses circulating in the community and overall cardiovascular deaths (which are dominated by statistics in middle-aged and elderly people).
Because the risk of cardiovascular death in young athletes is rare, any relative risk increase in cardiovascular deaths imposed by respiratory viruses may have very low absolute risk increase.
Implications for large sporting events
Mass participation fun runs and triathlons are generally held outdoors (which itself is healthy from a respiratory virus viewpoint). Mass events though do involve gathering in indoor situations such as public transport on the way to events. The events themselves give rise to a small but consistent number of cardiovascular events and deaths (approximately 1 per 100 000 participants).13 14 There is already advice against participating in endurance events when suffering from respiratory symptoms, although it is not absolute. Some experts suggest a ‘neck check rule’ feeling it is safe to participate if all symptoms are upper respiratory and not involving the chest.15 The COVID-19 pandemic response in many countries emphasised the imperative to ‘stay home when sick’, and we should now be asking the question of whether this advice should be permanent in the post-COVID-19 world. While there are very low absolute risks in the young, it is more about culture change across the community. It is harder to use the risk of myocarditis to convince athletes to potentially save their own lives, when the risk is very low. Indirectly though, isolating may save the lives of more vulnerable members of the community if you break the chain of the respiratory virus you are carrying.
Implication for team sports
The social responsibility to ‘stay home when sick’ is sound advice for team sports too, particularly at junior and amateur levels. However, it is at odds with the traditional culture of team sport where it was expected that you come for every match to avoid ‘leaving the team short’. It is also harder to expect junior players to pull out with illness if they watch their star idols ‘push through for the team’. The Netflix series The Last Dance gave a great historical record of Chicago Bulls players gathering in crowds in the lead-up to important playoff matches, and also of games that were jeopardised if one of the superstar players was ill on match day (where he inevitably played despite the illness). There is now some obligation for sport to be part of the culture change to avoid spreading respiratory viruses for the good of the community. It is easiest to start with training sessions (‘stay home from training if sick’), as you risk spreading virus on to teammates if you train while sick, potentially doing more harm than good. In a world yet to eliminate COVID-19, the spread of more benign respiratory viruses in a team will lead to stand-downs until COVID-19 can be ruled out. The threat of the team losing a match due to players underperforming through illness is also likely to be a key to changing the mindset.
It will also be interesting to see how medicine itself copes with a revised culture of ‘stay home when sick’, as traditionally doctors have been—like athletes—bad offenders at refusing to take time off!
Footnotes
Twitter: @DrJohnOrchard, @jessicajorchard
Contributors: Viewpoint: all authors contributed to writing.
Funding: JJO is supported by a Postdoctoral Fellowship (Award Reference No. 104809) from the National Heart Foundation of Australia.
Competing interests: None declared.
Provenance and peer review: Not commissioned; internally peer reviewed.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Frøbert O, Götberg M, Erlinge D, et al. Influenza vaccination after myocardial infarction: a randomized, double-blind, placebo-controlled, multicenter trial. Circulation 2021. 10.1161/CIRCULATIONAHA.121.057042. [Epub ahead of print: 30 Aug 2021]. [DOI] [PubMed] [Google Scholar]
- 2.Yedlapati SH, Khan SU, Talluri S, et al. Effects of influenza vaccine on mortality and cardiovascular outcomes in patients with cardiovascular disease: a systematic review and meta-analysis. J Am Heart Assoc 2021;10:e019636. 10.1161/JAHA.120.019636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Clar C, Oseni Z, Flowers N. Influenza vaccines for preventing cardiovascular disease. Cochrane Database Syst Rev 2015;5:Cd005050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Giattino C, Ritchie H, Roser M. Excess mortality during the coronavirus pandemic (COVID-19) ourworldindata.com, 2020. Available: https://ourworldindata.org/excess-mortality-covid
- 5.Woolf SH, Chapman DA, Sabo RT, et al. Excess deaths from COVID-19 and other causes in the US, March 1, 2020, to January 2, 2021. JAMA 2021;325:1786. 10.1001/jama.2021.5199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Haslbauer JD, Tzankov A, Mertz KD, et al. Characterisation of cardiac pathology in 23 autopsies of lethal COVID-19. J Pathol Clin Res 2021;7:326–37. 10.1002/cjp2.212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Puntmann VO, Carerj ML, Wieters I, et al. Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from coronavirus disease 2019 (COVID-19). JAMA Cardiol 2020;5:1265–73. 10.1001/jamacardio.2020.3557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Australian Bureau of Statistics . Provisional mortality statistics: provisional deaths data for measuring changes in patterns of mortality during the COVID-19 pandemic and recovery period, 2021. Available: https://www.abs.gov.au/statistics/health/causes-death/provisional-mortality-statistics/latest-release
- 9.Myhre PL, Grundvold I, Paulsen TH, et al. Cardiovascular hospitalizations, influenza activity, and COVID-19 measures. Circulation 2020;142:1302–4. 10.1161/CIRCULATIONAHA.120.049118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stewart S, Keates AK, Redfern A, et al. Seasonal variations in cardiovascular disease. Nat Rev Cardiol 2017;14:654–64. 10.1038/nrcardio.2017.76 [DOI] [PubMed] [Google Scholar]
- 11.Moulson N, Petek BJ, Drezner JA, et al. SARS-CoV-2 cardiac involvement in young competitive athletes. Circulation 2021;144:256–66. 10.1161/CIRCULATIONAHA.121.054824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Woods JA, Hutchinson NT, Powers SK, et al. The COVID-19 pandemic and physical activity. Sports Med Health Sci 2020;2:55–64. 10.1016/j.smhs.2020.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Waite O, Smith A, Madge L, et al. Sudden cardiac death in Marathons: a systematic review. Phys Sportsmed 2016;44:79–84. 10.1080/00913847.2016.1135036 [DOI] [PubMed] [Google Scholar]
- 14.Windsor JS, Newman J, Sheppard M. Cardiovascular disease and Triathlon-Related deaths in the United Kingdom. Wilderness Environ Med 2020;31:31–7. 10.1016/j.wem.2019.11.002 [DOI] [PubMed] [Google Scholar]
- 15.Metz JP. Upper respiratory tract infections: who plays, who SITS? Curr Sports Med Rep 2003;2:84–90. 10.1249/00149619-200304000-00007 [DOI] [PubMed] [Google Scholar]