Abstract
Objective
Documentation of middle ear pressure at different stages of balloon Eustachian tuboplasty and assessing risk of barotrauma with this procedure.
Main outcome measures
Middle ear pressure measurements in patients undergoing balloon Eustachian tuboplasty at the time of pre‐insertion, catheter insertion, inflation, one minute post inflation, deflation, and catheter withdrawal, as well as documentation of pressure change in the middle ear between different stages.
Results
A total of 24 patients and 45 Eustachian tubes, 11 females and 13 males, with an average age of 55.6 years were included in this study. Middle ear pressure values during the active stages of the procedure varied from −356 to +159 daPa. The overall greatest negative pressure change measured was −515 daPa from catheter insertion to immediately post balloon inflation. The overall greatest positive pressure change measured was +418 daPa from immediate catheter inflation to one minute post inflation.
Conclusions
There was no consistent pattern of middle ear pressure change noted during the different stages of balloon Eustachian tuboplasty as both positive and negative middle ear pressure changes were noted at the time of balloon dilation. Dangerous levels of middle ear pressure raising concern for barotrauma were not identified during the procedure.
Level of evidence
Level IV.
Keywords: balloon Eustachian tuboplasty, Eustachian tube dysfunction, middle ear pressure, tympanogram, tympanometry
1. INTRODUCTION
The new era of balloon Eustachian tuboplasty (BET) offers promises in restoring natural ventilation of the middle ear by directly optimizing Eustachian tube function in patients with chronic obstructive Eustachian tube dilatory dysfunction. This field is still being heavily investigated, which is warranted, as the bulk of otology practice is related to Eustachian tube dysfunction and its short‐ and long‐term sequelae. Understanding the potential risks and adverse consequences of this procedure is key in establishing safety protocols and broadly introducing this procedure into the field of otolaryngology. One concern has been the effect of middle ear pressure changes from Eustachian tube catheter manipulation and balloon dilation in fear of avoiding barotraumatic events that can lead to tympanic membrane rupture or inner ear trauma with resulting hearing loss, tinnitus, or dizziness. Thus far the literature has not demonstrated these potential risks at a level that would raise concern. A reason for this safety profile may be that the commonly used devices for BET in the United States (ie, FDA‐approved devices) have lumens that should serve as a vent to avoid dramatic changes in middle‐ear pressure during all stages. It is important to maintain the patency of this lumen throughout all stages of the procedure.
Demonstrating variations in middle ear pressure while performing BET in patients with Eustachian tube dysfunction provides information that can guide understanding potential mechanisms of action of this procedure and supports the risk assessment for barotraumatic consequences.
In 2017, a cadaveric study performed in sheep revealed a correlation between middle ear pressure amplitudes and speed of balloon dilation and degree of inflation pressure. 1 Negative pressure amplitudes were seen with and related to the speed of withdrawal of the balloon. 1 In another study, middle ear pressure measurements in 13 ears of 9 fresh human cadaver heads at the time of insertion, inflation, deflation, and catheter removal revealed middle ear pressures in the physiologic range at all times. 2 An in vivo study of transtympanic middle ear pressure measurement under general anesthesia of 5 patients, with normal middle ears undergoing cochlear implantation, concluded that the highest pressure changes occurred at the time of catheter removal. 3 In the latter study, middle ear pressures were measured at insertion, inflation, deflation, withdrawal, and at time of recovery. 3 In all three studies, middle ear pressures capable of causing barotrauma were not detected.
This study was designed to offer information on middle ear pressure variations in patients undergoing BET in order to assess the risk of barotrauma with this procedure and to offer valuable literature data. This study is the first in vivo study to measure middle ear pressure variations in patients undergoing BET under local anesthesia.
2. MATERIAL AND METHODS
A prospective study was undertaken in an outpatient private practice setting in patients undergoing BET under local anesthesia. Adult patients with active and chronic Eustachian tube dysfunction symptoms or sequelae of active Eustachian tube dysfunction were included in this study. Patients with various indications for surgery were included in the study, including barochallenged patients, patients with abnormal tympanic membrane exams, and patients with underlying pathology such as chronic non‐suppurative otitis media and cholesteatoma. Further, patients with normal tympanometry findings and normal tympanic membrane exams were included based on symptoms reported on a modified ETDQ‐7 questionnaire used to assess for Eustachian tube dysfunction, 4 based on absence of motion of the tympanic membrane during a form of Valsalva maneuver while the tympanic membrane was being directly visualized through an endoscope or microscope, and based on video endoscopic evaluation of the Eustachian Tube appearance and its dynamic function. 5 Although the ETDQ‐7 was not used to support a diagnosis of Eustachian Tube Dysfunction, it was utilized as an additional indication for surgery if the patient reported a score of 3 or more on any of the 7 symptoms listed. As a result of the different indications for surgery, there was significant intersubject variability. All data collected were on intact tympanic membranes. Informed consent was obtained from all patients. The Entellus XprESS ENT Dilation System (6 × 18 mm or 6 × 20 mm), and the Acclarent Aera balloons were used as devices for dilation. A handheld Amplivox Otowave 102‐1 tympanometer was used to measure middle ear pressures during the following stages of the procedure: (1) preinsertion (prior to catheter insertion), (2) insertion (this is referring to immediately post insertion), (3) inflation (this is referring to immediately post inflation), (4) over one minute of inflation (referred to as one minute inflation), (5) deflation, and (6) withdrawal (this is referring to immediately post withdrawal). The seventh data point for each ear was obtained during the 4‐week post‐procedure visit.
Data were collected from 24 patients and 45 Eustachian tubes. In 21 patients, data were collected bilaterally. A total of 22 right ears and 23 left ears were included. There were 11 females and 13 males. Ages ranged from 31 to 79 years with an average age of 55.6 years. Twenty‐one Eustachian tubes had all 7 data points successfully measured. The Acclarent Aera balloon was used in 4 patients and 8 Eustachian tubes. The Entellus device was used in 17 patients and 37 Eustachian tubes. Of the Eustachian tubes dilated with the Acclarent Aera balloon, 4 yielded complete data, with 2 coming from the same patient. The decision to use one device over the other was made based on availability and not selected based on any clinical factor. All devices used for balloon dilation had an outer diameter of 6 mm upon inflation and a maximum pressure of 12 atm. Stage 3 of the procedure, inflation, was considered to be immediately after the plunger on the Entellus device was depressed, and on the Acclarent device when the meter indicated that the pressure had reached 12 atm. Pressure readings were not available for the Entellus device, but the plunger was kept fully depressed throughout 2 minutes of dilation. Pressure was kept at 12 atm on the Acclarent device as well by using a locking mechanism to keep the balloon inflated and increasing pressure immediately to 12 atm as needed throughout the 2‐minute dilation. All Eustachian tubes were dilated for a total of 2 minutes. Measurements with the tympanometer were performed by an assistant as the surgeon operated. The handheld tympanometer was removed between readings for the different stages of the procedure. Because measurements taken were discrete, rather than continuous, the assistant needed to achieve a seal quickly. The withdrawal technique involved deflating the balloons and withdrawing the balloons over the catheter, and subsequently withdrawing the catheter from the Eustachian Tube.
IRB approval for this prospective study was obtained through Solutions IRB.
3. RESULTS
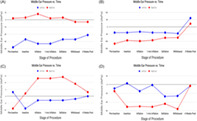
During the active stages of the procedure (from the time of catheter insertion), the overall most positive middle ear pressure measured was at the time of insertion (+159 daPa), and the most negative pressure was at the time of inflation (−356 daPa). Overall, the most positive average middle ear pressure was also documented during insertion (−10.56 daPa), and the most negative average middle ear pressure was noted immediately postinflation (−34.68 daPa) (Table 1 and Figure 1).
TABLE 1.
List of middle ear pressure reads in 21 ears with all data points measured
| Side | Gender | Age | Stage 1 | Stage 2 | Stage 3 | Stage 4 | Stage 5 | Stage 6 | Stage 7 |
|---|---|---|---|---|---|---|---|---|---|
| R | M | 32 | ‐32 | −39 | −26 | 103 | −21 | −16 | −4 |
| R | F | 57 | −15 | −51 | −50 | −51 | −44 | −56 | −3 |
| L | F | 57 | −9 | 3 | −15 | −14 | −27 | −26 | −3 |
| L | F | 60 | 51 | 56 | −16 | −10 | −4 | 14 | 3 |
| R | M | 56 | −99 | −46 | −213 | −212 | −200 | −182 | −196 |
| L | M | 56 | 2 | −81 | −99 | −93 | −68 | −62 | −58 |
| L | F | 43 | −10 | −3 | −129 | −9 | −3 | −9 | −10 |
| R | F | 72 | 16 | 14 | 15 | 3 | 9 | −2 | 10 |
| R | F | 75 | −45 | −39 | −44 | −39 | −39 | −45 | −87 |
| R | M | 71 | −9 | 2 | 13 | 13 | 14 | 9 | 3 |
| L | M | 71 | 3 | −9 | −3 | −3 | −3 | −2 | 0 |
| R | M | 54 | −45 | −51 | −56 | −50 | −51 | −57 | −31 |
| L | M | 52 | −33 | −44 | −33 | −39 | −39 | −32 | 2 |
| L | F | 51 | −51 | −32 | −26 | −32 | −26 | −21 | 3 |
| R | M | 66 | −116 | −93 | −98 | −92 | −75 | −74 | 22 |
| L | M | 66 | −39 | −39 | −33 | −39 | −39 | −45 | 61 |
| R | F | 58 | 20 | 3 | 9 | 2 | 2 | 14 | 1 |
| R | M | 31 | 2 | 3 | 8 | 2 | 3 | −3 | −3 |
| L | M | 31 | −38 | −27 | −33 | −33 | −27 | −27 | −21 |
| R | F | 62 | −9 | 2 | 8 | 9 | 3 | 8 | −27 |
| L | F | 62 | −3 | −3 | −4 | −3 | −4 | 2 | −21 |
Note: All results for stages 1–7 are in daPa (mm H20) (SD): Stage 1: middle ear pressure preinsertion (38). Stage 2: middle ear pressure on insertion (34). Stage 3: middle ear pressure on inflation (56). Stage 4: middle ear pressure on 1‐minute inflation (59). Stage 5: middle ear pressure on deflation (46). Stage 6: middle ear pressure on withdrawal (44). Stage 7: middle ear pressure 4 weeks post (50). Bold values are patients who have been dilated with the Acclarent Aera balloon and all others are patients who were dilated with an Entellus device.
FIGURE 1.
Average middle ear pressure during each stage of balloon Eustachian tuboplasty. Error bars refer to standard deviations
Middle ear pressure changes from pre‐ to postinsertion of the catheter ranged from −83 to +234 daPa with a mean change of +8.32 daPa.
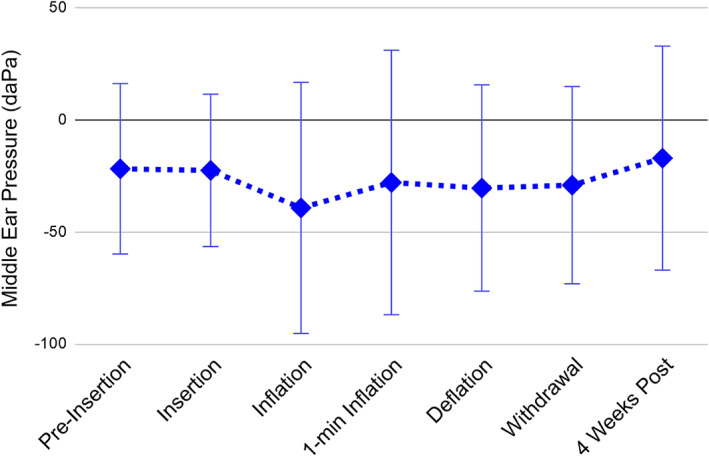
Middle ear pressure changes from time of insertion to immediately postinflation ranged from −515 to +18 daPa with a mean change of −26.6 daPa (Figure 2 and Table 2). The most negative average pressure change was noted during this interval (Figure 2).
FIGURE 2.
Average change in middle ear pressure during various stages of balloon Eustachian tuboplasty. Δ 1–2: pre‐insertion to insertion. Δ 2–3: insertion to inflation. Δ 3‐4: inflation to 1‐minute inflation. Δ 4‐5:1‐minute inflation to deflation. Δ 5‐6: deflation to withdrawal. Δ 1‐6: preinsertion to withdrawal. Δ 1‐7: preinsertion to 4 weeks post‐procedure
TABLE 2.
Pressure gradients during different stages of balloon Eustachian tuboplasty
| Preinsertion to insertion | Range | −83 to +234 daPa |
| Average | +8.3 daPa | |
| 𝜎 | 45 | |
| Insertion to inflation | Range | −515 to +18 daPa |
| Average | −26.6 daPa | |
| 𝜎 | 96 | |
| Inflation to 1‐minute inflation | Range | −12 to +418 daPa |
| Average | + 22.8 daPa | |
| 𝜎 | 80 | |
| 1‐minute inflation to deflation | Range | −124 to +27 daPa |
| Average | −1.9 daPa | |
| 𝜎 | 24 | |
| Deflation to withdrawal | Range | −11 to +18 daPa |
| Average | +1.1 daPa | |
| 𝜎 | 8 | |
| Preprocedure to withdrawal | Range | −84 to +115 daPa |
| Average | +10.6 daPa | |
| 𝜎 | 54 | |
| Preprocedure to 4‐weeks post procedure | Range | −97 to +138 daPa |
| Average | +4.4 daPa | |
| 𝜎 | 49 |
Note: 𝜎 = SD.
Middle ear pressure changes from inflation to over one minute of inflation ranged from −12 to +418 daPa with a mean change of +22.8 daPa (Figure 2 and Table 2). The highest average positive pressure change was noted during this interval (Figure 2).
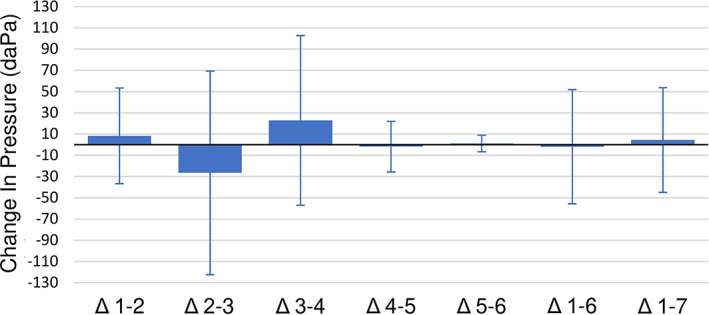
Maximum negative and positive pressure changes measured during this study was seen in the right ear of the same patient (Figure 3).
FIGURE 3.
Ear with greatest middle ear pressure variation during balloon Eustachian tuboplasty
Middle ear pressure changes from preprocedure to after catheter withdrawal ranged from −210 to +131 daPa with a mean of −1.9 daPa (Figure 2 and Table 2).
Although the study is not powered for a comparison, there does not appear to be any significant difference in middle‐ear pressure patterns between patients dilated with the Acclarent device compared to the Entellus device.
4. DISCUSSION
The mechanism of action of BET is yet to be fully understood. Biopsy of Eustachian tube lining before and immediately post dilation has revealed changes including thinning of mucosa, epithelial shearing, and crush injury of submucosal layers. 6 Delayed biopsy at 5‐12 weeks has shown formation of healthy pseudocolumnar epithelium and replacement of lymphocytic infiltrates with a thinner fibrous layer. 6 In vitro biomechanical findings have shown that energy dissipation during dilation is greater using a larger balloon and deeper device insertion but not as affected by increase of inflation pressure. 5 On histopathology, mucosal tearing and cartilage cracking are some of the noted mechanical changes. 7
Changes in middle ear pressure may also contribute to the success of BET by clearing the bony Eustachian tube, loosening middle ear scar formation, 1 and mobilizing retractions. 1 In our study, the greatest variations in middle ear pressure occurred at the time of balloon inflation. Surprisingly, the greatest negative middle ear pressure change was seen with inflation. Subsequently, the most positive middle ear pressure change occurred when comparing data from inflation to over one‐minute of inflation. The most negative change overall (−515 daPa) and the most negative average change (−26.6 daPa) occurred from the time of balloon insertion to inflation. The most positive overall change (+418 daPa) and the most positive average change (+22.8 daPa) occurred from the time of inflation to over one minute of inflation. It has been suggested that the immediate success of BET in some patients may be due to tissue deformation with widening of the cartilaginous Eustachian Tube, which is thought to result during BET either directly by the balloon itself or by inducing favorable tissue remodeling, which increases the patency of the cartilaginous Eustachian Tube. Factors that affect the degree of this success include the size of the balloon used, the depth of device insertion, and, to a lesser extent, the inflation pressure. 7 If the inflation pressure does contribute to the success of this technique, and with the most positive overall pressure change noted in these data occurring from the time of inflation to over one minute of inflation, this may suggest and support inflation for over one minute in BET. However, the authors acknowledge that the variability of absolute pressures and gradients measured in this study suggest the need for additional data and future studies. Measuring middle ear pressure at 2 minutes postinflation, and perhaps even further out, in a clinical trial may provide data that can guide our procedure protocols and answer the question of the ideal time and duration of balloon inflation that allows for the best outcome with the least risk of barotrauma or any other adverse events.
Although averages, maximum, and minimum absolute middle ear pressure values and gradients trended in one direction or the other, overall a consistent pattern of pressure increase, or decrease was not seen from one stage to the other in this study. Although middle ear pressures upon inflation trended toward a more negative value, middle ear pressure changes ranged from −515 to +18 daPa. The same degree of variability was seen amongst all phases, from pre‐insertion to insertion, insertion to inflation, and inflation to deflation. In addition, there was not much middle ear pressure variation seen from the deflation stage to balloon withdrawal (range: −11 to +18 daPa. Average: +1.1 daPa). The general trend was the development of a more negative middle ear pressure compared to preprocedure from inflation to balloon withdrawal. At 4 weeks, middle ear pressures were more positive and trending toward a more normal value than the preprocedure levels. (Figure 1).
The variability seen in the degree and direction of middle ear pressure changes measured between subjects and at various transition points of BET has been a clinical surprise and the reason for such variability is unknown. Perhaps the complexity of Eustachian tube dysfunction, all of its contributing factors, and variables involving this disease process, is yet to be understood. For years we have addressed Chronic Eustachian tube dilatory dysfunction by bypassing the Eustachian tube and providing artificial ventilation with tympanostomy tubes, and now that the natural function of this structure is being directly addressed, perhaps we need better classification of Eustachian tube dysfunction and better categorization of anatomic appearances of the nasopharyngeal Eustachian tube.
Predisposition to inner or middle ear barotraumatic events is seen in divers and individuals who are exposed to altitude change when underlying Eustachian tube dysfunction is present. Concerns can arise for patients subject to middle ear pressure changes undergoing balloon dilation, as the majority of these patients are barochallenged with poor tolerance of flying, diving, and mountain‐based activities. As such, investigating middle ear pressure changes during balloon dilation is important for risk assessment, patient counseling, and perhaps for establishing guidelines for safest surgical techniques. This study is the first to measure middle ear pressure readings and changes in patients undergoing BET in an office setting and under local anesthesia. The question that does not have a definitive answer is what pressure change, if any, during these procedures should raise a red flag and concern for the otolaryngologist prior to allowing for complications? A middle ear pressure of 10 000 daPa (100 kPa) is believed to be required for tympanic membrane perforation. 8 Normal middle ear pressure varies from −200 to +50 daPa. Many patients who undergo BET have middle ear pressures outside of the normal range both prior to the procedure and during the procedure; however, no study to date has reported pressures near 10 000 daPa with BET. Our results documented middle ear pressures during the active stages of the procedure from −356 daPa (inflation) to +158 daPa (insertion). Although these data are reassuring, due to the limitations of this study, they do not definitively exclude the possibility of an extreme, clinically significant pressure change. Although unlikely, there is a potential of missing extreme pressures that equilibrate immediately, as a continuous middle‐ear pressure read is not being obtained. We have to acknowledge that a timely pressure reading could not be obtained in all cases due to the restrictions imposed by using a handheld tympanometer. If a timely pressure reading was not obtained, these data were not included in the study.
It has been reported in the literature that the most pain seen in BET is at the level of catheter and balloon insertion. 9 In the senior author's experience, this has also been found to be the case. Interestingly, the greatest average pressure changes in the middle ear were not seen at the time of insertion, but post‐inflation (Figure 2). Dean and Pynnonen report that pain can be controlled by applying a topical anesthetic to the tympanic membrane surface, as pain is potentially arising from stretching of the tympanic membrane. 10 Based on our results and what has been previously reported in the literature, perhaps the main discomfort does not arise from navigating through the Eustachian tube, but from the dynamic changes that occur in the middle ear and within the tympanic membrane.
A lot of what is researched in the literature on barotrauma is related to divers and patients undergoing hyperbaric oxygen chamber therapy. There is a Teed and Modified Teed classification, as well as the O'Neill Grading System, which classify degrees of barotrauma based on otoscopic findings. The latter is geared mostly toward patients undergoing hyperbaric oxygen therapy. If these grading systems are applied to patients undergoing BET, minor erythema of the tympanic membrane, ruptured membrane vessels, or minor hemotympanum, which can be seen with this procedure, would imply a degree of barotrauma with balloon dilation. Based on our findings, and what is previously reported in the literature, middle ear pressure changes are not clinically significant enough to raise concern with BET. However, this does not imply that minor changes cannot be seen at the level of the tympanic membrane.
The positive safety profile of BET should not discourage reporting barotraumatic complications that are clinically significant to the otolaryngologists and patients, such as tympanic membrane perforation, major hemotympanum with associated conductive hearing loss, sensorineural hearing loss, new onset tinnitus, and dizziness. There is a lot to be learned on BET from its efficacy and true success rates, technique modifications and specific recommendations based on different anatomic and pathologic presentations of Eustachian tubes, and a clear representation of potential consequences of acute middle ear pressure changes.
5. CONCLUSION
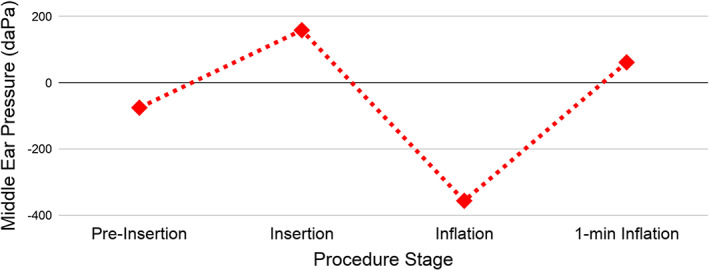
There was no consistent pattern of middle ear pressure change noted during the different stages of BET, as exemplified by Figure 4. Dangerous levels of middle ear pressure raising concern for clinically significant barotrauma were not identified. Overall, the most negative pressure change occurred between catheter insertion and inflation, and the most positive middle ear pressure change was seen from post inflation to over one minute of inflation.
FIGURE 4.
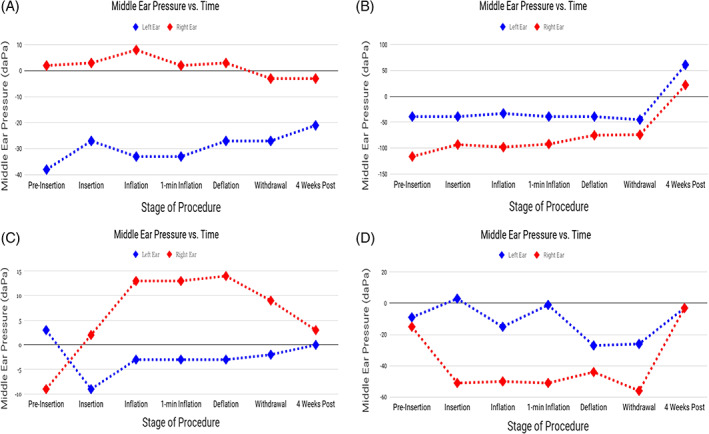
Middle ear pressure changes at various stages of balloon Eustachian tuboplasty of four selected patients with complete bilateral data. Red = right ear. Blue = left ear
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
FINANCIAL DISCLOSURE
The authors declare no financial disclose.
Azadarmaki R, How A, Dean C, DeLorenzo K. In vivo study measuring middle ear pressure during various stages of Eustachian tube balloon dilation. Laryngoscope Investigative Otolaryngology. 2021;6(5):1110‐1115. 10.1002/lio2.631
The content of this manuscript is being presented at the COSM 2020 Virtual Poster Session from May 15 to June 15, 2020. The poster will be a part of the Triological Society Meeting.
BIBLIOGRAPHY
- 1. Todt I, Abdel‐Aziz T, Mittmann P, et al. Measurement of middle ear pressure changes during balloon eustachian tuboplasty: a pilot study. Acta Otolaryngol. 2017;137(5):471‐475. 10.1080/00016489.2016.1253870 [DOI] [PubMed] [Google Scholar]
- 2. Smith ME, Tysome JR. Middle ear pressure changes during balloon Eustachian tuboplasty. Otolaryngol Head Neck Surg. 2017;156(1):161‐165. 10.1177/0194599816672842 [DOI] [PubMed] [Google Scholar]
- 3. Sudhoff H, Mittmann P, Todt I. In vivo measurement of middle ear pressure changes during balloon Eustachian tuboplasty. Biomed Res Int. 2018;2018:9519204. 10.1155/2018/9519204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. McCoul ED, Anand VK, Christos PJ. Validating the clinical assessment of eustachian tube dysfunction: the Eustachian tube dysfunction questionnaire (ETDQ‐7). Laryngoscope. 2012;122(5):1137‐1141. 10.1002/lary.23223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Azadarmaki R. Clinical tools to diagnose Eustachian tube dysfunction in patients with a normal tympanic membrane exam and a type a tympanogram. Arch Otolaryngol Rhinol. 2019;5(4):99‐101. 10.17352/2455-1759.000208 [DOI] [Google Scholar]
- 6. Kivekäs I, Chao W‐C, Faquin W, et al. Histopathology of balloon‐dilation eustachian tuboplasty. Laryngoscope. 2015;125(2):436‐441. 10.1002/lary.24894 [DOI] [PubMed] [Google Scholar]
- 7. Smith ME, Weir AE, Prior DC, Cope W, Tysome JR, Sutcliffe M. The mechanism of balloon Eustachian tuboplasty: a biomechanical study. Med Biol Eng Comput. 2020;58:689‐699. 10.1007/s11517-020-02121-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. ONeill OJ, Frank AJ. Ear Barotrauma. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020. https://www.ncbi.nlm.nih.gov/books/NBK499851/ Updated December 20 2019.
- 9. Luukkainen V, Kivekäs I, Hammarén‐Malmi S, et al. Balloon Eustachian tuboplasty under local anesthesia: is it feasible? Laryngoscope. 2017. May;127(5):1021‐1025. 10.1002/lary.26488 [DOI] [PubMed] [Google Scholar]
- 10. Dean M, Pynnonen MA. In‐office balloon dilation of the Eustachian tube under local anesthesia. Otolaryngol Clin North Am 2019. Jun;52(3):509–520. doi: 10.1016/j.otc.2019.02.005. [DOI] [PubMed] [Google Scholar]


