Abstract
The COVID-19 pandemic’s disproportionate impact on people from some racial and ethnic groups in the U.S. persisted throughout 2021. Black, Latinx, and American Indian persons have been hospitalized and died at a higher rate than White persons consistently from the start of the pandemic. Early data show that hospitalization and mortality rates for Black, Latinx, and American Indian children are higher than White children in a worrying trend. The pandemic has likely worsened the gaps in wealth, employment, housing, and access to health care: the social determinants of health that caused the disparities in the first place. School closures will have a long-lasting impact on the widening achievement gaps between Black and Latinx students and White students. In the earlier vaccination phase, Black and Latinx persons were being vaccinated at a lower rate than their proportion of cases due to vaccine hesitancy, misinformation, and barriers to access. Vaccine hesitancy rates among these groups have since decreased and are now comparable to White persons. Aggregated data make it challenging to paint a picture of the actual impact of COVID-19 on Asian Americans as they are a diverse group with significant disparities. All of this highlights that we have much work to do in dismantling systemic racism, engaging communities we serve, and advancing health equity to prepare us for future pandemics and a more just healthcare system.
Keywords: COVID-19 impact, Racial disparities, Race and ethnicity, Systemic racism
Introduction
It has been more than a year since we wrote about the disproportionate impact of COVID-19 on Black/African American (Black), Hispanic/Latinx, and American Indian persons [1]. Since then, many events have transpired, including waves and surges of COVID-19 throughout the different states, the discovery of effective therapeutics, and mass vaccinations. Our knowledge of COVID-19 has dramatically expanded. In this paper, we update our previous commentary using the most recent information on the epidemiology of COVID-19 in the United States (U.S.) and how it has affected racial and ethnic minority groups from biomedical and social determinants of health perspectives. We also discuss using the principles of health equity and community engagement in addressing disparities [2].
Updates on Disproportionate Health Impact of COVID-19 on Racial and Ethnic Minority Groups
As of October 1, 2021, Latinx persons comprise 27% of all COVID-19 cases, approximately 10% higher than their proportion in the general population. Black persons are 12% of all cases, which is more in line with the general population at 12.5% [3, 4]. However, case rates are misleading due to the lack of access to testing in some communities [5]. This is borne out by the persistently elevated median test positivity rates among Black persons (13.8%) and Latinx persons (11.9%) compared with White persons (7%) [6].
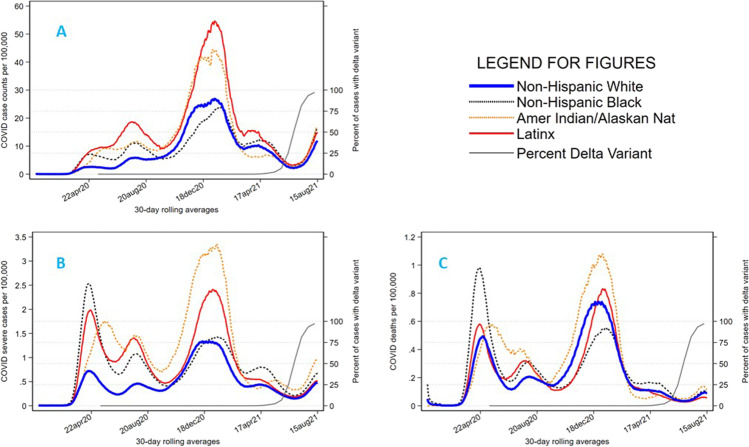
Black, Latinx, and American Indian persons are more likely to be hospitalized and die than White persons [5]. In a study of 35 states, the average Black persons to White persons crude death rate disparity ratio is 1.6. After adjusting for age and state, the disparity ratio grew to 2.7 [7]. American Indian, Alaska Native (AIAN), and Native Hawaiian (N.H.) persons have the highest incident cases and deaths per 100,000 populations for most of the pandemic up to the present. Despite this, research involving AIAN and N.H. persons is not extensive due to lack of data from states or uniformity of data across the nation. One concerning trend in 2021 is the increasing number of infections among American children. Early data has shown that Black, Latinx, and AIAN children have higher hospitalization and mortality rates than White children [8]. We summarized these in Fig. 1 and Table 1.
Fig. 1.
Temporal trends in 30-day running averages in COVID-19 cases, severe cases, and mortality rate by race and ethnicity. Note: Data are from the CDC COVID-19 case surveillance public-use data. Severe cases are defined as hospitalization, use of mechanical ventilation, or presence of acute respiratory distress
Table 1.
Key statistics in the disproportionate health impact of the COVID-19 pandemic on racial and ethnic minority groups in the U.S
| Black | Latinx | AIAN | White | |
|---|---|---|---|---|
| Risk of hospitalization ± [9] | 2.8x | 2.8x | 3.5x | reference |
| Risk of death ± [9, 10] | 2x | 3x | 2.4x | reference |
| Hospitalization rate among children (per 10,000)* [8] | 56.9 | 67.1 | 79.4 | 26.2 |
| Mortality rate among children (per 1,000,000)* [8] | 13.8 | 9.2 | 18.2 | 5.1 |
± , as of September 9, 2021; *, as of August 31, 2021
Asian American persons are thought to have the same outcomes regarding severity and mortality from COVID-19 compared to White persons [11]. However, Asian Americans are a diverse, heterogeneous group. On average, Asian American persons have higher educational attainment and income levels than White persons, but the poverty rate among Filipino persons is 5.8% compared to 14% among Hmong persons; 27% of Indian persons’ occupations are managerial positions compared to 8% of Hmong persons. Other disparities in insurance coverage and medical conditions are also pervasive among different groups [12]. Therefore, a lack of disaggregated data may mask the actual effect of COVID-19 on Asian American persons.
Our knowledge of risk factors for severe COVID-19 disease and death has become more precise. Studies show that comorbidities such as diabetes, hypertension, obesity, and coronary artery disease are risk factors for more severe disease and death from COVID-19 [13–16]. While such comorbidities disproportionately affect some racial and ethnic minority groups, these disparities of baseline health status alone likely did not account for COVID-19 outcome disparities [16].
Updates on Disproportionate Socioeconomic Impact of COVID-19 on Racial and Ethnic Minority Groups
We have previously written that social determinants of health contributed to the disproportionate impact of COVID-19 on minorities. There are significant gaps in wealth, employment, housing, and access to health care between White persons and people from some racial and ethnic groups [1]. Unfortunately, the COVID-19 pandemic has only worsened these disparities. The economic fallout and job losses disproportionately affected people from some racial and ethnic groups [17]. The unemployment rate peaks were 18.5% for Black and 16.7% for Latinx persons during the pandemic compared to 14.1% for White persons. This reflects the job losses in the service and retail sectors of the economy, which employs racial and ethnic minority groups at a higher rate. Upon economic recovery, these groups are last to gain employment. As of June 2021, unemployment stood at 9.2% for Black persons and 7.4% for Latinx persons compared to White persons at 5.2% [18]. Furthermore, for many individuals, health insurance is tied to employment. As of June 2, 2021, 15% of Black persons and 27% of Latinx persons reported being uninsured despite some recovery of jobs lost, relative to 7% among White persons.
The disproportionate socioeconomic impact of COVID-19 extends to children of color. On housing during the pandemic, Black and Latinx persons reported being unable to catch up with paying their rent and mortgage at a higher rate than White persons [19]. Before the pandemic, they were more likely to be cost-burdened than White persons [20]. Fueled by a systemic legacy of racist housing policies, the outcome is eviction rates that are now two times higher among Black persons than White persons [21]. The shutdown of schools disrupted many facets of the lives of families with children. Black and Latinx students have less access to in-person learning and less engagement with long-distance learning due to less reliable internet connectivity, possibly leading to long-lasting and worsening effects of the achievement gap between White and Black and Latinx children [19, 20]. School closures have also unintended consequences as Black and Latinx parents have more difficulty accessing childcare and children’s nutrition usually affordably provided by schools [21, 22].
These vicious cycles of worsening socioeconomic factors can further worsen the disparities in social determinants of health and lead to worse outcomes in future pandemics. There is evidence that higher eviction rates and food insecurity worsens infection rates [23, 24]. Due to the disproportionate socioeconomic impact of the pandemic on people from some racial and ethnic groups, they are depleting their wealth faster by tapping into their savings, retirement accounts, and selling assets to cover usual household expenses. These effects will likely widen the racial wealth gap even further, exacerbating a staggering eightfold wealth advantage for White persons compared with Black persons [25]. Lastly, people from racial and ethnic minority groups’ access to quality healthcare services are also at risk due to the trend of closures of safety net hospitals resulting from huge financial losses during the pandemic and may accelerate without proper intervention [26].
COVID-19 Disparities in Vaccinations
COVID-19 vaccination is credited with the progressive easing of restrictions and return to normalcy and lifting of COVID-19 restrictions. There were early reports of racial disparities when vaccines were in short supply relative to demand [27]. Now that supply outstrips demand, the racial disparities are still apparent. As of October 1, 2021, only 36% of Black persons have started or completed vaccination compared to 42% of White persons [3]. This gap has been attributed to barriers to access, mistrust of research, misinformation, and low confidence in the COVID-19 vaccine in the context of a legacy of historical social injustices [17]. In the earlier phases of vaccinations, vaccine hesitancy was high among Black and Latinx persons. However, throughout 2021, vaccine hesitancy among Black and Latinx persons significantly decreased compared to White persons. As of September 2021, the proportion of those who report that they will definitely not get vaccinated or only when required was 19% for Black persons and 14% for Latinx persons compared to 17% for White persons [28]. Therefore, upstream social determinants of health are accounting for the vaccine disparity, including disproportionate easy access to vaccines in wealthier neighborhoods, inability to skip work to receive a vaccine, lack of access to culturally and linguistically tailored information, and fear of deportation among some immigrant groups [29–32]. This is evident in previous vaccination programs such as the annual influenza vaccinations in which people from racial and ethnic minority groups have persistently low vaccination rates compared to White persons. One possible reason is the lack of health insurance among people from racial and ethnic minority groups [33].
Despite challenges that AIAN persons face, they lead the nation in the proportion of the population vaccinated [3], a testament to the success of community engagement and tremendous work by tribal leaders and health workers. On the other hand, Asian American persons, as a group, have one of the highest vaccination rates among all minority groups. Due to the lack of disaggregated data for Asian American persons, it is challenging to have a clear picture of the different ethnic subgroups. Cultural factors and migration patterns might contribute to differences in vaccine uptake among Asian American persons. There is some evidence that Filipino and Korean persons were likelier to have concerns about the vaccine than Vietnamese or Chinese persons [34]. Anecdotal evidence shows that the same systemic barriers that other racial and ethnic minority groups also face some Asian American subgroups [35, 36].
Although the data on vaccination of children is limited, concerning trends is emerging. Only six states and Washington DC are reporting this data as of September 7, 2021. The percentage of Black children vaccinated lagged behind White children in all seven states. The starkest example is in Washington DC where 74% of White children ages 12–17 are vaccinated compared to 26% of Black children [8].
Lessons for the Future
As we emerge from the COVID-19 pandemic in the U.S., healthcare institutions and clinicians have increased awareness of its disproportionate impact on racial and ethnic minority groups. First, community engagement initiatives such as the National Institutes of Health Community Engagement Alliance (CEAL) remain a critical tool for the promotion of health equity in future pandemics. This includes education and information dissemination centered around trusted community leaders. Collaboration with experts and local leaders through channels most appropriate for the community will overcome barriers particularly, language barriers [37, 38]. Many communities have established organizations and infrastructure that are invaluable resources for community intervention. Community organizers have deep insights into the needs of the population including their strengths and weaknesses. With the rapid transition to telehealth during the pandemic, institutional responses relied heavily on digital technology. However, the digital divide, defined as the gaps in access, usage/skills, and outcomes of information and communication technology, may have disproportionately disadvantaged people from some racial and ethnic groups due to difficulty with an adequate internet connection or navigating mobile health applications. Community engagement can also identify and help alleviate the root causes of the disparities such as the social determinants of health and pre-existing comorbidities [39]. The importance of community engagements has also been made more apparent in addressing vaccine inequity. An intervention to promote vaccine equity focused on engaging Black faith leaders and healthcare professionals and intentionally holding vaccination clinics in neighborhoods with predominantly Black persons [40].
Secondly, pandemics hit underresourced communities faster and harder. Thus, we are tasked to ensure that future pandemic mitigation policies should be evaluated early through an equity lens to avoid unintended consequences. As a foundation, institutional investment in widely accessible, integrated healthcare delivery will be important to ensure early access to care during future pandemics. Transportation to and from medical appointments, robust language services, and community health worker outreach may be utilized by medical homes to further bridge the gaps in healthcare access and utilization [41]. Long-term community investments are needed to support the goal of health equity [42].
Lastly, thoughtful, systemic collection of data on race and ethnicity should be standardized across jurisdictions to conduct better research. Prospective, longitudinal research on outcomes of different community engagement initiatives can help improve future programs and outreach. Community participation in clinical trials on cures and vaccines is also essential.
More broadly, the pandemic has taught us that it is incumbent on healthcare institutions and clinicians to advocate for the societal resources that their patients need to sustain their physical and mental health during a pandemic. This includes access to high-quality housing, education, transportation, and childcare. Unfortunately, these lessons are not new and reflect a collective short-term memory that belies the central role of systemic racism in downstream inequities. The concomitant reckoning with systemic factors highlighted by the murder of George Floyd and violent attacks against Asian American persons further underscores the need for change now in order to prevent stark inequities in the next pandemic. A legacy of structural racism continues to directly impact employment processes, financial institutions (and wealth accumulation), housing access, and criminal justice (mass incarceration). Healthcare institutions and clinicians must advocate for ongoing efforts to address these root causes of health disparities within and beyond healthcare institutions.
The next pandemic is not a matter of “if” but “when.” We had unprecedented successes in diagnostics, treatment, and prevention of a new disease at record-breaking speed. We also have the opportunity to learn and successfully create an equitable health care system for the next pandemic.
Data Availability
Not applicable.
Code Availability
Not applicable.
Declarations
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Competing Interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Don Bambino Geno Tai, Email: Tai.Don@mayo.edu.
Mark L. Wieland, Email: Wieland.Mark@mayo.edu
References
- 1.Tai DBG, Shah A, Doubeni CA, et al. The disproportionate impact of COVID-19 on racial and ethnic minorities in the United States. Clin Infect Dis. 2021;72(4):703–706. doi: 10.1093/cid/ciaa815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jones CP. Systems of power, axes of inequity: parallels, intersections, braiding the strands. Med Care. 2014;52:S71–S75. doi: 10.1097/MLR.0000000000000216. [DOI] [PubMed] [Google Scholar]
- 3.COVID Data Tracker Available at: https://covid.cdc.gov/covid-data-tracker/#demographics. Accessed 4 Oct 2021.
- 4.Racial and Ethnic Diversity in the United States: 2010 Census and 2020 Census. Available at: https://www.census.gov/library/visualizations/interactive/racial-and-ethnic-diversity-in-the-united-states-2010-and-2020-census.html. Accessed 22 Aug 2021.
- 5.Baker D.W. Breaking links in the chain of racial disparities for COVID-19. JAMA Network Open 2021; 4(6): e2112879-e. 10.1001/jamanetworkopen.2021.12879. [DOI] [PubMed]
- 6.Introduction to COVID-19 Racial and Ethnic Health Disparities. Available at: https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/racial-ethnic-disparities/index.html. Accessed 23 July 2021.
- 7.Siegel M, Critchfield-Jain I, Boykin M, et al. Actual racial/ethnic disparities in COVID-19 mortality for the non-Hispanic Black compared to non-Hispanic White population in 35 U.S. States and their association with structural racism. J Racial Ethn Health Disparities. 2021. 10.1007/s40615-021-01028-1. [DOI] [PMC free article] [PubMed]
- 8.Artiga S, Hill L, Ndugga N. Racial disparities in COVID-19 impacts and vaccinations for children. Available at: https://www.kff.org/racial-equity-and-health-policy/issue-brief/racial-disparities-in-covid-19-impacts-and-vaccinations-for-children/. Accessed 27 Sept 2021.
- 9.Risk for COVID-19 infection, hospitalization, and death by race/ethnicity. Available at: https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-race-ethnicity.html. Accessed 4 Oct 2021.
- 10.Arrazola J, Masiello MM, Joshi S, et al. COVID-19 mortality among American Indian and Alaska Native persons — 14 States January–June 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1853–1856. doi: 10.15585/mmwr.mm6949a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mackey K, Ayers CK, Kondo KK, et al. Racial and ethnic disparities in COVID-19–related infections, hospitalizations, and deaths. Ann Intern Med. 2021;174(3):362–373. doi: 10.7326/M20-6306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Profile: Asian Americans. Available at: https://minorityhealth.hhs.gov/omh/. Accessed 28 May 2021.
- 13.Sara Y. Tartof LQ, Hong V. Obesity and mortality among patients diagnosed with COVID-19: results from an integrated health care organization. Ann Intern Med. 2020; 173(10): 773–81. 10.7326/M20-3742. [DOI] [PMC free article] [PubMed]
- 14.Peters SAE, MacMahon S, Woodward M. Obesity as a risk factor for COVID-19 mortality in women and men in the U.K. biobank: comparisons with influenza/pneumonia and coronary heart disease. Diabetes Obes Metab. 2021; 23(1): 258–62. 10.1111/dom.14199. [DOI] [PMC free article] [PubMed]
- 15.Li J, Huang DQ, Zou B, et al. Epidemiology of COVID-19: a systematic review and meta-analysis of clinical characteristics, risk factors, and outcomes. J Med Virol. 2021;93(3):1449–1458. doi: 10.1002/jmv.26424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Goodman KE, Magder LS, Baghdadi J.D., et al. Impact of sex and metabolic comorbidities on coronavirus disease 2019 (COVID-19) mortality risk across age groups: 66 646 inpatients across 613 U.S. hospitals. Clin Infect Dis. 2020. 10.1093/cid/ciaa1787. [DOI] [PMC free article] [PubMed]
- 17.Falk G, Romero PD, Carter JA, Nicchitta IA, Nyhof EC. Unemployment rates during the COVID-19 pandemic. Washington, DC: Congressional Research Service; 2021. [Google Scholar]
- 18.Broady K, Romer C. Despite June’s positive jobs numbers, Black workers continue to face high unemployment. Available at: https://www.brookings.edu/blog/the-avenue/2021/07/02/despite-junes-positive-jobs-numbers-black-workers-continue-to-face-high-unemployment/. Accessed 1 Aug 2021.
- 19.Oster E, Jack R, Halloran C, et al. Disparities in learning mode access among K-12 students during the COVID-19 pandemic, by race/ethnicity, geography, and grade level - United States, September 2020-April 2021. MMWR Morb Mortal Wkly Rep. 2021;70(26):953–958. doi: 10.15585/mmwr.mm7026e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Francis DV, Weller CE. Economic inequality, the digital divide, and remote learning during COVID-19. The Review of Black Political Economy. 2021:00346446211017797. 10.1177/00346446211017797 [DOI] [PMC free article] [PubMed]
- 21.Marron JM. Structural racism in the COVID-19 pandemic: don’t forget about the children! The Am J Bioeth. 2021;21(3):94–97. doi: 10.1080/15265161.2020.1871114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee EK, Parolin Z. The care burden during COVID-19: a national database of child care closures in the United States. Socius. 2021;7:23780231211032028. doi: 10.1177/23780231211032028. [DOI] [Google Scholar]
- 23.Nande A, Sheen J, Walters EL, et al. The effect of eviction moratoria on the transmission of SARS-CoV-2. Nat Commun. 2021;12(1):2274. doi: 10.1038/s41467-021-22521-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kimani ME, Sarr M, Cuffee Y, et al. Associations of race/ethnicity and food insecurity with COVID-19 infection rates across U.S. Counties. JAMA Netw Open 2021; 4(6): e2112852-e. 10.1001/jamanetworkopen.2021.12852. [DOI] [PMC free article] [PubMed]
- 25.Bhutta N, Chang AC, Dettling LJ, Hsu JW. Disparities in wealth by race and ethnicity in the 2019 Survey of Consumer Finances. Available at: https://www.federalreserve.gov/econres/notes/feds-notes/disparities-in-wealth-by-race-and-ethnicity-in-the-2019-survey-of-consumer-finances-20200928.htm. Accessed 23 July 2021.
- 26.Sullivan L, Jingnan H. Hospitals serving the poor struggled during COVID. Wealthy Hospitals Made Millions. Available at: https://www.npr.org/2021/05/18/996207511/hospitals-serving-the-poor-struggled-during-covid-wealthy-hospitals-made-million. Accessed 16 June 2021.
- 27.Painter EM, Ussery EN, Patel A, et al. Demographic characteristics of persons vaccinated during the first month of the COVID-19 vaccination program - United States, December 14, 2020-January 14, 2021. MMWR Morb Mortal Wkly Rep. 2021;70(5):174–177. doi: 10.15585/mmwr.mm7005e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.KFF COVID-19 Vaccine monitor Available at: https://www.kff.org/coronavirus-covid-19/dashboard/kff-covid-19-vaccine-monitor-dashboard/. Accessed 4 Oct 2021.
- 29.Diaz AA, Celedón JC. COVID-19 vaccination: helping the Latinx community to come forward. E Clin Med 2021; 35. 10.1016/j.eclinm.2021.100860. [DOI] [PMC free article] [PubMed]
- 30.Feldman N. Why Black and Latino people still lag on COVID vaccines — and how to fix it. Available at: https://www.npr.org/sections/health-shots/2021/04/26/989962041/why-black-and-latino-people-still-lag-on-covid-vaccines-and-how-to-fix-it. Accessed 16 June 2021.
- 31.Lewis T. The biggest barriers to COVID vaccination for Black and Latinx people. Available at: https://www.scientificamerican.com/article/the-biggest-barriers-to-covid-vaccination-for-black-and-latinx-people1/. Accessed 16 June 2021.
- 32.Razai MS, Oakeshott P, Esmail A, Wiysonge CS, Viswanath K, Mills MC. COVID-19 vaccine hesitancy: the five Cs to tackle behavioural and sociodemographic factors. J R Soc Med. 2021;114(6):295–298. doi: 10.1177/01410768211018951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Artiga S, Michaud J, Kates J, Orgera K. Racial disparities in flu vaccination: implications for COVID-19 vaccination efforts. Available at: https://www.kff.org/policy-watch/racial-disparities-flu-vaccination-implications-covid-19-vaccination-efforts/. Accessed 27 Sept 2021.
- 34.Ta Park V, Dougan M, Meyer O, et al. Differences in COVID-19 vaccine concerns among Asian Americans and Pacific islanders: The COMPASS Survey. J Racial Ethn Health Disparities. 2021:1–13. 10.1007/s40615-021-01037-0. [DOI] [PMC free article] [PubMed]
- 35.Bohra N. Language barriers, technology hurdles and limited transportation hurt Asian American Texans’ access to vaccines. Available at: https://www.texastribune.org/2021/03/19/asian-americans-texas-language-vaccine/. Accessed 16 June 2021.
- 36.Tseng A. Not all Asian Americans are being vaccinated at high rates. A Chinatown clinic shows why. Available at: https://www.latimes.com/california/story/2021-04-21/chinatown-vaccine-clinic-asian-american-seniors. Accessed 16 June 2021.
- 37.McElfish PA, Cleek AB, Willis DE, Purvis RS, James LP. Leveraging community engagement capacity to address COVID-19 disparities among Pacific Islander and Latinx Communities in Arkansas. J Clin Transl Sci. 2021;5(1):e81. doi: 10.1017/cts.2020.562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wieland ML, Asiedu GB, Lantz K, et al. Leveraging community engaged research partnerships for crisis and emergency risk communication to vulnerable populations in the COVID-19 pandemic. J Clin Transl Sci. 2021;5(1):e6. doi: 10.1017/cts.2020.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Akintobi TH, Jacobs T, Sabbs D, et al. Community engagement of African Americans in the era of COVID-19: considerations, challenges, implications, and recommendations for public health. Prev Chronic Dis. 2020;17:E83. doi: 10.5888/pcd17.200255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Abdul-Mutakabbir JC, Casey S, Jews V, et al. A three-tiered approach to address barriers to COVID-19 vaccine delivery in the Black community. Lancet Glob Health. 2021;9(6):e749–e750. doi: 10.1016/S2214-109X(21)00099-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Peek ME, Simons RA, Parker WF, et al. COVID-19 among African Americans: an action plan for mitigating disparities. Am J Public Health. 2021;111(2):286–292. doi: 10.2105/AJPH.2020.305990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ojikutu BO, Stephenson KE, Mayer KH, et al. Building trust in COVID-19 vaccines and beyond through authentic community investment. Am J Public Health. 2021;111(3):366–368. doi: 10.2105/AJPH.2020.306087. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.
Not applicable.