SARS-CoV-2, as well as the measures that were taken around the world to limit its spread, has killed thousands of people and ruined industries and economies. Vigorous vaccination campaigns are being pursued in the hope of ending the pandemic. However, many people are afraid of vaccination side effects, and one of these suspected side effects is female infertility due to vaccine-induced autoreactive antibodies against Syncytin-1 [1]. The spike protein of SARS-CoV-2, which is the main target of all vaccination schemes, shares homology to Syncytin-1. Syncytin-1 enables the fusion of trophoblasts to syncytiotrophoblasts, cells that are essential for placenta formation, an early step in the establishment of a pregnancy [2, 3].
This concern was widely refuted by major media such as the New York Times [4] and in the scientific literature [5]. The most commonly used argument of critics is that the emergence of crossreactive antibodies would be unlikely due to the limited homology between the SARS-CoV-2 spike protein and Syncytin-1. However, this argument is not convincing, as the epitope recognized by an antibody can be as small as four amino acids [6]. To provide a scientific basis for a rational discussion about this question, we investigated the crossreactivity of anti-spike protein antibodies with Syncytin-1.
Based on an EMBOSS water pairwise analysis, the overall amino acid identity and similarity between Syncytin-1 and the SARS-CoV-2 spike protein are only 8.8% and 15.8%, respectively. Moreover, SARS-CoV-2 spike is much larger than Syncytin-1. If the comparison is focused on the region (amino acid 576–1196) that corresponds to smaller Syncytin-1 (538 amino acids), the amino acid identity and similarity increase to 16.8% and 30.2%, respectively. Although these numbers are low, they are deceiving because there are clusters with high degrees of homology (Supplementary Fig. 1A). Furthermore, it needs to be considered that the tertiary structure is more relevant than the primary sequence homology. Indeed, the two domains for which crystallography data are available show a highly similar 3D structure (Supplementary Fig. 1D and Supplementary Video 1). Given that the epitope that an antibody recognizes is typically 5–8 amino acids but can be as small as 4 [6], it is quite possible that antibodies against the SARS-CoV-2 spike protein crossreact with highly homologous clusters in Syncytin-1.
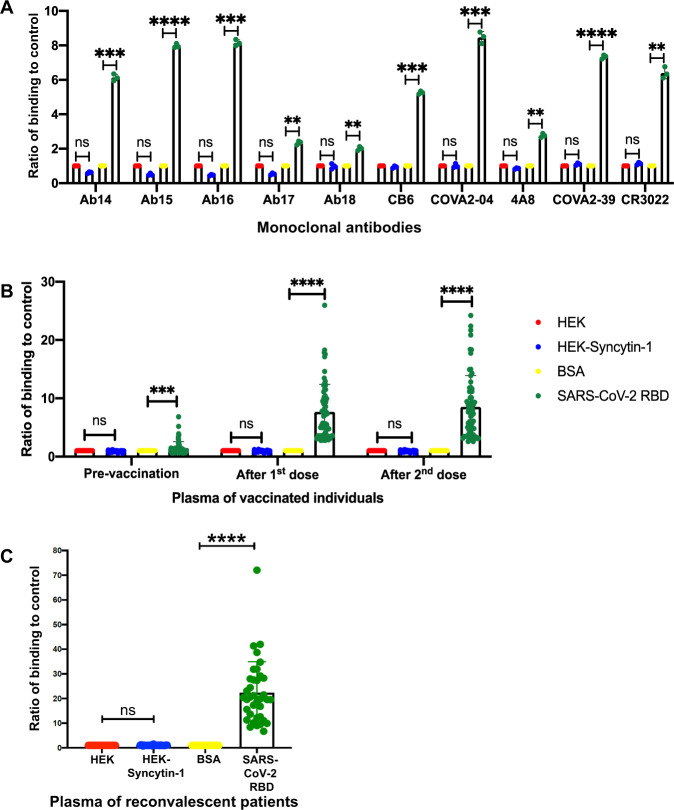
Monoclonal antibodies against the SARS-CoV-2 spike protein have been proposed as a way to treat COVID-19 patients and are currently being evaluated in clinical trials [7]. To reliably assess the presence of anti-Syncytin-1 reactivity, we generated a stable HEK293 cell line expressing Syncytin-1 on the cell surface (Supplementary Fig. 2). In an in-cell ELISA using HEK293 cells expressing Syncytin-1 and control HEK293 cells, none of the 10 monoclonal antibodies tested crossreacted with Syncytin-1 (Fig. 1A). As a control, the specificity of the monoclonal antibodies against spike was verified by testing their reactivity to a recombinant SARS-CoV-2 spike receptor-binding domain (RBD) (Fig. 1A).
Fig. 1. Anti-spike protein antibodies do not bind to Syncytin-1.
Ratio of the optical density (O.D.) values of binding of the indicated antibodies versus controls. HEK WT cells were used as a control for binding to HEK-Syncytin-1 cells; BSA is a control for SARS-CoV-2 receptor-binding domain (RBD). (A) Monoclonal antibodies. Each dot represents one technical replicate. B Plasma from vaccinated individuals, as collected pre-vaccination, 21 days after the 1st dose, and 2 months after the 2nd dose. Each dot represents one plasma sample. C Plasma of SARS-CoV-2 convalescent patients collected 28 days post-recovery. Each dot represents one plasma sample. Data representative from one experiment with 3 technical replicates per sample. Depicted are means ± standard deviations; ns not significant, **p < 0.01, ***p < 0.001, ****p < 0.0001 as determined by a two-sided Student’s t test.
To determine whether SARS-CoV-2 vaccination leads to the production of anti-Syncytin-1 antibodies, we analyzed plasma from 66 individuals collected at 3 different time points: prevaccination, 21 days after the first dose, and 2 months after the second dose; binding between the spike protein RBD and plasma components was verified as a positive control (Fig. 1B). We did not detect any crossreactivity with Syncytin-1 in the plasma of vaccinated individuals, in either the pre- or postvaccination samples, despite an increase in anti-spike protein titers (Fig. 1B). To determine whether SARS-CoV-2 infection induces antibodies against Syncytin-1, we tested the plasma of 37 COVID-19 patients collected at 28 days post recovery, and no anti-Syncytin-1 antibodies were detected in the plasma of these recovalescent patients (Fig. 1C). These results lead us to conclude that there is no - or at least no major - danger of female infertility due to the induction of Syncytin-1 crossreacting antibodies.
Our data are in line with findings from accidental pregnancies in COVID-19 vaccine trials in the United Kingdom. Their analysis demonstrated (1) no difference in the rate of accidental pregnancies between vaccinated and unvaccinated women and (2) no increased miscarriage rate [5]. Another recent study could not find evidence for an increased frequency of preterm delivery or fetal loss in women vaccinated during their pregnancy, suggesting that COVID-19 vaccines do not result in pregnancy disruption [8].
To our knowledge, this is the first study that experimentally addresses the question of whether vaccination against the SARS-CoV-2 spike protein induces antibodies against Syncytin-1. We did not detect crossreactivity between anti-SARS-CoV-2 spike protein antibodies and Syncytin-1.
Supplementary information
Acknowledgements
This study was funded by the Ministry of Education, Singapore (MOE2019‐T2‐2‐087). Plasma samples were collected in accordance with the Helsinki declaration after written consent from volunteers under an approved Institutional Review Board protocol NUS-IRB REF NO: LH-20-013.
Author contributions
J.L.L. generated the Syncytin-1-expressing cell line and performed the homology analysis of Syncytin-1 and the spike protein. M.P. measured anti-Syncytin-1 reactivity. Y.G. and R.G. measured anti-SARS-CoV-2 RBD protein reactivity. P.A.M. organized the plasma samples and supervised the study. H.S. wrote the paper and supervised the study.
Competing interests
The authors declare no competing interests.
Footnotes
These authors contributed equally: Mukul Prasad, Jia Le Lin.
Supplementary information
The online version contains supplementary material available at 10.1038/s41423-021-00773-x.
References
- 1.Wodrag W, Yeadon M. Petition/motion for administrative/regulatory action regarding confirmation of efficacy end points and use of data in connection with the following clinical trial(s). 2020. https://2020news.de/wp-content/uploads/2020/12/Wodarg_Yeadon_EMA_Petition_Pfizer_Trial_FINAL_01DEC2020_EN_unsigned_with_Exhibits.pdf.
- 2.Gallaher B. Response to nCoV2019 Against Backdrop of Endogenous Retroviruses. 2020. http://virological.org/t/response-to-ncov2019-against-backdrop-of-endogenous-retroviruses/396.
- 3.Lavillette D, Marin M, Ruggieri A, Mallet F, Cosset FL, Kabat D. The envelope glycoprotein of human endogenous retrovirus type W uses a divergent family of amino acid transporters/cell surface receptors. J Virol. 2002;76:6442–52. doi: 10.1128/jvi.76.13.6442-6452.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lu-Culligan, AIA;. in New York Times (26 Jan 2021) 2021. https://www.nytimes.com/2021/01/26/opinion/covid-vaccine-rumors.html.
- 5.Male V. Are COVID-19 vaccines safe in pregnancy? Nat Rev Immunol. 2021;21:200–1. doi: 10.1038/s41577-021-00525-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Buus S, Rockberg J, Forsström B, Nilsson P, Uhlen M, Schafer-Nielsen C. High-resolution mapping of linear antibody epitopes using ultrahigh-density peptide microarrays. Mol Cell Proteom. 2012;11:1790–1800. doi: 10.1074/mcp.M112.020800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Taylor PC, Adams AC, Hufford MM, de la Torre I, Winthrop K, Gottlieb RL. Neutralizing monoclonal antibodies for treatment of COVID-19. Nat Rev Immunol. 2021;21:382–93. doi: 10.1038/s41577-021-00542-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shanes ED, Otero S, Mithal LB, Mupanomunda CA, Miller ES, Goldstein JA. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) vaccination in pregnancy: measures of immunity and placental histopathology. Obstet Gynecol. 2021;138:281–3. doi: 10.1097/AOG.0000000000004457. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.