Abstract
Rationale: Limited data suggest racial disparities in continuous positive airway pressure (CPAP) adherence exist.
Objectives: To assess whether CPAP adherence varies by neighborhood racial composition at a national scale.
Methods: Telemonitoring data from a CPAP manufacturer database were used to assess adherence in adult patients initiating CPAP therapy between November 2015 and October 2018. Mapping ZIP code to ZIP code tabulation areas, age- and sex-adjusted CPAP adherence data at a neighborhood level was computed as a function of neighborhood racial composition. Secondary analyses adjusted for neighborhood education and poverty.
Measurements and Main Results: Among 787,236 patients living in 26,180 ZIP code tabulation areas, the prevalence of CPAP adherence was 1.3% (95% confidence interval [CI], 1.0–1.6%) lower in neighborhoods with high (⩾25%) versus low (<1%) percentages of Black residents and 1.2% (95% CI, 0.9–1.5%) lower in neighborhoods with high versus low percentages of Hispanic residents (P < 0.001 for both), even after adjusting for neighborhood differences in poverty and education. Mean CPAP usage was similar across neighborhoods for the first 2 days, but by 90 days, differences in CPAP usage increased to 22 minutes (95% CI, 18–27 min) between neighborhoods with high versus low percentages of Black residents and 22 minutes (95% CI 17–27 min) between neighborhoods with high versus low percentages of Hispanic residents (P < 0.001 for both).
Conclusions: CPAP adherence is lower in neighborhoods with greater proportions of Black and Hispanic residents, independent of education or poverty. These differences lead to a lower likelihood of meeting insurance coverage requirements for CPAP therapy, potentially exacerbating sleep health disparities.
Keywords: CPAP adherence, neighborhood, disparities, Black, Hispanic
At a Glance Commentary
Scientific Knowledge on the Subject
Treatment of obstructive sleep apnea is limited by adherence with the most common therapeutic option—continuous positive airway pressure (CPAP). Prior research suggests that Black Americans have lower rates of CPAP adherence, but this work has been limited by focusing on patients seeking care at academic medical centers or participating in clinical research. Data on disparities in CPAP adherence among Hispanic Americans are mixed.
What This Study Adds to the Field
Using a nationally representative telemonitoring database, we demonstrate that, independent of measures of poverty or education, residents of neighborhoods with either a high proportion of Black residents or a high proportion of Hispanic residents have lower rates of CPAP adherence compared with those residing in neighborhoods with low minority populations. Although CPAP usage was similar across residents of neighborhoods with high and low Black and Hispanic proportions over the first 2 days after CPAP initiation, differences emerged by 7 days and were more severe by 90 days. These results demonstrate that racial disparities in sleep apnea treatment exist. Dedicated efforts are required to develop and implement interventions to minimize these inequities.
Obstructive sleep apnea (OSA) is a highly prevalent disease that is an independent risk factor for hypertension, heart failure, and stroke (1). In the United States, Black and Hispanic individuals are at greater risk for these cardiovascular diseases, making effective treatment of OSA in minority populations a priority to promote health equity (2).
Small, single-center studies have suggested that Black patients with OSA initiated on continuous positive airway pressure (CPAP) therapy have lower adherence compared with White patients (3–5). However, these studies focus on patients served by academic medical centers, limiting generalizability. Research on CPAP adherence disparities in Hispanic patients has been less consistent, but again prior studies have been limited by small sample sizes at specialized centers of care (6). Given increasing evidence of structural barriers to health care, disparities at the community level likely contribute to racial disparities in OSA but will not be fully captured by single-site analyses.
To address sleep health disparities and improve health equity in OSA-related comorbidities, it is imperative to understand disparities in CPAP adherence. Therefore, we performed an ecologic analysis to determine whether CPAP adherence varies by neighborhood minority composition using a large national database of remotely monitored CPAP usage data.
Methods
CPAP adherence data were obtained from Encore Anywhere, a database developed to facilitate management of patients initiated on CPAP therapy with a Philips Respironics device. Demographic information was entered by the durable medical equipment (DME) company caring for each patient. We limited our analysis to patients who began using a CPAP machine between November 1, 2015, and October 31, 2018, as this is a timeframe during which DME companies were regularly using telemonitoring as the standard of care. We limited the study population to those initiated on either fixed or autotitrating CPAP devices with at least 30 seconds of CPAP usage who were aged 18–90 years, had nonmissing sex, and had a valid U.S. five-digit ZIP code, as previously described (7). Because of the deidentified nature of the dataset, the University of Pittsburgh institutional review board deemed this research to be exempt from human subjects research review.
Daily usage levels were used to calculate mean hours of CPAP use across the first 2, 7, and 90 days. Days with missing usage were imputed as 0 hours of use. CPAP adherence was defined by Centers for Medicare and Medicaid Services (CMS) criteria (⩾4 h of use per night on ⩾70% of nights during a consecutive 30-day period within the first 90 d from initiation) (8). Mean hours of CPAP use, percentage of days with no use, and percentage of users meeting CMS criteria were adjusted for age and sex.
Neighborhood data were derived from U.S. census block information by mapping five-digit ZIP codes to ZIP code tabulation areas (ZCTAs) using a publicly available mapping source (9). Demographic information for each ZCTA was obtained from the 2014–2018 American Community Survey 5-year estimates made available by the U.S. Census Bureau (10). Neighborhood characteristics extracted included the number of adult residents, percentage of adult residents who were Black, percentage of adult residents who were Hispanic, percentage of adult residents whose household income was below the poverty threshold, and percentage of adult residents without a bachelor’s degree.
Neighborhood demographic characteristics were categorized to correspond roughly with quintiles. Both the percentage of Black adults and the percentage of Hispanic adults in each ZCTA were categorized as <1.0%, 1.0–2.4%, 2.5–9.9%, 10.0–24.9%, and ⩾25.0%. In addition, the proportion of Black adults and the proportion of Hispanic adults were modeled continuously. The percentage of adults living below the poverty line was categorized as ⩽5.0%, 5.1–10.0%, 10.1–15.0%, 15.1–24.9%, and ⩾25%. The percentage of adults without a bachelor’s degree was categorized as ⩽50.0%, 50.1–75.0%, 75.1–85.0%, 85.1–90.0%, and >90.0%.
We restricted analyses to ZCTAs with at least 100 residing adults to ensure reasonably precise estimates of neighborhood demographics. Our primary analyses included all ZCTAs with at least one CPAP user. In sensitivity analyses, we restricted analyses to those ZCTAs with greater than 10 CPAP users to allow for more precise estimates of mean adherence levels within each ZCTA.
Linear regression was used to assess the association between neighborhood demographics and CPAP usage across ZCTAs. All analyses were conducted in Stata 16.0 (StataCorp). Further details are in the online supplement.
Results
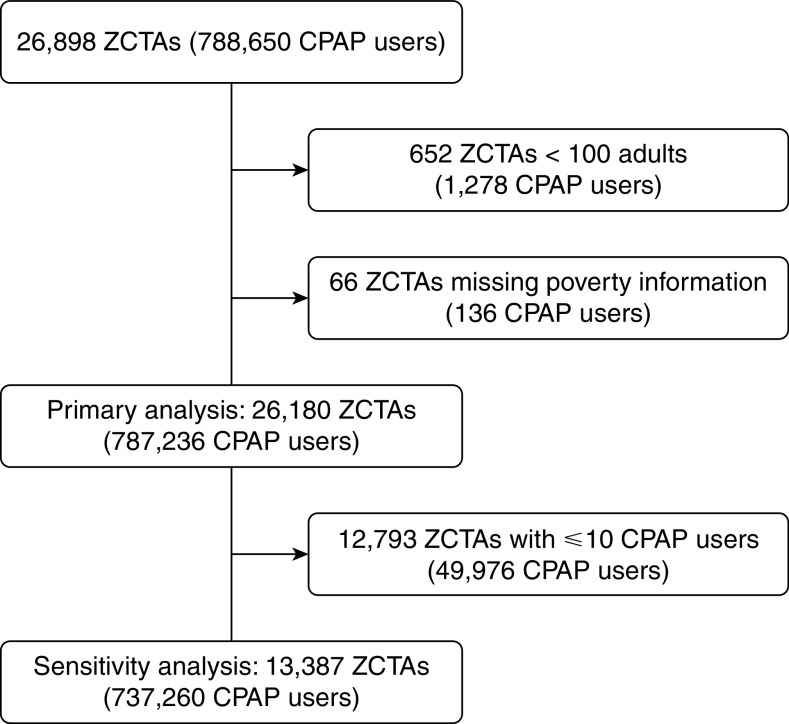
Data from 788,650 eligible individuals initiating CPAP therapy were available for analysis. These individuals’ ZIP codes mapped onto 26,898 unique ZCTAs (Figure 1). A total of 718 ZCTAs representing data from 1,414 patients were excluded from analysis because they had fewer than 100 adult residents or because poverty data were unavailable. This left 26,180 unique ZCTAs with 787,236 CPAP users in the primary analysis. Overall, 98% of the noninstitutionalized adult population of the United States reside in these 26,180 ZCTAs, covering all regions of the United States. Sensitivity analyses were performed that were limited to ZCTAs with more than 10 CPAP users to restrict to those ZCTAs with more precise estimates of CPAP use. There were 737,260 CPAP users residing in 13,387 ZCTAs included in the sensitivity analysis. This subset of ZCTAs accounts for 84% of the overall U.S. adult population. The age, sex, and socioeconomic measures of the ZCTAs included in this analysis reflected those of the United States overall, although the median population size of the included ZCTAs tended to be larger with greater proportions of Black and Hispanic residents as compared with the full distribution of ZCTAs across the nation (Table 1).
Figure 1.
Selection of the ZIP code tabulation areas (ZCTAs) included in the analyses of neighborhood demographics and continuous positive airway pressure (CPAP) adherence. Zip codes from all individuals initiated on CPAP therapy in the Philips Encore database between November 1, 2015, and October 31, 2018, were mapped onto ZCTAs. The analyses between neighborhood demographics and CPAP use included ZCTAs belonging to the 50 U.S. states and the District of Columbia with at least 100 adult residents, available poverty data, and at least one CPAP user in the database. The sensitivity analyses included only ZCTAs with more than 10 CPAP users.
Table 1.
Characteristics of ZCTAs Included in Analyses of the Association between Neighborhood Demographics and CPAP Adherence
| Primary Analysis (N = 26,180) | Sensitivity Analysis (N = 13,387) | All ZCTAs (N = 31,044) | |
|---|---|---|---|
| Adult residents per ZCTA | 3,815 (1,093–14,006) | 12,327 (2,969–23,075) | 2,550 (724–11,264 |
| Male adults, % | 49.0 (47.2–51.1) | 48.5 (47.1–50.1) | 49.1 (47.2–51.5) |
| Adults aged 65 or older, % | 20.7 (16.8–24.6) | 22.1 (17.6–26.8) | 22.3 (17.6–27.3) |
| Black adults, % | 1.5 (0.0–8.1) | 3.8 (1.0–12.7) | 1.1 (0.0–7.0) |
| Hispanic adults, % | 3.0 (0.9–8.7) | 4.7 (1.9–12.5) | 2.8 (0.7–8.2) |
| Adults without a bachelor’s degree, % | 81.0 (70.1–87.1) | 77.5 (64.3–85.0) | 81.6 (71.5–87.8) |
| Household income, $ | 54,600 (43,600–69,900) | 54,200 (43,300–68,500) | 57,800 (45,600–77,000) |
| Adults living below the poverty line, % | 10.8 (6.7–16.3) | 10.5 (6.6–15.8) | 10.8 (6.6–16.4) |
| Geographic region, n (%) | |||
| Northeast | 5,159 (19.7) | 2,986 (22.3) | 5,753 (18.5) |
| Southeast | 5,779 (22.1) | 3,308 (24.7) | 6,479 (20.9) |
| Midwest | 8,257 (31.5) | 3,255 (24.3) | 10,460 (33.7) |
| South Central | 2,987 (11.4) | 1,549 (11.6) | 3,467 (11.2) |
| Mountain West | 1,506 (5.8) | 780 (5.8) | 1,990 (6.4) |
| West Coast | 2,492 (9.5) | 1,509 (11.3) | 2,895 (9.2) |
| Number of CPAP users per ZCTA | 11 (3–36) | 35 (19–68) | — |
Definition of abbreviations: CPAP = continuous positive airway pressure; ZCTA = ZIP code tabulation area.
Median and interquartile range of demographic characteristics of ZCTAs included in analyses of the association between neighborhood demographics and CPAP adherence. The primary analysis included all ZCTAs in the 50 U.S. states plus the District of Columbia with 100 adult residents and at least one individual initiating CPAP between November 1, 2015, and October 31, 2018, in the Philips Encore database. The sensitivity analysis were restricted to those ZCTAs with more than 10 CPAP users. Data on all ZCTAs in the 50 U.S. states plus the District of Columbia with 100 adult residents are provided as a reference.
The median adult population of the ZCTAs included in the primary analysis was 3,815 residents (interquartile range [IQR], 1,093–14,006) (Table 1). The median number of CPAP users in the manufacturer database per ZCTA was 11 users (IQR, 3–36). Although the median percentages of Black and Hispanic residents were low overall, there were still a sizable number of ZCTAs with ⩾25% Black (2,785 ZCTAs) and Hispanic (2,416 ZCTAs) residents. The correlation between the percentages of Black and Hispanic residents across ZCTAs was low (r = 0.03). Similarly, all correlations between race and socioeconomic measures were low, with the strongest correlation observed between education and poverty measures (r = 0.40).
Overall, mean (SD) age- and sex-adjusted CPAP adherence was 72.6 ± 4.6%, and mean 90-day CPAP use was 4.7 ± 1.3 hours across ZCTAs. Similar values were obtained (72.3 ± 2.5% and 4.6 ± 0.7 h) in the sensitivity analysis.
CPAP Adherence by Neighborhood Composition
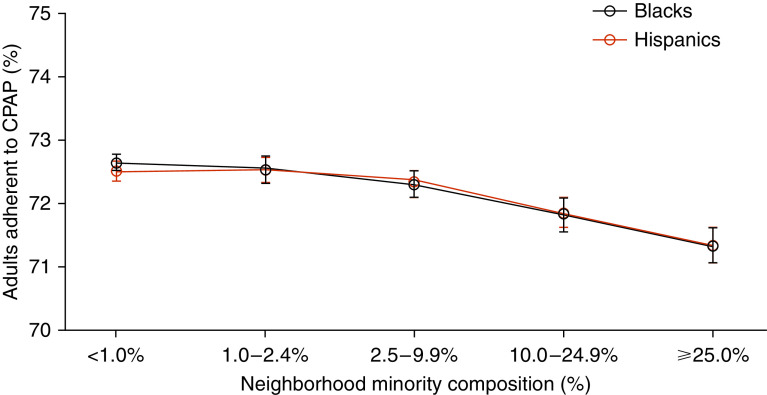
We found a steady decline in CPAP adherence as the proportion of Black residents in ZCTAs increased. The prevalence of CPAP adherence was 1.7% (95% confidence interval [CI], 1.4–2.0%) lower in ZCTAs with high (⩾25%) compared with low (<1%) percentages of Black residents (71.6% vs. 73.2%; P < 0.001). A significant difference persisted between lowest and highest quintile (1.3%; 95% CI, 1.0–1.6%) after adjustment for Hispanic composition, neighborhood poverty, and education (Figure 2 and Table E1 in the online supplement). The difference was even greater at 2.3% (95% CI, 2.1–2.4%) in sensitivity analyses restricted to ZCTAs with greater than 10 CPAP users (70.8% vs. 73.1%; P < 0.001; Figure E1). When modeled continuously and when other neighborhood characteristics were adjusted for, every 10% increase in the proportion of Black residents living in a ZCTA was associated with a 0.26% (95% CI, 0.21–0.32%) lower proportion achieving CMS adherence. In the sensitivity analysis, every 10% increase in the proportion of Black residents living in a ZCTA was associated with a 0.44% (95% CI, 0.41–0.46%) lower proportion achieving CMS adherence.
Figure 2.
Association of neighborhood minority composition and continuous positive airway pressure (CPAP) adherence across all ZIP code tabulation areas (ZCTAs) with at least one CPAP user. Mean prevalence of age- and sex-adjusted CPAP adherence based on Centers for Medicare and Medicaid Services criteria as a function of the percentage of Black and Hispanic adults living in each ZCTA with at least one CPAP user, adjusted for the percentage of Black adults, Hispanic adults, adults living below the poverty line, and adults without a bachelor’s degree. Error bars display 95% confidence intervals.
A similar pattern was observed with neighborhood Hispanic residential composition (Figure 2 and Table E1). The difference in CPAP adherence between ZCTAs with highest versus lowest percentages of Hispanic residents was 1.5% (95% CI, 1.2–1.8%), which remained significant at 1.2% (95% CI, 0.9–1.5%) in analyses adjusted for Black composition, poverty, and education (71.3% vs. 72.5% vs. 71.3%; P < 0.001). This adjusted difference was 2.4% (95% CI, 2.2–2.5%) in sensitivity analyses (70.6% vs. 73.0%; P < 0.001). When modeled continuously, every 10% increase in the proportion of Hispanic residents living in a ZCTA was associated with a 0.25% (95% CI, 0.20–0.31%) lower proportion achieving CMS adherence in the primary analysis and a 0.50% (95% CI, 0.47–0.53%) lower proportion achieving CMS adherence in the sensitivity analysis.
CPAP Use over Time by Neighborhood Composition
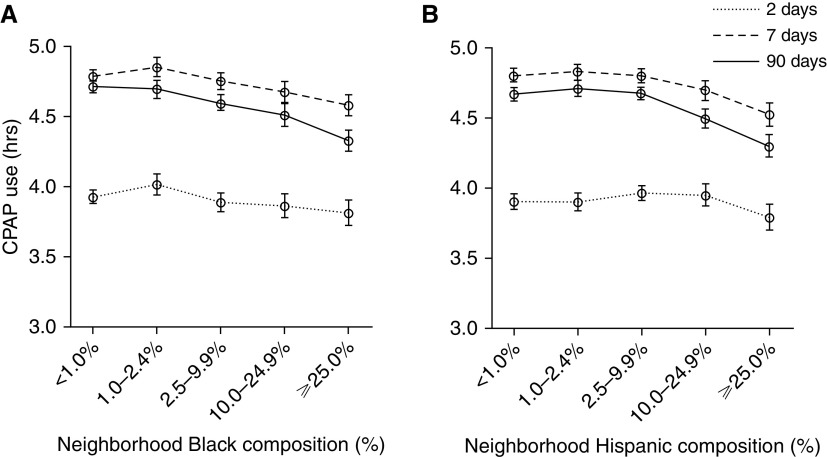
Although similar rates of CPAP use were observed across ZCTAs in the initial 2 days, differences were evident by 7 days and grew larger by 90 days. Comparing neighborhoods with ⩾25% with neighborhoods with <1% Black residents, the difference in usage was 7 minutes (95% CI, 1–13 min) at 2 days (3.8 vs. 3.9 h; P = 0.02), widening to 13 minutes (95% CI, 8–18 min) at 7 days (4.6 vs. 4.8 h; P < 0.001) and climbing to 22 minutes (95% CI, 18–27 min) at 90 days (4.3 vs. 4.7 h; P < 0.001) in analyses adjusting for Hispanic composition, poverty, and education (Figure 3). Between ZCTAs with the highest and lowest percentages of Black residents in the sensitivity analysis, differences in mean nightly CPAP use were 10 minutes (95% CI, 7–12 min) at 2 days, 24 minutes (95% CI, 21–26 min) at 7 days, and 37 minutes (95% CI, 34–39 min) at 90 days.
Figure 3.
Association of neighborhood minority composition and mean nightly use of continuous positive airway pressure (CPAP) over time across all ZIP code tabulation areas (ZCTAs) with at least one CPAP user. Age- and sex-adjusted mean nightly use of CPAP averaged over the initial 2, 7, and 90 days by (A) neighborhood Black resident composition and (B) neighborhood Hispanic resident composition across ZCTAs with at least one CPAP user. Analyses are adjusted for adults living below the poverty line, adults without a bachelor’s degree, and percentage of (A) Hispanic adults and (B) Black adults. Error bars display 95% confidence intervals.
The pattern of decline in CPAP use over time was similar across quintiles of Hispanic resident composition (Figure 3). At 2 days, mean nightly CPAP usage in ZCTAs with ⩾25% Hispanic residents was 6 minutes (95% CI, 0–13 min) lower than in ZCTAs with <1% Hispanic residents (3.8 vs. 3.9 h; P = 0.04). This difference increased to 17 minutes (95% CI, 11–22 min) at 7 days (4.5 vs. 4.8 h; P < 0.001) and 22 minutes (95% CI, 17–27 min) at 90 days (4.3 vs. 4.7 h; P < 0.001). In the sensitivity analysis, these differences were 8 minutes (95% CI, 5–11 min), 31 minutes (95% CI, 28–33 min), and 39 minutes (95% CI, 37–42 min) at 2, 7, and 90 days, respectively.
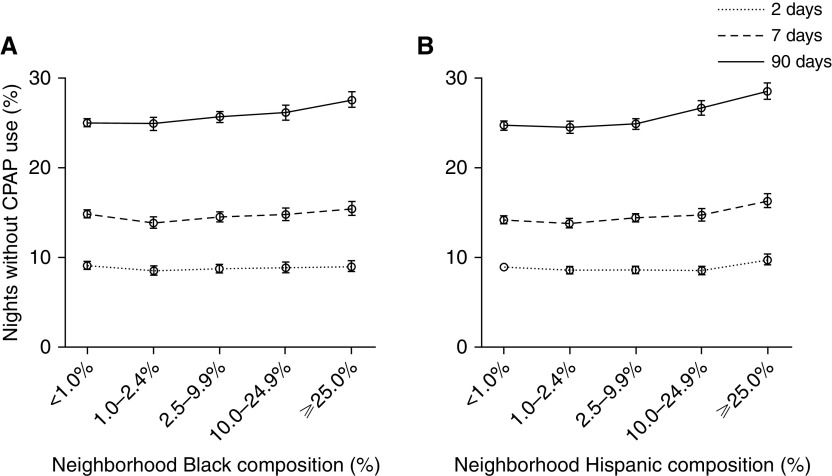
CPAP Nonuse by Neighborhood Composition
Over the initial 3 months of CPAP use, both neighborhoods with the greatest proportion of Black residents and those with the greatest proportion of Hispanic residents had a higher prevalence of nights without CPAP use compared with neighborhoods with the lowest proportions of these groups (Figure 4). The percentage of nights over the first 90 days with no CPAP use between neighborhoods with ⩾25% compared with <1% Black residents was 27.7% versus 25.1%, for a net difference of 2.6% (95% CI, 1.7–3.5%, P < 0.001). Similarly, the percentage of nights over the first 90 days with no CPAP use in neighborhoods with the highest and lowest proportions of Hispanic residents was 28.6% versus 24.8%, for a net difference of 3.8% (95% CI, 2.8–4.8%; P < 0.001).
Figure 4.
Association of neighborhood minority composition and nonuse of continuous positive airway pressure (CPAP) over time across all ZIP code tabulation areas (ZCTAs) with at least one CPAP user. Mean prevalence of age- and sex-adjusted CPAP nonuse over the initial 2, 7, and 90 days by (A) neighborhood Black resident composition and (B) neighborhood Hispanic resident composition across ZCTAs with at least one CPAP user. Analyses are adjusted for adults living below the poverty line, adults without a bachelor’s degree, and percentage of (A) Hispanic adults (B) Black adults. Error bars display 95% confidence intervals.
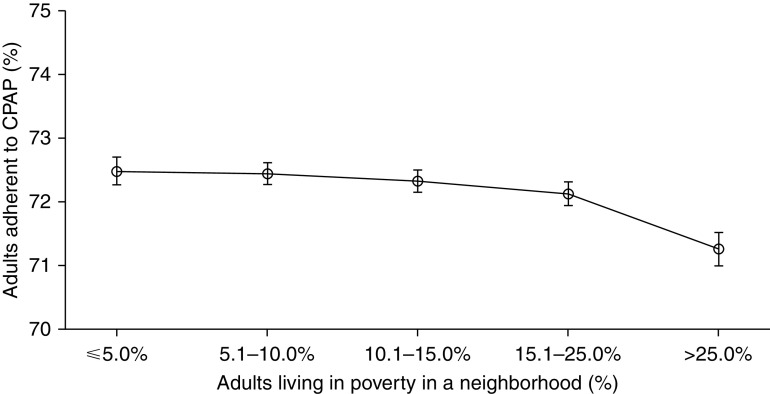
CPAP Use and Adherence by Neighborhood Poverty and Education Level
Greater neighborhood poverty was independently associated with reduced CPAP adherence (Figure 5 and Table E2). In analyses adjusting for race and education, ZCTAs with ⩾25% adults living below the poverty line had a CPAP adherence prevalence that was 1.2% (95% CI, 0.9–1.6%) lower than that of ZCTAs with <5% adults living below the poverty line (71.3% vs. 72.5%; P < 0.001). In contrast, neighborhood education level did not have a consistent trend in CPAP adherence after adjusting for racial composition and poverty (Figure E2 and Table E2).
Figure 5.
Association of neighborhood poverty prevalence and continuous positive airway pressure (CPAP) adherence across all ZIP code tabulation areas (ZCTAs) with at least one CPAP user. Mean prevalence of age- and sex-adjusted CPAP adherence based on Centers for Medicare and Medicaid Services criteria as a function of the percentage of adults living in poverty in each ZCTA with at least one CPAP user adjusted for the percentage of Black adults, Hispanic adults, and adults without a bachelor’s degree. Error bars display 95% confidence intervals.
Discussion
Using a national database, we found that CPAP adherence is lower in patients living in neighborhoods with a greater composition of either Black or Hispanic residents. The prevalence of CPAP adherence steadily declined as the percentage of neighborhood inhabitants who are Black or Hispanic increased. This association was not fully explained by differences in neighborhood levels of poverty and education. Differences in CPAP adherence prevalence were even greater in analyses limited to ZCTAs with more than 10 CPAP users.
The differences observed in 90-day CPAP use between neighborhoods with the highest prevalence and the lowest prevalence of minority residents were on the order of 30 minutes, a difference considered clinically meaningful based on the known dose–response relationships between CPAP use and improvements in sleepiness, quality of life, and blood pressure (11). Furthermore, because CMS policies deny CPAP coverage for patients who do not achieve 90-day adherence, a policy widely adopted by private payers, these differences likely translate into even greater disparities beyond 90 days, as greater proportions of patients in high-prevalence minority neighborhoods are denied long-term coverage of CPAP therapy (12, 13).
Our findings extend results from earlier studies that have reported consistently that Black patients have lower CPAP usage than White patients (6). Most prior studies have focused on patients receiving care at single-site academic sleep medical centers, which has limited generalizability to the majority of patients who receive care from community physicians. Focusing on a single center also minimizes variability in quality-of-care factors such as specialist versus nonspecialist management, which has been previously demonstrated to predict CPAP adherence (14). Although results from the HomePAP trial allowed for a multicenter analysis of race and CPAP adherence, the generalizability of those findings is uncertain given that the study focused on adherence within the context of a highly protocolized clinical trial with dedicated support staff (15). Studies investigating disparities in CPAP adherence among Hispanic patients have yielded mixed results, which likely reflect limitations due to small sample sizes, single centers, and differences in acculturation between cohorts compared with the national Hispanic population (6). A recent ecologic study using remote monitoring data did find lower CPAP usage levels in neighborhoods with greater proportions of Black and Hispanic residents, similar to our findings (16). Our study builds on earlier findings by restricting positive pressure device use to CPAP to focus analyses on patients with OSA and by narrowing analyses to a more recent timeframe, when remote monitoring has become standard of care, to reduce biases from earlier time periods, when DME providers were selective in which patients were remotely monitored.
Interestingly, we found that neighborhood differences in CPAP usage were minimal over the first 2 days but steadily grew over the subsequent 3 months. Although usage remained fairly constant from 7 days to 90 days in predominantly White neighborhoods, adherence declined over time in neighborhoods with a high prevalence of Black or Hispanic residents. These findings suggest similar motivation to use CPAP across neighborhoods initially but failure to sustain ongoing use in neighborhoods with greater minority composition. Furthermore, the differences in mean nightly CPAP use appear driven in large part by increased rates of nonuse, suggesting that patients with OSA in neighborhoods with greater minority composition are more likely to abandon CPAP therapy.
The reasons underlying the observed racial and ethnic differences in adherence almost certainly include factors at both the community and individual level. The historical legacy of structural racism, including discriminatory housing and lending policies, has led to residential segregation, whereby minority populations reside disproportionately in neighborhoods characterized by a lack of resources and high prevalence of external stressors (17). The resulting cumulative stress associated with residing in such neighborhoods diminishes the ability to adhere to medical treatments in general because of competing priorities (18). In addition, more OSA-specific effects may exist at a neighborhood level (19). Minority communities are more likely to be disadvantaged by the inequitable distribution of healthcare resources, including lesser likelihood of receiving their sleep apnea care from a sleep specialist (20, 21). Furthermore, DME providers, who deliver much of the education and troubleshooting early after CPAP initiation that has been demonstrated essential to improving long-term CPAP adherence, are inequitably distributed in the United States (22, 23). The ability to provide services in the patient’s preferred language is another important aspect of quality sleep health care, as data suggest lack of adequate interpreter services by both physicians and DME providers is a common barrier to care for Hispanic patients (24, 25). Air pollution is another potential neighborhood-level factor that may drive differences in CPAP adherence. Discriminatory housing practices have led minority neighborhoods to be more likely to exist in areas with greater amounts of air pollution and other toxins (26). Air pollution increases risk for chronic sinonasal disease, which in turn can contribute to poor CPAP adherence (27, 28).
On an individual level, mistrust of the medical system is much more common in minorities, in part because of the legacy of racism in the practice of medicine (29, 30). Although the relationship between medical mistrust and CPAP adherence has not been evaluated to date, adherence to prescribed medications and behavioral therapies is consistently lower in those with greater distrust of the healthcare system (31). Frequent change in sleeping location, as can occur with unstable housing, is another factor found to predict lower CPAP adherence among Black patients with OSA (32). In contrast, because the pattern of identified disparities appears to be related to increased abandonment of CPAP use rather than similar rates of use for shorter nightly durations, our findings suggest that the well-described racial differences in sleep duration were not an important driver for the CPAP adherence disparities observed (33, 34).
The relative importance of community-level versus individual-level factors to the observed disparities cannot be determined from this study, but research in other diseases, such as chronic obstructive pulmonary disease, suggests that both may be contributing (35). The striking similarity in CPAP adherence and nonuse trends over time between Black and Hispanic neighborhoods would argue for community-level factors playing a dominant role, with common upstream structural factors creating barriers for adherence in both communities.
Notably, the differences in CPAP use identified in this analysis likely underestimate the true magnitude of the disparities that exist at an individual level. Patients of a minority background with OSA are less likely to be diagnosed and offered treatment, and the financial barriers limiting CPAP acceptance disproportionately impact Black and Hispanic patients (36, 37). As a result, Black and Hispanic individuals are underrepresented among those contributing CPAP adherence data relative to the underlying composition of their neighborhood, which will skew the calculation of neighborhood averages toward the better adherence rates of White CPAP users.
Our findings have important implications. Black and Hispanic patients are at a much higher risk of consequences from untreated OSA, including higher burdens of excessive daytime sleepiness, drowsy driving, and cardiovascular morbidity and mortality (2, 38–40). As a result, these communities would potentially derive greater benefit from effective OSA treatment. Therefore, interventions to reduce the disparities in CPAP adherence identified would advance sleep health equity and decrease inequities in these downstream consequences. Further research to understand the causes of racial disparities in CPAP adherence will be vital to develop such interventions.
Our study has several limitations. First, our models are limited to data obtained from only one CPAP manufacturer. However, population-level 90-day adherence rates from a competing manufacturer are quite similar (41). Our ability to assess socioeconomic status and other sociologic measures was limited by the spatial granularity of our data, which were limited to five-digit ZIP codes mapped to the corresponding ZCTAs. Therefore, we were unable to effectively assess the impact of factors such as residential segregation or neighborhood deprivation, which require finer geospatial resolution (42). Similarly, we did not have access to individual-level data on race, ethnicity, socioeconomic status, or related measures, such as access to health care, to assess the relative importance of individual versus community-level factors on CPAP adherence. Lastly, no adjustments were made for CPAP pressure or leak so as to not bias against differences in quality of care, which may underlie the differences in CPAP use and abandonment observed.
In summary, across a nationally representative cohort of patients with OSA newly initiated on CPAP, we found that CPAP adherence is lower in neighborhoods with a greater prevalence of Black or Hispanic residents, and these differences cannot be explained by differences in education and poverty. These identified disparities will worsen inequities in downstream health effects of untreated or poorly treated OSA. Furthermore, insurance policies that tie CPAP coverage to adherence thresholds will further exacerbate these disparities. Unfortunately, there has been little research on individual and community factors that influence CPAP use in predominantly minority communities. A better understanding of interventions to minimize CPAP disparities in minority populations is needed together with policy reforms that minimize exacerbation of disparities.
Footnotes
Supported by a grant from Philips Respironics, the American Thoracic Society Academic Sleep Pulmonary Integrated Research/Clinical Fellowship, and NIH grants HL127307 and HL082610. S.R.P. has received grant funding through his university from Bayer Pharmaceuticals, Philips Respironics, and Respicardia. S.M.N. has received grant funding through his university from Philips Respironics.
Author Contributions: S.R.P. conceived the study. S.M.N. did the statistical analysis. P.V.B. wrote the first draft of the manuscript. J.P.B., C.J.S., and M.S.A. were involved with study design. E.C., U.R.E., and G.J.S. were involved with data interpretation and manuscript preparation. All authors critically reviewed this draft for important intellectual content and read and approved the final version. S.M.N. and S.R.P. had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
This article has an online supplement, which is accessible from this issue’s table of contents at www.atsjournals.org.
Originally Published in Press as DOI: 10.1164/rccm.202009-3685OC on March 9, 2021
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1. Somers VK, White DP, Amin R, Abraham WT, Costa F, Culebras A, et al. American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology; American Heart Association Stroke Council; American Heart Association Council on Cardiovascular Nursing; American College of Cardiology Foundation. Sleep apnea and cardiovascular disease: an American Heart Association/American College Of Cardiology Foundation scientific statement from the American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology, Stroke Council, and Council On Cardiovascular Nursing. In collaboration with the National Heart, Lung, and Blood Institute National Center on Sleep Disorders Research (National Institutes of Health) Circulation. 2008;118:1080–1111. doi: 10.1161/CIRCULATIONAHA.107.189375. [DOI] [PubMed] [Google Scholar]
- 2. Mensah GA, Mokdad AH, Ford ES, Greenlund KJ, Croft JB. State of disparities in cardiovascular health in the United States. Circulation. 2005;111:1233–1241. doi: 10.1161/01.CIR.0000158136.76824.04. [DOI] [PubMed] [Google Scholar]
- 3. Joo MJ, Herdegen JJ. Sleep apnea in an urban public hospital: assessment of severity and treatment adherence. J Clin Sleep Med. 2007;3:285–288. [PMC free article] [PubMed] [Google Scholar]
- 4. Balachandran JS, Yu X, Wroblewski K, Mokhlesi B. A brief survey of patients’ first impression after CPAP titration predicts future CPAP adherence: a pilot study. J Clin Sleep Med. 2013;9:199–205. doi: 10.5664/jcsm.2476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hsu N, Zeidler MR, Ryden AM, Fung CH. Racial disparities in positive airway pressure therapy adherence among veterans with obstructive sleep apnea. J Clin Sleep Med. 2020;16:1249–1254. doi: 10.5664/jcsm.8476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wallace DM, Williams NJ, Sawyer AM, Jean-Louis G, Aloia MS, Vieira DL, et al. Adherence to positive airway pressure treatment among minority populations in the US: a scoping review. Sleep Med Rev. 2018;38:56–69. doi: 10.1016/j.smrv.2017.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Patel SR, Bakker JP, Stitt CJ, Aloia MS, Nouraie SM. Age and sex disparities in adherence to CPAP. Chest. 2021;159:382–389. doi: 10.1016/j.chest.2020.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Centers for Medicare and Medicaid Services Atlanta, GA: Centers for Medicare and Medicaid Services; https://www.cms.gov/medicare-coverage-database/details/lcd-details.aspx?LCDId=33718&DocID=L33718. [PubMed] [Google Scholar]
- 9.American Academy of Family Physicians Leawood, KS: American Academy of Family Physicians; 2018https://www.udsmapper.org/. [Google Scholar]
- 10.United States Census Bureau. Suitland, MD: United States Census Bureau; 2019. [Google Scholar]
- 11. Patil SP, Ayappa IA, Caples SM, Kimoff RJ, Patel SR, Harrod CG. Treatment of adult obstructive sleep apnea with positive airway pressure: an American Academy of Sleep Medicine systematic review, meta-analysis, and GRADE assessment. J Clin Sleep Med. 2019;15:301–334. doi: 10.5664/jcsm.7638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Naik S, Al-Halawani M, Kreinin I, Kryger M. Centers for medicare and medicaid services positive airway pressure adherence criteria may limit treatment to many medicare beneficiaries. J Clin Sleep Med. 2019;15:245–251. doi: 10.5664/jcsm.7626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Brown LK. Use it or lose it: medicare’s new paradigm for durable medical equipment coverage? Chest. 2010;138:785–789. doi: 10.1378/chest.10-1168. [DOI] [PubMed] [Google Scholar]
- 14. Pamidi S, Knutson KL, Ghods F, Mokhlesi B. The impact of sleep consultation prior to a diagnostic polysomnogram on continuous positive airway pressure adherence. Chest. 2012;141:51–57. doi: 10.1378/chest.11-0709. [DOI] [PubMed] [Google Scholar]
- 15. Billings ME, Auckley D, Benca R, Foldvary-Schaefer N, Iber C, Redline S, et al. Race and residential socioeconomics as predictors of CPAP adherence. Sleep (Basel) 2011;34:1653–1658. doi: 10.5665/sleep.1428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Pandey A, Mereddy S, Combs D, Shetty S, Patel SI, Mashaq S, et al. Socioeconomic inequities in adherence to positive airway pressure therapy in population-level analysis. J Clin Med. 2020;9:442. doi: 10.3390/jcm9020442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Acevedo-Garcia D, Lochner KA, Osypuk TL, Subramanian SV. Future directions in residential segregation and health research: a multilevel approach. Am J Public Health. 2003;93:215–221. doi: 10.2105/ajph.93.2.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sabaté E. Adherence to long-term therapies: evidence for action. Geneva, Switzerland: World Health Organization; 2003. https://www.who.int/chp/knowledge/publications/adherence_report/en/ [Google Scholar]
- 19. Billings ME, Cohen RT, Baldwin CM, Johnson DA, Palen BN, Parthasarathy S, et al. Disparities in sleep health and potential intervention models: a focused review. Chest. 2021;159:1232–1240. doi: 10.1016/j.chest.2020.09.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Gaskin DJ, Dinwiddie GY, Chan KS, McCleary R. Residential segregation and disparities in health care services utilization. Med Care Res Rev. 2012;69:158–175. doi: 10.1177/1077558711420263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Wickwire EM, Jobe SL, Parthasarathy S, Collen J, Capaldi VF, II, Johnson A, et al. Which older adults receive sleep medicine specialty care? Predictors of being seen by a board-certified sleep medicine provider. J Clin Sleep Med. 2020;16:1909–1915. doi: 10.5664/jcsm.8722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Bakker JP, Weaver TE, Parthasarathy S, Aloia MS. Adherence to CPAP: what should we be aiming for, and how can we get there? Chest. 2019;155:1272–1287. doi: 10.1016/j.chest.2019.01.012. [DOI] [PubMed] [Google Scholar]
- 23.Dobson A, Heath S, Kilby D, Hu J, DaVanzo JE.Vienna, VA: Dobson DaVanzo & Associates, LLC; 2017https://www.aahomecare.org/uploads/userfiles/files/documents/Dobson%20DaVanzo%20Patient% 20Access%20Survey%20Final%20Report%2010_11_17_FINAL.pdf. [Google Scholar]
- 24. Diaz-Abad M, Chatila W, Lammi MR, Swift I, D’Alonzo GE, Krachman SL. Determinants of CPAP adherence in Hispanics with obstructive sleep apnea. Sleep Disord. 2014;2014:878213. doi: 10.1155/2014/878213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wilson E, Chen AH, Grumbach K, Wang F, Fernandez A. Effects of limited English proficiency and physician language on health care comprehension. J Gen Intern Med. 2005;20:800–806. doi: 10.1111/j.1525-1497.2005.0174.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Jones MR, Diez-Roux AV, Hajat A, Kershaw KN, O’Neill MS, Guallar E, et al. Race/ethnicity, residential segregation, and exposure to ambient air pollution: the Multi-Ethnic Study of Atherosclerosis (MESA) Am J Public Health. 2014;104:2130–2137. doi: 10.2105/AJPH.2014.302135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Velasquez N, Moore JA, Boudreau RM, Mady LJ, Lee SE. Association of air pollutants, airborne occupational exposures, and chronic rhinosinusitis disease severity. Int Forum Allergy Rhinol. 2020;10:175–182. doi: 10.1002/alr.22477. [DOI] [PubMed] [Google Scholar]
- 28. Inoue A, Chiba S, Matsuura K, Osafune H, Capasso R, Wada K. Nasal function and CPAP compliance. Auris Nasus Larynx. 2019;46:548–558. doi: 10.1016/j.anl.2018.11.006. [DOI] [PubMed] [Google Scholar]
- 29. Gamble VN. Under the shadow of Tuskegee: African Americans and health care. Am J Public Health. 1997;87:1773–1778. doi: 10.2105/ajph.87.11.1773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Halbert CH, Armstrong K, Gandy OH, Jr, Shaker L. Racial differences in trust in health care providers. Arch Intern Med. 2006;166:896–901. doi: 10.1001/archinte.166.8.896. [DOI] [PubMed] [Google Scholar]
- 31. Benkert R, Cuevas A, Thompson HS, Dove-Meadows E, Knuckles D. Ubiquitous yet unclear: a systematic review of medical mistrust. Behav Med. 2019;45:86–101. doi: 10.1080/08964289.2019.1588220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Liou HYS, Kapur VK, Consens F, Billings ME. The effect of sleeping environment and sleeping location change on positive airway pressure adherence. J Clin Sleep Med. 2018;14:1645–1652. doi: 10.5664/jcsm.7364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Lauderdale DS, Knutson KL, Yan LL, Rathouz PJ, Hulley SB, Sidney S, et al. Objectively measured sleep characteristics among early-middle-aged adults: the CARDIA study. Am J Epidemiol. 2006;164:5–16. doi: 10.1093/aje/kwj199. [DOI] [PubMed] [Google Scholar]
- 34. Chen X, Wang R, Zee P, Lutsey PL, Javaheri S, Alcántara C, et al. Racial/ethnic differences in sleep disturbances: the Multi-Ethnic Study of Atherosclerosis (MESA) Sleep (Basel) 2015;38:877–888. doi: 10.5665/sleep.4732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Ejike CO, Woo H, Galiatsatos P, Paulin LM, Krishnan JA, Cooper CB, et al. Contribution of individual and neighborhood factors to racial disparities in respiratory outcomes. Am J Respir Crit Care Med. doi: 10.1164/rccm.202002-0253OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Brin YS, Reuveni H, Greenberg S, Tal A, Tarasiuk A. Determinants affecting initiation of continuous positive airway pressure treatment. Isr Med Assoc J. 2005;7:13–18. [PubMed] [Google Scholar]
- 37. Dunietz GL, Chervin RD, Burke JF, Braley TJ. Obstructive sleep apnea treatment disparities among older adults with neurological disorders. Sleep Health. 2020;6:534–540. doi: 10.1016/j.sleh.2020.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Genuardi MV, Althouse AD, Sharbaugh MS, Ogilvie RP, Patel SR. Exploring the mechanisms of the racial disparity in drowsy driving. Sleep Health. 2018;4:331–338. doi: 10.1016/j.sleh.2018.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Carnethon MR, De Chavez PJ, Zee PC, Kim KY, Liu K, Goldberger JJ, et al. Disparities in sleep characteristics by race/ethnicity in a population-based sample: Chicago Area Sleep Study. Sleep Med. 2016;18:50–55. doi: 10.1016/j.sleep.2015.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Prasad B, Steffen AD, Van Dongen HPA, Pack FM, Strakovsky I, Staley B, et al. Determinants of sleepiness in obstructive sleep apnea. Sleep (Basel) 2018;41:zsx199. doi: 10.1093/sleep/zsx199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Cistulli PA, Armitstead J, Pepin JL, Woehrle H, Nunez CM, Benjafield A, et al. Short-term CPAP adherence in obstructive sleep apnea: a big data analysis using real world data. Sleep Med. 2019;59:114–116. doi: 10.1016/j.sleep.2019.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Riley AR. Neighborhood disadvantage, residential segregation, and beyond-lessons for studying structural racism and health. J Racial Ethn Health Disparities. 2018;5:357–365. doi: 10.1007/s40615-017-0378-5. [DOI] [PubMed] [Google Scholar]