Abstract
Rationale: Black race and Hispanic ethnicity are associated with increased risks for coronavirus disease (COVID-19) infection and severity. It is purported that socioeconomic factors may drive this association, but data supporting this assertion are sparse.
Objectives: To evaluate whether socioeconomic factors mediate the association of race/ethnicity with COVID-19 incidence and outcomes.
Methods: We conducted a retrospective cohort study of adults tested for (cohort 1) or hospitalized with (cohort 2) COVID-19 between March 1, 2020, and July 23, 2020, at the University of Miami Hospital and Clinics. Our primary exposure was race/ethnicity. We considered socioeconomic factors as potential mediators of our exposure’s association with outcomes. We used standard statistics to describe our cohorts and multivariable regression modeling to identify associations of race/ethnicity with our primary outcomes, one for each cohort, of test positivity (cohort 1) and hospital mortality (cohort 2). We performed a mediation analysis to see whether household income, population density, and household size mediated the association of race/ethnicity with outcomes.
Results: Our cohorts included 15,473 patients tested (29.0% non-Hispanic White, 48.1% Hispanic White, 15.0% non-Hispanic Black, 1.7% Hispanic Black, and 1.6% other) and 295 patients hospitalized (9.2% non-Hispanic White, 56.9% Hispanic White, 21.4% non-Hispanic Black, 2.4% Hispanic Black, and 10.2% other). Among those tested, 1,256 patients (8.1%) tested positive, and, of the hospitalized patients, 47 (15.9%) died. After adjustment for demographics, race/ethnicity was associated with test positivity—odds-ratio (95% confidence interval [CI]) versus non-Hispanic White for Non-Hispanic Black: 3.21 (2.60–3.96), Hispanic White: 2.72 (2.28–3.26), and Hispanic Black: 3.55 (2.33–5.28). Population density mediated this association (percentage mediated, 17%; 95% CI, 11–31%), as did median income (27%; 95% CI, 18–52%) and household size (20%; 95% CI, 12–45%). There was no association between race/ethnicity and mortality, although this analysis was underpowered.
Conclusions: Black race and Hispanic ethnicity are associated with an increased odds of COVID-19 positivity. This association is substantially mediated by socioeconomic factors.
Keywords: coronavirus, ethnic groups, race factors, socioeconomic factors, incidence
Racial and ethnic disparities in health are common in the United States, apparent as both striking differences in the prevalence (1) as well as outcomes (2) of disease. Such disparities exist in every aspect of care, from diagnosis to management (3), particularly with regard to Black and Hispanic patients compared with White patients (4). The underpinnings of these differences are complex, relating to factors such as access to care, implicit or explicit biases from healthcare workers and systems, and social determinants of health (5).
The coronavirus disease (COVID-19) is no exception (6–8). Racial and ethnic differences exist in the prevalence of comorbidities that impact the risk of severe COVID-19 infection as well as social determinants of health (e.g., underlying knowledge about the disease, ability to socially isolate by working from home, and environmental stressors) that may impact disease acquisition and acuity (9–11). Unfortunately, outcomes too have been found to differ across racial and ethnic groups. (12–39) To achieve better equity, we must identify actionable drivers of race/ethnicity-related disparities in health outcomes (40).
To this end, we sought to evaluate the association of race and ethnicity with COVID-19 incidence and outcomes in the context of other potential drivers of disease activity—specifically, local population density, income, and household size. We hypothesized that that these socioeconomic factors would be associated with race/ethnicity and would mediate the association of race/ethnicity with outcomes in COVID-19.
Methods
We performed a pair of retrospective cohort studies to assess the association of race and ethnicity with outcomes in the context of socioeconomic status and population crowding. Study 1 aimed to consider factors associated with test positivity and hospitalization rate; study 2 targeted understanding factors associated with worse outcomes among hospitalized patients.
Cohort Identification
Two patient cohorts were considered for study 1 and study 2, respectively. The first included all inpatient or outpatient adults (age ≥18 yr) who were tested using PCR for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) RNA (via nasopharyngeal swab or bronchial wash) at the University of Miami Hospital and Clinics (UMHC) between March 1, 2020, and July 23, 2020. The second cohort, a subset of cohort 1, included all adults who had a positive COVID-19 PCR test result and an inpatient encounter within the study period. Patients with missing race or ethnicity and those who did not have a documented address in the state of Florida (which was needed to determine several socioeconomic variables) were excluded from both cohorts. Furthermore, patients in study 2 who had not been discharged as of July 23, 2020, or were missing Sequential Organ Failure Assessment (SOFA) (41) scores were also excluded.
Data Extraction
Patient information, including demographics and outcomes, was obtained from UMHC’s UChart, an Epic electronic health record. To obtain additional socioeconomic variables, patients were assigned to census tracts based on their last home address in UChart. First, this was attempted using the Census Bureau’s geocoder (42); for the 28% of addresses that did not match using this tool, ArcGIS Pro One World Geocoding Service (43) was used to successfully match all addresses. All addresses matched by both tools were matched to the same census tract. For each patient, additional census tract–based sociodemographic variables were then extracted from the U.S. Census Bureau’s 2018 American Community Survey (44), including median household income, average household size, and population size. Using the square mileage per census tract found in the Census Bureau’s Gazetteer file (45), population density was calculated as population per square mile.
Exposure
For both studies, our primary exposure was race and ethnicity categorized as non-Hispanic White, non-Hispanic Black, Hispanic White, Hispanic Black, unknown, and other. Race/ethnicity are coded in UChart as reported by the patient or family member; if this information is unavailable from these sources, the fields are completed as “unknown.” All race/ethnicity categories that accounted for <1.5% of the total cohort each (Asian, American Indian, Pacific Islander, and multiple races) were categorized as “other” to enable statistical testing.
Outcomes
Our primary outcome for study 1 of all tested patients was a positive test result; our secondary outcome was hospitalization with COVID-19 (positive test result and inpatient admission to UMHC during the study period). The primary outcome of study 2, examining all patients hospitalized with a positive COVID-19 test, was hospital mortality; secondary outcomes were use of mechanical ventilation at any time during hospitalization and discharge to a post–acute care facility (long-term rehabilitation of skilled nursing facility) for survivors. Patients discharged to hospice or home hospice were classified as deaths.
Potential Mediation Variables
We considered socioeconomic factors—local median household income, local population density, and average household size by census tract—as potential mediators of the association of race/ethnicity and each of our outcomes. These factors were chosen as they are known to track with race and ethnicity in the United States (46, 47) and have plausible associations with access to health care and increased risk of exposure to a respiratory pathogen such as SARS-CoV-2. All three socioeconomic factors were converted to categorical variables based on tertile.
Other Patient Characteristics
We considered all available variables that we hypothesized may confound the association of race/ethnicity with outcomes. For study 1, this included only demographic data, as follows: age (18–30 yr, 31–49 yr, 50–64 yr, 65–79 yr, and ≥80 yr), gender (male or female), and health insurance payor (commercial, government, Medicaid, Medicare, or other).
For study 2, we also considered clinical information on comorbidities and severity of acute illness. Comorbidities believed to increase risk for COVID-19 by the Centers for Disease Control (48) were included; Elixhauser (49) or Charlson (50) comorbidities, based on International Classification of Diseases, tenth revision, diagnosis codes assigned to the current hospital encounter, were used. Specifically, we used Elixhauser to define heart conditions (congestive heart failure, cardiac arrhythmias, and/or valvular disease), cancer (lymphoma, metastatic cancer, and/or solid tumor without metastases), chronic kidney disease, lung disease (pulmonary circulation disorders and/or chronic pulmonary disease), sickle cell disease or thalassemia (deficiency anemia), diabetes (with or without complications), hypertension, and obesity. Cerebrovascular disease was defined by Charlson. We did not include pregnancy or solid organ transplant, as these were uncommon in our cohort; smoking and steroids were also not considered because of unreliable coding. To account for severity of acute illness, the maximum SOFA score within 24 hours of hospital admission was used.
Statistical Analysis
We described both study cohorts using standard summary statistics. For context, we also described the historic population of hospital admissions at UMHC (all inpatient encounters from January 2018 through December 2019) and the Miami-Dade County population (51). To evaluate the crude association of patient characteristics with each outcome, a univariate logistic regression was performed for each factor and outcome combination. We then constructed a series of multivariate regression models to assess the independent association of race/ethnicity with each outcome. In models for both studies, all demographic covariates listed above (age, sex, and health insurance payor) were included; for study 2, clinical covariate information was also included. Given the large number of hospitalized patients with missing SOFA scores, we conducted two sensitivity analyses to expand the cohort—one without including SOFA as a covariable (planned a priori) and another imputing SOFA (based on sex, age, and mortality) when missing (planned post hoc). Finally, to enhance statistical power for study 2, we conducted another post hoc sensitivity analysis with a more minimal covariate sample (sex, age 65+ yr, and SOFA score) and SOFA score imputation.
Finally, to answer the question “Do socioeconomic factors mediate the relationship between race/ethnicity and COVID-19 positivity?” we performed a mediation analysis. Mediation analyses are used to assess the relative magnitude of the “direct” and “indirect” (through a mediator) associations of an exposure with an outcome (52). To accomplish this, we first confirmed that our exposure, race/ethnicity, was associated, separately, with each potential mediator variable (e.g., local median household income) using multivariate linear regression (including demographic data as covariates). Second, we calculated the indirect effect of race/ethnicity on each outcome (e.g., test positivity) in the presence of the three potential mediators included together in a single model (53).
This study was approved by the Institutional Review Board of the University of Miami (#20200739). P values were considered significant if less than 0.05; correction for multiple comparisons was not used, and, therefore, all secondary analyses should be considered hypothesis generating. Statistical analyses were performed using R version 3.6.2.
Results
Our two study cohorts consisted of 15,473 patients tested (cohort 1) and 295 patients hospitalized (cohort 2) for COVID-19 (Figure E1 in the online supplement). Patients excluded because of missing data from cohort 1 tended to be younger and more commonly commercially insured than those remaining in the cohort; those excluded from cohort 2 were more frequently men (Table E1). The race/ethnic distribution of patients tested for COVID-19 was similar to that of patients historically admitted to UMHC but included more non-Hispanic White (29.0% vs. 13.0%) and fewer Hispanic White (48.1% vs. 62.0%) people than the general Miami-Dade County population (Table 1). Patients tested for COVID-19 also tended to be younger (32.6% vs. 23.9% <50 yr old) and more commonly insured by commercial payors (53.4% vs. 33.7%) than the historic UMHC population.
Table 1.
Demographic characteristics of cohort populations
| Characteristic | Cohort 1: Tested Patients | Cohort 2: Hospitalized Patients | UMHC Historic Population | Miami-Dade County |
|---|---|---|---|---|
| Patients/people, N | 15,473 | 295 | 35,970 | 2,715,516 |
| Race/ethnicity, n (%) | ||||
| Non-Hispanic White | 4,508 (29.0) | 27 (9.2) | 9,559 (26.6) | 353,017 (13.0) |
| Hispanic Black | 260 (1.7) | 7 (2.4) | 873 (2.4) | 54,310 (2.0) |
| Hispanic White | 7,441 (48.1) | 168 (56.9) | 15,893 (44.2) | 1,683,620 (62.0) |
| Non-Hispanic Black | 2,324 (15.0) | 63 (21.4) | 6,437 (17.9) | 434,482 (16.0) |
| Other* | 940 (6.1) | 30 (10.2) | 1,694 (4.7) | — |
| Unknown | — | — | 1,515 (4.2) | — |
| Sex, n (%) | ||||
| F | 8,264 (53.4) | 155 (52.5) | 17,383 (48.3) | 1,395,775 (51.4) |
| M | 7,209 (46.6) | 140 (47.5) | 18,588 (51.7) | 1,319,740 (48.6) |
| Payor, n (%) | ||||
| Commercial | 8,268 (53.4) | 86 (29.2) | 12,116 (33.7) | — |
| Government | 353 (2.3) | 11 (3.7) | 168 (0.5) | — |
| Medicaid | 1,229 (7.9) | 35 (11.9) | 4,915 (13.7) | — |
| Medicare | 5,107 (33.0) | 146 (49.5) | 17,031 (47.3) | — |
| Other | 516 (3.3) | 17 (5.8) | 1,740 (4.8) | — |
| Age, n (%) | ||||
| 18–30 yr | 1,327 (8.6) | 8 (2.7) | 2,145 (6.0) | 530,050 (19.5)† |
| 31–49 yr | 3,650 (23.6) | 47 (15.9) | 6,454 (17.9) | 771,261 (28.4)† |
| 50–64 yr | 5,074 (32.8) | 75 (25.4) | 11,633 (32.3) | 530,766 (19.5) |
| 65–79 yr | 4,201 (27.2) | 94 (31.9) | 11,133 (31.0) | 303,259 (11.2) |
| 80+ yr | 1,221 (7.9) | 71 (24.1) | 4,606 (12.8) | 120,094 (4.4) |
Definition of abbreviation: UMHC = University of Miami Hospital and Clinics.
Other includes Asian, American Indian, Pacific Islander, and multiple races.
†Age groups 15–29 yr (rather than 18–30 yr) and 30–49 yr (rather than 31–49 yr).
Patients hospitalized because of COVID-19 were more commonly Hispanic White (56.9% vs. 44.2%) and Black (23.8% vs. 20.3%) than historic UMHC-admitted patients; in fact, they more closely mirrored the Miami-Dade County population. Interestingly, they tended to be older (24.1% vs. 12.8% were 80+ yr old) than historic UMHC admissions; however, this result may be confounded by exclusion of patients remaining in the hospital (of whom only 14.3% were aged 80+ yr).
Study 1: Association of Race/Ethnicity and COVID-19 Test Positivity and Hospitalization
Non-Hispanic Black (odds ratio [OR], 3.30; 95% CI, 2.69–4.06; P < 0.001) and Hispanic White (OR, 2.76; 95% CI, 2.32–3.3; P < 0.001) and Black (OR, 3.84; 95% CI, 2.53–5.67; P < 0.001) people tested positive more commonly than did non-Hispanic White people (Table E2). These associations remained after adjustment for sex, age, and payor, as follows: Non-Hispanic Black (OR, 3.21; 95% CI, 2.60–3.96; P < 0.001), Hispanic White (OR, 2.72; 95% CI, 2.28–3.26; P < 0.001), and Hispanic Black (OR, 3.55; 95% CI, 2.33–5.28; P < 0.001) (Figure 1 and Table E3).
Figure 1.
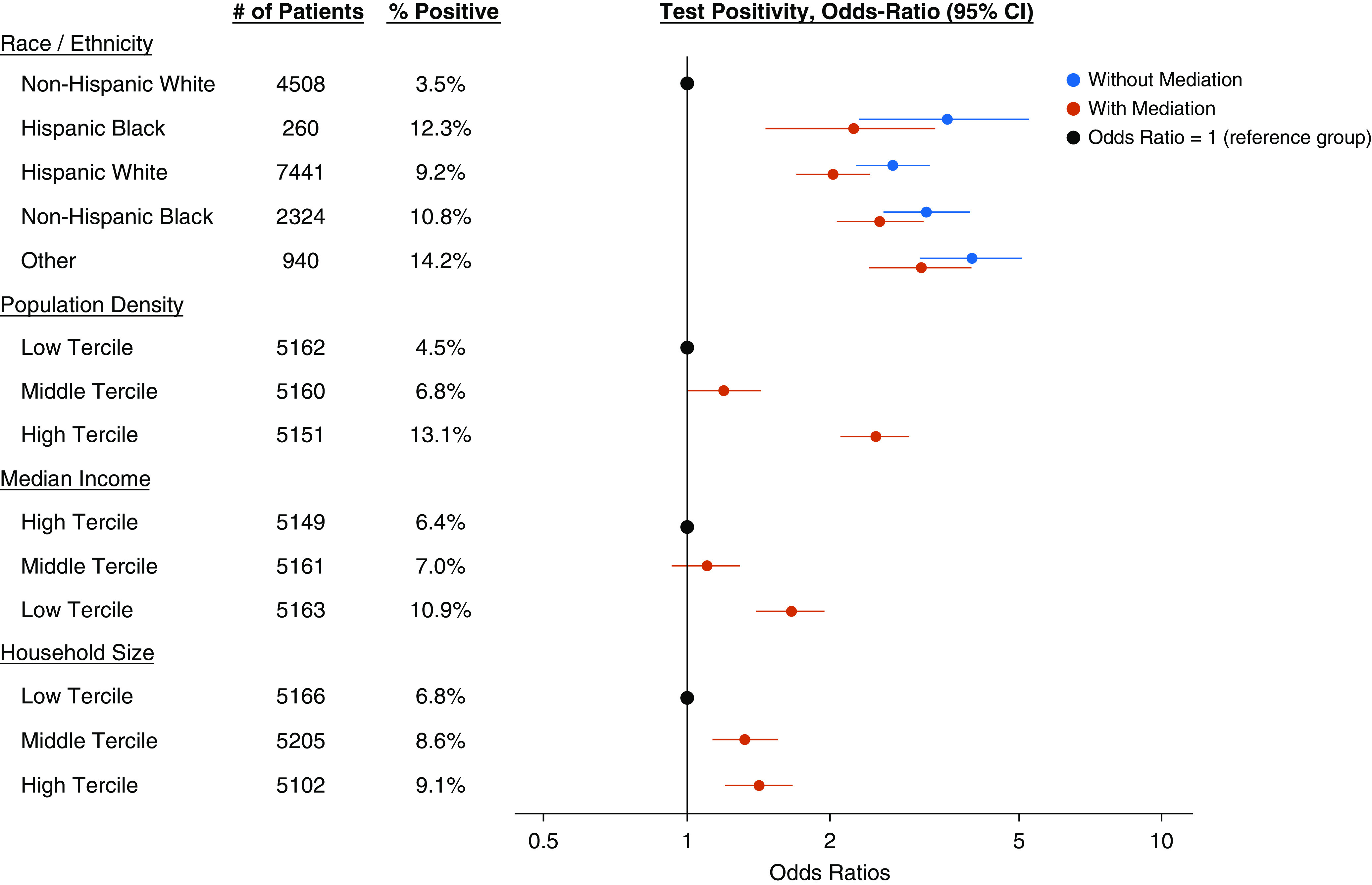
Adjusted association of race/ethnicity with test positivity in the absence and presence of socioeconomic factors. The model is also adjusted for demographic factors (age, sex, and payor). CI = confidence interval.
Race and ethnicity were associated with each of the socioeconomic factors considered as potential mediators (Figure 2). Upon inclusion of the potential mediation variables in the model, the associations of race/ethnicity with test positivity were reduced in magnitude, as follows: Non-Hispanic Black (OR, 2.55; 95% CI, 2.05–3.17; P < 0.001), Hispanic White (OR, 2.04; 95% CI, 1.69–2.46; P < 0.001), and Hispanic Black (OR, 2.25; 95% CI, 1.46–3.38; P < 0.001). Each of the socioeconomic factors mediated the association of race/ethnicity with test positivity; population density mediated 17% (95% CI, 11–31%), median income mediated 27% (95% CI, 18–52%), and household size mediated 20% (95% CI, 12–45%) (Figure 3 and Table E4).
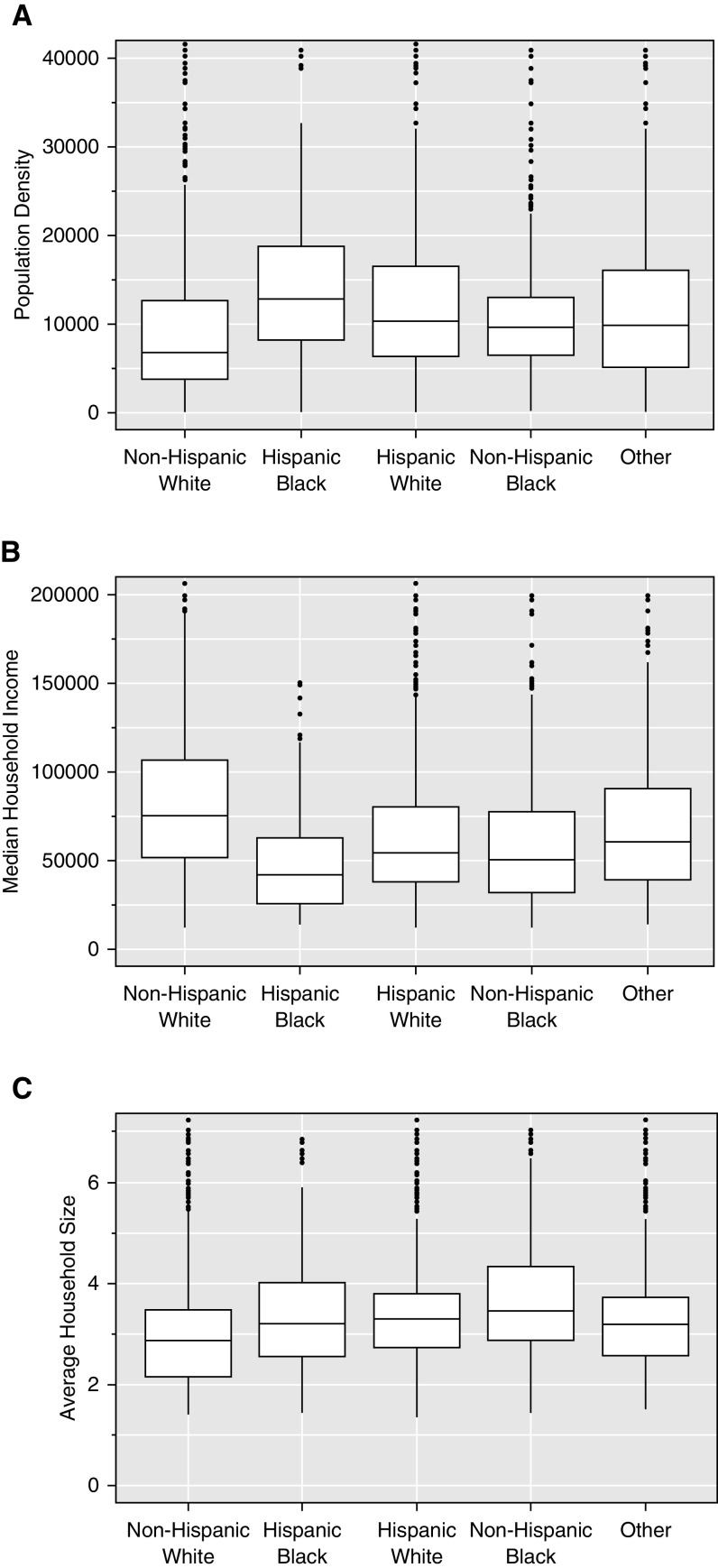
Figure 2.
Association of race and ethnicity with socioeconomic factors. (A) Population density. (B) Median household income. (C) Average household size. Data are given as medians with interquartile ranges (white boxes); in models inclusive of demographics (age, sex, and payor), race/ethnicity was associated with each of population density (P < 0.001), median household income (P < 0.001), and average household size (P < 0.001).
Figure 3.
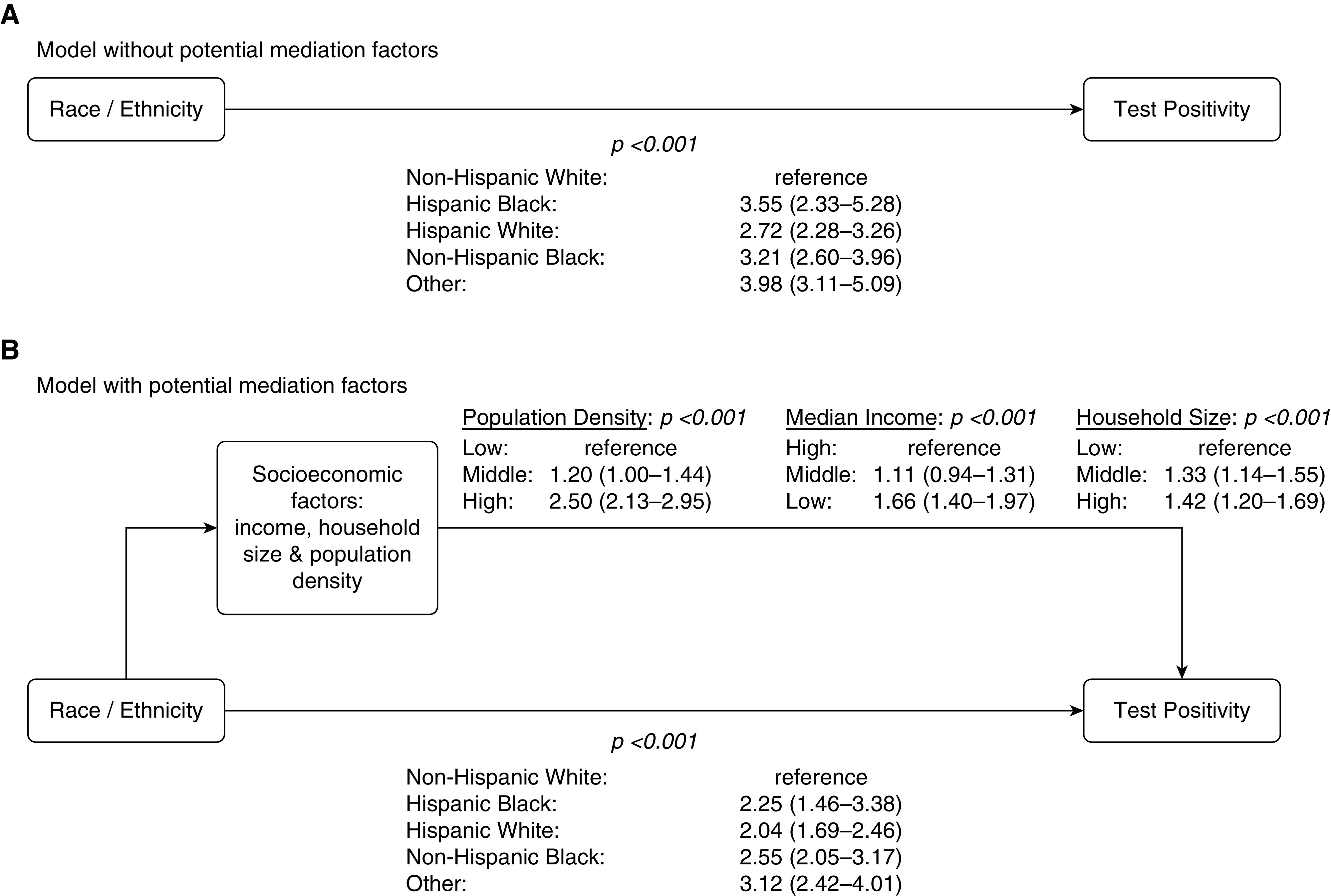
Mediation of the association of race and ethnicity with test positivity by socioeconomic factors. (A) Model without potential mediation factors. (B) Model with potential mediation factors. All socioeconomic factors were included in one model as a group; mediation analysis evaluating the impact of each factor separately determined that population density mediated 17% (95% confidence interval [CI], 11–31%), median income mediated 27% (95% CI, 18–52%), and household size mediated 20% (95% CI, 12–45%) of the association of race/ethnicity with test positivity.
Non-Hispanic Black (OR, 3.93; 95% CI, 2.82–5.55; P < 0.001) and Hispanic White (OR, 3.25; 95% CI, 2.43–4.43; P < 0.001) and Black (OR, 4.51; 95% CI, 2.33–8.14; P < 0.001) people were hospitalized more often than were non-Hispanic White people. As with test positivity, these associations with increased hospitalization persisted after adjustment for age, sex, and payor (non-Hispanic Black: OR, 4.75; 95% CI, 3.38–6.76; P < 0.001; Hispanic White: OR, 3.81; 95% CI, 2.84–5.21; P < 0.001; and Hispanic Black: OR, 4.34; 95% CI, 2.21–7.93; P < 0.001) (Table E5) and were mediated by socioeconomic factors (Figure E2 and Table E6).
Study 2: Association of Race/Ethnicity with Mortality and Morbidity in Hospitalized Patients
Mortality after hospitalization was no more common for Black or Hispanic White patients than it was for non-Hispanic White patients (Table E7). Even after adjustment for demographics and clinical characteristics, no association was found between race/ethnic groups and mortality (non-Hispanic Black: OR, 0.58; 95% CI, 0.09–3.78; P = 0.55; Hispanic White: OR, 1.08; 95% CI, 0.27–5.30; P = 0.92; and Hispanic Black: OR, 0.16; 95% CI, 0.002–6.92; P = 0.41) (Figure 4 and Table E8). The addition of socioeconomic factors did not change these findings. Moreover, our sensitivity analyses on an expanded cohort without adjustment for SOFA score, with imputed SOFA score, and with fewer covariables also demonstrated no association between race/ethnicity and mortality (Tables E9, E10, and E11). Similarly, no association was found between race/ethnicity and ventilator usage (Table E12) or disposition to a facility for survivors (Table E13). As race/ethnicity was not significantly associated with outcomes in hospitalized COVID-19–positive patients, mediation analyses were not conducted.
Figure 4.
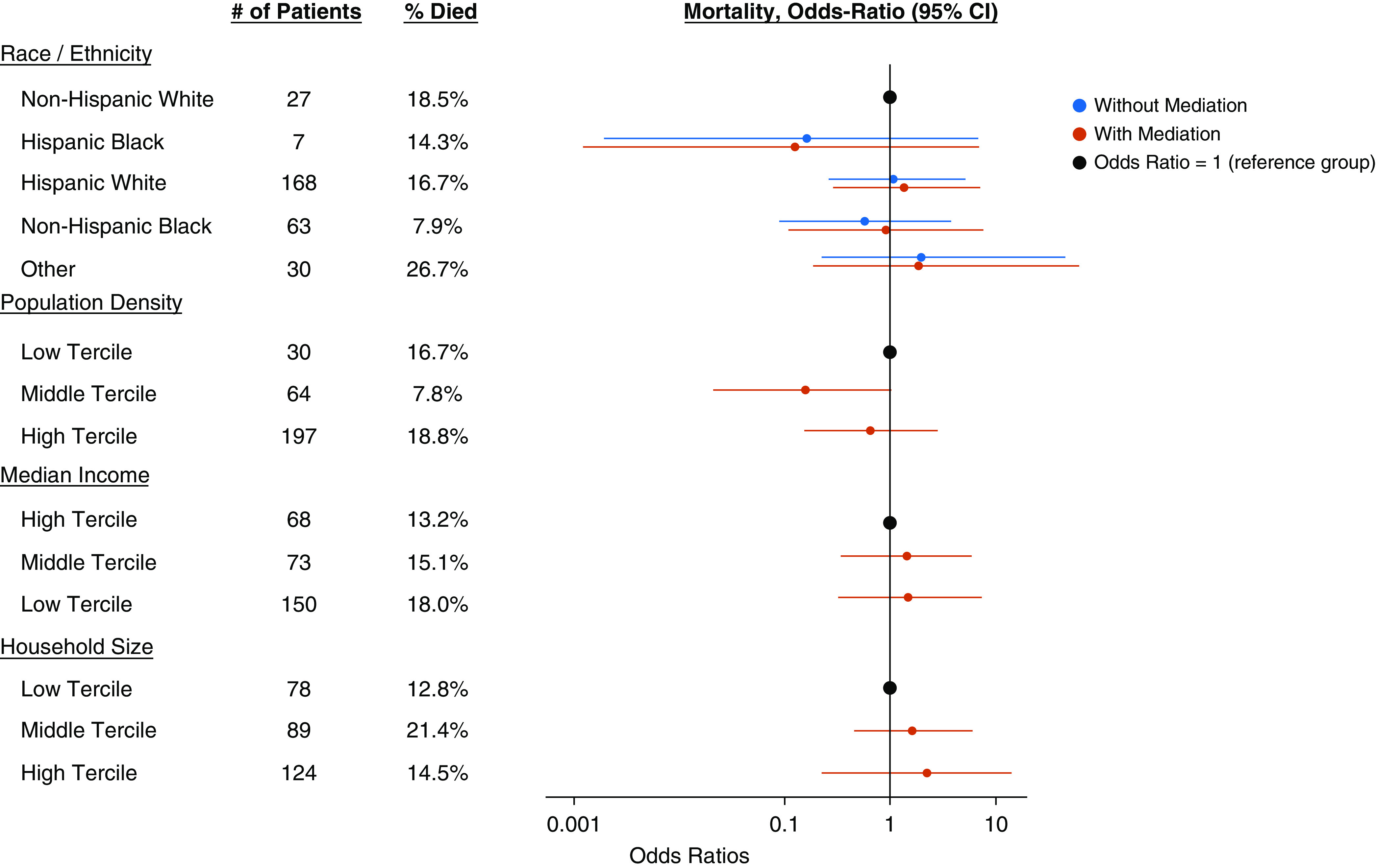
Adjusted association of race/ethnicity with mortality in the absence and presence of socioeconomic factors. The model is also adjusted for demographic factors (age, sex, and payor), comorbidities, and Sequential Organ Failure Assessment score. CI = confidence interval.
Discussion
We found that being of Black race or Hispanic ethnicity was associated with a 2.7- to 3.6-fold increased odds of testing positive and a 3.8- to 4.8-fold increased odds of being hospitalized after COVID-19 testing; however, we found no association of race/ethnicity with mortality or other outcomes in hospitalized patients, although these analyses were underpowered. Population density at the patient’s recorded address, median income, and household size were found to significantly mediate the association of race/ethnicity with both test positivity and hospitalization.
Our findings are consistent with published literature regarding the role of race and ethnicity in COVID-19 outcomes. Numerous studies have demonstrated an increased rate of test positivity (12, 14, 16, 21, 22, 27, 28, 32, 34–39) and hospitalization (12, 18–20, 23, 24, 28, 30, 31, 36) among Black and Hispanic people. Studies are less consistent regarding the impact of race/ethnicity on mortality, however, with some demonstrating an increased rate (13, 15, 17, 25, 29, 31, 36, 39) and others not (12, 18, 21, 26, 33, 35). The small sample size of our hospitalized cohort may have limited our ability to identify statistically significant associations with mortality; yet, as point estimates of ORs fall both above and below 1.0, we see no consistent trend toward worse survival in Black or Hispanic patients.
As Kaplan and Bennett eloquently detail, however, race and ethnicity may very well be risk markers of an outcome rather than risk factors for it (54). Specifically, as Osborne and Feit explain, “when race is used as a variable in research, there is a tendency to assume that the results obtained are a manifestation of the biology of racial differences” (i.e., a true risk factor) rather than, as they suggest, class, lifestyle, or socioeconomic status (i.e., a risk marker) (55). In a disease such as COVID-19 with droplet and airborne transmission, social determinants of health (e.g., living environment and working conditions) could play a large role in spread. Insofar as these determinants track with race and ethnicity, race and ethnicity are likely to be risk markers (and not risk factors) for disease acquisition and, potentially, disease severity.
Prior work has suggested that such socioeconomic determinants of health confer increased risk of infection and death in COVID-19. A county-level analysis demonstrated that U.S. counties with lower poverty rates, larger total populations (without accounting for density), and more education had higher rates of COVID-19 infection; more poverty, smaller population size, and less education were associated with higher death rates (56). Gu and colleagues reported a patient-level study similar to ours using data from patients tested at the University of Michigan in which both race (non-Hispanic Black people versus non-Hispanic White people: OR, 3.56; 95% CI, 2.90–4.37) and population density (persons per square mile: OR, 1.07 95% CI, 1.03–1.11) were associated with test positivity (57). Black race and socioeconomic factors were similarly associated with need for hospitalization in both the Michigan study and one from Wisconsin (28). Because only models inclusive of socioeconomic variables are presented in these analyses, however, it is unclear whether these factors mediate the association of race with outcomes and, if they do, to what degree. Our study is unique in assessing the mediation effects that socioeconomic factors have on race/ethnicity’s association with both test positivity and hospitalization in COVID-19. Palacio and Tamariz found, similarly, that income mediated the association of Black race (but not Hispanic ethnicity) with COVID-19 incidence rates in an ecological study in Miami-Dade County (58).
In addition to its novel approach, our study’s strength stems from the unique population in Miami, Florida, which is heterogeneous in terms of both race and ethnicity. Our study does suffer from several limitations, however. First, race/ethnicity was defined as entered into UChart; miscoding and data missingness create potential sources of bias. Second, socioeconomic variables were based on census tracts and may not accurately reflect the status of the individual patients to whom they were assigned. Moreover, this approach leads to artificial clustering of observations for which we did not account in our models. Third, a large proportion of hospitalized patients were excluded because of missing SOFA score information; however, the robustness of our results to sensitivity analyses including these patients in a model without SOFA scores and one with imputed values suggests that this source of potential bias is of minimal importance. Fourth, our estimates for the proportion of the associations of race/ethnicity with outcomes mediated by socioeconomic factors were based on models including each socioeconomic factor separately (as this is the standard format for mediation analysis), whereas our main models included all factors simultaneously. Fifth, we did not account for the proximity of patients’ residences to our testing facilities or hospital; proximity may have impacted their decision to seek care at our site versus alternate health facilities. Similarly, we had no data on hospitalizations outside of our health system, which may have introduced some misclassification bias in our analysis of hospitalization as an outcome. Sixth, limited access to testing—especially earlier in the study period and, likely, differentially across racial/ethnic groups—may have confounded our results. Seventh, we were only able to include a handful of demographic factors as potential confounders for our primary cohort because of data availability; as such, there is potential for significant residual confounding. Eighth, our mortality analysis was likely underpowered to detect true associations, and model fit was poor (measured by Hosmer-Lemeshow goodness-of-fit testing). Finally, our study relies on data from a single health system in a single city in the United States with a fairly unique population; the generalizability of our results to other settings is unknown.
We found Black race and Hispanic ethnicity to be clear markers of increased disease risk and hospitalization in COVID-19 but not mortality. However, these associations were notably mediated by social determinants of health. Our results cannot prove causality and, more importantly, cannot provide assurance that improving the socioeconomic conditions in which Black and Hispanic people find themselves will necessarily improve their COVID-19 risk. However, our findings suggest that it is certainly plausible that this may be the case. Moreover, it is very likely that the associations we found between the specific social determinants of health we evaluated and disease risk would be generalizable to other infections with droplet and airborne transmission. As such, even if it is too late for COVID-19, improvements in the social situations of all patients living in more crowded, less well-off communities may pay dividends for their health when the next pandemic or the next season of influenza hits.
Footnotes
Supported by the University of Miami Hospital and Clinics through funding to support the UHealth-DART Research Group, of which all authors are members.
Author Contributions: H.B.G., S.P., and P.R.W. had full access to all data. S.P. and P.R.W. performed all statistical analyses. H.B.G., S.P., and M.B. contributed to primary drafting of the manuscript. All authors were involved in primary study design, results interpretation, and critical review of the manuscript. H.B.G. is responsible for the integrity of the work as a whole.
This article has an online supplement, which is accessible from this issue’s table of contents at www.atsjournals.org.
Author disclosures are available with the text of this article at www.atsjournals.org.
Contributor Information
Collaborators: on behalf of the UHealth-DART Research Group
References
- 1. Doshi RP, Aseltine RH, Jr, Sabina AB, Graham GN. Racial and ethnic disparities in preventable hospitalizations for chronic disease: prevalence and risk factors. J Racial Ethn Health Disparities. 2017;4:1100–1106. doi: 10.1007/s40615-016-0315-z. [DOI] [PubMed] [Google Scholar]
- 2. Norton JM, Moxey-Mims MM, Eggers PW, Narva AS, Star RA, Kimmel PL, et al. Social determinants of racial disparities in CKD. J Am Soc Nephrol. 2016;27:2576–2595. doi: 10.1681/ASN.2016010027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. DiMeglio M, Dubensky J, Schadt S, Potdar R, Laudanski K. Factors underlying racial disparities in sepsis management. Healthcare (Basel) 2018;6:133. doi: 10.3390/healthcare6040133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Dominguez K, Penman-Aguilar A, Chang MH, Moonesinghe R, Castellanos T, Rodriguez-Lainz A, et al. Centers for Disease Control and Prevention (CDC) Vital signs: leading causes of death, prevalence of diseases and risk factors, and use of health services among Hispanics in the United States - 2009-2013. MMWR Morb Mortal Wkly Rep. 2015;64:469–478. [PMC free article] [PubMed] [Google Scholar]
- 5. Wallar LE, De Prophetis E, Rosella LC. Socioeconomic inequalities in hospitalizations for chronic ambulatory care sensitive conditions: a systematic review of peer-reviewed literature, 1990-2018. Int J Equity Health. 2020;19:60. doi: 10.1186/s12939-020-01160-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kullar R, Marcelin JR, Swartz TH, Piggott DA, Macias Gil R, Mathew TA, et al. Racial disparity of coronavirus disease 2019 in African American communities. J Infect Dis. 2020;222:890–893. doi: 10.1093/infdis/jiaa372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Macias Gil R, Marcelin JR, Zuniga-Blanco B, Marquez C, Mathew T, Piggott DA. COVID-19 pandemic: disparate health impact on the Hispanic/Latinx population in the United States. J Infect Dis. 2020;222:1592–1595. doi: 10.1093/infdis/jiaa474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Tai DBG, Shah A, Doubeni CA, Sia IG, Wieland ML. The disproportionate impact of COVID-19 on racial and ethnic minorities in the United States. Clin Infect Dis. 2021;72:703–706. doi: 10.1093/cid/ciaa815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Selden TM, Berdahl TA. COVID-19 and racial/ethnic disparities in health risk, employment, and household composition. Health Aff (Millwood) 2020;39:1624–1632. doi: 10.1377/hlthaff.2020.00897. [DOI] [PubMed] [Google Scholar]
- 10. Alobuia WM, Dalva-Baird NP, Forrester JD, Bendavid E, Bhattacharya J, Kebebew E. Racial disparities in knowledge, attitudes and practices related to COVID-19 in the USA. J Public Health (Oxf) 2020;42:470–478. doi: 10.1093/pubmed/fdaa069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Brandt EB, Beck AF, Mersha TB. Air pollution, racial disparities, and COVID-19 mortality. J Allergy Clin Immunol. 2020;146:61–63. doi: 10.1016/j.jaci.2020.04.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Adegunsoye A, Ventura IB, Liarski VM. Association of Black race with outcomes in COVID-19 disease: a retrospective cohort study. Ann Am Thorac Soc. 2020;17:1336–1339. doi: 10.1513/AnnalsATS.202006-583RL. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Adhikari S, Pantaleo NP, Feldman JM, Ogedegbe O, Thorpe L, Troxel AB. Assessment of community-level disparities in coronavirus disease 2019 (COVID-19) infections and deaths in large US metropolitan areas. JAMA Netw Open. 2020;3:e2016938. doi: 10.1001/jamanetworkopen.2020.16938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bassett MT, Chen JT, Krieger N. Variation in racial/ethnic disparities in COVID-19 mortality by age in the United States: a cross-sectional study. PLoS Med. 2020;17:e1003402. doi: 10.1371/journal.pmed.1003402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Cowger TL, Davis BA, Etkins OS, Makofane K, Lawrence JA, Bassett MT, et al. Comparison of weighted and unweighted population data to assess inequities in coronavirus disease 2019 deaths by race/ethnicity reported by the US centers for disease control and prevention. JAMA Netw Open. 2020;3:e2016933. doi: 10.1001/jamanetworkopen.2020.16933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Feehan AK, Velasco C, Fort D, Burton JH, Price-Haywood EG, Katzmarzyk PT, et al. Racial and workplace disparities in seroprevalence of SARS-CoV-2, Baton Rouge, Louisiana, USA. Emerg Infect Dis. 2021;27:314–317. doi: 10.3201/eid2701.203808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Holtgrave DR, Barranco MA, Tesoriero JM, Blog DS, Rosenberg ES. Assessing racial and ethnic disparities using a COVID-19 outcomes continuum for New York State. Ann Epidemiol. 2020;48:9–14. doi: 10.1016/j.annepidem.2020.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hsu HE, Ashe EM, Silverstein M, Hofman M, Lange SJ, Razzaghi H, et al. Race/ethnicity, underlying medical conditions, homelessness, and hospitalization status of adult patients with COVID-19 at an urban safety-net medical center - Boston, Massachusetts, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:864–869. doi: 10.15585/mmwr.mm6927a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Izzy S, Tahir Z, Cote DJ, Al Jarrah A, Roberts MB, Turbett S, et al. Characteristics and outcomes of Latinx patients with COVID-19 in comparison with other ethnic and racial groups. Open Forum Infect Dis. 2020;7:ofaa401. doi: 10.1093/ofid/ofaa401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Jehi L, Ji X, Milinovich A, Erzurum S, Merlino A, Gordon S, et al. Development and validation of a model for individualized prediction of hospitalization risk in 4,536 patients with COVID-19. PLoS One. 2020;15:e0237419. doi: 10.1371/journal.pone.0237419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kabarriti R, Brodin NP, Maron MI, Guha C, Kalnicki S, Garg MK, et al. Association of race and ethnicity with comorbidities and survival among patients with COVID-19 at an urban medical center in New York. JAMA Netw Open. 2020;3:e2019795. doi: 10.1001/jamanetworkopen.2020.19795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kaufman HW, Niles JK, Nash DB. Disparities in SARS-CoV-2 positivity rates: associations with race and ethnicity. Popul Health Manag. 2021;24:20–26. doi: 10.1089/pop.2020.0163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Killerby ME, Link-Gelles R, Haight SC, Schrodt CA, England L, Gomes DJ, et al. CDC COVID-19 Response Clinical Team. Characteristics associated with hospitalization among patients with COVID-19 - metropolitan Atlanta, Georgia, March-April 2020. MMWR Morb Mortal Wkly Rep. 2020;69:790–794. doi: 10.15585/mmwr.mm6925e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ko JY, Danielson ML, Town M, Derado G, Greenlund KJ, Daily Kirley P, et al. COVID-NET Surveillance Team. Risk factors for COVID-19-associated hospitalization: COVID-19-associated hospitalization surveillance network and behavioral risk factor surveillance system. Clin Infect Dis. 2020:ciaa1419. doi: 10.1093/cid/ciaa1419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Li AY, Hannah TC, Durbin JR, Dreher N, McAuley FM, Marayati NF, et al. Multivariate analysis of Black race and environmental temperature on COVID-19 in the US. Am J Med Sci. 2020;360:348–356. doi: 10.1016/j.amjms.2020.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. McCarty TR, Hathorn KE, Redd WD, Rodriguez NJ, Zhou JC, Bazarbashi AN, et al. How do presenting symptoms and outcomes differ by race/ethnicity among hospitalized patients with COVID-19 infection? Experience in Massachusetts. Clin Infect Dis. 2020:ciaa1245. doi: 10.1093/cid/ciaa1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Misa NY, Perez B, Basham K, Fisher-Hobson E, Butler B, King K, et al. Racial/ethnic disparities in COVID-19 disease burden & mortality among emergency department patients in a safety net health system. Am J Emerg Med. doi: 10.1016/j.ajem.2020.09.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Muñoz-Price LS, Nattinger AB, Rivera F, Hanson R, Gmehlin CG, Perez A, et al. Racial disparities in incidence and outcomes among patients with COVID-19. JAMA Netw Open. 2020;3:e2021892. doi: 10.1001/jamanetworkopen.2020.21892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ojinnaka CO, Adepoju OE, Burgess AV, Woodard L. Factors associated with COVID-related mortality: the case of Texas. J Racial Ethn Health Disparities. doi: 10.1007/s40615-020-00913-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Patel AP, Paranjpe MD, Kathiresan NP, Rivas MA, Khera AV. Race, socioeconomic deprivation, and hospitalization for COVID-19 in English participants of a national biobank. Int J Equity Health. 2020;19:114. doi: 10.1186/s12939-020-01227-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Poulson M, Geary A, Annesi C, Allee L, Kenzik K, Sanchez S, et al. National disparities in COVID-19 outcomes between Black and White Americans. J Natl Med Assoc. doi: 10.1016/j.jnma.2020.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Raine S, Liu A, Mintz J, Wahood W, Huntley K, Haffizulla F. Racial and ethnic disparities in COVID-19 outcomes: social determination of health. Int J Environ Res Public Health. 2020;17:8115. doi: 10.3390/ijerph17218115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Rodriguez F, Solomon N, de Lemos JA, Das SR, Morrow DA, Bradley SM, et al. Racial and ethnic differences in presentation and outcomes for patients hospitalized with COVID-19: findings from the American Heart Association’s COVID-19 cardiovascular disease registry. Circulation. doi: 10.1161/CIRCULATIONAHA.120.052278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Rozenfeld Y, Beam J, Maier H, Haggerson W, Boudreau K, Carlson J, et al. A model of disparities: risk factors associated with COVID-19 infection. Int J Equity Health. 2020;19:126. doi: 10.1186/s12939-020-01242-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Sze S, Pan D, Nevill CR, Gray LJ, Martin CA, Nazareth J, et al. Ethnicity and clinical outcomes in COVID-19: a systematic review and meta-analysis. EClinicalMedicine. 2020;29:100630. doi: 10.1016/j.eclinm.2020.100630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Thompson CN, Baumgartner J, Pichardo C, Toro B, Li L, Arciuolo R, et al. COVID-19 outbreak - New York city, February 29-June 1, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1725–1729. doi: 10.15585/mmwr.mm6946a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Tirupathi R, Muradova V, Shekhar R, Salim SA, Al-Tawfiq JA, Palabindala V. COVID-19 disparity among racial and ethnic minorities in the US: a cross sectional analysis. Travel Med Infect Dis. 2020;38:101904. doi: 10.1016/j.tmaid.2020.101904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Vahidy FS, Nicolas JC, Meeks JR, Khan O, Pan A, Jones SL, et al. Racial and ethnic disparities in SARS-CoV-2 pandemic: analysis of a COVID-19 observational registry for a diverse US metropolitan population. BMJ Open. 2020;10:e039849. doi: 10.1136/bmjopen-2020-039849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Zelner J, Trangucci R, Naraharisetti R, Cao A, Malosh R, Broen K, et al. Racial disparities in Coronavirus Disease 2019 (COVID-19) mortality are driven by unequal infection risks. Clin Infect Dis. 2021;72:e88–e95. doi: 10.1093/cid/ciaa1723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Iacobucci G. Covid-19: review of ethnic disparities is labelled “whitewash” for lack of recommendations. BMJ. 2020;369:m2208. doi: 10.1136/bmj.m2208. [DOI] [PubMed] [Google Scholar]
- 41. Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, et al. The SOFA (Sepsis-related organ failure assessment) score to describe organ dysfunction/failure: on behalf of the working group on sepsis-related problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996;22:707–710. doi: 10.1007/BF01709751. [DOI] [PubMed] [Google Scholar]
- 42.United States Census Bureau 2018https://www.census.gov/programs-surveys/geography/technical-documentation/complete-technical-documentation/census-geocoder.html.
- 43.ArcMap. 2016. https://desktop.arcgis.com/en/arcmap/10.3/guide-books/geocoding/working-with-arcgis-online-geocoding-service.htm
- 44.United Status Census Bureau. 2020. https://www.census.gov/programs-surveys/acs/about.html
- 45.United Status Census Bureau. 2019. https://www.census.gov/geographies/reference-files/time-series/geo/gazetteer-files.html
- 46.Maciag M.2017. https://www.governing.com/gov-data/population-density-land-area-cities-map.html
- 47.United Status Census Bureau. 2019. https://www.census.gov/quickfacts/fact/table/US/PST045219
- 48.Centers for Disease Control and Prevention. 2020. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html
- 49. Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 50. Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 51.United States Census Bureau 2018https://www.census.gov/data/developers/data-sets/acs-5year.html.
- 52. VanderWeele TJ. Mediation analysis: a practitioner’s guide. Annu Rev Public Health. 2016;37:17–32. doi: 10.1146/annurev-publhealth-032315-021402. [DOI] [PubMed] [Google Scholar]
- 53.Tingley D, Yamamoto T, Hirose K, Keele L, Imai K.Mediation: R package for causal mediation analysis J Stat Softw 201459:1–38..26917999 [Google Scholar]
- 54. Kaplan JB, Bennett T. Use of race and ethnicity in biomedical publication. JAMA. 2003;289:2709–2716. doi: 10.1001/jama.289.20.2709. [DOI] [PubMed] [Google Scholar]
- 55. Osborne NG, Feit MD. The use of race in medical research. JAMA. 1992;267:275–279. [PubMed] [Google Scholar]
- 56. Abedi V, Olulana O, Avula V, Chaudhary D, Khan A, Shahjouei S, et al. Racial, economic, and health inequality and COVID-19 infection in the United States. J Racial Ethn Health Disparities. doi: 10.1007/s40615-020-00833-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Gu T, Mack JA, Salvatore M, Prabhu Sankar S, Valley TS, Singh K, et al. Characteristics associated with racial/ethnic disparities in COVID-19 outcomes in an academic health care system. JAMA Netw Open. 2020;3:e2025197. doi: 10.1001/jamanetworkopen.2020.25197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Palacio A, Tamariz L. Social determinants of health mediate COVID-19 disparities in South Florida. J Gen Intern Med. 2021;36:472–477. doi: 10.1007/s11606-020-06341-9. [DOI] [PMC free article] [PubMed] [Google Scholar]