Abstract
Objective
Emerging adulthood is a period of heightened risk for young people with autism spectrum disorder (ASD). Due in part to lack of evidence-based services and supports during the transition to adulthood, many emerging adults fail to matriculate into postsecondary education or thrive in productive employment. The Stepped Transition in Education Program for Students with ASD (STEPS) was developed to address the psychosocial, transition-related needs of emerging adults with ASD.
Method
Adolescents and emerging adults (n = 59) with ASD were randomly assigned to either STEPS or Transition as Usual (TAU).
Results
Results indicate that STEPS is acceptable to young people with ASD and their parents and that it can be implemented with high fidelity. Among secondary school students, those who completed STEPS exhibited significantly greater gains in transition readiness from high school and these gains were largely sustained after program completion. Among students enrolled in postsecondary education, STEPS resulted in increased levels of student adaptation to college relative to those in TAU.
Conclusion
Programming to address ASD-related challenges can promote successful educational transitions.
Keywords: Autism Spectrum Disorder, STEPS, college, adult, transition
Approximately 1 in 59 youth have a diagnosis of autism spectrum disorder (ASD) based on CDC estimates (Baio et al., 2018). Rate of diagnosis of ASD began to rise in the 1990s, coinciding with heightened recognition of autism in cognitively high-functioning individuals (e.g., Asperger’s Disorder). The children from this generation are now college-age. Given that 50,000 teens with autism now enter adulthood every year (Shattuck, Narendorf, Cooper, Sterzing, Wagner, & Taylor, 2012), there will be upwards of a half-million more adults with ASD each decade, leading some to refer to the rise in this segment of the population as the ‘autism tsunami’.
As adolescents with ASD mature into adulthood they face a fairly unique set of circumstances; although capable of succeeding in higher education and often motivated to pursue specialized training, documented challenges exist which can impede a successful transition to postsecondary schooling. Specifically, adolescents and emerging adults with ASD exhibit underdeveloped independence, lagging interpersonal skills, and impaired ability to manage stress and intense emotion (Elias, Muskett, & White, 2017; Elias & White, 2018). The need for empirically based programming to support successful transition to postsecondary training and education is immense, owing to the steadily growing population of adolescents and young adults with ASD (Billstedt, Gillberg, & Gillberg, 2005; Farley et al., 2009). Most people diagnosed with ASD do not have co-occurring intellectual disability (Baio et al., 2018), and many are now enrolling in public and private higher education institutions (White, Ollendick, & Bray, 2011). Taylor and Seltzer (2011) found that nearly 50% of young adults with ASD without intellectual disability (ID) were pursuing a postsecondary degree. Using a broader and more representative sample (including those with ID), Wei et al. (2016) found that only about 32% of students with ASD matriculate into either 2- or 4-year college, making ASD the third lowest, of 12 special education categories, with respect to postsecondary enrollment. Although these estimates are lower than U.S. college enrollment rates for the general population immediately after high school, which hovers around 70% (U.S. Dept of Health and Human Services, 2017), it is clear that postsecondary education is a goal for a sizeable proportion of the student population with ASD.
The transition from adolescence to adulthood represents a distinct developmental period termed ‘emerging adulthood’ (Arnett, 2010). This period, which spans approximately ages 18 to 25, is characterized by achieving independence in decision-making, responsibility for oneself, and financial independence (Arnett, 2000). Unfortunately, for many emerging adults with ASD without ID, core symptoms of ASD persist and daily living skills plateau or sometimes regress after adolescence (Smith, Maenner & Seltzer, 2012; Taylor & Seltzer, 2010). Although adults with ASD without ID are more likely to be working in the community or going to college – relative to autistic adults who do have ID, they are also more likely to have no regular daytime activities (Taylor & Seltzer, 2011). Among the factors that contribute to suboptimal adult outcomes, unavailability of appropriate services and supports is central (Mazefsky & White, 2014; Taylor & Seltzer, 2011). There are no widely available, evidence-based programs designed to address the needs of cognitively able adolescents with ASD as they prepare for independent adult life and the transition to postsecondary education (Wehman et al., 2014).
Individualized and developmentally sensitive transition and support services may facilitate successful transition to adulthood for adolescents and emerging adults with ASD. The Stepped Transition in Education Program for Students with ASD (STEPS) is a transition support curriculum designed for emerging adults with ASD. STEPS was developed according to participatory process principles of treatment development (e.g., Chambers et al., 2007; Nicolaidis et al., 2011). Development, refinement, and testing of STEPS has evolved in a stepwise and iterative fashion, consistent with the ORBIT model for Behavioral Treatment Development (see Czajkowski et al., 2015) and NIH guidance on the design of intervention research and treatment manuals for ASD and related problems (Smith et al., 2007). Development included focus groups and nationwide surveys with students with ASD, their parents, and educators (Elias & White, 2017; White et al., 2016a). A preliminary open trial (White et al., 2016b) was then conducted per the Preliminary Testing phase of the ORBIT model. STEPS primarily targets self-determination and self-regulation in order to foster psychosocial preparedness for graduation from secondary school and success during postsecondary education, and more broadly in early adulthood. Given the different needs of secondary and postsecondary students, STEPS has two distinct curricula: STEP 1 is for secondary (high school) students and STEP 2 is for currently enrolled postsecondary (college/university) students or those who have exited secondary school but have not yet begun postsecondary education or further career training (see White et al., 2017 for a comprehensive description of the development and content of the program). Although the curricula are distinct, both programs focus on building the student’s self-determination and regulatory ability, given that these processes are impaired in ASD and have been shown important in improving educational and socio-emotional outcomes for students with a range of disabilities (e.g., Corbett, Constantine, Hendren, Rocke, & Ozonoff, 2009; Hendricks & Wehman, 2009; Mazefsky et al., 2013; Wehmeyer & Palmer, 2003).
The goal of this randomized controlled trial (RCT), consistent with Phase IIb (Pilot Testing) of ORBIT, was to evaluate the feasibility and preliminary efficacy of STEPS. We hypothesized that feasibility, including acceptability to consumers and counselor integrity to program manual, would be high (i.e., <15% attrition; at least average satisfaction ratings by >90% of consumers; and >90% average integrity). These thresholds are based on prior large-scale RCTs and those with ASD youth (e.g., Piacentini et al., 2014; White et al, 2013). We also hypothesized that the program would have a positive effect on both readiness for transition to postsecondary school (for STEP 1) and adjustment to college (for STEP 2). Finally, in the interest of moving toward more personalized treatment approaches (e.g., NIMH, 2015), exploratory analyses examine within-person variables - namely cognitive ability, self-determination, ASD severity, and co-occurring behavioral and emotional problems, as potential predictors of treatment response.
Methods
Participants
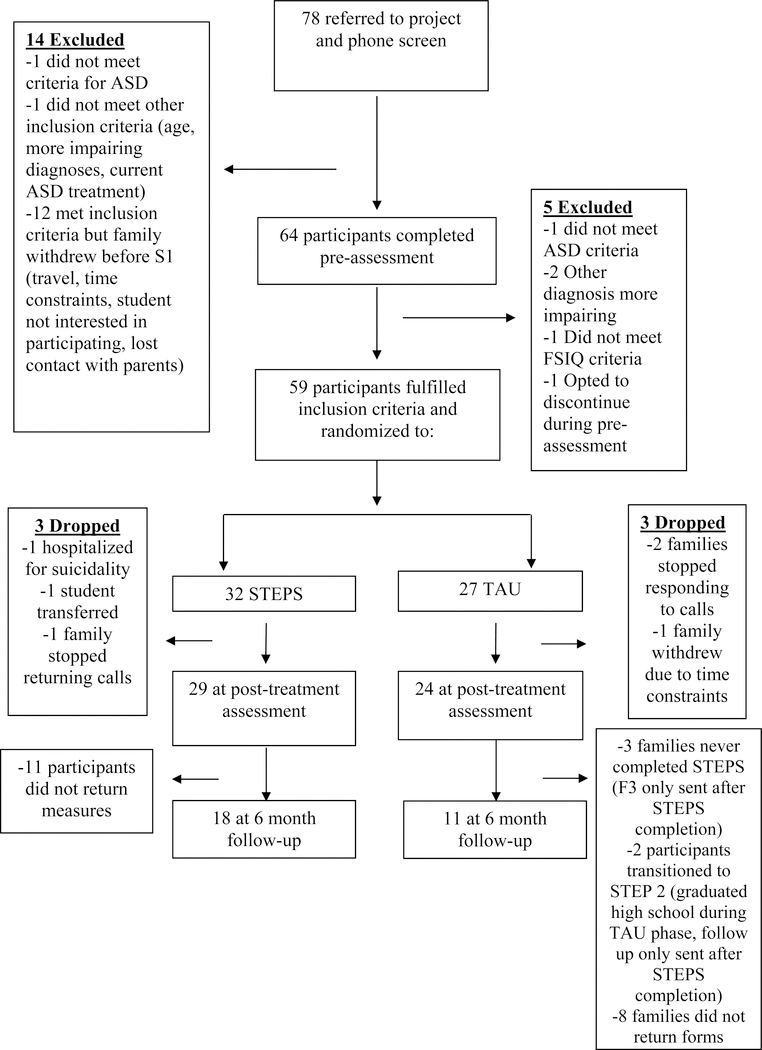
Participants (n = 59), 16–25 years of age (M = 18.65, SD = 2.07), were largely from small cities and rural areas in a southeastern state. Participating families were recruited through community advertisements, autism-specific email listservs and newsletters, university-affiliated clinics, and area schools and universities. Across both conditions, participants were 88.1% Caucasian, 3.39% African-American, 8.47% Asian, and 81.36% male (Table 1). To be eligible, participants had to have a diagnosis of ASD; for STEP 1, the student must have not yet graduated from high school and for STEP 2, the young person was either enrolled in postsecondary education or graduated from high school and uncertain of future plans/education (i.e., undecided). If a participant did not have a primary classification of ‘Autism’ on their Individualized Education Plan (IEP; STEP 1 participants), diagnosis was confirmed by the Autism Diagnostic Observation Schedule-Second Edition (Lord et al., 2012), completed by a research-reliable clinician. Participants also had at least average range cognitive ability (i.e., Full Scale IQ ≥ 85), on the Wechsler Abbreviated Scale of Intelligence-Second Edition (WASI-II; Wechsler, 2011). Exclusion criteria included (1) unmanaged psychopathology that warranted immediate clinical care (including clear suicidal intent, psychosis, or severe aggression), as determined by clinical interview and (2) student or family currently in therapy or receiving services considered redundant with STEPS (e.g., therapy for difficulties with emotion regulation, cognitive behavioral therapy). Comorbidity was common, with the majority of the sample presenting with at least one secondary psychiatric disorder based on clinical interview [Anxiety Disorders Interview Schedule for DSM-5 (ADIS-5; Brown & Barlow, 2014) for participants who were 18 or older and the Anxiety Disorders Interview Schedule for DSM-5-Child and Parent Versions (ADIS-5-C/P; Albano & Silverman, 2019) for those participants who were less than 18 years old, see Table 1)]. Across both STEPS, sixty-four adolescents and young adults with ASD were referred to the study and completed the initial eligibility assessment, of whom 59 were randomized (n = 24 for STEP 1; n = 35 for STEP 2; see Figure 1 for CONSORT). Based on a priori power analyses, calculated power to detect a large effect with our targeted sample size of n = 20 in STEP 1 and n = 30 in STEP 2 was .5–.7, somewhat lower than the commonly accepted .80 threshold. We considered these power values to be acceptable given the ORBIT model suggests small samples prior to more resource-intensive, large-scale trials (Czajkowski et al., 2015) and given that our primary aims were to examine feasibility and preliminary efficacy via within-person change.
Table 1.
Group Descriptive Data
| Mean (SD) | Mean (SD) | |||||
|
| ||||||
| STEP 1 (n = 24) | STEP 2 (n = 35) | |||||
| STEPS | TAU | Overalla | STEPS | TAU | Overallb | |
| Continuous Variable | (n = 15) | (n = 9) | (n = 17) | (n = 18) | ||
|
| ||||||
| Age (in years) | 17.00 (.76) | 17.25 (.89) | 17.09 (.79) | 19.94 (1.88) | 19.50 (2.15) | 19.71 (2.00) |
| FSIQ | 105.07 (13.51) | 100.38 (11.03) | 103.36 (14.31) | 103.87 (14.95) | 108.50 (12.19) | 106.39 (13.50) |
| SRS-2 | 69.67 (10.22) | 61.78 (8.74) | 66.71 (10.27) | 67.43 (8.41) | 72.27 (11.86) | 69.93 (10.45) |
| ASEBA | 62.08 (10.63) | 60.78 (5.74) | 61.55 (8.81) | 60.20 (13.03) | 62.17 (8.52) | 61.27 (10.67) |
| AIR-SD | 37.80 (5.07) | 41.22 (7.41) | 39.08 (6.14) | 36.23 (7.73) | 36.38 (6.84) | 36.31 (7.12) |
| TRS for STEP 1; SACQ for STEP 2 (Primary Outcome Measures) | ||||||
| Pre-treatment | 67.27 (11.18) | 71.89 (11.42) | 69.00 (11.26) | 38.70 (9.37) | 41.77 (7.41) | 40.43 (8.26) |
| Mid 1 | 76.67 (16.03) | 74.57 (7.80) | 75.75 (12.75) | NA | NA | NA |
| Mid 2 | 78.09 (17.20) | 77.33 (11.34) | 77.82 (15.01) | 44.58 (10.60) | 38.00 (8.14) | 41.16 (9.79) |
| Mid 3 | 89.00 (13.19) | 74.20 (10.57) | 82.27 (13.84) | 52.00 (10.89) | 44.63 (10.81) | 48.53 (11.17) |
| Post-treatment | 84.22 (18.32 | 71.80 (12.03) | 79.79 (17.01) | 43.78 (9.38) | 39.17 (8.01) | 41.93 (8.87) |
|
| ||||||
| n (% within group) | n (% within group) | |||||
| STEP 1 (n = 24) | STEP 2 (n = 35) | |||||
| Categorical Variable | STEPS | TAU | STEPS | TAU | ||
| (n = 15) | (n = 9) | (n = 17) | (n = 18) | |||
|
| ||||||
| Sex | ||||||
| Male | 15 (100.0) | 8 (88.9) | 23 (95.8) | 12 (70.6) | 13 (72.20) | 25 (71.43) |
| Female | 0 (0.0) | 1 (11.1) | 1 (4.2) | 5 (29.4) | 5 (27.80) | 10 (28.57) |
| Race | ||||||
| Caucasian | 15 (100.0) | 9 (100.0) | 24 (100.0) | 14 (82.4) | 14 (77.8) | 28 (80.0) |
| African-American | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (5.9) | 1 (5.6) | 2 (5.7) |
| Asian | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (11.8) | 3 (16.7) | 5 (14.3) |
| Latino/Hispanic | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Comorbidity | ||||||
| Social Anxiety Disorder | 6 (40.0) | 3 (33.3) | 9 (37.5) | 9 (52.9) | 14 (77.8) | 23 (65.7) |
| Generalized Anxiety Disorder | 4 (26.7) | 3 (33.3) | 7 (29.2) | 10 (58.8) | 9 (50.0) | 19 (54.3) |
| Specific Phobia | 1 (6.7) | 1 (11.1) | 2 (8.3) | 2 (11.8) | 3 (16.7) | 5 (14.3) |
| Major Depressive Disorder | 1 (6.7) | 1 (11.1) | 2 (8.3) | 2 (11.8) | 4 (22.2) | 6 (17.1) |
| Persistent Depressive Disorder | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (11.8) | 2 (11.1) | 4 (11.4) |
| Post Traumatic Stress Disorder | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (5.9) | 2 (11.1) | 3 (8.6) |
| Attention Deficit Hyperactivity Disorder | 6 (40.0) | 4 (44.4) | 10 (41.7) | NA | NA | NA |
| Oppositional Defiant Disorder | 2 (13.3) | 0 (0.0) | 2 (8.3) | NA | NA | NA |
Notes.
NA = Not applicable; SRS-2 = SRS-2 Total T-score; ASEBA = ASEBA Total Problems (emotional/behavioral problems) T-Score; AIR-SD = Self-determination Total Score
Overall = M (SD) for each STEP (STEPS and TAU combined)
= t-test result between STEP 1 and TAU
= t-test result between STEP 2 and TAU
Sample size varied across outcome measures due to missing data. There were no statistically significant difference in any of the comparisons conducted at .05 level (Two-tailed). Therefore, no signs (e.g., *) appear in the table.
Figure 1.
Consort Flow Chart
Intervention
STEPS was delivered at both the secondary and postsecondary levels, with the immediate goals of improving self-determination, self-knowledge, and emotion regulation (White et al., 2017). The two levels (STEP 1 and STEP 2) were designed to match the student’s specific developmental needs with respect to achieving independence and self-sufficiency as well as psychosocial tools to foster academic success. STEP 1 was for currently enrolled high school, or home-schooled, students who were within one year of anticipated graduation and unsure of post-graduation plans or contemplating entering postsecondary education. STEP 2 was for students with ASD who had graduated high school, or who were already enrolled in a 2-year (community college) or 4-year (university/college) postsecondary institution. STEPS counselors were advanced doctoral students in clinical psychology under the supervision of a licensed psychologist. Although STEPS is standardized as a manual, personalization occurs with respect to the student’s specific goals and needs.
For STEP 1, the high school student, parent(s), and one school personnel (the individual most involved with the student, identified by family; usually a teacher or school-based counselor) participated in program activities. Activities included 6 bi-weekly counseling sessions, 1 full-day college immersion day (at either a community college or college/university, depending on student’s goal), and an 8-hour in-service designed to help educators (the identified support person) facilitate students’ transition-related needs according to the STEPS model (White et al., 2017). In STEP 1, each of the six counseling sessions was approximately 1.5 hours in duration and occurred every two weeks. Each immersion day lasted for about 5 to 6 hours total. The student participated in all counseling sessions, while the parent(s) participated in components of most sessions (e.g., identifying between-session practice opportunities). The school personnel was invited to participate, either remotely or in person, during two of the sessions. During the immersion experience, which involved the student and counselor, the student engaged in activities such as talking with support staff in the school’s disability services office, sitting in a large class, reviewing syllabi from courses of interest to the student, and dining in a student area. All activities during immersion were personalized to the particular student to foster specific skill deficiencies (e.g., self-advocating for needed accommodations, functioning without parental support). Cumulatively for STEP 1, content delivery took approximately 16 hours. STEP 2 provided 12 to 16 one-on-one, approximately weekly, counseling sessions depending on the participant’s needs. Each of these weekly meetings were about 60 minutes in duration. In addition to the sessions, there were 4–6 counselor-accompanied outings in the community and weekly check-ins either by telephone or email (i.e., to ensure between-session practices were done, check in on goals). In both programs, in addition to the student with ASD, his/her parent(s) and school-based personnel were offered online content covering a range of topics related to transition supports for ASD (e.g., video tutorials on campus-based services, legal rights of parents of adult children). Regarding dosage for STEP 2, participants received 15–20 hours of total content delivery.
Procedures
Study procedures were approved by the university’s Institutional Review Board. Prior to data collection, participants provided consent and assent (depending on age). Once eligibility was confirmed, participants were randomly assigned to either STEPS or the control condition (transition as usual: TAU), by a statistician uninvolved in program implementation using a pre-determined random assignment sequence. Randomization was done within each STEP (1 or 2). In STEP 1, a dynamic, blocked randomization approach was used such that randomization occurred at the school level and so that school personnel, once trained in STEPS, would not be involved in a TAU case in order to prevent cross-condition contamination (Moerbeek, 2005). Initial blocking of secondary schools was based on school size (number of students) and SES (percentage of students qualifying for free/reduced lunch). With 16 high schools subject to randomization, there were 4 blocks ranging in size from 2 schools to 6 schools. In STEP 2, a blocked randomization approach was used with blocking based on school type (2-year community college or 4-year college/university). STEP 2 participants came from 3 community colleges and 3 universities.
STEPS program duration was approximately 4.5 months (16 weeks) per participant in both STEPS. All TAU participants received any transition-related services that were self-initiated for students outside of this study (e.g., via IEP, or disability support office), and all families were offered STEPS (open label) after completion of the 16-week TAU period. Families enrolling in STEP 2 after completion of STEP 1 did not provide follow-up data on STEP 1 measures.
Measures
Achenbach System of Empirically Based Assessment (ASEBA; Achenbach, 1991; Achenbach & Rescorla, 2003)
The severity of individual behavioral problems was measured through the ASEBA battery of scales. ASEBA comprises several measures of functioning across the lifespan. For the purposes of this study, the Child Behavior Checklist (CBCL; Achenbach, 1991) was administered to parents of STEP 1 participants and the Adult Behavior Checklist (ABCL; Achenbach & Rescorla, 2003) was administered to parents of STEP 2 participants. The measures are to be completed based on observations noted over a 6-month period. Reliability, validity, and stability are well documented for the ASEBA measures. For the current study, ASEBA measures were administered prior to starting treatment and at the post-treatment assessment, with the reporting timeframe adjusted to the past week.
American Institutes for Research Self Determination Scale (AIR-SD; Wolman, Campeau, DuBois, Mithaug, & Stolarski, 1994)
The AIR-SD, administered to parents, is a 16-item measure with Likert response fields ranging from 1 (never) to 5 (always). The content of the AIR-SD assessed opportunity and capacity to choose and behave in goal-directed ways. The summation of capacity and opportunity produce a self-determination total score. Psychometric properties of the measure are strong (Wolman et al., 1994) and prior research on the use of the AIR-SD with transition age individuals with ASD indicates that the measure is internally consistent and that the theoretical factor structure (subscales: opportunity and capacity) is supported (Chou, Wehmeyer, Shogren, Palmer, & Lee, 2017). Internal consistency for parent-reported AIR-SD scores in this sample was strong (α = .83).
Social Responsiveness Scale-Second Edition-Adult: Other Report (SRS-2; Constantino, 2012)
The SRS-2 is a measure of social impairment and ASD symptom severity. The measure, administered to the participants’ parents, yields five treatment subscales (social awareness, social cognition, social motivation, restricted interests and repetitive behavior). The measure can be completed in 15 minutes and has strong reliability and validity. Internal consistency for parent-reported SRS total scores for STEP 1 (α = .92) and STEP 2 (α = .97) were both excellent. The SRS-2 measures was administered prior to starting treatment and at the post-treatment assessment.
STEPS Program Satisfaction Survey (PSS)
Developed for this study, the PSS was completed at the post-treatment assessment. Five questions (helpfulness, impact, satisfaction with progress, acceptability, likelihood of recommending program to others) were rated on a 5-point (least to most helpful) Likert scale, such that higher scores indicate greater satisfaction.
Student Adaptation to College Questionnaire (SACQ; Baker & Siryk, 1999)
The SACQ is a self-report measure designed to examine postsecondary student adjustment in the academic, social, personal-emotional, and goal commitment domains. The measure has strong psychometric properties (Baker & Siryk, 1999) and is comprised of 67 items, all of which are on a 9-point Likert scale. Higher scores reflect better adjustment to the postsecondary setting. Internal consistency for baseline self-reported SACQ total scores was adequate, (α = .77). Although not developed specifically for students on the spectrum, a prior study found it to be psychometrically strong in a sample of college students with ASD (White et al., 2016b) and Trevisan and Birmingham (2016) found that undergraduate students with high levels of ASD traits scored significantly lower on academic and social adjustment to college using the SACQ. For STEP 2 students, the SACQ was the primary measure of treatment outcome.
Transition Readiness Scale (TRS; Elias & White, 2017)
The TRS is a 30-item measure available in student, parent, and educator formats. For this study, only the parent-report data were used because cell sizes were too small for meaningful analyses of student or educator TRS data. The measure was created for the purposes of this study as there are no measures, to our knowledge, assessing transition to adulthood in individuals with ASD are available. Polytomous Likert items were rated on a 4-point scale. The measure is comprised of 30 items, which assess student’s readiness to enter college from high-school across 3 domains: cognitive (expectancies, awareness), emotional (worries, fears about transition), and behavioral (possession of skills needed for success in college). Internal consistency for baseline parent-reported transition readiness was acceptable (α = .85). The TRS was the primary measure of treatment outcome for STEP 1 students.
Wechsler Abbreviated Scale of Intelligence, Second Edition (WASI-II; Wechsler, 2011)
The WASI-II provides an estimate of general cognitive ability. A clinician administered the two-subtest form in order to derive a Full Scale IQ score (FSIQ) at the pre-treatment assessment session to determine study eligibility. Four-subtest and two-subtest WASI-2 scores correlate highly for both children ages 12 to 17 and adults (Wechsler, 2011), and the two subtests have strong reliability and validity (Wechsler, 2011).
Data Analysis
IBM SPSS Statistics Version 24 was used for preliminary analyses and descriptive statistics. In order to investigate possible condition differences among demographic variables, we used a series of independent samples t-tests for the continuous variables and chi square analyses for the nominal variables. The nested nature of the data structures (i.e., repeated measures within participants over time) rendered two-level hierarchical linear models (HLM) an appropriate statistical approach (Raudenbush & Bryk, 2002). HLM models for change were fitted separately for STEP 1 and STEP 2 participants. The dependent variable (primary outcome) for STEP 1 was parent-reported total score on the TRS and the dependent variable for STEP 2 was the total T-score of the SACQ (primary outcome). Level-1 units consisted of measurement occasions (timepoints) and the level-2 units were participants. The treatment condition and other independent variables of interest were used as level-2 predictors to examine individual differences on initial status and treatment effects. Condition (i.e., STEPS versus TAU) was the primary level-2 predictor and the independent variables of interest included IQ, ASD symptom severity, severity of behavioral problems, and self-determination score. All multilevel model analyses for change were conducted using HLM7 Software (Raudenbush, Bryk, Cheong, Congdon, & Du Toit, 2011).
Treatment efficacy and correlates of effects were evaluated through a three-step process following the taxonomy of statistical models (Singer & Willett, 2003). That is, we first evaluated a baseline model containing only treatment condition as the level 2 predictor. We then added other independent variables of interest to the model, including IQ, parent-reported SRS-2 total score (ASD severity), and ASEBA total problems (emotional/behavioral problems). Third, we added self-determination total scores (AIR-SD) to the model, which was measured at pre-treatment; self-determination was a central component of the program, and was predicted to be related to transition readiness and college adjustment (primary outcomes), respectively. Models constructed for STEP 1 and STEP 2 participants were evaluated separately and are reported below.
It should be noted that, unlike repeated measures analysis of variance (ANOVA; Howell, 2013), which requires complete data for each participant, HLM allows missing observations at level 1. Intent-to-treat analyses of treatment effects were conducted using all enrolled individuals (n = 59) with pre-treatment data, regardless of attrition or infidelity to the STEPS program. That is, despite missing observations at certain measurement occasions, which is inevitable in longitudinal designs because of attrition, no participants were eliminated so long as they had at least one observation at certain measurement occasions. HLM is a suitable methodology for the intent-to-treat analyses since it makes an efficient estimation by utilizing all the available data even for the cases with only a single observation, and the estimates are valid (i.e., asymptotically unbiased) when missingness occurs at random (MAR; Little & Schenker, 1995) which is a less restrictive assumption compared to the missing completely at random (MCAR; Little & Rubin, 1987) assumption. MAR means that missingness may be nonrandom but the association between the probability of missingness and the missing value is explainable by the observed data. Further, even when MAR is not satisfied, robustness of the results is maximized when all available data are used in the analysis (Schafer, 1997). Despite the advantages of HLM with regard to robustness of results derived from incomplete data, attrition was substantial. As described above, participants were defined as having completed treatment based on completion of at least one measure at post-treatment. In some instances, the completed measure was not the primary outcome measure. Post-treatment TRS scores were available for 58% of STEP 1 study completers, and SACQ scores were available for 48% of STEP 2 completers.
STEP 1
Five time points were utilized for the growth model: pre-treatment, three time points during treatment spaced approximately two weeks apart, and a post-treatment time point that occurred approximately two weeks after program completion. The level-1 model was specified as a piecewise growth model, where two separate straight lines were connected at a time point, referred to as the node (Snijders & Boskers, 2012). The two slopes were represented as the regression coefficients of the two time variables included in the level model (Time 1 and Time 2). The Time 1 variable was coded as 0, 1, 2, 3, 3, and the Time 2 variable was coded 0, 0, 0, 0, 1, with each unit representing approximately four weeks; this coding scheme reflected the overall duration of treatment and post-treatment assessment. The two slopes represent the effect of the program from baseline to cessation of treatment and the maintenance of treatment from cessation of treatment to follow-up. Thus, the coefficient for Time 1 can be interpreted as the immediate treatment effects [i.e., change in transition readiness from pre- to post-treatment] while the coefficient for Time 2 can be interpreted as the maintenance of treatment effect from the final treatment time point through post-treatment assessment. This level 1 model was maintained throughout the three models that were fitted (i.e., Model 1, Model 2, and Model 3) for STEP 1. Finally, we evaluated the total treatment effect from pre- to post-treatment using a Wald test using the baseline model (Model 1).
STEP 2
For STEP 2, four time points were used to conduct the multilevel growth model analysis: pre-treatment, two mid-treatment time points, and a post-treatment time point. Similar to STEP 1, the level-1 model was specified as piecewise growth model using two time variables (Time 1 and Time 2). Assessment time points for STEP 2 consisted of pre-treatment, two mid-treatment time points, and a post-treatment time point. Thus, the Time 1 variable (Time 1) was coded as 0, 2, 3, 3 and the Time 2 variable (Time 2) was coded as 0, 0, 0, 1, where one unit represented approximately four weeks and the node was chosen as wave 3 (program cessation). The coefficient of Time 1 variable captured changes in college adjustment (SACQ) during treatment and the coefficient of Time 2 variable captured the sustained effect following treatment. This level 1 model was maintained throughout the three models that were fitted (i.e., Model 1, Model 2, and Model 3) for STEP 2. Again, a Wald test was used to examine the significance of the overall effect of the program using the baseline model (Model 1). Significance level for all analyses was set at α = 0.05 with two-tailed test; however, results at the α= 0.10 level with two-tailed test will also be mentioned given the rather small samples and the directional nature of our hypotheses.
Results
Across condition (STEPS vs TAU), there were not significant differences in participant sex, χ2 (1, 59) = .09, p = .77; race, χ2(3, 59) = .47, p =.79; cognitive ability, t = .44, p =.67; or ASD severity at baseline, t(44), −.54, p = .59 (Table 1). Before conducting the HLM growth model analysis, we looked at the descriptive statistics of the dependent variable for each program (i.e., TRS for STEP 1 and SACQ for STEP 2). Prior to intervention, there was no statistical difference on the mean level of the dependent variable between the treatment and control groups (STEP 1 TRS: t = .48, p = .63; STEP 2 SACQ: t = .57, p = .57), indicating that the random assignment worked as intended.
Feasibility
Program acceptability, as defined by less than 15% attrition, was achieved in both programs. Specifically, 87% of students in STEP 1 and 88.9% of students in the TAU condition completed (one participant was hospitalized for acute psychiatric concerns and one participant ceased responding to investigator telephone calls without a reason given; the one TAU drop also ceased responding to calls with no reason given). In STEP 2, 91.4% completed the RCT: 94% in STEPS and 88.9% in TAU. The STEPS drop was due to the student transferring schools, and the two TAU drops were due to one student failing to respond to repeated calls and one withdrawing due to stated lack of time. Overall, 89.8% of participants completed the trial.
In terms of program acceptability based on PSS responses, for STEP 1, 75% of students and 92.3% of parents reported that they found the program either “somewhat” or “very” helpful. Regarding impact, 75% of students and 84.62% of parents indicated that they found the program to provide “good” or “great” benefit. For STEP 2, 88.24% of students and 90% of parents reported that they found the program either “somewhat” or “very” helpful. Regarding impact, 70.59% of students and 90% of parents indicated that they found the program to provide “good” or “great” benefit (Table 2).
Table 2.
Program Helpfulness and Impact Ratings.
| Helpfulness: | Not at all % (n) | Not that helpful % (n) | Moderately % (n) | Somewhat % (n) | Very % (n) | Overall M (SD) |
| 1 | 2 | 3 | 4 | 5 | ||
|
| ||||||
| STEP 1 | ||||||
|
| ||||||
| Student | 0 | 0 | 33% (4) | 16.67 % (2) | 50% (6) | 4.17 (0.94) |
|
| ||||||
| Parent | 0 | 0 | 8.7% (2) | 26.09% (6) | 65.22% (15) | 4.46 (0.66) |
|
| ||||||
| STEP 2 | ||||||
|
| ||||||
| Student | 5.88% (1) | 0 | 5.88% (1) | 29.41% (5) | 58.82% (10) | 4.41 (0.87) |
|
| ||||||
| Parent | 0 | 0 | 10% (1) | 10% (1) | 80% (8) | 4.70 (0.68) |
|
| ||||||
| Impact: | No benefit % (n) | Minimal % (n) | Moderate % (n) | Good % (n) | Great % (n) | Overall M (SD) |
| Score | 1 | 2 | 3 | 4 | 5 | |
|
| ||||||
| STEP 1 | ||||||
|
| ||||||
| Student | 0 | 8.33% (1) | 25% (3) | 41.67% (5) | 25% (3) | 3.83 (0.94) |
|
| ||||||
| Parent | 0 | 0 | 18.18% (2) | 72.73% (8) | 27.27% (3) | 4.08 (0.64) |
|
| ||||||
| STEP 2 | ||||||
|
| ||||||
| Student | 0 | 11.76% (2) | 17.65% (3) | 29.41% (5) | 41.18% (7) | 4.0 (1.06) |
|
| ||||||
| Parent | 0 | 10% (1) | 0 | 20% (2) | 70% (7) | 4.50 (0.97) |
|
| ||||||
Fidelity to session objectives was coded (by the delivering therapist) after each session. In addition, an independent rater co-coded 20% of all treatment sessions, such that all treatment modules were coded at least once and at least two sessions from each participant were co-coded. Interrater reliability was greater than 90% for both STEPS. Primary analyses used therapist-rated fidelity. Average session fidelity to objectives (i.e., program integrity) was above 90% for both STEP 1 and STEP 2, in accordance with the first hypothesis. For STEP 1, therapist-rated fidelity to stated program objectives for each module ranged from 50–100% (M = 93.33%, SD = 12.47), with 76.3% of rated sessions meeting 100% of objectives. For STEP 2, fidelity ranged from 0–100% (M = 93.58%, SD = 16.83), with 85% of rated sessions meeting all stated objectives. Only one session had no objectives met; during the session the participant presented with acute symptoms that warranted attention and precluded completion of STEPS program content. Across both STEPS, session fidelity ranged from 0–100% (M = 93.61%, SD = 15.82%), and 83.20% of rated sessions met all objectives.
Efficacy
STEP 1
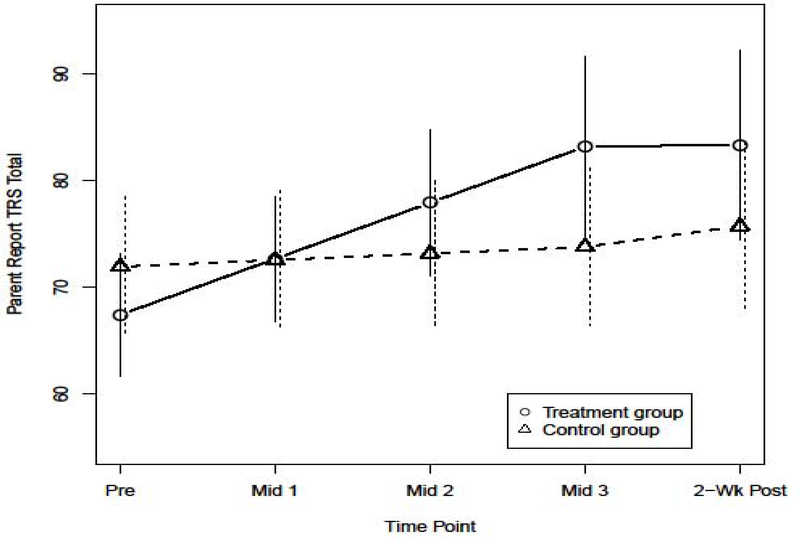
In the baseline model (Model 1), the condition variable was the sole predictor at level-2 for each initial status, the Time 1 slope, and the Time 2 slope. The baseline model indicated a significant immediate positive treatment effect (b = 4.64, p = .02). The long-term effect represented as the coefficient for Time 2 suggested that treatment effects did not diminish over time, though there was a tendency for transition readiness to decline toward baseline (b = −1.75, p = 0.76). Based on the Model 1 results (Table 3), the average trajectories for each condition are depicted in Figure 2.
Table 3.
HLM Results for STEP 1 Data
| Fixed Effects | Baseline (Model 1) | With L-2 Predictors (Model 2) | SD added (Model 3) | |
|---|---|---|---|---|
| Initial Status | Intercept | 71.95** | 73.26** | 71.09** |
| Treatment | −4.52 | 1.88 | 1.97 | |
| IQ | 0.04 | 0.02 | ||
| ASD Severity | −0.55* | −0.50* | ||
| Mental Health | −0.34 | −0.19 | ||
| Self-Determination | 0.59 | |||
| Time 1 Slope | Intercept | 0.62 | 2.16 | 0.54 |
| Treatment | 4.64** | 4.61* | 5.45** | |
| IQ | −0.05 | −0.06 | ||
| ASD Severity | 0.18 | 0.18 | ||
| Mental Health | −0.10 | 0.02 | ||
| Self-Determination | 0.34 | |||
| Time 2 Slope | Intercept | 1.94 | 1.32 | 1.07 |
| Treatment | −1.75 | −2.65 | −2.29 | |
| IQ | ||||
| ASD Severity | ||||
| Mental Health | ||||
| Self-Determination | ||||
|
| ||||
| Variance Components | ||||
|
| ||||
| Level 1 | Within-Person | 47.64** | 50.13** | 50.45** |
| Level 2 | In initial status | 89.55** | 27.94** | 28.11** |
| In Time 1 Slope | 4.02~ | 0.99 | 0.31 | |
| In Time 2 Slope | N.A. (fixed) | N.A. (fixed) | N.A. (fixed) | |
p<0.01
p<0.05
p<0.10
p values are based on t test for fixed effects parameters and z test for variance component parameters
Figure 2. Transition Readiness (TRS) Change over time for STEP 1 TAU.
Note. The vertical lines represent a 95 % confidence interval on the predicted mean at each time point for respective group.
Statistically significant residual variation on initial status and Time 1 slope was observed, but no statistically significant residual variation (at the 0.10 significance level) was indicated, so it was fixed throughout the analyses. In Model 2, in which we included IQ, ASD symptom severity, and total problem behaviors as independent variables, the positive treatment effect remained stable (b = 4.61, p = .04). Results indicated no independent variables other than condition (STEP 1 vs TAU) significantly predicted changes in transition readiness at the α < .05 level. ASD severity was a statistically significant predictor for initial status (b = −0.55, p = .02), suggesting that greater ASD severity predicted lower transition readiness at the outset of treatment. The third model (Model 3), which added self-determination scores, again suggested a significant positive treatment effect (b = 5.45, p = .02), and indicated no significant predictors of change other than treatment condition. ASD severity remained a significant predictor of the initial transition readiness (b = −0.50, p = .04). The Wald test examining the overall treatment effect (i.e., improvement in scores from pre-treatment, through post-treatment, to follow-up) indicated that STEP 1 significantly improved parent-reported TRS scores from pre-treatment through to follow-up, χ2(1) = 4.52, p = .03 (two-tailed).
STEP 2
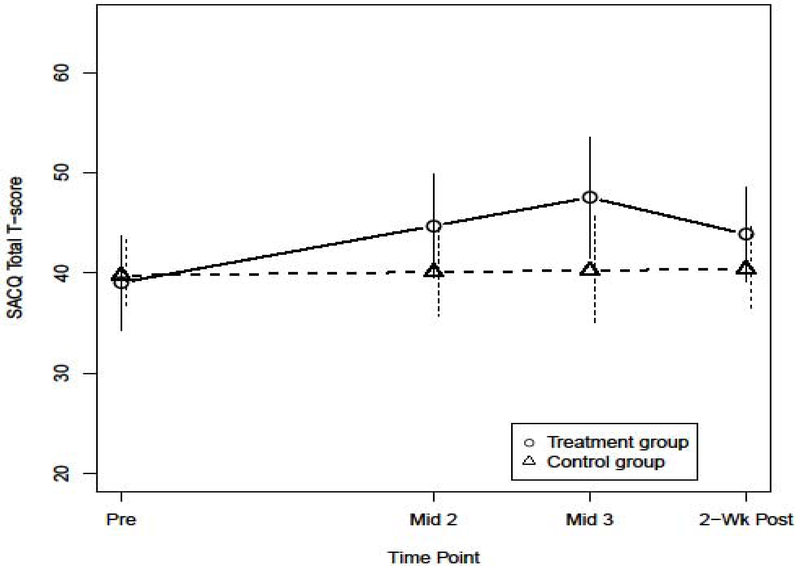
The results of the baseline model (Model 1) suggested a significant and positive immediate treatment effect (b = 2.67, p = .02). The Time 2 slope indicated decline in adjustment following program cessation, but it was not statistically significant at the 0.05 level (b = - 3.80, p = 0.198, two-tailed), suggesting that significantly improved college adjustment from baseline was maintained at the end of the follow-up period. The Wald test evaluating overall treatment effect indicated that there was not statistically significant improvement associated with receipt of STEPS, χ2(1) = 3.37, p = .06 (two-tailed). Although we conclude that there is not enough evidence to indicate an overall treatment effect for STEP 2 at the 0.05 significance level, considering the fact that the test marginally missed the conventional .05 level with a two-tailed test, that the immediate effect was significant (b = 2.67, p = .02), and that the sample size is relatively small, we interpret these results cautiously. Based on the Model 1 results (Table 4), the average trajectories for each treatment condition are depicted in Figure 3.
Table 4.
HLM Results for STEP 2 Data
| Fixed Effects | Baseline (Model 1) | With L-2 Predictors (Model 2) | SD added (Model 3) | |
|---|---|---|---|---|
| Initial Status | Intercept | 39.77** | 44.69** | 37.55** |
| Treatment | −0.73 | −1.65 | 1.21 | |
| IQ | −0.14 | −0.24 | ||
| ASD Severity | 0.01 | 0.09 | ||
| Mental Health | −0.44 | −0.14 | ||
| Self-Determination | 0.54 | |||
| Time 1 Slope | Intercept | 0.16 | −1.48 | 2.17 |
| Treatment | 2.67* | 3.16* | 2.13* | |
| IQ | 0.07~ | 0.10* | ||
| ASD Severity | 0.08 | 0.03 | ||
| Mental Health | −0.05 | −0.17** | ||
| Self-Determination | −0.21~ | |||
| Time 2 Slope | Intercept | 0.13 | 8.51 | 3.13 |
| Treatment | −3.80 | −3.97~ | −3.04 | |
| IQ | −0.04 | −0.11 | ||
| ASD Severity | −0.55** | −0.49** | ||
| Mental Health | 0.04 | 0.13 | ||
| Self-Determination | 0.35** | |||
|
| ||||
| Variance Components | ||||
|
| ||||
| Level 1 | Within-Person | 13.34** | 5.09** | 6.07** |
| Level 2 | In initial status | 46.50** | 52.40** | 73.93** |
| In Time 1 Slope | 1.79** | 3.93** | 1.09** | |
| In Time 2 Slope | 3.94* | 4.23 | 1.04 | |
p<0.01
p<0.05
p<0.10
p values are based on t test for fixed effects parameters and z test for variance component parameters
Note: HLM, full ML
Note. Robust Standard Error was used to conduct t tests
Figure 3. College Adjustment Score (SACQ) Change over time for STEP 2.
Note. The vertical lines represent a 95 % confidence interval on the predicted mean at each time point for respective group.
In terms of the variance component parameters, statistically significant residual variation on all the growth parameters such as initial status, Time 1 slope, and Time 2 slope were observed. In Model 2 and Model 3, the independent variables were added to each of the growth parameters. In Model 2, in which we included IQ, SRS-2 scores, and ABCL scores, the immediate treatment effect remained significant and positive (b = 3.16, p = .02). The effect of IQ on Time 1 slope was not significant (b = 0.07, p = 0.10). The sustained effect of the program was negative and statistically significant at 0.10 level (b = −3.97, p = 0.10), which indicates that there was some level of regression of the immediate treatment effect on college adjustment following program completion. SRS-2 scores negatively predicted sustained treatment effect (b = - 0.55, p < .001), suggesting that more severely affected individuals evidenced a larger decline in adjustment after cessation. In Model 3, where self-determination was added to the model, the immediate treatment effect remained statistically significant (b = 2.13, p = .04), though the size of the effect decreased. When controlling for self-determination scores, the effect of IQ slightly increased (b = 0.10, p = .02), suggesting that greater cognitive abilities were associated with steeper increases in college adjustment during intervention. Similarly, the effects of behavioral problems measured by ABCL scores on Time 1 slope became larger in absolute value and statistically significant (b = - 0.17, p = .002). This result suggests that changes in college adjustment were smaller for those with more behavioral or mental health problems, when further controlling for pre-treatment levels of self-determination. Finally, the effect of self-determination scores was also statistically significant at the more conservative 0.l0 level and negative (b = - 0.21, p = .07). Although the coefficient of Time 2 did not indicate significant decline in program effect over time, higher ASD severity predicted declines in college adjustment after program cessation (b = - 0.40, p < .001), and higher self-determination scores predicted increases in college adjustment (b = 0.35, p = .005) even after program completion.
Finally, in order to assess the practical significance of the treatment effect, we considered treatment effect size (ES), based on the mean change in treatment group () and that in the control group () divided by estimated pooled standard deviation of change scores. From this formula, we obtained standardized ES for the immediate treatment effect (d1, pre to Mid 3) and the overall treatment effect (d2, pre to Post-treatment). For STEP 1, d1 = 2.034 and d2 = 0.881. For STEP 2, d1 = 1.248 and d2 = 0.644. These ES estimates indicate that STEPS produces very large, immediate effects and moderate to large effects for two weeks after intervention cessation.
Discussion
There is a growing population of young adults with ASD and little in the way of evidence-based programming to support their needs related to higher education and independent adulthood (Elias & White, 2018; White et al., 2011). The Interagency Autism Coordinating Committee identified the need for development of services to support transition to adulthood as its first objective within the domain of lifespan research (IACC, 2017), in part because adults with ASD are less likely to take steps to prepare for further training, college, or employment on their own (U.S. Department of Health and Human Services, 2017). STEPS is a consumer-informed and empirically based curriculum designed to address transition-related needs of adolescents and young adults with ASD. We hypothesized that STEPS would be feasible to implement, acceptable to consumers, and efficacious with respect to impact on transition readiness and college adjustment. Results from this preliminary RCT support these hypotheses - STEPS was both efficacious and acceptable to students and their parents.
High school students who received STEP 1 demonstrated increased readiness for transition relative to students in the control condition. Moreover, levels of readiness did not decline to pre-treatment levels after program completion. Similarly, students who received STEP 2, which is for individuals who have exited secondary education, evinced increases in college adjustment relative to students in the control condition. Likewise, although gains diminished somewhat after program completion, there is evidence for longevity of program effects. Although the derived p-value was 0.06, this is close to the conventional 0.05 level of significance and based on the two-tailed test. As such, we cautiously infer some support for the overall effect of STEP 2. Student-specific variables, including cognitive ability, ASD severity, and secondary behavioral problems, did not predict response to STEP 1. However, behavioral and mental health problems dampened response to STEP 2 when effects of self-determination were controlled for. Self-determination also predicted retention of gains made during STEP 2 after program completion. ASD severity, on the other hand, predicted a steeper decline in adjustment after program completion. Findings suggests that mental health difficulties, which frequently present among cognitively able adults with ASD (White et al., 2018), as well as core symptoms (e.g., social impairments) of ASD, may need to be addressed therapeutically in order to maximize the impact of transition services for this population.
In terms of feasibility and acceptability, the high retention rate (>85%) and our finding that the majority of both parents and students report at least moderate benefit suggest that STEPS is acceptable. Curriculum integrity (or fidelity of implementation) is another indicator of feasibility. Across all sessions, average fidelity to program objectives exceeded 90%.
Although this study is novel given the dearth of research in this area, it is not without limitations. Outcome measures were completed by participants and their parents, and both groups were aware of their assigned treatment condition. Relatedly, there are no published measures to assess readiness for transition from secondary education related to the goals of the program; as such, one of our primary outcome measures (the TRS) was developed specifically for this study. Missing data was also considerable across timepoints, and longer term monitoring would be ideal to determine whether or not changes were sustained. Another limitation is the lack of data available on services received and hours of services received for participants in TAU, which limits our ability to fully characterize the TAU group. The sample is quite homogeneous with respect to race and SES, making generalizability to minority students, including first generation college students, uncertain. Additionally, for STEP 2 outcomes, effects are not statistically significant based on a conservative threshold. Further research, using larger and more diverse samples, is needed to replicate these findings and possibly extend STEPS to those with cognitive or verbal impairment.
In conclusion, the majority of cognitively capable adults with ASD have difficulty maintaining engagement in higher education or employment (Taylor, Henninger, & Mailick, 2015). STEPS is a unique contribution to the transition literature. Specifically, STEPS serves as one of the few empirically based postsecondary support programs targeting adolescent and emerging adult students with ASD. STEPS was found to be highly acceptable to students and to their parents, and counselors were able to implement sessions with fidelity to the manualized curriculum. There was a significant effect of STEPS on targeted primary outcomes, specifically readiness for transition among secondary school students in STEP 1 and college adjustment among students in STEP 2. Larger scale, multi-site evaluation of STEPS will inform how scalable STEPS is and how sustainable treatment gains are for this growing population.
References
- Achenbach TM (1991). Manual for the Child Behavior Checklist/4–18 and 1991 profile (p. 288). Burlington, VT: Department of Psychiatry, University of Vermont. [Google Scholar]
- Arnett JJ (2000). Emerging adulthood: A theory of development from the late teens through the twenties. American Psychologist, 55(5), 469–480. [PubMed] [Google Scholar]
- Arnett JJ (2010). Emerging adulthood (s). Bridging Cultural and Developmental Approaches to Psychology: New Syntheses in Theory, Research, and Policy, 255–275. [Google Scholar]
- Baio J, Wiggins, Christensen DL, Maenner MJ, Daniels J, Warren Z, …Dowling NF (2018). Prevalence of autism spectrum disorder among children aged 8 years – Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2014. MMWR Survell Summ 2018, 67(No. SS-6): 1–23. doi: 10.15585/mmwr.ss6706a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker RW, & Syrik B (1999). Student Adaptation to College Questionnaire (SACQ). Los Angeles, CA: Western Psychological Services. [Google Scholar]
- Billstedt E, Gillberg C, & Gillberg C (2005). Autism after adolescence: Population-based 13- to 22-year follow-up stud of 120 individuals with autism diagnosed in childhood. Journal of Autism and Developmental Disorders, 35(3), 351–360. doi: 10.1007/s10803-005-3302-5 [DOI] [PubMed] [Google Scholar]
- Brown TA, & Barlow DH (2014). Anxiety and related disorders interview schedule for DSM-5. (ADIS-5)—Adult and Lifetime version. [Google Scholar]
- Chambers CR, Wehmeyer ML, Saito Y, Lida KM, Lee Y, & Singh V (2007). Self-determination: What do we know? Where do we go? Exceptionality, 15(1), 3–15. [Google Scholar]
- Chou Y, Wehmeyer ML, Shogren KA, Palmer SB, & Lee J (2017). Autism and self-determination: Factor analysis of two measures of self-determination. Focus on Autism and Other Developmental Disabilities, 32(3), 163–175. doi: 10.1177/1088357615611391 [DOI] [Google Scholar]
- Constantino JN (2012). Social Responsiveness Scale, Second Edition (SRS-2). Los Angeles, CA: Western Psychological Services. [Google Scholar]
- Corbett BA, Constantine LJ, Hendren R, Rocke D, & Ozonoff S (2009). Examining executive functioning in children with autism spectrum disorder, attention deficit hyperactivity disorder and typical development. Psychiatry Research, 166(2–3), 210–222. Doi: 10.1016/j.psychres.2008.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czajkowski SM, Powell LH, Adler N, Naar-King S, Reynolds KD, Hunter CM, … Charlson ME (2015). From ideas to efficacy: The ORBIT model for developing behavioral treatments for chronic diseases. Health Psychology, 34(10), 971–982. Doi: 10.1037/hea0000161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elias R, Muskett A, & White SW (2017). Short report: Educator perspectives on the postsecondary transition difficulties of students with autism. Autism: International Journal of Research and Practice. Advance online publication. doi: 10.1177/1362361317726246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elias R & White SW (November 2017). Development of the Transition Readiness Scale. Poster presented at the Association for Behavioral and Cognitive Therapy (ABCT), New York, New York. [Google Scholar]
- Elias R & White SW (2018). Autism goes to college: Understanding the needs of a student population on the rise. Journal of Autism and Developmental Disorders, 48(3), 732–746. doi: 10.1007/s10803-017-3075-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farley MA, McMahon WM, Fombonne E, Jenson WR, Miller J, Gardner M, …Coon H (2009). Twenty-year outcome for individuals with autism and average or near-average cognitive abilities. Autism Research, 2, 109–118. doi: 10.1002/aut.69 [DOI] [PubMed] [Google Scholar]
- Hendricks DR, & Wehman P (2009). Transition from school to adulthood for youth with autism spectrum disorders. Focus on Autism and Other Developmental Disabilities, 24(2), 77–88. doi: 10.1177/1088357608329827 [DOI] [Google Scholar]
- Howell DC (2013). Statistical methods for psychology (8th ed.). Belmont, CA: Wadsworth. Interagency Autism Coordinating Committee (IACC). 2016–2017 Interagency Autism Coordinating Committee Strategic Plan for Autism Spectrum Disorder. October 2017. Retrieved from the U.S. Department of Health and Human Services interagency Autism Committee website: https://iacc.hhs.gov/publications/strategic-plan/2017/. [Google Scholar]
- Little RJA, & Rubin DB (1987). Statistical analysis with missing data. New York, NY: Wiley. [Google Scholar]
- Little RJA, & Schenker N (1995). Missing data. In Arminger G, Clogg CC, & Sobel ME (Eds.), Handbook of statistical modeling for the social sciences (pp. 39–75). New York, NY: Plenum Press. [Google Scholar]
- Lord C, Rutter M, DiLavore PC, Risi S, Gotham K, & Bishop SL (2012). Autism diagnostic observation schedule (ADOS-2) (2nd ed.). Torrence, CA: Western Psychological Services. [Google Scholar]
- Mazefsky CA, Herrington J, Siegel M, Scarpa A, Maddox BB, Scahill L, & White SW (2013). The role of emotion regulation in autism spectrum disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 52(7), 679–688. doi: 10.1016/j.jaac.2013.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazefsky CA & White SW (2014). Adults with autism. In Volkmar FR, Paul R, Rogers SJ, & Pelphrey KA (Eds.), Handbook of autism spectrum disorders, 4th Ed. (pp. 191–211). Hoboken, NJ: Wiley and Sons. [Google Scholar]
- Moerbeek M (2005). Randomization of clusters versus randomization of persons within clusters: which is preferable?. The American Statistician, 59(2), 173–179. doi: 10.1198/000313005X43542 [DOI] [Google Scholar]
- National Institute of Mental Health (2015). The National Institute of Mental Health Strategic Plan for Research. Retrieved from https://www.nimh.nih.gov/about/strategic-planning-reports/nimh_strategicplanforresearch_508compliant_corrected_final_149979.pdf (June 23, 2019).
- Nicolaidis C, Raymaker D, McDonald K, Dern S, Ashkenazy E, Boisclair S, … Baggs A (2011). Collaboration strategies in nontraditional community-based participatory research partnerships: Lessons from an academic-community partnership with autistic self-advocates. Progress in Community Health Partnerships, 5(2), 143–150. doi: 10.1353/cpr.2011.0022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piacentini J, Bennett S, Compton SN, Kendall PC, Birmaher B, Albano A, … Walkup J (2014). 24- and 36-week outcomes for the Child/Adolescent Anxiety Multimodal Study (CAMS). Journal of the American Academy of Child & Adolescent Psychiatry, 53(3), 297–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raudenbush SW, & Bryk AS (2002). Hierarchical linear models: Applications and data analysis methods (2nd ed.). Thousand Oaks, CA: Sage. [Google Scholar]
- Raudenbush S, Bryk A, Cheong YF, Congdon R, & du Toit M (2011). HLM7: Hierarchical linear and nonlinear modeling. Chicago, IL: Scientific Software International. [Google Scholar]
- Schafer JL (1997). Analysis of incomplete multivariate data. London: Chapman & Hall. [Google Scholar]
- Silverman WK, & Albano AM (in press). Anxiety Disorders Interview Schedule for DSM-5 (Child and Parent Versions). San Antonio, TX: Psychological Corporation. [Google Scholar]
- Singer JD & Willett JB (2003). Applied Longitudinal Data Analysis: Modeling Change and Event occurrence. New York, NY: Oxford University Press. [Google Scholar]
- Smith LE, Maenner MJ, & Seltzer MM (2012). Developmental trajectories in adolescents and adults with autism: The case of daily living skills. Journal of the American Academy of Child & Adolescent Psychiatry, 51(6), 622–631. doi: 10.1016/j.jaac.2012.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith T, Scahill L, Dawson G, Guthrie D, Lord C, Odom S, … Wagner A (2007). Designing research studies on psychosocial interventions in autism. Journal of Autism and Developmental Disorders, 37(2), 354–366. doi: 10.1007/s10803-006-0173-3 [DOI] [PubMed] [Google Scholar]
- Snijders TAB, & Bosker RJ (2012). Multilevel analysis: An introduction to basic and advanced multilevel modeling, second edition. London, UK: Sage Publishers. [Google Scholar]
- Taylor JL, Henninger NA, & Mailick MR (2015). Longitudinal patterns of employment and postsecondary education for adults with autism and average-range IQ. Autism, 19(7), 785–793. doi: 10.1177/1362361315585643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor JL, & Seltzer MM (2010). Changes in the autism behavioral phenotype during the transition to adulthood. Journal of Autism and Developmental Disorders, 40(12), 1431–1446. doi: 10.1007/s10803-010-1005-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor JL, & Seltzer MM (2011). Employment and post-secondary educational activities for young adults with autism spectrum disorders during the transition to adulthood. Journal of Autism and Developmental Disorders, 41(5), 566–574. doi: 10.1007/s10803-010-1070-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trevisan D, & Birmingham E (2016). Examining the relationship between autistic traits and college adjustment. Autism, 20(6), 719–729. doi: 10.1177/1362361315604530 [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services (2017). Report to Congress: Young Adults and Transitioning Youth with Autism Spectrum Disorder. October 2017. Retrieved from the U.S. Department of Health and Human Services; website: https://www.hhs.gov/sites/default/files/2017AutismReport.pdf [Google Scholar]
- Wechsler D (2011). Wechsler Abbreviated Scale of Intelligence–Second Edition (WASI-II). San Antonio, TX: NCS Pearson. [Google Scholar]
- Wehman P, Schall C, Carr S, Targett P, West M, & Cifu G (2014). Transition from school to adulthood for youth with autism spectrum disorder: What we know and what we need to know. Journal of Disability Policy Studies, 25(1), 30–40. doi: 10.1177/1044207313518071 [DOI] [Google Scholar]
- Wehmeyer ML, & Palmer SB (2003). Adult outcomes for students with cognitive disabilities three-years after high school: The impact of self-determination. Education and Training in Developmental Disabilities, 38(2), 131–144. [Google Scholar]
- Wei X, Yu JW, Shattuck P, McCracken M, & Blackorby J (2013). Science, technology, engineering, and mathematics (STEM) participation among college students with an autism spectrum disorder. Journal of Autism and Developmental Disorders, 43, 1539–1546. doi: 10.1007/s10803-012-1700-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- White SW, Elias R, Capriola-Hall NN, Smith IC, Conner CM, Asselin SB, Howling P, Getzel EE, & Mazefsky CA (2017). Development of a college transition and support program for students with autism spectrum disorder. Journal of Autism and Developmental Disorders, 47(10), 3072–3078. doi: 10.1007/s10803-017-3236-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- White SW, Elias RE, Salinas CE, Capriola N, Conner CM, Asselin SB, Miyazaki Y, Mazefsky CA, Howlin P, & Getzel EE (2016a). Students with autism spectrum disorder in college: Results from preliminary mixed methods needs analysis. Research in Developmental Disabilities, 56, 29–40. doi: 10.1016/j.ridd.2016.05.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- White SW, Ollendick T, Albano A, Oswald D, Johnson C, Southam-Gerow MA, Kim I, & Scahill L (2013). Randomized controlled trial: Multimodal anxiety and social skill intervention for adolescents with autism spectrum disorder. Journal of Autism and Developmental Disorders, 43(2), 382–394.doi: 10.1007/s10803-012-1577-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- White SW, Ollendick TH, & Bray BC (2011). College students on the autism spectrum: Prevalence and associated problems. Autism: The International Journal of Research and Practice, 15(6), 683–701. doi: 10.1177/1362361310393363 [DOI] [PubMed] [Google Scholar]
- White SW, Richey JA, Gracanin D, Coffman M, Elias R, LaConte S, & Ollendick TH (2016b). Psychosocial and computer-assisted intervention for college students with autism spectrum disorder. Education and Training in Autism and Developmental Disabilities, 51(3), 307–317. [PMC free article] [PubMed] [Google Scholar]
- White SW, Simmons GL, Gotham KO, Conner CM, Smith IC, Beck K, & Mazefsky CA (2018). Psychosocial treatments targeting anxiety and depression in adolescents and adults on the autism spectrum: Review of the latest research and recommended future directions. Current Psychiatry Reports, 20(82). doi: 10.1007/s11920-018-0949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolman JM, Campeau PL, DuBois PA, Mithaug DE, & Stolarski VS (1994). AIR Self-Determination Scale and user guide. Washington, DC: American Institutes for Research. [Google Scholar]