Abstract
Objective:
We aimed to assess the feasibility of teleneurorehabilitation (TNR) among persons with Parkinson's disease (PD), considering difficulties imposed by the COVID-19 pandemic in access to healthcare, particularly in low-resource settings. The feasibility of TNR in India has not been formally assessed so far.
Methods:
We conducted a single-center, prospective cohort study at a tertiary center in India. Persons with PD with Hoehn & Yahr (H&Y) stages 1-2.5, who were not enrolled into any formal exercise program, were offered TNR as per a predesigned program for 12 weeks. Baseline and post-intervention assessment included Movement Disorders Society-Unified Parkinson's Disease Rating Scale (MDS-UPDRS), part II and III, Parkinson's Disease Questionnaire (PDQ)-8 and Non-Motor Symptoms Scale (NMSS). We assessed adherence to TNR and problems expressed by patients/caregivers by means of open-ended surveys addressing barriers to rehabilitation.
Results:
We recruited 22 for TNR. Median age (interquartile range [IQR]) was 66.0 (44.0-71.0) years; 66.7% were H&Y stage 2.0. One patient died of COVID-19-related complications. Of the remaining 21, 14 (66.7%) had adherence of ≥75%; 16/21 (76.2%) patients had problems with attending TNR sessions as the family shared a single phone. Slow Internet speed was an issue among 13/21 (61.9%) of the patients. Other issues included lack of rapport, migration to distant hometowns and motor-hand impairment.
Conclusion:
Multiple challenges were faced in implementing a telerehabilitation program among persons with PD, exacerbated by the COVID-19 pandemic. These barriers were present at various levels: recruitment, adherence issues and maintenance. Future TNR programs must address these concerns.
Keywords: COVID-19, MDS-UPDRS, Non-Motor Symptoms Scale, PDQ-8, telemedicine, telerehabilitation
INTRODUCTION
The ongoing COVID-19 pandemic has enforced radical metamorphoses in healthcare with deep, and likely, long-lasting impacts on healthcare.[1,2] Persons with Parkinson's disease constitute a particularly vulnerable patient subgroup due to multiple reasons: they have inherent mobility issues, emotional vulnerability and susceptibility to loneliness compounded by pandemic-related lockdowns as well as immunological concerns increasing propensity to COVID-19 infection.[3] In low-resource settings such as India, non-availability of medications, lack of access to healthcare providers and their regular prescriptions has been shown to worsen various parameters, including motor- and non-motor symptoms and quality of life.[4,5] In the face of these massive concerns, rehabilitation is likely to be relegated relatively lower priority among these patients. However, rehabilitation forms an emerging and vital cornerstone of PD management and offers benefits in multiple aspects, including mobility, gait, speech and quality of life.[6]
Teleneurorehabilitation (TNR), a subset of telemedicine, has been shown to be a beneficial option among persons with PD.[7] TNR may be a potentially more feasible and economical option, the latter of practical implications in a low-resource country like India. In various studies in the literature, telerehabilitation has shown promise in specific aspects of PD, such as speech and language, voice, swallowing, posture and gait.[8,9,10,11] Despite the relatively small number of PD patients sampled in these reports, a few broad points have been consistently observed: technology-based strategies are feasible among patients with PD, and also have high satisfaction potential. There is paucity of literature from India assessing the potential of TNR in general, and for patients with PD in particular.
In this single-center, prospective study, we aimed to assess the feasibility of telerehabilitation among persons with PD. We present the barriers and challenges faced in conducting this study, with focus on impediments and putative solutions in a resource constrained setting.
MATERIAL AND METHODS
Study design
The study was designed as a prospective study of TNR in patients with PD. The study was conducted between September 2020 and January 2021. The study was approved by the Institutional Ethics Committee. Written informed consent was obtained from all the study participants.
Study participants
Participants were recruited from the outpatient Movement Disorders clinic of the Neurology department at a tertiary level referral center which caters to the population of Delhi and the adjacent National Capital Region. Eligible patients were 18 years or older, had been diagnosed to have idiopathic PD, had mild-to-moderate PD as defined by Hoehn and Yahr (H&Y) stage 1 to 2.5, score ≥24 on the Mini Mental State Examination, not enrolled into any formal rehabilitation or exercise program, and possessed a smartphone which would permit telerehabilitation via video calling. Patients were excluded if they had comorbid visual or hearing impairment which would preclude the ability to use the smartphone in order to undergo TNR, or if they refused consent.
Assessments
Participants received TNR via an Internet-connected device at home. Participants attended a 12-week structured rehabilitation program (detailed in Supplement 1). Informed consent was obtained in person. Baseline and post-intervention clinical assessments were conducted in person. Patients and caregivers were surveyed regarding their concerns about the study preceding enrollment by means of an open-ended questionnaire. Baseline clinical and demographic details were recorded. Movement Disorders Society-Unified Parkinson Disease Rating Scale (MDS-UPDRS) part II,[12] MDS-UPDRS part III,[12] Parkinson's Disease Questionnaire (PDQ)-8[13] and Non-Motor Symptoms Scale (NMSS)[14] wwere assessed at baseline and post-intervention. During TNR, patients were asked to enlist problems faced at every session and the results were noted.
Adherence to therapy was assessed as a percentage of the number of sessions during which the patients completed at least 20 minutes of the assigned 30 minutes. Patient and caregiver reports were used to determine adherence to the unsupervised sessions, and assessment by rehabilitation specialist for the supervised sessions. A satisfaction survey with multiple questions scored on a Likert scale was applied at the end of the intervention period.
Treatment
The participants underwent rehabilitation program in 30-minute sessions. Eight sessions were supervised—once a week for the first 4 weeks and once every 2 weeks for 8 weeks. The participant had to perform unsupervised sessions at home for at least five days per week (including the training session) and either the patient or their caretaker maintained a video log and PD diary regarding details of home-based program performed and adherence to the schedule. TNR was done in the “ON” state. Patients were advised to take the medicine before rehabilitation sessions to improve exercise capacity.
Participants attended a 12-week structured rehabilitation program. They underwent supervised rehabilitation program for a duration of 30 minutes in the department of Physical Medicine & Rehabilitation (PMR) on Day 1 followed by supervised tele rehabilitation once a week for the first 4 weeks and once every 2 weeks for 8 weeks. The participant had to perform therapeutic exercises at home for at least 5 days per week (including the training session) and either the patient or their caretaker maintained a video log and PD diary regarding details of home-based program performed and adherence to the schedule.
Baseline assessment:
Patient's physical fitness for performing therapeutic exercises will be assessed by a 6-minute walk[15] test to check for endurance (Supplement 2)
Assessment of balance by Functional Reach test (FRT)[16] (Supplement 3)
Need of any assistive device.
Rehabilitation included therapeutic exercises to improve postural control, active and assistive limb mobilization, flexibility training, aerobic exercises, balance and gait training. Patients were encouraged to exercise at a dyspnea score of about 3-4 (“moderate” to “somewhat severe”) on the modified Borg 0-10 scale (Supplement 4).
All the participants were provided with handouts of different therapeutic exercises in case they missed out any step and were encouraged to perform for at least 5 days a week throughout the 12-week period and maintain a logbook of exercises.
Statistical analysis
All data was entered into an Excel spreadsheet and analyzed using SPSS statistical software. Descriptive statistics were used to report demographic and clinical features, and clinical outcomes of the patients. Pre- and post-intervention measures were compared using Dependent t-test.
RESULTS
We screened 76 patients and could recruit 22 for TNR [Figure 1]. Key characteristics are enlisted in Table 1. Median age (interquartile range [IQR]) was 66.0 (44.0-71.0) years and median age (IQR) at onset was 63.0 (51.5-69.5) years. Thirteen patients were males. H&Y stage 2 was seen in 68.2% patients. The mean duration of symptoms was 4.9 (3.7). The mean score on MDS-UPDRS II was 12.2 (7.9) and the mean MDS-UPDRS III was 36.6 (17.1). The mean PDQ-8-SI was 27.4 (22.3) and the mean total NMSS score was 37.8 (38.3). There was no significant difference between pre- and post-rehabilitation measures [Table 2].
Figure 1.
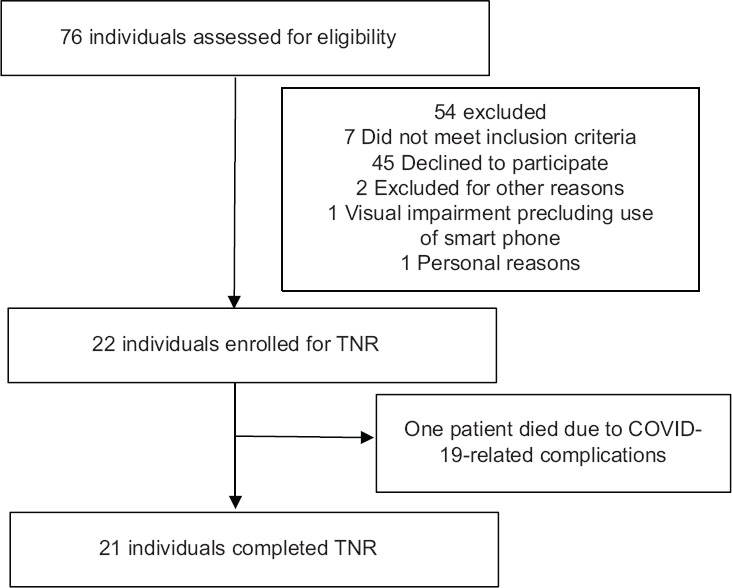
Study flow diagram
Table 1.
Baseline characteristics of patients enrolled in TNR
| Characteristic | (n=22) |
|---|---|
| Age (years) | |
| Median (IQR) | 66.0 (44.0-71.0) |
| Male (%) | 13 (59.1) |
| Age at onset (years) | |
| Median (IQR) | 63.0 (51.5-69.5) |
| Mean duration of symptoms (SD) (years) | 4.9 (3.7) |
| Modified Hoehn and Yahr stage | |
| 1.0 | 3 (13.6) |
| 1.5 | 1 (4.5) |
| 2.0 | 15 (68.2) |
| 2.5 | 3 (13.6) |
| MDS-UPDRS II | 12.2 (7.9) |
| MDS-UPDRS III | 36.6 (17.1) |
| PDQ-8-SI | 27.4 (22.3) |
| NMSS | 37.8 (38.3) |
| LDED (mg) | 264.9 (220.7) |
| Comorbidities | |
| Hypertension | 7 (31.8) |
| Diabetes | 3 (13.6) |
| Hypothyroidism | 2 (9.1) |
Values expresses as frequency (%) or mean (standard deviation) or median (interquartile range). IQR=interquartile range; LDED=Levodopa equivalent dose; MDS-UPDRS=Movement Disorders Society-Unified Parkinson’s Disease Rating Scale; NMSS=Non-Motor Symptoms Scale; PDQ-8-SI=Parkinson’s Disease Questionnaire-8-Summary Index; SD=Standard deviation
Table 2.
Pre- and post-rehabilitation assessment results
| Parameters | Pre-treatment | Post-treatment | t | P* |
|---|---|---|---|---|
| MDS-UPDRS II | 12.2 (7.9) | 12.1 (7.4) | -1.71 | 0.104 |
| MDS-UPDRS III | 36.6 (17.1) | 37.2 (18.1) | 2.02 | 0.060 |
| PDQ-8-SI | 27.4 (22.3) | 26.1 (21.1) | 1.71 | 0.104 |
| NMSS | 37.8 (38.3) | 38.1 (39.2) | 1.44 | 0.167 |
*Dependent t test used
Table 3 enlists the results of the pre-enrollment survey. Pre-enrollment, of the 45 patients who declined to participate, 24/45 (53.3%) patients expressed reservations regarding the potential of rehabilitation as an intervention. Two (4.4%) patients informed trepidation/lack of confidence/fear of falls in their personal ability to exercise. A further 10/45 patients (22.2%) refused to participate due to intense fear of contracting COVID-19 and did not wish to visit the PMR department, which was located in a highly crowded part of the hospital.
Table 3.
Barriers and challenges to TNR during the COVID-19 pandemic and potential solutions
| Study stage | Barriers | Suggested potential solutions |
|---|---|---|
| Pre-enrollment | -Nihilism towards rehabilitation as a form of therapy (24/45; 53.3%) | Patient education and counselling |
| - Fear of falls/lack of confidence (2/45; 4.4%) | Staged introduction of rehabilitation strategies to overcome fear | |
| -Fear of contracting COVID-19 in hospital during therapy (14/45; 22.2%) | Stress on the use of masks, hand hygiene. Ensure social distance while administering rehabilitation therapy | |
| During TNR | -Shared phones (16/22; 72.7%) | Dedicated time for TNR during which the phone is made available solely to the patient |
| - Slow Internet speed (13/22; 59.9%) | ||
| - Lack of rapport during TNR (6/22; 27.3%) | Sample videos shared with the patient with detailed instructions via audio call | |
| - Migration to hometown (4; 18.2%) | National level interventions to increase Internet speed | |
| - Initial deconditioning (n=2; 9.1%) | Motivational strategies; interdisciplinary sessions; group therapy | |
| - Motor-hand impairment (n=2; 9.1%) | Build up regimen gradually to permit patients to acclimatize; offer passive therapy in the initial sessions | |
| Suggest hands-free options including placing phone against a stand/use of computers |
In terms of adherence, 14/21 (66.7%) patients completed at least 6 of 8 sessions and were considered adherent; 11/21 (52.4%) completed all eight sessions. Of the remaining, one patient died of COVID-19-related complications after completing 4 sessions of TNR. Seven patients attended 2-4 sessions and were considered non-adherent.
During TNR, 16/22 (72.7%) patients had problems with attending TNR sessions as the family shared a single phone. Slow Internet speed was an issue among 13/22 (59.9%) of the patients. Six patients expressed a lack of rapport or sense of belonging to their treatment experienced during in-person visits. Migration to distant hometowns with lack of good Internet speed was an issue for four (18.2%) patients. Two patients had severe initial deconditioning and two had motor impairment of their hand, creating problems with handling their smartphone device during therapy.
DISCUSSION
We present the initial experience of TNR among persons with PD. We also present barriers faced while implementing the TNR program and outline possible solutions with several challenges being unique to the COVID-19 pandemic combined with low-resource settings in our country. This is evidenced by the fact that although we screened 76 patients, only 22 could be recruited for TNR despite eligibility in all except 7 patients. Most patients had bilateral involvement without balance impairment. Recruited patients had mild-to-moderate disability in motor experiences of daily living, as evidenced by the MDS-UPDRS II scores. Patients also had mild-to-moderate motor impairment, demonstrated by the MDS-UPDRS III scores. Among patients with PD, those with mild-to-moderate PD, as in this study, have been shown to most likely benefit from various forms of therapeutic exercises.[6]
Despite multiple challenges to implementing rehabilitation services during the ongoing COVID-19 pandemic, we found that TNR was a feasible option among patients with PD. The intervention was also found to be safe, without falls or any other major complications. Tele-based rehabilitation has been previously observed to be an acceptable and feasible option among patients with spinal disorders with a high degree of patient satisfaction.[17]
Many patients expressed a sense of nihilism with respect to the efficacy of exercise and were over-reliant on medications. This low outcome expectation related to exercises has also been previously reported among patients with PD in a cross-sectional study.[18] This study additionally identified 'lack of time' and 'fear of falling' as barriers to exercise. These factors have been identified as barriers to exercise among older adults in general in various studies.[19,20,21,22] Although none of our patients cited lack of time as a reason to refuse participation, extreme fatigue and lack of confidence in the ability to exercise due to fear of falling was quoted as a reason for not participating. These may have been circumvented by adding a preparatory counselling session to allay possible concerns. These findings also highlight the need to emphasize rehabilitation services as a form of therapy amongst patients with PD, in addition to the enormous symptomatic relief proffered by dopaminergic medications. In our setting, such education and counselling may be offered by the treating clinician in tandem with the PD nurse, counsellor and the physical therapist.
Lack of geographical proximity to our center, even within the city of Delhi and the adjacent National Capital Region, necessitated exclusion of several patients as lack of public conveyance during the pandemic made long-distance travel cumbersome. Since ours is a tertiary referral center, patients attended outpatient and clinic services even from other states of India, including Bihar and Uttarakhand. However, this is not a situational experience limited to pandemic times. In India, only 37% of the population in rural areas is able to access an inpatients' health facility within 5 km and 68% only are able to access outpatient services.[23] These patients could be easily recruited for TNR as they could follow the program after return, and TNR is a feasible alternative solution for rehabilitation in out-of-state patient populations.
There were certain unique barriers which led to the lack of adherence in nearly one-third of our patients. Many patients shared smartphones with one family member. This was usually the earning member who would travel with the phone to the workplace. Hence, often the smartphone was not available to conduct telerehabilitation sessions with these patients during hospital hours. Sometimes, smart phone at home had to be used for online classes for children of school-going age group, which always took precedence over rehabilitation. This barrier may be circumvented by emphasizing the rehabilitation session as a priority and cornerstone of management of the PD patient to the caregiver/family members so that alternate arrangements viz-a-viz the smartphone can be made. Although the family-based social fabric is often a support system for these patients, it may pose a potential barrier in the implementation of TNR services.
There were also issues with the Wi-Fi bandwidth at the patient's residence, so video calling was often interrupted or of poor quality, and several calls had to be made during one session. The barrier of slow Internet speed was observed as a significant barrier to telerehabilitation in a developing country in a systematic review, with studies involving Filipinos as participants/investigators.[22] An alternative way to deal with low bandwidth may be to organize rehabilitation sessions using pre-created demonstration videos, and explanation via an audio call.
Some patients had poor hand-motor skill, which made the use of a smartphone a handicap. The use of a computer would have circumvented this problem, but none of our patients felt technologically skilled enough to use the computer. Several patients expressed inadequate rapport that they otherwise experienced after seeing the doctor in person. Similar 'human' barriers to telerehabilitation have been noted previously.[22]
Moreover, many patients travelled back to their villages or hometown of origin during the study period after recruitment and the initial training session, in line with mass migration that was reported from India during these times.[24] At these usually remote regions, adequate broadband for receiving telerehabilitation services was not present. Despite an in-depth initial supervised training session in the first visit, some patients did not perform exercises correctly, which were subsequently challenging to rectify via tele-conferencing. Additionally, a few patients initially were very de-conditioned and needed passive exercises which could not be implemented at home.
We recognized several barriers to TNR in our setting. Lack of confidence in rehabilitation expressed by patients can be approached by educating patients, with specific considerations to the pandemic. It is known that moderate intensity exercise potentially is protective against COVID-19 as it strengthens the immune system, and also improves quality of life among patients with PD.[25]
We also found the lack of good speed Internet to be a hinderance in the delivery of rehabilitation. Solutions to this problem may be to use a video-based rehabilitation approach, in which instead of live calling, videos may be shared per session by the therapist to be viewed and followed by the patient. India's Internet penetration is reported to be around 38%, although the national capital of Delhi reports Internet penetration of 69%. However, nearly one-third of our patients hail from areas which are out of Delhi, and Internet connectivity poses an issue. Internet speed is a national issue, and India ranks 131 of 138 countries when ranked on average Internet speed connection.[26] This is an enormous hurdle to tele-based services in India. In order to overcome this, we prepared sample videos of exercises which were sent to them through freeware, and this may be considered a possible alternative which circumvents bandwidth issues. However, this mode of TNR will need further assessment. The need for universal and efficient Internet access is the need of the hour, and necessary steps are required at a national level.
Adherence issues may be addressed by continued positive reinforcement and motivation towards attending the sessions. These must necessarily be targeted towards the caregivers as well as the patients, since our patients depend on their caregivers to reach healthcare facilities.
Possible solutions to some of these problems are enlisted in Table 3.
As there are no telerehabilitation guidelines in India specific to PD, we ourselves designed a regimen that was considered suitable for our settings and acceptable to the participants. This protocol was easy to implement and may be considered by future programs. We report this experience of TNR among PD patients from India for the first time. There is a telerehabilitation program in place in a quaternary center in India, which found telerehabilitation to be an effective, feasible and economical alternative.[27] However, this center provided consultations for a diverse list of neurological disorders, ranging from stroke to muscular dystrophy.
Limitations of our study included relatively small numbers. Slow recruitment was a result of the pandemic and the multiple barriers mentioned above. Moreover, we assessed only motor aspects and did not assess the effect of TNR on other facets such as speech, voice, swallowing and posture, which may be a thrust of future studies.
CONCLUSIONS
Our article expands on barriers to implementation of a rehabilitation program in a resource-constrained setting, with specific focus on telerehabilitation, during the ongoing COVID-19 pandemic. We also highlight potential solutions to some of these impediments. Before efficacy of TNR as an intervention can be established, its feasibility and acceptability to patients, and overall safety needs to be ensured. Integration of neurology with rehabilitation services is imperative for the success of such endeavors. Future programs that are based on TNR in Indian settings need to keep these in mind before planning similar studies and/or interventions. The efficacy of TNR needs to be studied in randomized-controlled trial settings.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We thank the patients and their caregivers for their participation in this study. We thank our clinic nurses, Mini Mol and Sukhwinder Kaur, for their assistance in managing the patient flow and follow up. We also thank Mrs. Dimple Kashyap, physiotherapist, for her assistance in teaching therapeutic exercises to participants.
Supplement 1. Rehabilitation regimen employed in the study
Supplement 1.
Rehabilitation regimen employed in the study
| S.no. | Exercise | Repetition/Intensity | Duration | Dyspnea score | Remarks |
|---|---|---|---|---|---|
| 1 | Flexibility Exercises | ||||
| Lying Stretches | |||||
| Shoulder Stretch | |||||
| Rotation Stretch | |||||
| Seated Stretches | |||||
| Neck and Chest Stretch | |||||
| Hamstring Stretch | |||||
| Rotation Stretch | |||||
| Ankle Circles | |||||
| Overhead Stretch | |||||
| Seated Side Stretch | |||||
| Standing Stretches | |||||
| Chest Stretch Back Stretch Shoulder Stretch | |||||
| 2 | Aerobic Exercises | ||||
| Walking/Jogging/Running | |||||
| Swimming/Dancing | |||||
| Biking | |||||
| Any other | |||||
| 3. | Strengthening Exercises | ||||
| On-the-Ground Strengthening Exercises | |||||
| Bridge Quadruped | |||||
| Back Extension | |||||
| Seated Strengthening Exercise | |||||
| Shoulder Blade Squeeze | |||||
| Standing Strengthening | |||||
| Exercises | |||||
| Wall Slides Quad | |||||
| Strengthening | |||||
| Quad Strengthening | |||||
| 4 | Balance Exercise | ||||
| 5 | Deep Breathing | ||||
| Total duration |
Supplement 2. 6-minute walk test
Predicted heart rate max……….
Date and time of bronchodilator last taken:
Supplement 2.
Predicted heart rate maxNU Date and time of bronchodilator last taken:
| Time mins | SpO2 | HR | Dyspnea | Rest |
|---|---|---|---|---|
| Rest | ||||
| 2 | ||||
| 3 | ||||
| 4 | ||||
| 5 | ||||
| 6 | ||||
| Recovery 1 |
Distance:
Limiting factor to test………. Shortness of breath…………. Low SpO2 Leg fatigue………
Others……………….
Supplement 3
Functional Reach Test and Modified Functional Reach Instructions
General Information: The Functional Reach test can be administered while the patient is standing (Functional Reach) or sitting (Modified Functional Reach).
Functional Reach (standing instructions):
The patient is instructed to stand next to, but not touching, a wall and position the arm that is closer to the wall at 90° of shoulder flexion with a closed fist.
The assessor records the starting position at the third metacarpal head on the yardstick.
Instruct the patient to “Reach as far as you can forward without taking a step.”
The location of the third metacarpal is recorded.
Scores are determined by assessing the difference between the start and end position is the reach distance, usually measured in inches.
Three trials are done and the average of the last two is noted.
Modified Functional Reach Test (Adapted for individuals who are unable to stand):
Performed with a leveled yardstick that has been mounted on the wall at the height of the patient's acromion level in the non-affected arm while sitting in a chair
Hips, knees and ankles positioned are at 90° of flexion, with feet positioned flat on the floor.
The initial reach is measured with the patient sitting against the back of the chair with the upper-extremity flexed to 90°, measure was taken from the distal end of the third metacarpal along the yardstick.
-
Consists of three conditions over three trials
- Sitting with the unaffected side near the wall and leaning forward
- Sitting with the back to the wall and leaning right
- Sitting with the back to the wall leaning left.
Instructions should include leaning as far as possible in each direction without rotation and without touching the wall
Record the distance in centimeters covered in each direction
If the patient is unable to raise the affected arm, the distance covered by the acromion during leaning is recorded
First trial in each direction is a practice trial and should not be included in the final result
A 15-second rest break should be allowed between trials
Set-up:
A yardstick and duck tap will be needed for the assessment.
The yardstick should be affixed to the wall at the level of the patient's acromion.
References:
Duncan, P. W., D. K. Weiner, et al. (1990). “Functional reach: a new clinical measure of balance.” J Gerontol 45 (6): M192-197.
Katz-Leurer, M., I. Fisher, et al. (2009). “Reliability and validity of the modified functional reach test at the sub-acute stage post-stroke.” Disabil Rehabil 31 (3): 243-248.
Weiner, D. K., D. R. Bongiorni, et al. (1993). “Does functional reach improve with rehabilitation?” Arch Phys Med Rehabil 74 (8): 796-800.
Weiner, D. K., P. W. Duncan, et al. (1992). “Functional reach: a marker of physical frailty.” J Am Geriatr Soc 40 (3): 203-207.
Supplement 4
Modified Borg Dyspnea Scale
Supplement 4.
Modified Borg Dyspnea Scale
| 0 | Nothing at all |
| 0.5 | Very, very slight(just noticeable) |
| 1 | Very slight |
| 2 | Slight |
| 3 | Moderate |
| 4 | Somewhat severe |
| 5 | Severe |
| 6 | |
| 7 | Very severe |
| 8 | |
| 9 | Very, very severe(almost maximal) |
| 10 | Maximal |
This is a scale that asks you to rate the difficulty of your breathing. It starts at number 0 where your breathing is causing you no difficulty at all and progresses through to number 10 where your breathing difficulty is maximal. How much difficulty is your breathing causing you right now ?
REFERENCES
- 1.Cimerman S, Chebabo A, Cunha CA da, Rodríguez-Morales AJ. Deep impact of COVID-19 in the healthcare of Latin America: The case of Brazil. Braz J Infect Dis. 2020;24:93–5. doi: 10.1016/j.bjid.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chatterjee K, Chatterjee K, Kumar A, Shankar S. Healthcare impact of COVID-19 epidemic in India: A stochastic mathematical model. Med J Armed Forces India. 2020;76:147–55. doi: 10.1016/j.mjafi.2020.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pavel A, Murray DK, Stoessl AJ. COVID-19 and selective vulnerability to Parkinson's disease. Lancet Neurol. 2020;19:719. doi: 10.1016/S1474-4422(20)30269-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kumar N, Gupta R, Kumar H, Mehta S, Rajan R, Kumar D, et al. Impact of home confinement during COVID-19 pandemic on Parkinson's disease. Parkinsonism Relat Disord. 2020;80:32–4. doi: 10.1016/j.parkreldis.2020.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Prasad S, Holla VV, Neeraja K, Surisetti BK, Kamble N, Yadav R, et al. Impact of prolonged lockdown due to COVID-19 in patients with Parkinson's disease. Neurol India. 2020;68:792–5. doi: 10.4103/0028-3886.293472. [DOI] [PubMed] [Google Scholar]
- 6.Garg D, Dhamija RK. Rehabilitation in Parkinson's disease: Current status and future directions. Ann Mov Disord. 2020;3:79–85. [Google Scholar]
- 7.Isernia S, Di Tella S, Pagliari C, Jonsdottir J, Castiglioni C, Gindri P, et al. Effects of an innovative telerehabilitation intervention for people with Parkinson's disease on quality of life, motor, and non-motor abilities. Front Neurol. 2020;11:846. doi: 10.3389/fneur.2020.00846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gandolfi M, Geroin C, Dimitrova E, Boldrini P, Waldner A, Bonadiman S, et al. Virtual reality telerehabilitation for postural instability in Parkinson's disease: A multicenter, single-blind, randomized, controlled trial. Biomed Res Int. 2017;2017:7962826. doi: 10.1155/2017/7962826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cikajlo I, Hukić A, Dolinšek I, Zajc D, Vesel M, Krizmanič T, et al. Can telerehabilitation games lead to functional improvement of upper extremities in individuals with Parkinson's disease? Int J Rehabil Res. 2018;41:230–8. doi: 10.1097/MRR.0000000000000291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lei C, Sunzi K, Dai F, Liu X, Wang Y, Zhang B, et al. Effects of virtual reality rehabilitation training on gait and balance in patients with Parkinson's disease: A systematic review? PLoS One. 2019;14:e0224819. doi: 10.1371/journal.pone.0224819. doi: 10.1371/journal.pone.0224819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Theodoros DG, Hill AJ, Russell TG. Clinical and quality of life outcomes of speech treatment for Parkinson's disease delivered to the home via telerehabilitation: A noninferiority randomized controlled trial. Am J Speech Lang Pathol. 2016;25:214–32. doi: 10.1044/2015_AJSLP-15-0005. [DOI] [PubMed] [Google Scholar]
- 12.Goetz CG, Tilley BC, Shaftman SR, Stebbins GT, Fahn S, Martinez-Martin P, et al. Movement disorder society-sponsored revision of the unified Parkinson's disease rating scale (MDS-UPDRS): Scale presentation and clinimetric testing results. Mov Disord. 2008;23:2129–70. doi: 10.1002/mds.22340. [DOI] [PubMed] [Google Scholar]
- 13.Jenkinson C, Fitzpatrick R, Peto V, Greenhall R, Hyman N. The PDQ-8: Development and validation of a short-form parkinson's disease questionnaire. Psychol Health. 1997;12:805–14. [Google Scholar]
- 14.Chaudhuri KR, Martinez-Martin P, Brown RG, Sethi K, Stocchi F, Odin P, et al. The metric properties of a novel non-motor symptoms scale for Parkinson's disease: Results from an international pilot study. Mov Disord. 2007;22:1901–11. doi: 10.1002/mds.21596. [DOI] [PubMed] [Google Scholar]
- 15.Butland RJ, Pang J, Gross ER, Woodcock AA, Geddes DM. Two-, six-, and 12-minute walking tests in respiratory disease. Br Med J (Clin Res Ed) 1982;284:1607–8. doi: 10.1136/bmj.284.6329.1607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Duncan PW, Weiner DK, Chandler J, Studenski S. Functional reach: A new clinical measure of balance. J Gerontol. 1990;45:M192–7. doi: 10.1093/geronj/45.6.m192. [DOI] [PubMed] [Google Scholar]
- 17.Negrini S, Donzelli S, Negrini A, Negrini A, Romano M, Zaina F. Feasibility and acceptability of telemedicine to substitute outpatient rehabilitation services in the COVID-19 emergency in Italy: An observational everyday clinical-life study. Arch Phys Med Rehabil. 2020;101:2027–32. doi: 10.1016/j.apmr.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ellis T, Boudreau JK, DeAngelis TR, Brown LE, Cavanaugh JT, Earhart GM, et al. Barriers to exercise in people with Parkinson disease. Phys Ther. 2013;93:628–36. doi: 10.2522/ptj.20120279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Resnick B, Palmer MH, Jenkins LS, Spellbring AM. Path analysis of efficacy expectations and exercise behaviour in older adults. J Adv Nurs. 2000;31:1309–15. doi: 10.1046/j.1365-2648.2000.01463.x. [DOI] [PubMed] [Google Scholar]
- 20.Schutzer KA, Graves BS. Barriers and motivations to exercise in older adults. Prev Med. 2004;39:1056–61. doi: 10.1016/j.ypmed.2004.04.003. [DOI] [PubMed] [Google Scholar]
- 21.Forkan R, Pumper B, Smyth N, Wirkkala H, Ciol MA, Shumway-Cook A. Exercise adherence following physical therapy intervention in older adults with impaired balance. Phys Ther. 2006;86:401–10. [PubMed] [Google Scholar]
- 22.Leochico CFD, Espiritu AI, Ignacio SD, Mojica JAP. Challenges to the emergence of telerehabilitation in a developing country: A systematic review. Front Neurol. 2020;11:1007. doi: 10.3389/fneur.2020.01007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kasthuri A. Challenges to healthcare in India-The Five A's. Indian J Community Med. 2018;43:141–3. doi: 10.4103/ijcm.IJCM_194_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mukhra R, Krishan K, Kanchan T. COVID-19 sets off mass migration in India. Arch Med Res. 2020;51:736–8. doi: 10.1016/j.arcmed.2020.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hall ME, Church FC. Exercise for older adults improves the quality of life in Parkinson's disease and potentially enhances the immune response to COVID-19. Brain Sci. 2020;10:612. doi: 10.3390/brainsci10090612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.India ranks 131 out of 138 countries in mobile internet speed, even lower than Iraq-The Economic Times. [Last accessed on 2020 Nov 20]. Available from: https://economictimes.indiatimes.com/industry/telecom/telecom-news/india-ranks-131-outof-138-countries-in-mobile-internet-speed-ranking-even-lower-thaniraq/articleshow/78873643.cms?from=mdr .
- 27.Khanna M, Gowda GS, Bagevadi VI, Gupta A, Kulkarni K, S Shyam RP, et al. Feasibility and utility of tele-neurorehabilitation service in India: Experience from a quaternary center. J Neurosci Rural Pract. 2018;9:541–4. doi: 10.4103/jnrp.jnrp_104_18. [DOI] [PMC free article] [PubMed] [Google Scholar]


