Abstract
Background:
Internationally approved electrodiagnostic criteria for Guillain Barre syndrome lack in children. We intended to compare the diagnostic accuracy of the currently available five electrophysiological criteria for childhood Guillain Barre Syndrome (GBS) at the time of sentinel assessment.
Methodology:
In this single-center study, data of children diagnosed with GBS between January 2013 to December 2017 were retrieved. Patient charts were reviewed for clinical features, electrophysiological recordings. The electrodiagnostic results (4 motor nerves and two sensory nerves in upper limbs and lower limbs) were reanalyzed and were classified based on Dutch group; Ho; Hadden; Hughes and Rajabally criteria for GBS.
Results:
During this study period, of the 205 children with clinical features of GBS, 15 children had incomplete electrophysiological data, and four children were excluded due to missing data. The mean age of onset of the 186 children enrolled was 77 months; the median duration from symptom onset to electrodiagnostic evaluation was seven days; pure motor and motor-sensory form of GBS was seen in 71 and 115 children. Based on the Hadden criteria, a demyelinating pattern was noted in 57 children; axonal in 37; Inexcitable in 84 and Equivocal in 8 children. The sensitivity of the various criteria ranged from 71% to 100% for demyelination, 97% to 100% for axonal. The degree of agreement using Hadden and Rajabally criteria for Equivocal subtypes was 0.93.
Conclusions:
The Rajabally criteria showed the best sensitivity, specificity and diagnostic accuracy for electrodiagnosis of GBS in children when compared against Hadden criteria.
Keywords: Acute inflammatory demyelinating polyneuropathy, acute motor axonal neuropathy, electrodiagnosis, AIDP, AMAN, AMSAN, neurophysiology
INTRODUCTION
Guillain Barre Syndrome, the most common cause of acute flaccid paralysis, is an immune-mediated disease of the peripheral nerves with an annual global incidence of approximately 1-2 per 100000 person-years.[1] The prototypical presentation is a rapidly progressive bilateral limb weakness with hypo/areflexia and facial or bulbar palsy. Its diagnosis is based on history, neurological examination, and is confirmed by electrophysiological studies. Under the rubric of Guillain Barre Syndrome (GBS), electrophysiological subtypes include Acute Inflammatory Demyelinating Polyneuropathy (AIDP), Acute Motor Axonal Neuropathy (AMAN) and Acute Motor Sensory Axonal Neuropathy (AMSAN).[2] Segmental demyelination and remyelination are the classical pathological findings in AIDP. At the same time, antibody-mediated nodal dysfunction has been noted in Axonal subtypes. AIDP, AMAN, and AMSAN are difficult to distinguish on clinical grounds alone, and electrophysiological studies are the principal determinants of the subtype classification. Although the subtype distinction has no bearing on the treatment offered, it aids in comprehending the actual pathogenesis and delineate the ultimate prognosis and overall outcome of GBS. Electro physiologically, AIDP is illustrated by the slowing of conduction with temporal dispersion and conduction block. Decreased amplitude of Compound Muscle Action Potential is the presumed electrophysiological correlate for Axonal forms of GBS.[3,4] Over the last three decades, different sets of electrophysiological criteria have been proposed for the diagnosis of Guillain Barre Syndrome, ranging from Albers criteria of 1985 to the new Uncini criteria of 2017. To date, internationally approved electrodiagnostic criteria for GBS lack in children and adults. Attempts at the comparison of the published criteria for AIDP in adults yielded inconsistent sensitivity of 16.6% to 100%.[5] Data on electrodiagnostic comparison for axonal variants of GBS is non-existent, highlighting the need for a universally acceptable electrodiagnostic criteria for diagnosis of GBS. Besides, the available criteria have seldom been compared in a large population of childhood GBS. In this study, we intended to compare the diagnostic accuracy of the currently available five electrodiagnostic criteria for childhood Guillain Barre Syndrome.
METHODOLOGY
This study is a retrospective review of children with a clinical and electrophysiological diagnosis of Guillain Barre Syndrome presenting to a tertiary care referral hospital in North-West India during the period of January 2013 to December 2017. Children aged six months to 12 years with clinical suspicion of Guillain Barre Syndrome presenting within four weeks of the onset of illness were enrolled in the study. Children with complete electrophysiological recordings of four motor nerves and two sensory nerves in upper limbs and lower limbs were included in the study. Children of GBS with incomplete clinical and electrophysiological records (<4 motor and <2 sensory nerves) were excluded. The Institutional Ethics Committee approved the study. Clinical details and demographic profiles were obtained on a data recording form that was then transcribed into Microsoft Excel and analyzed using the SPSS (Statistical Product and Service Solutions) software. Electrophysiological parameters at the initial electrophysiological test obtained from motor nerves include Distal Latency (DL), Proximal and Distal Compound Muscle Action Amplitude (CMAP), and Duration, Nerve Conduction Velocity (NCV) and Minimal F-Waves Latency. Sensory Nerve Action Potential (SNAP) and NCV were obtained from sensory nerves. Two investigators reanalyzed the electrophysiological parameters and the data were classified using the five different published criteria sets for GBS identification. The criteria proposed by the Dutch group, Ho et al., Hadden et al., Hughes et al., and Rajabally et al. were compared [Table 1].[6,7,8,9,10]
Table 1.
Five electrophysiological criteria for the diagnosis of childhood Guillain Barre Syndrome
| Parameters | Ho et al. | Hadden et al. | Dutch et al. | Hughes et al. | Rajabally et al. |
|---|---|---|---|---|---|
| AIDP | |||||
| MCV | <90% LLN | <90% LLN | <70% LLN | <90% LLN | <70% LLN |
| <85% if D-amp <50% | <85% if d-amp <50% | <85% if d-amp <50% | |||
| DL | >110% ULN | >110% ULN | >150% ULN | >110% ULN | >150% ULN |
| >120% if D amp <LLN | >120% if d-amp <LLN | >120% if d-amp <LLN | |||
| TD | Unequivocal | Not considered | D-P duration ratio >150% ULN | Not considered | |
| D duration >300% ULN | |||||
| CB | Not considered | P-D amp ratio < 0.5 D amp > 20% LLN | Not considered | P-D amp ratio < 0.5 D amp > 20% LLN | <0.7 P-D amp ratio in two nerves with an additional parameter |
| D CMAP | >10% LLN | ||||
| F wave L | >120% ULN | >120% ULN | >150% ULN | >120% ULN | >120% ULN |
| >150% ULN if distal CMAP <50% LLN | |||||
| Absent in two nerves with dCMAP >20% LLN with an additional parameter | |||||
| AMAN | |||||
| No AIDP | No AIDP | Not considered | No AIDP | No AIDP | |
| CMAP | D amp <80 % LLN | D amp <80 % LLN | Normal SNAP | D amp <80 % LLN | |
| P-D amp ratio < 0.7 | |||||
| AMSAN | |||||
| Not considered | Not considered | Not considered | No AIDP | Not considered | |
| SNAP < LLN | |||||
| Inexcitable | |||||
| Not considered | Absent D CMAP in all nerves | Not considered | Absent D CMAP in all nerves | Absent D CMAP in all nerves | |
| Present in only one nerve with <10% LLN | Present in only one nerve with <10% LLN | Present in only one nerve with <10%LLN | |||
| Equivocal | |||||
| Not considered | Not fitting criteria | Not considered | Not considered | Not fitting criteria |
AIDP Acute Inflammatory Demyelinating Polyneuropathy. MCV Mean Conduction Velocity, DL Distal Latency. TD Temporal Dispersion, CB Conduction Block, SNAP Sensory Nerve Action Potential, LLN Lower Limit Normal, ULN Upper Limit Normal
Increased duration of the negative peak of proximal CMAP (p-CMAP) by >30% compared with distal CMAP (d-CMAP) was used to define the temporal dispersion of CMAP by Ho et al.'s criteria. An additional entity “Indecisive” is used by authors to depict the proportion of children not fitting the Ho et al., Dutch et al., and Hughes et al. criteria. For statistical testing, the sensitivity and specificity, the diagnostic accuracy of the different electrodiagnostic criteria were evaluated. Hadden et al. criteria is the widely used electrophysiological criteria for GBS in children and was taken as the reference for electrodiagnostic subtype classification in this study. Cohen's Kappa statistics were used to determine the agreement among the criteria. A P value of ≤ 0.05 was considered significant.
RESULTS
During the study period, 205 children with clinical and electrophysiological features suggestive of Guillain Barre Syndrome were diagnosed. Nineteen children were excluded from the study; four children had missing clinical data, and fifteen children had incomplete electrophysiological studies [Figure 1]. Of the 186 children with GBS included in the study, the mean age at onset of illness was 77 months [Table 2]. The median duration from onset of symptoms to sentinel electrophysiological evaluation was seven days. Pure motor form of GBS was seen in 71 children and motor-sensory variant of GBS was noted in 115 children. For axonal subtypes, 69 (37%) children were identified using Hughes criteria while only thirty-seven (20%) children were diagnosed by Hadden and Rajabally et al. [Table 3]. Remarkably, almost 46% of children were classified as inexcitable forms based on Hadden and Rajabally et al. criteria. When Hadden et criteria were taken as the reference, Dutch et al. criteria had the lowest sensitivity (71% [95%CI 58-83%]) for demyelination and the Hughes et al. criteria had the lowest specificity (85% [95%CI 79-90%]) for axonal subtypes. Rajabally et al. criteria showed the best combination of sensitivity and specificity for axonal, demyelinating and inexcitable forms of GBS [Table 4]. Using Kappa statistics, the inter-rater reliability for AIDP using the five criteria was 0.89. The degree of agreement for Axonal using the Ho, Hadden, Hughes, and Rajabally criteria was 0.73. The degree of agreement among Hadden, Hughes, and Rajabally criteria for inexcitable subtype was 0.77, and for Equivocal subtypes using Hadden and Rajabally criteria was 0.93, respectively.
Figure 1.
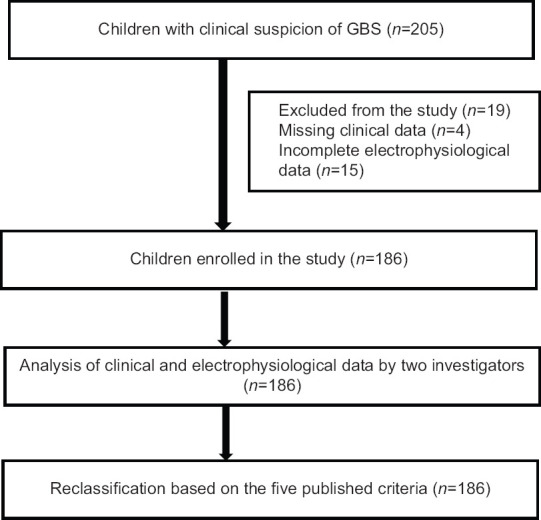
Flowchart of participants with clinical and electrophysiological diagnosis of Guillain Barre Syndrome (GBS)
Table 2.
Clinical profile of 186 children with Guillian Barre Syndrome
| Characteristics | Value n (%) |
|---|---|
| Males | 132 (71%) |
| Mean Age in months (SD) | 77 (44) |
| Median Age in months (IQR) | 70 (43-107) |
| Antecedent Gastroenteritis | 39 (21%) |
| Antecedent respiratory tract infection | 98 (53%) |
| Paraparesis | 29 (15.5%) |
| Quadriparesis | 154 (83%) |
| Bulbar dysfunction | 65 (35%) |
| Ataxia | 17 (9%) |
| Ophthalmoplegia | 3 (1.6%) |
| Ventilator requirement | 46 (25%) |
| Mean days for first EPS from symptom onset (SD) | 8 (5) |
| Median days for first EPS from symptom onset (IQR) | 7 (5-10) |
| GBS | |
| GBS | 182 (98%) |
| Miller Fischer syndrome | 3 (1.6%) |
| Polycranialis variant | 1 (0.5%) |
| Pharyngo Brachial variant | 0 |
Table 3.
Results of the five criteria sets at first electrophysiological evaluation showing the GBS subtypes in 186 children
| Criteria | AIDP | AMAN | AMSAN | Inexcitable | Equivocal | Indecisive |
|---|---|---|---|---|---|---|
| Dutch et al. | 41 | - | - | - | - | 145 |
| Ho et al. | 51 | 36 | - | - | - | 99 |
| Hughes et al. | 57 | 62 | 9 | 55 | - | 3 |
| Hadden et al. | 57 | 37 | - | 84 | 8 | - |
| Rajabally et al. | 55 | 37 | - | 85 | 9 | - |
Table 4.
Results of the Sensitivity and Specificity of the different electrodiagnostic criteria when compared with Hadden et al. criterion
| Criterion | AIDP | AMAN | Inexcitable | Equivocal |
|---|---|---|---|---|
| Sensitivity | ||||
| Dutch et al. | 72% | - | - | - |
| Ho et al. | 89% | 97% | - | - |
| Hughes et al. | 100% | 100% | 96% | - |
| Rajabally et al. | 96.5% | 100% | 100% | 100% |
| Specificity | ||||
| Dutch et al. | 100% | - | - | - |
| Ho et al. | 100% | 100% | - | - |
| Hughes et al. | 100% | 85% | 100% | |
| Rajabally et al. | 100% | 100% | 99% | 99% |
AIDP: Acute Inflammatory Demyelinating Polyneuropathy, AMAN: Acute Motor Axonal Neuropathy
DISCUSSION
Given the clinical continuum, the diagnosis of Guillain Barre syndrome is completed by electrophysiological examination. Multiple sets of electrodiagnostic criteria exist based on the presence of specific electrophysiological variables in at least two or more nerves. However, international consensus is yet to be attained on which set of criteria best defines the subtypes. Experts, in general, concur with the set of parameters to be tested but digress in the cut-off to fulfil the diagnosis. Furthermore, the traditional delineation of axonal forms of GBS was heralded by the exclusion of demyelinating variant of GBS. Emerging concepts such as Nodo-paranodopathy with transient/reversible conduction block without temporal dispersion in the axonal form of GBS have highlighted the classification errors in the first electrophysiological assessment.[11] In the current study, our focus was to compare the diagnostic accuracy of the five commonly used criteria. We did not come across a comparable study involving children with the clinical diagnosis of GBS for electrophysiological subtype classification.
The most widely recognized electrophysiological form of GBS in our study during the initial assessment was the “inexcitable” subtype, which was noted in 46% of the children as per Hadden and Rajabally et al. criteria. This is in stark contrast to the dominant subtype noted worldwide; AIDP from North America and Europe and AMAN from China. AIDP (30%) was the second most frequent subtype noted in our cohort. The mean duration between the onset of symptoms and the first electrophysiological evaluation in our study was eight days. Thirty percent of children underwent electrophysiological testing within five days of symptom onset. The reason behind the high preponderance of inexcitable subtype in our cohort is largely unknown and the role of early electrophysiological evaluation merits further exploration. In our study, 41 (22%) children were classified as AIDP by the conventional Dutch et al. criteria, while there was a substantial rise by 8% when the recent Hughes, Hadden, and Rajabally criteria were applied. This misclassification may be due to the stringent cut-off for conduction velocity used by Dutch et al. to be consistent with demyelination. Seventy percent of the lower limit of normal in conduction velocity was deemed acceptable by the Dutch et al. Conversely, liberal cut off criteria of 90% of the lower limit of normal was used by others to detect minimal to moderate demyelination that may occur in AIDP.[12] Likewise, a higher proportion of children (69 [37%]) were diagnosed as axonal variants by Hughes criteria when compared to others. However, Hughes's criteria had the lowest specificity (85%) for axonal forms. This can be attributed to the non-existence of specific criteria for axonal subtype after ruling out demyelination in the Hughes classification, unlike others. Similarly, a significantly large proportion of children remain unclassified following the Dutch et al. (78%) and Ho et al. criteria (50%) questioning their validity in the present scenario.
Based on the current study, Rajabally et al. criteria showed the optimal combination of sensitivity and specificity for electrodiagnosis of childhood GBS when compared with Hadden et al. Our results agree with similar reports from a prospective study by Scarpino et al. in 23 adults with GBS.[5] The Rajabally criteria were found to have good 82% sensitivity and 100% specificity at entry evaluation for the electrophysiological diagnosis of AIDP. The Scarpino study did have few concerns. No patients with axonal forms of GBS were noticed by their electrophysiological evaluation depicting a homogenous cohort, unlike our study population. The clinical consensus was taken as the reference standard by the authors. Lack of standard gold reference is one of the major handicaps for comparative studies on electrophysiological classification for GBS. Earlier studies used the clinical criteria developed by the National Institute of Neurological Disorders and Stroke for reference when the demyelinating form of GBS was the only accepted subtype. Given the paradigm shift in the understanding of GBS with axonal subtypes and pure sensory variants, GBS taxonomy based on clinical grounds is no longer practical. This significant lacuna has been addressed in recent studies by antiganglioside antibody positivity found in 37-78% of axonal forms of GBS. Thus, a combination of clinical criteria and antiganglioside antibody positivity is being adopted as the reference standard for comparative studies.[13,14] The retrospective nature of our study hindered antibody testing in our population.
The original work by Rajabally et al. stressed the classification shift from AIDP and equivocal subtypes to the axonal form of GBS in 44% of the patients at initial electrophysiological evaluation.[8] Such contradictory results were not obtained in our study, and the agreement between Rajabally and Hadden criteria for AIDP and equivocal subtypes were high. Rajabally et al. also pointed out the higher proportion of unambiguous diagnosis of AIDP or Axonal using a single study. This is contrasting from our study results, as two-fifths of our children had inexcitable subtype warranting further recordings for appropriate diagnoses. In the study done by Uncini et al. linear discriminant analysis was used on serial recordings of electrophysiological data for subtype classification.[15] Lack of serial follow data precluded its application in our study.
A clearly defined electrophysiological protocol, results from a single electrophysiological equipment, analysis by two investigators and application in a large cohort of children were the strengths of the study. To the best of our knowledge, the utility of the recently proposed Rajabally criteria has not been explored in children and our results from a cohort of 186 children has provided the preliminary data for further exploration. Nevertheless, our study has certain limitations. Serial recordings were available in very few patients impeding major classification shifts from inexcitable subtype on follow up. Pure electrophysiological focus without microbiological or immunological biomarkers is another limitation.
In conclusion, the present study has identified Rajabally et al. and Hadden et al. as the optimal methods for establishing the electrodiagnostic subtype of GBS during the initial assessment. Longitudinal follow up electrophysiological evaluation, nevertheless, remain pertinent for precise delineation of demyelinating and axonal subtypes, especially among the inexcitable subtypes.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Sejvar JJ, Baughman AL, Wise M, Morgan OW. Population incidence of Guillain-Barré syndrome: A systematic review and meta-analysis. Neuroepidemiology. 2011;36:123–33. doi: 10.1159/000324710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yuki N, Hartung H-P. Guillain-Barré syndrome. N Engl J Med. 2012;366:2294–304. doi: 10.1056/NEJMra1114525. [DOI] [PubMed] [Google Scholar]
- 3.Leonhard SE, Mandarakas MR, Gondim FAA, Bateman K, Ferreira MLB, Cornblath DR, et al. Diagnosis and management of Guillain-Barré syndrome in ten steps. Nat Rev Neurol. 2019;15:671–83. doi: 10.1038/s41582-019-0250-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Willison HJ, Jacobs BC, van Doorn PA. Guillain-Barré syndrome. Lancet. 2016;388:717–27. doi: 10.1016/S0140-6736(16)00339-1. [DOI] [PubMed] [Google Scholar]
- 5.Scarpino M, Lolli F, Carrai R, Lanzo G, Spalletti M, Barilaro A, et al. Diagnostic accuracy of neurophysiological criteria for early diagnosis of AIDP: A prospective study. Neurophysiol Clin. 2016;46:35–42. doi: 10.1016/j.neucli.2015.12.008. [DOI] [PubMed] [Google Scholar]
- 6.Ho TW, Mishu B, Li CY, Gao CY, Cornblath DR, Griffin JW, et al. Guillain-Barré syndrome in northern China. Relationship to Campylobacter jejuni infection and anti-glycolipid antibodies. Brain. 1995;118(Pt 3):597–605. doi: 10.1093/brain/118.3.597. [DOI] [PubMed] [Google Scholar]
- 7.Hadden RD, Cornblath DR, Hughes RA, Zielasek J, Hartung HP, Toyka KV, et al. Electrophysiological classification of Guillain-Barré syndrome: Clinical associations and outcome. Plasma Exchange/Sandoglobulin Guillain-Barré Syndrome Trial Group. Ann Neurol. 1998;44:780–8. doi: 10.1002/ana.410440512. [DOI] [PubMed] [Google Scholar]
- 8.Rajabally YA, Durand M-C, Mitchell J, Orlikowski D, Nicolas G. Electrophysiological diagnosis of Guillain-Barré syndrome subtype: Could a single study suffice? J Neurol Neurosurg Psychiatry. 2015;86:115–9. doi: 10.1136/jnnp-2014-307815. [DOI] [PubMed] [Google Scholar]
- 9.Hughes RAC, Cornblath DR. Guillain-Barré syndrome. Lancet. 2005;366:1653–66. doi: 10.1016/S0140-6736(05)67665-9. [DOI] [PubMed] [Google Scholar]
- 10.Meulstee J, Fg van der M. Electrodiagnostic criteria for polyneuropathy and demyelination: Application in 135 patients with Guillain-Barré syndrome. Dutch Guillain-Barré Study Group. J Neurol Neurosurg Psychiatry. 1995;59:482–6. doi: 10.1136/jnnp.59.5.482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Uncini A, Vallat J-M. Autoimmune nodo-paranodopathies of peripheral nerve: The concept is gaining ground. J Neurol Neurosurg Psychiatry. 2018;89:627–35. doi: 10.1136/jnnp-2017-317192. [DOI] [PubMed] [Google Scholar]
- 12.Franssen H. Towards international agreement on criteria for Guillain-Barré syndrome. Clin Neurophysiol. 2012;123:1483–4. doi: 10.1016/j.clinph.2012.02.078. [DOI] [PubMed] [Google Scholar]
- 13.Shahrizaila N, Kokubun N, Sawai S, Umapathi T, Chan Y-C, Kuwabara S, et al. Antibodies to single glycolipids and glycolipid complexes in Guillain-Barré syndrome subtypes. Neurology. 2014;83:118–24. doi: 10.1212/WNL.0000000000000577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kalita J, Misra UK. Antiganglioside antibody: A hope or hype? Neurol India. 2017;65:975–6. doi: 10.4103/neuroindia.NI_706_17. [DOI] [PubMed] [Google Scholar]
- 15.Uncini A, Ippoliti L, Shahrizaila N, Sekiguchi Y, Kuwabara S. Optimizing the electrodiagnostic accuracy in Guillain-Barré syndrome subtypes: Criteria sets and sparse linear discriminant analysis. Clin Neurophysiol. 2017;128:1176–83. doi: 10.1016/j.clinph.2017.03.048. [DOI] [PubMed] [Google Scholar]


