Abstract
Introduction:
Despite the fact that the goals for the management of hypertension are well-defined and effective therapies are available, control of hypertension remains poor in countries with low resources including Ethiopia. This study aimed to determine blood pressure control rate and its determinants among ambulatory adult hypertensive patients at Jimma University Medical Center.
Methods:
A general prospective cohort study was conducted among adult hypertensive patients who had regular follow-up at Jimma University Cardiac Clinic from 20 March to 20 June 2018. Hypertensive patients who fulfilled the inclusion criteria were selected in the first month of the data collection period. Then, only those patients who visited the clinic at the first month were consequently followed-up for the next 3 months. The Eighth Joint National Committee guideline was used to categorize controlled and uncontrolled blood pressures. Patients’ specific data were collected using a structured data collection tool. Data were analyzed using the statistical software package SPSS version 21.0. Bivariate and multivariable logistic regression analysis was used to identify independent variables influencing blood pressure control. p-values of less than 0.05 were considered statistically significant.
Results:
From a total of 416 patients, 237 (57.0%) were male with a mean age of 56.50 ± 11.96 years. Two hundred and fifty eight (62.0%) participants had comorbid conditions and 275 (66.1%) were on combination therapy. The rate of blood pressure control was 42.8%. Age ⩾60 years was negatively associated with uncontrolled blood pressure (adjusted odd ratio = 0.52, confidence interval = 0.31–0.88, p = 0.015). Medication non-adherence (adjusted odd ratio = 1.64, confidence interval = 1.04–2.58, p = 0.034) and non-adherence to international guidelines (adjusted odd ratio = 2.33, confidence interval = 1.49–3.64, p < 0001) were positively associated with uncontrolled blood pressure.
Conclusion:
The rate of blood pressure control among hypertensive patients was suboptimal. Age, clinicians’ non-adherence to international guidelines, and patients’ non-adherence to medications were independent predictors of blood pressure control. Physicians and clinical pharmacists should adhere to guidelines for better treatment and care of hypertensive patients.
Keywords: Hypertension, blood pressure control, guidelines, adherence
Introduction
Hypertension is a significant worldwide public health problem due to the high frequency and risk of developing cardiovascular and renal diseases. 1 It affects more than 1 billion people in the world with a terrifying projection to be 1.56 billion by the year 2025. 2 Almost three-quarters of people with hypertension (639 million people) live in developing countries with limited health resources.1,2 In Ethiopia, there is different prevalence report in different studies and across different regions of the country.3,4 Systematic meta-analyses conducted in 2014 using published and unpublished articles showed that the prevalence of hypertension in Ethiopia was 19.6%. 4
The prevention and control of hypertension has not yet gotten due consideration in many developing countries. 5 Hypertension is responsible for at least 40.6% of deaths due to all coronary heart diseases (CHDs), 38.5% of deaths due to stroke, and the second leading cause of end-stage renal disease (ESRD). 6 Blood pressure (BP) lowering significantly reduces vascular risk across various baseline BP levels and comorbidities.7–10 Unfortunately, the majority of patients’ BP was poorly controlled in most health care settings, especially in countries with minimal resources.7,9,11,12
Poorly controlled BP is also associated with various medical and psychosocial complications, low health-related quality of life, and increased health care costs. 13 Silent clinical picture and higher prevalence of hypertension, low people awareness (43%), poor adherence to antihypertensive medication, bad dietary habits, and high costs of drugs contribute to poor BP control.5,14–16 Moreover, in developing countries, government priority is given to acute disorders, child and maternal health care, and control of communicable diseases, giving very little emphasis on chronic non-communicable diseases. 4
The choice of antihypertensive drug classes is influenced by many factors such as age, race, stage of hypertension, presence of concomitant disease, and cost of medications.17,18 Initial treatment for the black population is either thiazide diuretics (TDs) or calcium channel blockers (CCBs) alone or in combination. For adult patients with hypertension and chronic kidney disease (CKD), or without diabetes, the initial choice will be angiotensin-converting enzyme inhibitors (ACEIs) or angiotensin receptor blockers (ARBs) alone or in combination with other drug classes irrespective of age and race.15,19 Hypertension management guidelines, in large part, are evidence-based and are usually dictated by randomized controlled trial data and observational studies. Published guidelines help in clinical decision-making, decrease practice variations, guide correctness, and measure the quality of health care.20,21 One of the most commonly used guidelines considered as the “gold standard” consensus guideline for the management of hypertension was the Eighth Joint National Committee (JNC-8). JNC-8 provides shreds of evidence on detection, evaluation, and treatment of elevated BP. This guideline was used as a standard reference for this study because awareness and accessibility of guidelines were initial criteria to evaluate the status of clinician’s adherence to hypertension treatment guidelines. 21 Besides, Ethiopia does not have its hypertension treatment guideline and for the time being, this guideline is widely used by both clinicians and clinical pharmacist. 22
The overall principles common to hypertension management guidelines are implementation of lifestyle modifications in addition to pharmacotherapy to control BP. However, clinical practice guidelines do not consistently change clinicians’ behavior, control of high BP remains suboptimal, so we need to evaluate it’s use and impact on BP control. 7
Several studies were conducted worldwide on the effect of guideline adherence on BP control.19,22,23 However, little data are available in Ethiopia and clinician’s guideline adherence relation to BP control is not well studied. Also, among previous studies, there are conflicting results between prescribing patterns and level BP control status. For example, a study conducted in Kenya concluded that combination therapy was associated with poor patient adherence and hence poor BP control. 24 In contrast, according to a study conducted in Gondar, Ethiopia, loose combination pills therapy produced better BP control than monotherapy. 25 Another study conducted in Jimma, Ethiopia, showed that the number of antihypertensive medications prescribed was not associated with BP control. 26 Furthermore, studies on guidelines adherence and rate of BP control have been limited by cross-sectional study design; therefore, this prospective cohort study was conducted to assess clinicians’ adherence to hypertension treatment guidelines and BP control among ambulatory adult hypertensive patients at Jimma University Medical Center (JUMC).
Methods
Study period and setting
This study was conducted for 3 months among hypertensive patients who had regular follow-up at Jimma University Ambulatory Cardiac Clinic from 20 March to 20 June 2018.
Study design
A general prospective cohort follow-up study was employed.
Study population
Patients included in the study were all hypertensive patients with age ⩾18 years, with a documented diagnosis of hypertension, had at least two medical appointments in the year preceding the study, having a medical appointment every month and complete medical records. We excluded pregnant women, patients with confirmed neurologic and psychiatric disorders with their respective specialists, since it was challenging to assess medication adherence statuses in acutely ill patients with similar tools like that of other study participants.
Sample size and sampling technique
The sample size of participants for this study was calculated using the Cochran formula for sample size calculation for categorical variables. A previous study at Jimma University Hospital, Ethiopia, reported that the rate of BP control was 50%. 26 The minimum sample size required for this study was 384 based on the standard normal distribution (Z = 1.96) with a confidence interval (CI) of 95% and margin of error of 0.05. Finally, 416 patients were included after adjusting for a 10% non-respondent rate. All hypertensive patients who visited the ambulatory cardiac clinic during the study period and fulfilled inclusion criteria were included in this study.
Data collection and tool
Questionnaire and data abstraction format were prepared by reviewing different literatures. To assure the validity of the data collection tool, a structured questionnaire was developed translated to local languages (Amharic and Afan Oromo) and then back to English. A pre-test of data collection format was performed on 5% of the sample before conducting the study. Primary data collected from patients by face-to-face interview. Secondary data such as prescribed drugs, BP measurements, and comorbid illness were collected from patients’ chart daily during their visit.
In this study, hypertensive patients that fulfill the inclusion criteria were selected at the first month of data collection period and BP measurement at this first visit was considered as a baseline. Then, only those patients who visited the clinic at the first month were consequently followed for the next 3 months.
Operational definitions
Physical activity
It was assessed by asking each participant the number of minutes per day and the number of days per week patients doing physical activity. Then, participants were classified as physically active if they reported that they were farmers or if they reported that they exercise greater than 30 min for greater than 5 days of the week otherwise they were classified as physically inactive.
Bodyweight
It was measured using a digital scale and height was measured using a portable height board at a standing position. Body mass index (BMI) was calculated as weight in kilogram divided by squared height. We defined overweight as BMI of 25–29.9 kg/m2 and obese when BMI is ⩾30 kg/m2.
Morisky Medication Adherence Scale-8
It was used to assess the medication taking behavior of patients, the total score = >2 (low adherence), score = 0.25–2 (medium adherence), and score = 0 (high adherence). 27
Guidelines adherence
It was measured by the proportion of total number of hypertensive patients treat based on JNC-8 guideline divided by the total number of participants. The primary outcome was the rate of BP control. 28
Controlled BP
Defined systolic blood pressure (SBP) measurement <140 mm Hg and diastolic blood pressure (DBP) of <90 mm Hg for age less than 60 years and SBP <150 mm Hg and DBP of <90 mm Hg for age greater than or equal to 60 years old based on average BP measurements, otherwise defined as uncontrolled BP. 22
Data processing and analysis
The data were entered using EpiData version 3.1 and exported to the Statistical Package for Social Science (SPSS) version 21.0 for analysis. Continuous variables were presented as mean values (standard deviation). Categorical variables were presented as frequency and percentages. The frequency of each pharmacological class and individual antihypertensive medications were expressed as a percentage. If there was switching from one drug to another drug during the visit, the last regimen was included for analysis. BP was calculated by taking the average of three consecutive visits BP measurement. BP was categorized as controlled and uncontrolled based on the JNC-8 treatment guidelines. Binary logistic regression was used to determine the effect of each independent variable on BP control. Variables with a p-value less than 0.25 in the bivariate analysis were then included in a multivariable logistic regression analysis to identify key independent variables influencing BP control. 29 In multivariate analysis, variables with a p-value of <0.05 were considered statistically significant.
Results
Patient selection processes and baseline characteristics of the participants
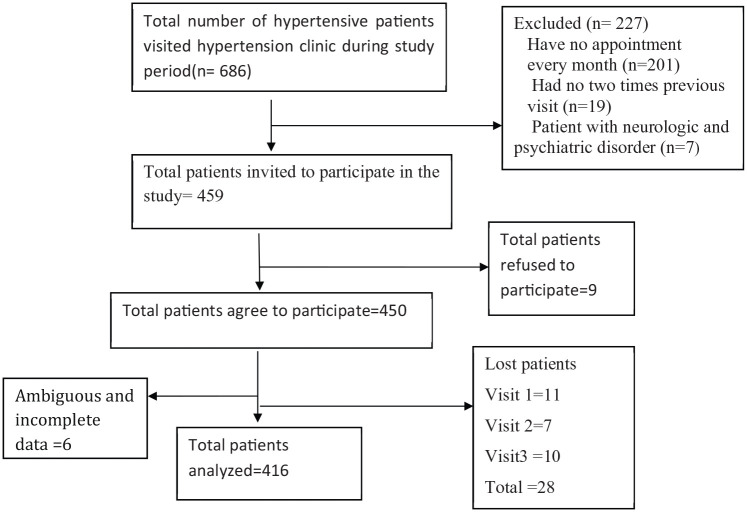
A total of 686 hypertensive patients visited the hypertension clinic during the study period. Four hundred and fifty-nine hypertensive patients fulfilled inclusion criteria and were invited to participate in the study, of these, 416 participants were finally included in the final analyses with a response rate of 90.6% (Figure 1). As depicted in Table 1, more than half (57.0%) of the participants were males. The mean age of the participants was 56.50 ± 11.96 years, with a minimum of 22 years old and a maximum of 89 years old. Nearly, two-thirds (68.3%) of the participants were married and the majority (65.9%) of them live in an urban area. Among participants, 114 (27.4%) had no formal education, 89 (21.4%) were merchants, and 109 (26.2%) had monthly income greater than 3000 Ethiopian birr (ETB).
Figure 1.
Hypertension patient selection flowchart at Jimma University Medical Center from 20 March 2018 to 20 June 2018.
Table 1.
Socio-demographic characteristics of hypertensive patients at JUMC, 2018.
| Variables | Characteristics | Frequency (%) |
|---|---|---|
| Age (years) | Mean ± SD | 56.50 ± 11.96 |
| <60 | 220 (52.9) | |
| ⩾60 | 196 (47.1) | |
| Sex | Male | 237 (57.0) |
| Female | 179 (43.0) | |
| BMI | Mean ± SD | 24.24 ± 2.32 |
| 18.5–24.9 | 314 (75.5) | |
| 25–29.9 | 89 (21.4) | |
| ⩾30 | 13 (3.1) | |
| Marital status | Single | 12 (2.9) |
| Married | 284 (68.3) | |
| Divorced | 55 (13.2) | |
| Widowed | 65 (15.6) | |
| Residency | Urban | 274 (65.9) |
| Rural | 142 (34.1) | |
| Education level | No formal education | 114 (27.4) |
| Primary education (1–8 grade) | 110 (26.4) | |
| Secondary education (9–12 grade) | 100 (24.0) | |
| Tertiary education (diploma and above) | 92 (22.1) | |
| Current occupation | Civil servant | 69 (16.6) |
| Merchant | 89 (21.4) | |
| Farmer | 74 (17.8) | |
| House wife | 47 (11.3) | |
| Retired | 36 (8.7) | |
| Jobless | 70 (16.8) | |
| Others a | 31 (7.5) | |
| Monthly income (ETB) | <1000 | 58 (13.9) |
| 1001–2000 | 68 (16.3) | |
| 2001–3000 | 74 (17.8) | |
| >3000 | 109 (26.2) | |
| Without well-defined monthly income | 107 (25.7) | |
| Living status | I live alone | 59 (14.2) |
| I live with family | 328 (78.8) | |
| Others b | 29 (7.0) |
SD: standard deviation; BMI: body mass index; ETB: Ethiopian birr.
Drivers, daily laborer, non-governmental organization, and private work.
Live with friends and prison.
The majority (63.5%) of participants have been taking salt with food. More than half, 222 (53.4%) of the participants were physically inactive and 89 (21.4%%) were overweight (BMI = 25–29.9) and 13 (3.1%) were obese (BMI ⩾30). One hundred and three (24.8%) participants were alcohol drinkers, 138 (33.2%) were chat chewers, 20 (4.8%) were cigarette smokers, and 238 (57.2%) drunk coffee. Out of the total study participants, 258 (62.0%) had comorbidities. One hundred and four (25.0%) of the participants had diabetes mellitus (DM), and 38 (9.1%) and 39 (9.4%) had CHD and dyslipidemia, respectively. Fourteen (3.4%) participants had other comorbidities (anemia, peripheral neuropathy, lung disease, liver disease, thyroid disorder, and human immunodeficiency virus infection). Most of the patients, 148 (35.6%) had been on antihypertensive therapy for between 1 and 5 years (Table 2).
Table 2.
Lifestyle-related factors and clinical characteristics of hypertensive patients at JUMC, 2018.
| Factors | Frequency (%) | |
|---|---|---|
| Add salt to food | Yes | 264 (63.5) |
| No | 152 (36.5) | |
| Alcohol use | Yes | 103 (24.8) |
| No | 313 (75.2) | |
| Chew chat | Yes | 138 (33.2) |
| No | 278 (66.8) | |
| Cigarette smoking | Never smoked | 303 (72.8) |
| Ex-smoker | 93 (22.4) | |
| Current smoker | 20 (4.8) | |
| Physical activity | Physically active | 194 (46.6) |
| Physically inactive | 222 (53.4) | |
| Drink coffee | Yes | 238 (57.2) |
| No | 178 (42.8) | |
| Use traditional medicine | Yes | 16 (3.8) |
| No | 400 (96.2) | |
| Comorbidity | Hypertension alone | 158 (38.0) |
| DM | 104 (25.0) | |
| CKD | 16 (3.8) | |
| CHF | 31 (7.5) | |
| CHD | 38 (9.1) | |
| DM and CKD | 16 (3.8) | |
| Dyslipidemia | 39 (9.4) | |
| Others a | 14 (3.4) | |
| Duration on treatment (years) | <1 | 67 (16.1) |
| 1–5 | 148 (35.6) | |
| >5–10 | 144 (34.6) | |
| >10 | 57 (13.7) |
DM: diabetes mellitus; CHF: chronic heart failure; CHD: coronary heart disease; CKD: chronic kidney disease.
Anemia, peripheral neuropathy, lung disease, liver disease, thyroid disorder, and human immunodeficiency virus infection.
Clinicians’ adherence to hypertension treatment guidelines
Most prescribers perceived that JNC-8 hypertension treatment guideline was evidence-based and helpful in the management of patients. However, the overall adherence of clinicians to JNC-8 guidelines was low, 184 (44.2%) (Figure 2).
Figure 2.
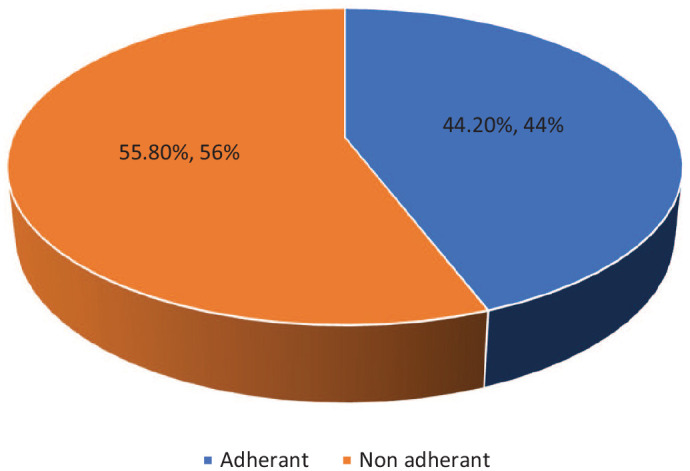
Proportion of clinicians’ adherence to JNC-8 hypertension treatment guidelines at JUMC, 2018.
Patients’ adherence to hypertension treatment
A total of 410 study participants were treated with one or more antihypertensive medication at JUMC during the study period. From patients’ self-response to the 8-item Morisky Medication Adherence Scale (MMAS-8), the overall prevalence of antihypertensive medication adherence was 191 (46.6%) (Figure 3).
Figure 3.
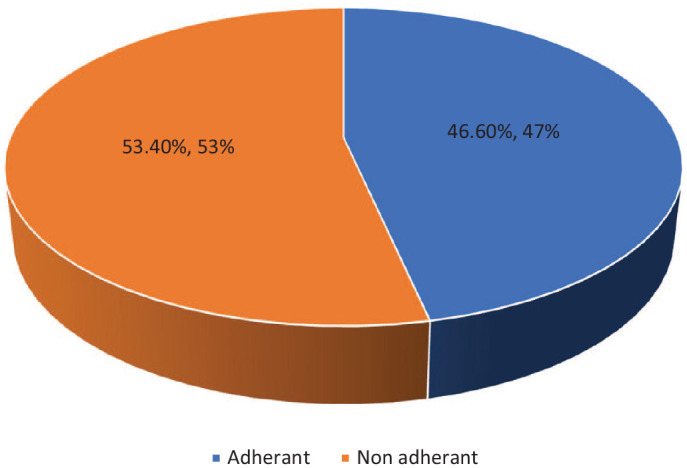
Prevalence of patients’ medication adherence at JUMC, 2018.
BP control levels among hypertensive patients
Overall, 178 (42.8%) hypertensive patients attained adequate BP control, which means BP below 140/90 mm Hg for age less than 60 years, and for DM and CKD patients, BP below 150/90 mm Hg was considered as a target for age ⩾60 years old based on average BP measurement. The mean SBP was 143.82 ± 15.08 mm Hg, while the mean DBP was 87.37 ± 8.40 mm Hg. From the total study participants, 207 (49.8%) of them had controlled SBP; while more than half of (52.2%) study participants had controlled DBP (Table 3).
Table 3.
Rate of blood pressure control among hypertensive patients at JUMC, 2018.
| Description | At first visit, n (%) | At second visit, n (%) | At third visit, n (%) | Average BP, n (%) |
|---|---|---|---|---|
| SBP (mm Hg) (mean ± SD) | 140.35 ± 19.05 | 143.18 ± 15.20 | 146.90 ± 15.84 | 143.82 ± 15.08 |
| Controlled | 224 (53.8) | 210 (50.5) | 187 (45.0) | 207 (49.8) |
| Uncontrolled | 192 (46.2) | 206 (49.5) | 229 (55.0) | 209 (50.2) |
| DBP (mm Hg) (mean ± SD) | 84.73 ± 10.57 | 87.05 ± 8.04 | 89.79 ± 10.07 | 87.37 ± 8.40 |
| Controlled | 231 (55.5) | 223 (53.6) | 207 (49.8) | 220 (52.9) |
| Uncontrolled | 185 (44.5) | 193 (46.4) | 209 (50.2) | 196 (47.1) |
| Both SBP and DBP | ||||
| Controlled | 179 (43.0) | 174 (41.8) | 180 (43.3) | 178 (42.8) |
| Uncontrolled | 237 (57.0) | 244 (58.2) | 236 (56.7) | 238 (57.2) |
BP: blood pressure; SD: standard deviation; SBP: systolic blood pressure; DBP: diastolic blood pressure.
Determinants of uncontrolled BP among hypertensive patients
After adjusting for covariates, in multivariate logistic regression analyses, age, medication non-adherence, and clinicians’ non-adherence to JNC-8 guidelines were significantly associated with uncontrolled BP. In this study, those aged ⩾60 years were 48% (adjusted odd ratio (AOR) = 0.52, CI = 0.31–0.88, p = 0.015) less likely to have uncontrolled BP than those aged <60 years. The rate of BP control was not significantly associated with monthly income (AOR = 2.29, CI = 0.93–5.65, p = 0.073). In addition, medication non-adherent patients were 1.64 times more likely to have uncontrolled BP than adherents (AOR = 1.64, CI = 1.04–2.58, p = 0.034). As well, patients treated not based on JNC-8 treatment guideline were two times more likely to have uncontrolled BP as compared to patients treated with recommendations of JNC-8 guideline (AOR = 2.33, CI = 1.49–3.64, p = 000) (Table 4).
Table 4.
Binary logistic and multiple regression analyses to identify factors associated with uncontrolled blood pressure among hypertensive patients at JUMC, 2018.
| Variables | BP control status | COR (95% CI) | p-value | AOR (95% CI) | p-value | ||
|---|---|---|---|---|---|---|---|
| Controlled | Uncontrolled | ||||||
| Age category | <60 | 75 | 139 | 1.00 | 1.000 | 1.00 | 1.000 |
| ⩾60 | 100 | 96 | 0.52 (0.35–0.77) | 0.001 | 0.52 (0.31–0.88) | 0.015 | |
| Residency | Urban | 108 | 162 | 1.00 | 1.000 | 1.00 | 1.000 |
| Rural | 67 | 73 | 0.73 (0.48–1.20) | 0.128 | 0.92 (0.49–1.75) | 0.807 | |
| Education status | No formal education | 56 | 58 | 0.81 (0.47–1.42) | 0.469 | 1.29 (0.50–3.36) | 0.603 |
| Primary | 49 | 61 | 1.08 (0.63–1.89) | 0.794 | 1.51 (0.62–3.67) | 0.362 | |
| Secondary | 32 | 68 | 1.60 (0.89–2.89) | 0.118 | 1.83 (0.77–4.40) | 0.174 | |
| Tertiary | 41 | 51 | 1.00 | 1.000 | 1.00 | 1.000 | |
| Occupation | Civil servant | 27 | 40 | 1.00 | 1.000 | 1.00 | 1.000 |
| Merchant | 31 | 57 | 1.24 (0.64–2.39) | 0.518 | 0.94 (0.36–2.45) | 0.895 | |
| Farmer | 32 | 40 | 0.84 (0.43–1.65) | 0.621 | 0.76 (0.24–2.39) | 0.640 | |
| House wife | 21 | 25 | 0.70 (0.36–1.72) | 0.572 | 0.67 (0.23–2.02) | 0.482 | |
| Retired | 15 | 21 | 0.95 (0.42–2.15) | 0.893 | 0.98 (0.32–3.02) | 0.966 | |
| Jobless | 38 | 32 | 0.57 (0.29–1.12) | 0.102 | 0.66 (0.22–1.99) | 0.465 | |
| Others a | 11 | 20 | 1.23 (0.51–2.97) | 0.649 | 1.11 (0.34–3.68) | 0.862 | |
| Monthly income (ETB) | <1000 | 18 | 40 | 1.61 (0.82–3.17) | 0.166 | 2.29 (0.93–5.65) | 0.073 |
| 1001–2000 | 32 | 35 | 0.79 (0.43–1.47) | 0.461 | 0.89 (0.41–1.92) | 0.766 | |
| 2001–3000 | 27 | 46 | 1.24 (0.67–2.28) | 0.496 | 1.22 (0.61–2.44) | 0.576 | |
| Not well known | 53 | 52 | 0.71 (0.41–1.22) | 0.219 | 1.07 (0.47–2.43) | 0.865 | |
| >3000 | 45 | 62 | 1.00 | 1.000 | 1.00 | 1.000 | |
| Treatment regimen | Monotherapy | 67 | 68 | 1.00 | 1.000 | 1.00 | 1.000 |
| Dual therapy | 75 | 118 | 1.55 (0.99–2.42) | 0.053 | 1.58 (0.95–2.65) | 0.080 | |
| Triple therapy | 27 | 44 | 1.61 (0.89–2.89) | 0.113 | 1.87 (0.95–3.71) | 0.069 | |
| Quadruple therapy | 6 | 5 | 0.82 (0.24–2.82) | 0.754 | 1.11 (0.27–4.71) | 0.894 | |
| Concurrent medications | One drug | 20 | 39 | 1.49 (0.80–2.78) | 0.211 | 1.54 (0.74–3.17) | 0.247 |
| Two drugs | 44 | 53 | 0.92 (0.53–1.53) | 0.749 | 0.80 (0.43–1.50) | 0.494 | |
| Three drugs | 31 | 44 | 1.08 (0.62–1.89) | 0.776 | 1.22 (0.58–2.53) | 0.602 | |
| ⩾Four drugs | 12 | 10 | 0.64 (0.26–1.56) | 0.324 | 0.92 (0.31–2.74) | 0.884 | |
| No medications | 68 | 89 | 1.00 | 1.000 | 1.00 | 1.000 | |
| Comorbidities | HTN alone | 63 | 93 | 1.00 | 1.000 | 1.00 | 1.000 |
| DM | 48 | 53 | 0.75 (0.45–1.24) | 0.260 | 0.64 (0.31–1.29) | 0.207 | |
| CKD | 7 | 9 | 0.87 (0.31–2.46) | 0.794 | 0.92 (0.30–2.83) | 0.888 | |
| CHF | 14 | 17 | 0.82 (0.38–1.79) | 0.622 | 0.61 (0.26–1.46) | 0.269 | |
| CHD | 13 | 25 | 1.30 (0.62–2.74) | 0.485 | 1.04 (0.44–2.49) | 0.933 | |
| DM + CKD | 8 | 8 | 0.68 (0.24–1.90) | 0.459 | 0.84 (0.25–2.48) | 0.770 | |
| Dyslipidemia | 19 | 19 | 0.68 (0.33–1.38) | 0.284 | 0.59 (0.27–1.32) | 0.200 | |
| Others b | 3 | 11 | 2.48 (0.67–9.26) | 0.175 | 1.50 (0.36–6.20) | 0.574 | |
| Duration of treatment | <1 | 23 | 40 | 1.93 (0.93–4.01) | 0.077 | 1.80 (0.80–4.08) | 0.157 |
| 1–5 | 58 | 88 | 1.67 (0.91–3.12) | 0.097 | 1.32 (0.67–2.63) | 0.426 | |
| >5–10 | 64 | 80 | 1.39 (0.75–2.57) | 0.295 | 1.22 (0.62–2.42) | 0.564 | |
| >10 | 30 | 27 | 1.00 | 1.000 | 1.00 | 1.000 | |
| Patient adherent status | Adherent | 93 | 98 | 1.00 | 1.000 | 1.000 | 1.000 |
| Non-adherent | 82 | 137 | 1.59 (1.07–2.35) | 0.022 | 1.64 (1.04–2.58) | 0.034 | |
| Guideline adherent status | Adherent | 96 | 86 | 1.00 | 1.000 | 1.00 | 1.000 |
| Non-adherent | 79 | 149 | 2.11 (1.41–3.14) | 0.000 | 2.33 (1.49–3.64) | 0.000 | |
BMI: body mass index; ETB: Ethiopian birr; BP: blood pressure DM: diabetes mellitus, CHF: chronic heart failure; CKD: chronic kidney disease, CHD: coronary heart disease, COR: crude odd ratio; AOR: adjusted odd ratio; HTN: hypertension.
Others denote drivers, daily laborer, non-governmental organization, and private work.
Live with friends and prison.
Anemia, peripheral neuropathy, lung disease, liver disease, thyroid disorder, and human immunodeficiency virus infect.
Discussion
Hypertension is a chronic disease that requires lifelong treatment. The result of this study showed that less than one-half (42.8%) of hypertensive patients had controlled BP. The result was closely similar to studies done in Nigeria (45.3%), Kenya (46%), and University of Gondar (42.9%).30–32 The finding is also similar to the result from Adama Hospital Medical College (43.6%) and previous study at Jimma University (43.51%).28,33 However, the rate of BP control was better than studies done in Southern China (13.5%) rural and urban communities in high-, middle-, and low-income countries (32.5%).34,35 The difference might be due to variation in inclusion criteria, site of studies, and the cut-off points used in defining the BP control. We used JNC-8 where BP control in >60 years was 150/90 mm Hg, but other studies used BP <140/90 mm Hg irrespective of the age. It was also higher as compared to a study done in Zewditu Memorial Hospital, Addis Ababa (30.1%). 22 The difference in the sample size (356 participants) might have contributed to this difference. However, the level of BP control found in this study was lower than studies done in Hong Kong, China (52.5%), Congo (54.2%), and Nekemte Referral Hospital, Ethiopia.36–38 The higher level of BP control rate might be due to better medical and pharmaceutical care to patients, better education and awareness of patients to hypertension treatment, and the use of different guidelines as a standard in these countries.
The factors that contributed to the inadequate BP control in this study were age, patients’ poor medication adherence, and inappropriate prescription pattern. The association between age and BP control remains a subject of debate; both negative and positive relationships have been reported in many literatures.39,40 In this study, patients with age ⩾60 years were less likely to have uncontrolled BP than patients with age <60 years. It was similar to studies done in Korea and Saudi Arabia,41,42 but contradictory to findings from Kenya and Taiwan.31,39 This might be due to the fact that older patients perceive themselves as being sick and therefore more likely to take their medication. It is also argued that older patients receive more attention from their family members and this entails more constant reminders to have close follow-up and to take their medication, although this needs further investigation.
This study showed that medication non-adherent patients were more likely to have uncontrolled BP than adherents. This finding was in line with studies conducted in Gondar University Hospital and Mekelle Public Hospital, Ethiopia.32,41 This might be due to that whenever there is poor medication adherence, it could be the single most important reason for uncontrolled hypertension, since hypertension treatment requires taking the right drug with the right dose at right time.
The result of this study showed that among study participants treated appropriately based on JNC-8 guidelines, 53.3% had controlled BP as compared to those treated inappropriately (34.5%). This result indicated that not adhering JNC-8 hypertensive treatment guideline was significantly associated with poor BP control (AOR = 2.33, CI = 1.49–3.64). The finding was similar to the studies conducted at Gondar University Hospital and Zewditu Memorial Hospital, Addis Ababa, Ethiopia, and it might be due to comparable health care professionals, health care service, and medication availability.22,25 The prevalence of appropriate use of antihypertensive medications was 44.2% in this study. It was lower than studies conducted in South Indian (65%) and South Africa (51.9%).17,42 This difference might be due to racial difference, health care setting difference, and lack of laboratory and imaging facilities for further screening of target organ damage in our setting. Besides, it might be explained by the difference in doctors’ profiles since the majority of physicians treating hypertensive patients in this study were general practitioners and first-year residency students.
Limitations of the study
There are some limitations to this study. The study was conducted in one facility; therefore, the findings may not be generalized to reflect the health care setting in Ethiopia. Only prescription and comorbidity data were used to examine compliance to treatment guidelines, which may reliable. Finally, this study was unable to identify factors affecting clinicians’ adherence to standard treatment guidelines but will be an interesting area for future research.
Conclusion
The rate of BP control among ambulatory adult hypertensive patients was suboptimal. Age, clinicians’ non-adherence to international guidelines, and patients’ non-adherence to medications were independent predictors of level of BP control among adult hypertensive patients at JUMC. ACEIs were the most frequently prescribed class of antihypertensive drugs in both monotherapy and combination therapy. This might be due to prescribers (clinicians) were not adhere to standard treatment guidelines (JNC-8). CCBs and TDs are the recommended first-line medicines for hypertension for Africa origin as per this guideline; the rate of BP-controlled status was suboptimal.
Supplemental Material
Supplemental material, sj-docx-1-smo-10.1177_20503121211006000 for Rate of blood pressure control and its determinants among adult hypertensive patients at Jimma University Medical Center, Ethiopia: Prospective cohort study by Bekalu Kebede, Legese Chelkeba and Bekalu Dessie in SAGE Open Medicine
Acknowledgments
The authors thank the participants of the study.
Footnotes
Author contributions: B.K. contributed to concept and design, data acquisition, interpretation of data, and manuscript preparation. L.C. contributed to concept and design, interpretation of data, manuscript preparation, manuscript revision, and manuscript review. B.D. has participated in the preparation of the manuscript. All authors read and approved the final manuscript.
Availability of data and materials: The data sets used and/or analyzed during this study are available from the corresponding author on reasonable request.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: Prior to data collection, appropriate ethical clearance was obtained from the Ethical Review Board of School of Pharmacy, Institute of Health Science Jimma University (reference no. IHRPGD/203/18).
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was funded by the Jimma University, College of Health Sciences. The university has no role in designing, conducting, and reporting this study.
Informed consent: Prior to data collection, individual informed verbal consent was obtained from the study participant. Written informed consent was waived since this study did not involve any procedure and presents no damage to patients as approved by the ethical review board committee of Board of School of Pharmacy, Institute of Health Science Jimma University. Patients were informed about the objective of the study; procedures of selection and assurance of confidentiality and their names were not registered to minimize social desirability bias and enhance anonymity. They were not forced to participate or receive any monetary incentive, and it was solely voluntary based.
ORCID iDs: Bekalu Kebede  https://orcid.org/0000-0001-9758-4265
https://orcid.org/0000-0001-9758-4265
Legese Chelkeba  https://orcid.org/0000-0002-0323-5011
https://orcid.org/0000-0002-0323-5011
Bekalu Dessie  https://orcid.org/0000-0002-0201-6829
https://orcid.org/0000-0002-0201-6829
Supplemental material: Supplemental material for this article is available online.
References
- 1. Benziger CP, Roth GA, Moran AE. The global burden of disease study and the preventable burden of NCD. Glob Heart 2016; 11(4): 393–397. [DOI] [PubMed] [Google Scholar]
- 2. Bromfield S, Muntner P. High blood pressure: the leading global burden of disease risk factor and the need for worldwide prevention programs. Curr Hypertens Rep 2013; 15(3): 134–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kibret KT, Mesfin YM. Prevalence of hypertension in Ethiopia: a systematic meta-analysis. Public Health Rev 2015; 36(1): 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Molla M. Systematic reviews of prevalence and associated factors of hypertension in Ethiopia: finding the evidence. Sci J Publ Health 2015; 3(4): 514–519. [Google Scholar]
- 5. Sarki AM, Nduka CU, Stranges S, et al. Prevalence of hypertension in low- and middle-income countries: a systematic review and meta-analysis. Medicine 2015; 94(50): e1959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Schmieder RE. End organ damage in hypertension. Dtsch Ärztebl Int 2010; 107(49): 866–873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Shin S, Song H, Oh S-K, et al. Effect of antihypertensive medication adherence on hospitalization for cardiovascular disease and mortality in hypertensive patients. Hypertens Res 2013; 36(11): 1000–1005. [DOI] [PubMed] [Google Scholar]
- 8. Stevens PE, Levin A. Evaluation and management of chronic kidney disease: synopsis of the kidney disease: improving global outcomes 2012 clinical practice guideline. Ann Intern Med 2013; 158(11): 825–830. [DOI] [PubMed] [Google Scholar]
- 9. Bundy JD, Li C, Stuchlik P, et al. Systolic blood pressure reduction and risk of cardiovascular disease and mortality: a systematic review and network meta-analysis. JAMA Cardiol 2017; 2(7): 775–781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Brunström M, Carlberg B. Association of blood pressure lowering with mortality and cardiovascular disease across blood pressure levels: a systematic review and meta-analysis. JAMA Intern Med 2018; 178(1): 28–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Aberhe W, Mariye T, Bahrey D, et al. Prevalence and factors associated with uncontrolled hypertension among adult hypertensive patients on follow-up at Northern Ethiopia, 2019: cross-sectional study. Pan Afr Med J 2020; 36: 187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Amare F, Hagos B, Sisay M, et al. Uncontrolled hypertension in Ethiopia: a systematic review and meta-analysis of institution-based observational studies. BMC Cardiovasc Disord 2020; 20(1): 129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bosu WK. The prevalence, awareness, and control of hypertension among workers in West Africa: a systematic review. Glob Health Action 2015; 8: 26227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Gebrihet TA, Mesgna KH, Gebregiorgis YS, et al. Awareness, treatment, and control of hypertension is low among adults in Aksum town, northern Ethiopia: a sequential quantitative-qualitative study. PLoS One 2017; 12(5): e0176904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Parati G, Omboni S, Compare A, et al. Blood pressure control and treatment adherence in hypertensive patients with metabolic syndrome: protocol of a randomized controlled study based on home blood pressure telemonitoring vs. conventional management and assessment of psychological determinants of adherence (TELEBPMET Study). Trials 2013; 14(1): 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Okai DE, Manu A, Amoah EM, et al. Patient-level factors influencing hypertension control in adults in Accra, Ghana. BMC Cardiovasc Disord 2020; 20: 123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Datta S. Utilization study of antihypertensives in a South Indian tertiary care teaching hospital and adherence to standard treatment guidelines. J Basic Clin Pharm 2016; 8(1): 33–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Weber MA, Schiffrin EL, White WB, et al. Clinical practice guidelines for the management of hypertension in the community: a statement by the American Society of Hypertension and the International Society of Hypertension. J Clin Hypertens 2014; 16(1): 14–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Romday R, Gupta AK, Bhambani P. An assessment of antihypertensive drug prescription patterns and adherence to Joint National Committee-8 hypertension treatment guidelines among hypertensive patients attending a tertiary care teaching hospital. Int J Res Med Sci 2016; 4(12): 5125–5133. [Google Scholar]
- 20. Jellinger PS, Handelsman Y, Rosenblit PD, et al. American Association of Clinical Endocrinologists and American College of Endocrinology guidelines for management of dyslipidemia and prevention of cardiovascular disease—executive summary. Endocr Pract 2017; 23(4): 479–497. [DOI] [PubMed] [Google Scholar]
- 21. James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014; 311(5): 507–520. [DOI] [PubMed] [Google Scholar]
- 22. Yazie D, Shibeshi W, Alebachew M, et al. Assessment of blood pressure control among hypertensive patients in Zewditu Memorial Hospital, Addis Ababa, Ethiopia: a cross-sectional study. J Bioanal Biomed 2018; 10(3): 80–87. [Google Scholar]
- 23. Tomas A, Tomić Z, Milijasević B, et al. Patterns of prescription antihypertensive drug utilization and adherence to treatment guidelines in the city of Novi Sad. Vojnosanit Pregl 2016; 73(6): 531–537. [DOI] [PubMed] [Google Scholar]
- 24. Mutua EM, Gitonga MM, Mbuthia B, et al. Level of blood pressure control among hypertensive patients on follow-up in a Regional Referral Hospital in Central Kenya. Pan Afr Med J 2014; 18: 278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Abegaz TM, Tefera YG, Abebe TB. Antihypertensive drug prescription patterns and their impact on outcome of blood pressure in Ethiopia: a hospital-based observational study. Value Health 2017; 20(9): A627–A628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Asgedom SW, Gudina EK, Desse TA. Assessment of blood pressure control among hypertensive patients in Southwest Ethiopia. PLoS One 2016; 11(11): e0166432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care 1986; 24(1): 67–74. [DOI] [PubMed] [Google Scholar]
- 28. Hussein M, Lenjisa JL, Woldu MA, et al. Assessment of drug related problems among hypertensive patients on follow up in Adama Hospital Medical College, East Ethiopia. Clin Pharmacol Biopharmaceut 2014; 3: 122. [Google Scholar]
- 29. Fekadu G, Adamu A, Gebre M, et al. Magnitude and determinants of uncontrolled blood pressure among adult hypertensive patients on follow-up at Nekemte Referral Hospital, Western Ethiopia. Integr Blood Press Control 2020; 13: 49–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Bakare OQ, Akinyinka MR, Goodman O, et al. Antihypertensive use, prescription patterns, and cost of medications in a Teaching Hospital in Lagos, Nigeria. Niger J Clin Pract 2016; 19(5): 668–672. [DOI] [PubMed] [Google Scholar]
- 31. Mbui JM, Oluka MN, Guantai EM, et al. Prescription patterns and adequacy of blood pressure control among adult hypertensive patients in Kenya; findings and implications. Expert Rev Clin Pharmacol 2017; 10(11): 1263–1271. [DOI] [PubMed] [Google Scholar]
- 32. Teshome DF, Demssie AF, Zeleke BM. Determinants of blood pressure control amongst hypertensive patients in Northwest Ethiopia. PLoS One 2018; 13(5): e0196535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Muleta S, Melaku T, Chelkeba L, et al. Blood pressure control and its determinants among diabetes mellitus co-morbid hypertensive patients at Jimma University Medical Center, South West Ethiopia. Clin Hypertens 2017; 23: 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Li W, Gu H, Teo KK, et al. Hypertension prevalence, awareness, treatment, and control in 115 rural and urban communities involving 47 000 people from China. J Hypertens 2016; 34(1): 39–46. [DOI] [PubMed] [Google Scholar]
- 35. Chow CK, Teo KK, Rangarajan S, et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA 2013; 310(9): 959–968. [DOI] [PubMed] [Google Scholar]
- 36. Kang CD, Tsang PP, Li WT, et al. Determinants of medication adherence and blood pressure control among hypertensive patients in Hong Kong: a cross-sectional study. Int J Cardiol 2015; 182: 250–257. [DOI] [PubMed] [Google Scholar]
- 37. Lulebo AM, Mutombo PB, Mapatano MA, et al. Predictors of non-adherence to antihypertensive medication in Kinshasa, Democratic Republic of Congo: a cross-sectional study. BMC Res Notes 2015; 8: 526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Khayyat SM, Khayyat SMS, Hyat Alhazmi RS, et al. Predictors of medication adherence and blood pressure control among Saudi hypertensive patients attending primary care clinics: a cross-sectional study. PLoS One 2017; 12(1): e0171255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Ettehad D, Emdin CA, Kiran A, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet 2016; 387(10022): 957–967. [DOI] [PubMed] [Google Scholar]
- 40. Lee CY, Huang CC, Shih HC, et al. Factors influencing antihypertensive medication compliance in Taiwan: a nationwide population-based study. Eur J Prev Cardiol 2013; 20(6): 930–937. [DOI] [PubMed] [Google Scholar]
- 41. Theodorou M, Stafylas P, Kourlaba G, et al. Physicians’ perceptions and adherence to guidelines for the management of hypertension: a national, multicentre, prospective study. Int J Hypertens 2012; 2012: 503821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Adedeji AR, Tumbo J, Govender I. Adherence of doctors to a clinical guideline for hypertension in Bojanala district, North-West Province, South Africa. Afr J Prim Health Care Fam Med 2015; 7(1): 776. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-smo-10.1177_20503121211006000 for Rate of blood pressure control and its determinants among adult hypertensive patients at Jimma University Medical Center, Ethiopia: Prospective cohort study by Bekalu Kebede, Legese Chelkeba and Bekalu Dessie in SAGE Open Medicine