Abstract
Purpose
Minimally invasive surgery (MIS) for total knee arthroplasty (TKA) is often marketed as being able to speed up healing times over standard invasive surgery (SIS) through the medial parapatellar approach. The advantages of these minimally invasive approaches, however, are not yet definitively established. A meta-analysis of studies comparing peri-operative and post-operative differences and long-term complications of MIS versus SIS for TKA was conducted.
Methods
This meta-analysis was conducted following the PRISMA guidelines. The Pubmed, Google Scholar, Scopus, and Embase databases were accessed in September 2020. All clinical trials comparing minimally-invasive versus standard approaches for TKA were considered. Only studies reporting quantitative data under the outcomes of interest were included. Methodological quality assessment was performed using the PEDro appraisal score.
Results
This meta-analysis covers a total of 38 studies (3296 procedures), with a mean 21.3 ± 24.3 months of follow-up. The MIS group had shorter hospitalization times, lower values of total estimated blood loss, quicker times of straight-leg raise, greater values for range of motion, higher scores on the Knee Society Clinical Rating System (KSS) and its related Function Subscale (KSFS). Pain scores, anterior knee pain and revision rate were similar between MIS and SIS. SIS allowed a quicker surgical duration.
Conclusion
The present meta-analysis encourages the use of minimally invasive techniques for total knee arthroplasty. However, MIS TKA is technically demanding and requires a long learning curve.
Level of evidence
III, meta-analysis of clinical trials.
Keywords: Total knee arthroplasty, Minimally invasive surgery, Standard invasive surgery
Introduction
The most common exposure for total knee arthroplasty (TKA) is the medial parapatellar arthrotomy (MPP) using standard incision surgery (SIS) [22]. Despite the satisfying surgical outcomes, this approach has been criticized as it produces extensive damage to the knee extensor muscle mechanism, and it may negatively affect the patellar blood supply [45]. Thus, a less invasive MPP which allowed to spare the quadriceps (quadriceps-sparing approach = QS) [30] and the limited- or mini-medial parapatellar approach (MMPP) [50]. The midvastus and subvastus [59] approaches became respectively the mini-midvastus (MMV) [15], and the mini-subvastus (MSV) [17]. MIS for TKA uses a surgical incision shorter than 14 cm, thus offering an attractive alternative for both surgeons and patients. Despite the large number of published studies comparing the MIS and standard approaches, there is still lack of consensus concerning the best approach for TKA. Under these premises, a meta-analysis comparing MIS versus the traditional MPP SIS approach for TKA was conducted, investigating outcomes and long-term complications between the two approaches. The goal of the present study is to update current evidence and offer new insights concerning the surgical exposure to the orthopaedic surgeons.
It was hypothesised that MIS for TKA may achieve superior surgical outcomes than the MPP SIS approach.
Material and methods
Search strategy
This meta-analysis was performed according to the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA guidelines) [39]. The search parameters were defined as follows:
(P) Population: patients requiring TKA;
(I) Intervention: SIS TKA though the MPP approach;
(C) Comparison: MIS TKA;
(O) Outcomes: peri-operative data, functional scores, complications.
The search was performed in September 2020. The databases accessed were Pubmed, Google Scholar, Scopus, and Embase, without any limitation on time of publication. The following keywords were used: total knee arthroplasty, total knee replacement, prosthesis, combined with minimally-invasive, medial parapatellar, mini-medial parapatellar, minivastus, subvastus, quadriceps-sparing, and further combined with anterior knee pain, revision, range of motion, scores, blood loss, surgical duration, outcomes. Two independent authors (**; **) performed the database search. If title and related abstract matched the topic, the full-text article was accessed. The bibliographies for each article of interest were screened by hand. Disagreements between the authors were debated and solved.
Eligibility criteria
Two independent authors (**; **) screened articles for inclusion. All clinical trials comparing minimally-invasive approaches for TKA to the standard approach were considered for inclusion. According to the authors’ capabilities, articles in English, French, Spanish, Italian, and German were included. Only clinical trials with evidence levels I to III were considered according to the Oxford Centre of Evidenced-Based Medicine [23]. Every type of TKA (cruciate or bi-cruciate retaining, posterior stabilized) was considered eligible. No distinction was made between different MIS approaches. Studies taking advantage of a navigation system were also included. Case series, reviews and meta-analyses, editorials and expert opinions were excluded. Biomechanical, in vitro, animal and cadaveric studies were also excluded. Only studies reporting quantitative data under the outcomes of interest were included.
Outcomes of interest
Two independent authors (**, **) screened the included studies and extracted the following generalities: year, type of study, number of knees, duration of follow-up (in months), surgical approach, percentage of osteoarthritic and female patients, mean age and body mass index (BMI) (kg/m2). For each approach, the following peri-operative endpoints were collected: duration of surgery and hospitalization, total estimated blood loss (intra-operative and post-operative). Functional scores included range of motion (ROM), knee flexion, time of straight-leg raise (SLR), the Knee Society Clinical Rating System (KSS) and its related Function Subscale (KSFS) [42] and the visual analogic scale for pain (VAS). Procedure-related complications, anterior knee pain and need for revision were also retrieved.
Methodological quality assessment
For methodological quality assessment, the PEDro scale was applied. This scale is a validated system for evaluating the quality of clinical trials [38]. Two authors (**; **) who already had extensive experience with this score independently evaluated each article. The PEDro scale evaluates studies based on the criteria: clearly eligibility criteria, allocation, baseline comparability, blinding, follow-up, analyses, point estimates and variability. A final mean value > 6 is considered to indicate good methodological quality.
Statistical analysis
The statistical analysis was performed by the main author (**). For the assessment of baseline comparability, the IBM SPSS Software was used. The unpaired t-test was performed, with values of P > 0.5 considered satisfactory. Statistical analyses were performed using Review Manager Software 5.3 (the Nordic Cochrane Collaboration, Copenhagen). For continuous variables, the inverse variance method with mean difference (MD) effect measure was adopted, while for binary data, the Mantel–Haenszel method with Odds Ratio (OR). The confidence interval was set to 95% in all comparisons. A fixed effect was set as default for every comparison. Heterogeneity was assessed through the Chi-square (χ2) and Higgins Tests (I2). If χ2 > 0.5, the I2 test was evaluated. I2 test values of 25, 50 and 75% detected respectively low, moderate and high levels of heterogeneity. If high heterogeneity was detected, a random effect model was used. The forest and funnel plot were performed to establish a visual representation of the effect measure and risk of publication bias, respectively.
Results
Literature search
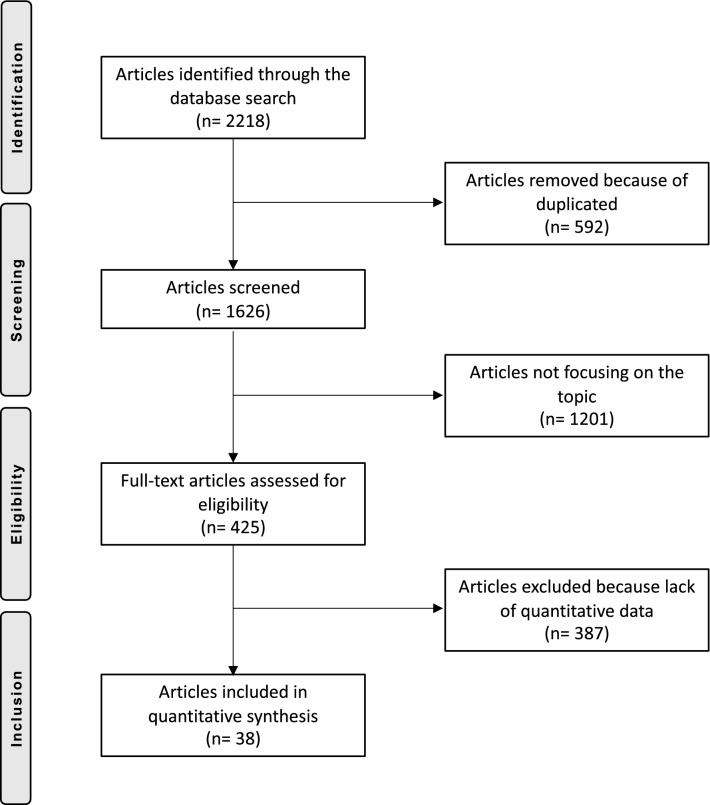
The initial literature search resulted in 2218 articles, of which 592 were duplicates. 1201 did not match the eligibility criteria and a further 371 did not report quantitative data under the outcomes of interest. Another 16 articles were excluded because of uncertain results or untrustworthy data origin. In the end, this left 38 articles for inclusion: 22 RCTs and 16 n-RCTs. Figure 1 shows the flow-chart of the literature search.
Fig. 1.
Flow-chart of the literature search
Methodological quality assessment
The mean PEDro score for included studies showed high quality at 7.3/10. The main limitation reflected in this score results from the impossibility of blinding the surgeons. This score evidenced that in 27% (10/38) of studies the follow-up was too short and 24% (9/38) did not provide any randomization of the samples. The PEDro score assigned to each study is shown in Table 1.
Table 1.
PEDro methodological assessment score
| Author | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Aslam et al. 2017 [4] | Y | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | 10 |
| Avci et al. 2013 [5] | Y | N | N | Y | N | N | N | Y | Y | Y | Y | 6 |
| Boerger et al. 2005 [6] | Y | N | N | Y | N | N | N | N | Y | Y | Y | 5 |
| Bridgman et al. 2009 [7] | Y | Y | Y | Y | N | N | Y | Y | Y | Y | Y | 9 |
| Chalidis et al. 2010 [8] | Y | Y | Y | Y | N | N | N | Y | Y | Y | Y | 8 |
| Chiang et al. 2012 [9] | Y | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | 10 |
| Cho et al. 2014 [10] | Y | Y | Y | Y | N | N | N | Y | Y | Y | Y | 8 |
| Dabboussi et al. 2012 [13] | Y | N | N | Y | N | N | N | N | Y | Y | Y | 5 |
| Feczko et al. 2016 [18] | Y | Y | Y | Y | N | N | N | N | Y | Y | Y | 7 |
| Han et al. 2008 [20] | Y | Y | Y | Y | N | N | Y | Y | Y | Y | Y | 9 |
| Hernandez-Vaquero et al. 2010 [22] | Y | Y | Y | Y | N | N | N | N | Y | Y | Y | 7 |
| Huang et al. 2015 [24] | Y | N | N | Y | N | N | N | Y | Y | Y | Y | 6 |
| Jung et al. 2009 [25] | Y | N | N | Y | N | N | N | Y | Y | Y | Y | 6 |
| Juosponis et al. 2009 [26] | Y | Y | Y | Y | N | N | Y | N | Y | Y | Y | 8 |
| Karachalios et al. 2008 [27] | Y | Y | Y | Y | N | N | N | Y | Y | Y | Y | 8 |
| Karpman et al. 2009 [28] | Y | Y | Y | Y | N | N | Y | N | Y | Y | Y | 8 |
| Kim et al. 2011 [29] | Y | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | 10 |
| King et al. 2007 [31] | Y | N | N | Y | N | N | N | N | Y | Y | Y | 5 |
| Laskin et al. 2004 [33] | Y | N | N | Y | N | N | N | N | Y | Y | Y | 5 |
| Li et al. 2017 [34] | Y | Y | Y | Y | N | N | N | Y | Y | Y | Y | 8 |
| Liebensteiner et al. 2012 [35] | Y | N | N | Y | N | N | N | N | Y | Y | Y | 5 |
| Mehta et al. 2017 [40] | Y | Y | Y | Y | N | N | N | N | Y | Y | Y | 7 |
| Rahman et al. 2015 [43] | Y | N | N | Y | N | N | N | N | Y | Y | Y | 5 |
| Schroer et al. 2008 [46] | Y | N | N | Y | N | N | N | Y | Y | Y | Y | 6 |
| Seon et al. 2007 [47] | Y | N | N | Y | N | N | N | Y | Y | Y | Y | 6 |
| Stevens-Lapsley et al. 2012 [48], 2013 [14] | Y | Y | Y | Y | N | N | Y | N | Y | Y | Y | 8 |
| Tasker et al. 2014 [49] | Y | Y | Y | Y | N | N | Y | Y | Y | Y | Y | 8 |
| Tenholder et al. 2005 [50] | Y | N | N | Y | N | N | N | Y | Y | Y | Y | 6 |
| Thienpont et al. 2013 [51] | Y | Y | Y | Y | N | N | N | Y | Y | Y | Y | 8 |
| Tsuji et al. 2010 [53] | Y | N | N | Y | N | N | N | N | Y | Y | Y | 5 |
| Unnanuntana et al. 2012 [54] | Y | N | N | Y | N | N | N | Y | Y | Y | Y | 6 |
| Unwin et al. 2017 [55] | Y | Y | Y | Y | N | N | N | Y | Y | Y | Y | 8 |
| Varela-Egocheaga et al. 2009 [56] | Y | Y | Y | Y | N | N | N | Y | Y | Y | Y | 8 |
| Watanabe et al. 2009 [57] | Y | N | N | Y | N | N | N | Y | Y | Y | Y | 6 |
| Wegrzyn et al. 2013 [58] | Y | Y | Y | Y | Y | N | Y | N | Y | Y | Y | 10 |
| Wülker et al. 2010 [60] | Y | Y | Y | Y | N | N | N | Y | Y | Y | Y | 8 |
| Zhu et al. 2015 [62] | Y | N | N | Y | N | N | N | Y | Y | Y | Y | 6 |
1. Eligibility criteria; 2. Random allocation; 3. Concealed allocation; 4. Baseline comparability; 5. Blind subject; 6. Blind clinician; 7. Blind assessor; 8. Adequate follow-up; 9. Intention-to-treat analysis; 10. Between-group analysis; 11. Point estimates and variability
Risk of publication bias
To evaluate the risk of publication bias, the funnel plot of the most reported outcome (surgical duration) was performed. The plot (Fig. 2) shows a moderate symmetrical distribution of the referral points. There is adequate distribution with respect to the no-effect line. Consequently, this meta-analysis shows a moderate risk of publication bias for.
Fig. 2.
Funnel plot of the most reported outcome, surgical duration
Patient demographic
In the present study, data from 3281 patients were collected. The mean follow-up time was 21.3 ± 24.3 months. 1697 patients had undergone TKA using a MIS approach, and 1584 patients using the SIS approach. There was baseline comparability between age, BMI, gender and diagnosis (P > 0.5). Study generalities and patient demographic are shown in Table 2, while Table 3 shows in detail the baseline characteristic of the two cohorts.
Table 2.
Study generalities and demographic baseline of the enrolled patients
| Author, year | Type of Study | Knees (n) | Follow-up (months) | Type of approach | Knees (n) | Osteoarthritis (%) | Female (%) | Mean age (years) | BMI (kg/m2) |
|---|---|---|---|---|---|---|---|---|---|
| Aslam et al. 2017 [4] | RCT | 84 | 12 | MMV | 42 | 100 | 30 | 68.8 | 30.6 |
| MPP | 42 | 100 | 57 | 68.6 | 30.1 | ||||
| Avci et al. 2013 [5] | RCT | 39 | 23.5 | MMV | 19 | 100 | 79 | 64.5 | 32.0 |
| Boerger et al. 2005 [6] | n-RCT | 120 | 3 | MSV | 60 | 100 | 77 | 69.0 | 28.0 |
| MPP | 60 | 100 | 75 | 68.0 | 29.0 | ||||
| Bridgman et al. 2009 [7] | RCT | 224 | 13 | MSV | 113 | 48 | 70.1 | ||
| MPP | 111 | 49 | 70.9 | ||||||
| Chalidis et al. 2010 [8] | RCT | 100 | 24 | MMV | 50 | 100 | 92 | 70.1 | 34.6 |
| MPP | 50 | 100 | 88 | 71.2 | 34.2 | ||||
| Chiang et al. 2012 [9] | RCT | 75 | 24 | QS | 38 | 100 | 90 | 69.7 | 28.6 |
| MPP | 37 | 100 | 90 | 69.8 | 29.6 | ||||
| Cho et al. 2014 [10] | RCT | 66 | 12 | MMV | 33 | 100 | 96 | 65.5 | 29.1 |
| MPP | 33 | 100 | 94 | 67.0 | 28.0 | ||||
| Dabboussi et al. 2012 [13] | n-RCT | 80 | 3 | MMV | 40 | 100 | |||
| MPP | 40 | 100 | |||||||
| Feczko et al. 2016 [18] | RCT | 69 | 6 | MMV | 36 | 95 | 64 | 65.1 | 28.3 |
| MPP | 33 | 100 | 67 | 64.9 | 28.6 | ||||
| Han et al.2008 [20] | RCT | 30 | 24 | MMPP | 15 | 100 | 66.0 | 26.9 | |
| MPP | 15 | 100 | 64.0 | 26.4 | |||||
| Hernandez-Vaquero et al. 2010 [22] | RCT | 62 | 6 | MMV | 26 | 100 | 81 | 70.8 | 32.1 |
| MPP | 36 | 100 | 80 | 70.5 | 30.8 | ||||
| Huang et al. 2015 [24] | n-RCT | 96 | 60 | MMPP | 35 | 100 | 86 | 69.2 | 27.0 |
| QS | 31 | 100 | 94 | 69.3 | 26.9 | ||||
| MPP | 30 | 100 | 93 | 71.2 | 26.7 | ||||
| Jung et al.2009 [25] | n-RCT | 40 | 58.4 | MSV | 21 | ||||
| MPP | 19 | ||||||||
| Juosponis et al. 2009 [26] | RCT | 70 | 3 | MMV | 35 | 100 | 86 | 72.0 | 28.0 |
| MPP | 35 | 100 | 86 | 71.4 | 29.1 | ||||
| Karachalios et al. 2008 [27] | RCT | 100 | 23 | MMV | 50 | 92 | 62 | 71.1 | 32.0 |
| MPP | 50 | 92 | 70 | 70.8 | 31.5 | ||||
| Karpman et al. 2009 [28] | RCT | 59 | 6 | MMV | 20 | 100 | 65 | 74.0 | 30.0 |
| QS | 20 | 100 | 60 | 73.0 | 28.0 | ||||
| MPP | 19 | 100 | 53 | 73.0 | 29.0 | ||||
| Kim et al. 2011 [29] | RCT | 50 | 12 | MMV | 23 | 100 | 67.0 | 27.1 | |
| MPP | 22 | 100 | 68.0 | 28.4 | |||||
| King et al. 2007 [31] | n-RCT | 150 | 1.5 | QS | 100 | 95 | 52 | 67.0 | 30.0 |
| MPP | 50 | 90 | 66 | 28.0 | 32.0 | ||||
| Laskin et al. 2004 [33] | n-RCT | 58 | 3 | MMV | 26 | 70.0 | 30.0 | ||
| MPP | 26 | 68.0 | 29.0 | ||||||
| Li et al. 2017 [34] | RCT | 50 | 12 | MSV | 25 | 100 | 64 | 69.9 | 25.8 |
| MPP | 25 | 100 | 64 | 68.1 | 25.5 | ||||
| Liebensteiner et al. 2012 [35] | n-RCT | 38 | 2 | MMV | 19 | 58 | 66.7 | 30.2 | |
| MPP | 19 | 53 | 67.6 | 31.5 | |||||
| Mehta et al. 2017 [40] | RCT | 55 | 6 | MSV/MMV | 26 | 73 | 59.8 | ||
| MPP | 29 | 73 | 61.4 | ||||||
| Rahman et al. 2015 [43] | n-RCT | 120 | 3 | MMPP | 60 | 100 | 75 | 59.8 | |
| MPP | 60 | 100 | 77 | 62.0 | |||||
| Schroer et al. 2008 [46] | n-RCT | 300 | 24 | QS | 150 | 62 | 71.0 | 31.0 | |
| MPP | 150 | 61 | 70.0 | 32.0 | |||||
| Seon et al. 2007 [47] | n-RCT | 84 | 12 | MMV | 41 | 100 | 80 | 64.2 | |
| MPP | 43 | 100 | 77 | 64.2 | |||||
| Stevens-Lapsley et al. 2012 [48], 2013 [14] | RCT | 41 | 3 | MMPP | 22 | 100 | 54 | 64.6 | 30.5 |
| MPP | 19 | 45 | 64.0 | 31.3 | |||||
| Tasker et al. 2014 [49] | RCT | 83 | 24 | MMV/MSV | 40 | 45 | 63 | 67.3 | |
| MPP | 43 | 99 | 63 | 68.2 | |||||
| Tenholder et al. 2005 [50] | n-RCT | 118 | MMPP | 69 | 56 | 66.8 | 29.3 | ||
| MPP | 49 | 47 | 63.5 | 31.5 | |||||
| Thienpont et al. 2013 [51] | RCT | 300 | 24 | MMPP | 150 | 100 | 67 | 68.0 | 30.4 |
| MPP | 150 | 100 | 70 | 69.0 | 29.8 | ||||
| Tsuji et al. 2010 [53] | n-RCT | 20 | 0.5 | MMV | 10 | 100 | 60 | 68.4 | 28.1 |
| MPP | 10 | 100 | 80 | 69.8 | 28.9 | ||||
| Unnanuntana et al. 2012 [54] | n-RCT | 64 | 60 | MMPP | 31 | ||||
| MPP | 29 | ||||||||
| Unwin et al. 2017 [55] | RCT | 66 | 72 | MMV/MSV | 32 | 76 | 67.0 | ||
| MPP | 34 | 76 | 67.0 | ||||||
| Varela-Egocheaga et al. 2009 [56] | RCT | 100 | 36 | MSV | 50 | 72 | 68.0 | 31.0 | |
| MPP | 50 | 74 | 70.6 | 30.6 | |||||
| Watanabe et al. 2009 [57] | n-RCT | 48 | 48 | MMV | 25 | 84 | 80 | 71.0 | 28.1 |
| MPP | 23 | 78 | 74 | 71.0 | 26.3 | ||||
| Wegrzyn et al. 2013 [58] | RCT | 36 | 2 | MSV | 18 | 100 | 72 | 67.0 | 30.0 |
| MPP | 18 | 100 | 72 | 64.0 | 31.0 | ||||
| Wülker et al. 2010 [60] | RCT | 134 | 12 | MSV | 66 | 92 | 73 | 70.2 | 29.3 |
| MPP | 68 | 88 | 70 | 29.3 | |||||
| Zhu et al. 2015 [62] | n-RCT | 67 | 109.2 | MMPP | 30 | 93 | 67.9 | 27.6 | |
| MPP | 37 | 84 | 65.3 | 27.7 |
MMV mini-midvastus, MSV mini-subvastus, QS quadriceps-sparing, MMPP mini-medial parapatellar, MPP medial parapatellar
Table 3.
Demographic baseline of the two cohorts
| Variable | MIS (n = 1697) | SIS (n = 1584) | P |
|---|---|---|---|
| Age (mean SD) | 68.4 ± 2.8 | 67.7 ± 2.7 | 0.8 |
| Female gender (%) | 67% | 67% | 0.9 |
| BMI (kg/m2) | 29.4 ± 1.7 | 29.2 ± 1.8 | 0.9 |
| OA patients (%) | 97% | 99% | 0.9 |
Outcomes of interest
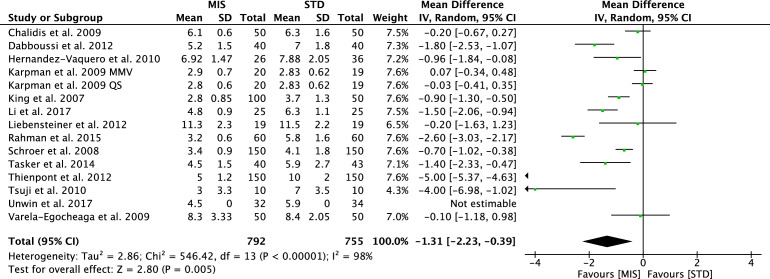
The traditional SIS approach allows a shorter surgical duration (MD − 15.51; CI 9.79–21.23; P < 0.0001, Fig. 3). The MIS group was associated with a shorter hospitalization length (MD − 1.31; CI − 2.23 to − 0.39; P = 0.005, Fig. 4), a lower total estimated blood loss (MD − 76.88; CI − 183.35–29.58; P = 0.006) and quicker time of straight-leg raise (MD − 1.47; CI − 2.89 to − 0.05; P = 0.04).
Fig. 3.
Forest plot of the comparison surgical duration
Fig. 4.
Forest plot of the comparison hospitalization length
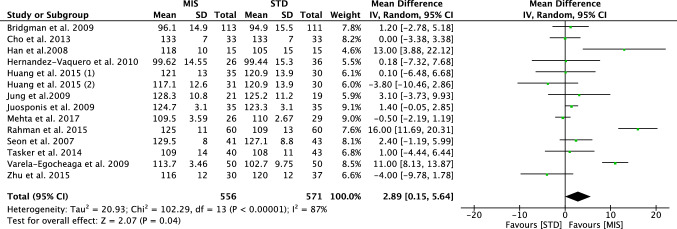
At a mean follow-up of 21.31 ± 24.3 months, greater values of ROM were evidenced in the MIS group (MD 2.89; CI − 0.15–5.64; P = 0.04, Fig. 5), flexion (MD 5.92; CI 3.26–8.57; P < 0.0001), greater values of KSS (MD 1.09; CI 0.55–1.64; P < 0.0001) and KSFS (MD 3.07; CI 1.08–7.21; P = 0.01).
Fig. 5.
Forest plot of the comparison range of motion
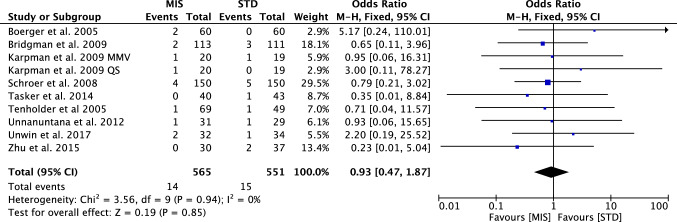
The visual analogic scale, the rate of anterior knee pain and revisions (Fig. 6) were similar between the two cohorts. Table 4 shows the main results of the meta-analyses, while Table 5 displayed the complications.
Fig. 6.
Forest plot of the comparison revision
Table 4.
Main results of the comparisons
| Outcome | Studies (n) | Knees (n) | MIS (mean ± SD) | SIS (mean ± SD) | Effect estimate, MD [95% CI] | P |
|---|---|---|---|---|---|---|
| Hospitalization length | 15 | 1547 | 5.10 ± 2.4 | 6.71 ± 2.3 | − 1.31 [− 2.23, − 0.39] | 0.005 |
| Surgical duration | 23 | 2077 | 86.97 ± 20.2 | 75.69 ± 14.3 | 15.51 [9.79, 21.23] | < 0.0001 |
| Total estimated blood loss | 19 | 1499 | 601.23 ± 197.8 | 680.14 ± 300.6 | − 76.88 [− 183.35, 29.58] | 0.006 |
| Straight-Leg Raise | 6 | 630 | 2.12 ± 0.8 | 3.77 ± 1.9 | − 1.47 [− 2.89, − 0.05] | 0.04 |
| ROM | 14 | 1127 | 117.06 ± 10.8 | 113.71 ± 11.8 | 2.89 [0.15, 5.64] | 0.04 |
| Flexion | 8 | 722 | 107.14 ± 11.6 | 104.79 ± 15.8 | 5.92 [3.26, 8.57] | < 0.0001 |
| KSS | 15 | 1411 | 89.69 ± 4.8 | 86.21 ± 5.5 | 1.09 [0.55, 1.64] | < 0.0001 |
| KSFS | 9 | 963 | 79.13 ± 3.5 | 75.41 ± 4.8 | 3.07 [− 1.08, 7.21] | 0.01 |
| VAS | 8 | 738 | 2.12 ± 0.6 | 2.62 ± 1.2 | − 9.25 [− 20.65, 2.14] | 0.1 |
Table 5.
Complications
| Outcome | Studies (n) | Knees (n) | MIS (events) | SIS (events) | Effect estimate, OR [95% CI] | P |
|---|---|---|---|---|---|---|
| Anterior knee pain (OR) | 2 | 169 | 21/258 | 14/249 | 3.54 [0.71, 17.55] | 0.1 |
| Revision surgery (OR) | 10 | 1116 | 14/565 | 15/551 | 0.93 [0.47, 1.87] | 0.9 |
Discussion
The main finding of the present meta-analysis is that MIS approaches may offer clinical and functional benefits over the conventional MPP SIS approach for TKA. Peri-operatively, these include a significantly shorter length of hospitalization and time to straight-leg raise, along with a reduction in total estimated blood loss. Overall, patients undergoing MIS TKA achieve greater ROM, flexion and KSS and KSFS scores, and the surgical procedure is shorter. Concerning complications, the two approaches yielded similar results.
MIS TKA procedures have been introduced to minimize quadriceps disruption, resulting in better quadriceps strength [19, 41, 44]. Furthermore, the shorter incision and limited knee arthrotomy, and avoidance of patellar eversion and dislocation and hyperflexion of the tibiofemoral joint, produce less damage to the muscles, collateral ligament, and posterior capsule. All these features may result in faster recovery [12, 16]. However, given to the difficulty in execution, the longer learning curve and the need for special instruments, MIS TKA has not become very popular [2, 36]. The instrumentation for MIS TKA necessitates special retractors and jigs (e.g., the sided cutting tools). These instruments require adequate technical training. The revised sided cutting tool allow the coronal and sagittal bony cuts in one step, while, with the traditional instrumentation, two bone cuts are necessary. To assist the surgeon, the use of mobile windows can facilitate exposure of knee surfaces, and adequately trained assistants have also been recommended [26, 33, 52]. In addition to the new surgical instrumentation, new implants designed specifically for MIS TKA (e.g., the uncemented tibial plateau with smaller keel) have been introduced into the market, along with specific recoated stems and modular implants. These implants are designed specifically for those situations with reduced visibility of the surgical field. Several companies are introducing new uncemented implants to avoid improper cementation because of the small field of vision of MIS TKA [45]. Moreover, for MIS TKA, navigation systems, along with patient-specific instrumentation, recently gained popularity [21, 37, 61]. However, despite noticeable improvements, there are still controversial, and the reliability and feasibility, cost-effectiveness and clinical advantages of these new tools and new implants is uncertain. This has discouraged many surgeons from performing minimally-invasive TKAs, and the MPP remains the most common approach for TKA.
The reduction in hospitalization time for MIS patients offers great potentials for cost- savings. Notwithstanding, MIS approaches require a long learning curve for the whole surgical team [1, 31]. Reduced visibility of anatomical landmarks, the number of surgical steps, and the need for different equipment play a role in extending the duration of surgery. Once surgeons are more familiar with the less invasive procedures, operating times do decrease [11, 26], and eventually no difference in surgical time are found after surgeons received adequate training.
The endpoint total estimated blood loss was evaluated under a random effect method, given the high grade of heterogeneity. This can be explained by the different protocols of tourniquet, drainages and antifibrinolytic agents used in the various studies. Thus, even though this endpoint resulted statistically significant in favour of the MIS group, this result must be interpreted with caution. The time to straight-leg raise is used to assess functional recovery of the quadriceps muscle after a TKA; the statistically significant reduction in time detected among the MIS group is noteworthy. The faster restoration of function of the extensor muscle mechanism may arise from to the limited knee arthrotomy and smaller incision in MIS TKA, together with the avoidance of patellar eversion. Reduced damage to soft tissues may also explain the statistically significant improvement of the analysed scores. The visual analogic scale for pain, even if not statistically significant, was remarkably lower in the MIS group. Similar consideration can be inferred also to the KSS and KSFS, which resulted statistically significant better outcomes in favour of the MIS group. A statistically significant improvement of joint motion was observed (ROM and flexion). Some studies found that MIS TKA resulted in an improvement of ROM and flexion in the early post-operative period, which disappeared after one week and three months [3, 32]. During TKA performed by SIS approach, the quadriceps tendons and muscles are incised and re-sutured, resulting in scar tissues and fibrosis, which can explain the reduced joint motion. However, evidences are lacking, and future studies should investigate and compare the trend of favourable joint motion in MIS over the time. This study encourages orthopaedic surgeons to consider MIS TKAs approaches, notwithstanding the difficulties that arise from the longer learning curve. In light of the present results, further studies should investigate the best approach for MIS TKA and establish with greater stringency what the correct indications for MIS TKA are.
Limitations
Given of the high overall heterogeneity, all comparisons were analysed under a random effect method. Moreover, the funnel plot detected a moderate risk of publication bias. Articles were compared regardless to the type of pre- and peri-operative protocols. The patient anatomical characteristics, time of tourniquet, use of antifibrinolytic agents and antibiotics administration, type of technique, type of implants, use of drainages and post-operative rehabilitation and antithrombotic protocols were source of major differences which could not be adjusted statistically. Limited follow-up times represent another important limitation of this study, resulting in unreliable data concerning long-term complications and implant survivorship. A lack of distinction between MIS approaches (QS, MMV, MSV, MMPP), a reflection of the available data, represent an important limitation of this study. This was necessary to improve the amount of pooling data for inclusion. Further studies are required to investigate the pros and cons of the various approaches separately when enough suitable studies will have been published. Another important limitation of this study is the number of analysed endpoints, which was limited by insufficient data in the literature which would allow for analysis of further endpoints. Computer-assisted TKA were not considered, and this may represent another limitation. Moreover, limitations in reported durations of follow-up prevents a more robust analysis of long-term benefits and risks. Given these limitations, results from the present study must be interpret with caution.
Strong points of the present work, on the other hand, are represented by the widespread nature of the literature search, along with the strict eligibility criteria, its methodological quality assessment, and good baseline comparability. This is crucial to provide more reliable and homogeneous results, leading to greater strength of scientific evidence.
Conclusion
MIS approaches may offer clinical and functional benefits over conventional SISI MPP approach for TKA. Peri-operatively, MIS patients experience lower total estimated blood loss and a reduction in hospitalization time. Post-operatively, MIS patients demonstrate improved joint function and other outcome scores during follow-up. Minimally invasive approaches for TKA involve a technically more complicated execution which requires a long learning curve for the whole surgical team. These results must be interpreted within the limitations of the present study.
Acknowledgements
We would like to thank Dr. Massimiliano Biagnini, PhD for his support in the statistical analyses.
Author contributions
FM: literature search, data extraction, methodological quality assessment, statistical analysis, paper writing; AB: literature search, data extraction, methodological quality assessment; JE: supervision; MT: supervision; NM: conception, supervision, revision.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study informed consent is not required.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Aglietti P, Baldini A, Giron F, Sensi L. Minimally invasive total knee arthroplasty: is it for everybody? HSS J. 2006;2:22–26. doi: 10.1007/s11420-005-0127-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aglietti P, Baldini A, Sensi L. Quadriceps-sparing versus mini-subvastus approach in total knee arthroplasty. Clin Orthop Relat Res. 2006;452:106–111. doi: 10.1097/01.blo.0000238789.51972.16. [DOI] [PubMed] [Google Scholar]
- 3.Alcelik I, Sukeik M, Pollock R, Misra A, Shah P, Armstrong P, et al. Comparison of the minimally invasive and standard medial parapatellar approaches for primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2012;20:2502–2512. doi: 10.1007/s00167-012-1944-3. [DOI] [PubMed] [Google Scholar]
- 4.Aslam MA, Sabir AB, Tiwari V, Abbas S, Tiwari A, Singh P. Approach to total knee replacement: a randomized double blind study between medial parapatellar and midvastus approach in the early postoperative period in asian population. J Knee Surg. 2017;30:793–797. doi: 10.1055/s-0036-1597978. [DOI] [PubMed] [Google Scholar]
- 5.Avci CC, Gulabi D, Erdem M, Kurnaz R, Gunes T, Bostan B. Minimal invasive midvastus versus standard parapatellar approach in total knee arthroplasty. Acta Orthop Traumatol Turc. 2013;47:1–7. doi: 10.3944/AOTT.2013.2801. [DOI] [PubMed] [Google Scholar]
- 6.Boerger TO, Aglietti P, Mondanelli N, Sensi L. Mini-subvastus versus medial parapatellar approach in total knee arthroplasty. Clin Orthop Relat Res. 2005;440:82–87. doi: 10.1097/01.blo.0000185755.09777.2d. [DOI] [PubMed] [Google Scholar]
- 7.Bridgman SA, Walley G, MacKenzie G, Clement D, Griffiths D, Maffulli N. Sub-vastus approach is more effective than a medial parapatellar approach in primary total knee arthroplasty: a randomized controlled trial. Knee. 2009;16:216–222. doi: 10.1016/j.knee.2008.11.012. [DOI] [PubMed] [Google Scholar]
- 8.Chalidis BE, Petsatodis G, Christodoulou AG, Christoforidis J, Papadopoulos PP, Pournaras J. Is obesity a contraindication for minimal invasive total knee replacement? A prospective randomized control trial. Obes Surg. 2010;20:1633–1641. doi: 10.1007/s11695-009-9968-6. [DOI] [PubMed] [Google Scholar]
- 9.Chiang H, Lee CC, Lin WP, Jiang CC. Comparison of quadriceps-sparing minimally invasive and medial parapatellar total knee arthroplasty: a 2-year follow-up study. J Formos Med Assoc. 2012;111:698–704. doi: 10.1016/j.jfma.2011.11.025. [DOI] [PubMed] [Google Scholar]
- 10.Cho KY, Kim KI, Umrani S, Kim SH. Better quadriceps recovery after minimally invasive total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2014;22:1759–1764. doi: 10.1007/s00167-013-2556-2. [DOI] [PubMed] [Google Scholar]
- 11.Chotanaphuti T, Ongnamthip P, Karnchanalerk K, Udombuathong P. Comparative study between 2 cm limited quadriceps exposure minimal invasive surgery and conventional total knee arthroplasty in quadriceps function: prospective randomized controlled trial. J Med Assoc Thai. 2008;91:203–207. [PubMed] [Google Scholar]
- 12.Cila E, Guzel V, Ozalay M, Tan J, Simsek SA, Kanatli U, et al. Subvastus versus medial parapatellar approach in total knee arthroplasty. Arch Orthop Trauma Surg. 2002;122:65–68. doi: 10.1007/s004020100319. [DOI] [PubMed] [Google Scholar]
- 13.Dabboussi N, Sakr M, Girard J, Fakih R. Minimally invasive total knee arthroplasty: a comparative study to the standard approach. N Am J Med Sci. 2012;4:81–85. doi: 10.4103/1947-2714.93381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dayton MR, Bade MJ, Muratore T, Shulman BC, Kohrt WM, Stevens-Lapsley JE. Minimally invasive total knee arthroplasty: surgical implications for recovery. J Knee Surg. 2013;26:195–201. doi: 10.1055/s-0032-1327449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Engh GA, Holt BT, Parks NL. A midvastus muscle-splitting approach for total knee arthroplasty. J Arthroplasty. 1997;12:322–331. doi: 10.1016/S0883-5403(97)90030-9. [DOI] [PubMed] [Google Scholar]
- 16.Engh GA, Parks NL. Surgical technique of the midvastus arthrotomy. Clin Orthop Relat Res. 1998 doi: 10.1097/00003086-199806000-00032270-274. [DOI] [PubMed] [Google Scholar]
- 17.Faure BT, Benjamin JB, Lindsey B, Volz RG, Schutte D. Comparison of the subvastus and paramedian surgical approaches in bilateral knee arthroplasty. J Arthroplasty. 1993;8:511–516. doi: 10.1016/S0883-5403(06)80216-0. [DOI] [PubMed] [Google Scholar]
- 18.Feczko P, Engelmann L, Arts JJ, Campbell D. Computer-assisted total knee arthroplasty using mini midvastus or medial parapatellar approach technique: a prospective, randomized, international multicentre trial. BMC Musculoskelet Disord. 2016;17:19. doi: 10.1186/s12891-016-0872-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Guy SP, Farndon MA, Conroy JL, Bennett C, Grainger AJ, London NJ. A prospective randomised study of minimally invasive midvastus total knee arthroplasty compared with standard total knee arthroplasty. Knee. 2012;19:866–871. doi: 10.1016/j.knee.2012.04.009. [DOI] [PubMed] [Google Scholar]
- 20.Han I, Seong SC, Lee S, Yoo JH, Lee MC. Simultaneous bilateral MIS-TKA results in faster functional recovery. Clin Orthop Relat Res. 2008;466:1449–1453. doi: 10.1007/s11999-008-0216-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hasegawa M, Miyazaki S, Yamaguchi T, Wakabayashi H, Sudo A. Comparison of midterm outcomes of minimally invasive computer-assisted vs minimally invasive jig-based total knee arthroplasty. J Arthroplasty. 2017;32:43–46. doi: 10.1016/j.arth.2016.07.005. [DOI] [PubMed] [Google Scholar]
- 22.Hernandez-Vaquero D, Noriega-Fernandez A, Suarez-Vazquez A. Total knee arthroplasties performed with a mini-incision or a standard incision. Similar results at six months follow-up. BMC Musculoskelet Disord. 2010;11:27. doi: 10.1186/1471-2474-11-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Howick J CI, Glasziou P, Greenhalgh T, Heneghan C, Liberati A, Moschetti I, Phillips B, Thornton H, Goddard O, Hodgkinson M (2011) The 2011 Oxford Levels of Evidence. Oxford Centre for Evidence-Based Medicine. https://www.cebm.net/index.aspx?o=5653
- 24.Huang AB, Wang HJ, Yu JK, Yang B, Ma D, Zhang JY. Optimal patellar alignment with minimally invasive approaches in total knee arthroplasty after a minimum five year follow-up. Int Orthop. 2016;40:487–492. doi: 10.1007/s00264-015-2896-2. [DOI] [PubMed] [Google Scholar]
- 25.Jung YB, Lee YS, Lee EY, Jung HJ, Nam CH. Comparison of the modified subvastus and medial parapatellar approaches in total knee arthroplasty. Int Orthop. 2009;33:419–423. doi: 10.1007/s00264-007-0510-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Juosponis R, Tarasevicius S, Smailys A, Kalesinskas RJ. Functional and radiological outcome after total knee replacement performed with mini-midvastus or conventional arthrotomy: controlled randomised trial. Int Orthop. 2009;33:1233–1237. doi: 10.1007/s00264-008-0630-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Karachalios T, Giotikas D, Roidis N, Poultsides L, Bargiotas K, Malizos KN. Total knee replacement performed with either a mini-midvastus or a standard approach: a prospective randomised clinical and radiological trial. J Bone Joint Surg Br. 2008;90:584–591. doi: 10.1302/0301-620X.90B5.20122. [DOI] [PubMed] [Google Scholar]
- 28.Karpman RR, Smith HL. Comparison of the early results of minimally invasive vs standard approaches to total knee arthroplasty: a prospective, randomized study. J Arthroplasty. 2009;24:681–688. doi: 10.1016/j.arth.2008.03.011. [DOI] [PubMed] [Google Scholar]
- 29.Kim JG, Lee SW, Ha JK, Choi HJ, Yang SJ, Lee MY. The effectiveness of minimally invasive total knee arthroplasty to preserve quadriceps strength: a randomized controlled trial. Knee. 2011;18:443–447. doi: 10.1016/j.knee.2010.08.008. [DOI] [PubMed] [Google Scholar]
- 30.Kim YH, Kim JS, Kim DY. Clinical outcome and rate of complications after primary total knee replacement performed with quadriceps-sparing or standard arthrotomy. J Bone Joint Surg Br. 2007;89:467–470. doi: 10.1302/0301-620X.89B4.18663. [DOI] [PubMed] [Google Scholar]
- 31.King J, Stamper DL, Schaad DC, Leopold SS. Minimally invasive total knee arthroplasty compared with traditional total knee arthroplasty. Assessment of the learning curve and the postoperative recuperative period. J Bone Joint Surg Am. 2007;89:1497–1503. doi: 10.2106/00004623-200707000-00013. [DOI] [PubMed] [Google Scholar]
- 32.Kolisek FR, Bonutti PM, Hozack WJ, Purtill J, Sharkey PF, Zelicof SB, et al. Clinical experience using a minimally invasive surgical approach for total knee arthroplasty: early results of a prospective randomized study compared to a standard approach. J Arthroplasty. 2007;22:8–13. doi: 10.1016/j.arth.2006.06.004. [DOI] [PubMed] [Google Scholar]
- 33.Laskin RS, Beksac B, Phongjunakorn A, Pittors K, Davis J, Shim JC, et al. Minimally invasive total knee replacement through a mini-midvastus incision: an outcome study. Clin Orthop Relat Res. 2004 doi: 10.1097/01.blo.0000148582.86102.4774-81. [DOI] [PubMed] [Google Scholar]
- 34.Li Z, Cheng W, Sun L, Yao Y, Cao Q, Ye S, et al. Mini-subvastus versus medial parapatellar approach for total knee arthroplasty: a prospective randomized controlled study. Int Orthop. 2018;42:543–549. doi: 10.1007/s00264-017-3703-z. [DOI] [PubMed] [Google Scholar]
- 35.Liebensteiner MC, Krismer M, Koller A, Semenitz B, Mayr E. Does minimally invasive total knee arthroplasty improve isokinetic torque? Clin Orthop Relat Res. 2012;470:3233–3239. doi: 10.1007/s11999-012-2545-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Liu Z, Yang H. Comparison of the minimally invasive and standard medial parapatellar approaches for total knee arthroplasty: systematic review and meta-analysis. J Int Med Res. 2011;39:1607–1617. doi: 10.1177/147323001103900503. [DOI] [PubMed] [Google Scholar]
- 37.Luring C, Beckmann J, Haibock P, Perlick L, Grifka J, Tingart M. Minimal invasive and computer assisted total knee replacement compared with the conventional technique: a prospective, randomised trial. Knee Surg Sports Traumatol Arthrosc. 2008;16:928–934. doi: 10.1007/s00167-008-0582-2. [DOI] [PubMed] [Google Scholar]
- 38.Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003;83:713–721. doi: 10.1093/ptj/83.8.713. [DOI] [PubMed] [Google Scholar]
- 39.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mehta N, Bhat MS, Goyal A, Mishra P, Joshi D, et al. Quadriceps sparing (subvastus/midvastus) approach versus the conventional medial parapatellar approach in primary knee arthroplasty. J Arthr Joint Surg. 2017;4(1):15–20. [Google Scholar]
- 41.Nestor BJ, Toulson CE, Backus SI, Lyman SL, Foote KL, Windsor RE. Mini-midvastus vs standard medial parapatellar approach: a prospective, randomized, double-blinded study in patients undergoing bilateral total knee arthroplasty. J Arthroplasty. 2010;25:5–11. doi: 10.1016/j.arth.2010.04.003. [DOI] [PubMed] [Google Scholar]
- 42.Noble PC, Scuderi GR, Brekke AC, Sikorskii A, Benjamin JB, Lonner JH, et al. Development of a new Knee Society scoring system. Clin Orthop Relat Res. 2012;470:20–32. doi: 10.1007/s11999-011-2152-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Obaid Ur R, Amin MS. Less invasive versus standard total knee replacement: Comparison of early outcome. J Pak Med Assoc. 2015;65:S82–86. [PubMed] [Google Scholar]
- 44.Pan WM, Li XG, Tang TS, Qian ZL, Zhang Q, Zhang CM. Mini-subvastus versus a standard approach in total knee arthroplasty: a prospective, randomized, controlled study. J Int Med Res. 2010;38:890–900. doi: 10.1177/147323001003800315. [DOI] [PubMed] [Google Scholar]
- 45.Picard F, Deakin A, Balasubramanian N, Gregori A. Minimally invasive total knee replacement: techniques and results. Eur J Orthop Surg Traumatol. 2018;28:781–791. doi: 10.1007/s00590-018-2164-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Schroer WC, Diesfeld PJ, Reedy ME, LeMarr AR. Mini-subvastus approach for total knee arthroplasty. J Arthroplasty. 2008;23:19–25. doi: 10.1016/j.arth.2006.12.100. [DOI] [PubMed] [Google Scholar]
- 47.Seon JK, Song EK, Yoon TR, Park SJ, Bae BH, Cho SG. Comparison of functional results with navigation-assisted minimally invasive and conventional techniques in bilateral total knee arthroplasty. Comput Aided Surg. 2007;12:189–193. doi: 10.3109/10929080701311861. [DOI] [PubMed] [Google Scholar]
- 48.Stevens-Lapsley JE, Bade MJ, Shulman BC, Kohrt WM, Dayton MR. Minimally invasive total knee arthroplasty improves early knee strength but not functional performance: a randomized controlled trial. J Arthroplasty. 2012;27(1812–1819):e1812. doi: 10.1016/j.arth.2012.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tasker A, Hassaballa M, Murray J, Lancaster S, Artz N, Harries W, et al. Minimally invasive total knee arthroplasty; a pragmatic randomised controlled trial reporting outcomes up to 2 year follow up. Knee. 2014;21:189–193. doi: 10.1016/j.knee.2013.07.010. [DOI] [PubMed] [Google Scholar]
- 50.Tenholder M, Clarke HD, Scuderi GR. Minimal-incision total knee arthroplasty: the early clinical experience. Clin Orthop Relat Res. 2005;440:67–76. doi: 10.1097/01.blo.0000185450.89364.10. [DOI] [PubMed] [Google Scholar]
- 51.Thienpont E. Faster recovery after minimally invasive surgery in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2013;21:2412–2417. doi: 10.1007/s00167-012-1978-6. [DOI] [PubMed] [Google Scholar]
- 52.Tria AJ, Scuderi GR. Minimally invasive knee arthroplasty: an overview. World J Orthop. 2015;6:804–811. doi: 10.5312/wjo.v6.i10.804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Tsuji S, Tomita T, Fujii M, Laskin RS, Yoshikawa H, Sugamoto K. Is minimally invasive surgery-total knee arthroplasty truly less invasive than standard total knee arthroplasty? A quantitative evaluation. J Arthroplasty. 2010;25:970–976. doi: 10.1016/j.arth.2009.06.016. [DOI] [PubMed] [Google Scholar]
- 54.Unnanuntana A, Pornrattanamaneewong C, Mow CS. Minimally invasive and standard total knee arthroplasty result in similar clinical outcomes at a minimum of five-year follow-up. J Med Assoc Thai. 2012;95(Suppl 9):S29–35. [PubMed] [Google Scholar]
- 55.Unwin O, Hassaballa M, Murray J, Harries W, Porteous A. Minimally invasive surgery (MIS) for total knee replacement; medium term results with minimum five year follow-up. Knee. 2017;24:454–459. doi: 10.1016/j.knee.2017.01.010. [DOI] [PubMed] [Google Scholar]
- 56.Varela-Egocheaga JR, Iglesias-Colao R, Suarez-Suarez MA, Fernandez-Villan M, Gonzalez-Sastre V, Murcia-Mazon A. Minimally invasive osteosynthesis in stable trochanteric fractures: a comparative study between Gotfried percutaneous compression plate and Gamma 3 intramedullary nail. Arch Orthop Trauma Surg. 2009;129:1401–1407. doi: 10.1007/s00402-009-0955-0. [DOI] [PubMed] [Google Scholar]
- 57.Watanabe T, Muneta T, Ishizuki M. Is a minimally invasive approach superior to a conventional approach for total knee arthroplasty? Early outcome and 2- to 4-year follow-up. J Orthop Sci. 2009;14:589–595. doi: 10.1007/s00776-009-1383-2. [DOI] [PubMed] [Google Scholar]
- 58.Wegrzyn J, Parratte S, Coleman-Wood K, Kaufman KR, Pagnano MW. The John Insall award: no benefit of minimally invasive TKA on gait and strength outcomes: a randomized controlled trial. Clin Orthop Relat Res. 2013;471:46–55. doi: 10.1007/s11999-012-2486-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.White RE Jr., Allman JK, Trauger JA, Dales BH (1999) Clinical comparison of the midvastus and medial parapatellar surgical approaches. Clin Orthop Relat Res 117–122 [PubMed]
- 60.Wulker N, Lambermont JP, Sacchetti L, Lazaro JG, Nardi J. A prospective randomized study of minimally invasive total knee arthroplasty compared with conventional surgery. J Bone Joint Surg Am. 2010;92:1584–1590. doi: 10.2106/JBJS.H.01070. [DOI] [PubMed] [Google Scholar]
- 61.Zhu M, Ang CL, Chong HC, Yeo SJ (2018) Computer-assisted minimally invasive total knee arthroplasty compared with conventional total knee arthroplasty: a prospective nine-year follow-up. Bone Joint J 98 [DOI] [PubMed]
- 62.Zhu M, Ang CL, Yeo SJ, Lo NN, Chia SL, Chong HC. Minimally invasive computer-assisted total knee arthroplasty compared with conventional total knee arthroplasty: a prospective 9-year follow-up. J Arthroplasty. 2016;31:1000–1004. doi: 10.1016/j.arth.2015.11.023. [DOI] [PubMed] [Google Scholar]